Nanomedicines for Dry Eye Syndrome: Targeting Oxidative Stress with Modern Nanomaterial Strategies
Abstract
:1. Introduction
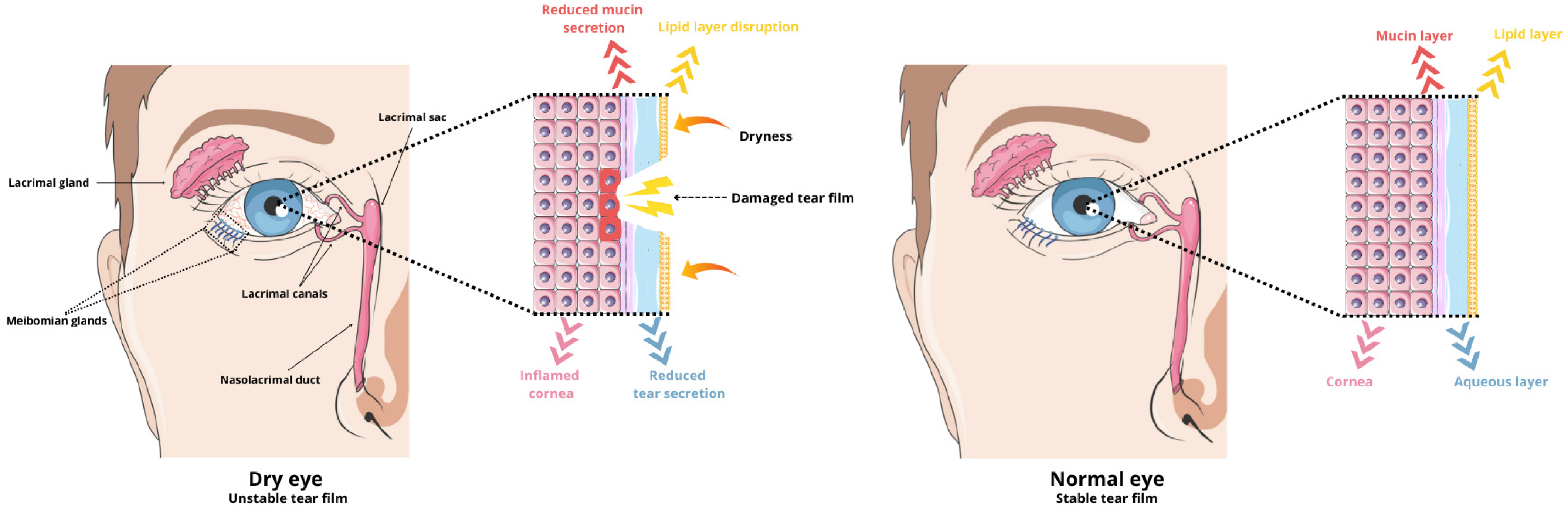
2. Common Causes and Pathophysiology of Dry Eye Syndrome
3. Oxidative Stress
3.1. Oxidative Stress Classification
3.2. Role of Oxidative Stress in the Development of Dry Eye Disease
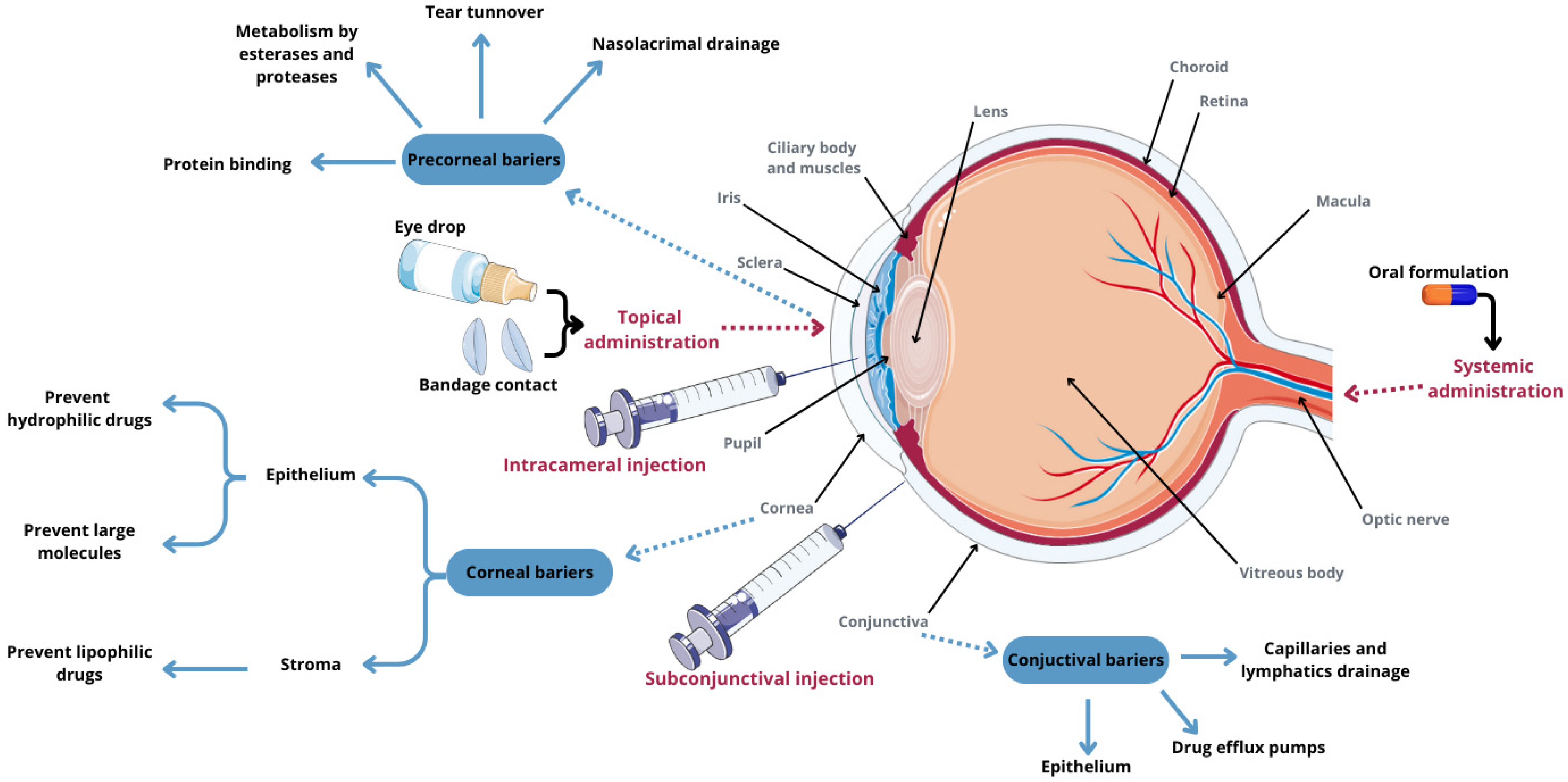
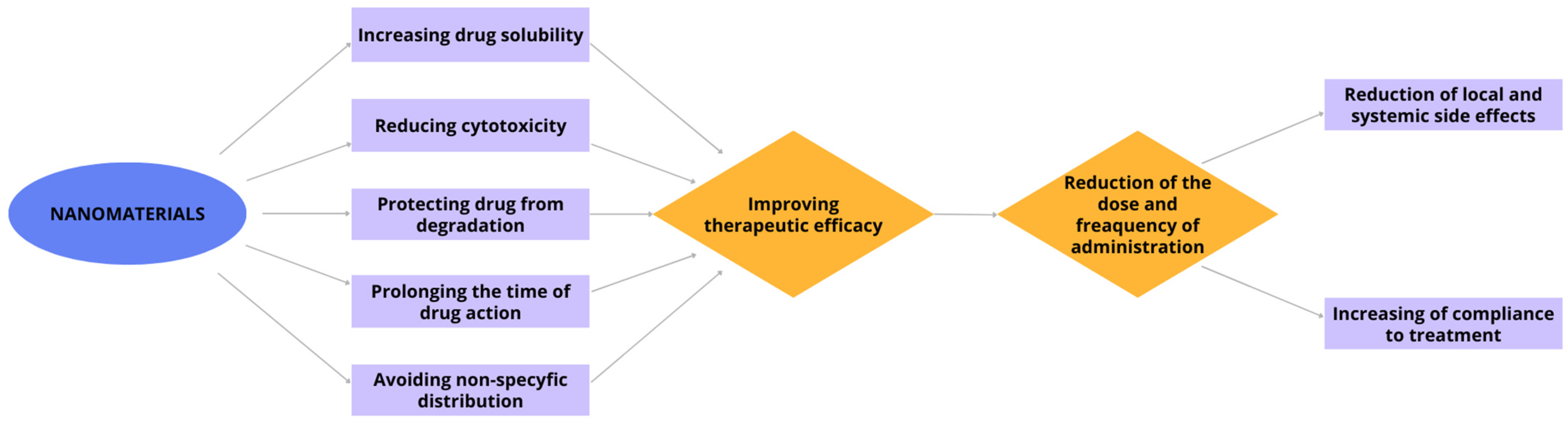
4. Nanomaterials and Drug Delivery to the Eye
4.1. Polymer Nanomaterials
4.1.1. Polymeric Nanoparticles
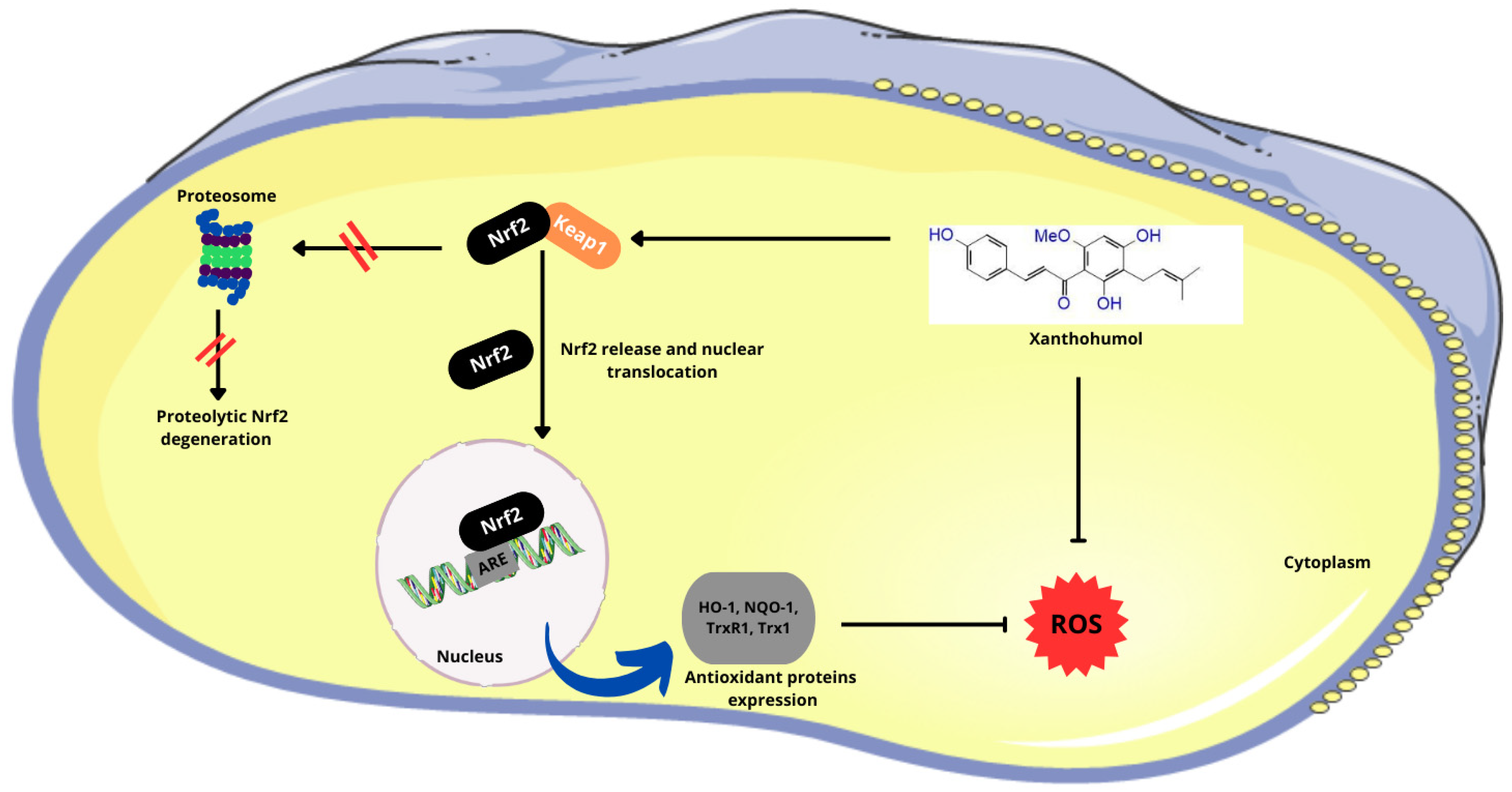
Poly(Lactic and Co-Glycolic Acid) Nanoparticles (PLGA NP) Encapsulating Xanthohumol
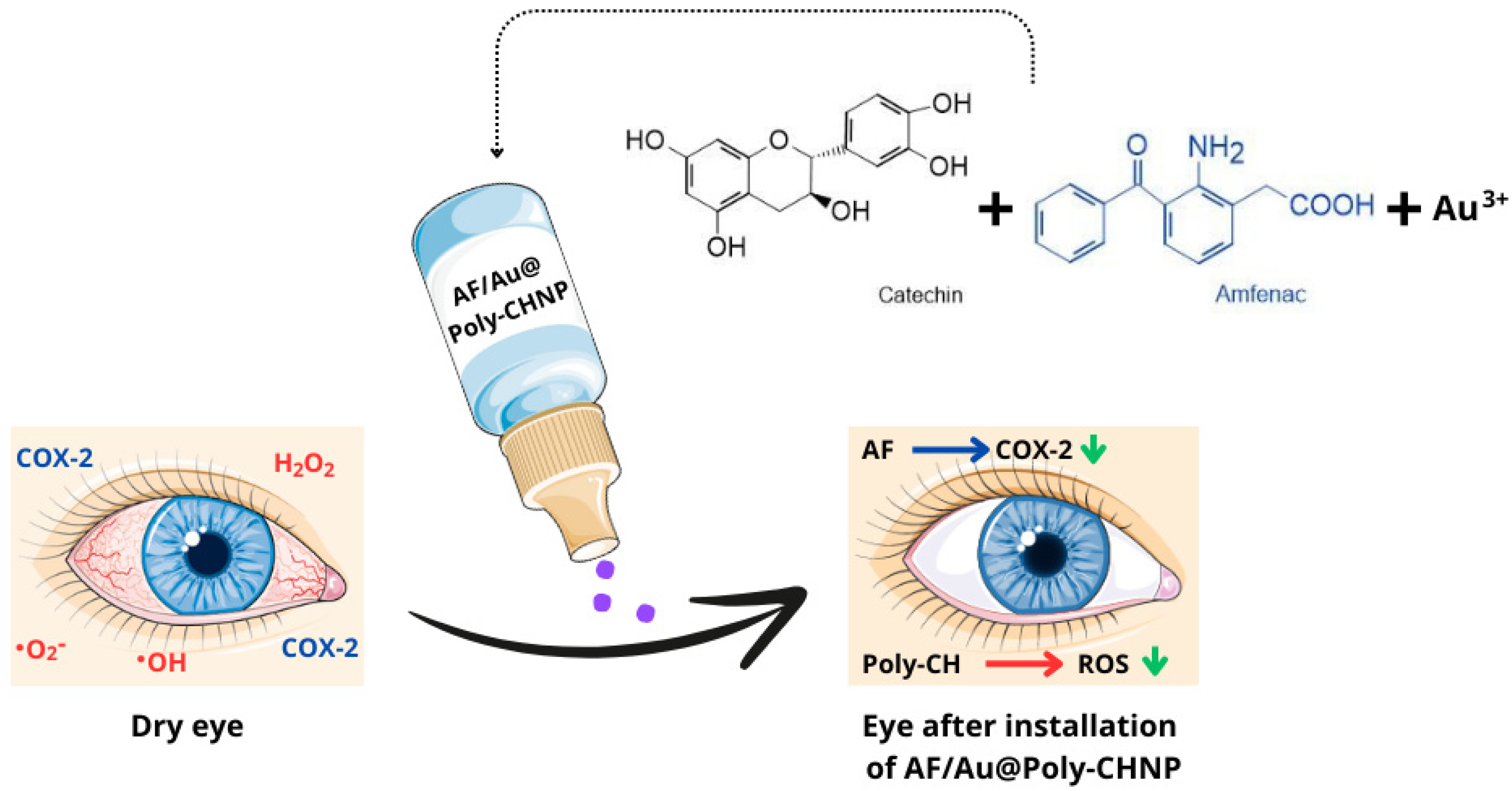
Poly(Catechin) Capped-Gold Nanoparticles (Au@Poly-CHNPs) Carrying Amfenac [AF; A Nonsteroidal Anti-Inflammatory Drug (NSAID)]
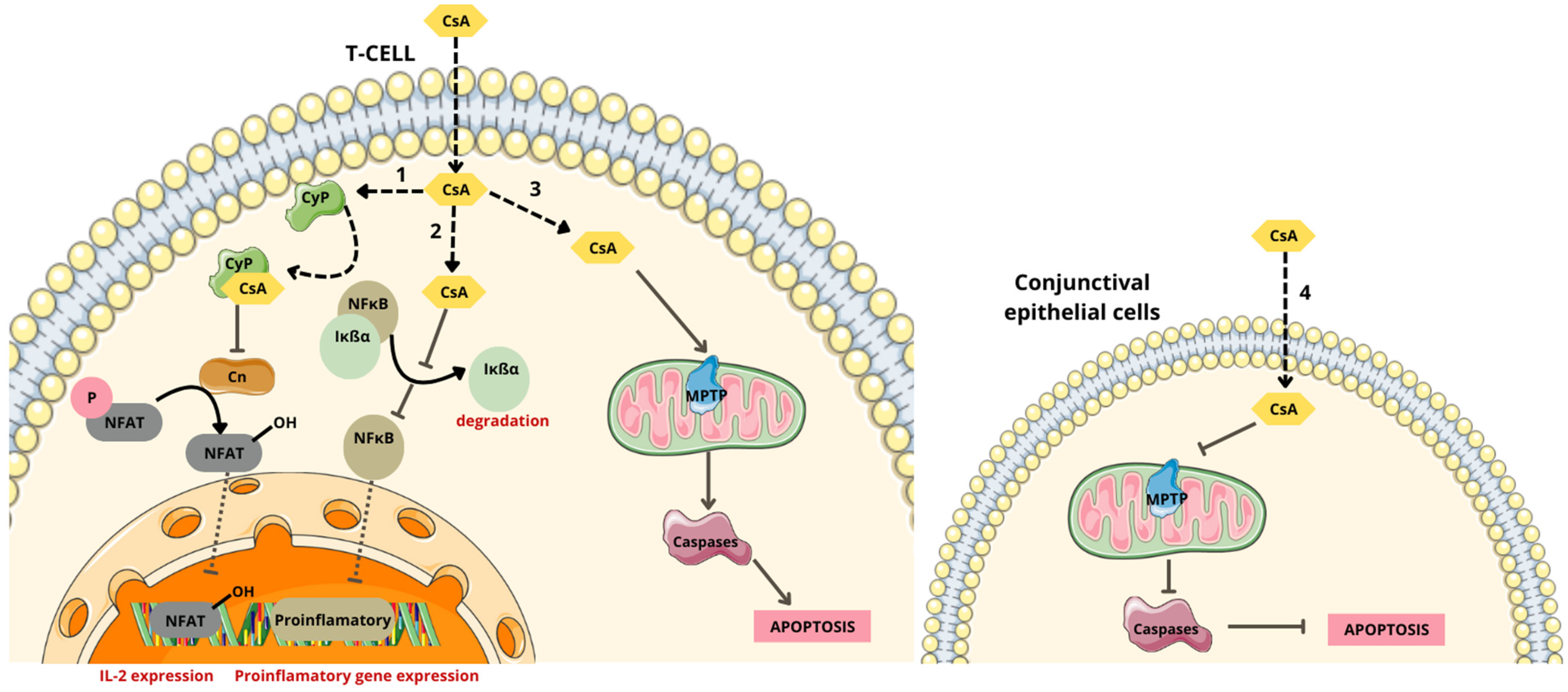
PLGA Nanoparticles Loaded with Cyclosporine A (CsA) and Cyclosporine A Lipid Nanocapsules (CsA-LNC)
Polyglycolic Acid-Loaded Tetrandrine Nanoparticles
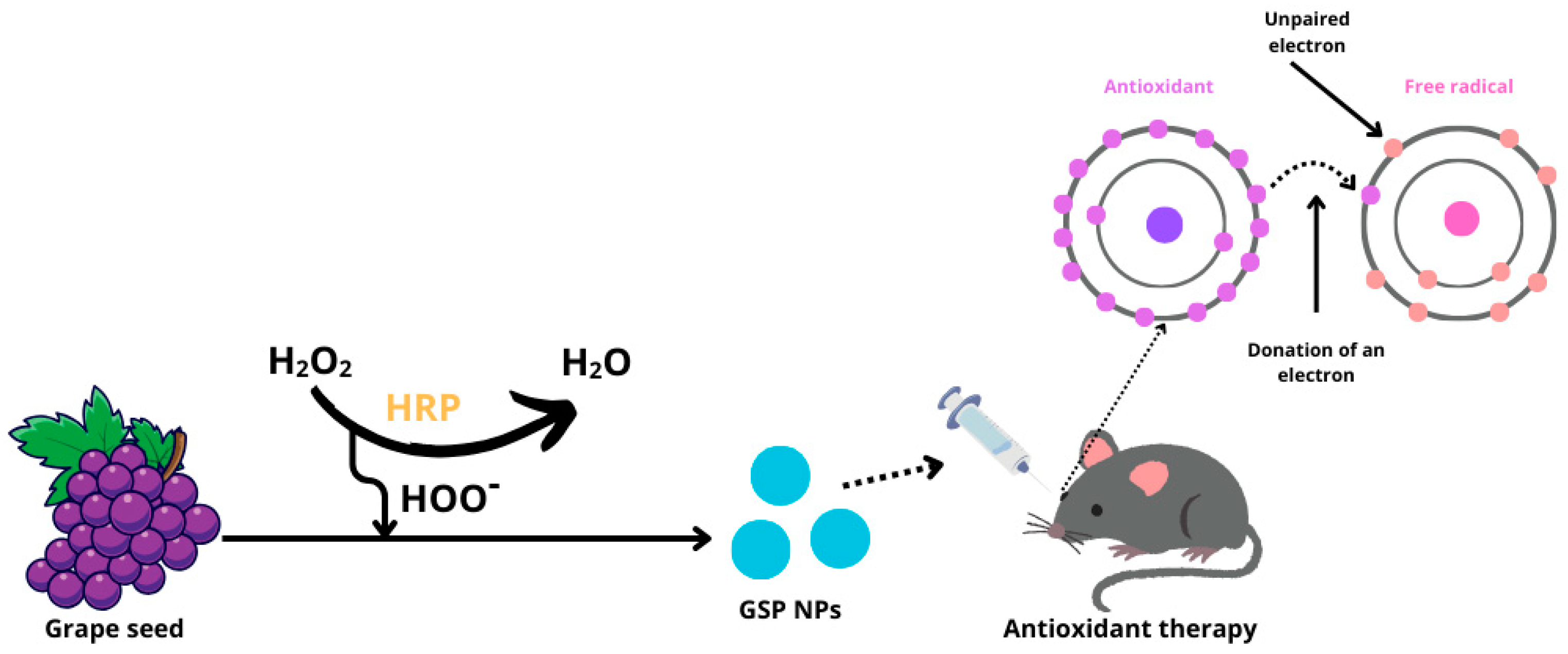
Grape Seed Nanochats
Gelatin-Based Nanoparticles
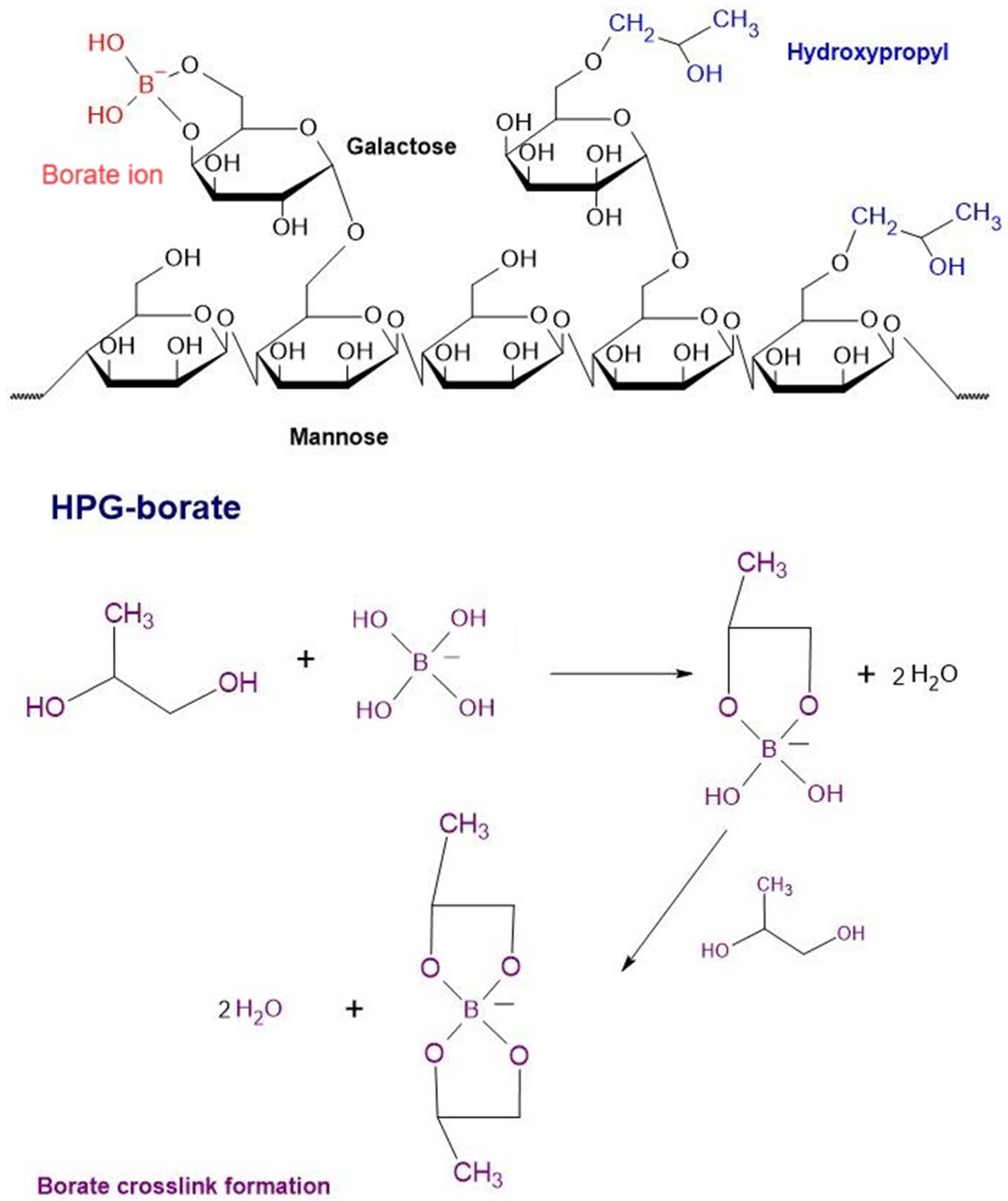
4.1.2. Hydrogels
Soft Hydrogel Based on Hyaluronic Acid
Thermosensitive Hydrogels
Reactive Oxygen Species-Scavenging Hydrogels
Lysine-Carbonized Mucoadhesive Nanogels
4.1.3. Nanoemulsions
Cyclosporine A Nanoemulsion
Nanoemulsion of Propylene Glycol and Hydroxypropyl Guar (PG-HPG)
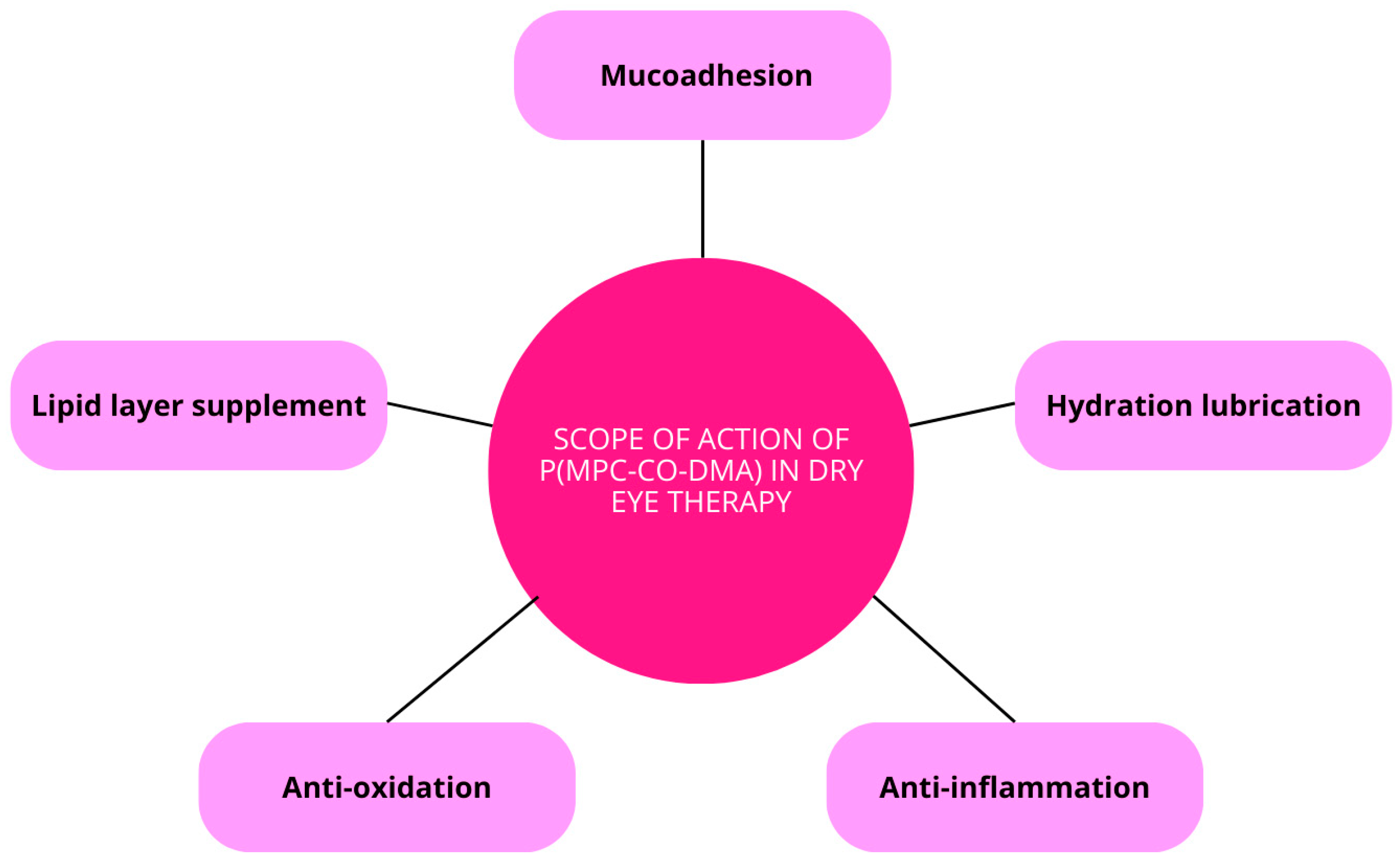
4.1.4. Nanopreparation: Polyphosphobetaine Functionalized with p(MPC-Co-DMA) Catechols
4.1.5. Carbohydrate-Based Nanomaterials (Charged Polysaccharides—Glycosaminoglycans)
Hyaluronic Acid
4.1.6. Metallic and Non-Metallic Nanomaterials
Selenium and Copper
Cerium Oxide
5. Therapeutic Contact Lenses to Remove Excess Reactive Oxygen Species from the Surface of the Eye
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rolando, M.; Barabino, S. Dry Eye Disease: What Is the Role of Vitamin D? Int. J. Mol. Sci. 2023, 24, 1458. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Pflugfelder, S.C.; Liu, Z.; Baudouin, C.; Kim, H.M.; Messmer, E.M.; Kruse, F.; Liang, L.; Carreno-Galeano, J.T.; Rolando, M.; et al. Defining Dry Eye from a Clinical Perspective. Int. J. Mol. Sci. 2020, 21, 9271. [Google Scholar] [CrossRef]
- Aljeaidi, M.; Keen, C.; Bell, J.S.; Cooper, T.; Robson, L.; Tan, E.C.K. Dry Eyes, Ocular Lubricants, and Use of Systemic Medications Known or Suspected to Cause Dry Eyes in Residents of Aged Care Services. Int. J. Environ. Res. Public Health 2020, 17, 5349. [Google Scholar] [CrossRef] [PubMed]
- Kassumeh, S.; Priglinger, S.G.; Messmer, E.M. Volkskrankheit: Das Trockene Auge. MMW Fortschr. Med. 2022, 164, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Su, C.; Fang, L.; Lu, J.; Chen, J.; Ding, Y. Dry eye syndrome: Comprehensive etiologies and recent clinical trials. Int. Ophthalmol. 2022, 42, 3253–3272. [Google Scholar] [CrossRef]
- Zhang, J.; Lin, H.; Li, F.; Wu, K.; Yang, S.; Zhou, S. Involvement of endoplasmic reticulum stress in trigeminal ganglion corneal neuron injury in dry eye disease. Front. Mol. Neurosci. 2023, 16, 1083850. [Google Scholar] [CrossRef]
- Grassiri, B.; Zambito, Y.; Bernkop-Schnürch, A. Strategies to prolong the residence time of drug delivery systems on ocular surface. Adv. Colloid Interface Sci. 2021, 288, 102342. [Google Scholar] [CrossRef]
- Jumelle, C.; Gholizadeh, S.; Annabi, N.; Dana, R. Advances and limitations of drug delivery systems formulated as eye drops. J. Control Release 2020, 321, 1–22. [Google Scholar] [CrossRef]
- Subrizi, A.; del Amo, E.M.; Korzhikov-Vlakh, V.; Tennikova, T.; Ruponen, M.; Urtti, A. Design principles of ocular drug delivery systems: Importance of drug payload, release rate, and material properties. Drug Discov. Today 2019, 24, 1446–1457. [Google Scholar] [CrossRef]
- De Matteis, V.; Rizzello, L. Noble Metals and Soft Bio-Inspired Nanoparticles in Retinal Diseases Treatment: A Perspective. Cells 2020, 9, 679. [Google Scholar] [CrossRef]
- Zhang, Y.; Tang, H.; Chen, W.; Zhang, J. Nanomaterials Used in Fluorescence Polarization Based Biosensors. Int. J. Mol. Sci. 2022, 23, 8625. [Google Scholar] [CrossRef]
- Fadeel, B. Nanomaterial characterization: Understanding nano-bio interactions. Biochem. Biophys. Res. Commun. 2022, 633, 45–51. [Google Scholar] [CrossRef]
- Moon, J.; Choi, S.H.; Yoon, C.H.; Kim, M.K. Gut dysbiosis is prevailing in Sjögren’s syndrome and is related to dry eye severity. PLoS ONE 2020, 15, e0229029. [Google Scholar] [CrossRef]
- Tsigalou, C.; Stavropoulou, E.; Bezirtzoglou, E. Current Insights in Microbiome Shifts in Sjogren’s Syndrome and Possible Therapeutic Interventions. Front. Immunol. 2018, 9, 1106. [Google Scholar] [CrossRef]
- Truong, S.; Cole, N.; Stapleton, F.; Golebiowski, B. Sex hormones and the dry eye. Clin. Exp. Optom. 2014, 97, 324–336. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Lambert, R.W.; Wickham, L.A.; Banting, G.; Sullivan, D.A. Androgen control of secretory component mRNA levels in the rat lacrimal gland. J. Steroid Biochem. Mol. Biol. 1995, 52, 239–249. [Google Scholar] [CrossRef]
- Mendoza-Santiesteban, C.E.; Hedges, T.R.; Norcliffe-Kaufmann, L.; Warren, F.; Reddy, S.; Axelrod, F.B.; Kaufmann, H. Clinical Neuro-ophthalmic Findings in Familial Dysautonomia. J. Neuroophthalmol. 2012, 32, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Gorimanipalli, B.; Khamar, P.; Sethu, S.; Shetty, R. Hormones and dry eye disease. Indian. J. Ophthalmol. 2023, 71, 1276–1284. [Google Scholar] [CrossRef]
- Moon, J.; Yoon, C.H.; Choi, S.H.; Kim, M.K. Can Gut Microbiota Affect Dry Eye Syndrome? Int. J. Mol. Sci. 2020, 21, 8443. [Google Scholar] [CrossRef] [PubMed]
- Trujillo-Vargas, C.M.; Schaefer, L.; Alam, J.; Pflugfelder, S.C.; Britton, R.A.; de Paiva, C.S. The Gut-Eye-Lacrimal Gland-Microbiome Axis in Sjögren Syndrome. Ocul. Surf. 2020, 18, 335–344. [Google Scholar] [CrossRef]
- Srivastava, A.; Makarenkova, H.P. Innate Immunity and Biological Therapies for the Treatment of Sjögren’s Syndrome. Int. J. Mol. Sci. 2020, 21, 9172. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.Y.; Lee, A.; Ge, S.; Nathan, S.; Knox, S.M.; McNamara, N.A. Aire-deficient mice provide a model of corneal and lacrimal gland neuropathy in Sjögren’s syndrome. PLoS ONE 2017, 12, e0184916. [Google Scholar] [CrossRef] [PubMed]
- Staaf, S.; Oerther, S.; Lucas, G.; Mattsson, J.P.; Ernfors, P. Differential regulation of TRP channels in a rat model of neuropathic pain. Pain 2009, 144, 187. [Google Scholar] [CrossRef] [PubMed]
- Andersen, H.H.; Yosipovitch, G.; Galor, A. Neuropathic Symptoms of the Ocular Surface: Dryness, Pain, and Itch. Curr. Opin. Allergy Clin. Immunol. 2017, 17, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Vazirani, J.; Sridhar, U.; Gokhale, N.; Doddigarla, V.R.; Sharma, S.; Basu, S. Autologous serum eye drops in dry eye disease: Preferred practice pattern guidelines. Indian J. Ophthalmol. 2023, 71, 1357. [Google Scholar] [CrossRef] [PubMed]
- Shoari, A.; Kanavi, M.R.; Rasaee, M.J. Inhibition of matrix metalloproteinase-9 for the treatment of dry eye syndrome; a review study. Exp. Eye Res. 2021, 205, 108523. [Google Scholar] [CrossRef] [PubMed]
- Kaur, K.; Stokkermans, T.J. Meibomian Gland Disease. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2024. [Google Scholar]
- Mohamed, H.; El-Hamid, B.; Fathalla, D.; Fouad, E. Current trends in pharmaceutical treatment of Dry Eye Disease: A review. Eur. J. Pharm. Sci. 2022, 175, 106206. [Google Scholar] [CrossRef] [PubMed]
- Lushchak, V.I. Interplay between bioenergetics and oxidative stress at normal brain aging. Aging as a result of increasing disbalance in the system oxidative stress–energy provision. Pflug. Arch.—Eur. J. Physiol. 2021, 473, 713–722. [Google Scholar] [CrossRef] [PubMed]
- Perez-Garmendia, R.; Lopez de Eguileta Rodriguez, A.; Ramos-Martinez, I.; Zuñiga, N.M.; Gonzalez-Salinas, R.; Quiroz-Mercado, H.; Zenteno, E.; Hernández, E.R.; Hernández-Zimbrón, L.F. Interplay between Oxidative Stress, Inflammation, and Amyloidosis in the Anterior Segment of the Eye; Its Pathological Implications. Oxid. Med. Cell. Longev. 2020, 2020, 6286105. [Google Scholar] [CrossRef] [PubMed]
- Wishart, T.F.L.; Flokis, M.; Shu, D.Y.; Das, S.J.; Lovicu, F.J. Hallmarks of lens aging and cataractogenesis. Exp. Eye Res. 2021, 210, 108709. [Google Scholar] [CrossRef]
- Sheppard, J.D.; Nichols, K.K. Dry Eye Disease Associated with Meibomian Gland Dysfunction: Focus on Tear Film Characteristics and the Therapeutic Landscape. Ophthalmol. Ther. 2023, 12, 1397–1418. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.Y.; Purt, B. Biochemistry, Tear Film. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2024. [Google Scholar]
- Butovich, I.A. Cholesteryl esters as a depot for very long chain fatty acids in human meibum. J. Lipid Res. 2009, 50, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Khanal, S.; Bai, Y.; Ngo, W.; Nichols, K.K.; Wilson, L.; Barnes, S.; Nichols, J.J. Human meibum and tear film derived cholesteryl and wax esters in meibomian gland dysfunction and tear film structure. Ocul. Surf. 2022, 23, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Yancey, P.H. Organic osmolytes as compatible, metabolic and counteracting cytoprotectants in high osmolarity and other stresses. J. Exp. Biol. 2005, 208, 2819–2830. [Google Scholar] [CrossRef] [PubMed]
- Dammak, A.; Pastrana, C.; Martin-Gil, A.; Carpena-Torres, C.; Cerda, A.P.; Simovart, M.; Alarma, P.; Huete-Toral, F.; Carracedo, G. Oxidative Stress in the Anterior Ocular Diseases: Diagnostic and Treatment. Biomedicines 2023, 11, 292. [Google Scholar] [CrossRef]
- Jîtcă, G.; Ősz, B.E.; Tero-Vescan, A.; Miklos, A.P.; Rusz, C.-M.; Bătrînu, M.-G.; Vari, C.E. Positive Aspects of Oxidative Stress at Different Levels of the Human Body: A Review. Antioxidants 2022, 11, 572. [Google Scholar] [CrossRef]
- Lei, L.; Mu, J.; Zheng, Y.; Liu, Y. Selenium Deficiency-Induced Oxidative Stress Causes Myocardial Injury in Calves by Activating Inflammation, Apoptosis, and Necroptosis. Antioxidants 2023, 12, 229. [Google Scholar] [CrossRef]
- Lushchak, V.I.; Storey, K.B. Oxidative stress concept updated: Definitions, classifications, and regulatory pathways implicated. EXCLI J. 2021, 20, 956. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zheng, Y. Oxidative stress and antioxidants in the trabecular meshwork. PeerJ 2019, 7, e8121. [Google Scholar] [CrossRef]
- Su, L.J.; Zhang, J.H.; Gomez, H.; Murugan, R.; Hong, X.; Xu, D.; Jiang, F.; Peng, Z.-Y. Reactive Oxygen Species-Induced Lipid Peroxidation in Apoptosis, Autophagy, and Ferroptosis. Oxid. Med. Cell. Longev. 2019, 2019, 5080843. [Google Scholar] [CrossRef]
- Zeng, X.; Li, J.; Yang, F.; Xia, R. The effect of narcotics on ferroptosis-related molecular mechanisms and signalling pathways. Front. Pharmacol. 2022, 13, 1020447. [Google Scholar] [CrossRef]
- Hsueh, Y.J.; Chen, Y.N.; Tsao, Y.T.; Cheng, C.M.; Wu, W.C.; Chen, H.C. The Pathomechanism, Antioxidant Biomarkers, and Treatment of Oxidative Stress-Related Eye Diseases. Int. J. Mol. Sci. 2022, 23, 1255. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Amin, M.M.; Sayed, S. Ocular Drug Delivery: A Comprehensive Review. AAPS PharmSciTech 2023, 24, 66. [Google Scholar] [CrossRef]
- Vision Impairment and Blindness. Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 31 July 2024).
- Vaneev, A.; Tikhomirova, V.; Chesnokova, N.; Popova, E.; Beznos, O.; Kost, O.; Klyachko, N. Nanotechnology for Topical Drug Delivery to the Anterior Segment of the Eye. Int. J. Mol. Sci. 2021, 22, 12368. [Google Scholar] [CrossRef]
- Chen, L.; Wu, F.; Pang, Y.; Yan, D.; Zhang, S.; Chen, F.; Wu, N.; Gong, D.; Liu, J.; Fu, Y.; et al. Therapeutic nanocoating of ocular surface. Nano Today 2021, 41, 101309. [Google Scholar] [CrossRef]
- Gorantla, S.; Rapalli, V.K.; Waghule, T.; Singh, P.P.; Dubey, S.K.; Saha, R.N.; Singhvi, G. Nanocarriers for ocular drug delivery: Current status and translational opportunity. RSC Adv. 2020, 10, 27835–27855. [Google Scholar] [CrossRef]
- Wei, J.; Mu, J.; Tang, Y.; Qin, D.; Duan, J.; Wu, A. Next-generation nanomaterials: Advancing ocular anti-inflammatory drug therapy. J. Nanobiotechnol. 2023, 21, 282. [Google Scholar] [CrossRef] [PubMed]
- Joshi, V.P.; Singh, S.; Thacker, M.; Pati, F.; Vemuganti, G.K.; Basu, S.; Singh, V. Newer approaches to dry eye therapy: Nanotechnology, regenerative medicine, and tissue engineering. Indian J. Ophthalmol. 2023, 71, 1292. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.K.; Thapa, R.; Hariani, H.N.; Volyanyuk, M.; Ogle, S.D.; Orloff, K.A.; Ankireddy, S.; Lai, K.; Žiniauskaitė, A.; Stubbs, E.B.; et al. Poly(lactic-co-glycolic acid) Nanoparticles Encapsulating the Prenylated Flavonoid, Xanthohumol, Protect Corneal Epithelial Cells from Dry Eye Disease-Associated Oxidative Stress. Pharmaceutics 2021, 13, 1362. [Google Scholar] [CrossRef]
- Yao, J.; Zhang, B.; Ge, C.; Peng, S.; Fang, J. Xanthohumol, a Polyphenol Chalcone Present in Hops, Activating Nrf2 Enzymes To Confer Protection against Oxidative Damage in PC12 Cells. J. Agric. Food Chem. 2015, 63, 1521–1531. [Google Scholar] [CrossRef]
- Zhang, Y. Nanomaterial-Mediated Drug Delivery in Eye Diseases; Scientific Research Publishing, Inc.: Irvine, CA, USA, 2023. [Google Scholar]
- Rodrigues, E.B.; Farah, M.E.; Bottós, J.M.; Aggio, F.B. CHAPTER 29—Nonsteroidal anti-inflammatory drugs (NSAIDs) in the treatment of retinal diseases. In Retinal Pharmacotherapy; Nguyen, Q.D., Rodrigues, E.B., Farah, M.E., Mieler, W.F., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2010; pp. 196–200. [Google Scholar] [CrossRef]
- Li, Y.J.; Luo, L.J.; Harroun, S.G.; Wei, S.-C.; Unnikrishnan, B.; Chang, H.-T.; Huang, Y.-F.; Lai, J.-Y.; Huang, C.-C. Synergistically dual-functional nano eye-drops for simultaneous anti-inflammatory and anti-oxidative treatment of dry eye disease. Nanoscale 2019, 11, 5580–5594. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Cai, S.; Wu, H.; Pan, J.; Su, M.; Wei, X.; Ye, J.; Ke, L.; Liu, G.; Chu, C. Revolutionizing eye care: The game-changing applications of nano-antioxidants in ophthalmology. Nanoscale 2024, 16, 7307–7322. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Kim, M.K.; Kim, E.C.; Kim, J.Y.; Kim, T.-I.; Kim, H.K.; Song, J.S.; Yoon, K.-C.; Lee, D.H.; Lee, H.K.; et al. Efficacy of Topical Cyclosporine Nanoemulsion 0.05% Compared with Topical Cyclosporine Emulsion 0.05% and Diquafosol 3% in Dry Eye. Korean J. Ophthalmol. 2019, 33, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Zhao, X.; Jin, H.; Jia, F.; Jiang, L.; Li, Z. A randomized controlled trial involving college student: Comparing 0.15% hyaluronic acid with 0.05% cyclosporine A and 3% diquafosol sodium in the Treatment of Dry Eye. Medicine 2023, 102, e34923. [Google Scholar] [CrossRef] [PubMed]
- Schultz, C. Safety and Efficacy of Cyclosporine in the Treatment of Chronic Dry Eye. Ophthalmol. Eye Dis. 2014, 6, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Jerkins, G.; Pattar, G.; Kannarr, S. A Review of Topical Cyclosporine A Formulations—A Disease-Modifying Agent for Keratoconjunctivitis Sicca. Clin. Ophthalmol. 2020, 14, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Periman, L.M.; Mah, F.S.; Karpecki, P.M. A Review of the Mechanism of Action of Cyclosporine A: The Role of Cyclosporine A in Dry Eye Disease and Recent Formulation Developments. Clin. Ophthalmol. 2020, 14, 4187–4200. [Google Scholar] [CrossRef]
- Wagh, V.D.; Apar, D.U. Cyclosporine A Loaded PLGA Nanoparticles for Dry Eye Disease: In Vitro Characterization Studies. J. Nanotechnol. 2014, 2014, e683153. [Google Scholar] [CrossRef]
- Zhang, A.; Sun, R.; Ran, M.; Deng, Y.; Ge, Y.; Zhu, Y.; Tao, X.; Shang, L.; Gou, J.; He, H.; et al. A Novel Eyes Topical Drug Delivery System: CsA-LNC for the Treatment of DED. Pharm. Res. 2020, 37, 146. [Google Scholar] [CrossRef]
- Ferreiro, D.U.; Komives, E.A. Molecular Mechanisms of System Control of NF-κB Signaling by IκBα. Biochemistry 2010, 49, 1560–1567. [Google Scholar] [CrossRef]
- Que, X.; Su, J.; Guo, P.; Kamal, Z.; Xu, E.; Liu, S.; Chen, J.; Qiu, M. Study on preparation, characterization and multidrug resistance reversal of red blood cell membrane-camouflaged tetrandrine-loaded PLGA nanoparticles. Drug Deliv. 2019, 26, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Radwan, S.E.S.; El-Moslemany, R.M.; Mehanna, R.A.; Thabet, E.H.; Abdelfattah, E.Z.A.; El-Kamel, A. Chitosan-coated bovine serum albumin nanoparticles for topical tetrandrine delivery in glaucoma: In Vitro and in vivo assessment. Drug Deliv. 2022, 29, 1150–1163. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Tang, J.; Wu, X.; Zhang, Y.; Du, Y.; Fang, Q.; Li, J.; Du, Z. Evaluating the Efficacy of Polyglycolic Acid-Loading Tetrandrine Nanoparticles in the Treatment of Dry Eye. Ophthalmic Res. 2023, 66, 1148–1158. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Yokoi, N.; Watanabe, H.; Dogru, M.; Kojima, T.; Yamada, M.; Kinoshita, S.; Kim, H.-M.; Tchah, H.-W.; Hyon, J.Y.; et al. A New Perspective on Dry Eye Classification: Proposal by the Asia Dry Eye Society. Eye Contact Lens 2020, 46, S2–S13. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Fan, Q.; Hong, J.; Chen, Z.; Zhou, X.; Zhang, J.; Dai, Y.; Jiang, H.; Gu, Z.; Cheng, Y.; et al. Therapeutic Nanoparticles from Grape Seed for Modulating Oxidative Stress. Small 2021, 17, 2102485. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Sang, H.; Wang, Y.; Zhu, F.; Hu, X.; Wang, X.; Wang, X.; Li, Y.; Cheng, Y. Foe to Friend: Supramolecular Nanomedicines Consisting of Natural Polyphenols and Bortezomib. Nano Lett. 2018, 18, 7045–7051. [Google Scholar] [CrossRef]
- Favero, G.; Moretti, E.; Krajčíková, K.; Tomečková, V.; Rezzani, R. Evidence of Polyphenols Efficacy against Dry Eye Disease. Antioxidants 2021, 10, 190. [Google Scholar] [CrossRef]
- Bielory, L.; Tabliago, N.R.A. Flavonoid and cannabinoid impact on the ocular surface. Curr. Opin. Allergy Clin. Immunol. 2020, 20, 482. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Z.; Yang, P.; Duan, G.; Liu, X.; Gu, Z.; Li, Y. Polyphenol scaffolds in tissue engineering. Mater. Horiz. 2021, 8, 145–167. [Google Scholar] [CrossRef]
- Hathout, R.M.; Omran, M.K. Gelatin-based particulate systems in ocular drug delivery. Pharm. Dev. Technol. 2016, 21, 379–386. [Google Scholar] [CrossRef]
- Milano, F.; Masi, A.; Madaghiele, M.; Sannino, A.; Salvatore, L.; Gallo, N. Current Trends in Gelatin-Based Drug Delivery Systems. Pharmaceutics 2023, 15, 1499. [Google Scholar] [CrossRef] [PubMed]
- Weiss, A.V.; Fischer, T.; Iturri, J.; Benitez, R.; Toca-Herrera, J.L.; Schneider, M. Mechanical properties of gelatin nanoparticles in dependency of crosslinking time and storage. Colloids Surf. B Biointerfaces 2019, 175, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Naskar, S.; Sharma, S.; Kuotsu, K. A smart gelatin nanoparticle for delivery of metoprolol succinate: A strategy for enhancing the therapeutic efficacy by improving bioavailability. J. Drug Deliv. Sci. Technol. 2019, 53, 101214. [Google Scholar] [CrossRef]
- Loepfe, M.; Duss, A.; Zafeiropoulou, K.A.; Björgvinsdóttir, O.; D’este, M.; Eglin, D.; Fortunato, G.; Klasen, J.; Ferguson, S.J.; Wuertz-Kozak, K.; et al. Electrospray-Based Microencapsulation of Epigallocatechin 3-Gallate for Local Delivery into the Intervertebral Disc. Pharmaceutics 2019, 11, 435. [Google Scholar] [CrossRef]
- de Carvalho, S.Y.B.; Almeida, R.R.; Pinto, N.A.R.; de Mayrinck, C.; Vieira, S.S.; Haddad, J.F.; Leitão, A.A.; Guimarães, L.G.d.L. Encapsulation of essential oils using cinnamic acid grafted chitosan nanogel: Preparation, characterization and antifungal activity. Int. J. Biol. Macromol. 2021, 166, 902–912. [Google Scholar] [CrossRef]
- Yu, D.; Wang, X.; Li, D.; Zhang, X.; Yu, C.; Pei, X.; Cheng, J.; Wang, L. A Novel Cinnamic Acid-Based Organogel: Effect of Oil Type on Physical Characteristics and Crystallization Kinetics. Eur. J. Lipid Sci. Technol. 2020, 122, 1800488. [Google Scholar] [CrossRef]
- Kuthati, Y.; Busa, P.; Tummala, S.; Rao, V.N.; Davuluri, V.N.G.; Ho, Y.-P.; Wong, C.-S. Mesoporous Polydopamine Nanoparticles Attenuate Morphine Tolerance in Neuropathic Pain Rats by Inhibition of Oxidative Stress and Restoration of the Endogenous Antioxidant System. Antioxidants 2021, 10, 195. [Google Scholar] [CrossRef]
- Zhong, G.; Yang, X.; Jiang, X.; Kumar, A.; Long, H.; Xie, J.; Zheng, L.; Zhao, J. Dopamine-melanin nanoparticles scavenge reactive oxygen and nitrogen species and activate autophagy for osteoarthritis therapy. Nanoscale 2019, 11, 11605–11616. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.C.; Lin, Y.K.; Lin, Y.T.; Lin, C.; Lan, G.; Su, Y.; Hu, F.; Chang, K.; Chen, V.; Yeh, Y.; et al. Injectable, Antioxidative, and Tissue-Adhesive Nanocomposite Hydrogel as a Potential Treatment for Inner Retina Injuries. Adv. Sci. 2024, 11, 2308635. [Google Scholar] [CrossRef]
- Li, Q.; Cao, Y.; Wang, P. Recent Advances in Hydrogels for the Diagnosis and Treatment of Dry Eye Disease. Gels 2022, 8, 816. [Google Scholar] [CrossRef]
- Kim, Y.E.; Kim, J. ROS-Scavenging Therapeutic Hydrogels for Modulation of the Inflammatory Response. ACS Appl. Mater. Interfaces 2022, 14, 23002–23021. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.C.; Chang, C.C.; Chan, H.P.; Chung, T.-W.; Shu, C.-W.; Chuang, K.-P.; Duh, T.-H.; Yang, M.-H.; Tyan, Y.-C. Hydrogels: Properties and Applications in Biomedicine. Molecules 2022, 27, 2902. [Google Scholar] [CrossRef] [PubMed]
- Romano, V.; Romano, D.; Semeraro, P.; Forbice, E.; Iaria, A.; Pizzolante, T.; Frassi, M.; Franceschini, F.; Semeraro, F. Therapeutic Hyper-CL soft contact lens in Sjögren’s syndrome. Am. J. Ophthalmol. Case Rep. 2022, 28, 101685. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Chow, D.W.Y.; Lau, C.M.L.; Zhou, G.; Back, W.; Xu, J.; Carim, S.; Chau, Y. A bioinspired synthetic soft hydrogel for the treatment of dry eye. Bioeng. Transl. Med. 2021, 6, e10227. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.L.; Mann, B.K. Efficacy of a Crosslinked Hyaluronic Acid-Based Hydrogel as a Tear Film Supplement: A Masked Controlled Study. PLoS ONE 2014, 9, e99766. [Google Scholar] [CrossRef]
- Williams, D.L.; Mann, B.K. A Crosslinked HA-Based Hydrogel Ameliorates Dry Eye Symptoms in Dogs. Int. J. Biomater. 2013, 2013, 460437. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Liu, Y.; Fu, W.; Yao, M.; Ding, Z.; Xuan, J.; Li, D.; Wang, S.; Xia, Y.; Cao, M. Poly(N-isopropylacrylamide)-Based Thermoresponsive Composite Hydrogels for Biomedical Applications. Polymers 2020, 12, 580. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Luo, M.; Huang, B.; Gao, W.; Jiang, Y.; Li, Q.; Nan, K.; Lin, S. Localized co-delivery of CNTF and FK506 using a thermosensitive hydrogel for retina ganglion cells protection after traumatic optic nerve injury. Drug Deliv. 2020, 27, 556–564. [Google Scholar] [CrossRef] [PubMed]
- Asfour, M.H.; Abd El-Alim, S.H.; Awad, G.E.A.; Kassem, A.A. Chitosan/β-glycerophosphate in situ forming thermo-sensitive hydrogel for improved ocular delivery of moxifloxacin hydrochloride. Eur. J. Pharm. Sci. 2021, 167, 106041. [Google Scholar] [CrossRef]
- Laradji, A.; Shui, Y.B.; Karakocak, B.B.; Evans, L.; Hamilton, P.; Ravi, N. Bioinspired Thermosensitive Hydrogel as a Vitreous Substitute: Synthesis, Properties, and Progress of Animal Studies. Materials 2020, 13, 1337. [Google Scholar] [CrossRef]
- Choi, S.W.; Cha, B.G.; Kim, J. Therapeutic Contact Lens for Scavenging Excessive Reactive Oxygen Species on the Ocular Surface. ACS Nano 2020, 14, 2483–2496. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zheng, H.; Zhou, L.; Cheng, F.; Liu, Z.; Zhang, H.; Zhang, Q. Injectable redox and light responsive MnO2 hybrid hydrogel for simultaneous melanoma therapy and multidrug-resistant bacteria-infected wound healing. Biomaterials 2020, 260, 120314. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Chen, Z.; Bai, J.; Li, X.; Chen, X.; Li, Z.; Pan, H.; Li, S.; Gao, Q.; Zhao, N.; et al. Multifunctional Hydrogel Eye Drops for Synergistic Treatment of Ocular Inflammatory Disease. ACS Nano 2023, 17, 25377–25390. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, C.A.; Ni, D.; Rosenkrans, Z.T.; Cai, W. Scavenging of reactive oxygen and nitrogen species with nanomaterials. Nano Res. 2018, 11, 4955–4984. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Suo, H.; Xie, Y.; Wang, K.; Wang, H.; Hou, Z.; Gao, Y.; Zhang, L.; Tao, J.; Jiang, H.; et al. Dopamine-Substituted Multidomain Peptide Hydrogel with Inherent Antimicrobial Activity and Antioxidant Capability for Infected Wound Healing. ACS Appl. Mater. Interfaces 2021, 13, 29380–29391. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wu, H.; Guo, B.; Dong, R.; Qiu, Y.; Ma, P.X. Antibacterial anti-oxidant electroactive injectable hydrogel as self-healing wound dressing with hemostasis and adhesiveness for cutaneous wound healing. Biomaterials 2017, 122, 34–47. [Google Scholar] [CrossRef] [PubMed]
- Utech, S.; Boccaccini, A.R. A review of hydrogel-based composites for biomedical applications: Enhancement of hydrogel properties by addition of rigid inorganic fillers. J. Mater. Sci. 2016, 51, 271–310. [Google Scholar] [CrossRef]
- Lin, P.H.; Jian, H.J.; Li, Y.J.; Huang, Y.-F.; Anand, A.; Huang, C.-C.; Lin, H.-J.; Lai, J.-Y. Alleviation of dry eye syndrome with one dose of antioxidant, anti-inflammatory, and mucoadhesive lysine-carbonized nanogels. Acta Biomater. 2022, 141, 140–150. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Zhou, B.; Chen, H.; Lu, K.; Wang, Y. Oxidative stress activates the Nrf2-mediated antioxidant response and P38 MAPK pathway: A possible apoptotic mechanism induced by BDE-47 in rainbow trout (Oncorhynchus mykiss) gonadal RTG-2 cells. Environ. Pollut. 2021, 287, 117341. [Google Scholar] [CrossRef]
- Huang, D.; Maulu, S.; Ren, M.; Liang, H.; Ge, X.; Ji, K.; Yu, H. Dietary Lysine Levels Improved Antioxidant Capacity and Immunity via the TOR and p38 MAPK Signaling Pathways in Grass Carp, Ctenopharyngodon idellus Fry. Front. Immunol. 2021, 12, 635015. [Google Scholar] [CrossRef]
- Dehvari, K.; Chiu, S.H.; Lin, J.S.; Girma, W.M.; Ling, Y.C.; Chang, J.Y. Heteroatom doped carbon dots with nanoenzyme like properties as theranostic platforms for free radical scavenging, imaging, and chemotherapy. Acta Biomater. 2020, 114, 343–357. [Google Scholar] [CrossRef] [PubMed]
- Ji, Z.; Sheardy, A.; Zeng, Z.; Zhang, W.; Chevva, H.; Allado, K.; Yin, Z.; Wei, J. Tuning the Functional Groups on Carbon Nanodots and Antioxidant Studies. Molecules 2019, 24, 152. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Tan, X.; Wang, Y.; Shen, B.; Yang, Y.; Huang, H. Heteroatom-doped nanozyme progress and perspectives: From synthesis strategies to biomedical applications. Chem. Eng. J. 2023, 468, 143703. [Google Scholar] [CrossRef]
- Lin, H.-Y.; Wang, S.-W.; Mao, J.-Y.; Chang, H.-T.; Harroun, S.G.; Lin, H.-J.; Huang, C.-C.; Lai, J.-Y. Carbonized nanogels for simultaneous antibacterial and antioxidant treatment of bacterial keratitis. Chem. Eng. J. 2021, 411, 128469. [Google Scholar] [CrossRef]
- Chávez-Hurtado, P.; Pesqueda-Pinedo, L.; Ceballos-Delgadillo, H.A.; Liñán-Segura, A.; Figueroa-Ponce, H.; Quintana-Hau, J.D. Physicochemical characterization of a DMPC-based nanoemulsion for dry eye and compatibility test with soft contact lenses in vitro. Contact Lens Anterior Eye 2022, 45, 101428. [Google Scholar] [CrossRef] [PubMed]
- Hadipour Jahromy, M.; Qomi, M.; Fazelipour, S.; Sami, N.; Faali, F.; Karimi, M.; Moghadam, F.A. Evaluation of curcumin-based ophthalmic nano-emulsion on atropine-induced dry eye in mice. Heliyon 2024, 10, e29009. [Google Scholar] [CrossRef] [PubMed]
- Coco, G.; Buffon, G.; Taloni, A.; Giannaccare, G. Recent Advances in Nanotechnology for the Treatment of Dry Eye Disease. Nanomaterials 2024, 14, 669. [Google Scholar] [CrossRef] [PubMed]
- Bang, S.P.; Yeon, C.Y.; Adhikari, N.; Neupane, S.; Kim, H.; Lee, D.C.; Son, M.J.; Lee, H.G.; Kim, J.-Y.; Jun, J.H. Cyclosporine A eyedrops with self-nanoemulsifying drug delivery systems have improved physicochemical properties and efficacy against dry eye disease in a murine dry eye model. PLoS ONE 2019, 14, e0224805. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.J.; Lee, J.E.; Lee, J.S. Clinical efficacy of 0.05% cyclosporine nano-emulsion in the treatment of dry eye syndrome associated with meibomian gland dysfunction. Int. J. Ophthalmol. 2022, 15, 1924–1931. [Google Scholar] [CrossRef]
- Choi, Y.S.; Paik, H.J.; Kim, D.H. Comparison of Consecutive Therapeutic Effects of Nanoemulsion and Emulsion Cyclosporin in Dry Eye Patients after Short-Term Treatment with Topical Fluorometholone. J. Ophthalmol. 2022, 2022, 6037401. [Google Scholar] [CrossRef]
- Garofalo, R.; Kunnen, C.; Rangarajan, R.; Manoj, V.; Ketelson, H. Relieving the symptoms of dry eye disease: Update on lubricating eye drops containing hydroxypropyl-guar. Clin. Exp. Optom. 2021, 104, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Silverstein, S.; Yeu, E.; Tauber, J.; Guillon, M.; Jones, L.; Galarreta, D.; Srinivasan, S.; Manoj, V. Symptom Relief Following a Single Dose of Propylene Glycol-Hydroxypropyl Guar Nanoemulsion in Patients with Dry Eye Disease: A Phase, IV, Multicenter Trial. Clin. Ophthalmol. 2020, 14, 3167–3177. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; Manoj, V. A Decade of Effective Dry Eye Disease Management with Systane Ultra (Polyethylene Glycol/Propylene Glycol with Hydroxypropyl Guar) Lubricant Eye Drops. Clin. Ophthalmol. 2021, 15, 2421–2435. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; Williams, R. Propylene Glycol and Hydroxypropyl Guar Nanoemulsion—Safe and Effective Lubricant Eye Drops in the Management of Dry Eye Disease. Clin. Ophthalmol. 2022, 16, 3311–3326. [Google Scholar] [CrossRef] [PubMed]
- Bickle, K.; Miller, J.R.; Tauber, J.; Awisi-Gyau, D. Multi-symptom Relief with Propylene Glycol-Hydroxypropyl-Guar Nanoemulsion Lubricant Eye Drops in Subjects with Dry Eye Disease: A Post-Marketing Prospective Study. Ophthalmol. Ther. 2024, 13, 481–494. [Google Scholar] [CrossRef] [PubMed]
- Bui, H.L.; Su, Y.H.; Yang, C.J.; Huang, C.J.; Lai, J.Y. Mucoadhesive, antioxidant, and lubricant catechol-functionalized poly(phosphobetaine) as biomaterial nanotherapeutics for treating ocular dryness. J. Nanobiotechnol. 2024, 22, 160. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Wang, H.; Han, Y.; Wang, H.; Sun, Y.; Zhang, H. Dopamine/Phosphorylcholine Copolymer as an Efficient Joint Lubricant and ROS Scavenger for the Treatment of Osteoarthritis. ACS Appl. Mater. Interfaces 2020, 12, 51236–51248. [Google Scholar] [CrossRef] [PubMed]
- Erfani, A.; Seaberg, J.; Aichele, C.P.; Ramsey, J.D. Interactions between Biomolecules and Zwitterionic Moieties: A Review. Biomacromolecules 2020, 21, 2557–2573. [Google Scholar] [CrossRef]
- Ishihara, K. Revolutionary advances in 2-methacryloyloxyethyl phosphorylcholine polymers as biomaterials. J. Biomed. Mater. Res. Part A 2019, 107, 933–943. [Google Scholar] [CrossRef]
- Iwasaki, Y.; Ishihara, K. Phosphorylcholine-containing polymers for biomedical applications. Anal. Bioanal. Chem. 2005, 381, 534–546. [Google Scholar] [CrossRef]
- Mosaiab, T.; Farr, D.C.; Kiefel, M.J.; Houston, T.A. Carbohydrate-based nanocarriers and their application to target macrophages and deliver antimicrobial agents. Adv. Drug Deliv. Rev. 2019, 151–152, 94–129. [Google Scholar] [CrossRef] [PubMed]
- Gim, S.; Zhu, Y.; Seeberger, P.H.; Delbianco, M. Carbohydrate-based nanomaterials for biomedical applications. WIREs Nanomed. Nanobiotechnol. 2019, 11, e1558. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front. Vet. Sci. 2019, 6, 192. [Google Scholar] [CrossRef] [PubMed]
- Laihia, J.; Järvinen, R.; Wylęgała, E.; Kaarniranta, K. Disease aetiology-based design of multifunctional microemulsion eye drops for moderate or severe dry eye: A randomized, quadruple-masked and active-controlled clinical trial. Acta Ophthalmol. 2020, 98, 244–254. [Google Scholar] [CrossRef] [PubMed]
- Marinho, A.; Nunes, C.; Reis, S. Hyaluronic Acid: A Key Ingredient in the Therapy of Inflammation. Biomolecules 2021, 11, 1518. [Google Scholar] [CrossRef] [PubMed]
- Hynnekleiv, L.; Magno, M.; Vernhardsdottir, R.R.; Moschowits, E.; Tønseth, K.A.; Dartt, D.A.; Vehof, J.; Utheim, T.P. Hyaluronic acid in the treatment of dry eye disease. Acta Ophthalmol. 2022, 100, 844–860. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Yu, C.; Dong, H.; Mu, Y.; Zhang, R.; Zhang, Q.; Liang, W.; Li, W.; Wang, X.; Zhang, L. Recent Developments About the Pathogenesis of Dry Eye Disease: Based on Immune Inflammatory Mechanisms. Front. Pharmacol. 2021, 12, 732887. [Google Scholar] [CrossRef]
- Zheng, Q.; Li, L.; Liu, M.; Huang, B.; Zhang, N.; Mehmood, R.; Nan, K.; Li, Q.; Chen, W.; Lin, S. In situ scavenging of mitochondrial ROS by anti-oxidative MitoQ/hyaluronic acid nanoparticles for environment-induced dry eye disease therapy. Chem. Eng. J. 2020, 398, 125621. [Google Scholar] [CrossRef]
- Huang, H.Y.; Wang, M.C.; Chen, Z.Y.; Chiu, W.Y.; Chen, K.H.; Lin, I.C.; Yang, W.C.V.; Wu, C.C.; Tseng, C.L. Gelatin–epigallocatechin gallate nanoparticles with hyaluronic acid decoration as eye drops can treat rabbit dry-eye syndrome effectively via inflammatory relief. Int. J. Nanomed. 2018, 13, 7251–7273. [Google Scholar] [CrossRef]
- Khiev, D.; Mohamed, Z.A.; Vichare, R.; Paulson, R.; Bhatia, S.; Mohapatra, S.; Lobo, G.P.; Valapala, M.; Kerur, N.; Passaglia, C.L.; et al. Emerging Nano-Formulations and Nanomedicines Applications for Ocular Drug Delivery. Nanomaterials 2021, 11, 173. [Google Scholar] [CrossRef]
- Au, A.; Mojadadi, A.; Shao, J.Y.; Ahmad, G.; Witting, P.K. Physiological Benefits of Novel Selenium Delivery via Nanoparticles. Int. J. Mol. Sci. 2023, 24, 6068. [Google Scholar] [CrossRef] [PubMed]
- Varlamova, E.G.; Turovsky, E.A.; Blinova, E.V. Therapeutic Potential and Main Methods of Obtaining Selenium Nanoparticles. Int. J. Mol. Sci. 2021, 22, 10808. [Google Scholar] [CrossRef] [PubMed]
- Ou, L.; Wu, Z.; Hu, X.; Huang, J.; Yi, Z.; Gong, Z.; Li, H.; Peng, K.; Shu, C.; Koole, L.H. A tissue-adhesive F127 hydrogel delivers antioxidative copper-selenide nanoparticles for the treatment of dry eye disease. Acta Biomater. 2024, 175, 353–368. [Google Scholar] [CrossRef] [PubMed]
- Woźniak-Budych, M.J.; Staszak, K.; Staszak, M. Copper and Copper-Based Nanoparticles in Medicine—Perspectives and Challenges. Molecules 2023, 28, 6687. [Google Scholar] [CrossRef] [PubMed]
- Zou, H.; Wang, H.; Xu, B.; Liang, L.; Shen, L.; Lin, Q. Regenerative cerium oxide nanozymes alleviate oxidative stress for efficient dry eye disease treatment. Regen. Biomater. 2022, 9, rbac070. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Zheng, M.; Zhang, A.Y.; Han, Z. A cerium oxide loaded glycol chitosan nano-system for the treatment of dry eye disease. J. Control Release 2019, 315, 40–54. [Google Scholar] [CrossRef] [PubMed]
- Alrobaian, M. Pegylated nanoceria: A versatile nanomaterial for noninvasive treatment of retinal diseases. Saudi Pharm. J. 2023, 31, 101761. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Zhang, Y.; Zhao, J.; Luan, F.; Wang, Y.; Lai, F.; Ouyang, D.; Tao, Y. Combining MSC Exosomes and Cerium Oxide Nanocrystals for Enhanced Dry Eye Syndrome Therapy. Pharmaceutics 2023, 15, 2301. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.W.; Kim, J. Therapeutic Contact Lenses with Polymeric Vehicles for Ocular Drug Delivery: A Review. Materials 2018, 11, 1125. [Google Scholar] [CrossRef]
- Naqvi, S.T.R.; Shirinfar, B.; Majeed, S.; Najam-Ul-Haq, M.; Hussain, D.; Iqbal, T.; Ahmed, N. Synthesis, design and sensing applications of nanostructured ceria-based materials. Analyst 2018, 143, 5610–5628. [Google Scholar] [CrossRef]

| Etiology | How It Leads to DES | References |
|---|---|---|
| Hormonal imbalance | Androgens have been demonstrated to regulate the lacrimal glands’ fluid and protein secretion by steroid-specific receptors in epithelial cells. The effect of the lack of androgens is dysfunction of the lacrimal glands and deficiency of tears. | [15,16,17,18] |
| Gut dysbiosis | Gut dysbiosis stimulates the migration of CD103 or CXCR1 dendritic cells, or monocytes/macrophages, to the surface of the eye. This contributes to the activation of T lymphocytes to secrete pro-inflammatory cytokines on the surface of the eye and lacrimal glands. | [19,20] |
| Autoimmunity | Activated CD8 T cells are associated with the death of lacrimal gland epithelial cells, reducing tear production. CD4 T cells, as the main immune effectors, interact with macrophages, causing inflammation and peripheral neuropathy of the lacrimal glands. | [21,22] |
| Nerve damage | Nerve damage causes a decrease in the sensitivity threshold of sensory neurons or their excessive excitation. This is related to malfunctioning ion channels affecting the generation and propagation of action potentials. | [23,24] |
| Type of Layer | Composition | Function |
|---|---|---|
| Lipid layer (outer layer) | Non-polar wax esters (25.2%, e.g., fatty esters, fatty alcohols), phospholipids (4.5%), fatty acids (3.5%), and cholesterol (free and esters 66.8%) | Delaying the evaporation of tears Uniform distribution of the tear film Maintaining a smooth eye surface |
| Aqueous layer (middle layer) | Proteins (lysozyme, lactoferrin), metabolites (includes peptides, lipids, amino acids, nucleic acids, carbohydrates, vitamins), inorganic salts (NaCl), glucose, oxygen, and electrolytes (magnesium, bicarbonate, calcium, urea) | Flushing out impurities and toxins Moisturizing and protecting the surface of the eye Calcium ions are essential for cell adhesion, aiding in the stabilization and integrity of the ocular surface by facilitating cell-to-cell and cell-to-matrix interactions. Magnesium ions, meanwhile, act as coenzymes in various protective processes on the eye surface, including stabilization of cellular membranes and modulation of oxidative stress responses. |
| Mucin layer (inner layer) | Immunoglobulins, urea, inorganic salts, glucose, and proteins | Ensuring even lubrication of the eye Lowering surface tension and increasing the stability of the tear film |
| Intensity Classification | Characteristics |
|---|---|
| Basal oxidative stress | Very low intensity of oxidative stress |
| No apparent symptoms Oxidative–redox homeostasis | |
| Low-intensity oxidative stress | Slight increase in the level of ROS modifiable molecules |
| Increased activity of antioxidant enzymes | |
| Strong oxidative stress | Disturbed balance between oxidants and antioxidants |
| Significant predominance of oxidants | |
| Very strong oxidative stress | Maximum level of modifiable ROS particles |
| Minimal activity of antioxidant enzymes |
| Time-Course Classification | Characteristics |
| Acute oxidative stress | Short-term increase in ROS levels, with change of conditions (e.g., use of an oxidative stress inducer) |
| Highly effective antioxidant defense, restoring homeostasis Presumed lack of stimulation of the expression of ROS-neutralizing genes | |
| Chronic oxidative stress | Long-term elevated levels of ROS, with change in conditions (e.g., use of an oxidative stress inducer) |
| Strong stimulation of the expression of ROS-neutralizing genes, due to weakened antioxidant defence |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krawczyk, A.; Stadler, S.M.; Strzalka-Mrozik, B. Nanomedicines for Dry Eye Syndrome: Targeting Oxidative Stress with Modern Nanomaterial Strategies. Molecules 2024, 29, 3732. https://doi.org/10.3390/molecules29163732
Krawczyk A, Stadler SM, Strzalka-Mrozik B. Nanomedicines for Dry Eye Syndrome: Targeting Oxidative Stress with Modern Nanomaterial Strategies. Molecules. 2024; 29(16):3732. https://doi.org/10.3390/molecules29163732
Chicago/Turabian StyleKrawczyk, Aleksandra, Sara Marta Stadler, and Barbara Strzalka-Mrozik. 2024. "Nanomedicines for Dry Eye Syndrome: Targeting Oxidative Stress with Modern Nanomaterial Strategies" Molecules 29, no. 16: 3732. https://doi.org/10.3390/molecules29163732






