14-Substituted Diquinothiazines as a New Group of Anticancer Agents
Abstract
1. Introduction
2. Results
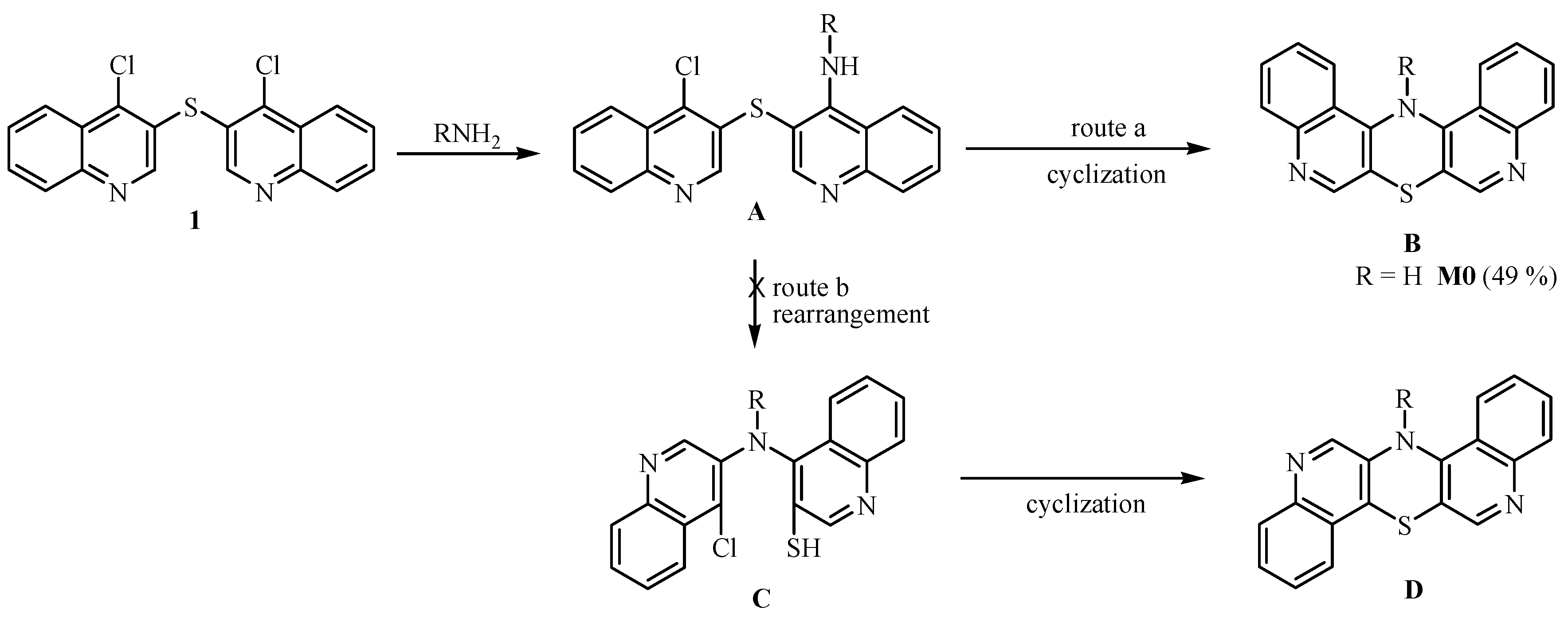
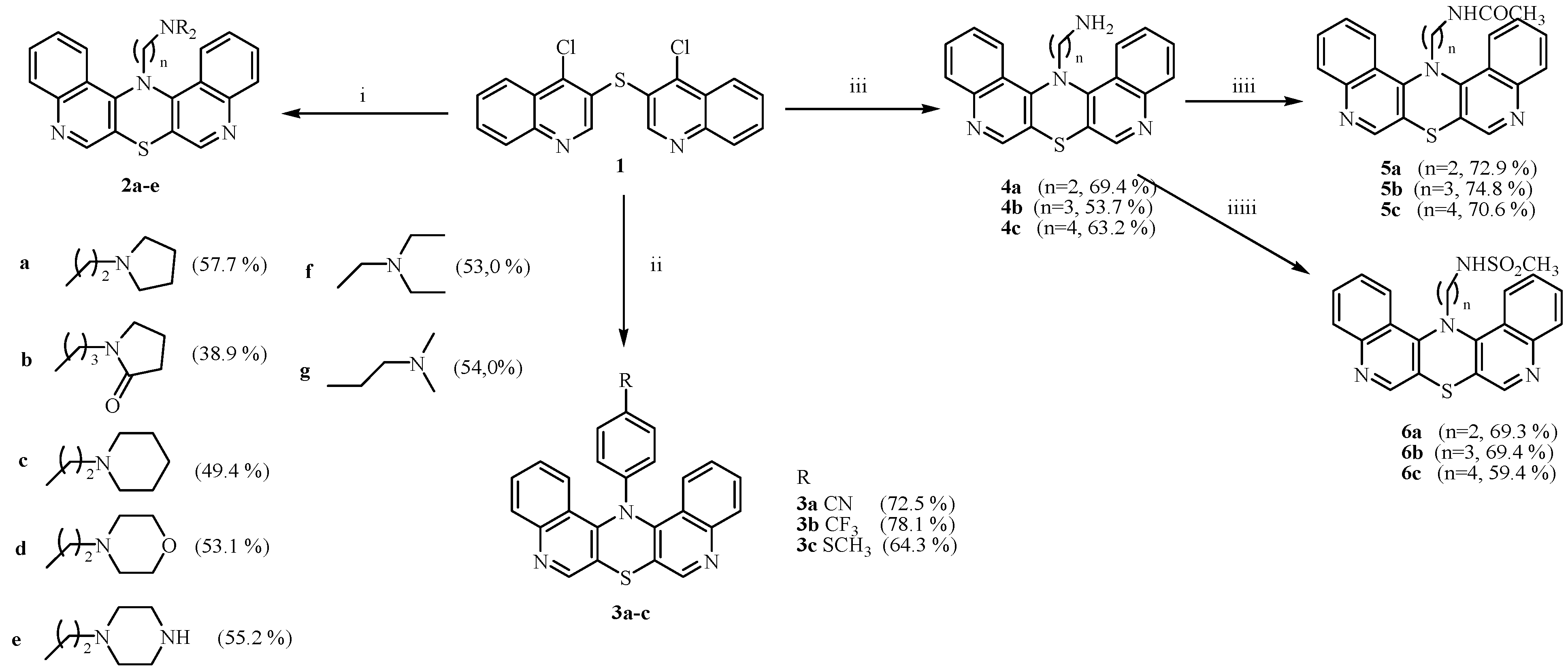
2.1. Chemistry
2.2. Anticancer Activity
2.2.1. Cytotoxicity and Tissue-Specific Anticancer Activities
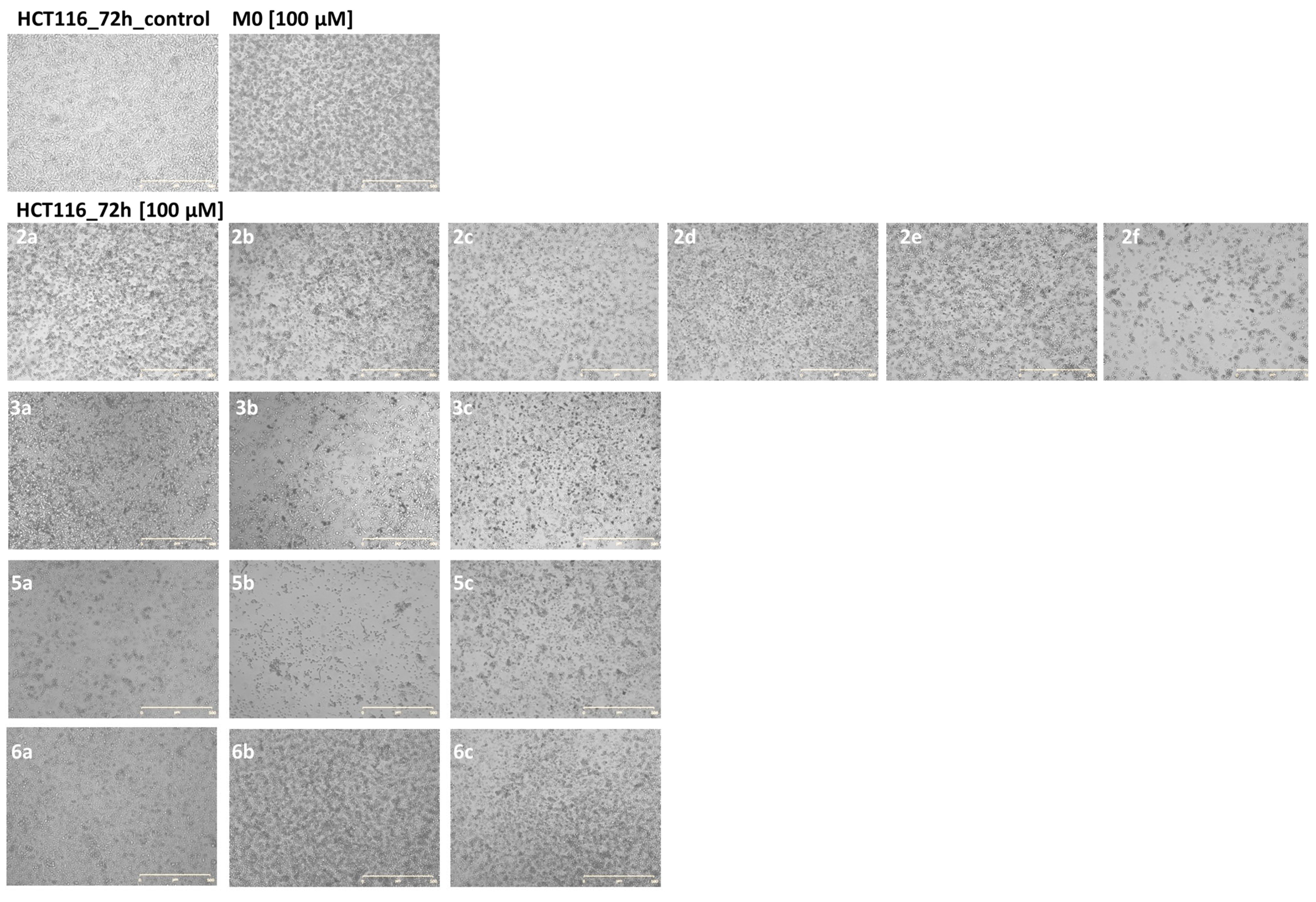
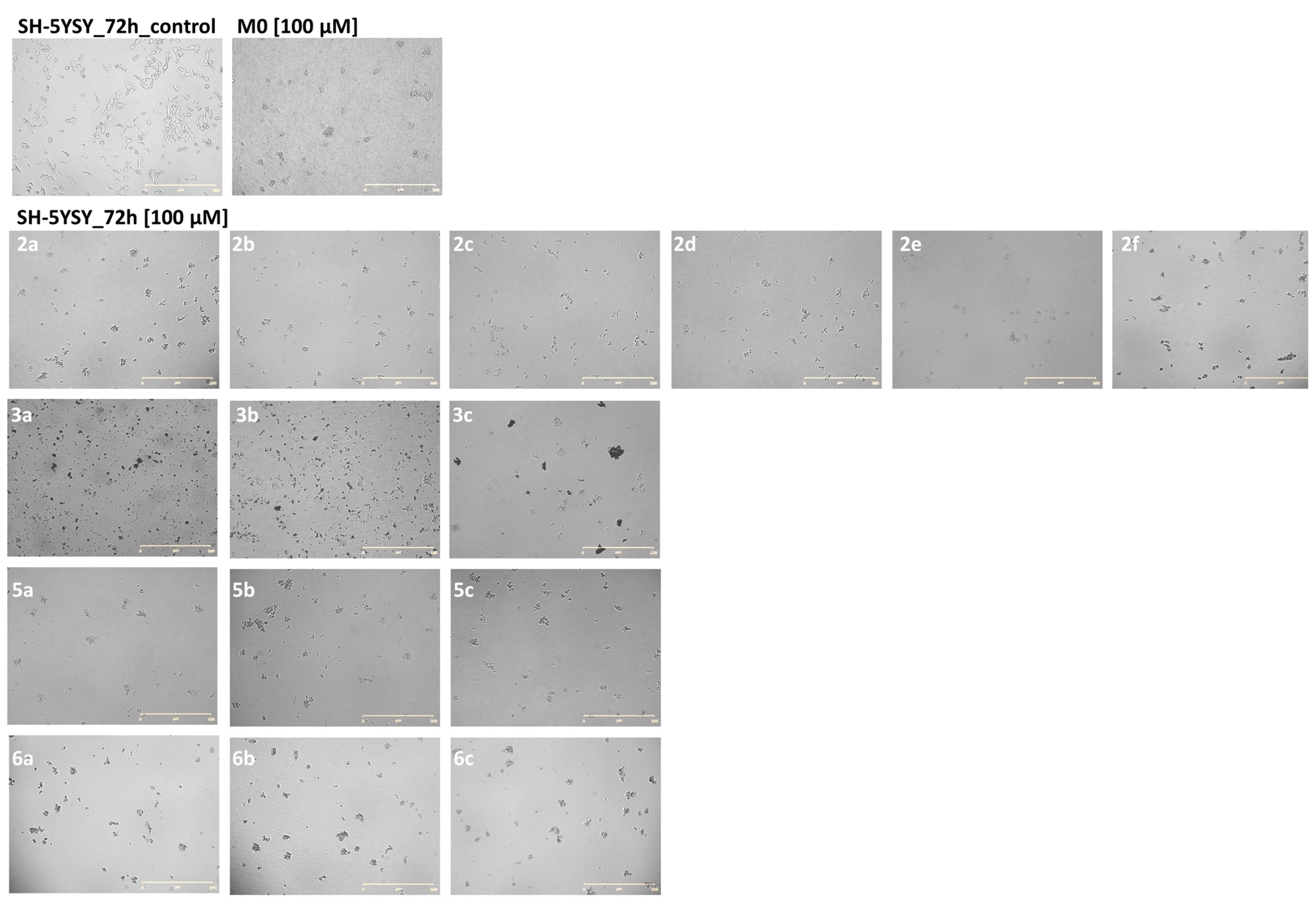
2.2.2. Live Long-Term Microscopic Observations
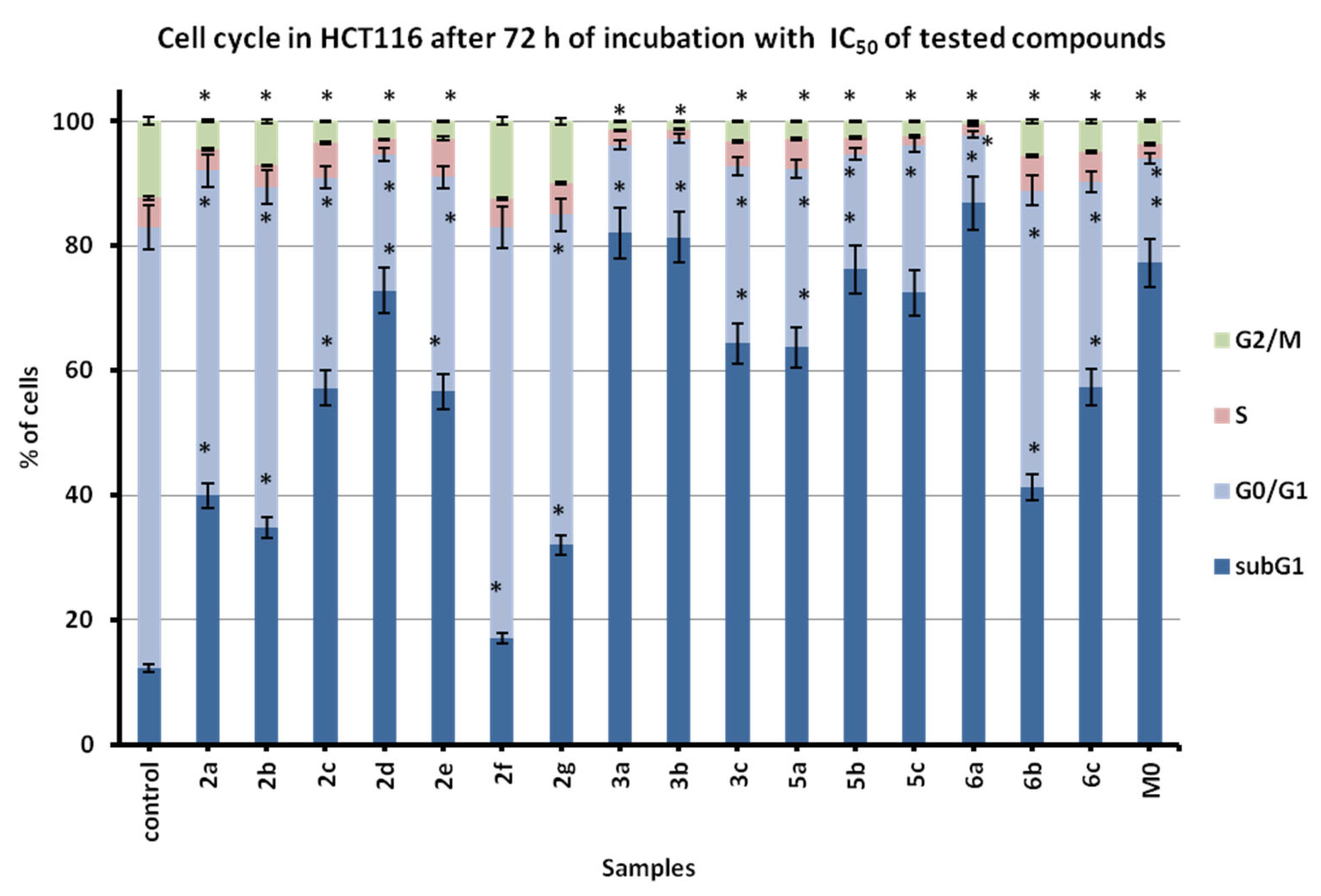
2.2.3. Proapoptotic and Cell Cycle Cytostatic Action
3. Materials and Methods
3.1. Chemistry
3.2. Biological Evaluation
3.2.1. Cell Culturing
3.2.2. Viability MTT Assay
3.2.3. Long-Term Life Microscopic Observations
3.2.4. Flow Cytometry Cell Cycle and Apoptosis Evaluation
3.2.5. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sneader, W. Chronology of Drug Introduction. In Comprehensive Medicinal Chemistry. The Rational Design, Mechanistic Study, and Therapeutic Application of Chemical Compounds; Hansch, C., Sammes, P.G., Taylor, J.B., Eds.; Pergamon Press: Oxford, UK, 1990; Volume 1, pp. 7–80. [Google Scholar]
- Li, J.J. Heterocyclic Chemistry in Drug Discovery; Wiley: Hoboken, NJ, USA, 2013; pp. 1–16. [Google Scholar]
- Gupta, R.R.; Kumar, M. Synthesis, properties and reactions of phenothiazines. In Phenothiazine and 1,4-Benzothiazines—Chemical and Biological Aspect; Elsevier: Amsterdam, The Netherlands, 1988; pp. 1–161. [Google Scholar]
- Mosnaim, A.D.; Ranade, V.V.; Wolf, M.E.; Puente, J.; Valenzuela, M.A. Phenothiazine molecule provides the basic chemical structure for various classes of pharmacotherapeutic agents. Am. J. Therapeut. 2006, 13, 261–273. [Google Scholar] [CrossRef]
- Huang, J.; Zhao, D.; Liu, Z.; Liu, F. Repurposing psychiatric drugs as anticancer agents. Cancer Lett. 2018, 419, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Sudeshna, G.; Parimal, K. Multiple non-psychiatric effects of phenothiazines: A review. Eur. J. Pharmacol. 2010, 648, 6–14. [Google Scholar] [CrossRef]
- Kristiansen, J.E.; Dastidar, S.G.; Palchoudhuri, S.; Roy, D.S.; Das, S.; Hendricks, O.; Christensen, J.B. Phenothiazines as a solution for multidrug resistant tuberculosis: From the origin to present. Int. Microb. 2015, 18, 1–12. [Google Scholar]
- Amaral, L.; Viveiros, M. Thioridazine: A non-antibiotic drug highly effective, in combination with first line antituberculosis drugs, against any form of antibiotic resistance of Mycobacterium tuberculosis due to its multimechanisms of action. Antibiotics 2017, 6, 3. [Google Scholar] [CrossRef]
- Yue, H.; Huang, D.; Qin, L.; Zheng, Z.; Hua, L.; Wang, G.; Huang, J.; Huang, H. Targeting lung cancer stem cells with antipsychological drug thioridazine. Biomed. Res. Int. 2016, 2016, 6709828. [Google Scholar] [CrossRef] [PubMed]
- Spengler, G.; Csonka, Á.; Molnár, J.; Amaral, L. The anticancer activity of the old neuroleptic phenothiazine-type drug thioridazine. Anticancer Res. 2016, 36, 5701–5706. [Google Scholar] [CrossRef]
- Varga, B.; Csonka, Á.; Csonka, A.; Molnár, J.; Amaral, L.; Spengler, G. Possible biological and clinical applications of phenothiazines. Anticancer Res. 2017, 37, 5983–5993. [Google Scholar]
- Motohashi, N.; Kawase, M.; Satoh, K.; Sakagami, H. Cytotoxic potential of phenothiazines. Curr. Drug Targets 2006, 7, 1055–1066. [Google Scholar] [CrossRef]
- Dasgupta, A.; Dastridara, S.G.; Shirataki, Y.; Motohashi, N. Antibacterial activity of artificial phenothiazines and isoflavones from plants. In Topics in Heterocyclic Chemistry; Springer-Verlag: Berlin/Heidelberg, Germany, 2008; pp. 67–132. [Google Scholar]
- Aaron, J.J.; Gaye Seye, M.D.; Trajkovska, S.; Motohashi, N. Bioactive Phenothiazines and Benzo[a]phenothiazines: Spectroscopic studies and biological and biomedical properties and applications. In Topics in Heterocyclic Chemistry; Springer-Verlag: Berlin/Heidelberg, Germany, 2009; pp. 153–231. [Google Scholar]
- Pluta, K.; Morak-Młodawska, B.; Jeleń, M. Recent progress in biological activities of synthesized phenothiazines. Eur. J. Med. Chem. 2011, 46, 3179–3189. [Google Scholar] [CrossRef]
- Jaszczyszyn, A.; Gąsiorowski, K.; Świątek, P.; Malinka, W.; Cieślik-Boczula, K.; Petrus, J.; Czarnik-Matusewicz, B. Chemical structure of phenothiazines and their biological activity. Pharmacol. Rep. 2012, 64, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Pluta, K.; Jeleń, M.; Morak-Młodawska, B.; Zimecki, M.; Artym, J.; Kocięba, M.; Zaczyńska, E. Azaphenothiazines a promising phenothiazine derivatives. An insight into nomenclature, synthesis, structure elucidation, and biological properties. Eur. J. Med. Chem. 2017, 138, 774–806. [Google Scholar] [CrossRef] [PubMed]
- Gopi, C.; Dhanaraj, M.D. Recent progress in synthesis, structure and biological activities of phenothiazine derivatives. Rev. J. Chem. 2019, 9, 95–126. [Google Scholar] [CrossRef]
- Ohlow, M.; Moosmann, B. Phenothiazine: The seven lives of pharmacology’s first lead structure. Drug Discov. Today 2011, 16, 119–131. [Google Scholar] [CrossRef]
- González-Muñoz, G.C.; Arce, M.P.; López, B.; Pérez, C.; Romero, A.; del Barrio, L.; Martín-de-Saavedra, M.D.; Egea, J.; León, R.; Villarroya, M.; et al. Old phenothiazine and dibenzothiadiazepine derivatives for tomorrow’s neuroprotective therapies against neurodegenerative diseases. Eur. J. Med. Chem. 2010, 45, 6152–6158. [Google Scholar] [CrossRef]
- González-Muñoz, G.C.; Arce, M.P.; López, B.; Pérez, C.; Romero, A.; del Barrio, L.; Martín-de-Saavedra, M.D.; Egea, J.; León, R.; Villarroya, M.; et al. N-Acylamino-phenothiazines: Neuroprotective agents displaying multifunctional activity for a potential treatment of Alzheimer’s disease. Eur. J. Med. Chem. 2011, 46, 2224–2235. [Google Scholar] [CrossRef]
- Achan, J.; Talisuna, A.O.; Erhart, A.; Yeka, A.; Tibenderana, J.K.; Baliraine, F.N.; Rosenthal, P.J.; D’Alessandro, U. Quinine, an old anti-malarial drug in a modern world: Role in the treatment of malaria. Malar. J. 2011, 144, 1–12. [Google Scholar] [CrossRef]
- Kaur, K.; Jain, M.; Reddy, R.P.; Jain, R. Quinolines and structurally related heterocycles as antimalarials. Eur. J. Med. Chem. 2010, 45, 3245–3264. [Google Scholar] [CrossRef]
- Kumar, S.; Bawa, S.; Gupta, H. Biological Activities of Quinoline Derivatives. Mini-Rev. Med. Chem. 2009, 9, 1648–1654. [Google Scholar] [CrossRef]
- Sharma, P.C.; Jain, A.; Jain, S. Fluoroquinolone Antibacterials: A review on chemistry, Microbiology and Therapeutic Prospects. Acta Polon. Pharm.-Drug Res. 2009, 66, 587–604. [Google Scholar]
- Oliphant, C.M.; Green, G.M. Quinolones: A Comprehensive Review. Clin. Pharmacol. 2002, 65, 455–464. [Google Scholar]
- Solomon, V.R.; Lee, H. Quinoline as a Privileged Scaffold in Cancer Drug Discovery. Curr. Med. Chem. 2011, 18, 1488–1508. [Google Scholar] [CrossRef] [PubMed]
- Zięba, A.; Latocha, M.; Sochanik, A. Synthesis and in vitro antiproliferative activity of novel 12(H)-quino[3,4-b][1,4]benzothiazine derivatives. Med. Chem. Res. 2013, 22, 4158–4163. [Google Scholar] [CrossRef] [PubMed]
- Jeleń, M.; Pluta, K.; Zimecki, M.; Morak-Młodawska, B.; Artym, J.; Kocięba, M. Synthesis and selected immunological properties of substituted quino[3,2-b]benzo[1,4]thiazines. Eur. J. Med. Chem. 2013, 63, 444–456. [Google Scholar] [CrossRef]
- Jeleń, M.; Pluta, K.; Zimecki, M.; Morak-Młodawska, B.; Artym, J.; Kocięba, M. 6-Substituted 9-fluoroquino[3,2-b]benzo[1,4]thiazines display strong antiproliferative and antitumor properties. Eur. J. Med. Chem. 2015, 89, 411–420. [Google Scholar] [CrossRef]
- Pluta, K.; Szmielew, M.; Suwińska, M.; Latocha, M. Synthesis, spectroscopic structure identification, X-ray study, and anticancer activities of new angularly fused quinobenzothiazines. J. Mol. Struct. 2016, 1122, 62–71. [Google Scholar] [CrossRef]
- Kigasawa, K.; Hiiragi, M.; Wakisaka, K.; Kusuma, O.; Kawasaki, K. Pyrido[2,3-b]benzothiazine Derivatives. Japan Patent No. 79 30,198, 1979. [Google Scholar]
- Refouvelet, B.; Guyon, C.; Jacquot, Y.; Girard, C.; Fein, H.; Bevalot, F.; Robert, J.; Heyd, B.; Mantion, G.; Richert, L.; et al. Synthesis of 4-hydroxycoumarin and 2,4-quinolinediol derivatives and evaluation of their effects on the viability of HepG2 cells and human hepatocytes culture. Eur. J. Med. Chem. 2004, 39, 931–937. [Google Scholar] [CrossRef]
- Virsdoia, V.; Shaikh, M.; Manavar, A.; Desai, B.; Parecha, A.; Loriya, R.; Dholariya, K.; Patel, G.; Vora, V.; Upadhyay, K.; et al. Screening for in vitro antimycobacterial activity and three-dimensional quantitative structure-activity relationship (3D-QUSAR) study of 4-(arylamino)coumarin derivatives. Chem. Biol. Drug Des. 2010, 76, 412–424. [Google Scholar] [CrossRef]
- Anireddy, J.; Rao, A.T.; Reddy, M.A. Molecular modeling studies of a few novel 3,4-heteroannelated quinolin-2-ones with DNA Gyrase and in vitro evaluation of their antibacterial activity. J. Pharm. Res. 2013, 6, 389–394. [Google Scholar]
- Czarny, A.; Zaczyńska, E.; Jeleń, M.; Zimecki, M.; Pluta, K.; Morak-Młodawska, B.; Artym, J.; Kocięba, M. Antibacterial properties of substituted quino[3,2-b]benzo[1,4]thiazines. Polish J. Microb. 2014, 63, 335–339. [Google Scholar] [CrossRef]
- Al-Sinjilavi, H.T.; El-Abadelah, M.M.; Mubarak, M.S.; Al-Aboudi, A.; Abadleh, M.M.; Mahaeneh, A.M.; Ahmad, A.K. Synthesis and antibacterial activity of some novel 4-oxopyrido[2,3-a]phenothiazines. Arch. Pharm. Chem. Life Sci. 2014, 347, 861–872. [Google Scholar] [CrossRef]
- Jeleń, M.; Bavavea, E.I.; Pappa, M.; Kourounakis, A.P.; Morak-Młodawska, B.; Pluta, K. Synthesis of quinoline/naphthalene-containing azaphenothiazines and their potent in vitro antioxidant properties. Med. Chem. Res. 2015, 24, 1725–1732. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Sharma, K.; Samarth, R.M.; Kumar, A. Synthesis and antioxidant activity of quinolinobenzothiazinones. Eur. J. Med. Chem. 2010, 45, 4467–4472. [Google Scholar] [CrossRef] [PubMed]
- Jeleń, M.; Pluta, K.; Zimecki, M.; Morak-Młodawska, B.; Artym, J.; Kocięba, M.; Kochanowska, I. Synthesis and biological evaluation of novel propargylquinobenzothiazines and their derivatives as potential antiproliferative, anti-inflammatory and anticancer agents. J. Enzym. Inhib. Med. Chem. 2016, 31, 83–88. [Google Scholar] [CrossRef]
- Lodarski, K.; Jończyk, J.; Guzior, N.; Bajda, M.; Gładysz, J.; Walczyk, J.; Jeleń, M.; Morak-Młodawska, B.; Pluta, K.; Malawska, B. Discovery of butyrylcholinesterase inhibitors among derivatives of azaphenothiazines. J. Enzym. Inhib. Med. Chem. 2015, 30, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Jończyk, J.; Godyń, J.; Stawarska, E.; Morak-Młodawska, B.; Jeleń, M.; Pluta, K.; Malawska, B. Dual action of dipyridothiazine and quinobenzothiazine derivatives—Anticancer and cholinesterase-inhibiting activity. Molecules 2020, 25, 2604. [Google Scholar] [CrossRef]
- Artym, J.; Kocięba, M.; Zaczyńska, E.; Zimecki, M.; Jeleń, M.; Morak-Młodawska, B.; Pluta, K. Selected azaphenothiazines inhibit delayed type hypersensitivity and carrageenan reaction in mice. Int. Immunopharmacol. 2016, 40, 265–268. [Google Scholar] [CrossRef]
- Artym, J.; Kocięba, M.; Zaczyńska, E.; Kochanowska, I.; Zimecki, M.; Kałas, W.; Fiedorowicz, A.; Pawlak, A.; Strządała, L.; Jeleń, M.; et al. Topically applied azaphenothiazines inhibit experimental psoriasis in mice. Int. Immunopharmacol. 2018, 59, 276–286. [Google Scholar] [CrossRef]
- Artym, J.; Kocięba, M.; Zaczyńska, E.; Zimecki, M.; Jeleń, M.; Morak-Młodawska, B.; Pluta, K.; Kaleta-Kuratewicz, K.; Madej, J.P.; Kuropka, P.; et al. Topically applied azaphenothiazines inhibit contact sensitivity to oxazolone in mice. Histol. Histopathol. 2018, 33, 223–236. [Google Scholar]
- Artym, J.; Kocięba, M.; Zaczyńska, E.; Zimecki, M.; Kałas, W.; Strządała, L.; Pawlak, A.; Jeleń, M.; Morak-Młodawska, B.; Pluta, K.; et al. Therapeutic effects of an azaphenothiazine derivative in mouse experimental colitis. Histol. Histopathol. 2020, 35, 691–699. [Google Scholar]
- Pluta, K.; Jeleń, M.; Morak-Młodawska, B.; Zimecki, M.; Artym, J.; Kocięba, M. Anticancer activity of newly synthesized azaphenothiazines in NCI’s anticancer screening. Pharmacol. Rep. 2010, 62, 319–332. [Google Scholar] [CrossRef]
- Jeleń, M.; Pluta, K.; Latocha, M.; Morak-Młodawska, B.; Suwińska, K.; Kuśmierz, D. Evaluation of angularly condensed diquinothiazines as potential anticancer agents. Bioorg. Chem. 2019, 87, 810–820. [Google Scholar] [CrossRef]
- Strzadala, L.; Fiedorowicz, A.; Wysokinska, E.; Zioło, E.; Grudzień, M.; Jeleń, M.; Pluta, K.; Morak-Młodawska, B.; Zimecki, M.; Kałas, W. An anti-inflammatory azaphenothiazine inhibits interferon β expression and CXCL10 production in KERTr cells. Molecules 2018, 23, 2433. [Google Scholar] [CrossRef]
- Silberg, I.A.; Cormos, G.; Oniciu, D.C. Retrosynthetic approach to the synthesis of phenothiazines. In Advances in Heterocyclic Chemistry; Katritzky, A.R., Ed.; Elsevier: New York, NY, USA, 2006; Volume 90, pp. 205–237. [Google Scholar]
- Pluta, K.; Morak-Młodawska, B.; Jeleń, M. Synthesis and properties of diaza-, triaza- and tetraazaphenothiazines. J. Heterocycl. Chem. 2009, 46, 355–391. [Google Scholar] [CrossRef]
- Pluta, K.; Jeleń, M.; Morak-Młodawska, B. The Smiles rearrangement in the syntheses of azaphenothiazines. Part I. J. Mol. Struct. 2020, 1204, 127501. [Google Scholar] [CrossRef]
- Pluta, K.; Morak-Młodawska, B.; Jeleń, M. The Smiles rearrangement in the syntheses of azaphenothiazines. Part II. The review of the various types of phenyl azinyl and diazinyl sulfides undergoing this rearrangement. J. Mol. Struct. 2020, 1216, 128320. [Google Scholar] [CrossRef]
- Pluta, K. Synthesis and properties of 14-substituted 1,4-thiazinodiquinolines. Phosphorus Sulfur Silicon Relat. Elem. 1997, 126, 145–156. [Google Scholar] [CrossRef]
- Maki, Y. Sulfur-containing pyridine derivatives. LIII. Smiles rearrangement in pyridine derivatives and syntheses of azaphenothiazine derivatives. Yakugaku Zasshi 1957, 77, 485–490. [Google Scholar] [CrossRef]
- Takahashi, T.; Maki, Y. Sulfur-containing pyridine derivatives. LVI. Smiles rearrangement of pyridine derivatives and synthesis of benzopyrido- and dipyrido-1,4-thiazine derivatives. Chem. Pharm. Bull. 1958, 6, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Maki, Y. Sulfur-containing pyridine derivatives. LV. Smiles rearrangement in pyridine derivatives and synthesis of benzopyrido-, dipyridothiazine derivatives. Yakugaku Zasshi 1958, 78, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Rodig, O.; Collier, R.; Schlatzer, R. Pyridine chemistry. II. Further studies on the Smiles rearrangement of the 3-amino-2,2‘-dipyridyl sulfide system. The synthesis of some 1,6-diazaphenothiazines. J. Med. Chem. 1965, 9, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Morak-Młodawska, B.; Pluta, K.; Latocha, M.; Jeleń, M. Synthesis, spectroscopic characterization, and anticancer activity of new 10-substituted 1,6-diazaphenothiazines. Med. Chem. Res. 2016, 25, 2425–2433. [Google Scholar] [CrossRef] [PubMed]
- Okafor, C.O. A novel diazaphenothiazine system. J. Org. Chem. 1967, 32, 2006–2007. [Google Scholar] [CrossRef]
- Morak-Młodawska, B.; Pluta, K.; Zimecki, M.; Jeleń, M.; Artym, J.; Kocięba, M. Synthesis and selected immunological properties of 10-substituted 1,8-diazaphenothiazines. Med. Chem. Res. 2015, 24, 1408–1418. [Google Scholar] [CrossRef]
- Morak-Młodawska, B.; Pluta, K.; Latocha, M.; Suwinska, K.; Jeleń, M.; Kuśmierz, D. 3,6-Diazaphenothiazines as potential lead molecules—synthesis, characterization and anticancer activity. J. Enzym. Inhib. Med. Chem. 2016, 31, 1512–1519. [Google Scholar] [CrossRef]
- Morak-Młodawska, B.; Pluta, K. Synthesis of novel dipyrido-1,4-thiazines. Heterocycles 2007, 71, 1347–1361. [Google Scholar]
- Pluta, K.; Maślankiewicz, A.; Zięba, A. Chlorination of 3,4-quinolinediyl bis-sulfides and 3-thiosubstituted 4-quinolinethiones with phosphoryl chloride. J. Heterocycl. Chem. 1994, 31, 447–451. [Google Scholar] [CrossRef]
- Pluta, K. Synthesis and NMR assignment of 1,4-oxathiino[3,2-c;5,6-c’]diquinoline. J. Heterocyc. Chem. 1994, 31, 557–560. [Google Scholar] [CrossRef]

| Compound No. | IC50 [μM] Cell Line | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| HCT116 | SI | SH-SY5Y | SI | A549 | SI | H1299 | SI | BEAS-2B | |
| M0 | 5.8 ± 0.63 | - | no effect | - | 18.0 ± 3.09 | - | 67.2 ± 9.64 | - | no effect |
| 2a | 11.1 ± 3.39 | 7.6 | 6.5 ± 1.22 | 13 | 13.3 ± 2.23 | 6.3 | 8.1 ± 1.83 | 10.4 | 84.5 ± 11.05 |
| 2b | 9.4 ± 4.41 | 8.9 | 7.7 ± 2.59 | 10.8 | 12.4 ± 2.25 | 6.7 | 5.3 ± 1.04 | 15.8 | 83.5 ± 12.26 |
| 2c | 2.8 ± 0.45 | - | 14.3 ± 1.49 | - | 14.7 ± 2.81 | - | 7.5 ± 1.97 | - | no effect |
| 2d | 23.1 ± 1.37 | 5 | 13.5 ± 2.69 | 8.7 | 20.7 ± 2.25 | 5.7 | 8.9 ± 1.02 | 13.2 | 117.8 ± 18.45 |
| 2e | 10.3 ± 1.82 | 2.5 | 4.9 ± 0.87 | 5.4 | 10.1 ± 2.26 | 2.6 | 7.0 ± 1.85 | 3.8 | 26.5 ± 1.85 |
| 2f | 16.9 ± 1.73 | 7.2 | no effect | - | 27.9 ± 2.07 | 4.4 | 22.2 ± 3.83 | 5.5 | 121.5 ± 12.04 |
| 2g | 13.1 ± 1.82 | - | no effect | - | 31.5 ± 2.36 | - | 24.5 ± 1.91 | - | no effect |
| 3a | 4.9 ± 1.97 | - | no effect | - | 84.9 ± 12.09 | - | 3.7 ± 0.91 | - | no effect |
| 3b | 17.1 ± 4.81 | 5.0 | no effect | - | 42.5 ± 16.53 | 2.0 | 14.6 ± 1.92 | 5.9 | 86.1 ± 10.96 |
| 3c | 2.3 ± 0.51 | 30 | 2.7 ± 0.21 | 31.9 | 17.2 ± 1.02 | 4.0 | 1.6 ± 0.86 | 43.1 | 69.0 ± 4.89 |
| 5a | 25.9 ± 4.87 | 4.1 | 24.7 ± 5.44 | 4.4 | 71.1 ± 14.71 | 1.5 | 26.2 ± 1.99 | 4.1 | 107.7 ± 9.83 |
| 5b | 17.7 ± 1.53 | 4.9 | 21.4 ± 4.02 | 4.1 | 56.5 ± 15.62 | 1.5 | 23.5 ± 1.97 | 3.7 | 86.9 ± 9.67 |
| 5c | 26.5 ± 1.15 | - | 21.9 ± 4.31 | - | 49.3 ± 15.91 | - | 30.3 ± 1.57 | - | no effect |
| 6a | 20.2 ± 1.01 | - | no effect | - | 65.4 ± 14.14 | - | 36.9 ± 6.06 | - | no effect |
| 6b | 15.6 ± 1.16 | - | no effect | - | 45.2 ± 17.16 | - | 25.9 ± 4.14 | - | no effect |
| 6c | 17.6 ± 1.85 | - | 21.6 ± 7.64 | - | 36.9 ± 16.77 | - | 13.4 ± 1.68 | - | no effect |
| etoposide | 8.6 ± 1.42 | 0.0004 | 3.9 ± 0.76 | 0.001 | 4.48 ± 0.21 | 0.001 | 0.6 ± 0.16 | 0.005 | 0.00311 ± 0.0002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeleń, M.; Pluta, K.; Szmielew, M.; Morak-Młodawska, B.; Herman, K.; Giercuszkiewicz, K.; Kasprzycka, A.; Skonieczna, M. 14-Substituted Diquinothiazines as a New Group of Anticancer Agents. Molecules 2023, 28, 3248. https://doi.org/10.3390/molecules28073248
Jeleń M, Pluta K, Szmielew M, Morak-Młodawska B, Herman K, Giercuszkiewicz K, Kasprzycka A, Skonieczna M. 14-Substituted Diquinothiazines as a New Group of Anticancer Agents. Molecules. 2023; 28(7):3248. https://doi.org/10.3390/molecules28073248
Chicago/Turabian StyleJeleń, Małgorzata, Krystian Pluta, Małgorzata Szmielew, Beata Morak-Młodawska, Kinga Herman, Klaudia Giercuszkiewicz, Anna Kasprzycka, and Magdalena Skonieczna. 2023. "14-Substituted Diquinothiazines as a New Group of Anticancer Agents" Molecules 28, no. 7: 3248. https://doi.org/10.3390/molecules28073248
APA StyleJeleń, M., Pluta, K., Szmielew, M., Morak-Młodawska, B., Herman, K., Giercuszkiewicz, K., Kasprzycka, A., & Skonieczna, M. (2023). 14-Substituted Diquinothiazines as a New Group of Anticancer Agents. Molecules, 28(7), 3248. https://doi.org/10.3390/molecules28073248








