Plant Phenolics in the Prevention and Therapy of Acne: A Comprehensive Review
Abstract
:1. Introduction
2. Flavonoids and Phenolic Acids—The Two Most Widespread Groups of Phenolic Compounds
3. Acne—One of the Most Common Skin Conditions
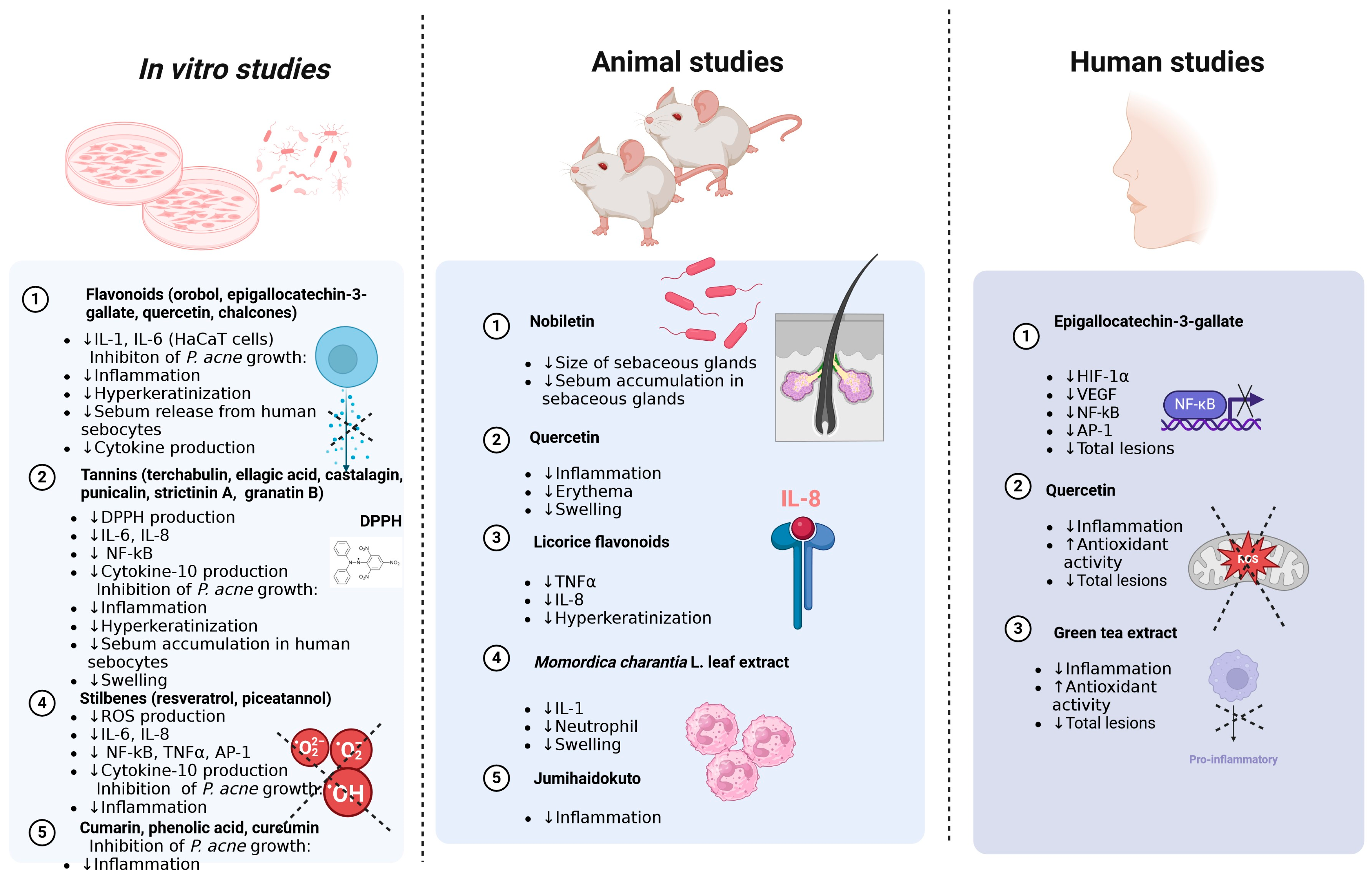
4. Antiacne Potential of Plant-Derived Phenolic Compounds—In Vitro Studies
4.1. Flavonoids
4.2. Tannins
4.3. Stilbenes
4.4. Coumarins
4.5. Phenolic Acids
4.6. Curcumin
5. Potential Application of Plant Phenolics in Acne Vulgaris—Animal Studies
6. Potential Application of Plant Phenolics in Various Types of Acne—Human Studies
7. Synergistic Effect of Polyphenols with Synthetic Drugs in the Treatment of Acne
8. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- McGrowder, D.A.; Miller, F.G.; Nwokocha, C.R.; Anderson, M.S.; Wilson-Clarke, C.; Vaz, K.; Anderson-Jackson, L.; Brown, J. Medicinal Herbs Used in Traditional Management of Breast Cancer: Mechanisms of Action. Medicines 2020, 7, 47. [Google Scholar] [CrossRef]
- Asgharian, P.; Quispe, C.; Herrera-Bravo, J.; Sabernavaei, M.; Hosseini, K.; Forouhandeh, H.; Ebrahimi, T.; Sharafi-Badr, P.; Tarhriz, V.; Soofiyani, S.R.; et al. Pharmacological Effects and Therapeutic Potential of Natural Compounds in Neuropsychiatric Disorders: An Update. Front. Pharmacol. 2022, 13, 926607. [Google Scholar] [CrossRef] [PubMed]
- Keskin, M.; Thiruvengadam, M. Phytochemicals from Natural Products for the Prevention and Treatment of Non-Communicable Diseases. Curr. Top. Med. Chem. 2022, 22, 1907–1908. [Google Scholar] [CrossRef]
- Arct, J.; Pytkowska, K. Flavonoids as Components of Biologically Active Cosmeceuticals. Clin. Dermatol. 2008, 26, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Koch, W.; Zagórska, J.; Marzec, Z.; Kukula-Koch, W. Applications of Tea (Camellia Sinensis) and Its Active Constituents in Cosmetics. Molecules 2019, 24, 4277. [Google Scholar] [CrossRef] [PubMed]
- Gianeti, M.D.; Mercurio, D.G.; Campos, P.M.B.G.M. The Use of Green Tea Extract in Cosmetic Formulations: Not Only an Antioxidant Active Ingredient. Dermatol. Ther. 2013, 26, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Koch, W. Dietary Polyphenols-Important Non-Nutrients in the Prevention of Chronic Noncommunicable Diseases. Syst. Rev. Nutr. 2019, 11, 1039. [Google Scholar] [CrossRef]
- Dai, J.; Mumper, R.J. Plant Phenolics: Extraction, Analysis and Their Antioxidant and Anticancer Properties. Molecules 2010, 15, 7313–7352. [Google Scholar] [CrossRef]
- Hano, C.; Tungmunnithum, D. Plant Polyphenols, More than Just Simple Natural Antioxidants: Oxidative Stress, Aging and Age-Related Diseases. Medicines 2020, 7, 26. [Google Scholar] [CrossRef]
- Pandey, K.B.; Rizvi, S.I. Plant Polyphenols as Dietary Antioxidants in Human Health and Disease. Oxid. Med. Cell Longev. 2009, 2, 270–278. [Google Scholar] [CrossRef]
- Neveu, V.; Perez-Jiménez, J.; Vos, F.; Crespy, V.; du Chaffaut, L.; Mennen, L.; Knox, C.; Eisner, R.; Cruz, J.; Wishart, D.; et al. Phenol-Explorer: An Online Comprehensive Database on Polyphenol Contents in Foods. Database 2010, 2010, bap024. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Jiménez, J.; Neveu, V.; Vos, F.; Scalbert, A. Systematic Analysis of the Content of 502 Polyphenols in 452 Foods and Beverages: An Application of the Phenol-Explorer Database. J. Agric. Food Chem. 2010, 58, 4959–4969. [Google Scholar] [CrossRef]
- Chirinos, R.; Betalleluz-Pallardel, I.; Huamán, A.; Arbizu, C.; Pedreschi, R.; Campos, D. HPLC-DAD Characterisation of Phenolic Compounds from Andean Oca (Oxalis Tuberosa Mol.) Tubers and Their Contribution to the Antioxidant Capacity. Food Chem. 2009, 113, 1243–1251. [Google Scholar] [CrossRef]
- Kumar, N.; Pruthi, V. Potential Applications of Ferulic Acid from Natural Sources. Biotechnol. Rep. 2014, 4, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Goel, N. Phenolic Acids: Natural Versatile Molecules with Promising Therapeutic Applications. Biotechnol. Rep. 2019, 24, e00370. [Google Scholar] [CrossRef]
- Chen, S.; Wang, X.; Cheng, Y.; Gao, H.; Chen, X. A Review of Classification, Biosynthesis, Biological Activities and Potential Applications of Flavonoids. Molecules 2023, 28, 4982. [Google Scholar] [CrossRef]
- Pereira, D.M.; Valentão, P.; Pereira, J.A.; Andrade, P.B. Phenolics: From Chemistry to Biology. Molecules 2009, 14, 2202–2211. [Google Scholar] [CrossRef]
- Dixon, R.A. Phytoestrogens. Annu. Rev. Plant Biol. 2004, 55, 225–261. [Google Scholar] [CrossRef]
- Khoddami, A.; Wilkes, M.A.; Roberts, T.H. Techniques for Analysis of Plant Phenolic Compounds. Molecules 2013, 18, 2328–2375. [Google Scholar] [CrossRef]
- Kumar, N.; Gupta, S.; Chand Yadav, T.; Pruthi, V.; Kumar Varadwaj, P.; Goel, N. Extrapolation of Phenolic Compounds as Multi-Target Agents against Cancer and Inflammation. J. Biomol. Struct. Dyn. 2019, 37, 2355–2369. [Google Scholar] [CrossRef]
- Manso, T.; Lores, M.; de Miguel, T. Antimicrobial Activity of Polyphenols and Natural Polyphenolic Extracts on Clinical Isolates. Antibiotics 2021, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Borowiec, K.; Stachniuk, A.; Szwajgier, D.; Trzpil, A. Polyphenols Composition and the Biological Effects of Six Selected Small Dark Fruits. Food Chem. 2022, 391, 133281. [Google Scholar] [CrossRef] [PubMed]
- Bouarab-Chibane, L.; Forquet, V.; Lantéri, P.; Clément, Y.; Léonard-Akkari, L.; Oulahal, N.; Degraeve, P.; Bordes, C. Antibacterial Properties of Polyphenols: Characterization and QSAR (Quantitative Structure–Activity Relationship) Models. Front. Microbiol. 2019, 10, 829. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, I.; Wilairatana, P.; Saqib, F.; Nasir, B.; Wahid, M.; Latif, M.F.; Iqbal, A.; Naz, R.; Mubarak, M.S. Plant Polyphenols and Their Potential Benefits on Cardiovascular Health: A Review. Molecules 2023, 28, 6403. [Google Scholar] [CrossRef]
- Behl, T.; Bungau, S.; Kumar, K.; Zengin, G.; Khan, F.; Kumar, A.; Kaur, R.; Venkatachalam, T.; Tit, D.M.; Vesa, C.M.; et al. Pleotropic Effects of Polyphenols in Cardiovascular System. Biomed. Pharmacother. 2020, 130, 110714. [Google Scholar] [CrossRef]
- Da Porto, A.; Cavarape, A.; Colussi, G.; Casarsa, V.; Catena, C.; Sechi, L.A. Polyphenols Rich Diets and Risk of Type 2 Diabetes. Nutrients 2021, 13, 1445. [Google Scholar] [CrossRef]
- Arias-Sánchez, R.A.; Torner, L.; Fenton Navarro, B. Polyphenols and Neurodegenerative Diseases: Potential Effects and Mechanisms of Neuroprotection. Molecules 2023, 28, 5415. [Google Scholar] [CrossRef]
- Grabska-Kobyłecka, I.; Szpakowski, P.; Król, A.; Książek-Winiarek, D.; Kobyłecki, A.; Głąbiński, A.; Nowak, D. Polyphenols and Their Impact on the Prevention of Neurodegenerative Diseases and Development. Nutrients 2023, 15, 3454. [Google Scholar] [CrossRef]
- Khurana, S.; Venkataraman, K.; Hollingsworth, A.; Piche, M.; Tai, T.C. Polyphenols: Benefits to the Cardiovascular System in Health and in Aging. Nutrients 2013, 5, 3779–3827. [Google Scholar] [CrossRef]
- Di Salvo, E.; Gangemi, S.; Genovese, C.; Cicero, N.; Casciaro, M. Polyphenols from Mediterranean Plants: Biological Activities for Skin Photoprotection in Atopic Dermatitis, Psoriasis, and Chronic Urticaria. Plants 2023, 12, 3579. [Google Scholar] [CrossRef]
- Souto, E.B.; Sampaio, A.C.; Campos, J.R.; Martins-Gomes, C.; Aires, A.; Silva, A.M. Chapter 2—Polyphenols for Skin Cancer: Chemical Properties, Structure-Related Mechanisms of Action and New Delivery Systems. In Studies in Natural Products Chemistry; Atta-ur-Rahman, Ed.; Bioactive Natural Products; Elsevier: Amsterdam, The Netherlands, 2019; Volume 63, pp. 21–42. [Google Scholar]
- Sun, M.; Deng, Y.; Cao, X.; Xiao, L.; Ding, Q.; Luo, F.; Huang, P.; Gao, Y.; Liu, M.; Zhao, H. Effects of Natural Polyphenols on Skin and Hair Health: A Review. Molecules 2022, 27, 7832. [Google Scholar] [CrossRef]
- de Lima Cherubim, D.J.; Buzanello Martins, C.V.; Oliveira Fariña, L.; da Silva de Lucca, R.A. Polyphenols as Natural Antioxidants in Cosmetics Applications. J. Cosmet. Dermatol. 2020, 19, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Zaenglein, A.L.; Pathy, A.L.; Schlosser, B.J.; Alikhan, A.; Baldwin, H.E.; Berson, D.S.; Bowe, W.P.; Graber, E.M.; Harper, J.C.; Kang, S.; et al. Guidelines of Care for the Management of Acne Vulgaris. J. Am. Acad. Dermatol. 2016, 74, 945–973.e33. [Google Scholar] [CrossRef]
- Lim, H.W.; Collins, S.A.B.; Resneck, J.S.; Bolognia, J.L.; Hodge, J.A.; Rohrer, T.A.; Van Beek, M.J.; Margolis, D.J.; Sober, A.J.; Weinstock, M.A.; et al. The Burden of Skin Disease in the United States. J. Am. Acad. Dermatol. 2017, 76, 958–972.e2. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhang, T.C.; Yin, X.L.; Man, J.Y.; Yang, X.R.; Lu, M. Magnitude and Temporal Trend of Acne Vulgaris Burden in 204 Countries and Territories from 1990 to 2019: An Analysis from the Global Burden of Disease Study 2019. Br. J. Dermatol. 2022, 186, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.C.; Dellavalle, R.P.; Garner, S. Acne Vulgaris. Lancet 2012, 379, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Melnik, B.C. Linking Diet to Acne Metabolomics, Inflammation, and Comedogenesis: An Update. Clin. Cosmet. Investig. Dermatol. 2015, 8, 371–388. [Google Scholar] [CrossRef]
- Goodman, G. Acne and Acne Scarring—The Case for Active and Early Intervention. Aust. Fam. Physician 2006, 35, 503–504. [Google Scholar]
- Fabbrocini, G.; Staibano, S.; De Rosa, G.; Battimiello, V.; Fardella, N.; Ilardi, G.; La Rotonda, M.I.; Longobardi, A.; Mazzella, M.; Siano, M.; et al. Resveratrol-Containing Gel for the Treatment of Acne Vulgaris: A Single-Blind, Vehicle-Controlled, Pilot Study. Am. J. Clin. Dermatol. 2011, 12, 133–141. [Google Scholar] [CrossRef]
- Toyoda, M.; Morohashi, M. Pathogenesis of Acne. Med. Electron. Microsc. 2001, 34, 29–40. [Google Scholar] [CrossRef]
- Knutsen-Larson, S.; Dawson, A.L.; Dunnick, C.A.; Dellavalle, R.P. Acne Vulgaris: Pathogenesis, Treatment, and Needs Assessment. Dermatol. Clin. 2012, 30, 99–106, viii–ix. [Google Scholar] [CrossRef] [PubMed]
- Condrò, G.; Guerini, M.; Castello, M.; Perugini, P. Acne Vulgaris, Atopic Dermatitis and Rosacea: The Role of the Skin Microbiota-A Review. Biomedicines 2022, 10, 2523. [Google Scholar] [CrossRef]
- Jeremy, A.H.T.; Holland, D.B.; Roberts, S.G.; Thomson, K.F.; Cunliffe, W.J. Inflammatory Events Are Involved in Acne Lesion Initiation. J. Investig. Dermatol. 2003, 121, 20–27. [Google Scholar] [CrossRef]
- Eichenfield, D.Z.; Sprague, J.; Eichenfield, L.F. Management of Acne Vulgaris: A Review. JAMA 2021, 326, 2055–2067. [Google Scholar] [CrossRef]
- van Zuuren, E.J. Rosacea. N. Engl. J. Med. 2017, 377, 1754–1764. [Google Scholar] [CrossRef] [PubMed]
- Rosas Vazquez, E.; Campos Macias, P.; Ochoa Tirado, J.G.; Garcia Solana, C.; Casanova, A.; Palomino Moncada, J.F. Chloracne in the 1990s. Int J Dermatol 1996, 35, 643–645. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, R.L. What Every Physician Should Know about Polycystic Ovary Syndrome. Dermatol. Ther. 2008, 21, 354–361. [Google Scholar] [CrossRef]
- Lucky, A.W. A Review of Infantile and Pediatric Acne. Dermatology 1998, 196, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Meixner, D.; Schneider, S.; Krause, M.; Sterry, W. Acne Inversa. J. Dtsch. Dermatol. Ges. 2008, 6, 189–196. [Google Scholar] [CrossRef]
- Valeyrie-Allanore, L.; Sassolas, B.; Roujeau, J.-C. Drug-Induced Skin, Nail and Hair Disorders. Drug Saf. 2007, 30, 1011–1030. [Google Scholar] [CrossRef]
- Tucker, S.B. Occupational Tropical Acne. Cutis 1983, 31, 79–81. [Google Scholar] [PubMed]
- Melnik, B.; Jansen, T.; Grabbe, S. Abuse of Anabolic-Androgenic Steroids and Bodybuilding Acne: An Underestimated Health Problem. J. Dutsch. Dermatol. Ges. 2007, 5, 110–117. [Google Scholar] [CrossRef]
- Bhat, Y.J.; Latief, I.; Hassan, I. Update on Etiopathogenesis and Treatment of Acne. Indian. J. Dermatol. Venereol. Leprol. 2017, 83, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, A.; Salame, N.; Armstrong, A.W.; Merola, J.F.; Parra, S.; Takeshita, J.; Chen, S.C.; Latella, J.; Van Beek, M. International Dermatology Outcome Measures and the American Academy of Dermatology A Provider Global Assessment Quality Measure for Clinical Practice for Inflammatory Skin Disorders. J. Am. Acad. Dermatol. 2019, 80, 823–828. [Google Scholar] [CrossRef]
- Shalita, A.R. Acne: Clinical Presentations. Clin. Dermatol. 2004, 22, 385–386. [Google Scholar] [CrossRef]
- Ederveen, T.H.A.; Smits, J.P.H.; Boekhorst, J.; Schalkwijk, J.; van den Bogaard, E.H.; Zeeuwen, P.L.J.M. Skin Microbiota in Health and Disease: From Sequencing to Biology. J. Dermatol. 2020, 47, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Egert, M.; Simmering, R.; Riedel, C.U. The Association of the Skin Microbiota With Health, Immunity, and Disease. Clin. Pharmacol. Ther. 2017, 102, 62–69. [Google Scholar] [CrossRef]
- Chen, Y.E.; Fischbach, M.A.; Belkaid, Y. Skin Microbiota-Host Interactions. Nature 2018, 553, 427–436. [Google Scholar] [CrossRef]
- Balato, A.; Cacciapuoti, S.; Di Caprio, R.; Marasca, C.; Masarà, A.; Raimondo, A.; Fabbrocini, G. Human Microbiome: Composition and Role in Inflammatory Skin Diseases. Arch. Immunol. Ther. Exp. 2019, 67, 1–18. [Google Scholar] [CrossRef]
- Chen, Y.E.; Tsao, H. The Skin Microbiome: Current Perspectives and Future Challenges. J. Am. Acad. Dermatol. 2013, 69, 143–155. [Google Scholar] [CrossRef]
- Zeeuwen, P.L.J.M.; Boekhorst, J.; van den Bogaard, E.H.; de Koning, H.D.; van de Kerkhof, P.M.C.; Saulnier, D.M.; van Swam, I.I.; van Hijum, S.A.F.T.; Kleerebezem, M.; Schalkwijk, J.; et al. Microbiome Dynamics of Human Epidermis Following Skin Barrier Disruption. Genome Biol. 2012, 13, R101. [Google Scholar] [CrossRef] [PubMed]
- Dréno, B.; Araviiskaia, E.; Berardesca, E.; Gontijo, G.; Sanchez Viera, M.; Xiang, L.F.; Martin, R.; Bieber, T. Microbiome in Healthy Skin, Update for Dermatologists. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 2038–2047. [Google Scholar] [CrossRef] [PubMed]
- Musthaq, S.; Mazuy, A.; Jakus, J. The Microbiome in Dermatology. Clin. Dermatol. 2018, 36, 390–398. [Google Scholar] [CrossRef]
- Jarmuda, S.; O’Reilly, N.; Żaba, R.; Jakubowicz, O.; Szkaradkiewicz, A.; Kavanagh, K. Potential Role of Demodex Mites and Bacteria in the Induction of Rosacea. J. Med. Microbiol. 2012, 61, 1504–1510. [Google Scholar] [CrossRef] [PubMed]
- De Pessemier, B.; Grine, L.; Debaere, M.; Maes, A.; Paetzold, B.; Callewaert, C. Gut-Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions. Microorganisms 2021, 9, 353. [Google Scholar] [CrossRef] [PubMed]
- Castillo, D.E.; Nanda, S.; Keri, J.E. Propionibacterium (Cutibacterium) Acnes Bacteriophage Therapy in Acne: Current Evidence and Future Perspectives. Dermatol. Ther. 2019, 9, 19–31. [Google Scholar] [CrossRef]
- Shibagaki, N.; Suda, W.; Clavaud, C.; Bastien, P.; Takayasu, L.; Iioka, E.; Kurokawa, R.; Yamashita, N.; Hattori, Y.; Shindo, C.; et al. Aging-Related Changes in the Diversity of Women’s Skin Microbiomes Associated with Oral Bacteria. Sci. Rep. 2017, 7, 10567. [Google Scholar] [CrossRef]
- Xu, Z.; Wang, Z.; Yuan, C.; Liu, X.; Yang, F.; Wang, T.; Wang, J.; Manabe, K.; Qin, O.; Wang, X.; et al. Dandruff Is Associated with the Conjoined Interactions between Host and Microorganisms. Sci. Rep. 2016, 6, 24877. [Google Scholar] [CrossRef]
- Kang, S.; Cho, S.; Chung, J.H.; Hammerberg, C.; Fisher, G.J.; Voorhees, J.J. Inflammation and Extracellular Matrix Degradation Mediated by Activated Transcription Factors Nuclear Factor-κB and Activator Protein-1 in Inflammatory Acne Lesions in Vivo. Am. J. Pathol. 2005, 166, 1691–1699. [Google Scholar] [CrossRef]
- Alestas, T.; Ganceviciene, R.; Fimmel, S.; Müller-Decker, K.; Zouboulis, C.C. Enzymes Involved in the Biosynthesis of Leukotriene B4 and Prostaglandin E2 Are Active in Sebaceous Glands. J. Mol. Med. 2006, 84, 75–87. [Google Scholar] [CrossRef]
- Zouboulis, C.C.; Seltmann, H.; Alestas, T. Zileuton Prevents the Activation of the Leukotriene Pathway and Reduces Sebaceous Lipogenesis. Exp. Dermatol. 2010, 19, 148–150. [Google Scholar] [CrossRef]
- Kim, J.; Ochoa, M.-T.; Krutzik, S.R.; Takeuchi, O.; Uematsu, S.; Legaspi, A.J.; Brightbill, H.D.; Holland, D.; Cunliffe, W.J.; Akira, S.; et al. Activation of Toll-like Receptor 2 in Acne Triggers Inflammatory Cytokine Responses. J. Immunol. 2002, 169, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- McInturff, J.E.; Kim, J. The Role of Toll-like Receptors in the Pathophysiology of Acne. Semin. Cutan. Med. Surg. 2005, 24, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Selway, J.L.; Kurczab, T.; Kealey, T.; Langlands, K. Toll-like Receptor 2 Activation and Comedogenesis: Implications for the Pathogenesis of Acne. BMC Dermatol. 2013, 13, 10. [Google Scholar] [CrossRef]
- Thiboutot, D.; Chen, W. Update and Future of Hormonal Therapy in Acne. Dermatology 2003, 206, 57–67. [Google Scholar] [CrossRef]
- George, R.; Clarke, S.; Thiboutot, D. Hormonal Therapy for Acne. Semin. Cutan. Med. Surg. 2008, 27, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Zouboulis, C.C. Acne and Sebaceous Gland Function. Clin. Dermatol. 2004, 22, 360–366. [Google Scholar] [CrossRef]
- Gollnick, H.; Cunliffe, W.; Berson, D.; Dreno, B.; Finlay, A.; Leyden, J.J.; Shalita, A.R.; Thiboutot, D. Global Alliance to Improve Outcomes in Acne Management of Acne: A Report from a Global Alliance to Improve Outcomes in Acne. J. Am. Acad. Dermatol. 2003, 49, S1–S37. [Google Scholar] [CrossRef]
- Glass, D.; Boorman, G.C.; Stables, G.I.; Cunliffe, W.J.; Goode, K. A Placebo-Controlled Clinical Trial to Compare a Gel Containing a Combination of Isotretinoin (0.05%) and Erythromycin (2%) with Gels Containing Isotretinoin (0.05%) or Erythromycin (2%) Alone in the Topical Treatment of Acne Vulgaris. Dermatology 1999, 199, 242–247. [Google Scholar] [CrossRef]
- Alexis, A.; Del Rosso, J.Q.; Desai, S.R.; Downie, J.B.; Draelos, Z.D.; Feser, C.; Forconi, R.; Fowler, J.F.; Gold, M.; Kaufman-Janette, J.; et al. BPX-01 Minocycline Topical Gel Shows Promise for the Treatment of Moderate-to-Severe Inflammatory Acne Vulgaris. J. Clin. Aesthet. Dermatol. 2018, 11, 25–35. [Google Scholar]
- Jarratt, M.T.; Brundage, T. Efficacy and Safety of Clindamycin-Tretinoin Gel versus Clindamycin or Tretinoin Alone in Acne Vulgaris: A Randomized, Double-Blind, Vehicle-Controlled Study. J. Drugs Dermatol. 2012, 11, 318–326. [Google Scholar]
- Stein Gold, L.; Baldwin, H.; Kircik, L.H.; Weiss, J.S.; Pariser, D.M.; Callender, V.; Lain, E.; Gold, M.; Beer, K.; Draelos, Z.; et al. Efficacy and Safety of a Fixed-Dose Clindamycin Phosphate 1.2%, Benzoyl Peroxide 3.1%, and Adapalene 0.15% Gel for Moderate-to-Severe Acne: A Randomized Phase II Study of the First Triple-Combination Drug. Am. J. Clin. Dermatol. 2022, 23, 93–104. [Google Scholar] [CrossRef]
- Kawashima, M.; Hashimoto, H.; Alio Sáenz, A.B.; Ono, M.; Yamada, M. Is Benzoyl Peroxide 3% Topical Gel Effective and Safe in the Treatment of Acne Vulgaris in Japanese Patients? A Multicenter, Randomized, Double-Blind, Vehicle-Controlled, Parallel-Group Study. J. Dermatol. 2014, 41, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Harper, J.C. The Efficacy and Tolerability of a Fixed Combination Clindamycin (1.2%) and Benzoyl Peroxide (3.75%) Aqueous Gel in Patients with Facial Acne Vulgaris: Gender as a Clinically Relevant Outcome Variable. J. Drugs Dermatol. 2015, 14, 381–384. [Google Scholar] [PubMed]
- Guerra-Tapia, A. Effects of Benzoyl Peroxide 5% Clindamycin Combination Gel versus Adapalene 0.1% on Quality of Life in Patients with Mild to Moderate Acne Vulgaris: A Randomized Single-Blind Study. J. Drugs Dermatol. 2012, 11, 714–722. [Google Scholar] [PubMed]
- Tyring, S.K.; Kircik, L.H.; Pariser, D.M.; Guenin, E.; Bhatt, V.; Pillai, R. Novel Tretinoin 0.05% Lotion for the Once-Daily Treatment of Moderate-to-Severe Acne Vulgaris: Assessment of Efficacy and Safety in Patients Aged 9 Years and Older. J. Drugs Dermatol. 2018, 17, 1084–1091. [Google Scholar]
- Tanghetti, E.A.; Werschler, W.P.; Lain, T.; Guenin, E.; Martin, G.; Pillai, R. Tazarotene 0.045% Lotion for Once-Daily Treatment of Moderate-to-Severe Acne Vulgaris: Results from Two Phase 3 Trials. J. Drugs Dermatol. 2020, 19, 70–77. [Google Scholar] [CrossRef]
- Thiboutot, D.; Pariser, D.M.; Egan, N.; Flores, J.; Herndon, J.H.; Kanof, N.B.; Kempers, S.E.; Maddin, S.; Poulin, Y.P.; Wilson, D.C.; et al. Adapalene Gel 0.3% for the Treatment of Acne Vulgaris: A Multicenter, Randomized, Double-Blind, Controlled, Phase III Trial. J. Am. Acad. Dermatol. 2006, 54, 242–250. [Google Scholar] [CrossRef]
- Tan, J.; Thiboutot, D.; Popp, G.; Gooderham, M.; Lynde, C.; Del Rosso, J.; Weiss, J.; Blume-Peytavi, U.; Weglovska, J.; Johnson, S.; et al. Randomized Phase 3 Evaluation of Trifarotene 50 Μg/g Cream Treatment of Moderate Facial and Truncal Acne. J. Am. Acad. Dermatol. 2019, 80, 1691–1699. [Google Scholar] [CrossRef]
- Dogra, S.; Sumathy, T.K.; Nayak, C.; Ravichandran, G.; Vaidya, P.P.; Mehta, S.; Mittal, R.; Mane, A.; Charugulla, S.N. Efficacy and Safety Comparison of Combination of 0.04% Tretinoin Microspheres plus 1% Clindamycin versus Their Monotherapy in Patients with Acne Vulgaris: A Phase 3, Randomized, Double-Blind Study. J. Dermatol. Treat. 2021, 32, 925–933. [Google Scholar] [CrossRef]
- Stein Gold, L.; Werschler, W.P.; Mohawk, J. Adapalene/Benzoyl Peroxide Gel 0.3%/2.5%: Effective Acne Therapy Regardless of Age or Gender. J. Drugs Dermatol. 2017, 16, 582–589. [Google Scholar]
- Webster, G.F.; Sugarman, J.; Levy-Hacham, O.; Toledano, O. Microencapsulated Benzoyl Peroxide and Tretinoin for the Treatment of Acne Vulgaris: Results from a Phase 2 Multicenter, Double-Blind, Randomized, Vehicle-Controlled Study. Skinmed 2020, 18, 343–351. [Google Scholar] [PubMed]
- Shalita, A.R. Treatment of Mild and Moderate Acne Vulgaris with Salicylic Acid in an Alcohol-Detergent Vehicle. Cutis 1981, 28, 556–558, 561. [Google Scholar]
- Iraji, F.; Sadeghinia, A.; Shahmoradi, Z.; Siadat, A.H.; Jooya, A. Efficacy of Topical Azelaic Acid Gel in the Treatment of Mild-Moderate Acne Vulgaris. Indian. J. Dermatol. Venereol. Leprol. 2007, 73, 94–96. [Google Scholar] [CrossRef]
- Hebert, A.; Thiboutot, D.; Stein Gold, L.; Cartwright, M.; Gerloni, M.; Fragasso, E.; Mazzetti, A. Efficacy and Safety of Topical Clascoterone Cream, 1%, for Treatment in Patients With Facial Acne: Two Phase 3 Randomized Clinical Trials. JAMA Dermatol. 2020, 156, 621–630. [Google Scholar] [CrossRef]
- Webster, G.F.; Leyden, J.J.; Gross, J.A. Results of a Phase III, Double-Blind, Randomized, Parallel-Group, Non-Inferiority Study Evaluating the Safety and Efficacy of Isotretinoin-Lidose in Patients with Severe Recalcitrant Nodular Acne. J. Drugs Dermatol. 2014, 13, 665–670. [Google Scholar] [PubMed]
- Lee, J.W.; Yoo, K.H.; Park, K.Y.; Han, T.Y.; Li, K.; Seo, S.J.; Hong, C.K. Effectiveness of Conventional, Low-Dose and Intermittent Oral Isotretinoin in the Treatment of Acne: A Randomized, Controlled Comparative Study. Br. J. Dermatol. 2011, 164, 1369–1375. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, R.V.; Yeung, H.; Cheng, C.E.; Cook-Bolden, F.; Desai, S.R.; Druby, K.M.; Freeman, E.E.; Keri, J.E.; Stein Gold, L.F.; Tan, J.K.L.; et al. Guidelines of Care for the Management of Acne Vulgaris. J. Am. Acad. Dermatol. 2024, 90, 1006.e1–1006.e30. [Google Scholar] [CrossRef] [PubMed]
- Pariser, D.M.; Green, L.J.; Lain, E.L.; Schmitz, C.; Chinigo, A.S.; McNamee, B.; Berk, D.R. Safety and Tolerability of Sarecycline for the Treatment of Acne Vulgaris: Results from a Phase III, Multicenter, Open-Label Study and a Phase I Phototoxicity Study. J. Clin. Aesthet. Dermatol. 2019, 12, E53–E62. [Google Scholar] [CrossRef]
- Stewart, D.M.; Torok, H.M.; Weiss, J.S.; Plott, R.T. Solodyn Phase 2 Study Group Dose-Ranging Efficacy of New Once-Daily Extended-Release Minocycline for Acne Vulgaris. Cutis 2006, 78, 11–20. [Google Scholar]
- Moore, A.; Ling, M.; Bucko, A.; Manna, V.; Rueda, M.-J. Efficacy and Safety of Subantimicrobial Dose, Modified-Release Doxycycline 40 Mg Versus Doxycycline 100 Mg Versus Placebo for the Treatment of Inflammatory Lesions in Moderate and Severe Acne: A Randomized, Double-Blinded, Controlled Study. J. Drugs Dermatol. 2015, 14, 581–586. [Google Scholar] [PubMed]
- Maloney, J.M.; Dietze, P.; Watson, D.; Niknian, M.; Lee-Rugh, S.; Sampson-Landers, C.; Korner, P. Treatment of Acne Using a 3-Milligram Drospirenone/20-Microgram Ethinyl Estradiol Oral Contraceptive Administered in a 24/4 Regimen: A Randomized Controlled Trial. Obstet. Gynecol. 2008, 112, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Plewig, G.; Cunliffe, W.J.; Binder, N.; Höschen, K. Efficacy of an Oral Contraceptive Containing EE 0.03 Mg and CMA 2 Mg (Belara) in Moderate Acne Resolution: A Randomized, Double-Blind, Placebo-Controlled Phase III Trial. Contraception 2009, 80, 25–33. [Google Scholar] [CrossRef]
- Palombo-Kinne, E.; Schellschmidt, I.; Schumacher, U.; Gräser, T. Efficacy of a Combined Oral Contraceptive Containing 0.030 Mg Ethinylestradiol/2 Mg Dienogest for the Treatment of Papulopustular Acne in Comparison with Placebo and 0.035 Mg Ethinylestradiol/2 Mg Cyproterone Acetate. Contraception 2009, 79, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Patiyasikunt, M.; Chancheewa, B.; Asawanonda, P.; Noppakun, N.; Kumtornrut, C. Efficacy and Tolerability of Low-Dose Spironolactone and Topical Benzoyl Peroxide in Adult Female Acne: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Dermatol. 2020, 47, 1411–1416. [Google Scholar] [CrossRef]
- Grandhi, R.; Alikhan, A. Spironolactone for the Treatment of Acne: A 4-Year Retrospective Study. Dermatology 2017, 233, 141–144. [Google Scholar] [CrossRef]
- Tangjaturonrusamee, C.; Rattanaumpawan, P.; Ditre, C.M. Comparison of Pneumatic Broadband Light plus Adapalene Gel 0.3% versus Adapalene Gel 0.3% Monotherapy in the Treatment of Mild to Moderate Acne. Cutis 2016, 98, 56–61. [Google Scholar]
- Levine, R.M.; Rasmussen, J.E. Intralesional Corticosteroids in the Treatment of Nodulocystic Acne. Arch. Dermatol. 1983, 119, 480–481. [Google Scholar] [CrossRef]
- Dréno, B.; Fischer, T.C.; Perosino, E.; Poli, F.; Viera, M.S.; Rendon, M.I.; Berson, D.S.; Cohen, J.L.; Roberts, W.E.; Starker, I.; et al. Expert Opinion: Efficacy of Superficial Chemical Peels in Active Acne Management--What Can We Learn from the Literature Today? Evidence-Based Recommendations. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 695–704. [Google Scholar] [CrossRef]
- Ilknur, T.; Demirtaşoğlu, M.; Biçak, M.U.; Ozkan, S. Glycolic Acid Peels versus Amino Fruit Acid Peels for Acne. J. Cosmet. Laser Ther. 2010, 12, 242–245. [Google Scholar] [CrossRef]
- Gether, L.; Overgaard, L.K.; Egeberg, A.; Thyssen, J.P. Incidence and Prevalence of Rosacea: A Systematic Review and Meta-Analysis. Br. J. Dermatol. 2018, 179, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Powell, F.C. Clinical Practice. Rosacea. N. Engl. J. Med. 2005, 352, 793–803. [Google Scholar] [CrossRef]
- Gallo, R.L.; Granstein, R.D.; Kang, S.; Mannis, M.; Steinhoff, M.; Tan, J.; Thiboutot, D. Standard Classification and Pathophysiology of Rosacea: The 2017 Update by the National Rosacea Society Expert Committee. J. Am. Acad. Dermatol. 2018, 78, 148–155. [Google Scholar] [CrossRef]
- Alexis, A.F.; Callender, V.D.; Baldwin, H.E.; Desai, S.R.; Rendon, M.I.; Taylor, S.C. Global Epidemiology and Clinical Spectrum of Rosacea, Highlighting Skin of Color: Review and Clinical Practice Experience. J. Am. Acad. Dermatol. 2019, 80, 1722–1729.e7. [Google Scholar] [CrossRef] [PubMed]
- Browning, D.J.; Proia, A.D. Ocular Rosacea. Surv. Ophthalmol. 1986, 31, 145–158. [Google Scholar] [CrossRef]
- Vieira, A.C.C.; Höfling-Lima, A.L.; Mannis, M.J. Ocular Rosacea--a Review. Arq. Bras. Oftalmol. 2012, 75, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Redd, T.K.; Seitzman, G.D. Ocular Rosacea. Curr. Opin. Ophthalmol. 2020, 31, 503–507. [Google Scholar] [CrossRef]
- Zuber, T.J. Rosacea. Prim. Care 2000, 27, 309–318. [Google Scholar] [CrossRef]
- Chiriac, A.; Wollina, U. Rosacea in Children: A Review. Eur. J. Pediatr. 2023, 182, 4323–4328. [Google Scholar] [CrossRef]
- van Zuuren, E.J.; Fedorowicz, Z.; Tan, J.; van der Linden, M.M.D.; Arents, B.W.M.; Carter, B.; Charland, L. Interventions for Rosacea Based on the Phenotype Approach: An Updated Systematic Review Including GRADE Assessments. Br. J. Dermatol. 2019, 181, 65–79. [Google Scholar] [CrossRef]
- Buddenkotte, J.; Steinhoff, M. Recent Advances in Understanding and Managing Rosacea. F1000Research 2018, 7, 1885. [Google Scholar] [CrossRef] [PubMed]
- Holmes, A.D.; Steinhoff, M. Integrative Concepts of Rosacea Pathophysiology, Clinical Presentation and New Therapeutics. Exp. Dermatol. 2017, 26, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Ahn, C.S.; Huang, W.W. Rosacea Pathogenesis. Dermatol. Clin. 2018, 36, 81–86. [Google Scholar] [CrossRef]
- Schwab, V.D.; Sulk, M.; Seeliger, S.; Nowak, P.; Aubert, J.; Mess, C.; Rivier, M.; Carlavan, I.; Rossio, P.; Metze, D.; et al. Neurovascular and Neuroimmune Aspects in the Pathophysiology of Rosacea. J. Investig. Dermatol. Symp. Proc. 2011, 15, 53–62. [Google Scholar] [CrossRef]
- Holmes, A.D. Potential Role of Microorganisms in the Pathogenesis of Rosacea. J. Am. Acad. Dermatol. 2013, 69, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, K.; Kanada, K.; Macleod, D.T.; Borkowski, A.W.; Morizane, S.; Nakatsuji, T.; Cogen, A.L.; Gallo, R.L. TLR2 Expression Is Increased in Rosacea and Stimulates Enhanced Serine Protease Production by Keratinocytes. J. Investig. Dermatol. 2011, 131, 688–697. [Google Scholar] [CrossRef]
- Woo, Y.R.; Lim, J.H.; Cho, D.H.; Park, H.J. Rosacea: Molecular Mechanisms and Management of a Chronic Cutaneous Inflammatory Condition. Int. J. Mol. Sci. 2016, 17, 1562. [Google Scholar] [CrossRef]
- Kelhälä, H.-L.; Palatsi, R.; Fyhrquist, N.; Lehtimäki, S.; Väyrynen, J.P.; Kallioinen, M.; Kubin, M.E.; Greco, D.; Tasanen, K.; Alenius, H.; et al. IL-17/Th17 Pathway Is Activated in Acne Lesions. PLoS ONE 2014, 9, e105238. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.L.S.; Raber, I.; Xu, J.; Li, R.; Spitale, R.; Chen, J.; Kiefer, A.K.; Tian, C.; Eriksson, N.K.; Hinds, D.A.; et al. Assessment of the Genetic Basis of Rosacea by Genome-Wide Association Study. J. Investig. Dermatol. 2015, 135, 1548–1555. [Google Scholar] [CrossRef]
- Thiboutot, D.; Anderson, R.; Cook-Bolden, F.; Draelos, Z.; Gallo, R.L.; Granstein, R.D.; Kang, S.; Macsai, M.; Gold, L.S.; Tan, J. Standard Management Options for Rosacea: The 2019 Update by the National Rosacea Society Expert Committee. J. Am. Acad. Dermatol. 2020, 82, 1501–1510. [Google Scholar] [CrossRef]
- Cole, C.; Shyr, T.; Ou-Yang, H. Metal Oxide Sunscreens Protect Skin by Absorption, Not by Reflection or Scattering. Photodermatol. Photoimmunol. Photomed. 2016, 32, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Schaller, M.; Almeida, L.M.C.; Bewley, A.; Cribier, B.; Dlova, N.C.; Kautz, G.; Mannis, M.; Oon, H.H.; Rajagopalan, M.; Steinhoff, M.; et al. Rosacea Treatment Update: Recommendations from the Global ROSacea COnsensus (ROSCO) Panel. Br. J. Dermatol. 2017, 176, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Draelos, Z.D.; Elewski, B.; Staedtler, G.; Havlickova, B. Azelaic Acid Foam 15% in the Treatment of Papulopustular Rosacea: A Randomized, Double-Blind, Vehicle-Controlled Study. Cutis 2013, 92, 306–317. [Google Scholar] [PubMed]
- Fowler, J.; Jackson, M.; Moore, A.; Jarratt, M.; Jones, T.; Meadows, K.; Steinhoff, M.; Rudisill, D.; Leoni, M. Efficacy and Safety of Once-Daily Topical Brimonidine Tartrate Gel 0.5% for the Treatment of Moderate to Severe Facial Erythema of Rosacea: Results of Two Randomized, Double-Blind, and Vehicle-Controlled Pivotal Studies. J. Drugs Dermatol. 2013, 12, 650–656. [Google Scholar] [PubMed]
- Schaller, M.; Kemény, L.; Havlickova, B.; Jackson, J.M.; Ambroziak, M.; Lynde, C.; Gooderham, M.; Remenyik, E.; Del Rosso, J.; Weglowska, J.; et al. A Randomized Phase 3b/4 Study to Evaluate Concomitant Use of Topical Ivermectin 1% Cream and Doxycycline 40-Mg Modified-Release Capsules, versus Topical Ivermectin 1% Cream and Placebo in the Treatment of Severe Rosacea. J. Am. Acad. Dermatol. 2020, 82, 336–343. [Google Scholar] [CrossRef]
- Koçak, M.; Yağli, S.; Vahapoğlu, G.; Ekşioğlu, M. Permethrin 5% Cream versus Metronidazole 0.75% Gel for the Treatment of Papulopustular Rosacea. A Randomized Double-Blind Placebo-Controlled Study. Dermatology 2002, 205, 265–270. [Google Scholar] [CrossRef]
- Del Rosso, J.Q.; Webster, G.F.; Jackson, M.; Rendon, M.; Rich, P.; Torok, H.; Bradshaw, M. Two Randomized Phase III Clinical Trials Evaluating Anti-Inflammatory Dose Doxycycline (40-Mg Doxycycline, USP Capsules) Administered Once Daily for Treatment of Rosacea. J. Am. Acad. Dermatol. 2007, 56, 791–802. [Google Scholar] [CrossRef]
- Sbidian, E.; Vicaut, É.; Chidiack, H.; Anselin, E.; Cribier, B.; Dréno, B.; Chosidow, O. A Randomized-Controlled Trial of Oral Low-Dose Isotretinoin for Difficult-To-Treat Papulopustular Rosacea. J. Investig. Dermatol. 2016, 136, 1124–1129. [Google Scholar] [CrossRef]
- Two, A.M.; Wu, W.; Gallo, R.L.; Hata, T.R. Rosacea: Part II. Topical and Systemic Therapies in the Treatment of Rosacea. J. Am. Acad. Dermatol. 2015, 72, 761–760; quiz 771–772. [Google Scholar] [CrossRef]
- Reinholz, M.; Tietze, J.K.; Kilian, K.; Schaller, M.; Schöfer, H.; Lehmann, P.; Zierhut, M.; Klövekorn, W.; Ruzicka, T.; Schauber, J. Rosacea—S1 Guideline. J. Dtsch. Dermatol. Ges. 2013, 11, 768–780. [Google Scholar] [CrossRef]
- Asai, Y.; Tan, J.; Baibergenova, A.; Barankin, B.; Cochrane, C.L.; Humphrey, S.; Lynde, C.W.; Marcoux, D.; Poulin, Y.; Rivers, J.K.; et al. Canadian Clinical Practice Guidelines for Rosacea. J. Cutan. Med. Surg. 2016, 20, 432–445. [Google Scholar] [CrossRef]
- Salam, M.A.; Al-Amin, M.Y.; Salam, M.T.; Pawar, J.S.; Akhter, N.; Rabaan, A.A.; Alqumber, M.A.A. Antimicrobial Resistance: A Growing Serious Threat for Global Public Health. Healthcare 2023, 11, 1946. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Wang, B.; Zhang, X.; Zhang, J.; Zhang, H.; Liu, X.; Gao, Z.; Yu, Z. The Spread of Antibiotic Resistance to Humans and Potential Protection Strategies. Ecotoxicol. Environ. Saf. 2023, 254, 114734. [Google Scholar] [CrossRef] [PubMed]
- Urban-Chmiel, R.; Marek, A.; Stępień-Pyśniak, D.; Wieczorek, K.; Dec, M.; Nowaczek, A.; Osek, J. Antibiotic Resistance in Bacteria—A Review. Antibiotics 2022, 11, 1079. [Google Scholar] [CrossRef]
- Akram, F.; Imtiaz, M.; Haq, I. ul Emergent Crisis of Antibiotic Resistance: A Silent Pandemic Threat to 21st Century. Microb. Pathog. 2023, 174, 105923. [Google Scholar] [CrossRef]
- Miklasińska-Majdanik, M.; Kępa, M.; Wojtyczka, R.D.; Idzik, D.; Wąsik, T.J. Phenolic Compounds Diminish Antibiotic Resistance of Staphylococcus Aureus Clinical Strains. Int. J. Environ. Res. Public Health 2018, 15, 2321. [Google Scholar] [CrossRef]
- Vuong, Q.V. Epidemiological Evidence Linking Tea Consumption to Human Health: A Review. Crit. Rev. Food Sci. Nutr. 2014, 54, 523–536. [Google Scholar] [CrossRef]
- Dell’Annunziata, F.; Cometa, S.; Della Marca, R.; Busto, F.; Folliero, V.; Franci, G.; Galdiero, M.; De Giglio, E.; De Filippis, A. In Vitro Antibacterial and Anti-Inflammatory Activity of Arctostaphylos Uva-Ursi Leaf Extract against Cutibacterium acnes. Pharmaceutics 2022, 14, 1952. [Google Scholar] [CrossRef] [PubMed]
- Zöngür, A. Antimicrobial, Antioxidant and Cytotoxic Effects of Essential Oil, Fatty Acids and Bioactive Compounds of Beta vulgaris var. crassa (Fodder Beet). Indian. J. Microbiol. 2024, 64, 719–731. [Google Scholar] [CrossRef]
- Krzemińska, B.; Dybowski, M.P.; Klimek, K.; Typek, R.; Miazga-Karska, M.; Dos Santos Szewczyk, K. The Anti-Acne Potential and Chemical Composition of Two Cultivated Cotoneaster Species. Cells 2022, 11, 367. [Google Scholar] [CrossRef]
- Kim, S.; Park, T.H.; Kim, W.I.; Park, S.; Kim, J.H.; Cho, M.K. The Effects of Green Tea on Acne Vulgaris: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Phytother. Res. 2021, 35, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Kurutas, E.B. The Importance of Antioxidants Which Play the Role in Cellular Response against Oxidative/Nitrosative Stress: Current State. Nutr. J. 2016, 15, 71. [Google Scholar] [CrossRef] [PubMed]
- Hoskin, D.W.; Coombs, M.R.P. Editorial: Immune Modulation by Flavonoids. Front. Immunol. 2022, 13, 899577. [Google Scholar] [CrossRef]
- Sun, Q.; Liu, Q.; Zhou, X.; Wang, X.; Li, H.; Zhang, W.; Yuan, H.; Sun, C. Flavonoids Regulate Tumor-Associated Macrophages—From Structure-Activity Relationship to Clinical Potential (Review). Pharmacol. Res. 2022, 184, 106419. [Google Scholar] [CrossRef]
- Oh, Y.; Hwang, H.J.; Yang, H.; Kim, J.H.; Park, J.H.Y.; Kim, J.-E.; Lee, K.W. Orobol, A Derivative of Genistein, Inhibits Heat-Killed Propionibacterium acnes-Induced Inflammation in HaCaT Keratinocytes. J. Microbiol. Biotechnol. 2020, 30, 1379–1386. [Google Scholar] [CrossRef] [PubMed]
- Alkufeidy, R.M.; Ameer Altuwijri, L.; Aldosari, N.S.; Alsakabi, N.; Dawoud, T.M. Antimicrobial and Synergistic Properties of Green Tea Catechins against Microbial Pathogens. J. King Saud. Univ. Sci. 2024, 36, 103277. [Google Scholar] [CrossRef]
- Yoon, J.Y.; Kwon, H.H.; Min, S.U.; Thiboutot, D.M.; Suh, D.H. Epigallocatechin-3-Gallate Improves Acne in Humans by Modulating Intracellular Molecular Targets and Inhibiting P. acnes. J. Investig. Dermatol. 2013, 133, 429–440. [Google Scholar] [CrossRef]
- Lim, H.-J.; Kang, S.-H.; Song, Y.-J.; Jeon, Y.-D.; Jin, J.-S. Inhibitory Effect of Quercetin on Propionibacterium acnes-Induced Skin Inflammation. Int. Immunopharmacol. 2021, 96, 107557. [Google Scholar] [CrossRef]
- Kim, S.; Oh, S.; Noh, H.B.; Ji, S.; Lee, S.H.; Koo, J.M.; Choi, C.W.; Jhun, H.P. In Vitro Antioxidant and Anti-Propionibacterium acnes Activities of Cold Water, Hot Water, and Methanol Extracts, and Their Respective Ethyl Acetate Fractions, from Sanguisorba officinalis L. Roots Mol. 2018, 23, 3001. [Google Scholar] [CrossRef]
- Coenye, T.; Brackman, G.; Rigole, P.; De Witte, E.; Honraet, K.; Rossel, B.; Nelis, H.J. Eradication of Propionibacterium acnes Biofilms by Plant Extracts and Putative Identification of Icariin, Resveratrol and Salidroside as Active Compounds. Phytomedicine 2012, 19, 409–412. [Google Scholar] [CrossRef]
- Zhao, P.; Zhang, Y.; Deng, H.; Meng, Y. Antibacterial Mechanism of Apple Phloretin on Physiological and Morphological Properties of Listeria monocytogenes. Food Sci. Technol. 2021, 42, e55120. [Google Scholar] [CrossRef]
- Birru, R.L.; Bein, K.; Bondarchuk, N.; Wells, H.; Lin, Q.; Di, Y.P.; Leikauf, G.D. Antimicrobial and Anti-Inflammatory Activity of Apple Polyphenol Phloretin on Respiratory Pathogens Associated With Chronic Obstructive Pulmonary Disease. Front. Cell. Infect. Microbiol. 2021, 11, 652944. [Google Scholar] [CrossRef] [PubMed]
- Barreca, D.; Bellocco, E.; Laganà, G.; Ginestra, G.; Bisignano, C. Biochemical and Antimicrobial Activity of Phloretin and Its Glycosilated Derivatives Present in Apple and Kumquat. Food Chem. 2014, 160, 292–297. [Google Scholar] [CrossRef]
- Kum, H.; Roh, K.-B.; Shin, S.; Jung, K.; Park, D.; Jung, E. Evaluation of anti-acne properties of phloretin in vitro and in vivo. Int. J. Cosmet. Sci. 2016, 38, 85–92. [Google Scholar] [CrossRef]
- Cheon, D.; Kim, J.; Jeon, D.; Shin, H.-C.; Kim, Y. Target Proteins of Phloretin for Its Anti-Inflammatory and Antibacterial Activities Against Propionibacterium acnes-Induced Skin Infection. Molecules 2019, 24, 1319. [Google Scholar] [CrossRef]
- Yang, G.; Lee, H.E.; Yeon, S.H.; Kang, H.C.; Cho, Y.-Y.; Lee, H.S.; Zouboulis, C.C.; Han, S.-H.; Lee, J.-H.; Lee, J.Y. Licochalcone A Attenuates Acne Symptoms Mediated by Suppression of NLRP3 Inflammasome. Phytother. Res. 2018, 32, 2551–2559. [Google Scholar] [CrossRef] [PubMed]
- Muddathir, A.M.; Yamauchi, K.; Mitsunaga, T. Anti-Acne Activity of Tannin-Related Compounds Isolated from Terminalia Laxiflora. J. Wood Sci. 2013, 59, 426–431. [Google Scholar] [CrossRef]
- You, J.; Ji, H.; Roh, K.-B.; Cho, E.; Chajra, H.; Frechet, M.; Park, D.; Jung, E. Anti-Acne Effects of Castanea Crenata Bur Extract and Identification of Active Compound. Appl. Biol. Chem. 2022, 65, 12. [Google Scholar] [CrossRef]
- Piazza, S.; Martinelli, G.; Maranta, N.; Pozzoli, C.; Fumagalli, M.; Nicolaci, V.; Sonzogni, E.; Colombo, L.; Sangiovanni, E.; Dell’Agli, M. Investigation into the Anti-Acne Effects of Castanea Sativa Mill Leaf and Its Pure Ellagitannin Castalagin in HaCaT Cells Infected with Cutibacterium acnes. Int. J. Mol. Sci. 2024, 25, 4764. [Google Scholar] [CrossRef]
- Lee, C.-J.; Chen, L.-G.; Liang, W.-L.; Wang, C.-C. Multiple Activities of Punica Granatum Linne against Acne vulgaris. Int. J. Mol. Sci. 2017, 18, 141. [Google Scholar] [CrossRef]
- Taylor, E.J.M.; Yu, Y.; Champer, J.; Kim, J. Resveratrol Demonstrates Antimicrobial Effects Against Propionibacterium acnes In Vitro. Dermatol. Ther. 2014, 4, 249–257. [Google Scholar] [CrossRef]
- Wei, Z.; Chen, G.; Hu, T.; Mo, X.; Hou, X.; Cao, K.; Wang, L.; Pan, Z.; Wu, Q.; Li, X.; et al. Resveratrol Ameliorates Lipid Accumulation and Inflammation in Human SZ95 Sebocytes via the AMPK Signaling Pathways in Vitro. J. Dermatol. Sci. 2021, 103, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.; Fang, F.; Sun, D.; Yang, S.; Zhang, X.; Yu, X.; Yang, L. Piceatannol Inhibits P. acnes–Induced Keratinocyte Proliferation and Migration by Downregulating Oxidative Stress and the Inflammatory Response. Inflammation 2020, 43, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Al-Khayri, J.M.; Mascarenhas, R.; Harish, H.M.; Gowda, Y.; Lakshmaiah, V.V.; Nagella, P.; Al-Mssallem, M.Q.; Alessa, F.M.; Almaghasla, M.I.; Rezk, A.A.-S. Stilbenes, a Versatile Class of Natural Metabolites for Inflammation—An Overview. Molecules 2023, 28, 3786. [Google Scholar] [CrossRef]
- Dos Santos, Z.M.Q.; Dos Santos, M.Q.; Zancanaro, V.; Bellaver, E.H.; Nardi, G.M.; Gelinski, J.M.L.; Locatelli, C. Topical Application of Phenolic Compounds Suppresses Propionibacterium acnes-Induced Inflammatory Responses in Mice with Ear Edema. Naunyn Schmiedebergs Arch. Pharmacol. 2019, 392, 529–540. [Google Scholar] [CrossRef] [PubMed]
- Kasprzak-Drozd, K.; Niziński, P.; Hawrył, A.; Gancarz, M.; Hawrył, D.; Oliwa, W.; Pałka, M.; Markowska, J.; Oniszczuk, A. Potential of Curcumin in the Management of Skin Diseases. Int. J. Mol. Sci. 2024, 25, 3617. [Google Scholar] [CrossRef] [PubMed]
- Bojar, R.A.; Holland, K.T. Acne and Propionibacterium acnes. Clin. Dermatol. 2004, 22, 375–379. [Google Scholar] [CrossRef]
- Chivot, M. Retinoid Therapy for Acne. A Comparative Review. Am. J. Clin. Dermatol. 2005, 6, 13–19. [Google Scholar] [CrossRef]
- Sato, T.; Imai, N.; Akimoto, N.; Sakiguchi, T.; Kitamura, K.; Ito, A. Epidermal Growth Factor and 1alpha,25-Dihydroxyvitamin D3 Suppress Lipogenesis in Hamster Sebaceous Gland Cells in Vitro. J. Investig. Dermatol. 2001, 117, 965–970. [Google Scholar] [CrossRef]
- Sato, T.; Takahashi, A.; Kojima, M.; Akimoto, N.; Yano, M.; Ito, A. A Citrus Polymethoxy Flavonoid, Nobiletin Inhibits Sebum Production and Sebocyte Proliferation, and Augments Sebum Excretion in Hamsters. J. Investig. Dermatol. 2007, 127, 2740–2748. [Google Scholar] [CrossRef]
- Akitomo, Y.; Akamatsu, H.; Okano, Y.; Masaki, H.; Horio, T. Effects of UV Irradiation on the Sebaceous Gland and Sebum Secretion in Hamsters. J. Dermatol. Sci. 2003, 31, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Suh, D.H.; Kwon, T.E.; Youn, J.I. Changes of Comedonal Cytokines and Sebum Secretion after UV Irradiation in Acne Patients. Eur. J. Dermatol. 2002, 12, 139–144. [Google Scholar] [PubMed]
- Vowels, B.R.; Yang, S.; Leyden, J.J. Induction of Proinflammatory Cytokines by a Soluble Factor of Propionibacterium acnes: Implications for Chronic Inflammatory Acne. Infect. Immun. 1995, 63, 3158–3165. [Google Scholar] [CrossRef] [PubMed]
- Mirza, M.A.; Mahmood, S.; Hilles, A.R.; Ali, A.; Khan, M.Z.; Zaidi, S.A.A.; Iqbal, Z.; Ge, Y. Quercetin as a Therapeutic Product: Evaluation of Its Pharmacological Action and Clinical Applications-A Review. Pharmaceuticals 2023, 16, 1631. [Google Scholar] [CrossRef]
- Ruijters, E.J.B.; Haenen, G.R.M.M.; Weseler, A.R.; Bast, A. The Anti-Inflammatory Efficacy of Dexamethasone Is Protected by (−)-Epicatechin. Pharma Nutr. 2014, 2, 47–52. [Google Scholar] [CrossRef]
- Ruan, S.; Xiang, S.; Wu, W.; Cao, S.; Du, Q.; Wang, Z.; Chen, T.; Shen, Q.; Liu, L.; Chen, H.; et al. Potential Role of mTORC1 and the PI3K-Akt Pathway in Anti-Acne Properties of Licorice Flavonoids. J. Funct. Foods 2020, 70, 103968. [Google Scholar] [CrossRef]
- Ruan, S.-F.; Hu, Y.; Wu, W.-F.; Du, Q.-Q.; Wang, Z.-X.; Chen, T.-T.; Shen, Q.; Liu, L.; Jiang, C.-P.; Li, H.; et al. Explore the Anti-Acne Mechanism of Licorice Flavonoids Based on Metabonomics and Microbiome. Front. Pharmacol. 2022, 13, 832088. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.-C.; Tsai, T.-H.; Huang, C.-J.; Li, Y.-Y.; Chyuan, J.-H.; Chuang, L.-T.; Tsai, P.-J. Inhibitory Effects of Wild Bitter Melon Leaf Extract on Propionibacterium acnes-Induced Skin Inflammation in Mice and Cytokine Production in Vitro. Food Funct. 2015, 6, 2550–2560. [Google Scholar] [CrossRef]
- Higaki, S.; Toyomoto, T.; Morohashi, M. Seijo-Bofu-to, Jumi-Haidoku-to and Toki-Shakuyaku-San Suppress Rashes and Incidental Symptoms in Acne Patients. Drugs Exp. Clin. Res. 2002, 28, 193–196. [Google Scholar]
- Matsumoto, T.; Matsubara, Y.; Mizuhara, Y.; Sekiguchi, K.; Koseki, J.; Tsuchiya, K.; Nishimura, H.; Watanabe, J.; Kaneko, A.; Maemura, K.; et al. Plasma Pharmacokinetics of Polyphenols in a Traditional Japanese Medicine, Jumihaidokuto, Which Suppresses Propionibacterium acnes-Induced Dermatitis in Rats. Molecules 2015, 20, 18031–18046. [Google Scholar] [CrossRef]
- Yang, X.; Wang, H.; Li, T.; Chen, L.; Zheng, B.; Liu, R.H. Nobiletin Delays Aging and Enhances Stress Resistance of Caenorhabditis elegans. Int. J. Mol. Sci. 2020, 21, 341. [Google Scholar] [CrossRef] [PubMed]
- Nishimuro, H.; Ohnishi, H.; Sato, M.; Ohnishi-Kameyama, M.; Matsunaga, I.; Naito, S.; Ippoushi, K.; Oike, H.; Nagata, T.; Akasaka, H.; et al. Estimated Daily Intake and Seasonal Food Sources of Quercetin in Japan. Nutrients 2015, 7, 2345–2358. [Google Scholar] [CrossRef] [PubMed]
- Działo, M.; Mierziak, J.; Korzun, U.; Preisner, M.; Szopa, J.; Kulma, A. The Potential of Plant Phenolics in Prevention and Therapy of Skin Disorders. Int. J. Mol. Sci. 2016, 17, 160. [Google Scholar] [CrossRef]
- Domingo, D.S.; Camouse, M.M.; Hsia, A.H.; Matsui, M.; Maes, D.; Ward, N.L.; Cooper, K.D.; Baron, E.D. Anti-Angiogenic Effects of Epigallocatechin-3-Gallate in Human Skin. Int. J. Clin. Exp. Pathol. 2010, 3, 705–709. [Google Scholar]
- Rigopoulos, D.; Kalogeromitros, D.; Gregoriou, S.; Pacouret, J.; Koch, C.; Fisher, N.; Bachmann, K.; Brown, M.; Schwarz, E.; Camel, E.; et al. Randomized Placebo-Controlled Trial of a Flavonoid-Rich Plant Extract-Based Cream in the Treatment of Rosacea. J. Eur. Acad. Dermatol. Venereol. 2005, 19, 564–568. [Google Scholar] [CrossRef]
- Habeshian, K.A.; Cohen, B.A. Current Issues in the Treatment of Acne Vulgaris. Pediatrics 2020, 145 (Suppl. S2), 225–230. [Google Scholar] [CrossRef] [PubMed]
- Amer, S.S.; Nasr, M.; Abdel-Aziz, R.T.A.; Moftah, N.H.; El Shaer, A.; Polycarpou, E.; Mamdouh, W.; Sammour, O. Cosm-Nutraceutical Nanovesicles for Acne Treatment: Physicochemical Characterization and Exploratory Clinical Experimentation. Int. J. Pharm. 2020, 577, 119092. [Google Scholar] [CrossRef]
- Ezike, T.C.; Okpala, U.S.; Onoja, U.L.; Nwike, C.P.; Ezeako, E.C.; Okpara, O.J.; Okoroafor, C.C.; Eze, S.C.; Kalu, O.L.; Odoh, E.C.; et al. Advances in drug delivery systems, challenges and future directions. Heliyon 2023, 9, e17488. [Google Scholar] [CrossRef]
- Lu, P.H.; Hsu, C.H. Does Supplementation with Green Tea Extract Improve Acne in Post-Adolescent Women? A Randomized, Double-Blind, and Placebo-Controlled Clinical Trial. Complement. Ther. Med. 2016, 25, 159–163. [Google Scholar] [CrossRef]
- Drake, L.; Reyes-Hadsall, S.; Barbieri, J.S.; Mostaghimi, A. New Developments in Topical Acne Therapy. Am. J. Clin. Dermatol. 2022, 23, 125–136. [Google Scholar] [CrossRef]
- Chutoprapat, R.; Kopongpanich, P.; Chan, L.W. A Mini-Review on Solid Lipid Nanoparticles and Nanostructured Lipid Carriers: Topical Delivery of Phytochemicals for the Treatment of Acne Vulgaris. Molecules 2022, 27, 3460. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.-H.; Kim, I.-H.; Seo, J.-J. In Vitro Activity of Kaempferol Isolated from the Impatiens Balsamina Alone and in Combination with Erythromycin or Clindamycin against Propionibacterium acnes. J. Microbiol. 2007, 45, 473–477. [Google Scholar] [PubMed]
- Boonchaya, P.; Rojhirunsakool, S.; Kamanamool, N.; Khunkhet, S.; Yooyongsatit, S.; Udompataikul, M.; Taweechotipatr, M. Minimum Contact Time of 1.25%, 2.5%, 5%, and 10% Benzoyl Peroxide for a Bactericidal Effect Against Cutibacterium acnes. Clin. Cosmet. Investig. Dermatol. 2022, 15, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-K.; Kim, N.; Lim, Y.-H. Evaluation of the Antibacterial Activity of Rhapontigenin Produced from Rhapontin by Biotransformation against Propionibacterium acnes. J. Microbiol. Biotechnol. 2010, 20, 82–87. [Google Scholar] [CrossRef]
- Lambrechts, I.A.; Thipe, V.C.; Katti, K.V.; Mandiwana, V.; Kalombo, M.L.; Ray, S.S.; Rikhotso, R.; Janse van Vuuren, A.; Esmear, T.; Lall, N. Targeting Acne Bacteria and Wound Healing In Vitro Using Plectranthus Aliciae, Rosmarinic Acid, and Tetracycline Gold Nanoparticles. Pharmaceuticals 2022, 15, 933. [Google Scholar] [CrossRef] [PubMed]
| Compound/Extract | Natural Sources | Study Model | Dosage | Results/Effect | References |
|---|---|---|---|---|---|
| Acne vulgaris | |||||
| Nobiletin | Citrus fruits (mandarin oranges, tangerines, oranges, grapefruits) | Auricles of 5-week-old male golden hamsters | Topical application (solution) 1% and 2% (1.25 and 2.5 µmol) | Size of sebaceous glands ↓ TG ↓ | [181,192] |
| Nobiletin | Citrus fruits (mandarin oranges, tangerines, oranges, grapefruits) | Auricles of 3-week-old male golden hamsters | Topical application (solution) 2% (2.5 µmol) | Sebum accumulation in sebaceous glands and ducts (after the UVB-irradiated) ↓ | [181,192] |
| Quercetin | Tea, onions, apples, lettuce, broccoli | Ears of 6-week-old male BALB/c mice (n = 8/group) | Topical application (solution) 1 and 10 µmol | Ear thickness ↓ Inflammation ↓ Erythema ↓ Swelling ↓ Inflammatory cells ↓ | [159,193] |
| Licorice flavonoids | Licorice (Glycyrrhiza glabra L.) | Back skin of 6- to 7-week-old male Sprague-Dawley rats (n = 8/group) | Topical application (drug gel patches) 67.3 mg/g | Size of sebaceous glands ↓ Hyperkeratinization ↓ Infiltration of inflammatory cells ↓ Acne lesions ↓ | [187] |
| Licorice flavonoids | Licorice (Glycyrrhiza glabra L.) | Back skin of 6- to 7-week-old male Sprague-Dawley rats (n = 8/group) | Topical application (drug gel patches) 67.3 mg/g | Hyperkeratinization ↓ TNF-α ↓ IL-8 ↓ Metabolic balance Microbial balance | [188] |
| Total phenolic extract of Momordica charantia L. leaf | Momordica charantia L. | Ears of 8-old male ICR mice (n = 5/group) | Intradermal injection (solution) 0.5 mg per site | Swelling ↓ Ear weight ↓ Ear thickness ↓ Microabscess ↓ | [189] |
| Total phenolic extract of Momordica charantia L. leaf | Momordica charantia L. | Ears of 8-old male ICR mice (n = 5/group) | Intradermal injection (solution) 0.5 mg per site | IL-1β+ ↓ Leukocyte ↓ Neutrophil ↓ Microabscess ↓ | [189] |
| Jumihaidokuto | Pharmaceutical-grade traditional Japanese (kampo) medicine | Ears of 7- to 8-week-old male Sprague-Dawley rats | Oral administration (solution) 0.5 g/10 mL/kg x2 | Ear thickness ↓ Inflammation ↓ | [191] |
| Compound/Extract | Natural Sources | Study Model | Dosage | Results/Effect | References |
|---|---|---|---|---|---|
| Rosacea | |||||
| EGCG | Tea, chocolate, red wine | Volunteers with rosacea (n = 40) | Topical application (cream) 2.5% w/w | VEGF expression ↓ HIF-1α expression ↓ Telangiectasia ↓ | [195] |
| Chrysanthellum indicum DC. extract | Chrysanthellum indicum DC. | Patients with moderate rosacea (n = 125) | Topical application (cream) 1.0% w/w | Erythema ↓ Overall rosacea severity ↓ | [196] |
| Acne vulgaris | |||||
| EGCG | Tea, chocolate, red wine | Patients with Acne vulgaris (n = 35) | Topical application (solution) 1 and 5 v/v | Inflammatory response ↓ NF-κB ↓ AP-1 ↓ Acne lesions ↓ | [158] |
| Quercetin (aspasomal formulation) | Tea, onions, apples, lettuce, broccoli | Patients with Acne vulgaris (n = 20) | Topical application (thin-layer film containing 100 µg of quercetin) | Inflammatory lesions ↓ Comedones ↓ Total lesions ↓ Antioxidant activity ↑ Activity against Propionibacterium acnes ↑ | [193,198] |
| Green tea extract (57.12% w/w of EGCG) | Camelia sinensis (L.) Kuntze | Patients with Acne vulgaris (n = 80) | Oral supplementation (1500 mg, 3 capsules per day) | Inflammatory lesions count on the nose, forehead, cheek, periorally and on the chin ↓ Total lesions count on the forehead and cheek ↓ | [200] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koch, W.; Zagórska, J.; Michalak-Tomczyk, M.; Karav, S.; Wawruszak, A. Plant Phenolics in the Prevention and Therapy of Acne: A Comprehensive Review. Molecules 2024, 29, 4234. https://doi.org/10.3390/molecules29174234
Koch W, Zagórska J, Michalak-Tomczyk M, Karav S, Wawruszak A. Plant Phenolics in the Prevention and Therapy of Acne: A Comprehensive Review. Molecules. 2024; 29(17):4234. https://doi.org/10.3390/molecules29174234
Chicago/Turabian StyleKoch, Wojciech, Justyna Zagórska, Magdalena Michalak-Tomczyk, Sercan Karav, and Anna Wawruszak. 2024. "Plant Phenolics in the Prevention and Therapy of Acne: A Comprehensive Review" Molecules 29, no. 17: 4234. https://doi.org/10.3390/molecules29174234






