Multifunctional Novel Nanoplatform for Effective Synergistic Chemo-Photodynamic Therapy of Breast Cancer by Enhancing DNA Damage and Disruptions of Its Reparation
Abstract
:1. Introduction
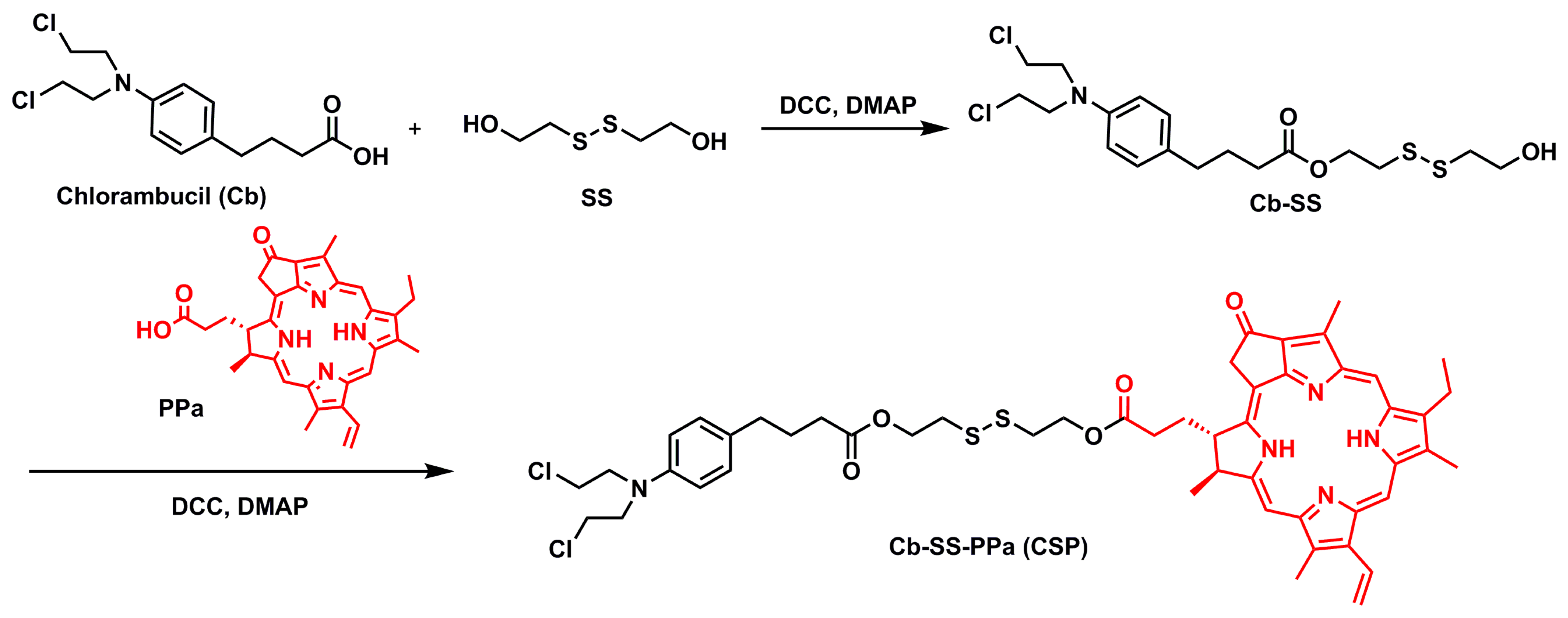
2. Results and Discussion
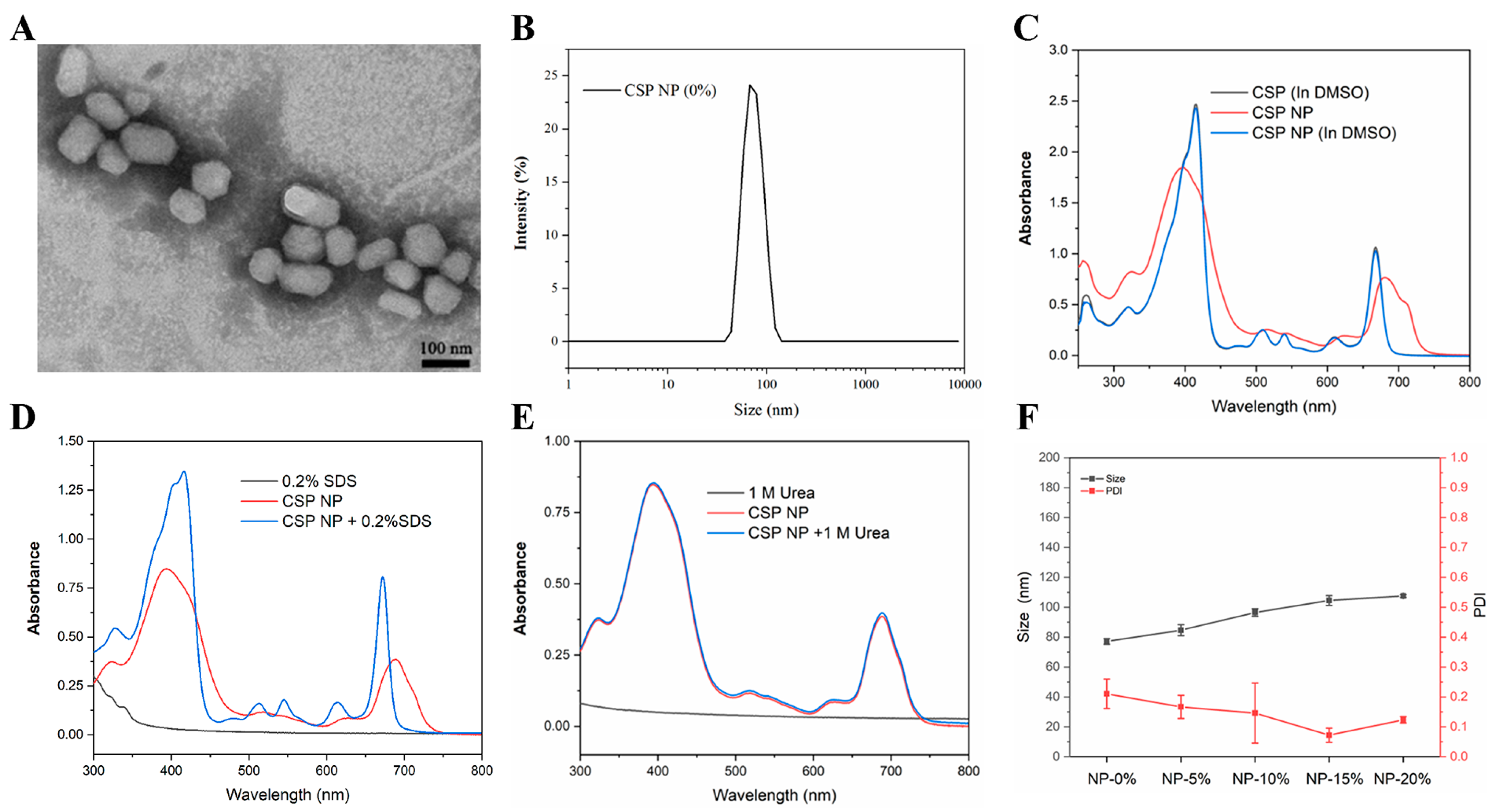
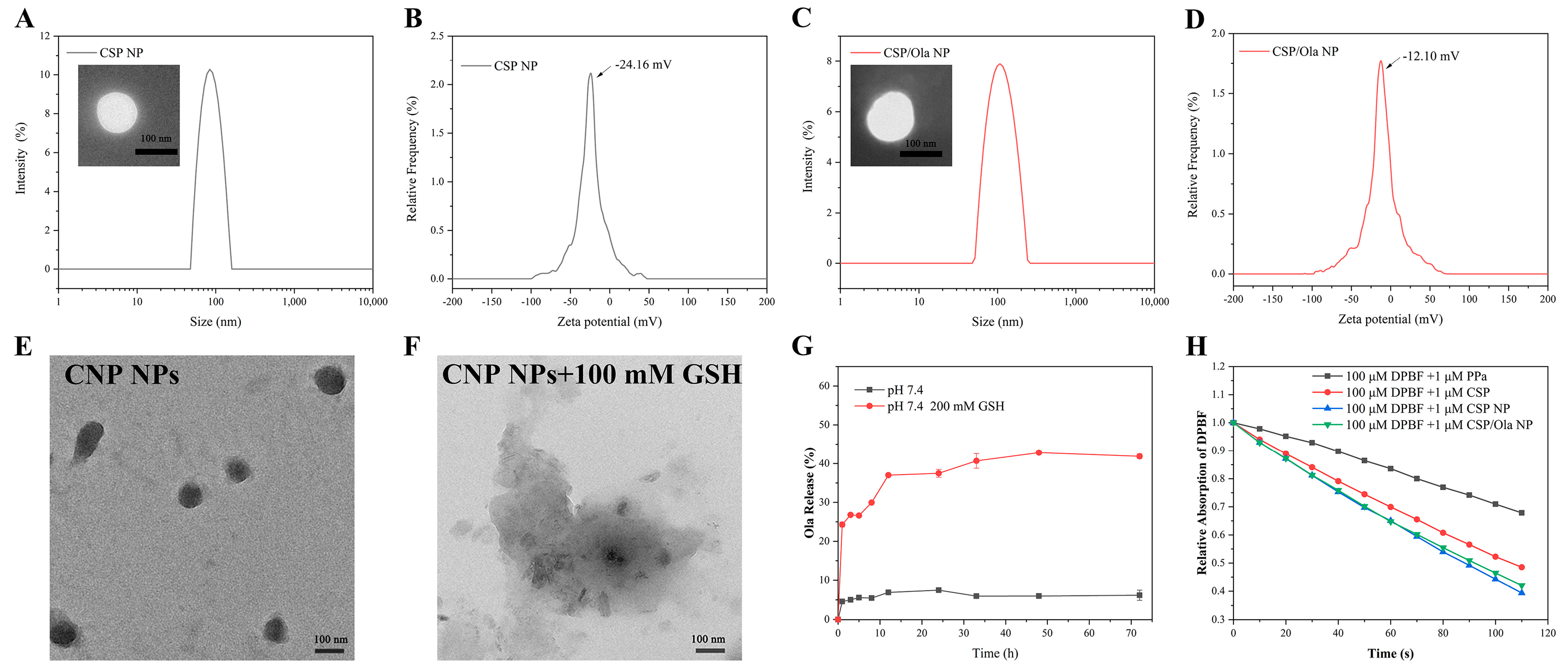
2.1. Preparation, Characterization and Spectroscopic Properties of CSP NPs and CSP/Ola NPs
2.2. Cell Internalization of CSP/Ola NPs for ROS Production, GSH Depletion and PARP Inhibition
2.3. In Vitro Chemo-Photodynamic Synergistic Antitumor Study
3. Materials and Methods
3.1. Synthesis of Cb-SS
3.2. Synthesis of CSP
3.3. Preparation of CSP/Ola NPs
3.4. Characterization of CSP/Ola NPs
3.5. In Vitro ROS Generation
3.6. Cell Culture
3.7. Cellular Uptake and Endocytic Pathway
3.8. Intracellular ROS Generation
3.9. Intracellular Glutathione (GSH) Levels
3.10. MTT Assays
3.11. Cell Apoptosis Detection
3.12. Live and Dead Cell Staining
3.13. γ-H2AX Immunofluorescence
3.14. Western Blotting
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [PubMed]
- Huang, Z.; Li, D.; Guo, F.; Xian, T.; Hu, H.-S.; Xu, J.; Luo, Y.-F.; Chen, Z.-Z.; Wang, B.-C.; Zhang, Y.-M. Mitochondria-targeted photosensitizer based nanoplatform loading glutathione inhibitor for enhanced breast cancer photodynamic therapy. Colloid. Surface B 2022, 220, 112956. [Google Scholar]
- Koren, S.; Bentires-Alj, M. Breast Tumor Heterogeneity: Source of Fitness, Hurdle for Therapy. Mol. Cell 2015, 60, 537–546. [Google Scholar] [PubMed]
- Liu, J.-N.; Bu, W.; Shi, J. Chemical Design and Synthesis of Functionalized Probes for Imaging and Treating Tumor Hypoxia. Chem. Rev. 2017, 117, 6160–6224. [Google Scholar]
- Li, S.; Zou, Q.; Li, Y.; Yuan, C.; Xing, R.; Yan, X. Smart Peptide-Based Supramolecular Photodynamic Metallo-Nanodrugs Designed by Multicomponent Coordination Self-Assembly. J. Am. Chem. Soc. 2018, 140, 10794–10802. [Google Scholar] [CrossRef]
- Liu, M.; Chen, Y.; Guo, Y.; Yuan, H.; Cui, T.; Yao, S.; Jin, S.; Fan, H.; Wang, C.; Xie, R.; et al. Golgi apparatus-targeted aggregation-induced emission luminogens for effective cancer photodynamic therapy. Nat. Commun. 2022, 13, 2179. [Google Scholar]
- Liu, L.-H.; Qiu, W.-X.; Li, B.; Zhang, C.; Sun, L.-F.; Wan, S.-S.; Rong, L.; Zhang, X.-Z. A Red Light Activatable Multifunctional Prodrug for Image-Guided Photodynamic Therapy and Cascaded Chemotherapy. Adv. Funct. Mater. 2016, 26, 6257–6269. [Google Scholar]
- Pham, T.C.; Nguyen, V.-N.; Choi, Y.; Lee, S.; Yoon, J. Recent Strategies to Develop Innovative Photosensitizers for Enhanced Photodynamic Therapy. Chem. Rev. 2021, 121, 13454–13619. [Google Scholar]
- Trachootham, D.; Alexandre, J.; Huang, P. Targeting cancer cells by ROS-mediated mechanisms: A radical therapeutic approach? Nat. Rev. Drug Discov. 2009, 8, 579–591. [Google Scholar]
- Vankayala, R.; Hwang, K.C. Near-Infrared-Light-Activatable Nanomaterial-Mediated Phototheranostic Nanomedicines: An Emerging Paradigm for Cancer Treatment. Adv. Mater. 2018, 30, 1706320. [Google Scholar]
- Xu, H.-Z.; Li, T.-F.; Ma, Y.; Li, K.; Zhang, Q.; Xu, Y.-H.; Zhang, Y.-C.; Zhao, L.; Chen, X. Targeted photodynamic therapy of glioblastoma mediated by platelets with photo-controlled release property. Biomaterials 2022, 290, 121833. [Google Scholar]
- Lord, C.J.; Ashworth, A. PARP inhibitors: Synthetic lethality in the clinic. Science 2017, 355, 1152–1158. [Google Scholar] [PubMed]
- Tan, P.; Cai, H.; Wei, Q.; Tang, X.; Zhang, Q.; Kopytynski, M.; Yang, J.; Yi, Y.; Zhang, H.; Gong, Q.; et al. Enhanced chemo-photodynamic therapy of an enzyme-responsive prodrug in bladder cancer patient-derived xenograft models. Biomaterials 2021, 277, 121061. [Google Scholar]
- Feng, L.; Chen, M.; Li, R.; Zhou, L.; Wang, C.; Ye, P.; Hu, X.; Yang, J.; Sun, Y.; Zhu, Z.; et al. Biodegradable oxygen-producing manganese-chelated metal organic frameworks for tumor-targeted synergistic chemo/photothermal/photodynamic therapy. Acta Biomater. 2022, 138, 463–477. [Google Scholar] [CrossRef] [PubMed]
- Lovell, J.F.; Liu, T.W.B.; Chen, J.; Zheng, G. Activatable Photosensitizers for Imaging and Therapy. Chem. Rev. 2010, 110, 2839–2857. [Google Scholar]
- Lucky, S.S.; Soo, K.C.; Zhang, Y. Nanoparticles in Photodynamic Therapy. Chem. Rev. 2015, 115, 1990–2042. [Google Scholar]
- Xue, Y.; Li, J.; Yang, G.; Liu, Z.; Zhou, H.; Zhang, W. Multistep Consolidated Phototherapy Mediated by a NIR-Activated Photosensitizer. ACS Appl. Mater. Interfaces 2019, 11, 33628–33636. [Google Scholar] [CrossRef]
- Huang, Z.; Hu, H.; Xian, T.; Xu, Z.; Tang, D.; Wang, B.; Zhang, Y. Carrier-free nanomedicines self-assembled from palbociclib dimers and Ce6 for enhanced combined chemo-photodynamic therapy of breast cancer. RSC Adv. 2023, 13, 1617–1626. [Google Scholar] [CrossRef]
- Maeda, H.; Nakamura, H.; Fang, J. The EPR effect for macromolecular drug delivery to solid tumors: Improvement of tumor uptake, lowering of systemic toxicity, and distinct tumor imaging in vivo. Adv. Drug Deliver. Rev. 2013, 65, 71–79. [Google Scholar]
- Wang, A.Z.; Langer, R.; Farokhzad, O.C. Nanoparticle Delivery of Cancer Drugs. Annu. Rev. Med. 2012, 63, 185–198. [Google Scholar] [CrossRef]
- Zhang, Y.-M.; Xia, M.; Ao, R.; Gao, L.-X.; Tang, Y.; Huang, J.-H.; Luo, Y.-F.; Chen, Z.-Z.; Wang, B.-C.; Huang, Z. Smart Design of Mitochondria-Targeted and ROS-Responsive CPI-613 Delivery Nanoplatform for Bioenergetic Pancreatic Cancer Therapy. Nanomaterials 2021, 11, 2875. [Google Scholar] [PubMed]
- Dong, Z.; Feng, L.; Chao, Y.; Hao, Y.; Chen, M.; Gong, F.; Han, X.; Zhang, R.; Cheng, L.; Liu, Z. Amplification of Tumor Oxidative Stresses with Liposomal Fenton Catalyst and Glutathione Inhibitor for Enhanced Cancer Chemotherapy and Radiotherapy. Nano Lett. 2019, 19, 805–815. [Google Scholar] [PubMed]
- Zhong, H.; Huang, P.-Y.; Yan, P.; Chen, P.-L.; Shi, Q.-Y.; Zhao, Z.-A.; Chen, J.-X.; Shu, X.; Wang, P.; Yang, B.; et al. Versatile Nanodrugs Containing Glutathione and Heme Oxygenase 1 Inhibitors Enable Suppression of Antioxidant Defense System in a Two-Pronged Manner for Enhanced Photodynamic Therapy. Adv. Healthc. Mater. 2021, 10, 2100770. [Google Scholar] [CrossRef]
- Zimmer, A.S.; Gillard, M.; Lipkowitz, S.; Lee, J.-M. Update on PARP Inhibitors in Breast Cancer. Curr. Treat. Options Oncol. 2018, 19, 21. [Google Scholar]
- Li, X.-Y.; Deng, F.-A.; Zheng, R.-R.; Liu, L.-S.; Liu, Y.-B.; Kong, R.-J.; Chen, A.-L.; Yu, X.-Y.; Li, S.-Y.; Cheng, H. Carrier Free Photodynamic Synergists for Oxidative Damage Amplified Tumor Therapy. Small 2021, 17, 2102470. [Google Scholar]
- Hu, J.-J.; Chen, Y.; Li, Z.-H.; Peng, S.-Y.; Sun, Y.; Zhang, X.-Z. Augment of Oxidative Damage with Enhanced Photodynamic Process and MTH1 Inhibition for Tumor Therapy. Nano Lett. 2019, 19, 5568–5576. [Google Scholar] [CrossRef] [PubMed]
- Kong, R.-J.; Li, X.-Y.; Huang, J.-Q.; Zhou, X.; Deng, F.-A.; Li, Y.-M.; Liu, L.-S.; Li, S.-Y.; Cheng, H. A self-delivery photodynamic sensitizer for enhanced DNA damage by PARP inhibition. Biomater. Sci. 2023, 11, 162–169. [Google Scholar] [CrossRef]
- Dias, M.P.; Moser, S.C.; Ganesan, S.; Jonkers, J. Understanding and overcoming resistance to PARP inhibitors in cancer therapy. Nat. Rev. Clin. Oncol. 2021, 18, 773–791. [Google Scholar]
- Xiong, Y.; Wang, W.; Deng, Q.; Zhang, Z.; Wang, Q.; Yong, Z.; Sun, C.; Yang, X.; Li, Z. Mild photothermal therapy boosts nanomedicine antitumor efficacy by disrupting DNA damage repair pathways and modulating tumor mechanics. Nano Today 2023, 49, 101767. [Google Scholar]
- Mao, Y.; Huang, X.; Shuang, Z.; Lin, G.; Wang, J.; Duan, F.; Chen, J.; Li, S. PARP inhibitor olaparib sensitizes cholangiocarcinoma cells to radiation. Cancer Med. 2018, 7, 1285–1296. [Google Scholar] [CrossRef]
- Loap, P.; Loirat, D.; Berger, F.; Rodrigues, M.; Bazire, L.; Pierga, J.-Y.; Vincent-Salomon, A.; Laki, F.; Boudali, L.; Raizonville, L.; et al. Concurrent Olaparib and Radiotherapy in Patients With Triple-Negative Breast Cancer: The Phase 1 Olaparib and Radiation Therapy for Triple-Negative Breast Cancer Trial. JAMA Oncol. 2022, 8, 1802–1808. [Google Scholar]
- Reiss, K.A.; Mick, R.; Teitelbaum, U.; O’Hara, M.; Schneider, C.; Massa, R.; Karasic, T.; Tondon, R.; Onyiah, C.; Gosselin, M.K.; et al. Niraparib plus nivolumab or niraparib plus ipilimumab in patients with platinum-sensitive advanced pancreatic cancer: A randomised, phase 1b/2 trial. Lancet Oncol. 2022, 23, 1009–1020. [Google Scholar] [CrossRef] [PubMed]
- Rottenberg, S.; Jaspers, J.E.; Kersbergen, A.; van der Burg, E.; Nygren, A.O.H.; Zander, S.A.L.; Derksen, P.W.B.; de Bruin, M.; Zevenhoven, J.; Lau, A.; et al. High sensitivity of BRCA1-deficient mammary tumors to the PARP inhibitor AZD2281 alone and in combination with platinum drugs. Proc. Natl. Acad. Sci. USA 2008, 105, 17079–17084. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Yang, Y.; Huang, C.; Ye, Z.; Lai, W.; Luo, J.; Li, X.; Yi, X.; Fan, J.-B.; Wang, Y.; et al. cRGD-targeted heparin nanoparticles for effective dual drug treatment of cisplatin-resistant ovarian cancer. J. Control. Release 2023, 356, 691–701. [Google Scholar] [PubMed]
- Robson, M.; Im, S.-A.; Senkus, E.; Xu, B.; Domchek, S.M.; Masuda, N.; Delaloge, S.; Li, W.; Tung, N.; Armstrong, A.; et al. Olaparib for Metastatic Breast Cancer in Patients with a Germline BRCA Mutation. New Engl. J. Med. 2017, 377, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Du, X.; Xu, J.; Kong, X.; Li, Y.; Liu, D.; Yang, X.; Ye, L.; Ji, J.; Xi, Y.; et al. Multifunctional biomimetic nanoplatform based on photodynamic therapy and DNA repair intervention for the synergistic treatment of breast cancer. Acta Biomater. 2023, 157, 551–565. [Google Scholar] [CrossRef]
- Dalpiaz, A.; Paganetto, G.; Botti, G.; Pavan, B. Cancer stem cells and nanomedicine: New opportunities to combat multidrug resistance? Drug Discov. Today 2020, 25, 1651–1667. [Google Scholar]
- Dréan, A.; Lord, C.J.; Ashworth, A. PARP inhibitor combination therapy. Crit. Rev. Oncol. Hematol. 2016, 108, 73–85. [Google Scholar]
- Wilson, A.; Menon, V.; Khan, Z.; Alam, A.; Litovchick, L.; Yakovlev, V. Nitric oxide-donor/PARP-inhibitor combination: A new approach for sensitization to ionizing radiation. Redox Biol. 2019, 24, 101169. [Google Scholar]
- Huang, Z.; Gao, L.; Guo, F.; Li, D.; Tang, Y.; Hu, H.; Luo, Y.; Tang, D.; Wang, B.; Zhang, Y. Novel prodrug supramolecular nanoparticles capable of rapid mitochondrial-targeting and ROS-responsiveness for pancreatic cancer therapy. New J. Chem. 2022, 46, 12632–12640. [Google Scholar]
- Kohn, K.W.; Hartley, J.A.; Mattes, W.B. Mechanisms of DNA sequence selective alkylation of guanine-N7 positions by nitrogen mustards. Nucleic Acids Res. 1987, 15, 10531–10549. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhang, Q.; Chang, H.; Cheng, Y. Surface-Engineered Dendrimers in Gene Delivery. Chem. Rev. 2015, 115, 5274–5300. [Google Scholar] [PubMed]
- Liu, L.-H.; Zhang, X.-Z. Carrier-free nanomedicines for cancer treatment. Prog. Mater. Sci. 2022, 125, 100919. [Google Scholar]
- Seidi, F.; Jenjob, R.; Crespy, D. Designing Smart Polymer Conjugates for Controlled Release of Payloads. Chem. Rev. 2018, 118, 3965–4036. [Google Scholar] [PubMed]
- Shymborska, Y.; Budkowski, A.; Raczkowska, J.; Donchak, V.; Melnyk, Y.; Vasiichuk, V.; Stetsyshyn, Y. Switching it Up: The Promise of Stimuli-Responsive Polymer Systems in Biomedical Science. Chem. Rec. 2023, e202300217. [Google Scholar]
- Zhang, Q.-F.; Yu, Q.-Y.; Geng, Y.; Zhang, J.; Wu, W.-X.; Wang, G.; Gu, Z.; Yu, X.-Q. Ring-Opening Polymerization for Hyperbranched Polycationic Gene Delivery Vectors with Excellent Serum Tolerance. ACS Appl. Mater. Interfaces 2014, 6, 15733–15742. [Google Scholar]
- Ivashkevich, A.; Redon, C.E.; Nakamura, A.J.; Martin, R.F.; Martin, O.A. Use of the γ-H2AX assay to monitor DNA damage and repair in translational cancer research. Cancer Lett. 2012, 327, 123–133. [Google Scholar]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Z.; Xian, T.; Meng, X.; Hu, H.; Gao, L.; Huang, J.; Yang, D.; Ou, K.; Wang, B.; Zhang, Y. Multifunctional Novel Nanoplatform for Effective Synergistic Chemo-Photodynamic Therapy of Breast Cancer by Enhancing DNA Damage and Disruptions of Its Reparation. Molecules 2023, 28, 6972. https://doi.org/10.3390/molecules28196972
Huang Z, Xian T, Meng X, Hu H, Gao L, Huang J, Yang D, Ou K, Wang B, Zhang Y. Multifunctional Novel Nanoplatform for Effective Synergistic Chemo-Photodynamic Therapy of Breast Cancer by Enhancing DNA Damage and Disruptions of Its Reparation. Molecules. 2023; 28(19):6972. https://doi.org/10.3390/molecules28196972
Chicago/Turabian StyleHuang, Zheng, Tong Xian, Xiangyi Meng, Huaisong Hu, Lixia Gao, Jiuhong Huang, Donglin Yang, Kepeng Ou, Bochu Wang, and Yimei Zhang. 2023. "Multifunctional Novel Nanoplatform for Effective Synergistic Chemo-Photodynamic Therapy of Breast Cancer by Enhancing DNA Damage and Disruptions of Its Reparation" Molecules 28, no. 19: 6972. https://doi.org/10.3390/molecules28196972
APA StyleHuang, Z., Xian, T., Meng, X., Hu, H., Gao, L., Huang, J., Yang, D., Ou, K., Wang, B., & Zhang, Y. (2023). Multifunctional Novel Nanoplatform for Effective Synergistic Chemo-Photodynamic Therapy of Breast Cancer by Enhancing DNA Damage and Disruptions of Its Reparation. Molecules, 28(19), 6972. https://doi.org/10.3390/molecules28196972





