Current and Potential Applications of Monoterpenes and Their Derivatives in Oral Health Care
Abstract
:1. Introduction
2. Biological Properties
2.1. Antimicrobial and Antiseptic Activity
2.1.1. Antibacterial Activity
2.1.2. Antifungal Activity
2.1.3. Antiviral Activity
2.2. Anti-Cancer Activity
2.3. Anti-Inflammatory Activity
2.4. Analgesic and Antinociceptive Activity
3. Use in Dentistry and Oral Health Care
3.1. Oral Hygiene
3.2. Halitosis
3.3. Dental Treatments
3.4. Periodontal Diseases
3.5. Mucosal Lesions
3.6. Dry Mouth
4. Side Effects
4.1. Allergic Reactions
4.2. Toxicity
5. Materials and Methods
- Availability of the full text;
- Appropriate methodology;
- Research regarding pure monoterpenes or monoterpenoids or mixed compounds containing monoterpenes or monoterpenoids.
6. Conclusions and Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Zhou, Z.-R.; Yu, H.-Y.; Zheng, J.; Qian, L.-M.; Yan, Y. Dental Biotribology; Springer: New York, NY, USA, 2013; ISBN 978-1-4614-4549-4. [Google Scholar]
- Alali, F.; Hudaib, M.; Aburjai, T.; Khairallah, K.; Al-Hadidi, N. GC-MS Analysis and Antimicrobial Activity of the Essential Oil from the Stem of the Jordanian Toothbrush Tree Salvadora persica. Pharm. Biol. 2005, 42, 577–580. [Google Scholar] [CrossRef]
- Farag, M.; Abdel-Mageed, W.M.; El Gamal, A.A.; Basudan, O.A. Salvadora persica L.: Toothbrush Tree with Health Benefits and Industrial Applications—An Updated Evidence-Based Review. Saudi Pharm. J. 2021, 29, 751–763. [Google Scholar] [CrossRef] [PubMed]
- Medico-Dental History of Cloves. Nature 1943, 151, 194. [CrossRef]
- Alqareer, A.; Alyahya, A.; Andersson, L. The Effect of Clove and Benzocaine versus Placebo as Topical Anesthetics. J. Dent. 2006, 34, 747–750. [Google Scholar] [CrossRef]
- Jirovetz, L.; Buchbauer, G.; Stoilova, I.; Stoyanova, A.; Krastanov, A.; Schmidt, E. Chemical Composition and Antioxidant Properties of Clove Leaf Essential Oil. J. Agric. Food Chem. 2006, 54, 6303–6307. [Google Scholar] [CrossRef] [PubMed]
- Zielińska-Błajet, M.; Feder-Kubis, J. Monoterpenes and Their Derivatives—Recent Development in Biological and Medical Applications. Int. J. Mol. Sci. 2020, 21, 7078. [Google Scholar] [CrossRef] [PubMed]
- Breitmaier, E. Terpenes: Importance, General Structure, and Biosynthesis. In Terpenes; WILEY-VCH: Weinheim, Germany, 2006; pp. 1–9. ISBN 978-3-527-60994-9. [Google Scholar]
- Loza-Tavera, H. Monoterpenes in Essential Oils: Biosynthesis and Properties. Adv. Exp. Med. Biol. 1999, 464, 49–62. [Google Scholar] [CrossRef]
- Breitmaier, E. Hemi- and Monoterpenes. In Terpenes; WILEY-VCH: Weinheim, Germany, 2006; pp. 10–23. ISBN 978-3-527-60994-9. [Google Scholar]
- Alcántara, A.R.; Hernaiz, M.-J.; Sinisterra, J.-V. 3.28—Biocatalyzed Production of Fine Chemicals. In Comprehensive Biotechnology, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2011; pp. 309–331. ISBN 978-0-08-088504-9. [Google Scholar]
- Sinclair, L. Consumers Demand Natural Oral Hygiene Products. Available online: https://www.colgateprofessional.com/students-faculty/practice-management/consumers-demand-natural-oral-hygiene-products (accessed on 16 January 2023).
- Howarth, J. Top 9 Dental Industry Trends (2023–2025). Available online: https://explodingtopics.com/blog/dental-industry-trends (accessed on 20 January 2023).
- Mazur, M.; Ndokaj, A.; Bietolini, S.; Duś-Ilnicka, I.; Ottolenghi, L. Green Dentistry: Organic Toothpaste Formulations. A Literature Review. Dent. Med. Probl. 2022, 59, 461–474. [Google Scholar] [CrossRef]
- Colgate Naturals Turmeric Gum Protect Whitening Toothpaste. Available online: https://www.colgate.com/en-ph/products/toothpaste/colgate-naturals-turmeric-gum-protect (accessed on 25 January 2023).
- Turmeric for Your Teeth. Available online: https://www.colgate.com/en-us/oral-health/teeth-whitening/turmeric-for-teeth-will-a-spice-whiten-your-smile (accessed on 4 April 2023).
- Vedshakti Oil Pulling—Uses and Benefits. Available online: https://www.colgate.com/en-in/products/colgate-vedshakti-oil-pulling (accessed on 25 January 2023).
- PubChem PubChem. Available online: https://pubchem.ncbi.nlm.nih.gov/ (accessed on 9 May 2023).
- Allenspach, M.; Steuer, C. α-Pinene: A Never-Ending Story. Phytochemistry 2021, 190, 112857. [Google Scholar] [CrossRef]
- (+)-α-Pinene. Available online: https://www.wikidata.org/wiki/Q2095629 (accessed on 1 May 2023).
- (−)-α-Pinene. Available online: https://www.wikidata.org/wiki/Q300852 (accessed on 1 May 2023).
- α-Pinene. Available online: https://www.wikidata.org/wiki/Q27104380 (accessed on 1 May 2023).
- Rahbar, I.; Abbasnejad, M.; Haghani, J.; Raoof, M.; Kooshki, R.; Esmaeili-Mahani, S. The Effect of Central Administration of Alpha-Pinene on Capsaicin-Induced Dental Pulp Nociception. Int. Endod. J. 2019, 52, 307–317. [Google Scholar] [CrossRef]
- Iraji, A.; Yazdanpanah, S.; Alizadeh, F.; Mirzamohammadi, S.; Ghasemi, Y.; Pakshir, K.; Yang, Y.; Zomorodian, K. Screening the Antifungal Activities of Monoterpenes and Their Isomers against Candida Species. J. Appl. Microbiol. 2020, 129, 1541–1551. [Google Scholar] [CrossRef]
- Bomfim de Barros, D.; de Oliveira e Lima, L.; Alves da Silva, L.; Cavalcante Fonseca, M.; Ferreira, R.C.; Diniz Neto, H.; da Nóbrega Alves, D.; da Silva Rocha, W.P.; Scotti, L.; de Oliveira Lima, E.; et al. α-Pinene: Docking Study, Cytotoxicity, Mechanism of Action, and Anti-Biofilm Effect against Candida Albicans. Antibiotics 2023, 12, 480. [Google Scholar] [CrossRef] [PubMed]
- Astani, A.; Reichling, J.; Schnitzler, P. Comparative Study on the Antiviral Activity of Selected Monoterpenes Derived from Essential Oils. Phytother. Res. 2010, 24, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Khaleel, C.; Tabanca, N.; Buchbauer, G. α-Terpineol, a Natural Monoterpene: A Review of Its Biological Properties. Open Chem. 2018, 16, 349–361. [Google Scholar] [CrossRef]
- α-Terpineol. Available online: https://www.wikidata.org/wiki/Q27109437 (accessed on 1 May 2023).
- Held, S.; Schieberle, P.; Somoza, V. Characterization of α-Terpineol as an Anti-Inflammatory Component of Orange Juice by in Vitro Studies Using Oral Buccal Cells. J. Agric. Food Chem. 2007, 55, 8040–8046. [Google Scholar] [CrossRef] [PubMed]
- Sivropoulou, A.; Nikolaou, C.; Papanikolaou, E.; Kokkini, S.; Lanaras, T.; Arsenakis, M. Antimicrobial, Cytotoxic, and Antiviral Activities of Salvia Fructicosa Essential Oil. J. Agric. Food Chem. 1997, 45, 3197–3201. [Google Scholar] [CrossRef]
- Ehrnhöfer-Ressler, M.M.; Fricke, K.; Pignitter, M.; Walker, J.M.; Walker, J.; Rychlik, M.; Somoza, V. Identification of 1,8-Cineole, Borneol, Camphor, and Thujone as Anti-Inflammatory Compounds in a Salvia officinalis L. Infusion Using Human Gingival Fibroblasts. J. Agric. Food Chem. 2013, 61, 3451–3459. [Google Scholar] [CrossRef]
- (−)-α-Thujone. Available online: https://www.wikidata.org/wiki/Q421838 (accessed on 1 May 2023).
- β-Pinene. Available online: https://www.wikidata.org/wiki/Q300928 (accessed on 1 May 2023).
- Machado, T.Q.; Felisberto, J.R.S.; Guimarães, E.F.; Queiroz, G.A.D.; Fonseca, A.C.C.D.; Ramos, Y.J.; Marques, A.M.; Moreira, D.d.L.; Robbs, B.K. Apoptotic Effect of β-Pinene on Oral Squamous Cell Carcinoma as One of the Major Compounds from Essential Oil of Medicinal Plant Piper Rivinoides Kunth. Nat. Prod. Res. 2022, 36, 1636–1640. [Google Scholar] [CrossRef]
- Astani, A.; Schnitzler, P. Antiviral Activity of Monoterpenes Beta-Pinene and Limonene against Herpes Simplex Virus In Vitro. Iran. J. Microbiol. 2014, 6, 149–155. [Google Scholar]
- β-Thujone. Available online: https://www.wikidata.org/wiki/Q27121861 (accessed on 2 May 2023).
- Borneol. Available online: https://www.wikidata.org/wiki/Q27103499 (accessed on 2 May 2023).
- Croteau, R.; Lee Hooper, C.; Felton, M. Biosynthesis of Monoterpenes: Partial Purification and Characterization of a Bicyclic Monoterpenol Dehydrogenase from Sage (Salvia officinalis). Arch. Biochem. Biophys. 1978, 188, 182–193. [Google Scholar] [CrossRef]
- Camphor. Available online: https://www.wikidata.org/wiki/Q181559 (accessed on 2 May 2023).
- Lee, S.-H.; Kim, D.-S.; Park, S.-H.; Park, H. Phytochemistry and Applications of Cinnamomum Camphora Essential Oils. Molecules 2022, 27, 2695. [Google Scholar] [CrossRef] [PubMed]
- Carvacrol. Available online: https://www.wikidata.org/wiki/Q225543 (accessed on 2 May 2023).
- De Vincenzi, M.; Stammati, A.; De Vincenzi, A.; Silano, M. Constituents of Aromatic Plants: Carvacrol. Fitoterapia 2004, 75, 801–804. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.C.; Almeida, J.R.G.S.; Quintans, J.S.S.; Gopalsamy, R.G.; Shanmugam, S.; Serafini, M.R.; Oliveira, M.R.C.; Silva, B.A.F.; Martins, A.O.B.P.B.; Castro, F.F.; et al. Enhancement of Orofacial Antinociceptive Effect of Carvacrol, a Monoterpene Present in Oregano and Thyme Oils, by β-Cyclodextrin Inclusion Complex in Mice. Biomed. Pharmacother. 2016, 84, 454–461. [Google Scholar] [CrossRef] [PubMed]
- (RS)-Citronellal. Available online: https://www.wikidata.org/wiki/Q61651085 (accessed on 2 May 2023).
- Mahalwal, V.S.; Ali, M. Volatile Constituents of Cymbopogon nardus (Linn.) Rendle. Flavour Fragr. J. 2003, 18, 73–76. [Google Scholar] [CrossRef]
- Api, A.M.; Belsito, D.; Biserta, S.; Botelho, D.; Bruze, M.; Burton, G.A.; Buschmann, J.; Cancellieri, M.A.; Dagli, M.L.; Date, M.; et al. RIFM Fragrance Ingredient Safety Assessment, Citronellal, CAS Registry Number 106-23-0. Food Chem. Toxicol. 2021, 149, 111991. [Google Scholar] [CrossRef]
- Quintans-Júnior, L.J.; Melo, M.S.; De Sousa, D.P.; Araujo, A.A.S.; Onofre, A.C.S.; Gelain, D.P.; Gonçalves, J.C.R.; Araújo, D.A.M.; Almeida, J.R.G.S.; Bonjardim, L.R. Antinociceptive Effects of Citronellal in Formalin-, Capsaicin-, and Glutamate-Induced Orofacial Nociception in Rodents and Its Action on Nerve Excitability. J. Orofac. Pain 2010, 24, 305–312. [Google Scholar]
- (±)-β-Citronellol. Available online: https://www.wikidata.org/wiki/Q27122080 (accessed on 2 May 2023).
- Fekri, N.; El Amir, D.; Owis, A.; AbouZid, S. Studies on Essential Oil from Rose-Scented Geranium, Pelargonium graveolens L’Hérit. (Geraniaceae). Nat. Prod. Res. 2021, 35, 2593–2597. [Google Scholar] [CrossRef]
- Silva, D.; Diniz-Neto, H.; Cordeiro, L.; Silva-Neta, M.; Silva, S.; Andrade-Júnior, F.; Leite, M.; Nóbrega, J.; Morais, M.; Souza, J.; et al. (R)-(+)-β-Citronellol and (S)-(−)-β-Citronellol in Combination with Amphotericin B against Candida spp. Int. J. Mol. Sci. 2020, 21, 1785. [Google Scholar] [CrossRef]
- Sharma, Y.; Rastogi, S.K.; Perwez, A.; Rizvi, M.A.; Manzoor, N. β-Citronellol Alters Cell Surface Properties of Candida Albicans to Influence Pathogenicity Related Traits. Med. Mycol. 2020, 58, 93–106. [Google Scholar] [CrossRef]
- Eucalyptol. Available online: https://www.wikidata.org/wiki/Q161572 (accessed on 2 May 2023).
- Eugenol. Available online: https://www.wikidata.org/wiki/Q423357 (accessed on 2 May 2023).
- Mallavarapu, G.R.; Ramesh, S.; Chandrasekhara, R.S.; Rajeswara Rao, B.R.; Kaul, P.N.; Bhattacharya, A.K. Investigation of the Essential Oil of Cinnamon Leaf Grown at Bangalore and Hyderabad. Flavour Fragr. J. 1995, 10, 239–242. [Google Scholar] [CrossRef]
- Moon, S.-E.; Kim, H.-Y.; Cha, J.-D. Synergistic Effect between Clove Oil and Its Major Compounds and Antibiotics against Oral Bacteria. Arch. Oral Biol. 2011, 56, 907–916. [Google Scholar] [CrossRef] [PubMed]
- Ulanowska, M.; Olas, B. Biological Properties and Prospects for the Application of Eugenol—A Review. Int. J. Mol. Sci. 2021, 22, 3671. [Google Scholar] [CrossRef] [PubMed]
- Geraniol. Available online: https://www.wikidata.org/wiki/Q410836 (accessed on 2 May 2023).
- Martin, D.M.; Bohlmann, J. Identification of Vitis Vinifera (-)-Alpha-Terpineol Synthase by in Silico Screening of Full-Length cDNA ESTs and Functional Characterization of Recombinant Terpene Synthase. Phytochemistry 2004, 65, 1223–1229. [Google Scholar] [CrossRef] [PubMed]
- Madankumar, A.; Tamilarasi, S.; Premkumar, T.; Gopikrishnan, M.; Nagabhishek, N.; Devaki, T. Geraniol Attenuates 4NQO-Induced Tongue Carcinogenesis through Downregulating the Activation of NF-κB in Rats. Mol. Cell. Biochem. 2017, 434, 7–15. [Google Scholar] [CrossRef] [PubMed]
- β-Thujaplicin. Available online: https://www.wikidata.org/wiki/Q2705171 (accessed on 2 May 2023).
- Hiyoshi, T.; Domon, H.; Maekawa, T.; Yonezawa, D.; Kunitomo, E.; Tabeta, K.; Terao, Y. Protective Effect of Hinokitiol against Periodontal Bone Loss in Ligature-Induced Experimental Periodontitis in Mice. Arch. Oral Biol. 2020, 112, 104679. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.-H.; Chang, K.-W.; Hsia, S.-M.; Yu, C.-C.; Fuh, L.-J.; Chi, T.-Y.; Shieh, T.-M. In Vitro Antimicrobial and Anticancer Potential of Hinokitiol against Oral Pathogens and Oral Cancer Cell Lines. Microbiol. Res. 2013, 168, 254–262. [Google Scholar] [CrossRef]
- Lin, H.-C.; Wang, C.-C.; Wu, C.-F.; Lin, Y.-H.; Lee, W.-C.; Chen, P.-J.; Chang, Y.U.; Su, Y.-C. Hinokitiol Inhibits the Viability of Oral Squamous Carcinoma Cells by Inducing Apoptosis and Autophagy. Anticancer Res. 2023, 43, 1167–1173. [Google Scholar] [CrossRef]
- Domon, H.; Hiyoshi, T.; Maekawa, T.; Yonezawa, D.; Tamura, H.; Kawabata, S.; Yanagihara, K.; Kimura, O.; Kunitomo, E.; Terao, Y. Antibacterial Activity of Hinokitiol against Both Antibiotic-Resistant and -Susceptible Pathogenic Bacteria That Predominate in the Oral Cavity and Upper Airways. Microbiol. Immunol. 2019, 63, 213–222. [Google Scholar] [CrossRef]
- Morita, Y.; Sakagami, Y.; Okabe, T.; Ohe, T.; Inamori, Y.; Ishida, N. The Mechanism of the Bactericidal Activity of Hinokitiol. Biocontrol Sci. 2007, 12, 101–110. [Google Scholar] [CrossRef]
- Jin, X.; Zhang, M.; Lu, J.; Duan, X.; Chen, J.; Liu, Y.; Chang, W.; Lou, H. Hinokitiol Chelates Intracellular Iron to Retard Fungal Growth by Disturbing Mitochondrial Respiration. J. Adv. Res. 2021, 34, 65–77. [Google Scholar] [CrossRef]
- (+)-Isoborneol. Available online: https://www.wikidata.org/wiki/Q27270411 (accessed on 3 May 2023).
- (−)-Isoborneol. Available online: https://www.wikidata.org/wiki/Q15644616 (accessed on 3 May 2023).
- Armaka, M.; Papanikolaou, E.; Sivropoulou, A.; Arsenakis, M. Antiviral Properties of Isoborneol, a Potent Inhibitor of Herpes Simplex Virus Type 1. Antivir. Res. 1999, 43, 79–92. [Google Scholar] [CrossRef] [PubMed]
- (±)-Limonene. Available online: https://www.wikidata.org/wiki/Q278809 (accessed on 3 May 2023).
- Evans, W.C.; Evans, D. Volatile Oils and Resins. In Trease and Evans’ Pharmacognosy; Elsevier: Amsterdam, The Netherlands, 2009; pp. 263–303. ISBN 978-0-7020-2933-2. [Google Scholar]
- Thakre, A.; Zore, G.; Kodgire, S.; Kazi, R.; Mulange, S.; Patil, R.; Shelar, A.; Santhakumari, B.; Kulkarni, M.; Kharat, K.; et al. Limonene Inhibits Candida Albicans Growth by Inducing Apoptosis. Med. Mycol. 2018, 56, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Ahmedi, S.; Pant, P.; Raj, N.; Manzoor, N. Limonene Inhibits Virulence Associated Traits in Candida Albicans: In-Vitro and in-Silico Studies. Phytomed. Plus 2022, 2, 100285. [Google Scholar] [CrossRef]
- Hamdi, A.; Halouani, A.; Aouf, I.; Viaene, J.; Marzouk, B.; Kraiem, J.; Jaïdane, H.; Heyden, Y.V. Cytotoxicity and Antiviral Activities of Haplophyllum Tuberculatum Essential Oils, Pure Compounds, and Their Combinations against Coxsackievirus B3 and B4. Planta Med. 2021, 87, 827–835. [Google Scholar] [CrossRef] [PubMed]
- L-Menthol. Available online: https://www.wikidata.org/wiki/Q407418 (accessed on 9 May 2023).
- Taylor, D.J.R.; Hamid, S.M.; Andres, A.M.; Saadaeijahromi, H.; Piplani, H.; Germano, J.F.; Song, Y.; Sawaged, S.; Feuer, R.; Pandol, S.J.; et al. Antiviral Effects of Menthol on Coxsackievirus B. Viruses 2020, 12, 373. [Google Scholar] [CrossRef]
- Myrtenol. Available online: https://www.wikidata.org/wiki/Q15425810 (accessed on 3 May 2023).
- Varlet, V.; Augsburger, M. Monitoring of Aglycons of Yew Glycosides (3,5-Dimethoxyphenol, Myrtenol and 1-Octen-3-Ol) as First Indicator of Yew Presence. Drug Test. Anal. 2013, 5, 474–479. [Google Scholar] [CrossRef]
- Oliveira, J.P.; Abreu, F.F.; Bispo, J.M.M.; Cerqueira, A.R.A.; Dos Santos, J.R.; Correa, C.B.; Costa, S.K.P.; Camargo, E.A. Myrtenol Reduces Orofacial Nociception and Inflammation in Mice Through P38-MAPK and Cytokine Inhibition. Front. Pharmacol. 2022, 13, 910219. [Google Scholar] [CrossRef]
- Perillic Acid. Available online: https://www.wikidata.org/wiki/Q27104388 (accessed on 9 May 2023).
- Wang, X.-F.; Li, H.; Jiang, K.; Wang, Q.-Q.; Zheng, Y.-H.; Tang, W.; Tan, C.-H. Anti-Inflammatory Constituents from Perilla frutescens on Lipopolysaccharide-Stimulated RAW264.7 Cells. Fitoterapia 2018, 130, 61–65. [Google Scholar] [CrossRef]
- Mello, C.P.; Quirico-Santos, T.; Amorim, L.F.; Silva, V.G.; Fragel, L.M.; Bloom, D.C.; Paixão, I.P. Perillyl Alcohol and Perillic Acid Exert Efficient Action upon HSV-1 Maturation and Release of Infective Virus. Antivir. Ther. 2020, 25, 1–11. [Google Scholar] [CrossRef]
- Opdyke, D.L.J. Monographs on Fragrance Raw Materials. Food Cosmet. Toxicol. 1981, 19, 237–254. [Google Scholar] [CrossRef]
- Karp, F.; Mihaliak, C.A.; Harris, J.L.; Croteau, R. Monoterpene Biosynthesis: Specificity of the Hydroxylations of (−)-Limonene by Enzyme Preparations from Peppermint (Mentha piperita), Spearmint (Mentha spicata), and Perilla (Perilla frutescens) Leaves. Arch. Biochem. Biophys. 1990, 276, 219–226. [Google Scholar] [CrossRef]
- Perillyl Alcohol. Available online: https://www.wikidata.org/wiki/Q15391928 (accessed on 9 May 2023).
- Wagner, C.S.; De Gezelle, J.; Robertson, M.; Robertson, K.; Wilson, M.; Komarnytsky, S. Antibacterial Activity of Medicinal Plants from The Physicians of Myddvai, a 14th Century Welsh Medical Manuscript. J. Ethnopharmacol. 2017, 203, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Dosoky, N.S.; Satyal, P.; Barata, L.M.; da Silva, J.K.R.; Setzer, W.N. Volatiles of Black Pepper Fruits (Piper nigrum L.). Molecules 2019, 24, 4244. [Google Scholar] [CrossRef] [PubMed]
- Sabinene. Available online: https://www.wikidata.org/wiki/Q421278 (accessed on 3 May 2023).
- Park, B.-I.; Kim, B.-S.; Kim, K.-J.; You, Y.-O. Sabinene Suppresses Growth, Biofilm Formation, and Adhesion of Streptococcus Mutans by Inhibiting Cariogenic Virulence Factors. J. Oral Microbiol. 2019, 11, 1632101. [Google Scholar] [CrossRef]
- Thymol. Available online: https://www.wikidata.org/wiki/Q408883 (accessed on 3 May 2023).
- Salehi, B.; Mishra, A.P.; Shukla, I.; Sharifi-Rad, M.; Contreras, M.D.M.; Segura-Carretero, A.; Fathi, H.; Nasrabadi, N.N.; Kobarfard, F.; Sharifi-Rad, J. Thymol, Thyme, and Other Plant Sources: Health and Potential Uses. Phytother. Res. 2018, 32, 1688–1706. [Google Scholar] [CrossRef] [PubMed]
- Priya, A.; Selvaraj, A.; Divya, D.; Karthik Raja, R.; Pandian, S.K. In Vitro and In Vivo Anti-Infective Potential of Thymol Against Early Childhood Caries Causing Dual Species Candida Albicans and Streptococcus Mutans. Front. Pharmacol. 2021, 12, 760768. [Google Scholar] [CrossRef]
- Khan, S.T.; Khan, M.; Ahmad, J.; Wahab, R.; Abd-Elkader, O.H.; Musarrat, J.; Alkhathlan, H.Z.; Al-Kedhairy, A.A. Thymol and Carvacrol Induce Autolysis, Stress, Growth Inhibition and Reduce the Biofilm Formation by Streptococcus Mutans. AMB Express 2017, 7, 49. [Google Scholar] [CrossRef]
- De La Chapa, J.J.; Singha, P.K.; Lee, D.R.; Gonzales, C.B. Thymol Inhibits Oral Squamous Cell Carcinoma Growth via Mitochondria-Mediated Apoptosis. J. Oral Pathol. Med. Off. Publ. Int. Assoc. Oral Pathol. Am. Acad. Oral Pathol. 2018, 47, 674–682. [Google Scholar] [CrossRef]
- Jafri, H.; Ahmad, I. Thymus Vulgaris Essential Oil and Thymol Inhibit Biofilms and Interact Synergistically with Antifungal Drugs against Drug Resistant Strains of Candida Albicans and Candida Tropicalis. J. Mycol. Médicale 2020, 30, 100911. [Google Scholar] [CrossRef]
- Kotan, R.; Kordali, S.; Cakir, A. Screening of Antibacterial Activities of Twenty-One Oxygenated Monoterpenes. Z. Für Naturforschung C 2007, 62, 507–513. [Google Scholar] [CrossRef]
- Pattnaik, S.; Subramanyam, V.R.; Bapaji, M.; Kole, C.R. Antibacterial and Antifungal Activity of Aromatic Constituents of Essential Oils. Microbios 1997, 89, 39–46. [Google Scholar] [PubMed]
- Kilian, M.; Chapple, I.L.C.; Hannig, M.; Marsh, P.D.; Meuric, V.; Pedersen, A.M.L.; Tonetti, M.S.; Wade, W.G.; Zaura, E. The Oral Microbiome—An Update for Oral Healthcare Professionals. Br. Dent. J. 2016, 221, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Al-Manei, K.; Ghorbani, M.; Naud, S.; Al-Manei, K.K.; Sobkowiak, M.J.; Lund, B.; Hazirolan, G.; Sällberg Chen, M.; Özenci, V. Clinical Microbial Identification of Severe Oral Infections by MALDI-TOF Mass Spectrometry in Stockholm County: An 11-Year (2010 to 2020) Epidemiological Investigation. Microbiol. Spectr. 2022, 10, e02487-22. [Google Scholar] [CrossRef]
- de Jongh, C.A.; de Vries, T.J.; Bikker, F.J.; Gibbs, S.; Krom, B.P. Mechanisms of Porphyromonas Gingivalis to Translocate over the Oral Mucosa and Other Tissue Barriers. J. Oral Microbiol. 2023, 15, 2205291. [Google Scholar] [CrossRef]
- Bifulco, M.; Amato, M.; Gangemi, G.; Marasco, M.; Caggiano, M.; Amato, A.; Pisanti, S. Dental Care and Dentistry Practice in the Medieval Medical School of Salerno. Br. Dent. J. 2016, 221, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and Multi-National Prevalence of Fungal Diseases—Estimate Precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef]
- WHO. Fungal Priority Pathogens List to Guide Research, Development and Public Health Action; World Health Organization: Geneva, Switzerland, 2022.
- Jensena, J.L.; Barkvoll, P. Clinical Implications of the Dry Mouth: Oral Mucosal Diseases. Ann. N. Y. Acad. Sci. 1998, 842, 156–162. [Google Scholar] [CrossRef]
- Shaban, S.; Patel, M.; Ahmad, A. Improved Efficacy of Antifungal Drugs in Combination with Monoterpene Phenols against Candida Auris. Sci. Rep. 2020, 10, 1162. [Google Scholar] [CrossRef]
- Fourie, R.; Kuloyo, O.O.; Mochochoko, B.M.; Albertyn, J.; Pohl, C.H. Iron at the Centre of Candida Albicans Interactions. Front. Cell. Infect. Microbiol. 2018, 8, 185. [Google Scholar] [CrossRef]
- Neville, B.W.; Damm, D.D.; Allen, C.M.; Chi, A.C. Chapter 7 Viral Infections. In Oral and Maxillofacial Pathology; Elsevier Health Sciences: Amsterdam, The Netherlands, 2015; ISBN 978-1-4557-7052-6. [Google Scholar]
- Mouth and Oral Cancer Statistics. Available online: https://www.wcrf.org/cancer-trends/mouth-and-oral-cancer-statistics/ (accessed on 14 February 2023).
- Cancer Facts & Figures 2022; American Cancer Society: Atlanta, GA, USA, 2022.
- NSAIDs. Available online: https://www.nhs.uk/conditions/nsaids/ (accessed on 15 February 2023).
- Finoti, L.S.; Nepomuceno, R.; Pigossi, S.C.; Corbi, S.C.; Secolin, R.; Scarel-Caminaga, R.M. Association between Interleukin-8 Levels and Chronic Periodontal Disease: A PRISMA-Compliant Systematic Review and Meta-Analysis. Medicine 2017, 96, e6932. [Google Scholar] [CrossRef]
- Caldeira, F.I.D.; Hidalgo, M.A.R.; De Carli Dias, M.L.; Scarel-Caminaga, R.M.; Pigossi, S.C. Systematic Review of Ratios between Disease /Health Periodontitis Modulators and Meta-Analysis of Their Levels in Gingival Tissue and Biological Fluids. Arch. Oral Biol. 2021, 127, 105147. [Google Scholar] [CrossRef] [PubMed]
- Plemmenos, G.; Evangeliou, E.; Polizogopoulos, N.; Chalazias, A.; Deligianni, M.; Piperi, C. Central Regulatory Role of Cytokines in Periodontitis and Targeting Options. Curr. Med. Chem. 2021, 28, 3032–3058. [Google Scholar] [CrossRef]
- Pau, A.; Croucher, R.; Marcenes, W.; Leung, T. Development and Validation of a Dental Pain-Screening Questionnaire. Pain 2005, 119, 75–81. [Google Scholar] [CrossRef]
- Luccarini, P.; Childeric, A.; Gaydier, A.-M.; Voisin, D.; Dallel, R. The Orofacial Formalin Test in the Mouse: A Behavioral Model for Studying Physiology and Modulation of Trigeminal Nociception. J. Pain 2006, 7, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Janakiram, C.; Venkitachalam, R.; Fontelo, P.; Iafolla, T.J.; Dye, B.A. Effectiveness of Herbal Oral Care Products in Reducing Dental Plaque & Gingivitis—A Systematic Review and Meta-Analysis. BMC Complement. Med. Ther. 2020, 20, 43. [Google Scholar] [CrossRef]
- Kroona, L.; Warfvinge, G.; Isaksson, M.; Ahlgren, C.; Dahlin, J.; Sörensen, Ö.; Bruze, M. Quantification of L-Carvone in Toothpastes Available on the Swedish Market. Contact Dermat. 2017, 77, 224–230. [Google Scholar] [CrossRef]
- Iha, K.; Suzuki, N.; Yoneda, M.; Takeshita, T.; Hirofuji, T. Effect of Mouth Cleaning with Hinokitiol-Containing Gel on Oral Malodor: A Randomized, Open-Label Pilot Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 433–439. [Google Scholar] [CrossRef]
- Smyle Toothpaste Tabs Ingredients. Available online: https://wesmyle.com/pages/ingredients (accessed on 5 April 2023).
- Refresher Toothpaste Tabs. Available online: https://www.lushusa.com/face/oral-care/refresher/9999961260.html (accessed on 2 March 2023).
- Adams, D.; Addy, M. Mouthrinses. Adv. Dent. Res. 1994, 8, 291–301. [Google Scholar] [CrossRef]
- Radzki, D.; Wilhelm-Węglarz, M.; Pruska, K.; Kusiak, A.; Ordyniec-Kwaśnica, I. A Fresh Look at Mouthwashes-What Is Inside and What Is It for? Int. J. Environ. Res. Public Health 2022, 19, 3926. [Google Scholar] [CrossRef]
- PNGEgg—Image Hosting. Available online: https://www.pngegg.com/ (accessed on 7 August 2023).
- Silva, M.F.; Leite, F.R.M.; Ferreira, L.B.; Pola, N.M.; Scannapieco, F.A.; Demarco, F.F.; Nascimento, G.G. Estimated Prevalence of Halitosis: A Systematic Review and Meta-Regression Analysis. Clin. Oral Investig. 2018, 22, 47–55. [Google Scholar] [CrossRef]
- Kapoor, U.; Sharma, G.; Juneja, M.; Nagpal, A. Halitosis: Current Concepts on Etiology, Diagnosis and Management. Eur. J. Dent. 2016, 10, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Nakasugi, T.; Murakawa, T.; Shibuya, K.; Morimoto, M. Deodorizing Substance in Black Cumin (Nigella sativa L.) Seed Oil. J. Oleo Sci. 2017, 66, 877–882. [Google Scholar] [CrossRef]
- Osada, K.; Hanawa, M.; Tsunoda, K.; Izumi, H. Evaluation of the Masking of Dimethyl Sulfide Odors by Citronellal, Limonene and Citral through the Use of Trained Odor Sensor Mice. Chem. Senses 2013, 38, 57–65. [Google Scholar] [CrossRef]
- Ma, L.; Pang, C.; Yan, C.; Chen, J.; Wang, X.; Hui, J.; Zhou, L.; Zhang, X. Effect of Lemon Essential Oil on Halitosis. Oral Dis. 2022, 29, 1845–1854. [Google Scholar] [CrossRef] [PubMed]
- Satthanakul, P.; Taweechaisupapong, S.; Paphangkorakit, J.; Pesee, M.; Timabut, P.; Khunkitti, W. Antimicrobial Effect of Lemongrass Oil against Oral Malodour Micro-Organisms and the Pilot Study of Safety and Efficacy of Lemongrass Mouthrinse on Oral Malodour. J. Appl. Microbiol. 2015, 118, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; World Health Organization: Geneva, Switzerland, 2022.
- Xiao, J.; Huang, X.; Alkhers, N.; Alzamil, H.; Alzoubi, S.; Wu, T.T.; Castillo, D.A.; Campbell, F.; Davis, J.; Herzog, K.; et al. Candida Albicans and Early Childhood Caries: A Systematic Review and Meta-Analysis. Caries Res. 2018, 52, 102–112. [Google Scholar] [CrossRef]
- Parisotto, T.M.; Steiner-Oliveira, C.; Silva, C.M.; Rodrigues, L.K.; Nobre-dos-Santos, M. Early Childhood Caries and Mutans Streptococci: A Systematic Review. Oral Health Prev. Dent. 2010, 8, 59–70. [Google Scholar]
- Kirthiga, M.; Murugan, M.; Saikia, A.; Kirubakaran, R. Risk Factors for Early Childhood Caries: A Systematic Review and Meta-Analysis of Case Control and Cohort Studies. Pediatr. Dent. 2019, 41, 95–112. [Google Scholar]
- Orlova, E.; Dudding, T.; Chernus, J.M.; Alotaibi, R.N.; Haworth, S.; Crout, R.J.; Lee, M.K.; Mukhopadhyay, N.; Feingold, E.; Levy, S.M.; et al. Association of Early Childhood Caries with Bitter Taste Receptors: A Meta-Analysis of Genome-Wide Association Studies and Transcriptome-Wide Association Study. Genes 2022, 14, 59. [Google Scholar] [CrossRef]
- Flamee, S.; Gizani, S.; Caroni, C.; Papagiannoulis, L.; Twetman, S. Effect of a Chlorhexidine/Thymol and a Fluoride Varnish on Caries Development in Erupting Permanent Molars: A Comparative Study. Eur. Arch. Paediatr. Dent. 2015, 16, 449–454. [Google Scholar] [CrossRef]
- Splieth, C.; Steffen, H.; Rosin, M.; Welk, A. Caries Prevention with Chlorhexidine-Thymol Varnish in High Risk Schoolchildren. Community Dent. Oral Epidemiol. 2000, 28, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Ben Khadra, G.M.; Arrag, E.A.; Alammori, M.; AlKadi, M.F. The Effect of Chlorhexidine-Thymol and Fluoride Varnishes on the Levels of Streptococcus Mutans in Saliva in Children Aged 6–8 Years. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 2019, 30, 67–72. [Google Scholar] [CrossRef]
- Marchese, A.; Orhan, I.E.; Daglia, M.; Barbieri, R.; Di Lorenzo, A.; Nabavi, S.F.; Gortzi, O.; Izadi, M.; Nabavi, S.M. Antibacterial and Antifungal Activities of Thymol: A Brief Review of the Literature. Food Chem. 2016, 210, 402–414. [Google Scholar] [CrossRef] [PubMed]
- Brailsford, S.R.; Fiske, J.; Gilbert, S.; Clark, D.; Beighton, D. The Effects of the Combination of Chlorhexidine/Thymol- and Fluoride-Containing Varnishes on the Severity of Root Caries Lesions in Frail Institutionalised Elderly People. J. Dent. 2002, 30, 319–324. [Google Scholar] [CrossRef]
- Baca, P.; Clavero, J.; Baca, A.P.; González-Rodríguez, M.P.; Bravo, M.; Valderrama, M.J. Effect of Chlorhexidine-Thymol Varnish on Root Caries in a Geriatric Population: A Randomized Double-Blind Clinical Trial. J. Dent. 2009, 37, 679–685. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, P.; Wang, L.; Shi, Y.; Chen, J.; Wang, H.; Zhang, X. Inhibitory Effects of Citrus Lemon Oil and Limonene on Streptococcus Sobrinus—Induced Dental Caries in Rats. Arch. Oral Biol. 2020, 118, 104851. [Google Scholar] [CrossRef]
- Ma, L.; Chen, J.; Han, H.; Liu, P.; Wang, H.; Lin, S.; Zhang, Q.; Lu, D.; Zhang, X. Effects of Lemon Essential Oil and Limonene on the Progress of Early Caries: An In Vitro Study. Arch. Oral Biol. 2020, 111, 104638. [Google Scholar] [CrossRef]
- Huang, M.-H.; Shen, Y.-F.; Hsu, T.-T.; Huang, T.-H.; Shie, M.-Y. Physical Characteristics, Antimicrobial and Odontogenesis Potentials of Calcium Silicate Cement Containing Hinokitiol. Mater. Sci. Eng. C 2016, 65, 1–8. [Google Scholar] [CrossRef]
- Shieh, T.-M.; Hsu, S.-M.; Chang, K.-C.; Chen, W.-C.; Lin, D.-J. Calcium Phosphate Cement with Antimicrobial Properties and Radiopacity as an Endodontic Material. Materials 2017, 10, 1256. [Google Scholar] [CrossRef]
- Liu, X.; Xu, J.; Li, S.; Wang, X.; Liu, J.; Li, X. The Prevalence of Gingivitis and Related Risk Factors in Schoolchildren Aged 6-12 Years Old. BMC Oral Health 2022, 22, 623. [Google Scholar] [CrossRef]
- Erchick, D.J.; Rai, B.; Agrawal, N.K.; Khatry, S.K.; Katz, J.; LeClerq, S.C.; Reynolds, M.A.; Mullany, L.C. Oral Hygiene, Prevalence of Gingivitis, and Associated Risk Factors among Pregnant Women in Sarlahi District, Nepal. BMC Oral Health 2019, 19, 2. [Google Scholar] [CrossRef]
- Kassab, M.M.; Cohen, R.E. The Etiology and Prevalence of Gingival Recession. J. Am. Dent. Assoc. 2003, 134, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Botelho, M.A.; Martins, J.G.; Ruela, R.S.; Rachid, I.; Santos, J.A.; Soares, J.B.; França, M.C.; Montenegro, D.; Ruela, W.S.; Barros, L.P.; et al. Protective Effect of Locally Applied Carvacrol Gel on Ligature-Induced Periodontitis in Rats: A Tapping Mode AFM Study. Phytother. Res. 2009, 23, 1439–1448. [Google Scholar] [CrossRef]
- Botelho, M.A.; Rao, V.S.; Montenegro, D.; Bandeira, M.A.M.; Fonseca, S.G.C.; Nogueira, N.A.P.; Ribeiro, R.A.; Brito, G.A.C. Effects of a Herbal Gel Containing Carvacrol and Chalcones on Alveolar Bone Resorption in Rats on Experimental Periodontitis. Phytother. Res. 2008, 22, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Kuo, P.-J.; Hung, T.-F.; Lin, C.-Y.; Hsiao, H.-Y.; Fu, M.-W.; Hong, P.-D.; Chiu, H.-C.; Fu, E. Carvacrol Ameliorates Ligation-Induced Periodontitis in Rats. J. Periodontol. 2017, 88, e120–e128. [Google Scholar] [CrossRef]
- Zhuang, C.; Zhang, W.; Sheng, C.; Zhang, W.; Xing, C.; Miao, Z. Chalcone: A Privileged Structure in Medicinal Chemistry. Chem. Rev. 2017, 117, 7762–7810. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.J.; Campbell, P.M.; Rees, T.D.; Buschang, P.H. A Randomized Controlled Trial Evaluating Antioxidant–Essential Oil Gel as a Treatment for Gingivitis in Orthodontic Patients. Angle Orthod. 2016, 86, 407–412. [Google Scholar] [CrossRef]
- Alvarez Echazú, M.I.; Olivetti, C.E.; Anesini, C.; Perez, C.J.; Alvarez, G.S.; Desimone, M.F. Development and Evaluation of Thymol-Chitosan Hydrogels with Antimicrobial-Antioxidant Activity for Oral Local Delivery. Mater. Sci. Eng. C 2017, 81, 588–596. [Google Scholar] [CrossRef]
- Patole, V.C.; Chaudhari, S.P. Eugenyl Methacrylate Microsponges Loaded with Eugenol Incorporated In Situ Gel for Treatment of Periodontitis. J. Pharm. Innov. 2021, 16, 408–418. [Google Scholar] [CrossRef]
- Patole, V.C.; Chaudhari, S.P. Development of Thymol Microsponges Loaded in Situ Gel for the Treatment of Periodontitis. Curr. Drug Deliv. 2021, 18, 71–87. [Google Scholar] [CrossRef]
- Weinberg, M.A.; Maloney, W.J. Treatment of Common Oral Lesions. Available online: https://www.uspharmacist.com/article/treatment-of-common-oral-lesions (accessed on 27 March 2023).
- do Nascimento-Júnior, B.J.; Brito, L.S.; Barros, W.N.; Gonçalves, D.M.; Matos, L.S.; Nascimento, C.R.B.; Ribeiro, L.A.A.; de Lima, R.S.; Silva-Júnior, R.G.C.; Reis, S.A.G.B.; et al. Anti-Inflammatory and Healing Action of Oral Gel Containing Borneol Monoterpene in Chemotherapy-Induced Mucositis in Rats (Rattus Norvegicus). Braz. J. Pharm. Sci. 2017, 53, e00081. [Google Scholar] [CrossRef]
- Ghaderi, F.; Ebrahimi, E.; Sari Aslani, F.; Koohi-Hosseinabadi, O.; Koohpeyma, F.; Irajie, C.; Tanideh, N.; Iraji, A. The Effect of Hydroalcoholic Extract of Psidium guajava L. on Experimentally Induced Oral Mucosal Wound in Rat. BMC Complement. Med. Ther. 2022, 22, 201. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, A.; Lodi, G.; Porter, S.; Fedele, S.; Mercadante, V. Interventions for Dry Mouth and Hyposalivation in Sjögren’s Syndrome: A Systematic Review and Meta-Analysis. Oral Dis. 2019, 25, 1027–1047. [Google Scholar] [CrossRef] [PubMed]
- Furness, S.; Worthington, H.V.; Bryan, G.; Birchenough, S.; McMillan, R. Interventions for the Management of Dry Mouth: Topical Therapies. Cochrane Database Syst. Rev. 2011, 12, CD008934. [Google Scholar] [CrossRef] [PubMed]
- Brand, H.S.; Ouzzine, R.; Bots, C.P. Sticky Saliva Products. Br. Dent. J. 2013, 214, 95. [Google Scholar] [CrossRef]
- Niklander, S.E.; Martínez, M.; Miranda, A.; Rodriguez, M. Treatment Alternatives for Dry Mouth: A Scoping Review. J. Clin. Exp. Dent. 2022, 14, e846–e853. [Google Scholar] [CrossRef]
- Assy, Z.; Bikker, F.J.; Mashhour, E.; Asadi, M.; Brand, H.S. Preferences of Sjögren’s Syndrome Patients Regarding Potential New Saliva Substitutes. Clin. Oral Investig. 2022, 26, 6245–6252. [Google Scholar] [CrossRef]
- Zhang, M.; Zhao, R.; Wang, D.; Wang, L.; Zhang, Q.; Wei, S.; Lu, F.; Peng, W.; Wu, C. Ginger Zingiber officinale and Its Bioactive Components Are Potential Resources for Health Beneficial Agents. Phytother. Res. 2021, 35, 711–742. [Google Scholar] [CrossRef]
- Wohlmuth, H.; Smith, M.K.; Brooks, L.O.; Myers, S.P.; Leach, D.N. Essential Oil Composition of Diploid and Tetraploid Clones of Ginger (Zingiber officinale Roscoe) Grown in Australia. J. Agric. Food Chem. 2006, 54, 1414–1419. [Google Scholar] [CrossRef]
- Gupta, S.; Pandotra, P.; Ram, G.; Anand, R.; Gupta, A.P.; Husain, M.K.; Bedi, Y.S.; Mallavarapu, G.R. Composition of a Monoterpenoid-Rich Essential Oil from the Rhizome of Zingiber officinale from North Western Himalayas. Nat. Prod. Commun. 2011, 6, 1934578X1100600122. [Google Scholar] [CrossRef]
- Kan, C.Y.; H’ng, J.X.; Goh, A.; Smales, F.; Tan, E.L.; Zhang, S.; Pichika, M.R.; Parolia, A. Effect of Sustained Systemic Administration of Ginger (Z officinale) Rhizome Extracts on Salivary Flow in Mice. Int. Dent. J. 2023, 73, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, M.; Silva, M.; Moncada, M.; Bernardo, M.; Silva, M.; Proença, L. Effect of a Ginger Infusion in Smokers with Reduced Salivary Flow Rate. Int. J. Clin. Res. Trials 2018, 3, 121. [Google Scholar] [CrossRef]
- Mardani, H.; Ghannadi, A.; Rashnavadi, B.; Kamali, R. The Effect of Ginger Herbal Spray on Reducing Xerostomia in Patients with Type II Diabetes. Avicenna J. Phytomed. 2017, 7, 308–316. [Google Scholar]
- Delfine, S.; Marrelli, M.; Conforti, F.; Formisano, C.; Rigano, D.; Menichini, F.; Senatore, F. Variation of Malva Sylvestris Essential Oil Yield, Chemical Composition and Biological Activity in Response to Different Environments across Southern Italy. Ind. Crops Prod. 2017, 98, 29–37. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Melgar-Lalanne, G.; Hernández-Álvarez, A.J.; Taheri, Y.; Shaheen, S.; Kregiel, D.; Antolak, H.; Pawlikowska, E.; Brdar-Jokanović, M.; Rajkovic, J.; et al. Malva Species: Insights on Its Chemical Composition towards Pharmacological Applications. Phytother. Res. 2020, 34, 546–567. [Google Scholar] [CrossRef] [PubMed]
- Ameri, A.; Heydarirad, G.; Rezaeizadeh, H.; Choopani, R.; Ghobadi, A.; Gachkar, L. Evaluation of Efficacy of an Herbal Compound on Dry Mouth in Patients with Head and Neck Cancers: A Randomized Clinical Trial. J. Evid.-Based Complement. Altern. Med. 2016, 21, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Heydarirad, G.; Rezaeizadeh, H.; Choopani, R.; Mosavat, S.H.; Ameri, A. Efficacy of a Traditional Persian Medicine Preparation for Radiation-Induced Xerostomia: A Randomized, Open-Label, Active-Controlled Trial. J. Integr. Med. 2017, 15, 201–208. [Google Scholar] [CrossRef]
- Firoznejhad, M.; Ghasemi Pirbalouti, A.; Abdoosi, V.; Aliahmadi, A. Chemical Composition of Essential Oils from the Underground Parts of Glycyrrhiza echinata L. Accessions Growing Wild in Northern Iran. Nat. Prod. Res. 2021, 35, 162–166. [Google Scholar] [CrossRef]
- Yu, I.-C.; Tsai, Y.-F.; Fang, J.-T.; Yeh, M.-M.; Fang, J.-Y.; Liu, C.-Y. Effects of Mouthwash Interventions on Xerostomia and Unstimulated Whole Saliva Flow Rate among Hemodialysis Patients: A Randomized Controlled Study. Int. J. Nurs. Stud. 2016, 63, 9–17. [Google Scholar] [CrossRef]
- Deng, W.; Liu, K.; Cao, S.; Sun, J.; Zhong, B.; Chun, J. Chemical Composition, Antimicrobial, Antioxidant, and Antiproliferative Properties of Grapefruit Essential Oil Prepared by Molecular Distillation. Molecules 2020, 25, 217. [Google Scholar] [CrossRef]
- Suda, K.; Takahashi, Y.; Matsuki-Fukushima, M.; Satoh, K. Effect of the Scent from Grapefruit Oil on Salivary Secretion in Rats. Int. J. Oral-Med. Sci. 2010, 9, 31–35. [Google Scholar] [CrossRef]
- Yamagami, A.; Imura, H.; Shibuya, K.; Murakawa, T.; Kono, Y.; Sugimoto, K. Effects of aroma on saliva secretion and activities of autonomic nerves and brain; Essential oil of kuromoji and bergamot. Jpn. J. Taste Smell Res. 2012, 19, 453–456. [Google Scholar]
- Nanashima, N.; Kitajima, M.; Takamagi, S.; Fujioka, M.; Tomisawa, T. Comparison of Chemical Composition between Kuromoji (Lindera Umbellata) Essential Oil and Hydrosol and Determination of the Deodorizing Effect. Molecules 2020, 25, 4195. [Google Scholar] [CrossRef] [PubMed]
- Sawamura, M.; Onishi, Y.; Ikemoto, J.; Tu, N.T.M.; Phi, N.T.L. Characteristic Odour Components of Bergamot (Citrus bergamia Risso) Essential Oil. Flavour Fragr. J. 2006, 21, 609–615. [Google Scholar] [CrossRef]
- Nakayama, M.; Okizaki, A.; Takahashi, K. A Randomized Controlled Trial for the Effectiveness of Aromatherapy in Decreasing Salivary Gland Damage Following Radioactive Iodine Therapy for Differentiated Thyroid Cancer. BioMed Res. Int. 2016, 2016, 9509810. [Google Scholar] [CrossRef]
- Faruque, M.R.J.; Nazmi, K.; van Splunter, A.; Laine, M.L.; Bikker, F.J. Sialogogic Effects through Olfactory Stimulation with Mastic Resin and α-Pinene Volatiles In Vivo. Biomed. Pharmacother. 2023; accepted. [Google Scholar]
- Houghton, J.W.; Carpenter, G.; Hans, J.; Pesaro, M.; Lynham, S.; Proctor, G. Agonists of Orally Expressed TRP Channels Stimulate Salivary Secretion and Modify the Salivary Proteome. Mol. Cell. Proteom. MCP 2020, 19, 1664–1676. [Google Scholar] [CrossRef]
- Sarrami, N.; Pemberton, M.N.; Thornhill, M.H.; Theaker, E.D. Adverse Reactions Associated with the Use of Eugenol in Dentistry. Br. Dent. J. 2002, 193, 257–259. [Google Scholar] [CrossRef]
- Barkin, M.E.; Boyd, J.P.; Cohen, S. Acute Allergic Reaction to Eugenol. Oral Surg. Oral Med. Oral Pathol. 1984, 57, 441–442. [Google Scholar] [CrossRef]
- Deshpande, A.; Verma, S.; Macwan, C. Allergic Reaction Associated with the Use of Eugenol Containing Dental Cement in a Young Child. Austin J. Dent. 2014, 1, 1007. [Google Scholar]
- Tammannavar, P.; Pushpalatha, C.; Jain, S.; SV, S. An Unexpected Positive Hypersensitive Reaction to Eugenol. BMJ Case Rep. 2013, 2013, bcr2013009464. [Google Scholar] [CrossRef] [PubMed]
- Silvestre, J.F.; Albares, M.P.; Blanes, M.; Pascual, J.C.; Pastor, N. Allergic Contact Gingivitis Due to Eugenol Present in a Restorative Dental Material. Contact Dermat. 2005, 52, 341. [Google Scholar] [CrossRef] [PubMed]
- Bhalla, M.; Thami, G.P. Acute Urticaria Due to Dental Eugenol. Allergy 2003, 58, 158. [Google Scholar] [CrossRef] [PubMed]
- Bui, T.N.P.T.; Mose, K.F.; Andersen, F. Eugenol Allergy Mimicking Burning Mouth Syndrome. Contact Dermat. 2019, 80, 54–55. [Google Scholar] [CrossRef] [PubMed]
- Navarro Triviño, F.J.; Cuenca-Barrales, C.; Ruiz-Villaverde, R. Eugenol Allergy Mimicking Recurrent Aphthous Stomatitis and Burning Mouth Syndrome. Contact Dermat. 2019, 81, 462–463. [Google Scholar] [CrossRef]
- de Groot, A. Contact Allergy to (Ingredients of) Toothpastes. Dermatitis 2017, 28, 95–114. [Google Scholar] [CrossRef]
- Bourgeois, P.; Goossens, A. Allergic Contact Cheilitis Caused by Menthol in Toothpaste and Throat Medication: A Case Report. Contact Dermat. 2016, 75, 113–115. [Google Scholar] [CrossRef]
- Worm, M.; Jeep, S.; Sterry, W.; Zuberbier, T. Perioral Contact Dermatitis Caused by L-Carvone in Toothpaste. Contact Dermat. 1998, 38, 338. [Google Scholar] [CrossRef]
- Hansson, C.; Bergendorff, O.; Wallengren, J. Contact Urticaria Caused by Carvone in Toothpaste. Contact Dermat. 2011, 65, 362–364. [Google Scholar] [CrossRef]
- Corazza, M.; Levratti, A.; Virgili, A. Allergic Contact Cheilitis Due to Carvone in Toothpastes. Contact Dermat. 2002, 46, 366–367. [Google Scholar] [CrossRef]
- Kroona, L.; Ahlgren, C.; Dahlin, J.; Isaksson, M.; Bruze, M. Use Test with L-Carvone in Toothpaste on Sensitized Individuals. Contact Dermat. 2023, 88, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Kroona, L.; Isaksson, M.; Ahlgren, C.; Dahlin, J.; Bruze, M.; Warfvinge, G. Carvone Contact Allergy in Southern Sweden: A 21-Year Retrospective Study. Acta Derm. Venereol. 2018, 98, 938–942. [Google Scholar] [CrossRef] [PubMed]
- European Chemicals Agency (ECHA). Available online: https://echa.europa.eu (accessed on 10 May 2023).
- Generally Recognized as Safe (GRAS). Available online: https://www.fda.gov/food/food-ingredients-packaging/generally-recognized-safe-gras (accessed on 10 May 2023).
- Api, A.M.; Belsito, D.; Botelho, D.; Bruze, M.; Burton, G.A.; Buschmann, J.; Cancellieri, M.A.; Dagli, M.L.; Date, M.; Dekant, W.; et al. Update to RIFM Fragrance Ingredient Safety Assessment, Eugenol, CAS Registry Number 97-53-0. Food Chem. Toxicol. 2022, 163, 113027. [Google Scholar] [CrossRef]
- Api, A.M.; Belsito, D.; Botelho, D.; Bruze, M.; Burton, G.A.; Buschmann, J.; Cancellieri, M.A.; Dagli, M.L.; Date, M.; Dekant, W.; et al. RIFM Fragrance Ingredient Safety Assessment, α-Pinene, CAS Registry Number 80-56-8. Food Chem. Toxicol. 2022, 159, 112702. [Google Scholar] [CrossRef]
- Nikolić, B.; Vasilijević, B.; Mitić-Ćulafić, D.; Vuković-Gačić, B.; Knežević-Vukćević, J. Comparative Study of Genotoxic, Antigenotoxic and Cytotoxic Activities of Monoterpenes Camphor, Eucalyptol and Thujone in Bacteria and Mammalian Cells. Chem. Biol. Interact. 2015, 242, 263–271. [Google Scholar] [CrossRef]
- Koh, T.; Machino, M.; Murakami, Y.; Umemura, N.; Sakagami, H. Cytotoxicity of Dental Compounds towards Human Oral Squamous Cell Carcinoma and Normal Oral Cells. In Vivo 2013, 27, 85–95. [Google Scholar] [PubMed]
- Souza, A.C.S.; Silva, L.K.; Queiroz, T.B.; Marques, E.S.; Hiruma-Lima, C.A.; Gaivão, I.O.M.; Maistro, E.L. Citral Presents Cytotoxic and Genotoxic Effects in Human Cultured Cells. Drug Chem. Toxicol. 2020, 43, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Wessels, M.; Rimkus, J.; Leyhausen, G.; Volk, J.; Geurtsen, W. Genotoxic Effects of Camphorquinone and DMT on Human Oral and Intestinal Cells. Dent. Mater. 2015, 31, 1159–1168. [Google Scholar] [CrossRef]
- Moorthy, B.; Madyastha, P.; Madyastha, K.M. Hepatotoxicity of Pulegone in Rats: Its Effects on Microsomal Enzymes, in Vivo. Toxicology 1989, 55, 327–337. [Google Scholar] [CrossRef]
- Ramos, C.A.F.; Sá, R.d.C.d.S.; Alves, M.F.; Benedito, R.B.; de Sousa, D.P.; Diniz, M.d.F.F.M.; Araújo, M.S.T.; de Almeida, R.N. Histopathological and Biochemical Assessment of D-Limonene-Induced Liver Injury in Rats. Toxicol. Rep. 2015, 2, 482–488. [Google Scholar] [CrossRef]
- Baldissera, M.D.; Souza, C.F.; Grando, T.H.; Sagrillo, M.R.; De Brum, G.F.; Nascimento, K.; Peres, D.S.; Maciel, M.F.; Silveira, S.O.; Da Luz, S.C.A.; et al. Memory Deficit, Toxic Effects and Activity of Na+, K+-ATPase and NTPDase in Brain of Wistar Rats Submitted to Orally Treatment with Alpha-Terpinene. Environ. Toxicol. Pharmacol. 2016, 46, 1–8. [Google Scholar] [CrossRef]
- Huang, F.-M.; Tai, K.-W.; Chou, M.-Y.; Chang, Y.-C. Cytotoxicity of Resin-, Zinc Oxide-Eugenol-, and Calcium Hydroxide-Based Root Canal Sealers on Human Periodontal Ligament Cells and Permanent V79 Cells. Int. Endod. J. 2002, 35, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Wojtunik-Kulesza, K.A. Toxicity of Selected Monoterpenes and Essential Oils Rich in These Compounds. Molecules 2022, 27, 1716. [Google Scholar] [CrossRef] [PubMed]
- Zárybnický, T.; Boušová, I.; Ambrož, M.; Skálová, L. Hepatotoxicity of Monoterpenes and Sesquiterpenes. Arch. Toxicol. 2018, 92, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pelkonen, O.; Abass, K.; Wiesner, J. Thujone and Thujone-Containing Herbal Medicinal and Botanical Products: Toxicological Assessment. Regul. Toxicol. Pharmacol. 2013, 65, 100–107. [Google Scholar] [CrossRef]
- Zámboriné Németh, É.; Thi Nguyen, H. Thujone, a Widely Debated Volatile Compound: What Do We Know about It? Phytochem. Rev. 2020, 19, 405–423. [Google Scholar] [CrossRef]
- Committee on Herbal Medicinal Products (HMPC) Public Statement on the Use of Herbal Medicinal Products Containing Thujone; European Medicine Agency: London, UK, 2011.
| Compound Name | Chemical Structure | Occurrence | Biological Properties | Potential Mechanisms |
|---|---|---|---|---|
| α-Pinene | 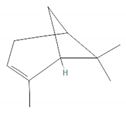 | Cannabis sativa L. Curcuma spp. (turmeric) Daucus carota (wild carrot) Juniperus spp. (junipers) Pinophyta spp. (conifers) Piper nigrum (black pepper) [19,20,21,22] | Analgesic and antinociceptive [23] | Interaction with γ-aminobutyric acid type A (GABAA) receptor [23] |
| Antifungal [24] | Ergosterol complexation [25] | |||
| Antiviral [26] | Interference with the virion envelope or masking of necessary viral structures [26] | |||
| α-Terpineol |  | Citrus aurantium ssp. amara (bitter orange) Melaleuca spp. (tea trees) Origanium vulgare L. (oregano) Pinus spp. (pines) Salvia rosmarinus (rosemary) Vitex agnus-castus (chaste tree) Zingiber officinale (ginger) [27,28] | Anti-inflammatory [29] | IL-6 inhibition [29] |
| α-Thujone | 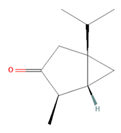 | Artemisia absinthium (wormwood) Artemisia herba-alba (white wormwood) Artemisia tridentata (big sagebrush) Salvia fruticosa (Greek sage) Salvia officinalis (common sage) Tanacetum vulgare (tansy) Thymus spp. (thymes) [30,31,32] | Anti-inflammatory [31] | Inhibition of PMA/I-induced interleukin-6 (IL-6) and interleukin-8 (IL-8) release [31] |
| Antiviral [30] | Unknown | |||
| β-Pinene | 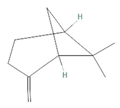 | Anethum graveolens (dill) Melaleuca alternifolia (narrow-leaved paperbark) Pinus spp. (pines) Salvia fruticosa (Greek sage) Salvia officinalis (common sage) Salvia rosmarinus (rosemary) Vitex agnus-castus (chaste tree) [33] | Anti-cancer [34] | Apoptosis [34] |
| Antiviral [35] | Interference with the virion envelope or masking of necessary viral structures [26] | |||
| β-Thujone |  | Artemisia absinthium (wormwood) Salvia fruticosa (Greek sage) Salvia officinalis (common sage) Thuja occidentalis (northern white cedar) Thymus spp. (thymes) [30,31,36] | Anti-inflammatory [31] | Inhibition of PMA/I-induced IL-6 and IL-8 release [31] |
| Antiviral [30] | Unknown | |||
| Borneol |  | Daucus carota (wild carrot) Mentha spicata (spearmint) Salvia officinalis (common sage) Salvia rosmarinus (rosemary) Thymus vulgaris (common thyme) Zingiber spp. (true gingers) [31,37,38] | Anti-inflammatory [31] | Inhibition of PMA/I-induced IL-6 and IL-8 release [31] |
| Camphor |  | Artemisia annua (sweet wormwood) Cinnamomum camphora (camphor tree) Salvia fruticosa (Greek sage) Salvia officinalis (common sage) Salvia rosmarinus (rosemary) Tanacetum vulgare (tansy) [31,38,39,40] | Anti-inflammatory [31] | Inhibition of PMA/I-induced IL-6 and IL-8 release [31] |
| Antiviral [30] | Unknown | |||
| Carvacrol | 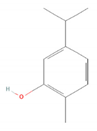 | Lippia origanoides Origanum Dictamnus (dittany of Crete) Origanum vulgare (oregano) Satureja thymbra (savory of Crete) Thymus capitatus (conehead thyme) Thymus serpyllum (white thyme) Thymus vulgaris (common thyme) [41,42] | Analgesic and antinociceptive [43] | Interaction with opioid, vanilloid, and glutamate systems [43] |
| Citronellal |  | Corymbia citriodora (lemon-scented gum) Cymbopogon spp. (lemongrass) Ocimum spp. (basil) Zingiber spp. (gingers) [44,45,46] | Analgesic and antinociceptive [47] | Inhibition of substance P release or neurokinin-1 (NK-1) receptor [47] |
| Citronellol | 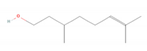 | Citrus × deliciosa (Mediterranean Mandarin) Corymbia citriodora (lemon-scented gum) Cymbopogon spp. (lemongrass) Pelargonium spp. (geraniums) Rosa × damascena (Damask rose) Rosa gallica (Gallic rose) Zingiber spp. (gingers) [48,49] | Antifungal [24] | Fungal membrane disruption [50,51] |
| Eucalyptol (1,8-Cineole) | 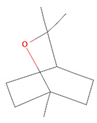 | Curcuma spp. (turmerics) Eucalyptus spp. (eucalyptuses) Mentha pulegium (pennyroyal) Mentha × piperita (peppermint) Salvia fruticosa (Greek sage) Salvia officinalis (common sage) [30,31,52] | Anti-inflammatory [31] | Inhibition of PMA/I-induced IL-6 and IL-8 release [31] |
| Antiviral [26,30] | Interference with the virion envelope or masking of necessary viral structures [26] | |||
| Eugenol | 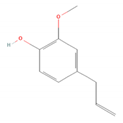 | Cinnamomum spp. (cinnamon) Myristica fragrans (nutmeg) Ocimum spp. (basils) Pimenta dioica (allspice) Syzygium aromaticum (clove) [4,53,54] | Antibacterial [55] | Biofilm disruption [56] |
| Geraniol | 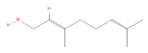 | Camellia sinensis (tea plant) Citrus × deliciosa (Mediterranean Mandarin) Cymbopogon spp. (lemongrass) Vitis vinifera (common grape) Humulus lupulus (hops) Pelargonium spp. (geraniums) Rosa spp. (roses) Zingiber officinale (ginger) [49,57,58] | Anti-cancer [59] | Downregulation of nuclear factor kappa B (NF-κB) pathway [59] |
| Hinokitiol (β-thujaplicin) | 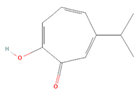 | Chamaecyparis (false cypresses) Cupressus spp. (cypresses) Thuja spp. (thujas) Thujopsis dolabrata [60] | Anti-inflammatory [61] | Downregulation of mRNA transcription of proinflammatory cytokine-related genes [61] |
| Anti-cancer [62] | Induction of apoptosis and autophagy [63] | |||
| Antibacterial [64] | Inhibition of nutrient transport and cell respiration [65] | |||
| Antifungal [66] | Chelating of fungal intracellular iron and respiration inhibition of fungal cells [66] | |||
| Isoborneol | 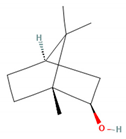 | Artemisia annua (sweet wormwood) Curcuma amada (mango ginger) Cinnamomum camphora (camphor tree) Salvia fruticosa (Greek sage) Salvia officinalis (common sage) Thymus vulgaris (common thyme) Zingiber officinale (ginger) [67,68] | Antiviral [69] | Inhibition of viral glycosylation [69] |
| Limonene |  | Anethum graveolens (dill) Citrus spp. (citruses) Eucalyptus globulus (southern blue gum) Melaleuca alternifolia (narrow-leaved paperbark) Salvia officinalis (common sage) Salvia rosmarinus (rosemary) Vitex agnus-castus (chaste tree) [70,71] | Antifungal [24] | Disruption of cell wall and cell membrane, which leads to apoptosis [72]; inhibition of adhesion, enzyme secretion, and biofilm formation [73] |
| Antiviral [35,74] | Interference with virion envelope structures or masking of necessary viral structures [35] | |||
| Menthol | 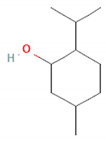 | Mentha spp. (mints) [75] | Antiviral [76] | Attenuation of infection by stimulating TRPM8, which blocks TRPV1-mediated mitochondrial fragmentation [76] |
| Myrtenol | 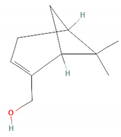 | Achillea spp. (yarrows) Eucalyptus spp. (eucalyptuses) Myrtus communis (common myrtle) Taxus spp. (yews) [77,78] | Analgesic and antinociceptive [79] | Cytokine inhibition and p38 mitogen-activated protein kinase (p38-MAPK) signal transduction pathway in trigeminal ganglia [79] |
| Perillic acid | 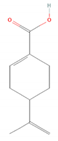 | Perilla frutescens (beefsteak plant) [80,81] | Antiviral [82] | Inhibition of maturation, fusion, and viral infectivity [82] |
| Perillyl alcohol | 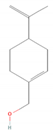 | Carum carvi (caraway) Lavandula × intermedia (lavandin) Mentha piperita (peppermint) Mentha spicata (spearmint) Perilla frutescens (beefsteak plant) [83,84,85] | Antiviral [82] | Inhibition of maturation, fusion, and viral infectivity [82] |
| Sabinene | 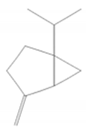 | Artemisia annua (sweet wormwood) Juniperus communis (common juniper) Mesosphaerum suaveolens (pignut) Piper nigrum (black pepper) Salvia rosmarinus (rosemary) Vitex agnus-castus (chaste tree) Zingiber montanum [86,87,88] | Antibacterial [86,89] | Inhibition of bacterial adherence, growth and biofilm formation [89] |
| Thymol |  | Lippia spp. Nigella sativa (black caraway) Ocimum spp. (basils) Origanum spp. (oreganos) Satureja thymbra (savory of Crete) Thymus spp. (thymes) Trachyspermum ammi (ajowan caraway) [90,91] | Antibacterial [92] | Biofilm disruption, decrease in virulence [92,93], reduction of viability and metabolic activity, autolysis [93] |
| Anti-cancer [94] | Mitochondria-mediated apoptosis [94] | |||
| Antifungal [95] | Disruption of cell membrane integrity [95] |
| Type of Toxicity | Compound Name | Type of Assay | Cell Line/Animal | Toxicity |
|---|---|---|---|---|
| Cytotoxicity | Camphor | In vitro | MRC-5 fetal lung fibroblasts | IC50 11 mM [203] |
| Eucalyptol | In vitro | MRC-5 fetal lung fibroblasts | IC50 11 mM [203] | |
| Thujone | In vitro | MRC-5 fetal lung fibroblasts | IC50 2.2 mM [203] | |
| Eugenol | In vitro | Primary gingival fibroblasts, hemopoietic progenitor cells, human periodontal ligament cells | CC50 > 755 μM [204] | |
| Citral | In vitro | Peripheral blood mononuclear cells, human hepatoma cell line HepG2 | ≥50 μg/mL [205] | |
| Genotoxicity | Camphorquinone | In vitro | OKF6/TERT-2 telomerase-immortalized cells | ≥2.5 mM [206] |
| Pulegone | In vivo | Male albino rats (Indian Institute of Science strain) | 400 mg/kg [207] | |
| Hepatotoxicity | Limonene | In vivo | Male Wistar rats | 25 mg/kg, 75 mg/kg [208] |
| Neurotoxicity | Thujone | In vivo | Rats, Mice, Guinea Pigs | LD50 192 mg/kg (rats), 230 mg/kg (mice), 396 mg/kg guinea pigs [205] |
| α-Terpinene | In vivo | Female Wistar rats | ≥0.5 mL/kg [209] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Potocka, W.; Assy, Z.; Bikker, F.J.; Laine, M.L. Current and Potential Applications of Monoterpenes and Their Derivatives in Oral Health Care. Molecules 2023, 28, 7178. https://doi.org/10.3390/molecules28207178
Potocka W, Assy Z, Bikker FJ, Laine ML. Current and Potential Applications of Monoterpenes and Their Derivatives in Oral Health Care. Molecules. 2023; 28(20):7178. https://doi.org/10.3390/molecules28207178
Chicago/Turabian StylePotocka, Wiktoria, Zainab Assy, Floris J. Bikker, and Marja L. Laine. 2023. "Current and Potential Applications of Monoterpenes and Their Derivatives in Oral Health Care" Molecules 28, no. 20: 7178. https://doi.org/10.3390/molecules28207178






