Multi-Functional Chitosan Nanovesicles Loaded with Bioactive Manganese for Potential Wound Healing Applications
Abstract
:1. Introduction
2. Results and Discussion
2.1. Characterization of Nanoscale Chitosan Vesicles Loaded with Bioactive Manganese Ions
2.2. Determination of Antioxidant Activity
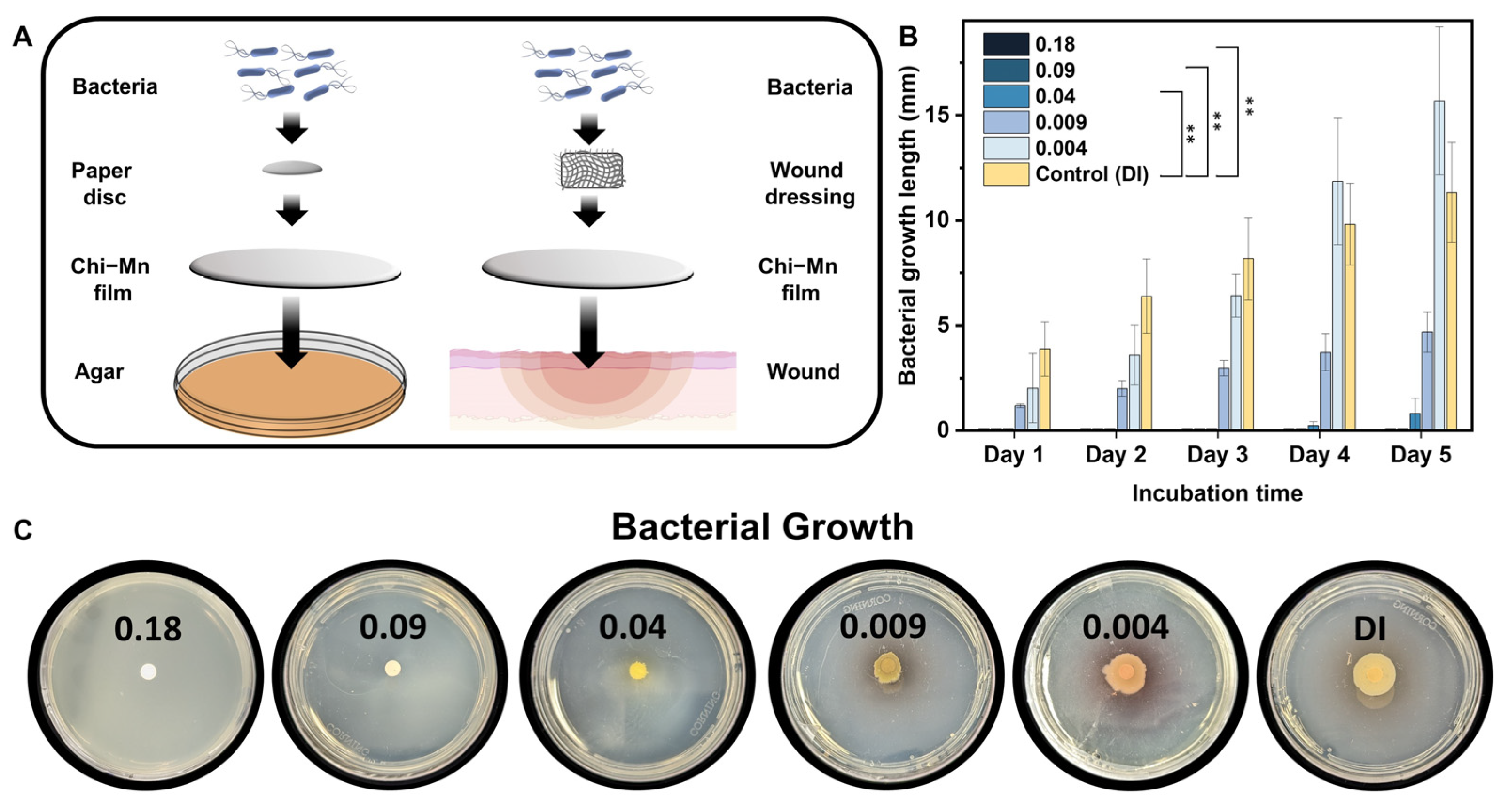
2.3. Antimicrobial Studies
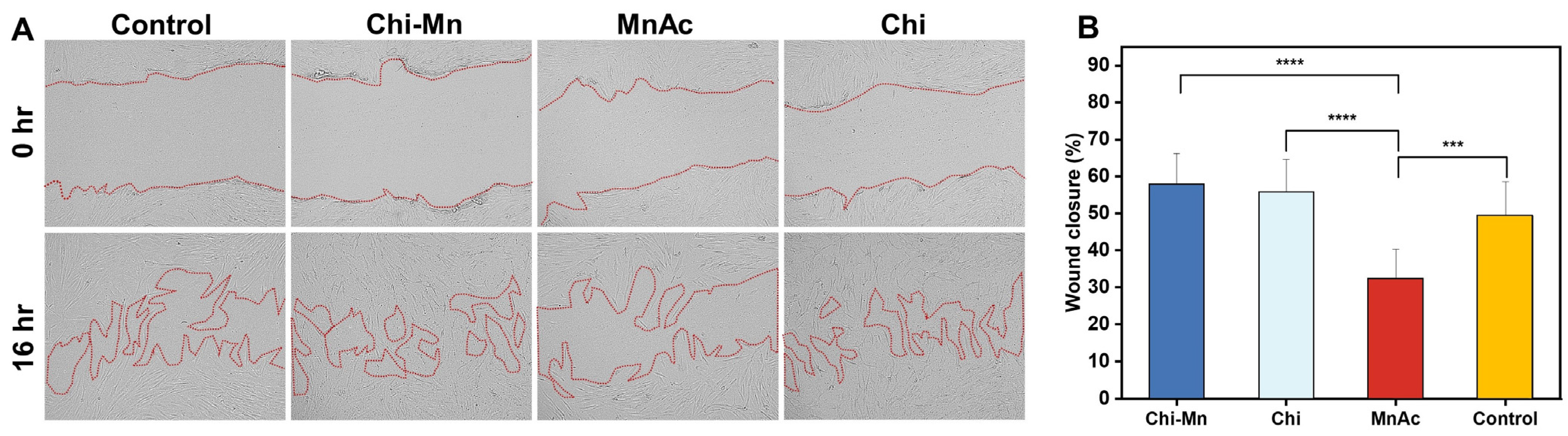
2.4. Biocompatibility Studies
3. Materials and Methods
3.1. Synthesis and Characterization
3.1.1. Preparation of Nanoscale Chitosan Vesicles Loaded with Manganese Ions
3.1.2. Fourier-Transform Infrared Spectroscopy (FTIR)
3.1.3. Scanning Electron Microscopy (SEM)
3.1.4. Energy-Dispersive X-ray Spectroscopy (EDS)
3.1.5. Dynamic Light Scattering (DLS) and Zeta Potential (ζ)
3.1.6. Ultraviolet-Visible (UV-Vis) Spectroscopy
3.1.7. Inductive Coupled Plasma Mass Spectrometry (ICP-MS)
3.2. Determination of Antioxidant Activity
3.3. Antimicrobial and Biocompatibility Studies
3.3.1. Determination of Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC)
3.3.2. Checkerboard Assay
3.3.3. Bacterial Motility Assay
3.3.4. Determination of Cell Viability
3.3.5. Determination of In Vitro Wound Healing Activity
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Xu, Z.; Liu, G.; Zheng, L.; Wu, J. A polyphenol-modified chitosan hybrid hydrogel with enhanced antimicrobial and antioxidant activities for rapid healing of diabetic wounds. Nano Res. 2023, 16, 905–916. [Google Scholar] [CrossRef]
- Matoori, S.; Veves, A.; Mooney, D.J. Advanced bandages for diabetic wound healing. Sci. Transl. Med. 2021, 13, eabe4839. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, S.R. An Economic Evaluation of the Impact, Cost, and Medicare Policy Implications of Chronic Nonhealing Wounds. Value Health 2018, 21, 27–32. [Google Scholar] [CrossRef]
- Takeo, M.; Lee, W.; Ito, M. Wound healing and skin regeneration. Cold Spring Harb. Perspect. Med. 2015, 5, a023267. [Google Scholar] [CrossRef]
- Velnar, T.; Bailey, T.; Smrkolj, V. The wound healing process: An overview of the cellular and molecular mechanisms. J. Int. Med. Res. 2009, 37, 1528–1542. [Google Scholar] [CrossRef] [PubMed]
- Gurtner, G.C. Wound repair and regeneration. Nature 2008, 453, 314–321. [Google Scholar] [CrossRef]
- Broughton, G.I.; Janis, J.E.; Attinger, C.E. The Basic Science of Wound Healing. Plast. Reconstr. Surg. 2006, 117, 12S–34S. [Google Scholar] [CrossRef]
- Tottoli, E.M. Skin Wound Healing Process and New Emerging Technologies for Skin Wound Care and Regeneration. Pharmaceutics 2020, 12, 735. [Google Scholar] [CrossRef]
- Järbrink, K. The humanistic and economic burden of chronic wounds: A protocol for a systematic review. Syst. Rev. 2017, 6, 15. [Google Scholar] [CrossRef]
- Khameneh, B. Breakthroughs in bacterial resistance mechanisms and the potential ways to combat them. Microb. Pathog. 2016, 95, 32–42. [Google Scholar] [CrossRef]
- Mouton, J. Combination therapy as a tool to prevent emergence of bacterial resistance. Infection 1999, 27 (Suppl. 2), S24–S28. [Google Scholar] [CrossRef]
- Polaka, S. Emerging ROS-Modulating Technologies for Augmentation of the Wound Healing Process. ACS Omega 2022, 7, 30657–30672. [Google Scholar] [CrossRef]
- Bilgen, F. The effect of oxidative stress and Raftlin levels on wound healing. Int. Wound J. 2019, 16, 1178–1184. [Google Scholar] [CrossRef] [PubMed]
- Dunnill, C. Reactive oxygen species (ROS) and wound healing: The functional role of ROS and emerging ROS-modulating technologies for augmentation of the healing process. Int. Wound J. 2017, 14, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z. Advances and impact of antioxidant hydrogel in chronic wound healing. Adv. Healthc. Mater. 2020, 9, 1901502. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z. M1 macrophage mediated increased reactive oxygen species (ROS) influence wound healing via the MAPK signaling in vitro and in vivo. Toxicol. Appl. Pharmacol. 2019, 366, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Koo, M.-A. Effective stacking and transplantation of stem cell sheets using exogenous ROS-producing film for accelerated wound healing. Acta Biomater. 2019, 95, 418–426. [Google Scholar] [CrossRef]
- Saoudi, M. The Role of Allium subhirsutum L. in the attenuation of dermal wounds by modulating oxidative stress and inflammation in Wistar albino rats. Molecules 2021, 26, 4875. [Google Scholar] [CrossRef]
- Hanna, J.R.; Giacopelli, J.A. A review of wound healing and wound dressing products. J. Foot Ankle Surg. 1997, 36, 2–14. [Google Scholar] [CrossRef]
- Negut, I.; Dorcioman, G.; Grumezescu, V. Scaffolds for Wound Healing Applications. Polymers 2020, 12, 2010. [Google Scholar] [CrossRef]
- Valizadeh, A. Preparation and Comparison of Effects of Different Herbal Oil Ointments as Wound-Healing Agents. Cells Tissues Organs 2019, 207, 177–186. [Google Scholar] [CrossRef]
- Koria, P. Delivery of Growth Factors for Tissue Regeneration and Wound Healing. BioDrugs 2012, 26, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Cheema, S.K. Regulation and guidance of cell behavior for tissue regeneration via the siRNA mechanism. Wound Repair Regen. 2007, 15, 286–295. [Google Scholar] [CrossRef] [PubMed]
- O'Meara, S. Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration. Health Technol. Assess. 2000, 4, 1–237. [Google Scholar] [CrossRef] [PubMed]
- Chouhan, D. Emerging and innovative approaches for wound healing and skin regeneration: Current status and advances. Biomaterials 2019, 216, 119267. [Google Scholar] [CrossRef]
- Ho, J.; Walsh, C.; Yue, D.; Dardik, A.; Cheema, U. Current Advancements and Strategies in Tissue Engineering for Wound Healing: A Comprehensive Review. Adv. Wound Care 2017, 6, 191–209. [Google Scholar] [CrossRef]
- Mirhaj, M. Emerging treatment strategies in wound care. Int. Wound J. 2022, 19, 1934–1954. [Google Scholar] [CrossRef]
- Dai, T. Chitosan preparations for wounds and burns: Antimicrobial and wound-healing effects. Expert Rev. Anti-Infect. Ther. 2011, 9, 857–879. [Google Scholar] [CrossRef]
- Patrulea, V. Chitosan as a starting material for wound healing applications. Eur. J. Pharm. Biopharm. 2015, 97, 417–426. [Google Scholar] [CrossRef]
- Yilmaz, E. Chitosan: A versatile biomaterial. Biomater. Mol. Eng. Tissue 2004, 553, 59–68. [Google Scholar]
- Muzzarelli, R. Biochemistry, histology and clinical uses of chitins and chitosans in wound healing. EXS 1999, 87, 251–264. [Google Scholar]
- Whang, H.S. Hemostatic Agents Derived from Chitin and Chitosan. J. Macromol. Sci. Part C 2005, 45, 309–323. [Google Scholar] [CrossRef]
- Haque, S.; Tripathy, S.; Patra, C.R. Manganese-based advanced nanoparticles for biomedical applications: Future opportunity and challenges. Nanoscale 2021, 13, 16405–16426. [Google Scholar] [CrossRef] [PubMed]
- Tenaud, I. In vitro modulation of keratinocyte wound healing integrins by zinc, copper and manganese. Br. J. Dermatol. 1999, 140, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Barrat, J. Le gluconate de cuivre et de manganèse dans le traitement des crevasses du sein lors de l'allaitement maternel. Rev. Fr. Gynécol. Obstét. 1992, 87, 49–51. [Google Scholar]
- Coassin, M.; Ursini, F.; Bindoli, A. Antioxidant effect of manganese. Arch. Biochem. Biophys. 1992, 299, 330–333. [Google Scholar] [CrossRef]
- Ahmadi, F. Chitosan based hydrogels: Characteristics and pharmaceutical applications. Res. Pharm. Sci. 2015, 10, 1–16. [Google Scholar]
- Clay, J.G.; Grayson, J.K.; Zierold, D. Comparative Testing of New Hemostatic Agents in a Swine Model of Extremity Arterial and Venous Hemorrhage. Mil. Med. 2010, 175, 280–284. [Google Scholar] [CrossRef]
- Basumallick, S. Hydrothermally treated chitosan spontaneously forms water-soluble spherical particles stable at a wide pH range. Int. J. Polym. Mater. Polym. Biomater. 2016, 65, 751–758. [Google Scholar] [CrossRef]
- Gartner, C.; López, B.L. Stiffness of chitosan in solution through intrinsic viscosity measurem. Rev. Fac. Ing. Univ. Antioq. 2010, 2010, 20–29. [Google Scholar]
- Lee, S.-H.; Park, S.-M.; Kim, Y. Effect of the concentration of sodium acetate (SA) on crosslinking of chitosan fiber by epichlorohydrin (ECH) in a wet spinning system. Carbohydr. Polym. 2007, 70, 53–60. [Google Scholar] [CrossRef]
- Larkin, P.J. Chapter 6—IR and Raman Spectra–Structure Correlations: Characteristic Group Frequencies. In Infrared and Raman Spectroscopy, 2nd ed.; Larkin, P.J., Ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 85–134. [Google Scholar]
- Cakic, S. Spectroscopic characteristics of highly selective manganese catalysis in acqueous polyurethane systems. Sensors 2006, 6, 1708–1720. [Google Scholar] [CrossRef]
- Kamiński, W.; Modrzejewska, Z. Application of chitosan membranes in separation of heavy metal ions. Sep. Sci. Technol. 1997, 32, 2659–2668. [Google Scholar] [CrossRef]
- Ali, M.E.A. Chitosan nanoparticles extracted from shrimp shells, application for removal of Fe(II) and Mn(II) from aqueous phases. Sep. Sci. Technol. 2018, 53, 2870–2881. [Google Scholar] [CrossRef]
- Huang, Y. Evaluation of diethylenetriaminepentaacetic acid–manganese(II) complexes modified by narrow molecular weight distribution of chitosan oligosaccharides as potential magnetic resonance imaging contrast agents. Magn. Reson. Imaging 2011, 29, 554–560. [Google Scholar] [CrossRef]
- Muzzarelli, R.A.; Rocchetti, R.; Muzzarelli, M.G. The isolation of cobalt, nickel, and copper from manganese nodules by chelation chromatography on chitosan. Sep. Sci. Technol. 1978, 13, 153–163. [Google Scholar] [CrossRef]
- Guan, B. Removal of Mn(II) and Zn(II) ions from flue gas desulfurization wastewater with water-soluble chitosan. Sep. Purif. Technol. 2009, 65, 269–274. [Google Scholar] [CrossRef]
- Guibal, E. Interactions of metal ions with chitosan-based sorbents: A review. Sep. Purif. Technol. 2004, 38, 43–74. [Google Scholar] [CrossRef]
- Zhu, Y. Sustained release of stromal cell derived factor-1 from an antioxidant thermoresponsive hydrogel enhances dermal wound healing in diabetes. J. Control. Release 2016, 238, 114–122. [Google Scholar] [CrossRef]
- Liu, M. Antioxidant thermogelling formulation for burn wound healing. Chem. Asian J. 2022, 17, e202200396. [Google Scholar] [CrossRef]
- Xiao, J. A cooperative copper metal–organic framework-hydrogel system improves wound healing in diabetes. Adv. Funct. Mater. 2017, 27, 1604872. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y. Sustained oxygenation accelerates diabetic wound healing by promoting epithelialization and angiogenesis and decreasing inflammation. Sci. Adv. 2021, 7, eabj0153. [Google Scholar] [CrossRef] [PubMed]
- Divya, K.; Smitha, V.; Jisha, M.S. Antifungal, antioxidant and cytotoxic activities of chitosan nanoparticles and its use as an edible coating on vegetables. Int. J. Biol. Macromol. 2018, 114, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y. Multienzymatic Antioxidant Activity of Manganese-Based Nanoparticles for Protection against Oxidative Cell Damage. ACS Biomater. Sci. Eng. 2022, 8, 638–648. [Google Scholar] [CrossRef]
- Puca, V. Microbial species isolated from infected wounds and antimicrobial resistance analysis: Data emerging from a three-years retrospective study. Antibiotics 2021, 10, 1162. [Google Scholar] [CrossRef]
- Centre for Disease, Control and Prevention. Antibiotic Resistance Threats in the United States, 2013; Centers for Disease Control and Prevention. US Department of Health and Human Services: Atlanta, GA, USA, 2013. [Google Scholar]
- Peralta, G. Impact of antibiotic resistance and of adequate empirical antibiotic treatment in the prognosis of patients with Escherichia coli bacteraemia. J. Antimicrob. Chemother. 2007, 60, 855–863. [Google Scholar] [CrossRef]
- Ito, A. Increased antibiotic resistance of Escherichia coli in mature biofilms. Appl. Environ. Microbiol. 2009, 75, 4093–4100. [Google Scholar] [CrossRef]
- Thi, M.T.T.; Wibowo, D.; Rehm, B.H. Pseudomonas aeruginosa biofilms. Int. J. Mol. Sci. 2020, 21, 8671. [Google Scholar] [CrossRef]
- Nagoba, B.S. A simple and effective approach for the treatment of chronic wound infections caused by multiple antibiotic resistant Escherichia coli. J. Hosp. Infect. 2008, 69, 177–180. [Google Scholar] [CrossRef]
- Zhao, G. Delayed wound healing in diabetic (db/db) mice with Pseudomonas aeruginosa biofilm challenge: A model for the study of chronic wounds. Wound Repair Regen. 2010, 18, 467–477. [Google Scholar] [CrossRef]
- Gupta, P. Bacteriophage Therapy of Chronic Nonhealing Wound: Clinical Study. Int. J. Low. Extrem. Wounds 2019, 18, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Du, W.-L. Antibacterial activity of chitosan tripolyphosphate nanoparticles loaded with various metal ions. Carbohydr. Polym. 2009, 75, 385–389. [Google Scholar] [CrossRef]
- Sarwar, A.; Katas, H.; Zin, N.M. Antibacterial effects of chitosan–tripolyphosphate nanoparticles: Impact of particle size molecular weight. J. Nanoparticle Res. 2014, 16, 2517. [Google Scholar] [CrossRef]
- Wu, T. Integration of lysozyme into chitosan nanoparticles for improving antibacterial activity. Carbohydr. Polym. 2017, 155, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, M.; Kim, K.D.; Chun, S.C. Antibacterial Activity of Chitosan Nanoparticles: A Review. Processes 2020, 8, 1173. [Google Scholar] [CrossRef]
- Owen, L.; Laird, K. Synchronous application of antibiotics and essential oils: Dual mechanisms of action as a potential solution to antibiotic resistance. Crit. Rev. Microbiol. 2018, 44, 414–435. [Google Scholar] [CrossRef]
- Georgescu, M. Bioactive wound dressings for the management of chronic wounds. Curr. Org. Chem. 2017, 21, 53–63. [Google Scholar] [CrossRef]
- Ramalingam, R. Core–shell structured antimicrobial nanofiber dressings containing herbal extract and antibiotics combination for the prevention of biofilms and promotion of cutaneous wound healing. ACS Appl. Mater. Interfaces 2021, 13, 24356–24369. [Google Scholar] [CrossRef]
- Mi, F.L. Control of wound infections using a bilayer chitosan wound dressing with sustainable antibiotic delivery. J. Biomed. Mater. Res. Off. J. Soc. Biomater. Jpn. Soc. Biomater. Aust. Soc. Biomater. Korean Soc. Biomater. 2002, 59, 438–449. [Google Scholar] [CrossRef]
- Nation, R.L.; Li, J. Colistin in the 21st century. Curr. Opin. Infect. Dis. 2009, 22, 535–543. [Google Scholar] [CrossRef]
- Werner, S.; Krieg, T.; Smola, H. Keratinocyte–fibroblast interactions in wound healing. J. Investig. Dermatol. 2007, 127, 998–1008. [Google Scholar] [CrossRef] [PubMed]
- Rodero, M.P.; Khosrotehrani, K. Skin wound healing modulation by macrophages. Int. J. Clin. Exp. Pathol. 2010, 3, 643–653. [Google Scholar]
- Standardization, I. Biological Evaluation of Medical Devices—Part 5: Tests for In Vitro Cytotoxicity; ISO: Geneva, Switzerland, 2009. [Google Scholar]
- Biranje, S.S. Hemostasis and anti-necrotic activity of wound-healing dressing containing chitosan nanoparticles. Int. J. Biol. Macromol. 2019, 121, 936–946. [Google Scholar] [CrossRef]
- Fahimirad, S. Antimicrobial Activity, Stability and Wound Healing Performances of Chitosan Nanoparticles Loaded Recombinant LL37 Antimicrobial Peptide. Int. J. Pept. Res. Ther. 2021, 27, 2505–2515. [Google Scholar] [CrossRef]
- Shaw, T.J.; Martin, P. Wound repair at a glance. J. Cell Sci. 2009, 122, 3209–3213. [Google Scholar] [CrossRef]
- Blois, M.S. Antioxidant determinations by the use of a stable free radical. Nature 1958, 181, 1199–1200. [Google Scholar] [CrossRef]
- Kedare, S.B.; Singh, R.P. Genesis and development of DPPH method of antioxidant assay. J. Food Sci. Technol. 2011, 48, 412–422. [Google Scholar] [CrossRef]
- Wikler, M.A. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically: APPROVED Standard; CLSI: Wayne, PA, USA, 2006; Volume 26, pp. M7–A7. [Google Scholar]
- Bellio, P. New and simplified method for drug combination studies by checkerboard assay. MethodsX 2021, 8, 101543. [Google Scholar] [CrossRef]
- Bernal-Mercado, A.T. Hydrophobic Chitosan Nanoparticles Loaded with Carvacrol against Pseudomonas aeruginosa Biofilms. Molecules 2022, 27, 699. [Google Scholar] [CrossRef]
- Martinotti, S.; Ranzato, E. Scratch Wound Healing Assay. In Epidermal Cells; Springer: Berlin/Heidelberg, Germany, 2019; pp. 225–229. [Google Scholar]
- Suarez-Arnedo, A. An image J plugin for the high throughput image analysis of in vitro scratch wound healing assays. PLoS ONE 2020, 15, e0232565. [Google Scholar] [CrossRef]



| MnAc | Chi | Chi-Mn | ||||
|---|---|---|---|---|---|---|
| Bacteria | MIC | MBC | MIC | MBC | MIC | MBC |
| E. coli K-12 | 256 | >256 | 8 | 8 | 8 | 8 |
| P. aeruginosa PA01 | 256 | >256 | 256 | 256 | 256 | >256 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davidson, E.; Pereira, J.; Gan Giannelli, G.; Murphy, Z.; Anagnostopoulos, V.; Santra, S. Multi-Functional Chitosan Nanovesicles Loaded with Bioactive Manganese for Potential Wound Healing Applications. Molecules 2023, 28, 6098. https://doi.org/10.3390/molecules28166098
Davidson E, Pereira J, Gan Giannelli G, Murphy Z, Anagnostopoulos V, Santra S. Multi-Functional Chitosan Nanovesicles Loaded with Bioactive Manganese for Potential Wound Healing Applications. Molecules. 2023; 28(16):6098. https://doi.org/10.3390/molecules28166098
Chicago/Turabian StyleDavidson, Edwin, Jorge Pereira, Giuliana Gan Giannelli, Zachary Murphy, Vasileios Anagnostopoulos, and Swadeshmukul Santra. 2023. "Multi-Functional Chitosan Nanovesicles Loaded with Bioactive Manganese for Potential Wound Healing Applications" Molecules 28, no. 16: 6098. https://doi.org/10.3390/molecules28166098






