Cancer Vaccines Based on Fluorine-Modified KH-1 Elicit Robust Immune Response
Abstract
:1. Introduction
2. Results and Discussion
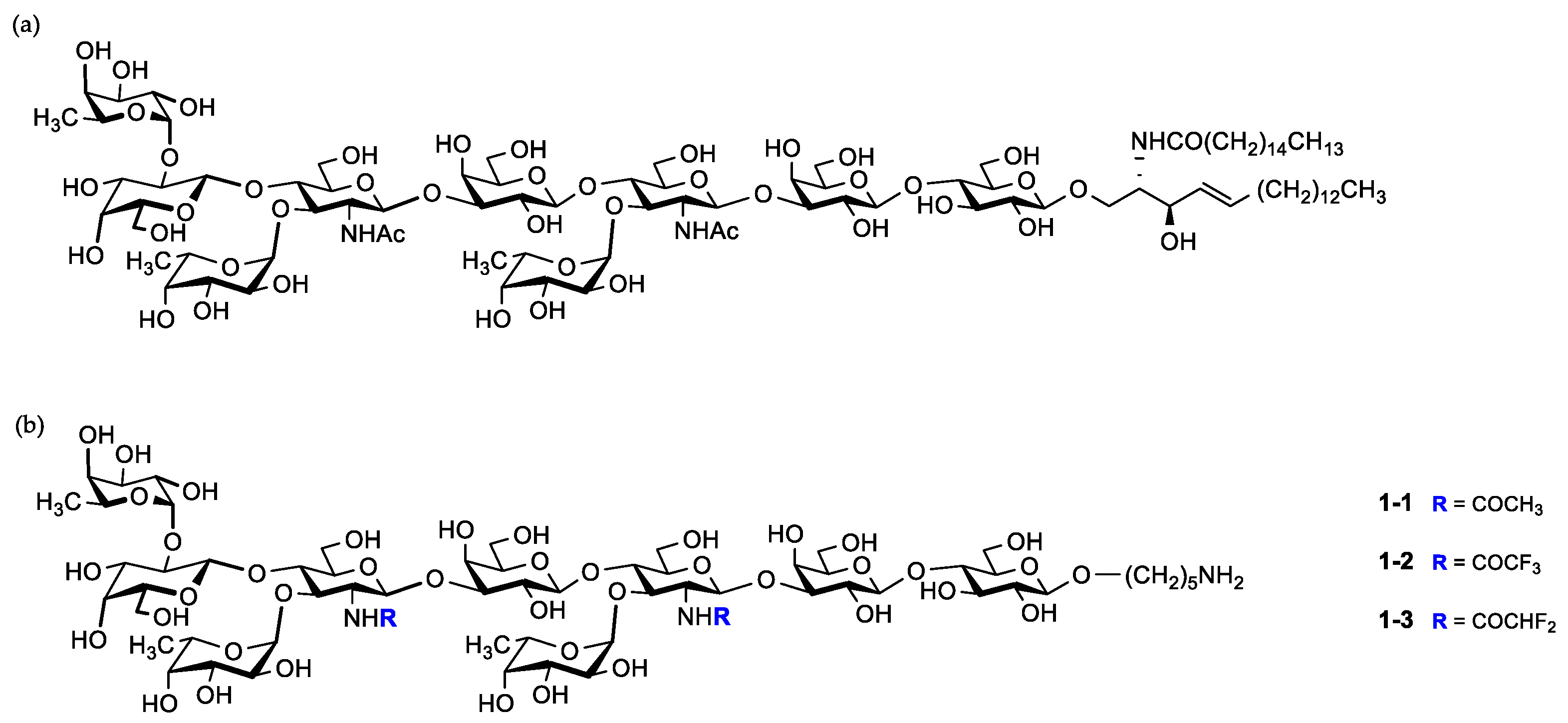
2.1. Synthesis of KH-1 Antigen and Its Fluorinated Derivatives
2.2. Synthesis of Glycoconjugates
2.3. Evaluation of the Antibodies
2.4. Recognition of KH-1-Positive Tumor Cells with IgG Antibodies in Antisera
2.5. Complement-Dependent Cytotoxicity of Antisera Induced by Vaccines
3. Materials and Methods
3.1. Chemical Synthesis
3.1.1. Synthesis of Compound 1-1
3.1.2. Synthesis of Compound 1-2
3.1.3. Synthesis of Compound 1-3
3.1.4. Synthesis of Compound 3-1
3.1.5. Synthesis of Compound 3-2
3.1.6. Synthesis of Compound 2
3.1.7. Synthesis of CRM197 Glycoconjugates
3.1.8. Synthesis of BSA Glycoconjugates
3.2. Immunization of Mice
3.3. Serological Assays
3.4. Flow Cytometry
3.5. Complement-Dependent Cytotoxicity (CDC) Assay
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Pinho, S.S.; Reis, C.A. Glycosylation in cancer: Mechanisms and clinical implications. Nat. Rev. Cancer 2015, 15, 540–555. [Google Scholar] [CrossRef]
- Sanders, D.S.; Kerr, M.A. Lewis blood group and CEA related antigens; coexpressed cell-cell adhesion molecules with roles in the biological progression and dissemination of tumors. Mol. Pathol. 1999, 52, 174–178. [Google Scholar] [CrossRef] [Green Version]
- Thurin, M. Tumor-associated glycans as targets for immunotherapy: The Wistar institute experience/legacy. Monoclon. Antib. Immunodiagn. Immunother. 2021, 40, 89–100. [Google Scholar] [CrossRef]
- Heimburg-Molinaro, J.; Lum, M.; Vijay, G.; Jain, M.; Almogren, A.; Rittenhouse-Olson, K. Cancer vaccines and carbohydrate epitopes. Vaccine 2011, 29, 8802–8826. [Google Scholar] [CrossRef] [Green Version]
- Hakomori, S. Tumor-associated carbohydrate antigens defining tumor malignancy: Basis for development of anti-cancer vaccines. Adv. Exp. Med. Biol. 2001, 491, 369–402. [Google Scholar] [CrossRef]
- Livingston, P.O. Augmenting the immunogenicity of carbohydrate tumor antigens. Semin. Cancer Biol. 1995, 6, 357–366. [Google Scholar] [CrossRef]
- Krug, L.M.; Ragupathi, G.; Ng, K.K.; Hood, C.; Jennings, H.J.; Guo, Z.; Kris, M.G.; Miller, V.; Pizzo, B.; Tyson, L.; et al. Vaccination of small cell lung cancer patients with polysialic acid or N-propionylated polysialic acid conjugated to keyhole limpet hemocyanin. Clin Cancer Res. 2004, 10, 916–923. [Google Scholar] [CrossRef] [Green Version]
- Sadraei, S.I.; Reynolds, M.R.; Trant, J.F. The synthesis and biological characterization of acetal-free mimics of the tumor-associated carbohydrate antigens. Adv. Carbohydr. Chem. Biochem. 2017, 74, 137–237. [Google Scholar] [CrossRef]
- Weiwer, M.; Huang, F.; Chen, C.-C.; Yuan, X.; Tokuzaki, K.; Tomiyama, H.; Linhardt, R.J. Synthesis and evaluation of anticancer vaccine candidates: C-glycoside analogues of STn and PSA. ACS Symp. Ser. 2008, 990, 216–238. [Google Scholar]
- Bundle, D.R.; Rich, J.R.; Jacques, S.; Yu, H.N.; Nitz, M.; Ling, C.C. Thiooligosaccharide conjugate vaccines evoke antibodies specific for native antigens. Angew. Chem. Int. Ed. 2005, 44, 7725–7729. [Google Scholar] [CrossRef]
- Hoffmann-Roder, A.; Kaiser, A.; Wagner, S.; Gaidzik, N.; Kowalczyk, D.; Westerlind, U.; Gerlitzki, B.; Schmitt, E.; Kunz, H. Synthetic antitumor vaccines from tetanus toxoid conjugates of MUC1 glycopeptides with the Thomsen-Friedenreich antigen and a fluorine-substituted analogue. Angew. Chem. Int. Ed. 2010, 49, 8498–8503. [Google Scholar] [CrossRef]
- Nudelman, E.; Levery, S.B.; Kaizu, T.; Hakomori, S. Novel fucolipids of human adenocarcinoma: Characterization of the major Ley antigen of human adenocarcinoma as trifucosylnonaosyl Ley glycolipid (III3FucV3FucVI2FucnLc6). J. Biol. Chem. 1986, 261, 11247–11253. [Google Scholar] [CrossRef]
- Kaizu, T.; Levery, S.B.; Nudelman, E.; Stenkamp, R.E.; Hakomori, S. Novel fucolipids of human adenocarcinoma: Monoclonal antibody specific for trifucosyl Ley (III3FucV3FucVI2FucnLc6) and a possible three-dimensional epitope structure. J. Biol. Chem. 1986, 261, 11254–11258. [Google Scholar] [CrossRef]
- Hellström, I.; Garrigues, H.J.; Garrigues, U.; Hellström, K.E. Highly tumor-reactive, internalizing, mouse monoclonal antibodies to Le(y)-related cell surface antigens. Cancer Res. 1990, 50, 2183–2190. [Google Scholar] [CrossRef]
- Kim, Y.S.; Yuan, M.; Itzkowitz, S.H.; Sun, Q.B.; Kaizu, T.; Palekar, A.; Trump, B.F.; Hakomori, S. Expression of Ley and extended Ley blood group-related antigens in human malignant, premalignant, and nonmalignant colonic tissues. Cancer Res. 1986, 46, 5985–5992. [Google Scholar] [CrossRef]
- Stocks, S.C.; Albrechtsen, M.; Kerr, M.A. Expression of the CD15 differentiation antigen (3-fucosyl-N-acetyl-lactosamine, LeX) on putative neutrophil adhesion molecules CR3 and NCA-160. Biochem. J. 1990, 268, 275–280. [Google Scholar] [CrossRef] [Green Version]
- Buskas, T.; Li, Y.; Boons, G.J. Synthesis of a dimeric Lewis antigen and the evaluation of the epitope specificity of antibodies elicited in mice. Chem. Eur. J. 2005, 11, 5457–5467. [Google Scholar] [CrossRef]
- Deshpande, P.P.; Danishefsky, S.J. Total synthesis of the potential anticancer vaccine KH-1 adenocarcinoma antigen. Nature 1997, 387, 164–166. [Google Scholar] [CrossRef]
- Spassova, M.K.; Bornmann, W.G.; Ragupathi, G.; Sukenick, G.; Livingston, P.O.; Danishefsky, S.J. Synthesis of selected LeY and KH-1 analogues: A medicinal chemistry approach to vaccine optimization. J. Org. Chem. 2005, 70, 3383–3395. [Google Scholar] [CrossRef]
- Hummel, G.; Schmidt, R.R. A versatile synthesis of the lactoneo-series antigens—Synthesis of sialyl dimer Lewis X and of dimer Lewis Y. Tetrahedron Lett. 1997, 38, 1173–1176. [Google Scholar] [CrossRef]
- Routenberg Love, K.; Seeberger, P.H. Automated solid-phase synthesis of protected tumor-associated antigen and blood group determinant oligosaccharides. Angew. Chem. Int. Ed. 2004, 116, 612–615. [Google Scholar] [CrossRef]
- Li, Q.; Guo, Z. Synthesis of the cancer-associated KH-1 antigen by block assembly of its backbone structure followed by one-step grafting of three fucose residues. Org. Lett. 2017, 19, 6558–6561. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Zheng, X.J.; Huo, C.X.; Wang, Y.; Zhang, Y.; Ye, X.-S. Enhancement of the immunogenicity of synthetic carbohydrate vaccines by chemical modifications of STn antigen. ACS Chem. Biol. 2011, 6, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Zhai, C.; Zheng, X.J.; Song, C.; Ye, X.-S. Synthesis and immunological evaluation of N-acyl modified Globo H derivatives as anticancer vaccine candidates. RSC Med. Chem. 2021, 12, 1239–1243. [Google Scholar] [CrossRef]
- Song, C.; Zheng, X.J.; Guo, H.; Cao, Y.; Zhang, F.; Li, Q.; Ye, X.-S.; Zhou, Y. Fluorine-modified sialyl-Tn-CRM197 vaccine elicits a robust immune response. Glycoconj. J. 2019, 36, 399–408. [Google Scholar] [CrossRef]
- Song, C.; Zheng, X.J.; Liu, C.C.; Zhou, Y.; Ye, X.-S. A cancer vaccine based on fluorine-modified sialyl-Tn induces robust immune responses in a murine model. Oncotarget 2017, 8, 47330–47343. [Google Scholar] [CrossRef] [Green Version]
- Li, B.-H.; Yao, W.; Yang, H.; Wu, C.; Xiong, D.-C.; Yin, Y.; Ye, X.-S. Total synthesis of tumor-associated KH-1 antigen core nonasaccharide via photo-induced glycosylation. Org. Chem. Front. 2020, 7, 1255–1259. [Google Scholar] [CrossRef]
- Huang, X.; Huang, L.; Wang, H.; Ye, X.-S. Iterative one-pot synthesis of oligosaccharides. Angew. Chem. Int. Ed. 2004, 43, 5221–5224. [Google Scholar] [CrossRef]
- Mao, R.Z.; Guo, F.; Xiong, D.-C.; Li, Q.; Duan, J.; Ye, X.-S. Photoinduced C-S bond cleavage of thioglycosides and glycosylation. Org. Lett. 2015, 17, 5606–5609. [Google Scholar] [CrossRef]
- Mao, R.-Z.; Xiong, D.-C.; Guo, F.; Li, Q.; Duan, J.; Ye, X.-S. Light-driven highly efficient glycosylation reactions. Org. Chem. Front. 2016, 3, 737–743. [Google Scholar] [CrossRef]
- Badahdah, A.M.; Rashid, H.; Khatami, A. Update on the use of meningococcal serogroup C CRM197-conjugate vaccine (Meningitec) against meningitis. Expert. Rev. Vaccines 2016, 15, 9–29. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.L.; Hung, J.T.; Cheung, S.K.; Lee, H.Y.; Chu, K.C.; Li, S.T.; Lin, Y.C.; Ren, C.T.; Cheng, T.J.; Hsu, T.L.; et al. Carbohydrate-based vaccines with a glycolipid adjuvant for breast cancer. Proc. Natl. Acad. Sci. USA 2013, 110, 2517–2522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, J.R.; Markl, J. Keyhole limpet hemocyanin (KLH): A biomedical review. Micron 1999, 30, 597–623. [Google Scholar] [CrossRef] [PubMed]
- Guo, K.; Chu, C.C.; Chkhaidze, E.; Katsarava, R. Synthesis and characterization of novel biodegradable unsaturated poly(ester amide)s. J. Polym. Sci. A Polym. Chem. 2005, 43, 1463–1477. [Google Scholar] [CrossRef]
- Guttormsen, H.K.; Paoletti, L.C.; Mansfield, K.G.; Jachymek, W.; Jennings, H.J.; Kasper, D.L. Rational chemical design of the carbohydrate in a glycoconjugate vaccine enhances IgM-to-IgG switching. Proc. Natl. Acad. Sci. USA 2008, 105, 5903–5908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, M.-M.; Wang, Y.-S.; Ye, X.-S. Carbohydrate-based vaccines for oncotherapy. Med. Res. Rev. 2018, 38, 1003–1026. [Google Scholar] [CrossRef] [PubMed]
- Finkelman, F.D.; Holmes, J.; Katona, I.M.; Urban, J.F.; Beckmann, M.P.; Park, L.S.; Schooley, K.A.; Coffman, R.L.; Mosmann, T.R.; Paul, W.E. Lymphokine control of in vivo immunoglobulin isotype selection. Annu. Rev. Immunol. 1990, 8, 303–333. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, J.; Furukawa, K.; Cordon-Cardo, C.; Yin, B.W.; Rettig, W.J.; Oettgen, H.F.; Old, L.J.; Lloyd, K.O. Expression of Lewis a, Lewis b, X, and Y blood group antigens in human colonic tumors and normal tissue and in human tumor-derived cell lines. Cancer Res. 1986, 46, 1553–1561. [Google Scholar]
- Guo, J.; Jiang, W.; Li, Q.; Jaiswal, M.; Guo, Z. Comparative immunological studies of tumor-associated Lewis X, Lewis Y, and KH-1 antigens. Carbohydr. Res. 2020, 492, 107999. [Google Scholar] [CrossRef]
- Bordron, A.; Bagacean, C.; Tempescul, A.; Berthou, C.; Bettacchioli, E.; Hillion, S.; Renaudineau, Y. Complement system: A neglected pathway in immunotherapy. Clin. Rev. Allergy. Immunol. 2020, 58, 155–171. [Google Scholar] [CrossRef]
- Sörman, A.; Zhang, L.; Ding, Z.; Heyman, B. How antibodies use complement to regulate antibody responses. Mol. Immunol. 2014, 61, 79–88. [Google Scholar] [CrossRef] [PubMed]







| Conjugate | Molecular Weight of Glycoconjugate | Total Molecular Weight of Carbohydrate on Conjugate | Molecular Weight of Single Nonasaccharide | Concentration of Carbohydrate (μg/mL) | Concentration of Protein (μg/mL) | Number of Nonasaccharide | Percentage of Carbohydrate Loading |
|---|---|---|---|---|---|---|---|
| KH-1-CRM197 | 67,285 | 8968 | 1596 | 213 | 1600 | 5.62 | 13.32% |
| KH-1-TF-CRM197 | 67,908 | 9591 | 1704 | 165 | 1167 | 5.63 | 14.12% |
| KH-1-DF-CRM197 | 70,134 | 11,817 | 1668 | 195 | 1145 | 7.08 | 16.85% |
| KH-1-BSA | 80,787 | 14,350 | 1596 | 206 | 1156 | 8.99 | 17.76% |
| KH-1-TF-BSA | 83,936 | 17,499 | 1704 | 221 | 1057 | 10.27 | 20.85% |
| KH-1-DF-BSA | 79,742 | 13,305 | 1668 | 197 | 1079 | 7.98 | 16.69% |
| ELISA Titer Anti-KH-1 and Ratio of IgG/IgM after the Third and the Fourth Vaccination | ELISA Titer Anti-Modified-KH-1 | ||||||
|---|---|---|---|---|---|---|---|
| Vaccine | After the Third Vaccination | After the Fourth Vaccination | After the Fourth Vaccination | ||||
| IgG | IgM | IgG/IgM | IgG | IgM | IgG/IgM | IgG* | |
| KH-1-CRM197/FA | <100 | 242 | - | 45,268 | 8952 | 5.06 | 45,268 |
| KH-1-DF-CRM197/FA | 11,686 | 4480 | 2.61 | 101,447 | 20,437 | 4.96 | 216,853 |
| KH-1-TF-CRM197/FA | 848,249 | 6307 | 134.49 | 1,180,228 | 9670 | 122.05 | 2,259,394 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Li, B.; Zheng, X.; Xiong, D.; Ye, X. Cancer Vaccines Based on Fluorine-Modified KH-1 Elicit Robust Immune Response. Molecules 2023, 28, 1934. https://doi.org/10.3390/molecules28041934
Liu Y, Li B, Zheng X, Xiong D, Ye X. Cancer Vaccines Based on Fluorine-Modified KH-1 Elicit Robust Immune Response. Molecules. 2023; 28(4):1934. https://doi.org/10.3390/molecules28041934
Chicago/Turabian StyleLiu, Yang, Bohan Li, Xiujing Zheng, Decai Xiong, and Xinshan Ye. 2023. "Cancer Vaccines Based on Fluorine-Modified KH-1 Elicit Robust Immune Response" Molecules 28, no. 4: 1934. https://doi.org/10.3390/molecules28041934
APA StyleLiu, Y., Li, B., Zheng, X., Xiong, D., & Ye, X. (2023). Cancer Vaccines Based on Fluorine-Modified KH-1 Elicit Robust Immune Response. Molecules, 28(4), 1934. https://doi.org/10.3390/molecules28041934






