Modulation of the Antimelanoma Activity Imparted to Artemisinin Hybrids by the Monoterpene Counterpart
Abstract
:1. Introduction

2. Results and Discussion
3. Materials and Methods
3.1. Chemistry—General Part
3.2. Chemistry—Experimental Procedures and Compound Characterization
3.2.1. Procedure for the Synthesis of Hybrids 9a
3.2.2. General Procedure for the Synthesis of Hybrids 9b–g
3.2.3. General Procedure for the Synthesis of Hybrids 10a–g
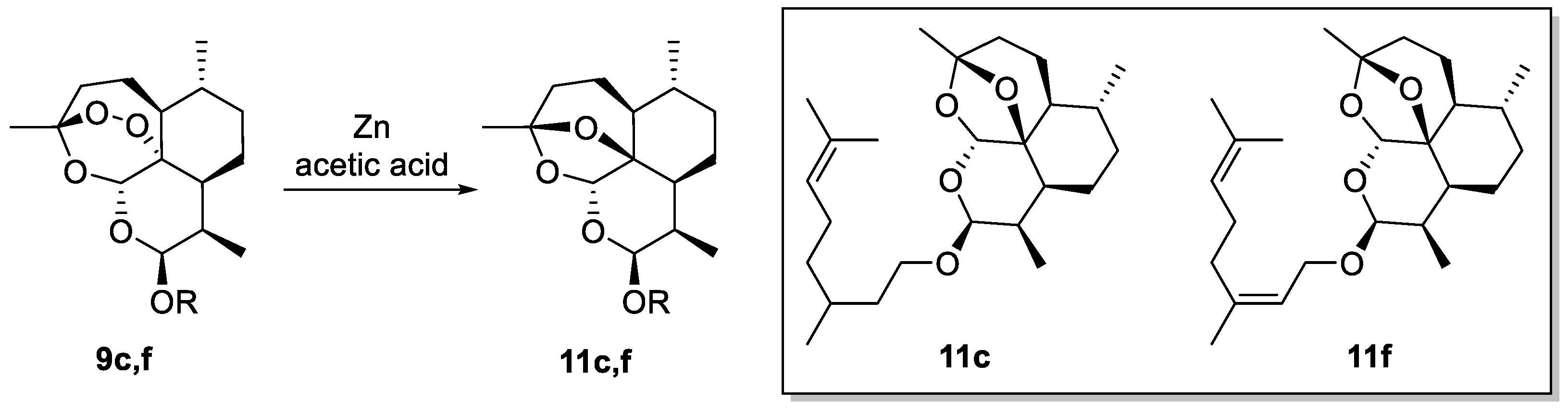
3.2.4. General Procedure for the Synthesis of 2-Deoxy-artemisinin Derivatives 11c and 11f
3.3. Biology
3.3.1. Cell Culture Conditions
3.3.2. General Treatment Protocol and Cell Viability Assay
3.3.3. Co-Administration Analyses
3.3.4. Treatment Protocol for DFO Assay
3.3.5. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anibogwu, R.; Jesus, K.D.; Pradhan, S.; Pashikanti, S.; Mateen, S.; Sharma, K. Extraction, Isolation and Characterization of Bioactive Compounds from Artemisia and Their Biological Significance: A Review. Molecules 2021, 26, 6995. [Google Scholar] [CrossRef] [PubMed]
- Tu, Y. The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nat. Med. 2011, 17, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Appalasamy, S.; Lo, K.Y.; Ch’ng, S.J.; Nornadia, K.; Othman, A.S.; Chan, L.K. Antimicrobial activity of artemisinin and precursor derived from in vitro plantlets of Artemisia annua L. Biomed. Res. Int. 2014, 2014, 215872. [Google Scholar] [CrossRef] [PubMed]
- Romero, M.R.; Efferth, T.; Serrano, M.A.; Castaño, B.; Macias, R.I.R.; Briz, O.; Marin, J.J.G. Effect of artemisinin/artesunate as inhibitors of hepatitis B virus production in an “in vitro” replicative system. Antivir. Res. 2005, 68, 75–83. [Google Scholar] [CrossRef]
- Singh, N.P.; Lai, H.C. Artemisinin induces apoptosis in human cancer cells. Anticancer Res. 2004, 24, 2277–2280. [Google Scholar] [PubMed]
- O’Neill, P.M.; Barton, V.E.; Ward, S.A. The molecular mechanism of action of artemisinin the debate continues. Molecules 2010, 15, 1705–1721. [Google Scholar] [CrossRef] [PubMed]
- Woodley, C.M.; Amado, P.S.M.; Cristiano, M.L.S.; O’Neill, P.M. Artemisinin inspired synthetic endoperoxide drug candidates: Design, synthesis, and mechanism of action studies. Med. Res. Rev. 2021, 41, 3062–3095. [Google Scholar] [CrossRef] [PubMed]
- Augustin, Y.; Staines, H.M.; Krishna, S. Artemisinins as a novel anti-cancer therapy: Targeting a global cancer pandemic through drug repurposing. Pharmacol Ther. 2020, 216, 107706. [Google Scholar] [CrossRef]
- Zeng, Z.W.; Chen, D.; Chen, L.; He, B.; Li, Y. A comprehensive overview of Artemisinin and its derivatives as anticancer agents. Eur. J. Med. Chem. 2023, 247, 115000. [Google Scholar] [CrossRef]
- van Agtmael, M.A.; Eggelte, T.A.; van Boxtel, C.J. Artemisinin drugs in the treatment of malaria: From medicinal herb to registered medication. Trends Pharmacol. Sci. 1999, 20, 199–205. [Google Scholar] [CrossRef]
- China Co-operative Research Group on Qinghaosu and its Derivatives as Antimalarials. J. Tradit. Chin. Med. 1982, 2, 25–30.
- Berköz, M.; Özkan-Yılmaz, F.; Özlüer-Hunt, A.; Krośniak, M.; Türkmen, Ö.; Korkmaz, D.; Keskin, S. Artesunate inhibits melanoma progression in vitro via suppressing STAT3 signaling pathway. Pharmacol. Rep. 2021, 73, 650–663. [Google Scholar] [CrossRef] [PubMed]
- Curti, B.D.; Faries, M.B. Recent Advances in the Treatment of Melanoma. N. Engl. J. Med. 2021, 384, 2229–2240. [Google Scholar] [CrossRef] [PubMed]
- Salvador, D.; Bastos, V.; Oliveira, H. Combined Therapy with Dacarbazine and Hyperthermia Induces Cytotoxicity in A375 and MNT-1 Melanoma Cells. Int. J. Mol. Sci. 2022, 23, 3586. [Google Scholar] [CrossRef] [PubMed]
- Augustine, C.; Yoo, J.S.; Potti, A.; Yoshimoto, Y.; Zipfel, P.; Friedman, H.; Nevins, J.; Ali-Orman, F.; Tyler, D. Predicting sensitivity to temozolomide in melanoma: Genomic and molecular profiling to identify prevailing resistance mechanisms. Cancer Res. 2008, 68, 4786. [Google Scholar]
- Radić, M.; Vlašić, I.; Jazvinšćak Jembrek, M.; Horvat, A.; Tadijan, A.; Sabol, M.; Dužević, M.; Herak Bosnar, M.; Slade, N. Characterization of Vemurafenib-Resistant Melanoma Cell Lines Reveals Novel Hallmarks of Targeted Therapy Resistance. Int. J. Mol. Sci. 2022, 23, 9910. [Google Scholar] [CrossRef] [PubMed]
- Lopes, J.; Rodrigues, C.M.P.; Gaspar, M.M.; Reis, C.P. Melanoma Management: From Epidemiology to Treatment and Latest Advances. Cancers 2022, 14, 4652. [Google Scholar] [CrossRef] [PubMed]
- Huangh, A.C.; Zappasodi, R.A. A decade of checkpoint blockade immunotherapy in melanoma: Understanding the molecular basis for immune sensitivity and resistance. Nat. Immunol. 2022, 23, 660–670. [Google Scholar] [CrossRef]
- Mishra, S.; Singh, P. Hybrid molecules: The privileged scaffolds for various pharmaceuticals. Eur. J. Med. Chem. 2016, 124, 500–536. [Google Scholar] [CrossRef]
- Viegas, C., Jr.; Danuello, A.; da Silva Bolzani, V.; Barreiro, E.J.; Fraga, C.A. Molecular hybridization: A useful tool in the design of new drug prototypes. Curr. Med. Chem. 2007, 14, 1829–1852. [Google Scholar]
- Decker, M. Hybrid molecules incorporating natural products: Applications in cancer therapy, neurodegenerative disorders and beyond. Curr. Med. Chem. 2011, 18, 1464–1475. [Google Scholar] [CrossRef] [PubMed]
- Botta, L.; Filippi, S.; Bizzarri, B.M.; Zippilli, C.; Meschini, R.; Pogni, R.; Baratto, M.C.; Villanova, L.; Saladino, R. Synthesis and Evaluation of Artemisinin-Based Hybrid and Dimer Derivatives as Antimelanoma Agents. ACS Omega 2020, 5, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Tzenkova, R.; Kamenarska, Z.; Draganov, A.; Atanassov, A. Composition of Artemisia annua Essential Oil Obtained from Species Growing Wild in Bulgaria. Biotechnol. Biotechnol. Equip. 2010, 24, 1833–1835. [Google Scholar] [CrossRef]
- Septembre-Malaterre, A.; Lalarizo Rakoto, M.; Marodon, C.; Bedoui, Y.; Nakab, J.; Simon, E.; Hoarau, L.; Savriama, S.; Strasberg, D.; Guiraud, P.; et al. Artemisia annua, a Traditional Plant Brought to Light. Int. J. Mol. Sci. 2020, 21, 4986. [Google Scholar] [CrossRef] [PubMed]
- Haynes, R.K.; Chan, H.-W.; Cheung, M.-K.; Lam, W.-L.; Soo, M.-K.; Tsang, H.-W.; Voerste, A.; Williams, I.D. C-10 Ester and Ether Derivatives of Dihydroartemisinin 2 10-α Artesunate, Preparation of Authentic 10-β Artesunate, and of Other Ester and Ether Derivatives Bearing Potential Aromatic Intercalating Groups at C-10. Eur. J. Org. Chem. 2002, 2002(1), 113–132. [Google Scholar] [CrossRef]
- Herrmann, L.; Hahn, F.; Grau, B.W.; Wild, M.; Niesar, A.; Wangen, C.; Kataev, E.; Marschall, M.; Tsogoeva, S.B. Autofluorescent Artemisinin-Benzimidazole Hybrids via Organo-Click Reaction: Study of Antiviral Properties and Mode of Action in Living Cells. Chemistry 2023, 29, e202301194. [Google Scholar] [CrossRef] [PubMed]


| Entry | Compound | S.C. b | IC50 (µM ± SD) c | TSI d | |||
|---|---|---|---|---|---|---|---|
| C3PV | WM115 | WM266 | WM115 | WM266 | |||
| 1 | DHA 2 | - | 0.7 ± 0.19 | 1.6 ± 0.4 | 1.6 ± 0.03 | 0.4 | 0.4 |
| 2 | ARTA 3 | - | 1.7 ± 0.44 | 1.5 ± 0.01 | 1.3 ± 0.2 | 1.1 | 1.3 |
| 3 | Eugenol 4 | - | 1.0 ± 0.1 | 3.0 ± 0.02 | 0.9 ± 0.05 | 0.3 | 1.1 |
| 4 | Perillyl alcohol 5 | - | 52.5 ± 9.5 | 1.2 ± 0.02 | 0.6 ± 0.04 | 43.8 | 87.5 |
| 5 | (±)-citronellol (±)-6 | - | 3.0 ± 1.2 | 2.6 ± 0.05 | 0.3 ± 0.23 | 1.2 | 10.0 |
| 6 | (+)-citronellol (+)-6 | - | 1.9 ± 0.8 | 1.5 ± 0.07 | 0.6 ± 0.02 | 1.3 | 3.2 |
| 7 | (-)-citronellol (-)-6 | - | 1.0 ± 0.9 | 0.9 ± 0.03 | 0.5 ± 0.3 | 1.1 | 2.0 |
| 8 | Nerol 7 | - | 3.8 ± 1.5 | 1.4 ± 0.03 | 0.5 ± 0.01 | 2.7 | 7.6 |
| 9 | Geraniol 8 | - | 0.5 ± 0.02 | 0.5 ± 0.01 | 0.5 ± 0.09 | 1.0 | 1.0 |
| 10 | 9a | DHA | 0.7 ± 0.04 | 0.1 ± 0.01 | 1.0 ± 0.09 | 7.0 | 0.7 |
| 11 | 9b | DHA | 0.3 ± 0.1 | 0.2 ± 0.01 | 0.2 ± 0.01 | 1.5 | 1.5 |
| 12 | 9c | DHA | 364.2 ± 7.9 | 2.1 ± 0.3 | 1.4 ± 0.56 | 173.4 | 260.1 |
| 13 | 9d | DHA | 51.0 ± 0.3 | 2.9 ± 0.6 | 2.7 ± 0.2 | 17.6 | 18.9 |
| 14 | 9e | DHA | 50.0 ± 0.03 | 2.4 ± 0.1 | 2.2 ± 0.6 | 20.8 | 22.7 |
| 15 | 9f | DHA | 87.3 ± 2.5 | 3.0 ± 0.4 | 1.9 ± 0.5 | 29.1 | 45.9 |
| 16 | 9g | DHA | 6.2 ± 0.7 | 14.5 ± 1.1 | 13.4 ± 1.5 | 0.4 | 0.5 |
| 17 | 10a | ARTA | 1.6 ± 0.3 | 1.5 ± 0.8 | 0.6 ± 0.1 | 1.1 | 2.7 |
| 18 | 10b | ARTA | 20.3 ± 5.5 | 0.03 ± 0.01 | 0.02 ± 0.01 | 676.7 | 1015.0 |
| 19 | 10c | ARTA | 4.4 ± 2.9 | 1.3 ± 0.9 | 0.6 ± 0.02 | 3.4 | 7.3 |
| 20 | 10d | ARTA | 4.8 ± 0.9 | 1.7 ± 0.5 | 1.3 ± 0.8 | 2.8 | 3.7 |
| 21 | 10e | ARTA | 5.1 ± 1.7 | 1.9 ± 0.6 | 1.6 ± 0.9 | 2.7 | 3.2 |
| 22 | 10f | ARTA | 7.9 ± 4.5 | 0.4 ± 0.04 | 0.09 ± 0.03 | 19.8 | 87.8 |
| 23 | 10g | ARTA | 2.4 ± 0.9 | 1.5 ± 0.7 | 1.0 ± 0.1 | 1.6 | 2.4 |
| 24 | PTX | - | 78.9 ± 0.8 | 2.3 ± 0.7 | 0.9 ± 0.04 | 34.3 | 87.7 |
| 25 | 11c | 2-dDHA e | - | - | 35.1 ± 2.5 | - | - |
| 26 | 11f | 2-dDHA e | - | - | 76.3 ± 9.5 | - | - |
| Entry | Combination | R.H. b | IC50 ± SD WM266 c | IC50 ± SD R.H. d |
|---|---|---|---|---|
| 1 | DHA+citronellol (±)-6 | 9c | 4.56 ± 07 | 1.4 ± 0.56 |
| 2 | DHA+nerol 7 | 9f | 5.49 ± 0.6 | 1.9 ± 0.5 |
| 3 | ARTA+perillyl alcohol 5 | 10b | 1.8 ± 0.3 | 0.02 ± 0.01 |
| 4 | ARTA+nerol 7 | 10f | 2.9 ± 0.9 | 0.09 ± 0.03 |
| Entry | Compound b | IC50 ± SD WM266 b,c | |
|---|---|---|---|
| without DFO | with DFO | ||
| 1 | 9c | 1.4 ± 0.56 | 12.7 ± 0.3 |
| 2 | 9f | 1.9 ± 0.5 | 132.7 ± 0.4 |
| 3 | 10b | 0.02 ± 0.01 | 0.31 ± 0.1 |
| 4 | 10f | 0.09 ± 0.03 | 0.5 ± 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Marchi, E.; Filippi, S.; Cesarini, S.; Di Maio, B.; Bizzarri, B.M.; Saladino, R.; Botta, L. Modulation of the Antimelanoma Activity Imparted to Artemisinin Hybrids by the Monoterpene Counterpart. Molecules 2024, 29, 3421. https://doi.org/10.3390/molecules29143421
De Marchi E, Filippi S, Cesarini S, Di Maio B, Bizzarri BM, Saladino R, Botta L. Modulation of the Antimelanoma Activity Imparted to Artemisinin Hybrids by the Monoterpene Counterpart. Molecules. 2024; 29(14):3421. https://doi.org/10.3390/molecules29143421
Chicago/Turabian StyleDe Marchi, Elisa, Silvia Filippi, Silvia Cesarini, Beatrice Di Maio, Bruno Mattia Bizzarri, Raffaele Saladino, and Lorenzo Botta. 2024. "Modulation of the Antimelanoma Activity Imparted to Artemisinin Hybrids by the Monoterpene Counterpart" Molecules 29, no. 14: 3421. https://doi.org/10.3390/molecules29143421
APA StyleDe Marchi, E., Filippi, S., Cesarini, S., Di Maio, B., Bizzarri, B. M., Saladino, R., & Botta, L. (2024). Modulation of the Antimelanoma Activity Imparted to Artemisinin Hybrids by the Monoterpene Counterpart. Molecules, 29(14), 3421. https://doi.org/10.3390/molecules29143421









