Advances in Brain Stimulation, Nanomedicine and the Use of Magnetoelectric Nanoparticles: Dopaminergic Alterations and Their Role in Neurodegeneration and Drug Addiction
Abstract
1. Innovations in Brain Stimulation and Their Applications in Psychiatry and Neurodegeneration
2. Brain Stimulation Therapeutic Intervention in Neurodegenerative and Psychiatric Conditions
2.1. Therapeutic Targets: Dopaminergic Alterations
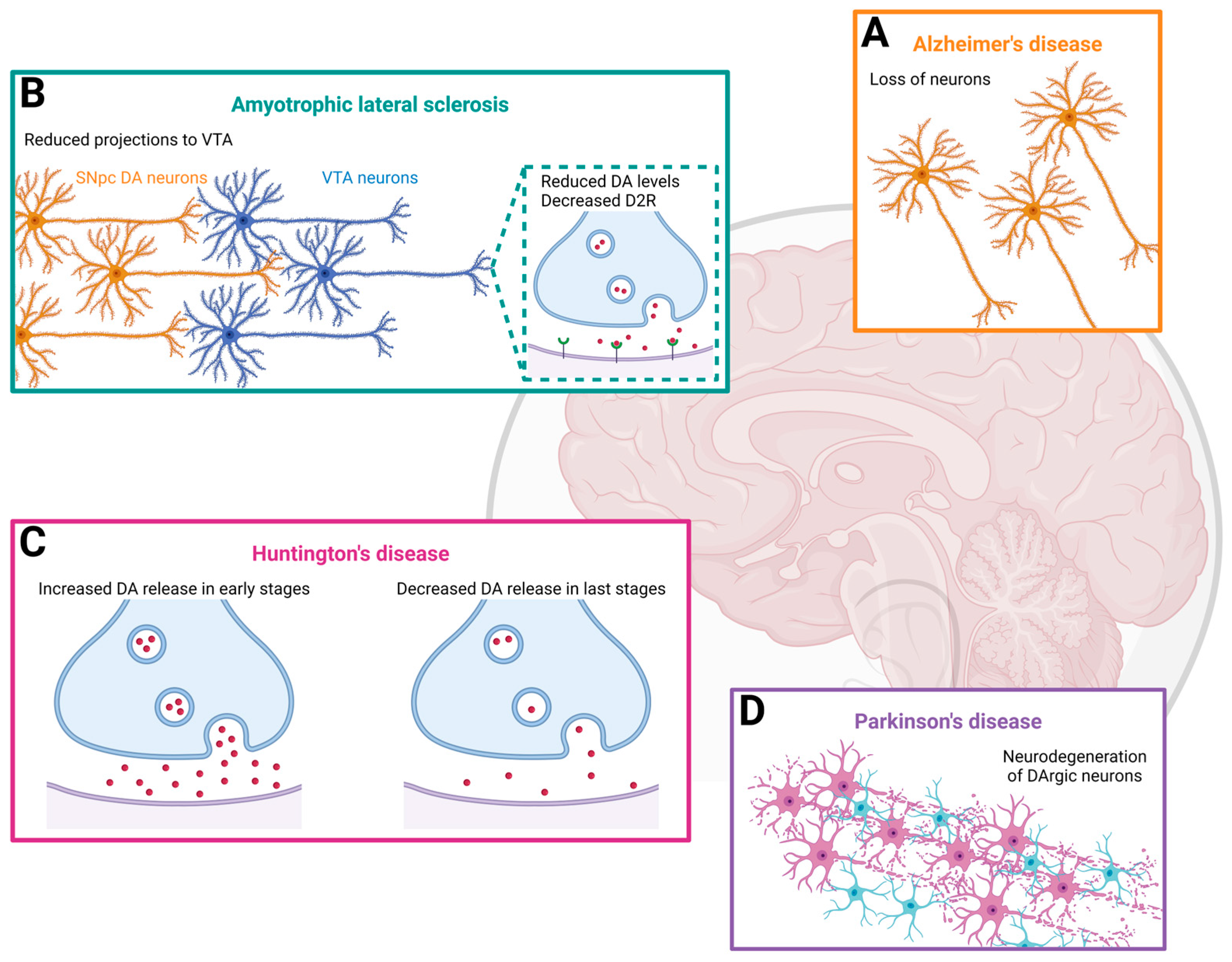
2.1.1. Amyotrophic Lateral Sclerosis (ALS) Symptomatology and Underlying Mechanisms: Hyperexcitability and Dopaminergic Implication
2.1.2. Huntington’s Disease (HD) Symptomatology and Underlying Mechanisms: Dopaminergic Hyperactivity
2.1.3. Alzheimer’s Disease (AD) Symptomatology and Underlying Mechanisms: DA and DA Receptor Reduction
2.1.4. Parkinson’s Disease (PD) Symptomatology and Underlying Mechanisms: Dopaminergic Loss
2.1.5. Drug Addiction: Underlying Mechanism Related to Dopaminergic Implication
2.2. Brain Localization of Aberrant Signaling
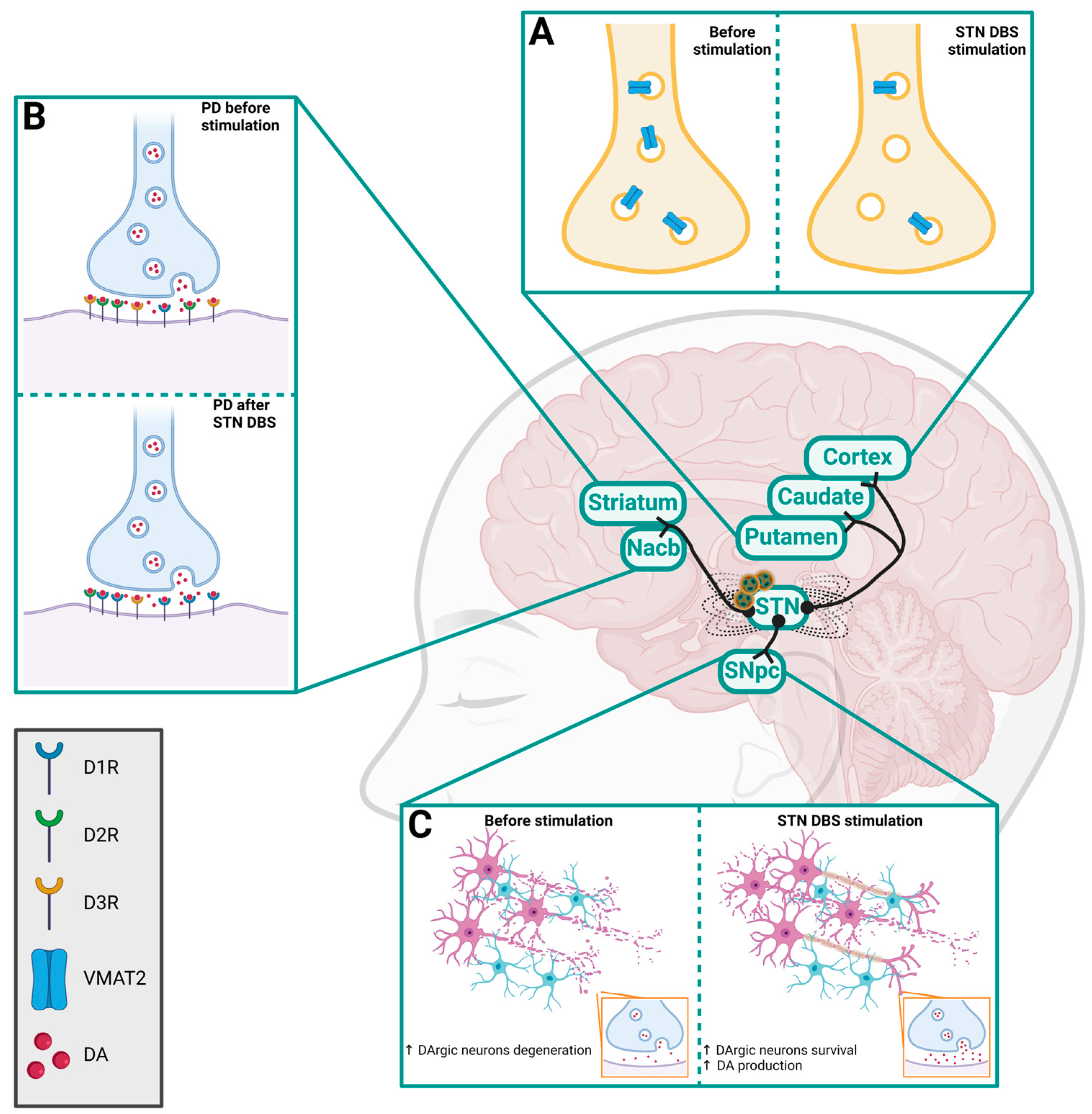
2.2.1. Subthalamic Nucleus (STN)
2.2.2. Substantia Nigra Pars Compacta (SNpc)
2.2.3. Cortical Cortex (CC)
2.2.4. Striatum
2.2.5. Pedunculopontine Nucleus (PPN)
2.2.6. Globus Pallidus (GP)
2.2.7. Additional Brain Areas
3. Innovations on Nanomedicine to Target Aberrant Signaling in Neurodegeneration: Focus on the Dopaminergic Pathway
3.1. Nanotechnology Highlights
3.2. Nanotechnology for DArgic Target in Neurodegeneration and Addiction
4. Introduction of Upcoming Technologies for Brain Stimulation: Magnetoelectric Nanoparticles, the Missing Link between Nanoformulation and Stimulation Approaches
4.1. Current Limitations
4.2. The Progress and Evolution of the New Era: Magnetoelectric Nanoparticles (MENPs)
4.3. Magnetoelectric Nanoparticles (MENPs) for DArgic Target
5. Conclusions: Peculiarity of the DArgic System and Its Target Using MENPs
6. Materials and Methods
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Wu, C.; Yang, L.; Feng, S.; Zhu, L.; Yang, L.; Liu, T.C.-Y.; Duan, R. Therapeutic non-invasive brain treatments in Alzheimer’s disease: Recent advances and challenges. Inflamm. Regen. 2022, 42, 31. [Google Scholar] [CrossRef]
- Van Wamelen, D.J.; Rukavina, K.; Podlewska, A.M.; Chaudhuri, K.R. Advances in the pharmacological and non-pharmacological management of non-motor symptoms in Parkinson’s disease: An update since 2017. Curr. Neuropharmacol. 2023, 21, 1786. [Google Scholar] [CrossRef]
- Frey, J.; Cagle, J.; Johnson, K.A.; Wong, J.K.; Hilliard, J.D.; Butson, C.R.; Okun, M.S.; de Hemptinne, C. Past, present, and future of deep brain stimulation: Hardware, software, imaging, physiology and novel approaches. Front. Neurol. 2022, 13, 825178. [Google Scholar] [CrossRef]
- Fariba, K.A. Deep Brain Stimulation. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024; Available online: https://www.ncbi.nlm.nih.gov/books/NBK557847/ (accessed on 8 March 2024).
- Deep Brain Stimulation. AANS. (n.d.). Available online: https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Deep-Brain-Stimulation (accessed on 3 May 2024).
- Saini, R.K.; Chail, A.; Bhat, P.; Srivastava, K.; Chauhan, V. Transcranial magnetic stimulation: A review of its evolution and current applications. Ind. Psychiatry J. 2018, 27, 172. [Google Scholar] [CrossRef]
- Woods, A.J.; Antal, A.; Bikson, M.; Boggio, P.S.; Brunoni, A.R.; Celnik, P.; Cohen, L.G.; Fregni, F.; Herrmann, C.S.; Kappenman, E.S.; et al. A technical guide to tDCS, and related non-invasive brain stimulation tools. Clin. Neurophysiol. 2016, 127, 1031–1048. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chase, H.W.; Boudewyn, M.A.; Carter, C.S.; Phillips, M.L. Transcranial direct current stimulation: A roadmap for research, from mechanism of action to clinical implementation. Mol. Psychiatry 2020, 25, 397–407. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beisteiner, R.; Lozano, A.M. Transcranial ultrasound innovations ready for broad clinical application. Adv. Sci. 2020, 7, 2002026. [Google Scholar] [CrossRef]
- Beisteiner, R.; Hallett, M.; Lozano, A.M. Ultrasound neuromodulation as a new brain therapy. Adv. Sci. 2023, 10, 2205634. [Google Scholar] [CrossRef]
- Miladinovic, A.; Ajcevic, M.; Busan, P.; Jarmolowska, J.; Silveri, G.; Deodato, M.; Mezzarobba, S.; Battaglini, P.P.; Accardo, A. Evaluation of Motor Imagery-Based BCI methods in neurorehabilitation of Parkinson’s Disease patients. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) in Conjunction with the 43rd Annual Conference of the Canadian Medical and Biological Engineering Society, Montreal, QC, Canada, 20–24 July 2020; pp. 3058–3061. [Google Scholar] [CrossRef] [PubMed]
- Arlotti, M.; Colombo, M.; Bonfanti, A.; Mandat, T.; Lanotte, M.M.; Pirola, E.; Borellini, L.; Rampini, P.; Eleopra, R.; Rinaldo, S.; et al. A New Implantable Closed-Loop Clinical Neural Interface: First Application in Parkinson’s Disease. Front. Neurosci. 2021, 15, 763235. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pirasteh, A.; Ghiyasvand, M.S.; Pouladian, M. EEG-based brain-computer interface methods with the aim of rehabilitating advanced stage ALS patients. Disabil. Rehabil. Assist. Technol. 2024, 24, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wolpaw, J.R. Brain–computer interfaces as new brain output pathways. J. Physiol. 2007, 579, 613–619. [Google Scholar] [CrossRef]
- Vidal, J.J. Toward direct brain-computer communication. Annu. Rev. Biophys. Bioeng. 1973, 2, 157–180. [Google Scholar] [CrossRef] [PubMed]
- Young, M.J.; Lin, D.J.; Hochberg, L.R. Brain-Computer Interfaces in Neurorecovery and Neurorehabilitation. Semin. Neurol. 2021, 41, 206–216. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Musk, E. Neuralink an Integrated Brain-Machine Interface Platform with Thousands of Channels. J. Med. Internet Res. 2019, 21, e16194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Original Records of Each Monkey Used by Neuralink at UC Davis. Physicians Committee for Responsible Medicine. (n.d.). Available online: https://www.pcrm.org/ethical-science/animals-in-medical-research/original-records-neuralink (accessed on 8 May 2024).
- Ryan, H. Elon Musk’s Neuralink Confirms Monkeys Died in Project, Denies Animal Cruelty Claims. CNN Bus, 17 February 2022. Available online: https://edition.cnn.com/2022/02/17/business/elon-musk-neuralink-animal-cruelty-intl-scli/index.html (accessed on 9 May 2024).
- Winkler, R. Elon Musk’s Neuralink Gets FDA Green Light for Second Patient, as First Describes His Emotional Journey. Wall Street Journal, 20 May 2024. [Google Scholar]
- Neuralink Corp. Precise Robotically IMplanted Brain-Computer InterfacE (PRIME). Clin.Trials.gov (n.d.). Available online: https://www.clinicaltrials.gov/study/NCT06429735?term=neuralink&rank=1 (accessed on 9 May 2024).
- Zhang, Z.; Dai, J. Fully implantable wireless brain-computer interface for humans: Advancing toward the future. Innovation 2024, 5, 100595. [Google Scholar] [CrossRef]
- John, S.E.; Grayden, D.B.; Yanagisawa, T. The future potential of the Stentrode. Expert Rev. Med. Devices 2019, 16, 841–843. [Google Scholar] [CrossRef]
- Aguilar-Pérez, M.; Martinez-Moreno, R.; Kurre, W.; Wendl, C.; Bäzner, H.; Ganslandt, O.; Unsöld, R.; Henkes, H. Endovascular treatment of idiopathic intracranial hypertension: Retrospective analysis of immediate and long-patients. Neuroradiology 2017, 59, 277–287. [Google Scholar] [CrossRef]
- Vansteensel, M.J.; Klein, E.; van Thiel, G.; Gaytant, M.; Simmons, Z.; Wolpaw, J.R.; Vaughan, T.M. Towards clinical application of implantable brain–computer interfaces for people with late-stage ALS: Medical and ethical considerations. J. Neurol. 2022, 270, 1323–1336. [Google Scholar] [CrossRef]
- Tayebi, H.; Azadnajafabad, S.; Maroufi, S.F.; Pour-Rashidi, A.; Khorasanizadeh, M.; Faramarzi, S.; Slavin, K.V. Applications of brain-computer interfaces in neurodegenerative diseases. Neurosurg. Rev. 2023, 46, 131. [Google Scholar] [CrossRef] [PubMed]
- Fiani, B.; Reardon, T.; Ayres, B.; Cline, D.; Sitto, S.R. An examination of prospective uses and future directions of Neuralink: The brain-machine interface. Cureus 2021, 13, e14192. [Google Scholar] [CrossRef] [PubMed]
- Sonmez, A.I.; Camsari, D.D.; Nandakumar, A.L.; Voort, J.L.V.; Kung, S.; Lewis, C.P.; Croarkin, P.E. Accelerated TMS for depression: A systematic review and meta-analysis. Psychiatry Res. 2019, 273, 770–781. [Google Scholar] [CrossRef] [PubMed]
- Maia, A.; Almeida, S.; Cotovio, G.; da Silva, D.R.; Viana, F.F.; Grácio, J.; Oliveira-Maia, A.J. Symptom provocation for treatment of obsessive-compulsive disorder using transcranial magnetic stimulation: A step-by-step guide for professional training. Front. Psychiatry 2022, 13, 924370. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reyes-Leiva, D.; Dols-Icardo, O.; Sirisi, S.; Cortés-Vicente, E.; Turon-Sans, J.; de Luna, N.; Blesa, R.; Belbin, O.; Montal, V.; Alcolea, D.; et al. Pathophysiological Underpinnings of Extra-Motor Neurodegeneration in Amyotrophic Lateral Sclerosis: New Insights From Biomarker Studies. Front. Neurol. 2022, 12, 750543. [Google Scholar] [CrossRef] [PubMed]
- Vucic, S.; Ziemann, U.; Eisen, A.; Hallett, M.; Kiernan, M.C. Transcranial magnetic stimulation and amyotrophic lateral sclerosis: Pathophysiological insights. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1161–1170. [Google Scholar] [CrossRef] [PubMed]
- Medhi, B.; Batra, G.; Jain, M.; Singh, R.S.; Sharma, A.R.; Singh, A.; Prakash, A.; Medhi, B. Novel therapeutic targets for amyotrophic lateral sclerosis. Indian J. Pharmacol. 2019, 51, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Tzeplaeff, L.; Wilfling, S.; Requardt, M.V.; Herdick, M. Current state and future directions in the therapy of ALS. Cells 2023, 12, 1523. [Google Scholar] [CrossRef] [PubMed]
- Hoogendam, J.M.; Ramakers, G.M.J.; Di Lazzaro, V. Physiology of repetitive transcranial magnetic stimulation of the human brain. Brain Stimul. 2010, 3, 95–118. [Google Scholar] [CrossRef] [PubMed]
- Blasco, H.; Mavel, S.; Corcia, P.; Gordon, P. The glutamate hypothesis in ALS: Pathophysiology and drug development. Curr. Med. Chem. 2014, 21, 3551–3575. [Google Scholar] [CrossRef]
- Takahashi, H.; Snow, B.J.; Bhatt, M.H.; Peppard, R.F.; Eisen, A.; Calne, D.B. Evidence for a dopaminergic deficiency in sporadic amyotrophic lateral sclerosis on positron emission scanning. Lancet 1993, 342, 1016–1018. [Google Scholar] [CrossRef]
- Hardiman, O.; Al-Chalabi, A.; Chio, A.; Corr, E.M.; Logroscino, G.; Robberecht, W.; Shaw, P.J.; Simmons, Z.; van den Berg, L.H. Amyotrophic lateral sclerosis. Nat. Rev. Dis. Primers 2017, 3, 17071. [Google Scholar] [CrossRef]
- Brunet, A.; Stuart-Lopez, G.; Burg, T.; Scekic-Zahirovic, J.; Rouaux, C. Cortical Circuit Dysfunction as a Potential Driver of Amyotrophic Lateral Sclerosis. Front. Neurosci. 2020, 14, 363. [Google Scholar] [CrossRef] [PubMed]
- Vogels, O.; Veltman, J.; Oyen, W.; Horstink, M. Decreased striatal dopamine D2 receptor binding in amyotrophic lateral sclerosis (ALS) and multiple system atrophy (MSA): D2 receptor down-regulation versus striatal cell degeneration. J. Neurol. Sci. 2000, 180, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Nagata, E.; Ogino, M.; Iwamoto, K.; Kitagawa, Y.; Iwasaki, Y.; Yoshii, F.; Ikeda, J.-E.; ALS Consortium Investigators. Bromocriptine Mesylate Attenuates Amyotrophic Lateral Sclerosis: A Phase 2a, Randomized, Double-Blind, Placebo-Controlled Research in Japanese Patients. PLoS ONE 2016, 11, e0149509, Erratum in PLoS ONE 2016, 11, e0152845. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Roet, K.C.; Zhang, L.; Brault, A.; Berg, A.P.; Jefferson, A.B.; Klug-McLeod, J.; Leach, K.L.; Vincent, F.; Yang, H.; et al. Human amyotrophic lateral sclerosis excitability phenotype screen: Target discovery and validation. Cell Rep. 2021, 35, 109224. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tanaka, K.; Kanno, T.; Yanagisawa, Y.; Yasutake, K.; Hadano, S.; Yoshii, F.; Ikeda, J.-E. Bromocriptine methylate suppresses glial inflammation and moderates disease progression in a mouse model of amyotrophic lateral sclerosis. Exp. Neurol. 2011, 232, 41–52. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, F.; Lüningschrör, P.; Nam, J.; Beckett, L.; Pilotto, F.; Galli, E.; Lindholm, P.; von Collenberg, C.R.; Mungwa, S.T.; Jablonka, S.; et al. CDNF rescues motor neurons in models of amyotrophic lateral sclerosis by targeting endoplasmic reticulum stress. Brain 2023, 146, 3783–3799. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cleveland, D.W.; Rothstein, J.D. From Charcot to Lou Gehrig: Deciphering selective motor neuron death in ALS. Nat. Rev. Neurosci. 2001, 2, 806–819. [Google Scholar] [CrossRef] [PubMed]
- Roos, R.A.C. Huntington’s disease: A clinical review. Orphanet. J. Rare Dis. 2010, 5, 40. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cepeda, C.; Murphy, K.P.S.; Parent, M.; Levine, M.S. The role of dopamine in Huntington’s disease. Prog. Brain Res. 2014, 211, 235–254. [Google Scholar] [CrossRef]
- Kim, A.; Lalonde, K.; Truesdell, A.; Gomes Welter, P.; Brocardo, P.S.; Rosenstock, T.R.; Gil-Mohapel, J. New avenues for the treatment of Huntington’s disease. Int. J. Mol. Sci. 2021, 22, 8363. [Google Scholar] [CrossRef]
- André, V.M.; Cepeda, C.; Levine, M.S. Dopamine and glutamate in Huntington’s disease: A balancing act. CNS Neurosci. Ther. 2010, 16, 163–178. [Google Scholar] [CrossRef] [PubMed]
- Koch, E.T.; Raymond, L.A. Dysfunctional striatal dopamine signaling in Huntington’s disease. J. Neurosci. Res. 2019, 97, 1636–1654. [Google Scholar] [CrossRef] [PubMed]
- Tang, T.-S.; Chen, X.; Liu, J.; Bezprozvanny, I. Dopaminergic signaling and striatal neurodegeneration in Huntington’s disease. J. Neurosci. 2007, 27, 7899–7910. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.L.; Mason, S.L.; Vallin, B.; Barker, R.A. Reduced expression of dopamine D2 receptors on astrocytes in R6/1 HD mice and HD post-mortem tissue. Neurosci. Lett. 2022, 767, 136289. [Google Scholar] [CrossRef] [PubMed]
- Squitieri, F.; Di Pardo, A.; Favellato, M.; Amico, E.; Maglione, V.; Frati, L. Pridopidine, a dopamine stabilizer, improves motor performance and shows neuroprotective effects in Huntington disease R6/2 mouse model. J. Cell Mol. Med. 2015, 19, 2540–2548. [Google Scholar] [CrossRef] [PubMed]
- Schwab, L.C.; Garas, S.N.; Drouin-Ouellet, J.; Mason, S.L.; Stott, S.R.; Barker, R.A. Dopamine and Huntington’s disease. Expert Rev. Neurother. 2015, 15, 445–458. [Google Scholar] [CrossRef] [PubMed]
- Jabłońska, M.; Grzelakowska, K.; Wiśniewski, B.; Mazur, E.; Leis, K.; Gałązka, P. Pridopidine in the treatment of Huntington’s disease. Rev. Neurosci. 2020, 31, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Grachev, I.D.; Meyer, P.M.; Becker, G.A.; Bronzel, M.; Marsteller, D.; Pastino, G.; Voges, O.; Rabinovich, L.; Knebel, H.; Zientek, F.; et al. Sigma-1 and dopamine D2/D3 receptor occupancy of pridopidine in healthy volunteers and patients with Huntington disease: A [18F] fluspidine and [18F] fallypride PET study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1103–1115. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; Clarence-Smith, K. Tetrabenazine therapy of dystonia, chorea, tics, and other dyskinesias and disorders of movement. J. Clin. Psychiatry 1993, 54, 25–28. [Google Scholar]
- Cepeda, C.; Levine, M.S. Synaptic Dysfunction in Huntington’s Disease: Lessons from Genetic Animal Models. Neuroscientist 2022, 28, 20–40. [Google Scholar] [CrossRef]
- Bonomo, R.; Elia, A.E.; Bonomo, G.; Romito, L.M.; Mariotti, C.; Devigili, G.; Cilia, R.; Giossi, R.; Eleopra, R. Deep brain stimulation in Huntington’s disease: A literature review. Neurol. Sci. 2021, 42, 4447–4457. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Xu, Y.-Y.; Gao, Y.; Li, J.-M.; Liu, X.-W.; Wang, M.-Q.; Deng, H.; Xiao, L.-L.; Ren, H.-B.; Xiong, B.-T.; et al. Deep brain stimulation for chorea-acanthocytosis: A systematic review. Neurosurg. Rev. 2022, 45, 1861–1871. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.; Kaminga, A.C.; Wen, S.W.; Wu, X.; Acheampong, K.; Liu, A. Dopamine and Dopamine Receptors in Alzheimer’s Disease: A Systematic Review and Network Meta-Analysis. Front. Aging Neurosci. 2019, 11, 175. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, M.T.; Iulita, M.F.; Cavedo, E.; Chiesa, P.A.; Schumacher Dimech, A.; Santuccione Chadha, A.; Baracchi, F.; Girouard, H.; Misoch, S.; Giacobini, E.; et al. Sex Differences in Alzheimer Disease—The Gateway to Precision Medicine. Nat. Rev. Neurol. 2018, 14, 457–469. [Google Scholar] [CrossRef] [PubMed]
- Tiernan, C.T.; Ginsberg, S.D.; He, B.; Ward, S.M.; Guillozet-Bongaarts, A.L.; Kanaan, N.M.; Mufson, E.J.; Counts, S.E. Pretangle Pathology within Cholinergic Nucleus Basalis Neurons Coincides with Neurotrophic and Neurotransmitter Receptor Gene Dysregulation during the Progression of Alzheimer’s Disease. Neurobiol. Dis. 2018, 117, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Koch, G.; Di Lorenzo, F.; Bonnì, S.; Giacobbe, V.; Bozzali, M.; Caltagirone, C.; Martorana, A. Dopaminergic Modulation of Cortical Plasticity in Alzheimer’s Disease Patients. Neuropsychopharmacology 2014, 39, 2654–2661. [Google Scholar] [CrossRef] [PubMed]
- Martorana, A.; Mori, F.; Esposito, Z.; Kusayanagi, H.; Monteleone, F.; Codecà, C.; Sancesario, G.; Bernardi, G.; Koch, G. Dopamine Modulates Cholinergic Cortical Excitability in Alzheimer’s Disease Patients. Neuropsychopharmacology 2009, 34, 2323–2328. [Google Scholar] [CrossRef] [PubMed]
- Drayton, S.J.; Davies, K.; Steinberg, M.; Leroi, I.; Rosenblatt, A.; Lyketsos, C.G. Amantadine for Executive Dysfunction Syndrome in Patients with Dementia. Psychosomatics 2004, 45, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, N.; Rothenburg, L.S.; Black, S.E.; Ryan, M.; Liu, B.A.; Busto, U.E.; Lanctôt, K.L. Methylphenidate for the Treatment of Apathy in Alzheimer Disease: Prediction of Response Using Dextroamphetamine Challenge. J. Clin. Psychopharmacol. 2008, 28, 296–301. [Google Scholar] [CrossRef]
- Mintzer, J.; Greenspan, A.; Caers, I.; Van Hove, I.; Kushner, S.; Weiner, M.; Gharabawi, G.; Schneider, L.S. Risperidone in the Treatment of Psychosis of Alzheimer Disease: Results from a Prospective Clinical Trial. Am. J. Geriatr. Psychiatry 2006, 14, 280–291. [Google Scholar] [CrossRef]
- Lanctôt, K.L.; Herrmann, N.; Black, S.E.; Ryan, M.; Rothenburg, L.S.; Liu, B.A.; Busto, U.E. Apathy Associated with Alzheimer Disease: Use of Dextroamphetamine Challenge. Am. J. Geriatr. Psychiatry 2008, 16, 551–557. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.-Q.; Tang, X.-C. Comparative Studies of Huperzine A, Donepezil, and Rivastigmine on Brain Acetylcholine, Dopamine, Norepinephrine, and 5-Hydroxytryptamine Levels in Freely-Moving Rats. Acta Pharmacol. Sin. 2006, 27, 1127–1136. [Google Scholar] [CrossRef] [PubMed]
- Schilström, B.; Ivanov, V.B.; Wiker, C.; Svensson, T.H. Galantamine Enhances Dopaminergic Neurotransmission In Vivo Via Allosteric Potentiation of Nicotinic Acetylcholine Receptors. Neuropsychopharmacology 2007, 32, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, C.H.; Swanson, C.J.; Aisen, P.; Bateman, R.J.; Chen, C.; Gee, M.; Kanekiyo, M.; Li, D.; Reyderman, L.; Cohen, S.; et al. Lecanemab in Early Alzheimer’s Disease. N. Engl. J. Med. 2023, 388, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Kurkinen, M.T. Lecanemab (Leqembi) is Not the Right Drug for Patients with Alzheimer’s Disease. Adv. Clin. Exp. Med. 2023, 32, 943–947. [Google Scholar] [CrossRef]
- Cools, R. The Costs and Benefits of Brain Dopamine for Cognitive Control. Wiley Interdiscip. Rev. Cogn. Sci. 2016, 7, 317–329. [Google Scholar] [CrossRef]
- Cools, R.; Froböse, M.; Aarts, E.; Hofmans, L. Dopamine and the Motivation of Cognitive Control. Handb. Clin. Neurol. 2019, 163, 123–143. [Google Scholar]
- Kemppainen, N.; Laine, M.; Laakso, M.P.; Kaasinen, V.; Någren, K.; Vahlberg, T.; Kurki, T.; Rinne, J.O. Hippocampal Dopamine D2 Receptors Correlate with Memory Functions in Alzheimer’s Disease. Eur. J. Neurosci. 2003, 18, 149–154. [Google Scholar] [CrossRef]
- Cordella, A.; Krashia, P.; Nobili, A.; Pignataro, A.; La Barbera, L.; Viscomi, M.T.; Valzania, A.; Keller, F.; Ammassari-Teule, M.; Mercuri, N.B.; et al. Dopamine Loss Alters the Hippocampus-Nucleus Accumbens Synaptic Transmission in the Tg2576 Mouse Model of Alzheimer’s Disease. Neurobiol. Dis. 2018, 116, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Sprugnoli, G.; Munsch, F.; Cappon, D.; Paciorek, R.; Macone, J.; Connor, A.; El Fakhri, G.; Salvador, R.; Ruffini, G.; Donohoe, K.; et al. Impact of Multisession 40Hz tACS on Hippocampal Perfusion in Patients with Alzheimer’s Disease. Alzheimer’s Res. Ther. 2021, 13, 203. [Google Scholar] [CrossRef]
- Laxton, A.W.; Tang-Wai, D.F.; McAndrews, M.P.; Zumsteg, D.; Wennberg, R.; Keren, R.; Wherrett, J.; Naglie, G.; Hamani, C.; Smith, G.S.; et al. A Phase I Trial of Deep Brain Stimulation of Memory Circuits in Alzheimer’s Disease. Ann. Neurol. 2010, 68, 521–534. [Google Scholar] [CrossRef] [PubMed]
- Sankar, T.; Chakravarty, M.M.; Bescos, A.; Lara, M.; Obuchi, T.; Laxton, A.W.; McAndrews, M.P.; Tang-Wai, D.F.; Workman, C.I.; Smith, G.S.; et al. Deep Brain Stimulation Influences Brain Structure in Alzheimer’s Disease. Brain Stimul. 2015, 8, 645–654. [Google Scholar] [CrossRef]
- Lozano, A.M.; Fosdick, L.; Chakravarty, M.M.; Leoutsakos, J.-M.; Munro, C.; Oh, E.; Drake, K.E.; Lyman, C.H.; Rosenberg, P.B.; Anderson, W.S.; et al. A Phase II Study of Fornix Deep Brain Stimulation in Mild Alzheimer’s Disease. J. Alzheimer’s Dis. 2016, 54, 777–787. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Warner, T.T.; Schapira, A.H.V. Genetic and environmental factors in the cause of Parkinson’s disease. Ann. Neurol. 2003, 53 (Suppl. S3), S16–S23; discussion S23–S25. [Google Scholar] [CrossRef] [PubMed]
- Escande, M.V.; Taravini, I.R.; Zold, C.L.; Belforte, J.E.; Murer, M.G. Loss of homeostasis in the direct pathway in a mouse model of asymptomatic Parkinson’s disease. J. Neurosci. 2016, 36, 5686–5698. [Google Scholar] [CrossRef] [PubMed]
- Bartels, A.L.; Leenders, K.L. Parkinson’s disease: The syndrome, the pathogenesis and pathophysiology. Cortex 2009, 45, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Kalia, L.V.; Lang, A.E. Parkinson’s disease. Lancet 2015, 386, 896–912. [Google Scholar] [CrossRef] [PubMed]
- LeWitt, P.A. Levodopa therapy for Parkinson’s disease: Pharmacokinetics and pharmacodynamics. Mov. Disord. 2015, 30, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Buck, K.; Ferger, B. L-DOPA-induced dyskinesia in Parkinson’s disease: A drug discovery perspective. Drug Discov. Today 2010, 15, 867–875. [Google Scholar] [CrossRef]
- Braun, A.; Fabbrini, G.; Mouradian, M.M.; Serrati, C.; Barone, P.; Chase, T.N. Selective D-1 dopamine receptor agonist treatment of Parkinson’s disease. J. Neural Transm. 1987, 68, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Bracco, F.; Battaglia, A.; Chouza, C.; Dupont, E.; Gershanik, O.; Masso, J.F.M.; Montastruc, J.-L.; PKDS009 Study Group. The long-acting dopamine receptor agonist cabergoline in early Parkinson’s disease: Final results of a 5-year, double-blind, levodopa-controlled study. CNS Drugs 2004, 18, 733–746, Erratum in CNS Drugs 2005, 19, 633. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Lewis, M.M.; Van Scoy, L.J.; De Jesus, S.; Eslinger, P.J.; Arnold, A.C.; Miller, A.J.; Fernandez-Mendoza, J.; Snyder, B.; Harrington, W.; et al. The D1/D5 dopamine partial agonist PF-06412562 in advanced-stage Parkinson’s disease: A feasibility study. J. Park. Dis. 2020, 10, 1515–1527. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, R.; Li, J.; Wu, Y.; Liang, S.; Xu, L. Association of Multiple Dopamine D3 Receptor Gene 3′UTR Polymorphisms with Susceptibility to Parkinson’s Disease and Clinical Efficacy of Piribedil Therapy. Genet. Test. Mol. Biomark. 2021, 25, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Soileau, M.J.; Aldred, J.; Budur, K.; Fisseha, N.; Fung, V.S.; Jeong, A.; Kimber, T.E.; Klos, K.; Litvan, I. Safety and efficacy of continuous subcutaneous foslevodopa-foscarbidopa in patients with advanced Parkinson’s disease: A randomised, double-blind, active-controlled, phase 3 trial. Lancet Neurol. 2022, 21, 1099–1109. [Google Scholar] [CrossRef] [PubMed]
- Aldred, J.; Freire-Alvarez, E.; Amelin, A.V.; Antonini, A.; Bergmans, B.; Bergquist, F.; Bouchard, M.; Budur, K.; Carroll, C.; Chaudhuri, K.R.; et al. Continuous subcutaneous foslevodopa/foscarbidopa in Parkinson’s disease: Safety and efficacy results from a 12-month, single-arm, open-label, phase 3 study. Neurol. Ther. 2023, 12, 1937–1958. [Google Scholar] [CrossRef]
- Zheng, H.-B.; Liu, B.; Shen, J.; Xie, F.; Ji, Q.-M.; Zhu, X.-Y. Non-invasive brain stimulation for treating psychiatric symptoms in Parkinson’s disease: A systematic review and meta-analysis. J. Clin. Neurosci. 2022, 106, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Bucur, M.; Papagno, C. Deep brain stimulation in Parkinson disease: A meta-analysis of the long-term neuropsychological outcomes. Neuropsychol. Rev. 2023, 33, 307–346. [Google Scholar] [CrossRef]
- Witjas, T.; Baunez, C.; Henry, J.M.; Delfini, M.; Regis, J.; Cherif, A.A.; Peragut, J.C.; Azulay, J.P. Addiction in Parkinson’s disease: Impact of subthalamic nucleus deep brain stimulation. Mov. Disord. 2005, 20, 1052–1055. [Google Scholar] [CrossRef] [PubMed]
- Heymann, D.; Stern, Y.; Cosentino, S.; Tatarina-Nulman, O.; Dorrejo, J.N.; Gu, Y. The Association Between Alcohol Use and the Progression of Alzheimer’s Disease. Curr. Alzheimer Res. 2016, 13, 1356–1362. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Berríos-Cárcamo, P.; Quezada, M.; Quintanilla, M.E.; Morales, P.; Ezquer, M.; Herrera-Marschitz, M.; Israel, Y.; Ezquer, F. Oxidative Stress and Neuroinflammation as a Pivot in Drug Abuse. A Focus on the Therapeutic Potential of Antioxidant and Anti-Inflammatory Agents and Biomolecules. Antioxidants 2020, 9, 830. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Simpson, D.S.A.; Oliver, P.L. ROS Generation in Microglia: Understanding Oxidative Stress and Inflammation in Neurodegenerative Disease. Antioxidants 2020, 9, 743. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Trifilieff, P.; Martinez, D. Imaging addiction: D2 receptors and dopamine signaling in the striatum as biomarkers for impulsivity. Neuropharmacology 2014, 76 Pt B, 498–509. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Volkow, N.D.; Wang, G.; Fowler, J.S.; Tomasi, D.; Telang, F.; Baler, R. Addiction: Decreased reward sensitivity and increased expectation sensitivity conspire to overwhelm the brain’s control circuit. Bioessays 2010, 32, 748–755. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Koob, G.F.; Volkow, N.D. Neurobiology of addiction: A neurocircuitry analysis. Lancet Psychiatry 2016, 3, 760–773. [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.-J.; Fowler, J.S.; Tomasi, D.; Telang, F. Addiction: Beyond dopamine reward circuitry. Proc. Natl. Acad. Sci. USA 2011, 108, 15037–15042. [Google Scholar] [CrossRef]
- Yuan, S.; Jiang, S.-C.; Zhang, Z.-W.; Li, Z.-L.; Hu, J. Substance Addiction Rehabilitation Drugs. Pharmaceuticals 2024, 17, 615. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhaskar, L.V.K.S.; Thangaraj, K.; Wasnik, S.; Singh, L.; Rao, V.R. Dopamine transporter (DAT1) VNTR polymorphism and alcoholism in two culturally different populations of south India. Am. J. Addict. 2012, 21, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Koijam, A.S.; Hijam, A.C.; Singh, A.S.; Jaiswal, P.; Mukhopadhyay, K.; Rajamma, U.; Haobam, R. Association of Dopamine Transporter Gene with Heroin Dependence in an Indian Subpopulation from Manipur. J. Mol. Neurosci. 2021, 71, 122–136. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, J.J.; Hanlon, C.A.; Marshalek, P.J.; Rezai, A.R.; Krinke, L. Transcranial magnetic stimulation, deep brain stimulation, and other forms of neuromodulation for substance use disorders: Review of modalities and implications for treatment. J. Neurol. Sci. 2020, 418, 117149. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bach, P.; Luderer, M.; Müller, U.J.; Jakobs, M.; Baldermann, J.C.; Voges, J.; Kiening, K.; Lux, A.; Visser-Vandewalle, V.; Klosterkötter, J.; et al. Deep brain stimulation of the nucleus accumbens in treatment-resistant alcohol use disorder: A double-blind randomized controlled multi-center trial. Transl. Psychiatry 2023, 13, 49. [Google Scholar] [CrossRef]
- Kuhn, J.; Möller, M.; Treppmann, J.F.; Bartsch, C.; Lenartz, D.; Gruendler, T.O.J.; Maarouf, M.; Brosig, A.; Barnikol, U.B.; Klosterkötter, J.; et al. Deep brain stimulation of the nucleus accumbens and its usefulness in severe opioid addiction. Mol. Psychiatry 2014, 19, 145–146. [Google Scholar] [CrossRef]
- Taremian, F.; Nazari, S.; Moradveisi, L.; Moloodi, R. Transcranial direct current stimulation on opium craving, depression, and anxiety: A preliminary study. J. ECT 2019, 35, 201. [Google Scholar] [CrossRef]
- Chen, L.; Li, N.; Ge, S.; Lozano, A.M.; Lee, D.J.; Yang, C.; Li, L.; Bai, Q.; Lu, H.; Wang, J.; et al. Long-term results after deep brain stimulation of nucleus accumbens and the anterior limb of the internal capsule for preventing heroin relapse: An open-label pilot study. Brain Stimul. 2019, 12, 175–183. [Google Scholar] [CrossRef]
- Iqbal, J.; Mansour, M.N.M.; Saboor, H.A.; Suyambu, J.; Lak, M.A.; Zeeshan, M.H.; Hafeez, M.H.; Arain, M.; Mehmood, M.; Mehmood, D.; et al. Role of deep brain stimulation (DBS) in addiction disorders. Surg. Neurol. Int. 2023, 14, 434. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mehta, D.D.; Praecht, A.; Ward, H.B.; Sanches, M.; Sorkhou, M.; Tang, V.M.; Steele, V.R.; Hanlon, C.A.; George, T.P. A systematic review and meta-analysis of neuromodulation therapies for substance use disorders. Neuropsychopharmacology 2024, 49, 649–680. [Google Scholar] [CrossRef]
- Kuhn, J.; Buhrle, C.P.; Lenartz, D.; Sturm, V. Deep brain stimulation in addiction due to psychoactive substance use. Handb. Clin. Neurol. 2013, 116, 259–269. [Google Scholar] [CrossRef]
- Wang, T.R.; Moosa, S.; Dallapiazza, R.F.; Elias, W.J.; Lynch, W.J. Deep brain stimulation for the treatment of drug addiction. Neurosurg. Focus 2018, 45, E11. [Google Scholar] [CrossRef]
- Rajamani, N.; Friedrich, H.; Butenko, K.; Dembek, T.; Lange, F.; Navrátil, P.; Zvarova, P.; Hollunder, B.; de Bie, R.M.A.; Odekerken, V.J.J.; et al. Deep brain stimulation of symptom-specific networks in Parkinson’s disease. Nat. Commun. 2024, 15, 4662. [Google Scholar] [CrossRef]
- Dieckmann, N.; Stubendorff, B.; Ilse, B.; Rödiger, A.; Witte, O.; Mayer, T.; Steinbach, R.; Grosskreutz, J. P 1 Grey matter atrophy in Amyotrophic Lateral Sclerosis correlates with quantitative disease progression. Clin. Neurophysiol. 2022, 137, e15. [Google Scholar] [CrossRef]
- Cai, W.; Young, C.B.; Yuan, R.; Lee, B.; Ryman, S.; Kim, J.; Yang, L.; Levine, T.F.; Henderson, V.W.; Poston, K.L.; et al. Subthalamic nucleus–language network connectivity predicts dopaminergic modulation of speech function in Parkinson’s disease. Proc. Natl. Acad. Sci. USA 2024, 121, e2316149121. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zavala, B.; Zaghloul, K.; Brown, P. The subthalamic nucleus, oscillations, and conflict. Mov. Disord. 2015, 30, 328–338. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bostan, A.C.; Dum, R.P.; Strick, P.L. The basal ganglia communicate with the cerebellum. Proc. Natl. Acad. Sci. USA 2010, 107, 8452–8456. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Smith, G.S.; Mills, K.A.; Pontone, G.M.; Anderson, W.S.; Perepezko, K.M.; Brasic, J.; Zhou, Y.; Brandt, J.; Butson, C.R.; Holt, D.P.; et al. Effect of STN DBS on vesicular monoamine transporter 2 and glucose metabolism in Parkinson’s disease. Park. Relat. Disord. 2019, 64, 235–241. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Spieles-Engemann, A.; Behbehani, M.; Collier, T.; Wohlgenant, S.; Steece-Collier, K.; Paumier, K.; Daley, B.; Gombash, S.; Madhavan, L.; Mandybur, G.; et al. Stimulation of the rat subthalamic nucleus is neuroprotective following significant nigral dopamine neuron loss. Neurobiol. Dis. 2010, 39, 105–115. [Google Scholar] [CrossRef]
- Temel, Y.; Visser-Vandewalle, V.; Kaplan, S.; Kozan, R.; Daemen, M.A.; Blokland, A.; Schmitz, C.; Steinbusch, H.W. Protection of nigral cell death by bilateral subthalamic nucleus stimulation. Brain Res. 2006, 1120, 100–105. [Google Scholar] [CrossRef]
- Maesawa, S.; Kaneoke, Y.; Kajita, Y.; Usui, N.; Misawa, N.; Nakayama, A.; Yoshida, J. Long-term stimulation of the subthalamic nucleus in hemiparkinsonian rats: Neuroprotection of dopaminergic neurons. J. Neurosurg. 2004, 100, 679–687. [Google Scholar] [CrossRef]
- Wallace, B.A.; Ashkan, K.; Heise, C.E.; Foote, K.D.; Torres, N.; Mitrofanis, J.; Benabid, A.-L. Survival of midbrain dopaminergic cells after lesion or deep brain stimulation of the subthalamic nucleus in MPTP-treated monkeys. Brain 2007, 130, 2129–2145. [Google Scholar] [CrossRef]
- Benazzouz, A.; Gao, D.; Ni, Z.; Benabid, A.-L. High frequency stimulation of the STN influences the activity of dopamine neurons in the rat. NeuroReport 2000, 11, 1593–1596. [Google Scholar] [CrossRef]
- Helf, C.; Kober, M.; Markert, F.; Lanto, J.; Overhoff, L.; Badstübner-Meeske, K.; Storch, A.; Fauser, M. Subthalamic nucleus deep brain stimulation induces nigrostriatal dopaminergic plasticity in a stable rat model of Parkinson’s disease. NeuroReport 2023, 34, 506–511. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Carcenac, C.; Favier, M.; Vachez, Y.; Lacombe, E.; Carnicella, S.; Savasta, M.; Boulet, S. Subthalamic deep brain stimulation differently alters striatal dopaminergic receptor levels in rats. Mov. Disord. 2015, 30, 1739–1749. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.H.; Koch, R.J.; Moore, C.; Meshul, C.K. Subthalamic nucleus stimulation and lesioning have distinct state-dependent effects upon striatal dopamine metabolism. Synapse 2009, 63, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Davidson, B.; Milosevic, L.; Kondrataviciute, L.; Kalia, L.V.; Kalia, S.K. Neuroscience fundamentals relevant to neuromodulation: Neurobiology of deep brain stimulation in Parkinson’s disease. Neurotherapeutics 2024, 21, e00348. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rouaud, T.; Lardeux, S.; Panayotis, N.; Paleressompoulle, D.; Cador, M.; Baunez, C. Reducing the desire for cocaine with subthalamic nucleus deep brain stimulation. Proc. Natl. Acad. Sci. USA 2009, 107, 1196–1200. [Google Scholar] [CrossRef]
- Sahai, S.; Effendi, E.T.; Mahoney, E.C.; Tucker, H.R.; Moolick, B.J.; Mamone, G.; Mikkilineni, S.; Gupta, M.; Nicholson, A.; Chua, F.Y.; et al. Effects of subthalamic nucleus deep brain stimulation on neuronal spiking activity in the substantia nigra pars compacta in a rat model of Parkinson’s disease. Neurosci. Lett. 2020, 739, 135443. [Google Scholar] [CrossRef] [PubMed]
- Villadóniga, M.; Cabañes-Martínez, L.; López-Viñas, L.; Fanjul, S.; del Álamo, M.; Regidor, I. Combined Stimulation of the Substantia Nigra and the Subthalamic Nucleus for the Treatment of Refractory Gait Disturbances in Parkinson’s Disease: A Preliminary Study. J. Clin. Med. 2022, 11, 2269. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Obeso, J.A.; Olanow, C.W.; Rodriguez-Oroz, M.C.; Krack, P.; Kumar, R.; Lang, A.E. Deep-brain stimulation of the subthalamic nucleus or the pars interna of the globus pallidus in Parkinson’s disease. N. Engl. J. Med. 2001, 345, 956–963. [Google Scholar]
- Hesse, S.; Strecker, K.; Winkler, D.; Luthardt, J.; Scherfler, C.; Reupert, A.; Oehlwein, C.; Barthel, H.; Schneider, J.-P.; Wegner, F.; et al. Effects of subthalamic nucleus stimulation on striatal dopaminergic transmission in patients with Parkinson’s disease within one-year follow-up. J. Neurol. 2008, 255, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Gülşen, Ç.; Koçer, B.; Çomoğlu, S.S.; Gündüz, A.G. The effect of subthalamic nucleus deep brain stimulation and dopaminergic treatment on dual-task manual dexterity in Parkinson’s disease. Neurol. Sci. 2023, 44, 1633–1641. [Google Scholar] [CrossRef] [PubMed]
- Gruber, D.; Kuhn, A.A.; Schoenecker, T.; Kopp, U.A.; Kivi, A.; Huebl, J.; Lobsien, E.; Mueller, B.; Schneider, G.-H.; Kupsch, A. Quadruple deep brain stimulation in Huntington’s disease, targeting pallidum and subthalamic nucleus: Case report and review of the literature. J. Neural Transm. 2014, 121, 1303–1312. [Google Scholar] [CrossRef]
- Kaymak, A.; Vissani, M.; Lenge, M.; Melani, F.; Fino, E.; Cappelletto, P.; Tuccinardi, G.; Cavallo, M.A.; Giordano, F.; Mazzoni, A. Patterns of neural activity and clinical outcomes in a juvenile Huntington’s Disease patient undergoing Deep Brain Stimulation of the subthalamic nucleus. Deep. Brain Stimul. 2023, 1, 15–19. [Google Scholar] [CrossRef]
- Ni, A.; Ernst, C. Evidence that substantia nigra pars compacta dopaminergic neurons are selectively vulnerable to oxidative stress because they are highly metabolically active. Front. Cell Neurosci. 2022, 16, 826193. [Google Scholar] [CrossRef] [PubMed]
- Mittal, S.K.; Eddy, C. The role of dopamine and glutamate modulation in Huntington disease. Behav. Neurol. 2013, 26, 255–263. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ramesh, S.; Arachchige, A.S.P.M. Depletion of dopamine in Parkinson’s disease and relevant therapeutic options: A review of the literature. AIMS Neurosci. 2023, 10, 200–231. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kazee, A.M.; Cox, C.; Richfield, E.K. Substantia nigra lesions in Alzheimer disease and normal aging. Alzheimer Dis. Assoc. Disord. 1995, 9, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.T.; Yu, M.A.; Zhang, K.; Zhang, J.G. Effect of deep brain stimulation on substantia nigra neurons in a rat model of Parkinson’s disease. Chin. Med. J. 2012, 125, 4072–4075. [Google Scholar] [PubMed]
- Sutton, A.C.; Yu, W.; Calos, M.E.; Smith, A.B.; Ramirez-Zamora, A.; Molho, E.S.; Pilitsis, J.G.; Brotchie, J.M.; Shin, D.S. Deep brain stimulation of the substantia nigra pars reticulata improves forelimb akinesia in the hemiparkinsonian rat. J. Neurophysiol. 2013, 109, 363–374. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhang, L.; Meng, S.; Chen, W.; Chen, Y.; Huang, E.; Zhang, G.; Liang, Y.; Ding, Z.; Xue, Y.; Shi, J.; et al. High-frequency deep brain stimulation of the substantia nigra pars reticulata facilitates extinction and prevents reinstatement of methamphetamine-induced conditioned place preference. Front. Pharmacol. 2021, 12, 705813. [Google Scholar] [CrossRef] [PubMed]
- Haslinger, B.; Kalteis, K.; Boecker, H.; Alesch, F.; Ceballos-Baumann, A.O. Frequency-correlated decreases of motor cortex activity associated with subthalamic nucleus stimulation in Parkinson’s disease. NeuroImage 2005, 28, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Qian, Z.M.; Arbuthnott, G.W.; Ke, Y.; Yung, W.H. Cortical effects of deep brain stimulation: Implications for pathogenesis and treatment of Parkinson disease. JAMA Neurol. 2014, 71, 100–103. [Google Scholar] [CrossRef]
- Ranieri, F.; Mariotto, S.; Dubbioso, R.; Di Lazzaro, V. Brain Stimulation as a Therapeutic Tool in Amyotrophic Lateral Sclerosis: Current Status and Interaction with Mechanisms of Altered Cortical Excitability. Front. Neurol. 2021, 11, 605335. [Google Scholar] [CrossRef]
- Fakhrieh-Asl, G.; Sadr, S.S.; Karimian, S.M.; Riahi, E. Deep brain stimulation of the orbitofrontal cortex prevents the development and reinstatement of morphine place preference. Addict. Biol. 2020, 25, e12780. [Google Scholar] [CrossRef] [PubMed]
- Fattahi, M.; Eskandari, K.; Riahi, E.; Khosrowabadi, R.; Haghparast, A. Distinct suppressing effects of deep brain stimulation in the orbitofrontal cortex on the development, extinction, and reinstatement of methamphetamine-seeking behaviors. Life Sci. 2023, 322, 121613. [Google Scholar] [CrossRef] [PubMed]
- Rangel-Barajas, C.; Rebec, G.V. Dysregulation of Corticostriatal Connectivity in Huntington’s Disease: A Role for Dopamine Modulation. J. Huntington’s Dis. 2016, 5, 303–331. [Google Scholar] [CrossRef] [PubMed]
- Cataldi, S.; Stanley, A.T.; Miniaci, M.C.; Sulzer, D. Interpreting the role of the striatum during multiple phases of motor learning. FEBS J. 2022, 289, 2263–2281. [Google Scholar] [CrossRef] [PubMed]
- Shohamy, D. Learning and motivation in the human striatum. Curr. Opin. Neurobiol. 2011, 21, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Zhu, W.; Guo, Z.; Shu, G.; Cui, F.; Yang, F.; Zhang, Y.; Ren, Y.; Zhang, X.; Zhang, X.; et al. 18F-fallypride PET-CT of dopamine D2/D3 receptors in patients with sporadic amyotrophic lateral sclerosis. J. Neurol. Sci. 2017, 377, 79–84. [Google Scholar] [CrossRef]
- Zhang, C.; Li, J.; Li, D.; Sun, B. Deep brain stimulation removal after successful treatment for heroin addiction. Aust. N. Z. J. Psychiatry 2019, 54, 543–544. [Google Scholar] [CrossRef]
- Vassoler, F.M.; White, S.L.; Hopkins, T.J.; Guercio, L.A.; Espallergues, J.; Berton, O.; Schmidt, H.D.; Pierce, R.C. Deep brain stimulation of the nucleus accumbens shell attenuates cocaine reinstatement through Local and ANTIDROMIC activation. J. Neurosci. 2013, 33, 14446–14454. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guo, L.; Zhou, H.; Wang, R.; Xu, J.; Zhou, W.; Zhang, F.; Tang, S.; Liu, H.; Jiang, J. DBS of nucleus accumbens on heroin seeking behaviors in self-administering rats. Drug Alcohol Depend. 2013, 129, 70–81. [Google Scholar] [CrossRef]
- Zhu, Y.; Wang, K.; Ma, T.; Ji, Y.; Lou, Y.; Fu, X.; Lu, Y.; Liu, Y.; Dang, W.; Zhang, Q.; et al. Nucleus accumbens D1/D2 circuits control opioid withdrawal symptoms in mice. J. Clin. Investig. 2023, 133. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, H.; Jin, J.; Tang, J.; Sun, W.; Jia, H.; Yang, X.; Cui, J.; Wang, C. PRECLINICAL STUDY: Chronic deep brain stimulation in the rat nucleus accumbens and its effect on morphine reinforcement. Addict. Biol. 2008, 13, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Swinford-Jackson, S.E.; Huffman, P.J.; Knouse, M.C.; Thomas, A.S.; Rich, M.T.; Mankame, S.; Worobey, S.J.; Sarmiento, M.; Coleman, A.; Pierce, R.C. High frequency DBS-like optogenetic stimulation of nucleus accumbens dopamine D2 receptor-containing neurons attenuates cocaine reinstatement in male rats. Neuropsychopharmacology 2023, 48, 459–467. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vassoler, F.M.; Schmidt, H.D.; Gerard, M.E.; Famous, K.R.; Ciraulo, D.A.; Kornetsky, C.; Knapp, C.M.; Pierce, R.C. Deep brain stimulation of the nucleus accumbens shell attenuates cocaine priming-induced reinstatement of drug seeking in rats. J. Neurosci. 2008, 28, 8735–8739. [Google Scholar] [CrossRef] [PubMed]
- Müller, U.J.; Sturm, V.; Voges, J.; Heinze, H.-J.; Galazky, I.; Büntjen, L.; Heldmann, M.; Frodl, T.; Steiner, J.; Bogerts, B. Nucleus accumbens deep brain stimulation for alcohol addiction—safety and clinical long-term results of a pilot trial. Pharmacopsychiatry 2016, 49, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Henderson, M.B.; Green, A.I.; Bradford, P.S.; Chau, D.T.; Roberts, D.W.; Leiter, J.C. Deep brain stimulation of the nucleus accumbens reduces alcohol intake in alcohol-preferring rats. Neurosurg. Focus 2010, 29, E12. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.; Gründler, T.O.J.; Bauer, R.; Huff, W.; Fischer, A.G.; Lenartz, D.; Maarouf, M.; Bührle, C.; Klosterkötter, J.; Ullsperger, M.; et al. Successful deep brain stimulation of the nucleus accumbens in severe alcohol dependence is associated with changed performance monitoring. Addict. Biol. 2011, 16, 620–623. [Google Scholar] [CrossRef] [PubMed]
- Morita, H.; Hass, C.J.; Moro, E.; Sudhyadhom, A.; Kumar, R.; Okun, M.S. Pedunculopontine Nucleus Stimulation: Where are We Now and What Needs to be Done to Move the Field Forward? Front. Neurol. 2014, 5, 243. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thevathasan, W.; Moro, E. What is the therapeutic mechanism of pedunculopontine nucleus stimulation in Parkinson’s disease? Neurobiol. Dis. 2019, 128, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Thevathasan, W.; Cole, M.H.; Graepel, C.L.; Hyam, J.A.; Jenkinson, N.; Brittain, J.-S.; Coyne, T.J.; Silburn, P.A.; Aziz, T.Z.; Kerr, G.; et al. A spatiotemporal analysis of gait freezing and the impact of pedunculopontine nucleus stimulation. Brain 2012, 135 Pt 5, 1446–1454. [Google Scholar] [CrossRef] [PubMed]
- Dayal, V.; Rajabian, A.; Jahanshahi, M.; Aviles-Olmos, I.; Cowie, D.; Peters, A.; Day, B.; Hyam, J.; Akram, H.; Limousin, P.; et al. Pedunculopontine Nucleus Deep Brain Stimulation for Parkinsonian Disorders: A Case Series. Ster. Funct. Neurosurg. 2021, 99, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Benarroch, E.E. Pedunculopontine nucleus: Functional organization and clinical implications. Neurology 2013, 80, 1148–1155. [Google Scholar] [CrossRef] [PubMed]
- Doshi, P.K.; Desai, J.D.; Karkera, B.; Wadia, P.M. Bilateral pedunculopontine nucleus stimulation for progressive supranuclear palsy. Ster. Funct. Neurosurg. 2015, 93, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Javed, N.; Cascella, M. Neuroanatomy, Globus Pallidus. [Updated 2023 Feb 20]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024; Available online: https://www.ncbi.nlm.nih.gov/books/NBK557755/ (accessed on 12 April 2024).
- Meissner, W.; Paul, G.; Reum, T.; Reese, R.; Sohr, R.; Morgenstern, R.; Kupsch, A. The influence of pallidal deep brain stimulation on striatal dopaminergic metabolism in the rat. Neurosci. Lett. 2000, 296, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Wojtecki, L.; Groiss, S.J.; Ferrea, S.; Elben, S.; Hartmann, C.J.; Dunnett, S.B.; Rosser, A.; Saft, C.; Südmeyer, M.; Ohmann, C.; et al. A prospective pilot trial for pallidal deep brain stimulation in Huntington’s disease. Front. Neurol. 2015, 6, 177. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, V.; Cif, L.; Biolsi, B.; Garcia-Ptacek, S.; Seychelles, A.; Sanrey, E.; Descours, I.; Coubes, C.; de Moura, A.-M.R.; Corlobe, A.; et al. Deep brain stimulation for Huntington’s disease: Long-term results of a prospective open-label study. J. Neurosurg. 2014, 121, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Harrow-Mortelliti, M.; Reddy, V.; Jimsheleishvili, G. Physiology, Spinal Cord. [Updated 2023 Mar 17]. In StatPearls [Internet]; Treasure Island, FL, USA, January 2024; Available online: https://www.ncbi.nlm.nih.gov/books/NBK544267/ (accessed on 8 June 2024).
- Fuentes, R.; Petersson, P.; Siesser, W.B.; Caron, M.G.; Nicolelis, M.A.L. Spinal cord stimulation restores locomotion in animal models of Parkinson’s disease. Science 2009, 323, 1578–1582. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Santana, M.B.; Halje, P.; Simplício, H.; Richter, U.; Freire, M.A.M.; Petersson, P.; Fuentes, R.; Nicolelis, M.A. Spinal cord stimulation alleviates motor deficits in a primate model of Parkinson disease. Neuron 2014, 84, 716–722. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Andrade, E.M.; Ghilardi, M.G.; Cury, R.G.; Barbosa, E.R.; Fuentes, R.; Teixeira, M.J.; Fonoff, E.T. Spinal cord stimulation for Parkinson’s disease: A systematic review. Neurosurg. Rev. 2016, 39, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Fonoff, E.T.; de Lima-Pardini, A.C.; Coelho, D.B.; Monaco, B.A.; Machado, B.; de Souza, C.P.; Ghilardi, M.G.d.S.; Hamani, C. Spinal Cord Stimulation for Freezing of Gait: From Bench to Bedside. Front. Neurol. 2019, 10, 905. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lammel, S.; Lim, B.K.; Malenka, R.C. Reward and aversion in a heterogeneous midbrain dopamine system. Neuropharmacology 2014, 76 Pt B, 351–359. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Friedman, A.; Frankel, M.; Flaumenhaft, Y.; Merenlender, A.; Pinhasov, A.; Feder, Y.; Taler, M.; Gil-Ad, I.; Abeles, M.; Yadid, G. Programmed Acute Electrical Stimulation of Ventral Tegmental Area Alleviates Depressive-like Behavior. Neuropsychopharmacology 2009, 34, 1057–1066. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhang, L.; Meng, S.; Huang, E.; Di, T.; Ding, Z.; Huang, S.; Chen, W.; Zhang, J.; Zhao, S.; Yuwen, T.; et al. High frequency deep brain stimulation of the dorsal raphe nucleus prevents methamphetamine priming-induced reinstatement of drug seeking in rats. Transl. Psychiatry 2024, 14, 190. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yuen, J.; Goyal, A.; Rusheen, A.E.; Kouzani, A.Z.; Berk, M.; Kim, J.H.; Tye, S.J.; Blaha, C.D.; Bennet, K.E.; Lee, K.H.; et al. High frequency deep brain stimulation can mitigate the acute effects of cocaine administration on tonic dopamine levels in the rat nucleus accumbens. Front. Neurosci. 2023, 17, 1061578. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Minbashi Moeini, M.M.; Sadr, S.S.; Riahi, E. Deep Brain Stimulation of the Lateral Hypothalamus Facilitates Extinction and Prevents Reinstatement of Morphine Place Preference in Rats. Neuromodulation 2021, 24, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Davidson, B.; Vetkas, A.; Germann, J.; Tang-Wai, D.; Lozano, A.M. Deep brain stimulation for Alzheimer’s disease—Current status and next steps. Expert Rev. Med. Devices 2024, 21, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Yaseri, A.; Roozbeh, M.; Kazemi, R.; Lotfinia, S. Brain stimulation for patients with multiple sclerosis: An umbrella review of therapeutic efficacy. Neurol. Sci. 2024, 45, 2549–2559. [Google Scholar] [CrossRef] [PubMed]
- Emerich, D.F.; Thanos, C.G. Nanotechnology and medicine. Expert Opin. Biol. Ther. 2003, 3, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Sun, Y.; Xu, X. Nanoparticles as Drug Delivery Systems: A Review of the Implications of Nanoparticles’ Physicochemical Properties on Responses in Biological Systems. Polymers 2023, 15, 1596. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wu, B.M. Current Advances in Stimuli-Responsive Hydrogels as Smart Drug Delivery Carriers. Gels 2023, 9, 838. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kook, J.K.; Phung, V.-D.; Koh, D.-Y.; Lee, S.-W. Facile synthesis of boronic acid-functionalized magnetic nanoparticles for efficient dopamine extraction. Nano Converg. 2019, 6, 30. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Volov, A.; Shkodenko, L.; Koshel, E.; Drozdov, A.S. Bio-Inspired Surface Modification of Magnetite Nanoparticles with Dopamine Conjugates. Nanomaterials 2022, 12, 2230. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mayeen, A.; Kala, M.S.; Jayalakshmy, M.S.; Thomas, S.; Rouxel, D.; Philip, J.; Bhowmik, R.N.; Kalarikkal, N. Dopamine functionalization of BaTiO3: An effective strategy for the enhancement of electrical, magnetoelectric and thermal properties of BaTiO3-PVDF-TrFE nanocomposites. Dalton Trans. 2018, 47, 2039–2051. [Google Scholar] [CrossRef] [PubMed]
- Monge-Fuentes, V.; Mayer, A.B.; Lima, M.R.; Geraldes, L.R.; Zanotto, L.N.; Moreira, K.G.; Martins, O.P.; Piva, H.L.; Felipe, M.S.S.; Amaral, A.C.; et al. Dopamine-loaded nanoparticle systems circumvent the blood–brain barrier restoring motor function in mouse model for Parkinson’s Disease. Sci. Rep. 2021, 11, 15185. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alabrahim, O.A.A.; Azzazy, H.M.E.-S. Polymeric nanoparticles for dopamine and levodopa replacement in Parkinson’s disease. Nanoscale Adv. 2022, 4, 5233–5244. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morales, V.; McConnell, J.; Pérez-Garnes, M.; Almendro, N.; Sanz, R.; García-Muñoz, R.A. l-Dopa release from mesoporous silica nanoparticles engineered through the concept of drug-structure-directing agents for Parkinson’s disease. J. Mater. Chem. B 2021, 9, 4178–4189. [Google Scholar] [CrossRef] [PubMed]
- Arisoy, S.; Sayiner, O.; Comoglu, T.; Onal, D.; Atalay, O.; Pehlivanoglu, B. In vitro and in vivo evaluation of levodopa-loaded nanoparticles for nose to brain delivery. Pharm. Dev. Technol. 2020, 25, 735–747. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.H.; Mir, M.; Ngowi, E.E.; Zafar, U.; Khakwani, M.M.A.K.; Khattak, S.; Zhai, Y.-K.; Jiang, E.-S.; Zheng, M.; Duan, S.-F.; et al. Nanomedicine: A Promising Way to Manage Alzheimer’s Disease. Front. Bioeng. Biotechnol. 2021, 9, 630055. [Google Scholar] [CrossRef]
- Abd Elmonem, H.A.; Morsi, R.M.; Mansour, D.S.; El-Sayed, E.S.R. Myco-fabricated ZnO nanoparticles ameliorate neurotoxicity in mice model of Alzheimer’s disease via acetylcholinesterase inhibition and oxidative stress reduction. Biometals 2023, 36, 1391–1404. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.-H.; Tsai, P.-H.; Wang, K.-Y.; Wei, Y.-T.; Chiou, S.-H.; Mou, C.-Y. Generation of Functional Dopaminergic Neurons from Reprogramming Fibroblasts by Nonviral-based Mesoporous Silica Nanoparticles. Sci. Rep. 2018, 8, 11. [Google Scholar] [CrossRef]
- Neganova, M.E.; Aleksandrova, Y.R.; Sukocheva, O.A.; Klochkov, S.G. Benefits and limitations of nanomedicine treatment of brain cancers and age-dependent neurodegenerative disorders. Semin. Cancer Biol. 2022, 86 Pt 2, 805–833. [Google Scholar] [CrossRef]
- Waris, A.; Ali, A.; Khan, A.U.; Asim, M.; Zamel, D.; Fatima, K.; Raziq, A.; Khan, M.A.; Akbar, N.; Baset, A.; et al. Applications of Various Types of Nanomaterials for the Treatment of Neurological Disorders. Nanomaterials 2022, 12, 2140. [Google Scholar] [CrossRef] [PubMed]
- Yeon, P.; Bakir, M.S.; Ghovanloo, M. Towards a 1.1 mm2 free-floating wireless implantable neural recording SoC. In Proceedings of the 2018 IEEE Custom Integrated Circuits Conference (CICC), San Diego, CA, USA, 8–11 April 2018; pp. 1–4. [Google Scholar]
- Lee, S.; Cortese, A.J.; Gandhi, A.P.; Agger, E.R.; McEuen, P.L.; Molnar, A.C. A 250 μm × 57 μm microscale opto-electronically transduced electrodes (MOTEs) for neural recording. IEEE Trans. Biomed. Circuits Syst. 2018, 12, 1256–1266. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Cortese, A.J.; Trexel, P.; Agger, E.R.; McEuen, P.L.; Molnar, A.C. A 330 μm × 90 μm opto-electronically integrated wireless system-on-chip for recording of neural activities. In Proceedings of the 2018 IEEE International Solid-State Circuits Conference (ISSCC), San Francisco, CA, USA, 11–15 February 2018; pp. 292–294. [Google Scholar]
- Yue, K.; Guduru, R.; Hong, J.; Liang, P.; Nair, M.; Khizroev, S. Magneto-electric nano-particles for non-invasive brain stimulation. PLoS ONE 2012, 7, e44040. [Google Scholar] [CrossRef]
- Pardo, M.; Khizroev, S. Where Do We Stand Now Regarding Treatment of Psychiatric and Neurodegenerative Disorders? Considerations in Using Magnetoelectric Nanoparticles as an Innovative approach. WIREs Nanomed. Nanobiotechnol. 2022, 14, e1781. [Google Scholar] [CrossRef] [PubMed]
- Khizroev, S.; Liang, P. Engineering future medicines with magnetoelectric nanoparticles: Wirelessly controlled, targeted therapies. IEEE Nanotechnol. Mag. 2020, 14, 23–29. [Google Scholar] [CrossRef]
- Khizroev, S. Technobiology’s Enabler: The Magnetoelectric Nanoparticle. Cold Spring Harb. Perspect. Med. 2019, 9, a034207. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Apu, E.H.; Nafiujjaman, M.; Sandeep, S.; Makela, A.V.; Khaleghi, A.; Vainio, S.; Contag, C.H.; Li, J.; Balasingham, I.; Kim, T.; et al. Biomedical applications of multifunctional magnetoelectric nanoparticles. Mater. Chem. Front. 2022, 6, 1368–1390. [Google Scholar] [CrossRef]
- Kozielski, K.L.; Jahanshahi, A.; Gilbert, H.B.; Yu, Y.; Erin, Ö.; Francisco, D.; Alosaimi, F.; Temel, Y.; Sitti, M. Nonresonant powering of injectable nanoelectrodes enables wireless deep brain stimulation in freely moving mice. Sci. Adv. 2021, 7, eabc4189. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alosaimi, F.; Dominguez-Paredes, D.; Knoben, R.; Almasabi, F.; Hescham, S.; Kozielski, K.; Temel, Y.; Jahanshahi, A. Wireless stimulation of the subthalamic nucleus with nanoparticles modulates key monoaminergic systems similar to contemporary deep brain stimulation. Behav. Brain Res. 2023, 444, 114363. [Google Scholar] [CrossRef] [PubMed]
- Neudorfer, C.; Chow, C.T.; Boutet, A.; Loh, A.; Germann, J.; Elias, G.J.; Hutchison, W.D.; Lozano, A.M. Kilohertz-frequency stimulation of the nervous system: A review of underlying mechanisms. Brain Stimul. 2021, 14, 513–530. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Gao, J.; Wang, P.; Nagesetti, A.; Andrews, P.; Masood, S.; Vriesman, Z.; Liang, P.; Khizroev, S.; Jin, X. In Vivo Wireless Brain Stimulation via Non-invasive and Targeted Delivery of Magnetoelectric Nanoparticles. Neurotherapeutics 2021, 18, 2091–2106. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, E.; Abdel-Mottaleb, M.; Liang, P.; Navarrete, B.; Yildirim, Y.A.; Campos, M.A.; Smith, I.; Wang, P.; Yildirim, B.; Yang, L.; et al. Magnetic-field-synchronized wireless modulation of neural activity by magnetoelectric nanoparticles. Brain Stimul. 2022, 15, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wu, X.; Ding, J.; Su, B.; Chen, Z.; Xiao, Z.; Wu, C.; Wei, D.; Sun, J.; Luo, F.; et al. Wireless-Powering Deep Brain Stimulation Platform Based on 1D-Structured Magnetoelectric Nanochains Applied in Antiepilepsy Treatment. ACS Nano 2023, 17, 15796–15809. [Google Scholar] [CrossRef] [PubMed]
- Guduru, R.; Liang, P.; Hong, J.; Rodzinski, A.; Hadjikhani, A.; Horstmyer, J.; Levister, E.; Khizroev, S. Magnetoelectric ‘spin’ on stimulating the brain. Nanomedicine 2015, 10, 2051–2061. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaushik, A.K.; Rodriguez, J.; Rothen, D.; Bhardwaj, V.; Jayant, R.D.; Pattany, P.; Fuentes, B.; Chand, H.S.; Kolishetti, N.; El-Hage, N.; et al. MRI-Guided, Noninvasive Delivery of Magneto-Electric Drug Nanocarriers to the Brain in a Nonhuman Primate. ACS Appl. Bio Mater. 2019, 2, 4826–4836. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pardo, M.; Roberts, E.R.; Pimentel, K.; Yildirim, Y.A.; Navarrete, B.; Wang, P.; Zhang, E.; Liang, P.; Khizroev, S. Size-dependent intranasal administration of magnetoelectric nanoparticles for targeted brain localization. Nanomed. Nanotechnol. Biol. Med. 2020, 32, 102337. [Google Scholar] [CrossRef] [PubMed]
- Kaushik, A.; Jayant, R.D.; Nikkhah-Moshaie, R.; Bhardwaj, V.; Roy, U.; Huang, Z.; Ruiz, A.; Yndart, A.; Atluri, V.; El-Hage, N.; et al. Magnetically guided central nervous system delivery and toxicity evaluation of magneto-electric nanocarriers. Sci. Rep. 2016, 6, 25309. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hadjikhani, A.; Rodzinski, A.; Wang, P.; Nagesetti, A.; Guduru, R.; Liang, P.; Runowicz, C.; Shahbazmohamadi, S.; Khizroev, S. Biodistribution and clearance of magnetoelectric nanoparticles for nanomedical applications using energy dispersive spectroscopy. Nanomedicine 2017, 12, 1801–1822. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nair, M.; Guduru, R.; Liang, P.; Hong, J.; Sagar, V.; Khizroev, S. Externally controlled on-demand release of anti-HIV drug using magneto-electric nanoparticles as carriers. Nat. Commun. 2013, 4, 1707. [Google Scholar] [CrossRef] [PubMed]
- Stewart, T.S.; Nagesetti, A.; Guduru, R.; Liang, P.; Stimphil, E.; Hadjikhani, A.; Salgueiro, L.; Horstmyer, J.; Cai, R.; Schally, A.; et al. Magnetoelectric nanoparticles for delivery of antitumor peptides into glioblastoma cells by magnetic fields. Nanomedicine 2018, 13, 423–438. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shahzad, K.; Mushtaq, S.; Rizwan, M.; Khalid, W.; Atif, M.; Din, F.U.; Ahmad, N.; Abbasi, R.; Ali, Z. Field-controlled magnetoelectric core-shell CoFe2O4@BaTiO3 nanoparticles as effective drug carriers and drug release in vitro. Mater. Sci. Eng. C 2020, 119, 111444. [Google Scholar] [CrossRef] [PubMed]
- Waters, M.; Hopf, J.; Tam, E.; Wallace, S.; Chang, J.; Bennett, Z.; Aquino, H.; Roeder, R.K.; Helquist, P.; Stack, M.S.; et al. Biocompatible, Multi-Mode, Fluorescent, T2 MRI Contrast Magnetoelectric-Silica Nanoparticles (MagSiNs), for On-Demand Doxorubicin Delivery to Metastatic Cancer Cells. Pharmaceuticals 2022, 15, 1216. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mathiopoulou, V.; Lofredi, R.; Feldmann, L.K.; Habets, J.; Darcy, N.; Neumann, W.-J.; Faust, K.; Schneider, G.-H.; Kühn, A.A. Modulation of subthalamic beta oscillations by movement, dopamine, and deep brain stimulation in Parkinson’s disease. Npj Park. Dis. 2024, 10, 77. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giménez, S.; Millan, A.; Mora-Morell, A.; Ayuso, N.; Gastaldo-Jordán, I.; Pardo, M. Advances in Brain Stimulation, Nanomedicine and the Use of Magnetoelectric Nanoparticles: Dopaminergic Alterations and Their Role in Neurodegeneration and Drug Addiction. Molecules 2024, 29, 3580. https://doi.org/10.3390/molecules29153580
Giménez S, Millan A, Mora-Morell A, Ayuso N, Gastaldo-Jordán I, Pardo M. Advances in Brain Stimulation, Nanomedicine and the Use of Magnetoelectric Nanoparticles: Dopaminergic Alterations and Their Role in Neurodegeneration and Drug Addiction. Molecules. 2024; 29(15):3580. https://doi.org/10.3390/molecules29153580
Chicago/Turabian StyleGiménez, Silvia, Alexandra Millan, Alba Mora-Morell, Noa Ayuso, Isis Gastaldo-Jordán, and Marta Pardo. 2024. "Advances in Brain Stimulation, Nanomedicine and the Use of Magnetoelectric Nanoparticles: Dopaminergic Alterations and Their Role in Neurodegeneration and Drug Addiction" Molecules 29, no. 15: 3580. https://doi.org/10.3390/molecules29153580
APA StyleGiménez, S., Millan, A., Mora-Morell, A., Ayuso, N., Gastaldo-Jordán, I., & Pardo, M. (2024). Advances in Brain Stimulation, Nanomedicine and the Use of Magnetoelectric Nanoparticles: Dopaminergic Alterations and Their Role in Neurodegeneration and Drug Addiction. Molecules, 29(15), 3580. https://doi.org/10.3390/molecules29153580





