Effect of Interaction between Chromium(VI) with 17β-Estradiol and Its Metabolites on Breast Cancer Cell Lines MCF-7/WT and MDA-MB-175-VII: Preliminary Study
Abstract
1. Introduction
2. Results
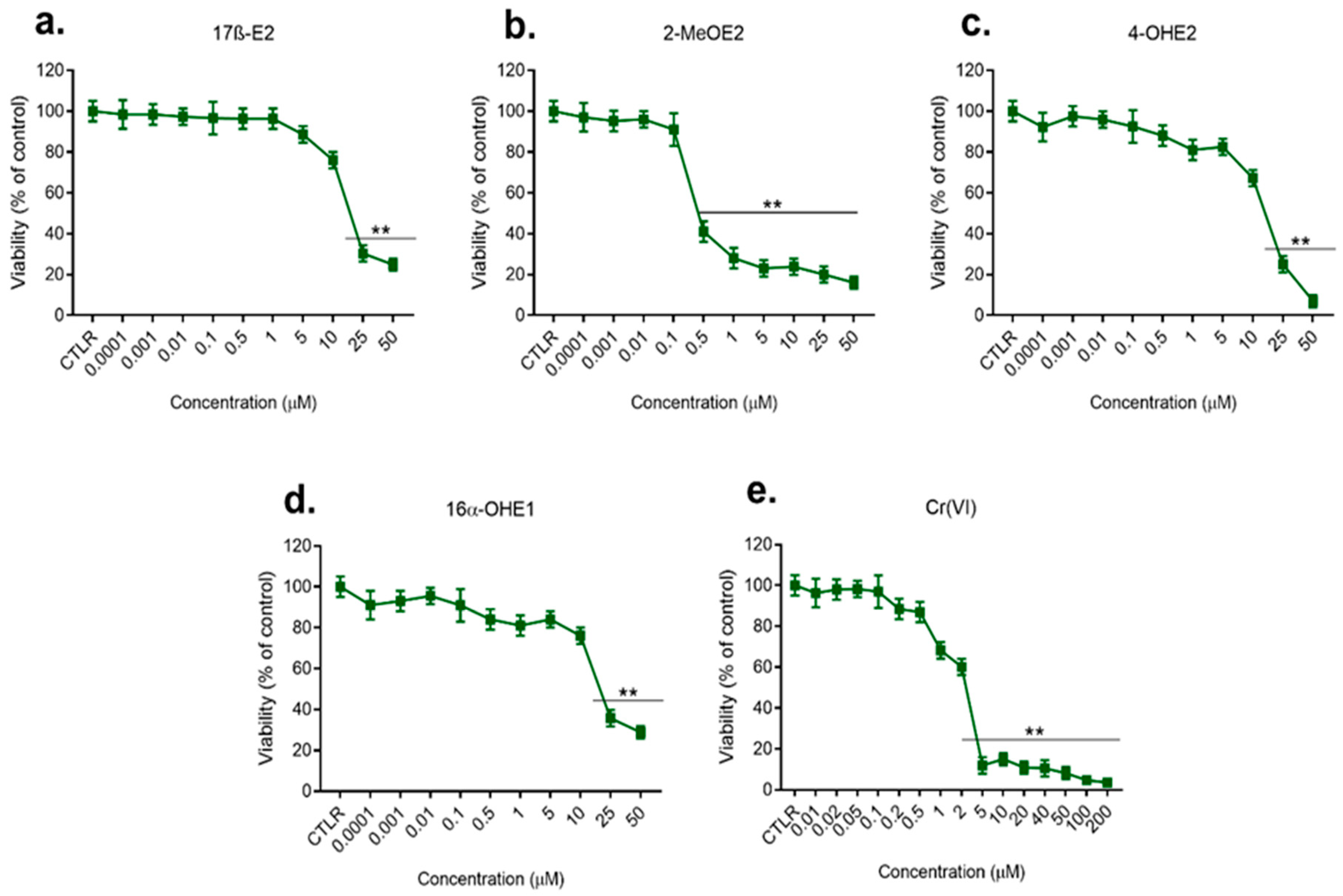
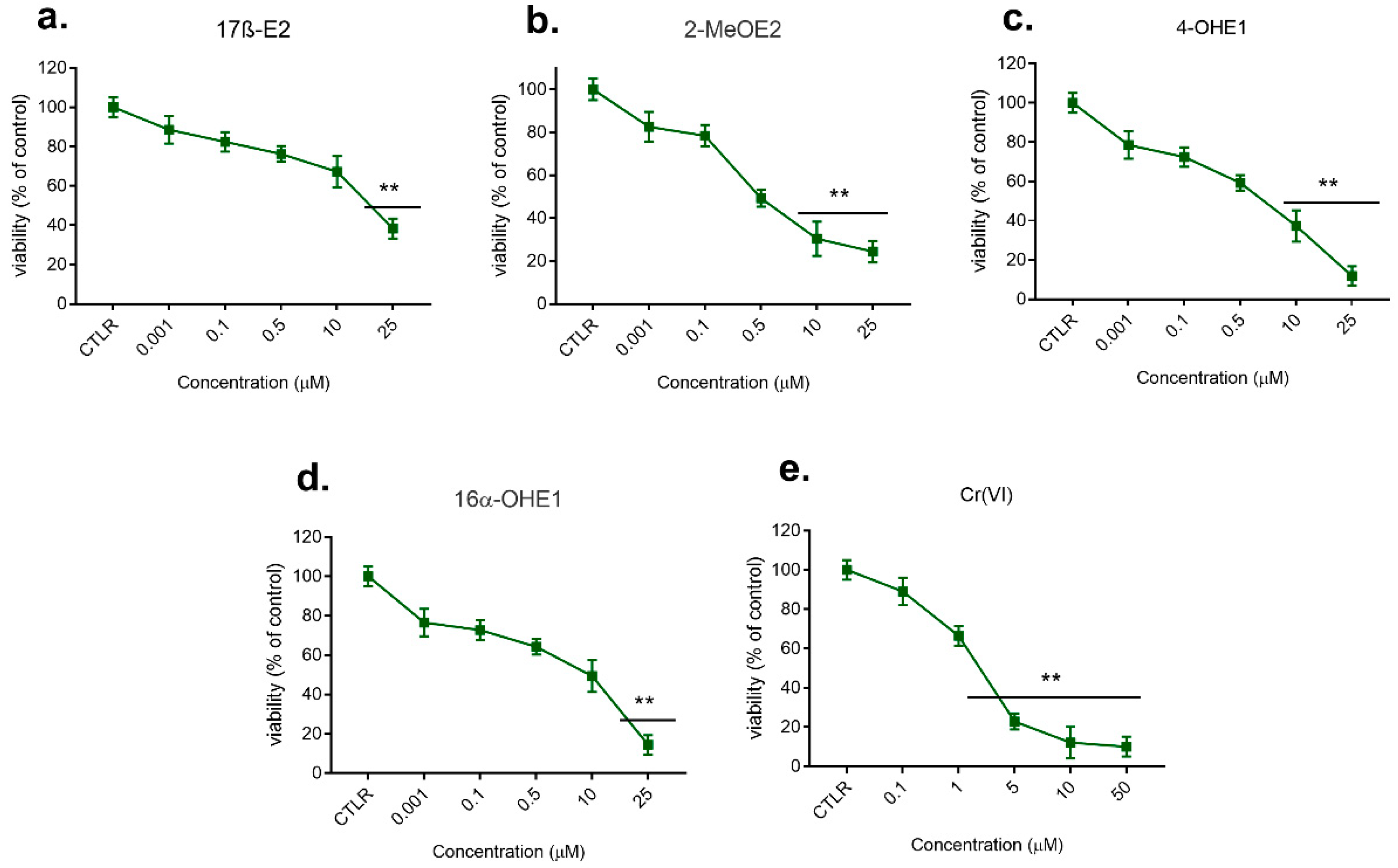
2.1. Viability Assay of Single Compounds (First Stage, First Model)
2.1.1. Effect of 17β-E2, Its Metabolites, and Cr(VI) on MCF-7/WT Viability
2.1.2. Effect of 17β-E2, Its Metabolites, and Cr(VI) on MDA-MB-175-VII Viability
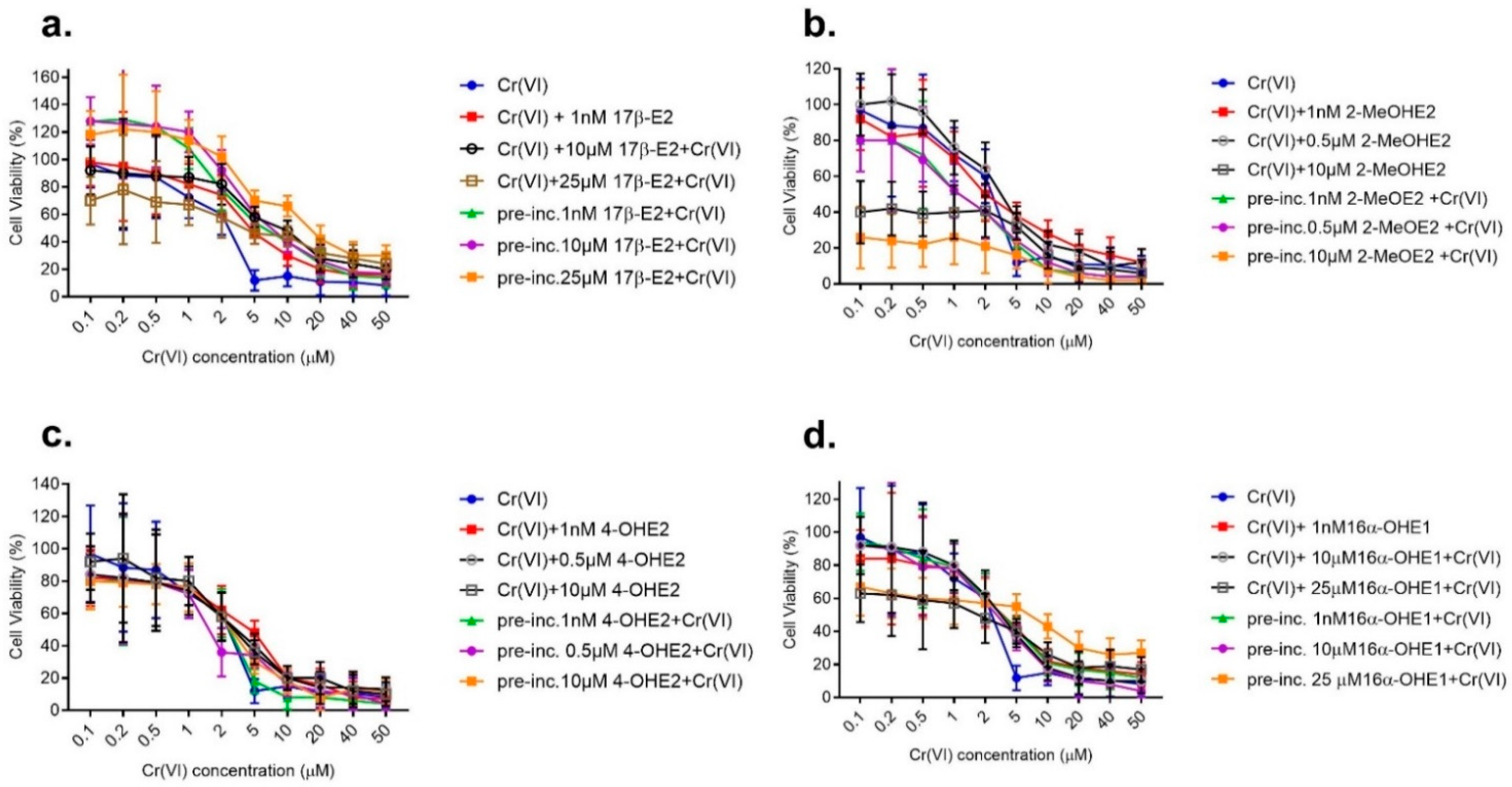
2.2. Viability Assay of Combined Action of Estrogens with Cr(VI) (First Stage, Second Model)
2.2.1. Effect of Combined Action of 17β-E2 with Cr(VI) on MCF-7/WT Viability
2.2.2. Effect of Combined Action of 2-MeOE2 with Cr(VI) on MCF-7/WT Viability
2.2.3. Effect of Combined Action of 4-OHE2 with Cr(VI) on MCF-7/WT Viability
2.2.4. Effect of Combined Action of 16α-OHE1 with Cr(VI) on MCF-7/WT Viability
2.2.5. Effect of Combined Action of 17β-E2 with Cr(VI) on MDA-MB-175-VII Viability
2.2.6. Effect of Combined Action of 17β-E2 Metabolites with Cr(VI) on MDA-MB-175-VII Viability
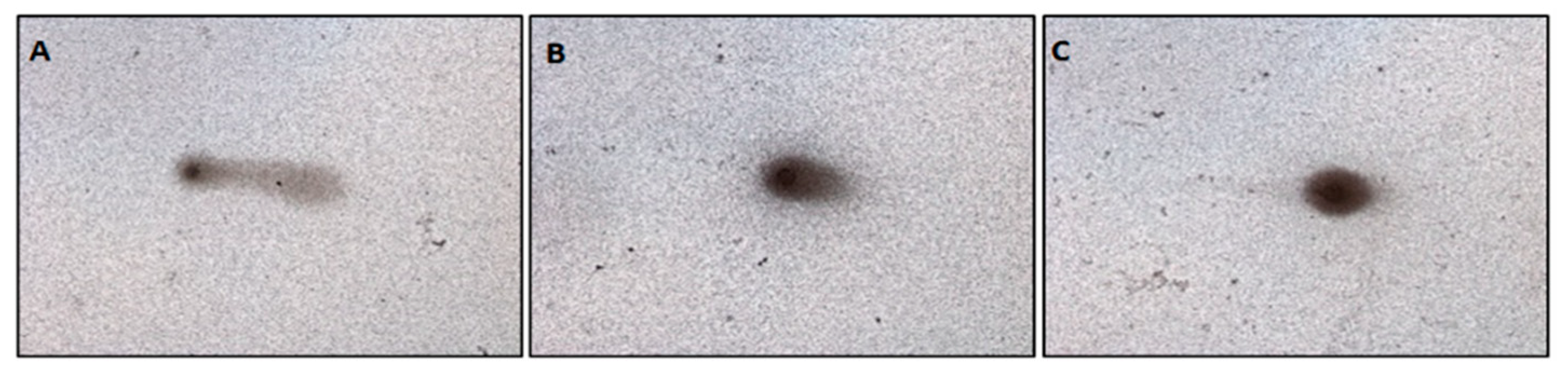
2.3. Genotoxicity of Single Compounds (Second Stage, First Model: Single Action) Genotoxicity of 17β-E2 and Its Metabolites
Genotoxicity of Cr(VI)
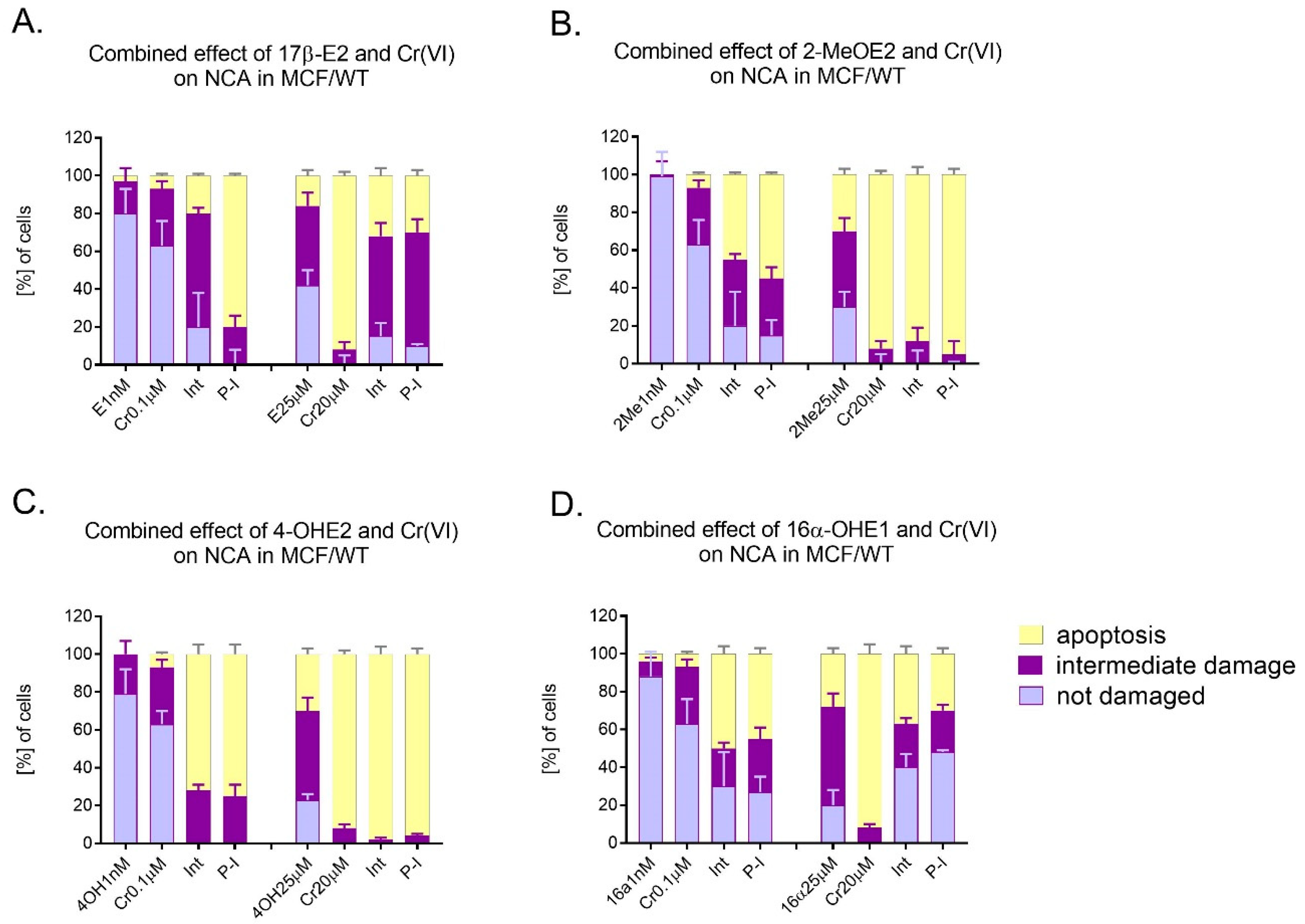
2.4. Genotoxicity of Combined Action of Estrogens with Cr(VI) (Second Stage, Second Model)
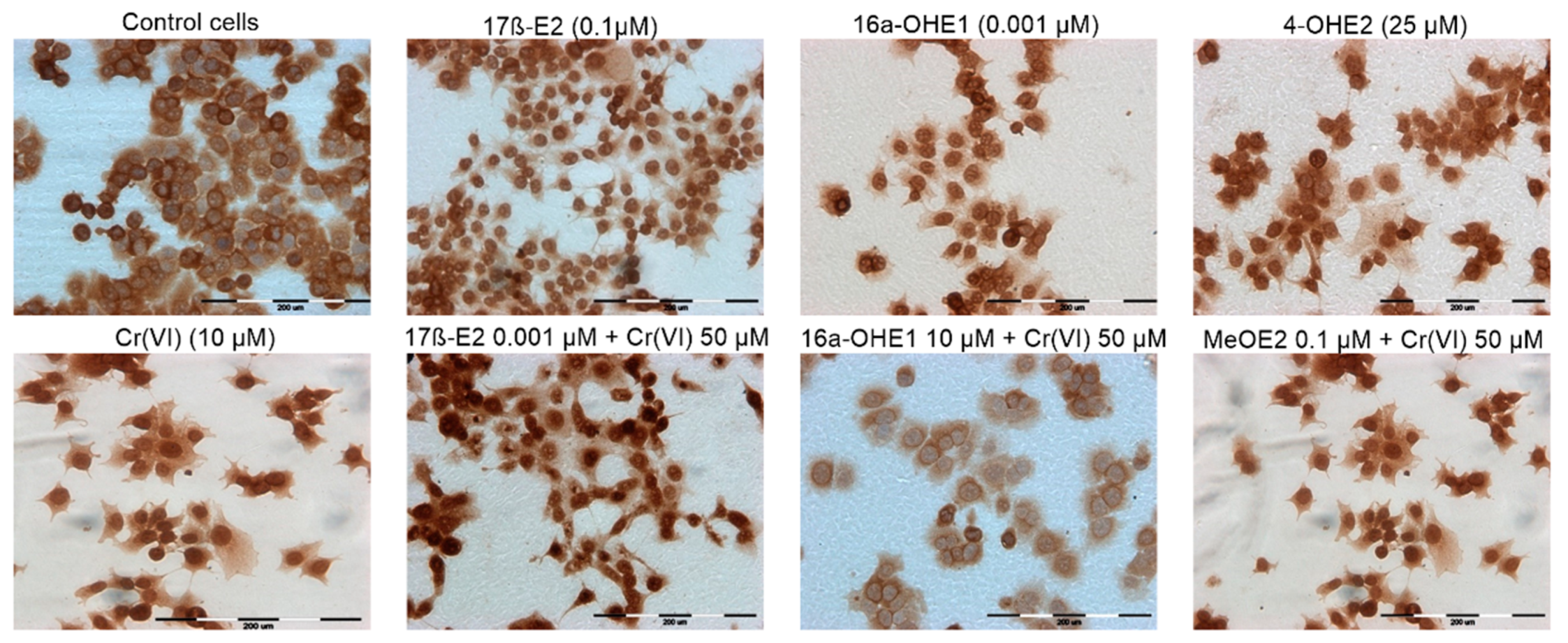
2.5. SOD1 Estimation: Immunocytochemical Staining
3. Discussion
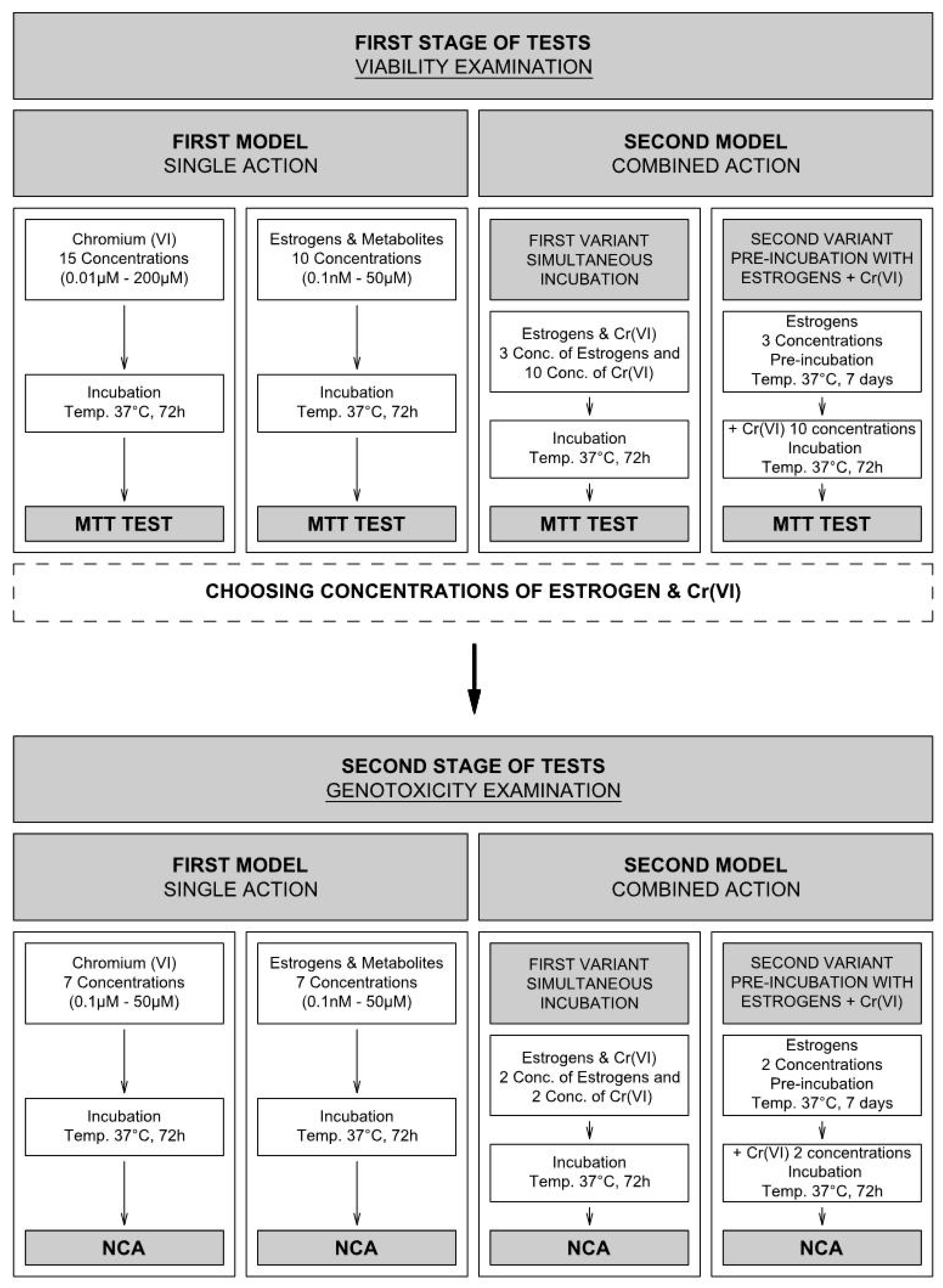
4. Materials and Methods
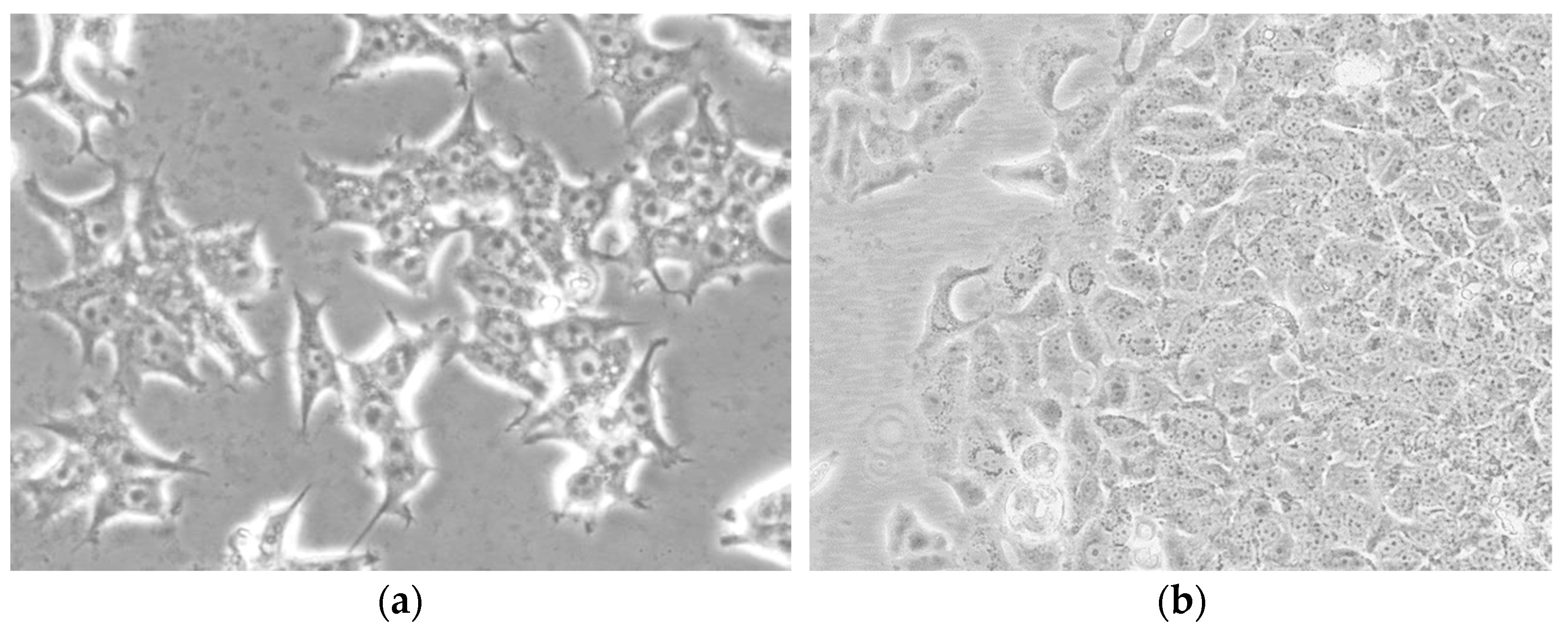
4.1. Cell Culture
4.2. Compounds
4.3. MTT Assay
4.4. Neutral Comet Assay (NCA)
4.5. SOD1 Estimation: Immunocytochemical Staining
4.6. Schematic Model for Viability and Genotoxicity Testing
4.7. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Sample Availability
References
- Bayuo, J. An extensive review on chromium (vi) removal using natural and agricultural wastes materials as alternative biosorbents. J. Environ. Health Sci. Eng. 2021, 19, 1193–1207. [Google Scholar] [CrossRef]
- Darbre, P.D. Metalloestrogens: An emerging class of inorganic xenoestrogens with potential to add to the oestrogenic burden of the human breast. J. Appl. Toxicol. 2006, 26, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Sawicka, E.; Jurkowska, K.; Piwowar, A. Chromium (III) and chromium (VI) as important players in the induction of genotoxicity—Current view. Ann. Agric. Environ. Med. 2021, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hodges, N.J.; Smart, D.; Lee, A.J.; Lewis, N.A.; Chipman, J.K. Induction of DNA-strand breaks in human peripherial blood lymphocytes and A549 lung cells by sodium dichromate: Association with 8-oxo-2-deoxyguanosine formation and in-terindywidual variability. Mutagenesis 2001, 16, 467–474. [Google Scholar] [CrossRef]
- Jurkowska, K.; Kratz, E.M.; Sawicka, E.; Piwowar, A. The impact of metalloestrogens on the physiology of male reproductive health as a current problem of the XXI century. J. Physiol. Pharmacol. 2019, 70, 337–355. [Google Scholar]
- Choe, S.-Y.; Kim, S.-J.; Kim, H.-G.; Lee, J.H.; Choi, Y.; Lee, H.; Kim, Y. Evaluation of estrogenicity of major heavy metals. Sci. Total. Environ. 2003, 312, 15–21. [Google Scholar] [CrossRef]
- Jouybari, L.; Saei Ghare Naz, M.; Sanagoo, A.; Kiani, F.; Sayehmiri, F.; Sayehmiri, K.; Hasanpour Dehkordi, A.H. Toxic elements as biomarkers for breast cancer: A meta-analysis study. Cancer Manag. Res. 2018, 10, 69–79. [Google Scholar] [CrossRef]
- Lim, D.S.; Roh, T.H.; Kim, M.K.; Kwon, Y.C.; Choi, S.M.; Kwack, S.J.; Kim, K.B.; Yoon, S.; Kim, H.S.; Lee, B.-M. Non-cancer, cancer, and dermal sensitization risk assessment of heavy metals in cosmetics. J. Toxicol. Environ. Health Part A 2018, 81, 432–452. [Google Scholar] [CrossRef] [PubMed]
- Byrne, C.; Divekar, S.D.; Storchan, G.B.; Parodi, D.A.; Martin, M.B. Metals and Breast Cancer. J. Mammary Gland. Biol. Neoplasia 2013, 18, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Sawicka, E.; Długosz, A. The role of 17β-estradiol metabolites in chromium-induced. Adv. Clin. Exp. Med. 2017, 26, 215–221. [Google Scholar] [CrossRef]
- Song, R.X.; Mor, G.; Naftolin, F.; McPherson, R.A.; Song, J.; Zhang, Z.; Yue, W.; Wang, J.; Santen, R.J. Effect of long-term es-trogen deprivation on apoptotic responses of breast cancer cells to 17β-estradiol. J. Natl. Cancer Inst. 2001, 93, 1714–1723. [Google Scholar] [CrossRef]
- Sepkovic, D.W.; Bradlow, H.L. Estrogen Hydroxylation-The Good and the Bad. Ann. N. Y. Acad. Sci. 2009, 1155, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Domazetovic, V.; Falsetti, I.; Ciuffi, S.; Iantomasi, T.; Marcucci, G.; Vincenzini, M.T.; Maria Luisa Brandi, M.L. Effect of Oxidative Stress-Induced Apoptosis on Active FGF23 Levels in MLO-Y4 Cells: The Protective Role of 17-β-Estradiol. Int. J. Mol. Sci. 2022, 23, 2103–2110. [Google Scholar] [CrossRef] [PubMed]
- Mohamad, N.V.; Ima-Nirwana, S.; Chin, K.Y. Are Oxidative Stress and Inflammation Mediators of Bone Loss Due to Estrogen Deficiency? A Review of Current Evidence. Endocr. Metab. Immune Disord. Drug Targets 2020, 201, 478–1487. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. World Health Organization. Breast Cancer Estimated Incidence, Mortality and Prevalence Worldwide in 2012. Available online: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx?cancer=breast (accessed on 3 April 2015).
- Broggi, G.; Filetti, V.; Ieni, A.; Rapisarda, V.; Ledda, C.; Vitale, E.; Varricchio, S.; Russo, D.; Lombardo, C.; Tuccari, G.; et al. Macro H2A1 immunoexpression in breast cancer. Front. Oncol. 2020, 10, 1519. [Google Scholar] [CrossRef] [PubMed]
- Martin, M.B.; Reiter, R.; Pham, T.; Avellanet, Y.R.; Camara, J.; Lahm, M.; Pentecost, E.; Pratap, K.; Gilmore, B.A.; Divekar, S.; et al. Estrogen-Like Activity of Metals in Mcf-7 Breast Cancer Cells. Endocrinology 2003, 144, 2425–2436. [Google Scholar] [CrossRef] [PubMed]
- Magro, G.; Salvatorelli, L.; Puzzo, L.; Piombino, E.; Bartoloni, G.; Broggi, G.; Vecchio, G.M. Practical approach to diagnosis of bland-looking spindle cell lesions of the breast. Pathologica 2019, 111, 344–360. [Google Scholar] [CrossRef]
- Wellejus, A.; Olsen, A.; Tjonneland, A.; Thomsen, B.L.; Overvad, K.; Loft, S. Urinary Hydroxyestrogens and Breast Cancer Risk among Postmenopausal Women: A Prospective Study. Cancer Epidemiol. Biomark. Prev. 2005, 14, 2137–2142. [Google Scholar] [CrossRef]
- Bustamante, A.P.; Valencia, C.; Reuquen, P.; Diaz, P.; Rincion-Rodriguez, R.; Orihuela, P. Role of 2-methoxyestradiol, an Endogenous Estrogen Metabolite, in Health and Disease. Mini-Rev. Med. Chem. 2015, 15, 427–438. [Google Scholar] [CrossRef]
- Saczko, J.; Choromańska, A.; Rembiałkowska, N.; Dubińska-Magiera, M.; Bednarz-Misa, I.; Bar, J.; Marcinkowska, A.; Kulbacka, J. Oxidative modification induced by photodynamic therapy with Photofrin®II and 2-methoxyestradiol in human ovarian clear carcinoma (OvBH-1) and human breast adenocarcinoma (MCF-7) cells. Biomed. Pharmacother. 2015, 71, 30–36. [Google Scholar] [CrossRef]
- Lee, S.-U.; Rhee, M.; Min, Y.K.; Kim, S.H. Involvement of peroxiredoxin IV in the 16α-hydroxyestrone-induced proliferation of human MCF-7 breast cancer cells. Cell Biol. Int. 2008, 32, 401–405. [Google Scholar] [CrossRef]
- Shull, J.D.; Dennison, K.L.; Chack, A.C.; Trentham-Dietz, A. Rat models of 17β-estradiol-induced mammary cancer reveal novel insights into breast canceretiology and prevention. Physiol. Genomics. 2018, 50, 215–234. [Google Scholar] [CrossRef] [PubMed]
- Saczko, J.; Michel, O.; Chwiłkowska, A.; Sawicka, E.; Mączyńska, J.; Kulbacka, J. Estrogen receptors in cell membranes: Regulation and signaling. Adv. Anat. Embryol. Cell Biol. 2017, 227, 93–105. [Google Scholar] [PubMed]
- Samavat, H.; Kurzer, S. Estrogen metabolism and breast cancer. Cancer Lett. 2015, 356, 231–243. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.; Wu, L.; Fu, L.; Wang, B.; Zhou, H. Unifying mechanism in the mitigation of breast cancer by metabolism of estrogen (Review). Mol. Med. Rep. 2017, 16, 1001–1006. [Google Scholar] [CrossRef]
- Paithankara, J.G.; Shiwangi, S.S.; Anurag, D.; Debapratim, S.; Chowdhurib, K. Heavy metal associated health hazards: An inter-play of oxidative stress and signal transduction. Chemosphere 2021, 262, 128350. [Google Scholar] [CrossRef]
- Rembacz, K.P.; Sawicka, E.; Długosz, A. Role of estradiol in chromium-induced oxidative stress. Acta Pol. Pharm. 2012, 69, 1372–1379. [Google Scholar]
- Bednarek-Tupikowska, G.; Tupikowski, K.; Bidzinska, B.; Kuliczkowska, J.; Filus, A.; Milewicz, A. The effect ofestrogen deficiency, estrogen and estro-progestagene therapy on totalplasma homocysteine and serum lipid peroxide levels in postmenopausal women. Ginekol. Pol. 2005, 76, 687–692. [Google Scholar]
- Comsa, S.; Cimpean, A.M.; Raica, M. The story of MCF-7 breast cancer cell line: 40 years of experience in research. Anticancer Res. 2015, 35, 3147–3154. [Google Scholar]
- Fan, T.J.; Han Han, L.H.; Cong, R.S.; Liang, J. Caspase Family Proteases and Apoptosis. Acta. Biochim. Biophys. Sin. 2005, 37, 719–727. [Google Scholar] [CrossRef]
- Nair, S.K.; Verma, A.; Thomas, T.; Chou, T.; Gallo, M.A.; Shirahata, A.; Thomas, T. Synergistic apoptosis of MCF-7 breast cancer cells by 2-methoxyestradiol and bis(ethyl)norspermine. Cancer Lett. 2007, 250, 311–322. [Google Scholar] [CrossRef]
- Chen, Z.H.; Na, H.K.; Hurh, Y.J.; Surh, Y.J. 4-Hydroxyestradiol induces oxidative stress and apoptosis in human mammary epithelial cells: Possible protection by NF-kappaB and ERK/MAPK. Toxicol. Appl. Pharmacol. 2005, 208, 46–56. [Google Scholar] [CrossRef]
- Fussell, K.C.; Udasin, R.G.; Smith, P.J.; Gallo, M.A.; Laskin, J.D. Catechol metabolites of endogenous estrogens induce redox cycling and generate reactive oxygen species in breast epithelial cells. Carcinogenesis 2011, 32, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Hu, L.-L.; Chen, M.-L.; Yang, T.; Wang, J.-H. Analysis of the Distribution Pattern of Chromium Species in Single Cells. Anal. Chem. 2016, 88, 12437–12444. [Google Scholar] [CrossRef] [PubMed]
- Yared, E.; McMillan, T.J.; Martin, F.L. Genotoxic effects of oestrogens in brest cells detected by the micronucleus assay and the Comet assay. Mutagenesis 2002, 17, 345–352. [Google Scholar] [CrossRef]
- Bajpayee, M.; Pandey, A.K.; Parmar, D.; Mathur, N.; Seth, P.K.; Dhawan, A. Comet assay responses in human lymphocytes are not influenced by the menstrual cycle: A study in healthy Indian females. Mutat. Res. Toxicol. Environ. Mutagen. 2005, 565, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Iso, T.; Watanabe, T.; Iwamoto, T.; Shimamoto, A.; Furuichi, Y. DNA Damage Caused by Bisphenol A and Estradiol through Estrogenic Activity. Biol. Pharm. Bull. 2006, 29, 206–210. [Google Scholar] [CrossRef]
- Rajapakse, N.; Butterworth, M.; Kortenkamp, A. Detection of DNA strand breaks and oxidized DNA bases at the single-cell level resulting from exposure to estradiol and hydroxylated metabolites. Environ. Mol. Mutagen. 2005, 45, 397–404. [Google Scholar] [CrossRef]
- Wakeel, A.; Xu, M.; Gan, Y. Chromium-Induced Reactive Oxygen Species Accumulation by Altering the Enzymatic Antioxidant System and Associated Cytotoxic, Genotoxic, Ultrastructural, and Photosynthetic Changes in Plants. Int. J. Mol. Sci. 2020, 2, 728–747. [Google Scholar] [CrossRef] [PubMed]
- Cavallo, D.; Ursini, C.L.; Fresegna, A.M.; Ciervo, A.; Maiello, R.; Rondinone, B.; D’Agata, V.; Iavicoli, S. Direct-oxidative DNA damage and apoptosis induction in different human respiratory cells exposed to low concentrations of sodium chromate. J. Appl. Toxicol. 2010, 30, 218–225. [Google Scholar] [CrossRef]
- Man, S.M.; Kanneganti, T.D. Converging roles of caspases in inflammasome, activataton, cell death and innate immunity. Nat. Rev. Immunol. 2016, 16, 7–21. [Google Scholar] [CrossRef]
- Liehr, J.G. Role of DNA Adducts in Hormonal Carcinogenesis. Regul. Toxicol. Pharmacol. 2000, 32, 276–282. [Google Scholar] [CrossRef]
- Batsi, C.; Markopolou, S.; Kontargiris, E.; Charalambous, C.; Thomas, C.; Christoforidis, S.; Kanaaros, P.; Constantinou, A.I.; Marcu, K.B.; Kolettas, E. Bcl-2-blocks 2-methoxyestradiol induced leukemia cell apoptosis by a p27 Kip1-dependent G1S cell cycle arrest in conjunction with NF-κB activation. Biochem. Pharmacol. 2009, 78, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Tsutsui, T.; Tamura, Y.; Hagiwara, M.; Miyachi, T.; Hikiba, H.; Kubo, C.; Barrett, J.C. Induction of mammalian cell transformation and genotoxicity by 2 methoxyestradiol, an endogenous metabolite of estrogen. Carcinogenesis 2000, 21, 735–740. [Google Scholar] [CrossRef]
- Khoei, S.; Delfan, S.; Neshasteh-Riz, A.; Mahdai, S.R. Evaluation of the combined effect of 2ME2 and 60Co on the inducenebt of DNA damageby IUdR in a spheroid model of the U87MG glioblastoma cancer cell line using alkaline comet assay. Cell J. 2011, 13, 83–90. [Google Scholar] [PubMed]
- Papa, L.; Manfredi, G.; Germain, D. SOD1, an unexpected novel target for cancer therapy. Genes Cancer 2014, 5, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Kepinska, M.; Kizek, R.; Milnerowicz, H. Metallothionein and Superoxide Dismutase—Antioxidative Protein Status in Fullerene-Doxorubicin Delivery to MCF-7 Human Breast Cancer Cells. Int. J. Mol. Sci. 2018, 19, 3253. [Google Scholar] [CrossRef]
- Rao, A.K.; Ziegler, Y.S.; McLeod, I.X.; Yates, J.R.; Nardulli, A.M. Effects of Cu/Zn superoxide dismutase on estrogen responsiveness and oxidative stress in human breast cancer cells. Mol. Endocrinol. 2008, 22, 1113–1124. [Google Scholar] [CrossRef]
- Glasauer, A.; Sena, L.A.; Diebold, L.P.; Mazar, A.P.; Chandel, N.S. Targeting SOD1 reduces experimental non–small-cell lung cancer. J. Clin. Investig. 2013, 124, 117–128. [Google Scholar] [CrossRef]
- Seeger, H.; Wallwiener, D.; Kraemer, E.; Mueck, A.O. Comparison of possible carcinogenic estradiol metabolites: Effects on proliferation, apoptosis and metastasis of human breast cancer cells. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 2084–2090. [Google Scholar] [CrossRef]
- Mueck, A.O.; Seeger, H.; Lippert, T.H. Estradiol metabolism and malignant disease. Maturitas 2002, 43, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ke, H.; Suzuki, A.; Miyamoto, T.; Kashima, H.; Shiozawa, T. 4-hydroxyestrogen induces DNA damage on codon 130/131 of PTEN in endometrial carcinoma cells. Mol. Cell. Endocrinol. 2015, 400, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Zahid, M.; Gaikwad, N.W.; Rogan, E.G.; Cavalieri, E.L. Inhibition of Depurinating Estrogen−DNA Adduct Formation by Natural Compounds. Chem. Res. Toxicol. 2007, 20, 1947–1953. [Google Scholar] [CrossRef]
- Tsutsui, T.; Tamura, Y.; Yagi, E.; Barretti, C. Involvement of genotoxic effects initiation of estrogens-inducted cellular trans-formation: Studies using Syrian hamster embryo cells treated with 17β-estradiol and eight of its metabolites. Int. J. Cancer 2000, 86, 8–14. [Google Scholar] [CrossRef]
- Sawicka, E.; Woźniak, A.; Drąg-Zalesińska, M.; Piwowar, A. Effect of estrogens and their metabolites genotoxicity on the pathogenesis and progression of estrogen-dependent breast cancer. Postepy. Hig. Med. Dosw. 2019, 73, 909–919. [Google Scholar] [CrossRef]
- Mauras, N.; Santen, R.J.; Colón-Otero, G.; Hossain, J.; Wang, Q.; Mesaros, C.; Blair, I.A. Estrogens and their genotoxic metabolites are increased in obese prepubertal girls. J. Clin. Endocrinol. Metab. 2015, 100, 2322–2328. [Google Scholar] [CrossRef] [PubMed]
- Collins, A.R. The Comet Assay for DNA Damage and Repair: Principles, Applications, and Limitations. Appl. Biochem. Biotechnol.—Part B Mol. Biotechnol. 2004, 26, 249–261. [Google Scholar] [CrossRef]
- Cerda, H.; Delincée, H.; Haine, H.; Rupp, H. The DNA ‘comet assay’ as a rapid screening technique to control irradiated food. Mutat. Res. Mol. Mech. Mutagen. 1997, 375, 167–181. [Google Scholar] [CrossRef] [PubMed]
- Kulbacka, J.; Choromańska, A.; Drąg-Zalesińska, M.; Nowak, P.; Baczyńska, D.; Kotulska, M.; Bednarz-Misa, I.; Saczko, J.; Chwiłkowska, A. Proapoptotic activity induced by photodynamic reaction with novel cyanine dyes in caspase-3-deficient human breast adenocarcinoma cell lines (MCF/WT and MCF/DX). Photodiagn. Photodyn. Ther. 2020, 30, 101775. [Google Scholar] [CrossRef]


| IC 50 for Examined Compounds | |||
|---|---|---|---|
| Cr(VI) | 0.001 µM 17β-E2 | 10 µM 17β-E2 | 25 µM 17β-E2 |
| 5.2251 | 4.2423 | 2.1506 | 0.4278 |
| Cr(VI) | 0.001 µM2-MeOE2 | 0.5 µM 2-MeOE2 | 10 µM 2-MeOE2 |
| 5.2251 | 6.4528 | 3.2515 | 2.1813 |
| Cr(VI) | 0.001 µM 4-OHE2 | 0.5 µM 4-OHE2 | 10 µM 4-OHE2 |
| 5.2251 | 3.2589 | 4.5478 | 6.8237 |
| Cr(VI) | 0.001 µM 16α-OHE1 | 10 µM16α-OHE1 | 25 µM16α-OHE1 |
| 5.2251 | 4.2465 | 3.5783 | 6.8957 |
| IC 50 for Examined Compounds | ||||
|---|---|---|---|---|
| 17β-E2 | Cr(VI) | 7 days pre-inc. 0.001 µM 17β-E2 | 7 days pre-inc. 10 µM 17β-E2 | 7 days pre-inc. 25 µM 17β-E2 |
| 5.2251 | 6.6895 | 4.9685 | 12.3467 | |
| 2-MeOE2 | Cr(VI) | 7 days pre-inc. 0.001 µM 2-MeOE2 | 7 days pre-inc. 0.5 µM 2-MeOE2 | days pre-inc. 10 µM 2-MeOE2 |
| 5.2251 | 4.2584 | 6.9854 | 0.2584 | |
| 4-OHE2 | Cr(VI) | 7 days pre-inc. 0.001 µM 4-OHE2 | 7 days pre-inc. 0.5 µM 4-OHE2 | 7 days pre-inc. 10 µM 4-OHE2 |
| 5.2251 | 3.8255 | 4.2857 | 7.2824 | |
| 16α-OHE1 | Cr(VI) | 7 days pre-inc. 0.001µM 16α-OHE1 | 7 days pre-inc. 10 µM 16α-OHE1 | 7 days pre-inc. 25 µM16α-OHE1 |
| 5.2251 | 7.2867 | 9.5857 | 2.9487 | |
| IC 50 for Examined Compounds | |||
|---|---|---|---|
| Cr(VI) | 0.001 µM 17β-E2 | 10 µM 17β-E2 | 25 µM 17β-E2 |
| 5.2251 | 3.9223 | 2.1789 | 0.6267 |
| Cr(VI) | 0.001 µM2-MeOE2 | 0.5 µM 2-MeOE2 | 10 µM 2-MeOE2 |
| 5.2251 | 5.8728 | 3.9875 | 1.9874 |
| Cr(VI) | 0.001 µM 4-OHE2 | 0.5 µM 4-OHE2 | 10 µM 4-OHE2 |
| 5.2251 | 2.9749 | 3.7838 | 7.4537 |
| Cr(VI) | 0.001 µM 16α-OHE1 | 10 µM16α-OHE1 | 25 µM16α-OHE1 |
| 5.2251 | 3.9865 | 2.9783 | 6.0743 |
| IC 50 for Examined Compounds | ||||
|---|---|---|---|---|
| 17β-E2 | Cr(VI) | 7 days pre-inc. 0.001 µM 17β-E2 | 7 days pre-inc. 10 µM 17β-E2 | 7 days pre-inc. 25 µM 17β-E2 |
| 4.5671 | 5.9795 | 5.3485 | 10.8767 | |
| 2-MeOE2 | Cr(VI) | 7 days pre-inc. 0.001 µM 2-MeOE2 | 7 days pre-inc. 0.5 µM 2-MeOE2 | 7 days pre-inc. 10 µM 2-MeOE2 |
| 6.1151 | 3.9985 | 7.1540 | 0.1875 | |
| 4-OHE2 | Cr(VI) | 7 days pre-inc. 0.001 µM 4-OHE2 | 7 days pre-inc. 0.5 µM 4-OHE2 | 7 days pre-inc. 10 µM 4-OHE2 |
| 5.5461 | 4.1563 | 4.7854 | 6.8374 | |
| 16α-OHE1 | Cr(VI) | 7 days pre-inc. 0.001µM 16α-OHE1 | 7 days pre-inc. 10 µM16α-OHE1 | 7 days pre-inc. 25 µM16α-OHE1 |
| 4.8451 | 6.1127 | 7.9987 | 2.3567 | |
| Compound | % of Stained Cells | Intensity of the Reaction |
|---|---|---|
| 17β-E2 [µM] | ||
| 0.001 | 42% | +++ |
| 0.1 | 59% | ++ |
| 10 | 56% | ++/+++ |
| 25 | 45% | ++/+++ |
| Cr(VI)[µM] | ||
| 0.1 | 29% | +/++ |
| 1 | 32% | ++ |
| 5 | 22% | ++ |
| 10 | 37% | ++ |
| 50 | 18% | ++ |
| 2ME2 [µM] | ||
| 0.001 | 38% | ++ |
| 0.1 | 42% | ++ |
| 0.5 | 39% | ++ |
| 10 | 27% | ++ |
| 4-OH [µM] | ||
| 0.001 | 25% | ++ |
| 0.5 | 18% | ++ |
| 10 | 14% | ++ |
| 25 | 34% | ++/+++ |
| 16α-OHE1 [µM] | ||
| 0.001 | 28% | ++ |
| 1 | 32% | ++ |
| 10 | 19% | ++ |
| 25 | 35% | ++ |
| Control | 43% | ++/+++ |
| Cr(VI) [µM] | % of Stained Cells | Intensity of the Reaction | Cr(VI) [µM] | % of Stained Cells | Intensity of the Reaction |
|---|---|---|---|---|---|
| 17β-E2 0.001 µM | 17β-E2 10 µM | ||||
| 0.1 | 21% | ++ | 0.1 | 49% | ++ |
| 1 | 39% | +/++ | 1 | 41% | ++ |
| 5 | 28% | ++ | 5 | 38% | ++ |
| 10 | 27% | ++/+++ | 10 | 46% | ++/+++ |
| 50 | 52% | ++/+++ | 50 | 68% | +++ |
| 17β-E2 0.1 µM | 17β-E2 25 µM | ||||
| 0.1 | 32% | ++/+++ | 0.1 | 47% | ++ |
| 1 | 38% | ++/+++ | 1 | 38% | ++ |
| 5 | 41% | ++ | 5 | 39% | ++ |
| 10 | 49% | ++ | 10 | 37% | ++ |
| 50 | 43% | ++ | 50 | 24% | ++ |
| Control | 43% | ++/+++ | Control | 43% | ++/+++ |
| Cr(VI) [µM] | % of Stained Cells | Intensity of the Reaction | Cr(VI) [µM] | % of Stained Cells | Intensity of the Reaction |
|---|---|---|---|---|---|
| 2-MeOE2 0.001 µM | 2-MeOE2 0.5 µM | ||||
| 0.1 | 42% | ++ | 0.1 | 54% | ++ |
| 1 | 56% | ++ | 1 | 44% | ++ |
| 5 | 61% | ++/+++ | 5 | 27% | ++ |
| 10 | 70% | ++/+++ | 10 | 42% | ++ |
| 50 | 76% | ++/+++ | 50 | 51% | ++ |
| 2-MeOE2 0.1 µM | 2-MeOE2 10 µM | ||||
| 0.1 | 60% | ++ | 0.1 | 45% | ++ |
| 1 | 50% | ++ | 1 | 43% | ++ |
| 5 | 45% | ++ | 5 | 35% | + |
| 10 | 30% | ++/+++ | 10 | 43% | ++ |
| 50 | 50% | ++/+++ | 50 | 59% | ++ |
| Control | 43% | ++/+++ | Control | 43% | ++/+++ |
| Cr(VI) [µM] | % of Stained Cells | Intensity of the Reaction | Cr(VI) [µM] | % of Stained Cells | Intensity of the Reaction |
|---|---|---|---|---|---|
| 4-OHE2 0.001 µM | 4-OHE2 0.5 µM | ||||
| 0.1 | 42% | +++ | 0.1 | 22% | ++ |
| 1 | 36% | ++ | 1 | 32% | ++ |
| 5 | 47% | ++ | 5 | 17% | ++ |
| 10 | 40% | ++ | 10 | 22% | +/++ |
| 50 | 56% | +++ | 50 | 21% | ++ |
| 4-OHE2 10 µM | 4-OHE2 25 µM | ||||
| 0.1 | 25% | ++ | 0.1 | 25% | ++ |
| 1 | 16% | ++ | 1 | 34% | ++ |
| 5 | 27% | ++ | 5 | 21% | + |
| 10 | 23% | ++ | 10 | 29% | +/++ |
| 50 | 37% | ++ | 50 | 28% | ++ |
| Control | 43% | ++/+++ | Control | 43% | ++/+++ |
| Cr(VI) [µM] | % of Stained Cells | Intensity of the Reaction | Cr(VI)2 [µM] | % of Stained Cells | Intensity of the Reaction |
|---|---|---|---|---|---|
| 16α-OHE1 0.001 µM | 16α-OHE1 10 µM | ||||
| 0.1 | 35% | ++ | 0.1 | 43% | ++ |
| 1 | 29% | ++ | 1 | 44% | ++ |
| 5 | 45% | ++ | 5 | 38% | ++ |
| 10 | 28% | ++ | 10 | 56% | + |
| 50 | 35% | + | 50 | 34% | + |
| 16α-OHE1 1 µM | 16α-OHE1 25 µM | ||||
| 0.1 | 50% | ++ | 0.1 | 45% | ++ |
| 1 | 42% | ++ | 1 | 33% | ++ |
| 5 | 39% | ++ | 5 | 45% | ++ |
| 10 | 49% | +/++ | 10 | 53% | ++ |
| 50 | 38% | ++ | 50 | 59% | ++ |
| Control | 43% | ++/+++ | Control | 43% | ++/+++ |
| Name of Compound | Structure and Manufacturer’s Name | Molecular Mass of Compound |
|---|---|---|
| 17β-E2 | 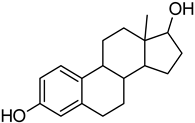 SIGMA-ALDRICH | 272.38 g/mol |
| 2-MeOE2 |  SIGMA-ALDRICH | 302.41 g/mol |
| 4-OHE2 |  SIGMA-ALDRICH | 288.38 g/mol |
| 16α-OHE1 | 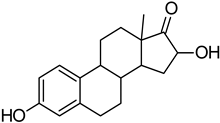 STERALOIDS | 286.40 g/mol |
| potassium chromate (VI) | K2CrO4 SIGMA-ALDRICH | 194.19 g/mol |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sawicka, E.; Kulbacka, J.; Drąg-Zalesińska, M.; Woźniak, A.; Piwowar, A. Effect of Interaction between Chromium(VI) with 17β-Estradiol and Its Metabolites on Breast Cancer Cell Lines MCF-7/WT and MDA-MB-175-VII: Preliminary Study. Molecules 2023, 28, 2752. https://doi.org/10.3390/molecules28062752
Sawicka E, Kulbacka J, Drąg-Zalesińska M, Woźniak A, Piwowar A. Effect of Interaction between Chromium(VI) with 17β-Estradiol and Its Metabolites on Breast Cancer Cell Lines MCF-7/WT and MDA-MB-175-VII: Preliminary Study. Molecules. 2023; 28(6):2752. https://doi.org/10.3390/molecules28062752
Chicago/Turabian StyleSawicka, Ewa, Julita Kulbacka, Małgorzata Drąg-Zalesińska, Arkadiusz Woźniak, and Agnieszka Piwowar. 2023. "Effect of Interaction between Chromium(VI) with 17β-Estradiol and Its Metabolites on Breast Cancer Cell Lines MCF-7/WT and MDA-MB-175-VII: Preliminary Study" Molecules 28, no. 6: 2752. https://doi.org/10.3390/molecules28062752
APA StyleSawicka, E., Kulbacka, J., Drąg-Zalesińska, M., Woźniak, A., & Piwowar, A. (2023). Effect of Interaction between Chromium(VI) with 17β-Estradiol and Its Metabolites on Breast Cancer Cell Lines MCF-7/WT and MDA-MB-175-VII: Preliminary Study. Molecules, 28(6), 2752. https://doi.org/10.3390/molecules28062752







