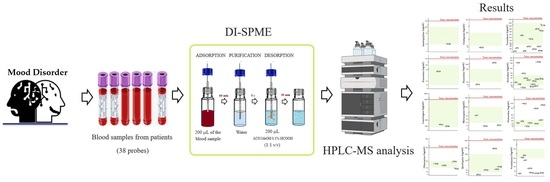
Direct Immersion–Solid Phase Microextraction for Therapeutic Drug Monitoring of Patients with Mood Disorders
Abstract
1. Introduction
2. Results and Discussion
2.1. I-SPME Extraction
2.2. Validation Process
2.3. Analysis of Patient Samples
3. Materials and Methods
3.1. Chemicals and Laboratory Equipment
3.2. The HPLC-MS Apparatus, Conditions, and Software
3.3. DI-SPME Procedure
3.3.1. Conditioning
3.3.2. Adsorption
3.3.3. Purification
3.3.4. Desorption
3.3.5. Fiber Cleaning
3.4. Validation Procedure
3.5. Sample Collection
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- López-Muñoz, F.; Shen, W.W.; Docon, P.; Romero, A.; Álamo, C. A history of the pharmacological treatment of bipolar disorder. Int. J. Mol. Sci. 2018, 19, 2143. [Google Scholar] [CrossRef] [PubMed]
- Gorostowicz, A.; Siwek, M. Difficulties in the diagnosis of bipolar affective disorder. J. Psychiatry Clin. Psychol. 2018, 18, 61–73. [Google Scholar] [CrossRef]
- Gutiérrez-Rojas, L.; Porras-Segovia, A.; Dunne, H.; Andrade-González, N.; Cervilla, J.A. Prevalence and correlates of major depressive disorder: A systematic review. Braz. J. Psychiatry 2020, 42, 657–672. [Google Scholar] [CrossRef] [PubMed]
- Piacentino, D.; Bianchi, E.; De Donatis, D.; Florio, V.; Conca, A. Therapeutic Drug Monitoring of Antidepressants: An Underused but Potentially Valuable Tool in Primary Care. Front. Psychiatry. 2022, 13, 867840. [Google Scholar] [CrossRef]
- Kang, J.S.; Lee, M.H. Overview of therapeutic drug monitoring. Korean J. Intern. Med. 2009, 24, 867840. [Google Scholar] [CrossRef] [PubMed]
- Sasajima, Y.; Lim, L.W.; Takeuchi, T.; Suenami, K.; Sato, K.; Takekoshi, Y. Simultaneous determination of antidepressants by non-aqueous capillary electrophoresis-time of flight mass spectrometry. J. Chromatogr. A 2010, 1217, 7598–7604. [Google Scholar] [CrossRef]
- Moretti, M.; Freni, F.; Valentini, B.; Vignali, C.; Groppi, A.; Visonà, S.D.; Osculati, A.M.M.; Morini, L. Determination of antidepressants and antipsychotics in dried blood spots (DBSs) collected from post-mortem samples and evaluation of the stability over three months. Molecules 2019, 24, 3636. [Google Scholar] [CrossRef]
- Majda, A.; Wietecha-Posłuszny, R.; Świądro, M.; Mrochem, K.; Kościelniak, P. Dried blood spots sampling in case samples deprived of hematocrit level information—Investigation and calculation strategy. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2019, 1124, 308–312. [Google Scholar] [CrossRef]
- Lee, H.; Park, Y.; Jo, J.; In, S.; Park, Y.; Kim, E.; Pyo, J.; Choe, S. Analysis of benzodiazepines and their metabolites using DBS cards and LC-MS/MS. Forensic Sci. Int. 2015, 255, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Pawliszyn, J. Chapter 13 Solid Phase Microextraction. Compr. Anal. Chem. 2002, 37, 389–477. [Google Scholar]
- Lord, H.; Bojko, B. Drug Analysis by SPME; Elsevier Inc.: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Majda, A.; Mrochem, K.; Wietecha-Posłuszny, R.; Zapotoczny, S.; Zawadzki, M. Fast and efficient analyses of the post-mortem human blood and bone marrow using DI-SPME/LC-TOFMS method for forensic medicine purposes. Talanta 2020, 209, 120533. [Google Scholar] [CrossRef] [PubMed]
- Althoff, M.A.; Bertsch, A.; Metzulat, M.; Klapötke, T.M.; Karaghiosoff, K.L. Application of headspace and direct immersion solid-phase microextraction in the analysis of organothiophosphates related to the Chemical Weapons Convention from water and complex matrices. Talanta 2017, 174, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Fucci, N.; De Giovanni, N.; Chiarotti, M. Simultaneous detection of some drugs of abuse in saliva samples by SPME technique. Forensic Sci. Int. 2003, 134, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Kloskowski, A.; Pilarczyk, M. Membrane Solid-Phase Microextraction—A New Concept of Sorbent Preparation. Anal. Chem. 2009, 81, 7363–7367. [Google Scholar] [CrossRef] [PubMed]
- Snow, N.H. Solid-phase micro-extraction of drugs from biological matrices. J. Chromatogr. A 2000, 885, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Gałuszka, A.; Migaszewski, Z.; Namiesnik, J. The 12 principles of green analytical chemistry and the SIGNIFICANCE mnemonic of green analytical practices. TrAC Trends Anal. Chem. 2013, 50, 78–84. [Google Scholar] [CrossRef]
- European Medicines Agency. Guideline on Bioanalytical Method Validation; European Medicines Agency: Amsterdam, The Netherlands, 2011; Volume 44, pp. 1–23.




| Drug Abbreviation | [M + H]+ | tR [min] in Spiked Blood | Deuterated Analogue | [M + H]+ | tR [min] in Spiked Blood |
|---|---|---|---|---|---|
| Tricyclic antidepressants | |||||
| AMI | 278.1903 ± 0.01 | 6.44 ± 0.02 | AMI-d3 | 281.2092 ± 0.01 | 6.26 ± 0.01 |
| NORT | 264.1747 ± 0.01 | 6.29 ± 0.02 | AMI-d3 | 281.2092 ± 0.01 | 6.26 ± 0.01 |
| IMI | 281.2012 ± 0.01 | 6.26 ± 0.01 | VEN-d6 | 284.2491 ± 0.01 | 3.83 ± 0.03 |
| DEZ | 267.1856 ± 0.01 | 6.10 ± 0.02 | AMI-d3 | 281.2092 ± 0.01 | 6.26 ± 0.01 |
| CLOM | 315.1622 ± 0.01 | 7.10 ± 0.03 | FLUX-d6 | 316.1789 ± 0.01 | 6.65 ± 0.02 |
| Selective serotonin reuptake inhibitors | |||||
| CIT | 325.1722 ± 0.01 | 5.68 ± 0.02 | PAR-d6 | 336.1877 ± 0.01 | 6.16 ± 0.02 |
| FLU | 310.1413 ± 0.01 | 6.67 ± 0.02 | FLU-d6 | 316.1789 ± 0.01 | 6.65 ± 0.02 |
| FLUV | 319.1621 ± 0.01 | 6.04 ± 0.02 | FLU-d6 | 316.1789 ± 0.01 | 6.65 ± 0.02 |
| PAR | 330.1494 ± 0.01 | 6.18 ± 0.03 | PAR-d6 | 336.1877 ± 0.01 | 6.15 ± 0.02 |
| SER | 306.0807 ± 0.01 | 6.93 ± 0.02 | FLU-d6 | 316.1789 ± 0.01 | 6.64 ± 0.02 |
| Serotonin and norepinephrine reuptake inhibitors | |||||
| DUL | 298.1256 ± 0.01 | 6.38 ± 0.02 | VEN-d6 | 284.2491 ± 0.01 | 3.81 ± 0.03 |
| MIR | 266.1667 ± 0.01 | 2.03 ± 0.02 | AMI-d3 | 281.2092 ± 0.01 | 6.26 ± 0.01 |
| VEN | 278.2110 ± 0.01 | 3.83 ± 0.03 | VEN-d6 | 284.2491 ± 0.01 | 3.80 ± 0.03 |
| TRA | 372.1605 ± 0.01 | 4.91 ± 0.03 | PAR-d6 | 336.1877 ± 0.01 | 6.15 ± 0.02 |
| Anticonvulsants and atypical neuroleptics | |||||
| ARI | 448.1548 ± 0.01 | 6.78 ± 0.02 | PAR-d6 | 336.1877 ± 0.01 | 6.16 ± 0.02 |
| CBZ | 237.1021 ± 0.01 | 5.40 ± 0.02 | CBZ-d10 | 247.1650 ± 0.01 | 5.34 ± 0.03 |
| LAM | 256.0165 ± 0.01 | 1.83 ± 0.02 | CBZ-d10 | 247.1650 ± 0.01 | 5.34 ± 0.03 |
| QUET | 384.1733 ± 0.01 | 4.91 ± 0.03 | PAR-d6 | 336.1877 ± 0.01 | 6.16 ± 0.02 |
| OLA | 313.1475 ± 0.01 | 0.87 ± 0.02 | FLU-d6 | 316.1789 ± 0.01 | 6.65 ± 0.02 |
| “Date rape drugs” | |||||
| FLUN | 314.0935 ± 0.05 | 6.63 ± 0.02 | FLU-d6 | 316.1789 ± 0.01 | 6.65 ± 0.02 |
| KET | 238.0993 ± 0.05 | 1.62 ± 0.03 | CBZ-d10 | 247.1650 ± 0.01 | 5.34 ± 0.03 |
| Parameters | AMI | CIT | FLU | PAR | SER | TRA | DUL | MIR | VEN | LAM | QUE | OLA |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Linearity [ng/mL] | LLOQ—300 | |||||||||||
| R2 | 0.9907 | 0.9966 | 0.9922 | 0.9979 | 0.9940 | 0.9937 | 0.9975 | 0.9904 | 0.9978 | 0.9950 | 0.9960 | 0.9985 |
| LLOQ [ng/mL] | 0.92 | 4.87 | 2.32 | 2.60 | 8.43 | 2.69 | 21.47 | 0.70 | 2.91 | 5.73 | 4.58 | 7.62 |
| LOD [ng/mL] | 0.18 | 0.97 | 0.46 | 0.52 | 1.69 | 0.54 | 4.29 | 0.14 | 0.58 | 0.37 | 0.92 | 1.52 |
| Precision [%] Intraday * | ||||||||||||
| 50 [ng/mL] | 12.55 | 10.23 | 8.44 | 16.61 | 5.80 | 9.20 | 6.04 | 19.60 | 3.47 | 7.54 | 16.24 | 10.94 |
| 150 [ng/mL] | 6.80 | 3.68 | 5.97 | 7.84 | 7.35 | 10.59 | 8.51 | 6.07 | 3.13 | 9.39 | 8.01 | 5.36 |
| 250 [ng/mL] | 5.27 | 6.14 | 12.38 | 13.85 | 11.08 | 13.38 | 11.04 | 8.31 | 9.53 | 1.85 | 12.62 | 13.41 |
| Precision [%] Interday ** | ||||||||||||
| 50 [ng/mL] | 19.05 | 19.05 | 3.34 | 17.85 | 13.57 | 11.74 | 10.03 | 16.94 | 8.84 | 16.85 | 18.89 | 16.47 |
| 150 [ng/mL] | 10.88 | 10.88 | 1.57 | 11.69 | 12.11 | 7.63 | 3.67 | 12.58 | 5.69 | 14.30 | 9.16 | 7.61 |
| 250 [ng/mL] | 12.48 | 12.48 | 7.34 | 12.46 | 7.85 | 7.48 | 11.59 | 10.17 | 5.05 | 11.70 | 5.60 | 12.84 |
| Matrix effect [%] | 7.54 | 4.58 | 6.02 | 8.15 | 9.02 | 8.51 | 6.41 | 4.99 | 2.46 | 7.54 | 7.32 | 3.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Świądro-Piętoń, M.; Dudek, D.; Wietecha-Posłuszny, R. Direct Immersion–Solid Phase Microextraction for Therapeutic Drug Monitoring of Patients with Mood Disorders. Molecules 2024, 29, 676. https://doi.org/10.3390/molecules29030676
Świądro-Piętoń M, Dudek D, Wietecha-Posłuszny R. Direct Immersion–Solid Phase Microextraction for Therapeutic Drug Monitoring of Patients with Mood Disorders. Molecules. 2024; 29(3):676. https://doi.org/10.3390/molecules29030676
Chicago/Turabian StyleŚwiądro-Piętoń, Magdalena, Dominika Dudek, and Renata Wietecha-Posłuszny. 2024. "Direct Immersion–Solid Phase Microextraction for Therapeutic Drug Monitoring of Patients with Mood Disorders" Molecules 29, no. 3: 676. https://doi.org/10.3390/molecules29030676
APA StyleŚwiądro-Piętoń, M., Dudek, D., & Wietecha-Posłuszny, R. (2024). Direct Immersion–Solid Phase Microextraction for Therapeutic Drug Monitoring of Patients with Mood Disorders. Molecules, 29(3), 676. https://doi.org/10.3390/molecules29030676