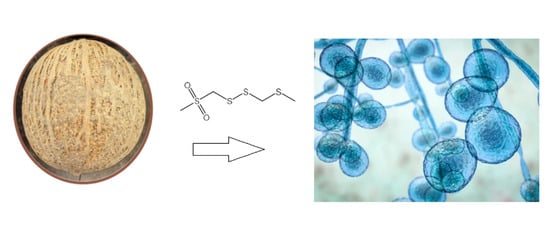
The Garlic Tree of Borneo, Scorodocarpus borneensis (Baill.) Becc. (Olacaceae): Potential Utilization in Pharmaceutical, Nutraceutical, and Functional Cosmetic Industries
Abstract
:1. Introduction
2. Methods
3. Results
3.1. Taxonomy, Habitat, Distribution, Ecology, and Botanical Description
3.2. Medicinal Uses
3.3. Antibacterial and Antifungal Activity of Extracts
| Extract/Secondary Metabolites | Activities In Vitro | References |
|---|---|---|
| Petroleum ether extract of seeds | Bacillus cereus, IZD = 25 mm | [25] |
| Pseudomonas aeruginosa, IZD = 50 mm | [25] | |
| Candida albicans, IZD = 19.2 mm | [25] | |
| Aspergillus ochraceus, IZD = 25 mm | [25] | |
| n-hexane extract of seeds | Mouse lymphocytic leukemia cells, IC50 = 15.3 μg/mL | [33] |
| DPPH, IC50 = 60 ppm | [55] | |
| Methanol extract of seeds | DPPH, IC50 = 86.2 ppm | [55] |
| Ethanol extract of seeds | DPPH, IC50 = 14.5 ppm | [55] |
| n-Hexane extract of bark | C. curvignathus, LC50 = 0.01% | [13] |
| Ethyl acetate extract of bark | C. curvignathus, LC50 = 0.02% | [13] |
| Brine shrimps, LC50 = 31.1 ppm | [34] | |
| DPPH, IC50 = 55.5 ppm | [24] | |
| Methanol extract of bark | DPPH, IC50 = 52.4 ppm | [24] |
| Methanol extract from leaves | DPPH, IC50 = 36.8 ppm | [24] |
| Essential oil of leaves | DPPH, IC50 = 715.9 µg/mL | [52] |
| (1) | S. aureus, MIC = 12.5 μg/mL | [26,27,28,29] |
| Micrococcus luteus, MIC = 25 μg/mL | [26,27,28,29] | |
| Bacillus subtilis, MIC = 12.5 μg/mL | [26,27,28,29] | |
| Mycobacterium smegmatis, MIC = 12.5 μg/mL | [26,27,28,29] | |
| Escherichia coli, MIC = 12.5 μg/mL | [26,27,28,29] | |
| Candida albicans, MIC = 25 μg/mL | [26,27,28,29] | |
| Saccharomyces cerevisae, MIC = 25 μg/mL | [26,27,28,29] | |
| Mucor racemosus, MIC = 12.5 μg/mL | [26,27,28,29] | |
| Aspergillus niger, MIC = 25 μg/mL | [26,27,28,29] | |
| Platelets aggregation, IC50 = 2.3 × 10−4 M | [32] | |
| (2) | Platelets aggregation, IC50 = 2.9 × 10−4 M | [32] |
| (3) | Staphylococcus aureus, MIC = 50 μg/mL | [26,27,28,29] |
| Micrococcus luteus, MIC = 50 μg/mL | [26,27,28,29] | |
| Bacillus subtilis, MIC = 12.5 μg/mL | [26,27,28,29] | |
| Mycobacterium smegmatis, MIC = 50 μg/mL | [26,27,28,29] | |
| Escherichia coli, MIC = 50 μg/mL | [26,27,28,29] | |
| Candida albicans, MIC = 50 μg/mL | [26,27,28,29] | |
| Saccharomyces cerevisae, MIC = 12.5 μg/mL | [26,27,28,29] | |
| Mucor racemosus, MIC = 25 μg/mL | [26,27,28,29] | |
| Aspergillus niger, MIC = 12.5 μg/mL | [26,27,28,29] | |
| Bacillus cereus, MM = 25 mg/disc | [25] | |
| Pseudomonas aeruginosa, MM = 25 mg/disc | [25] | |
| Aspergillus ochraceus, MM = 12.5 mg/disc | [25] | |
| Saccharomyces lipolytica, MM =12.5 mg/disc | [25] | |
| Candida lipolytica, MM = 12.5 mg/disc | [25] | |
| Penicillium sp., MM = 20 mg/disc | [25] | |
| Acremonium sp., MM = 1 mg/disc | [25] | |
| Microsporium sp., MM = 0.5 mg/disc | [25] | |
| Pseudoscaellia boedes, MM = 22 mg/disc | [25] | |
| Platelets aggregation, IC50 = 0.4 × 10−4 M | [32] | |
| T-Lymphoblastic leukemia cells, IC50 = 3 µg/mL | [25] | |
| (4) | Platelets aggregation, IC50 = 1.2 × 10−4 M | [32] |
| (7) | T-Lymphoblastic leukemia cells, IC50 = 24 µg/mL | [25] |
| (9) | Mouse lymphocytic leukemia cells, IC50 = 1.1 µg/mL | [33] |
| DPPH, IC50 = 51.1 ppm | [56] | |
| (11) | Mouse lymphocytic leukemia cells, IC50 = 1.7 µg/mL | [56] |
| DPPH, IC50 = 42.2 ppm | [56] | |
| (12) | Bacillus cereus, IZD = 12 mm | [25] |
| Pseudomonas aeruginosa, IZD = 11 mm | [25] | |
| T-Lymphoblastic leukemia cells, IC50 = 0.3–1 µg/mL | [25] | |
| (13) | Brine shrimps, LC50 = 42.3 ppm | [51] |
3.4. Cytotoxicity and Brine Shrimp Toxicity of Extracts
3.5. Termiticidal Activity of Extracts
3.6. Radical-Scavenging Activity of Extracts
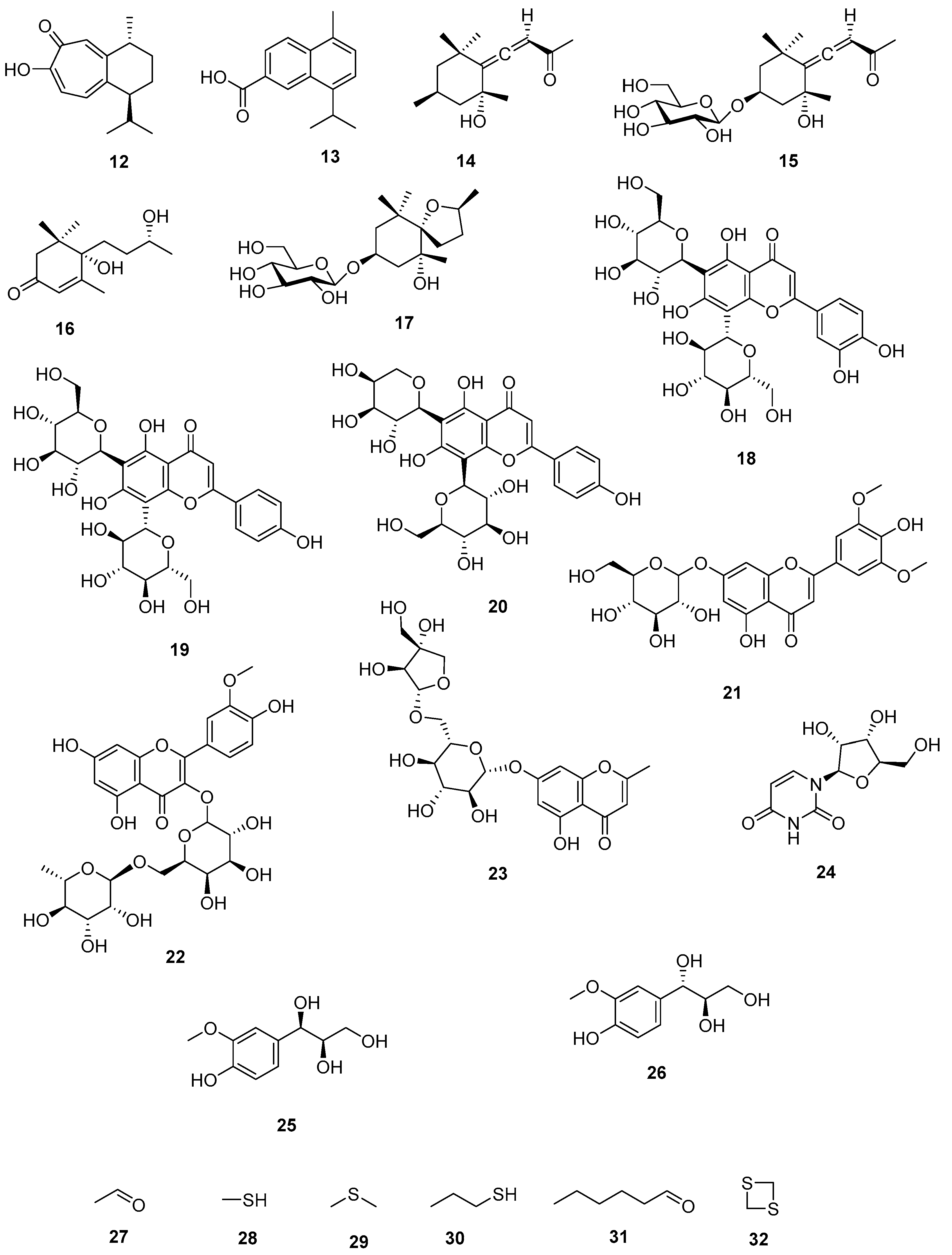
3.7. Organosulfur Compounds
3.8. Indole Alkaloids
3.9. Sesquiterpenes
3.10. Megastigmanes
3.11. Flavonoid Glycosides
3.12. Miscellaneous
3.13. Toxicity, Side Effects, and Drug Interaction
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kulip, J.; Fan, L.N.; Manshoor, N.; Julius, A.; Said, I.M.; Gisil, J.; Joseph, J.A.; Tukin, W.F. Medicinal plants in Maliau Basin, Sabah, Malaysia. J. Trop. Biol. Conserv. 2010, 6, 21–33. [Google Scholar]
- Fuller, R.W.; Bokesch, H.R.; Gustafson, K.R.; McKee, T.C.; Cardellina, I.I.J.H.; McMahon, J.B.; Cragg, G.M.; Soejarto, D.D.; Boyd, M.R. HIV-inhibitory coumarins from latex of the tropical rainforest tree Calophyllum teysmannii var. inophylloide. Bioorganic Med. Chem. Lett. 1994, 4, 1961–1964. [Google Scholar] [CrossRef]
- Boyer, E.W.; Babu, K.M.; Adkins, J.E.; McCurdy, C.R.; Halpern, J.H. Self-treatment of opioid withdrawal using kratom (Mitragynia speciosa korth). Addiction 2008, 103, 1048–1050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norhayati, M.N.; George, A.; Nik Hazlina, N.H.; Azidah, A.K.; Intan Idiana, H.; Law, K.S.; Shaiful Bahari, I.; Wan Zahiruddin, W.M.; Liske, E.; Azreena, A. Efficacy and safety of Labisia pumila var alata water extract among pre-and postmenopausal women. J. Med. Food. 2014, 17, 929–938. [Google Scholar] [CrossRef]
- Faisal, G.G.; Alahmad, B.E.; Mustafa, N.S.; Najmuldeen, G.F.; Althunibat, O.; Azzubaidi, M.S. Histopathological effects of Eurycoma longifolia Jack extract (Tongkat Ali) on the prostate of rats. J. Asian Sci. Res. 2013, 3, 843–851. [Google Scholar]
- Fitzherbert, E.B.; Struebig, M.J.; Morel, A.; Danielsen FBrühl, C.A.; Donald, P.F.; Phalan, B. How will oil palm expansion affect biodiversity? Trends Ecol. Evol. 2008, 23, 538–545. [Google Scholar] [CrossRef]
- Holmes, A.H.; Moore, L.S.; Sundsfjord, A.; Steinbakk, M.; Regmi, S.; Karkey, A.; Guerin, P.J.; Piddock, L.J. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet 2016, 387, 176–187. [Google Scholar]
- Hu, S.; Zhu, F.; Jiang, W.; Wang, Y.; Quan, Y.; Zhang, G.; Gu, F.; Yang, Y. Retrospective analysis of the clinical characteristics of Candida auris infection worldwide from 2009 to 2020. Front. Microbiol. 2021, 12, 658329. [Google Scholar] [CrossRef]
- Álvarez-Pérez, S.; García, M.E.; Anega, B.; Blanco, J.L. Antifungal Resistance in Animal Medicine: Current State and Future Challenges. In Fungal Diseases in Animals; Springer: Cham, Switzerland, 2021; pp. 163–179. [Google Scholar]
- Lamb, C.J.; Ryals, J.A.; Ward, E.R.; Dixon, R.A. Emerging strategies for enhancing crop resistance to microbial pathogens. Bio/technology 1992, 10, 1436–1445. [Google Scholar]
- Walsh, T.K.; Heckel, D.G.; Wu, Y.; Downes, S.; Gordon, K.H.J.; Oakeshott, J.G. Determinants of insecticide resistance evolution: Comparative analysis among heliothines. Annu. Rev. Entomol. 2022, 67, 387–406. [Google Scholar] [CrossRef]
- Sudrajat, S.; Kustiawan, W.; Mardji, D.; Kusuma, I.R. Chemical composition and termicidal activity of Scorodocarpus borneensis Becc. bark extracts. J. Adv. Sci. Res. 2018, 9, 24–30. [Google Scholar]
- Smith, T.; Majid, F.; Eckl, V.; Reynolds, C.M. Herbal supplement sales in US increase by record-breaking 17.3% in 2020. HerbalGram 2021, 131, 52–65. [Google Scholar]
- Angka, L.; Spagnuolo, P.A. From food to clinical medicine—Nutraceuticals as clinical therapeutics for hematological malignancies. Curr. Opin. Food Sci. 2015, 4, 7–12. [Google Scholar] [CrossRef]
- Wiart, C. Medicinal Plants of Southeast Asia, 2nd ed.; Prentice Hall: Hoboken, NJ, USA, 2002. [Google Scholar]
- Wiart, C. Medicinal Plants of the Asia-Pacific: Drugs for the Future? World Scientific Publishing Co., Pte. Ltd.: London, UK, 2006. [Google Scholar]
- Wiart, C. Medicinal Plants of Asia and the Pacific; CRC Press: Boca Raton, FL, USA, 2006. [Google Scholar]
- Wiart, C. Ethnopharmacology of Medicinal Plants: Asia and the Pacific; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Wiart, C. Medicinal Plants in the Asia Pacific for Zoonotic Pandemics: Family Zygophyllaceae to Salvadoraceae; CRC Press: Boca Raton, FL, USA, 2021. [Google Scholar]
- Soepadmo, E.; Wong, K.M. Tree Flora of Sabah and Sarawak; Forest Research Institute of Malaysia: Kuala Lumpur, Malaysia; Ampang Press Sdn. Bhd.: Kuala Lumpur, Malaysia, 1995. [Google Scholar]
- Kodoh, J. Surveys of non-timber forest products traded in tamu, Sabah, Malaysia. Sepilok Bull. 2005, 3, 27–36. [Google Scholar]
- Kustiawan, P.M.; Siregar, K.A.A.K.; Saleh, L.O.; Batistuta, M.A.; Setiawan, I.M. A review of botanical characteristics, chemical composition, pharmacological activity and use of Scorodocarpus borneensis. Biointerface Res. Appl. Chem. 2021, 12, 8324–8334. [Google Scholar]
- Dewi, Y.S.K.; Simamora, C.J.K.; Fadly, D. Antioxidant and antimicrobial activities of methanolic extracts of Scorodocarpus borneensis Becc. Syst. Rev. Pharm. 2020, 11, 246–252. [Google Scholar]
- Heriyanto, N.M.; Garsetiasih, R. Potensi pohon kulim (Scorodocarpus borneensis Becc.) di kelompok hutan Gelawan Kampar, Riau. Bul. Plasma Nutfah 2004, 10, 37–42. [Google Scholar] [CrossRef] [Green Version]
- Wiart, C. Antimicrobial and Cytotoxic Compounds of Scorodocarpus borneensis (Olacaceae) and Glycosmis calcicola (Rutaceae). Ph.D. Thesis, Universiti Putra Malaysia, Kuala Lumpur, Malaysia, 2001. [Google Scholar]
- Kubota, K.; Matsumoto, M.; Ueda, M.; Kobayashi, A. New antimicrobial compound from Scorodocarpus borneensis Becc. Biosci. Biotechnol. Biochem. 1994, 58, 430–431. [Google Scholar] [CrossRef] [Green Version]
- Kubota, K.; Kobayashi, A. Sulfur compounds in wood garlic (Scorodocarpus borneensis Becc.) as versatile food components. In Sulfur Compounds in Foods; ACS Symposium Series, No. 564; American Chemical Society: Washington, DC, USA, 1994; pp. 238–246. [Google Scholar]
- Kubota, K.; Ohhira, S.; Kobayashi, A. Identification and antimicrobial activity of the volatile flavor constituents from Scorodocarpus borneensis Becc. Biosci. Biotechnol. Biochem. 1994, 58, 644–646. [Google Scholar] [CrossRef] [Green Version]
- Lim, H.; Kubota, K.; Kobayashi, A.; Sugawara, F. Sulfur-containing compounds from Scorodocarpus borneensis and their antimicrobial activity. Phytochemistry 1998, 48, 787–790. [Google Scholar] [CrossRef]
- Akisue, M.; Wasicky, R.; Akisue, R.; De Oliveira, F. Gallesia integrifolia (Sprengel) harms-essential oil of leaves. Rev. Farm. Bioquímica Univ. Sao Paulo 1984, 20, 145–147. [Google Scholar]
- Kubota, K.; Hirayama, H.; Sato, Y.; Kobayashi, A.; Sugawara, F. Amino acid precursors of the garlic-like odour in Scorodocarpus borneensis. Phytochemistry 1998, 49, 99–102. [Google Scholar] [CrossRef]
- Lim, H.; Kubota, K.; Kobayashi, A.; Seki, T.; Ariga, T. Inhibitory effect of sulfur-containing compounds in Scorodocarpus borneensis Becc. on the aggregation of rabbit platelets. Biosci. Biotechnol. Biochem. 1999, 63, 298–301. [Google Scholar] [CrossRef] [Green Version]
- Kartika, R.; Bustanussalam, B.; Simanjuntak, P. Identification of cadalene-β-carboxylic acid from barks of bawang hutan (Scorodocarpus borneensis Becc.). Ann. Bogor. 2012, 16, 19–22. [Google Scholar]
- Kadir, R.; Hassan, B. Toxicity and repellent effects of wood extractives of five Malaysian wood species on Asian subterranean termite Coptotermes gestroi Wasmann. Eur. J. Wood Prod. 2020, 78, 1249–1262. [Google Scholar] [CrossRef]
- Kim, M.J.; Jeong, S.M.; Kang, B.K. Anti-inflammatory effects of grasshopper ketone from Sargassum fulvellum ethanol extract on lipopolysaccharide-induced inflammatory responses in RAW 264.7 cells. J. Microbiol. Biotechnol. 2019, 9, 820–826. [Google Scholar] [CrossRef]
- Kato-Noguchi, H.; Tamura, K.; Sasaki, H.; Suenaga, K. Identification of two phytotoxins, blumenol A and grasshopper ketone, in the allelopathic Japanese rice variety Awaakamai. J. Plant Physiol. 2012, 169, 682–685. [Google Scholar] [CrossRef]
- Tseng, M.H.; Kuo, Y.H.; Chen, Y.M.; Chou, C.H. Allelopathic potential of Macaranga tanarius (L.). Muell.—Arg. J. Chem. Ecol. 2003, 29, 1269–1286. [Google Scholar] [CrossRef]
- Basile, A.; Giordano, S.; López-Sáez, J.A.; Cobianchi, R.C. Antibacterial activity of pure flavonoids isolated from mosses. Phytochemistry 1999, 52, 1479–1482. [Google Scholar] [CrossRef]
- Islam, M.N.; Ishita, I.J.; Jung, H.A.; Choi, J.S. Vicenin 2 isolated from Artemisia capillaris exhibited potent anti-glycation properties. Food Chem. Toxicol. 2014, 69, 55–62. [Google Scholar] [CrossRef]
- Marrassini, C.; Davicino, R.; Acevedo, C.; Anesini, C.; Gorzalczany, S.; Ferraro, G. Vicenin-2, a potential anti-inflammatory constituent of Urtica circularis. J. Nat. Prod. 2011, 74, 1503–1507. [Google Scholar] [CrossRef]
- Tan, W.S.; Arulselvan, P.; Ng, S.F.; Mat Taib, C.N.; Sarian, M.N.; Fakurazi, S. Improvement of diabetic wound healing by topical application of vicenin-2 hydrocolloid film on Sprague Dawley rats. BMC 2019, 19, 20. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhao, Q.; Liu, T.; Zhao, H.; Wang, R.; Li, H.; Zhang, Y.; Shan, L.; He, B.; Wang, X.; et al. Effect of vicenin-2 on ovariectomy-induced osteoporosis in rats. Biomed. Pharmacother. 2020, 129, 10474. [Google Scholar] [CrossRef]
- Nagaprashantha, L.D.; Vatsyayan, R.; Singhal, J.; Fast, S.; Roby, R.; Awasthi, S.; Singhal, S.S. Anti-cancer effects of novel flavonoid vicenin-2 as a single agent and in synergistic combination with docetaxel in prostate cancer. Biochem. Pharmacol. 2011, 82, 1100–1109. [Google Scholar] [CrossRef] [Green Version]
- Yang, D.; Zhang, X.; Zhang, W.; Rengarajan, T. Vicenin-2 inhibits Wnt/β-catenin signaling and induces apoptosis in HT-29 human colon cancer cell line. Drug Des. Dev. Ther. 2018, 56, 1303–1310. [Google Scholar] [CrossRef] [Green Version]
- Hooper, A.M.; Tsanuo, M.K.; Chamberlain, K.; Tittcomb, K.; Scholes, J.; Hassanali, A.; Khan, Z.R.; Pickett, J.A. Isoschaftoside, a C-glycosylflavonoid from Desmodium uncinatum root exudate, is an allelochemical against the development of Striga. Phytochemistry 2010, 71, 904–908. [Google Scholar] [CrossRef]
- Su, Y.; Kang, Y.; Yi, J.; Lin, Q.; Zhang, C.; Lin, Z.; Yan, Z.; Qu, J.; Liu, J. Isoschaftoside reverses nonalcoholic fatty liver disease via activating autophagy in vivo and in vitro. eCAM 2022, 12, 135. [Google Scholar] [CrossRef]
- Gomes, A.C.C.; Sampaio, L.D.S.; Silva, P.A.D.; Lamas, M.E.; Sakuragui, C.M.; Barreto Junior, C.B.; Simas, N.K.; Kuster, R.M. In vitro effect of isoschaftoside isolated from Syngonium podophyllum on pig kidney Na+, K+-ATPase. Química Nova 2014, 37, 1606–1609. [Google Scholar]
- Boubaker, J.; Sghaier, M.B.; Skandrani, I.; Ghedira, K.; Chekir-Ghedira, L. Isorhamnetin 3-O-robinobioside from Nitraria retusa leaves enhance antioxidant and antigenotoxic activity in human chronic myelogenous leukemia cell line K562. BMC 2012, 12, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ajaghaku, D.L.; Akah, P.A.; Ilodigwe, E.E.; Nduka, S.O.; Osonwa, U.E.; Okoye, F.B.C. Upregulation of CD4+ T-lymphocytes by isomeric mixture of quercetin-3-O-rutinoside and quercetin-3-o-robinobioside isolated from Millettia aboensis. Immunol. Investig. 2018, 47, 372–388. [Google Scholar] [CrossRef] [PubMed]
- Brochado, C.D.O.; Almeida, A.P.D.; Barreto, B.P.; Costa, L.P.; Ribeiro, L.S.; Pereira, R.L.D.C.; Koatz, V.L.G.; Costa, S.S. Flavonol robinobiosides and rutinosides from Alternanthera brasiliana (Amaranthaceae) and their effects on lymphocyte proliferation in vitro. J. Braz. Chem. Soc. 2003, 14, 449–451. [Google Scholar] [CrossRef]
- Kuspradini, H.; Sinta Putri, A.; Edi Sukaton, E.; Tohru Mitsunaga, T. Bioactivity of essential oils from leaves of Dryobalanops lanceolata, Cinnamomum burmannii, Cananga odorata and Scorodocarpus borneensis. Agric. Sci. Procedia 2016, 9, 411–418. [Google Scholar] [CrossRef] [Green Version]
- Kuspradini, H.; Egra, S.; Wulandari, I.; Putri, A.S. Chemical composition and bioactivity of essential oil from the leaves of Scorodocarpus borneensis Becc. (Olacaceae) grown in Indonesia. Asia Life Sci. 2018, 27, 343–353. [Google Scholar]
- Wahyuni, T.S.; Permanasari, A.A.; Widyawaruyanti, A.; Hotta, H.; Aoki-Utsubo, C.; Hafid, A.F. Antiviral activity of Indonesian medicinal plants against hepatitis B virus. Pharmacogn. J. 2020, 12, 1108–1114. [Google Scholar] [CrossRef]
- Sudrajat, S.; Kartika, R.; Kustiawan, W. Analysis phytochemical compounds of ethyl acetate extract garlic tree, Scorodocarpus borneensis Becc. as a source of bioactive ingredients. Int. J. Sci. Technol. Res. 2019, 8, 183–186. [Google Scholar]
- Dewi, Y.S.; Purwayantie, P. Phytochemical and antioxidant activity from fruits of Kulim (Scorodocarpus borneensis Becc.). In Proceedings of the Second International on Food and Agriculture, Bali, Indonesia, 2–3 November 2019; Volume 2, pp. 519–524. [Google Scholar]
- Kartika, R.; Barus, T.; Surbakti, R.; Simanjuntak, P. Structure characterization of alkaloid scorodocarpines derivative from fruits of Scorodocarpus borneensis Becc. (Olacaceae). Asian J. Chem. 2014, 26, 6047–6049. [Google Scholar] [CrossRef]
- Jacob, C. A scent of therapy: Pharmacological implications of natural products containing redox-active sulfur atoms. Nat. Prod. Rep. 2006, 23, 851–863. [Google Scholar] [CrossRef]
- Shukla, Y.; Kalra, N. Cancer chemoprevention with garlic and its constituents. Cancer Lett. 2007, 247, 167–181. [Google Scholar] [CrossRef]
- Wiart, C.; Martin, M.T.; Awang, K.; Hue, N.; Serani, L.; Laprévote, O.; Païs, M.; Rahmani, M. Sesquiterpenes and alkaloids from Scorodocarpus borneensis. Phytochemistry 2001, 58, 653–656. [Google Scholar] [CrossRef]
- Coowar, D.; Bouissac, J.; Hanbali, M.; Paschaki, M.; Mohier, E.; Luu, B. Effects of indole fatty alcohols on the differentiation of neural stem cell derived neurospheres. J. Med. Chem. 2004, 47, 6270–6282. [Google Scholar] [CrossRef]
- Kang, B.K.; Kim, M.J.; Ahn, D.H. In vivo and in vitro inhibitory activity of an ethanolic extract of Sargassum fulvellum and its component grasshopper ketone on atopic dermatitis. Int. Immunopharmacol. 2016, 40, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Abe, F.; Yamauchi, T. Megastigmanes and flavonoids from the leaves of Scorodocarpus borneensis. Phytochemistry 1993, 33, 1499–1501. [Google Scholar] [CrossRef]


| SM | PP | Activities In Vitro | References |
|---|---|---|---|
| (1) | Seeds | Antibacterial, antifungal | [26,27,28,29,30,31] |
| Platelet aggregation inhibitor | [32] | ||
| (2) | Seeds | Platelet aggregation inhibitor | [32] |
| (3) | Seeds | Antibacterial, antifungal | [25] |
| Platelet aggregation inhibitor | [32] | ||
| Cytotoxic | [25] | ||
| (4) | Seeds | Platelet aggregation inhibitor | [32] |
| (7) | Seeds | Cytotoxic | [15] |
| (9) | Seeds | Cytotoxic | [33] |
| (11) | Seeds | Cytotoxic | [33] |
| (12) | Seeds | Antibacterial | [25] |
| Cytotoxic | [25] | ||
| (13) | Seeds | Toxic of Artemia salina | [34] |
| (14) | Leaves | Anti-inflammatory in vitro | [35] |
| Leaves | Phytotoxic | [36] | |
| (16) | Leaves | Phytotoxic | [37] |
| (18) | Leaves | Antibacterial | [38] |
| (19) | Leaves | Antiglycation | [39] |
| Anti-inflammatory | [40] | ||
| Antiseptic | [41] | ||
| Antiosteoporosis | [42] | ||
| Cytotoxic | [43,44] | ||
| (20) | Leaves | Phytotoxic | [45] |
| Hepatoprotective | [46] | ||
| Diuretic | [47] | ||
| (22) | Leaves | Antigenotoxic | [48] |
| Immunostimulant | [49,50] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiart, C.; Shorna, A.A.; Rahmatullah, M.; Nissapatorn, V.; Seelan, J.S.S.; Rahman, H.; Rusdi, N.A.; Mustaffa, N.; Elbehairy, L.; Sulaiman, M. The Garlic Tree of Borneo, Scorodocarpus borneensis (Baill.) Becc. (Olacaceae): Potential Utilization in Pharmaceutical, Nutraceutical, and Functional Cosmetic Industries. Molecules 2023, 28, 5717. https://doi.org/10.3390/molecules28155717
Wiart C, Shorna AA, Rahmatullah M, Nissapatorn V, Seelan JSS, Rahman H, Rusdi NA, Mustaffa N, Elbehairy L, Sulaiman M. The Garlic Tree of Borneo, Scorodocarpus borneensis (Baill.) Becc. (Olacaceae): Potential Utilization in Pharmaceutical, Nutraceutical, and Functional Cosmetic Industries. Molecules. 2023; 28(15):5717. https://doi.org/10.3390/molecules28155717
Chicago/Turabian StyleWiart, Christophe, Afsana Amin Shorna, Mohammed Rahmatullah, Veeranoot Nissapatorn, Jaya Seelan Sathya Seelan, Homathevi Rahman, Nor Azizun Rusdi, Nazirah Mustaffa, Layane Elbehairy, and Mazdida Sulaiman. 2023. "The Garlic Tree of Borneo, Scorodocarpus borneensis (Baill.) Becc. (Olacaceae): Potential Utilization in Pharmaceutical, Nutraceutical, and Functional Cosmetic Industries" Molecules 28, no. 15: 5717. https://doi.org/10.3390/molecules28155717
APA StyleWiart, C., Shorna, A. A., Rahmatullah, M., Nissapatorn, V., Seelan, J. S. S., Rahman, H., Rusdi, N. A., Mustaffa, N., Elbehairy, L., & Sulaiman, M. (2023). The Garlic Tree of Borneo, Scorodocarpus borneensis (Baill.) Becc. (Olacaceae): Potential Utilization in Pharmaceutical, Nutraceutical, and Functional Cosmetic Industries. Molecules, 28(15), 5717. https://doi.org/10.3390/molecules28155717