Intravascular Targets for Molecular Contrast-Enhanced Ultrasound Imaging
Abstract
:1. Introduction
2. Ultrasound Contrast Agents
2.1. Advantages and Disadvantages of Ultrasound Compared to Other Modalities
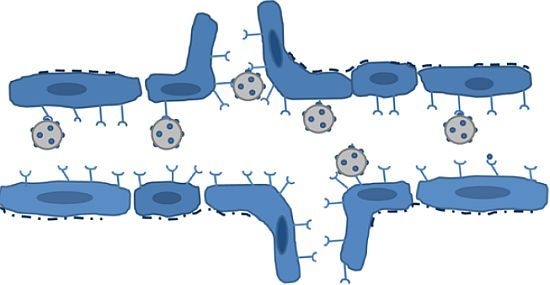
2.2. Requirements for Intravascular Targets in Ultrasound Imaging
3. Molecular Ultrasound Imaging of Cancer
3.1. VEGFR2
3.2. Integrins
3.3. Endoglin
3.4. Prostate-Specific Membrane Antigen
3.5. Inflammatory Markers
4. Therapy Monitoring in Cancer Using Molecular Contrast-Enhanced Ultrasound Imaging
5. Evaluation of Intravascular Biomarkers for Angiogenesis Using Targeted Microbubbles
6. Considerations for Evaluating Contrast Agent Performance
7. Summary and Outlook
References
- Feinstein, S.B.; Ten Cate, F.J.; Zwehl, W.; Ong, K.; Maurer, G.; Tei, C.; Shah, P.M.; Meerbaum, S.; Corday, E. Two-dimensional contrast echocardiography. I. In vitro development and quantitative analysis of echo contrast agents. J. Am. Coll. Cardiol 1984, 3, 14–20. [Google Scholar]
- Ten Cate, F.J.; Feinstein, S.; Zwehl, W.; Meerbaum, S.; Fishbein, M.; Shah, P.M.; Corday, E. Two-dimensional contrast echocardiography. II. Transpulmonary studies. J. Am. Coll. Cardiol 1984, 3, 21–27. [Google Scholar]
- Deshpande, N.; Needles, A.; Willmann, J.K. Molecular ultrasound imaging: Current status and future directions. Clin. Radiol 2010, 65, 567–581. [Google Scholar]
- Hansen, R.; Angelsen, B.A. Contrast imaging by non-overlapping dual frequency band transmit pulse complexes. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2011, 58, 290–297. [Google Scholar]
- Skotland, T.; Iversen, T.G.; Sandvig, K. New metal-based nanoparticles for intravenous use: Requirements for clinical success with focus on medical imaging. Nanomedicine 2010, 6, 730–737. [Google Scholar]
- Klibanov, A.L.; Rasche, P.T.; Hughes, M.S.; Wojdyla, J.K.; Galen, K.P.; Wible, J.H., Jr; Brandenburger, G.H. Detection of individual microbubbles of an ultrasound contrast agent: Fundamental and pulse inversion imaging. Acad. Radiol. 2002, 9, S279–S281. [Google Scholar]
- Chomas, J.E.; Dayton, P.; Allen, J.; Morgan, K.; Ferrara, K.W. Mechanisms of contrast agent destruction. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2001, 48, 232–248. [Google Scholar]
- Willmann, J.K.; Cheng, Z.; Davis, C.; Lutz, A.M.; Schipper, M.L.; Nielsen, C.H.; Gambhir, S.S. Targeted microbubbles for imaging tumor angiogenesis: Assessment of whole-body biodistribution with dynamic micro-PET in mice. Radiology 2008, 249, 212–219. [Google Scholar]
- Anderson, C.R.; Hu, X.; Zhang, H.; Tlaxca, J.; Decleves, A.E.; Houghtaling, R.; Sharma, K.; Lawrence, M.; Ferrara, K.W.; Rychak, J.J. Ultrasound molecular imaging of tumor angiogenesis with an integrin targeted microbubble contrast agent. Invest Radiol 2011, 46, 215–224. [Google Scholar]
- Barrett, T.; Brechbiel, M.; Bernardo, M.; Choyke, P.L. MRI of tumor angiogenesis. J. Magn. Reson. Imaging 2007, 26, 235–249. [Google Scholar]
- Battle, M.R.; Goggi, J.L.; Allen, L.; Barnett, J.; Morrison, M.S. Monitoring tumor response to antiangiogenic sunitinib therapy with 18F-fluciclatide, an 18F-labeled alphaVbeta3-integrin and alphaV beta5-integrin imaging agent. J. Nucl. Med 2011, 52, 424–430. [Google Scholar]
- Shi, J.; Wang, L.; Kim, Y.S.; Zhai, S.; Liu, Z.; Chen, X.; Liu, S. Improving tumor uptake and excretion kinetics of 99mTc-labeled cyclic arginine-glycine-aspartic (RGD) dimers with triglycine linkers. J. Med. Chem 2008, 51, 7980–7990. [Google Scholar]
- Von Wallbrunn, A.; Holtke, C.; Zuhlsdorf, M.; Heindel, W.; Schafers, M.; Bremer, C. In vivo imaging of integrin alpha v beta 3 expression using fluorescence-mediated tomography. Eur. J. Nucl. Med. Mol. Imaging 2007, 34, 745–754. [Google Scholar]
- Willmann, J.K.; Kimura, R.H.; Deshpande, N.; Lutz, A.M.; Cochran, J.R.; Gambhir, S.S. Targeted contrast-enhanced ultrasound imaging of tumor angiogenesis with contrast microbubbles conjugated to integrin-binding knottin peptides. J. Nucl. Med 2010, 51, 433–440. [Google Scholar]
- Skotland, T. Molecular imaging: Challenges of bringing imaging of intracellular targets into common clinical use. Contrast. Media Mol. Imaging 2012, 7, 1–6. [Google Scholar]
- Jain, M.; Kamal, N.; Batra, S.K. Engineering antibodies for clinical applications. Trends Biotechnol 2007, 25, 307–316. [Google Scholar]
- Pillai, R.; Marinelli, E.R.; Fan, H.; Nanjappan, P.; Song, B.; von Wronski, M.A.; Cherkaoui, S.; Tardy, I.; Pochon, S.; et al. A Phospholipid-PEG2000 Conjugate of a Vascular Endothelial Growth Factor Receptor 2 (VEGFR2)-Targeting Heterodimer Peptide for Contrast-Enhanced Ultrasound Imaging of Angiogenesis. Bioconjug. Chem 2010, 21, 556–562. [Google Scholar]
- Pochon, S.; Tardy, I.; Bussat, P.; Bettinger, T.; Brochot, J.; von, W.M.; Passantino, L.; Schneider, M. BR55: A lipopeptide-based VEGFR2-targeted ultrasound contrast agent for molecular imaging of angiogenesis. Invest Radiol 2010, 45, 89–95. [Google Scholar]
- Hanahan, D.; Folkman, J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 1996, 86, 353–364. [Google Scholar]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar]
- Hylton, N. Dynamic contrast-enhanced magnetic resonance imaging as an imaging biomarker. J. Clin. Oncol 2006, 24, 3293–3298. [Google Scholar]
- Turnbull, L.W. Dynamic contrast-enhanced MRI in the diagnosis and management of breast cancer. NMR Biomed 2009, 22, 28–39. [Google Scholar]
- Fukumura, D.; Jain, R.K. Tumor microvasculature and microenvironment: Targets for anti-angiogenesis and normalization. Microvasc. Res 2007, 74, 72–84. [Google Scholar]
- Kerbel, R.S. Reappraising antiangiogenic therapy for breast cancer. Breast 2011, 20, S56–S60. [Google Scholar]
- Adams, R.H.; Alitalo, K. Molecular regulation of angiogenesis and lymphangiogenesis. Nat. Rev. Mol. Cell Biol 2007, 8, 464–478. [Google Scholar]
- Pysz, M.A.; Foygel, K.; Rosenberg, J.; Gambhir, S.S.; Schneider, M.; Willmann, J.K. Antiangiogenic cancer therapy: Monitoring with molecular US and a clinically translatable contrast agent (BR55). Radiology 2010, 256, 519–527. [Google Scholar]
- Bzyl, J.; Lederle, W.; Rix, A.; Grouls, C.; Tardy, I.; Pochon, S.; Siepmann, M.; Penzkofer, T.; Schneider, M.; Kiessling, F.; et al. Molecular and functional ultrasound imaging in differently aggressive breast cancer xenografts using two novel ultrasound contrast agents (BR55 and BR38). Eur. Radiol 2011, 21, 1988–1995. [Google Scholar]
- Tardy, I.; Pochon, S.; Theraulaz, M.; Emmel, P.; Passantino, L.; Tranquart, F.; Schneider, M. Ultrasound molecular imaging of VEGFR2 in a rat prostate tumor model using BR55. Invest Radiol 2010, 45, 573–578. [Google Scholar]
- Lee, D.J.; Lyshchik, A.; Huamani, J.; Hallahan, D.E.; Fleischer, A.C. Relationship between retention of a vascular endothelial growth factor receptor 2 (VEGFR2)-targeted ultrasonographic contrast agent and the level of VEGFR2 expression in an in vivo breast cancer model. J. Ultrasound. Med 2008, 27, 855–866. [Google Scholar]
- Korpanty, G.; Carbon, J.G.; Grayburn, P.A.; Fleming, J.B.; Brekken, R.A. Monitoring response to anticancer therapy by targeting microbubbles to tumor vasculature. Clin. Cancer Res 2007, 13, 323–330. [Google Scholar]
- Willmann, J.K.; Paulmurugan, R.; Chen, K.; Gheysens, O.; Rodriguez-Porcel, M.; Lutz, A.M.; Chen, I.Y.; Chen, X.; Gambhir, S.S. US imaging of tumor angiogenesis with microbubbles targeted to vascular endothelial growth factor receptor type 2 in mice. Radiology 2008, 246, 508–518. [Google Scholar]
- Palmowski, M.; Huppert, J.; Ladewig, G.; Hauff, P.; Reinhardt, M.; Mueller, M.M.; Woenne, E.C.; Jenne, J.W.; Maurer, M.; Kauffmann, G.W.; et al. Molecular profiling of angiogenesis with targeted ultrasound imaging: Early assessment of antiangiogenic therapy effects. Mol. Cancer Ther 2008, 7, 101–109. [Google Scholar]
- Ellegala, D.B.; Leong-Poi, H.; Carpenter, J.E.; Klibanov, A.L.; Kaul, S.; Shaffrey, M.E.; Sklenar, J.; Lindner, J.R. Imaging tumor angiogenesis with contrast ultrasound and microbubbles targeted to alpha(v)beta3. Circulation 2003, 108, 336–341. [Google Scholar]
- Deshpande, N.; Ren, Y.; Foygel, K.; Rosenberg, J.; Willmann, J.K. Tumor angiogenic marker expression levels during tumor growth: Longitudinal assessment with molecularly targeted microbubbles and US imaging. Radiology 2011, 258, 804–811. [Google Scholar]
- Weller, G.E.; Wong, M.K.; Modzelewski, R.A.; Lu, E.; Klibanov, A.L.; Wagner, W.R.; Villanueva, F.S. Ultrasonic imaging of tumor angiogenesis using contrast microbubbles targeted via the tumor-binding peptide arginine-arginine-leucine. Cancer Res 2005, 65, 533–539. [Google Scholar]
- Palmowski, M.; Peschke, P.; Huppert, J.; Hauff, P.; Reinhardt, M.; Maurer, M.; Karger, C.P.; Scholz, M.; Semmler, W.; Huber, P.E.; et al. Molecular ultrasound imaging of early vascular response in prostate tumors irradiated with carbon ions. Neoplasia 2009, 11, 856–863. [Google Scholar]
- Willmann, J.K.; Lutz, A.M.; Paulmurugan, R.; Patel, M.R.; Chu, P.; Rosenberg, J.; Gambhir, S.S. Dual-targeted contrast agent for US assessment of tumor angiogenesis in vivo. Radiology 2008, 248, 936–944. [Google Scholar]
- Warram, J.M.; Sorace, A.G.; Saini, R.; Umphrey, H.R.; Zinn, K.R.; Hoyt, K. A triple-targeted ultrasound contrast agent provides improved localization to tumor vasculature. J. Ultrasound. Med 2011, 30, 921–931. [Google Scholar]
- Holmes, K.; Roberts, O.L.; Thomas, A.M.; Cross, M.J. Vascular endothelial growth factor receptor-2: Structure, function, intracellular signalling and therapeutic inhibition. Cell Signal 2007, 19, 2003–2012. [Google Scholar]
- Plate, K.H.; Breier, G.; Weich, H.A.; Mennel, H.D.; Risau, W. Vascular endothelial growth factor and glioma angiogenesis: Coordinate induction of VEGF receptors, distribution of VEGF protein and possible in vivo regulatory mechanisms. Int. J. Cancer 1994, 59, 520–529. [Google Scholar]
- Backer, M.V.; Levashova, Z.; Patel, V.; Jehning, B.T.; Claffey, K.; Blankenberg, F.G.; Backer, J.M. Molecular imaging of VEGF receptors in angiogenic vasculature with single-chain VEGF-based probes. Nat. Med 2007, 13, 504–509. [Google Scholar]
- Deshpande, N.; Pysz, M.A.; Willmann, J.K. Molecular ultrasound assessment of tumor angiogenesis. Angiogenesis 2010, 13, 175–188. [Google Scholar]
- Blankenberg, F.G.; Backer, M.V.; Levashova, Z.; Patel, V.; Backer, J.M. In vivo tumor angiogenesis imaging with site-specific labeled (99m)Tc-HYNIC-VEGF. Eur. J. Nucl. Med. Mol. Imaging 2006, 33, 841–848. [Google Scholar]
- Cai, W.; Chen, K.; Mohamedali, K.A.; Cao, Q.; Gambhir, S.S.; Rosenblum, M.G.; Chen, X. PET of vascular endothelial growth factor receptor expression. J. Nucl. Med 2006, 47, 2048–2056. [Google Scholar]
- Wijkstra, H.; Smeenge, M.; de la Rosette, J.; Pochon, S.; Tardy-Cantalupi, I.; Tranquart, F. Targeted Microbubble Prostate Cancer Imaging with BR55. Proceedings of the 18th European Symposium on Ultrasound Contrast Imaging, Rotterdam, The Netherlands, 17–18 January 2013. abstract submission, 2012.
- Avraamides, C.J.; Garmy-Susini, B.; Varner, J.A. Integrins in angiogenesis and lymphangiogenesis. Nat. Rev. Cancer 2008, 8, 604–617. [Google Scholar]
- Brooks, P.C.; Clark, R.A.; Cheresh, D.A. Requirement of vascular integrin alpha v beta 3 for angiogenesis. Science 1994, 264, 569–571. [Google Scholar]
- Pepper, M.S. Role of the matrix metalloproteinase and plasminogen activator-plasmin systems in angiogenesis. Arterioscler. Thromb. Vasc. Biol 2001, 21, 1104–1117. [Google Scholar]
- Gurrath, M.; Muller, G.; Kessler, H.; Aumailley, M.; Timpl, R. Conformation/activity studies of rationally designed potent anti-adhesive RGD peptides. Eur. J. Biochem 1992, 210, 911–921. [Google Scholar]
- Leong-Poi, H.; Christiansen, J.; Klibanov, A.L.; Kaul, S.; Lindner, J.R. Noninvasive assessment of angiogenesis by ultrasound and microbubbles targeted to alpha(v)-integrins. Circulation 2003, 107, 455–460. [Google Scholar]
- Hong, H.; Yang, Y.; Zhang, Y.; Engle, J.W.; Barnhart, T.E.; Nickles, R.J.; Leigh, B.R.; Cai, W. Positron emission tomography imaging of CD105 expression during tumor angiogenesis. Eur. J. Nucl. Med Mol. Imaging 2011, 38, 1335–1343. [Google Scholar]
- Zhang, Y.; Yang, Y.; Hong, H.; Cai, W. Multimodality molecular imaging of CD105 (Endoglin) expression. Int. J. Clin. Exp. Med 2011, 4, 32–42. [Google Scholar]
- Korpanty, G.; Grayburn, P.A.; Shohet, R.V.; Brekken, R.A. Targeting vascular endothelium with avidin microbubbles. Ultrasound. Med. Biol 2005, 31, 1279–1283. [Google Scholar]
- Sanna, V.; Pintus, G.; Bandiera, P.; Anedda, R.; Punzoni, S.; Sanna, B.; Migaleddu, V.; Uzzau, S.; Sechi, M. Development of polymeric microbubbles targeted to prostate-specific membrane antigen as prototype of novel ultrasound contrast agents. Mol. Pharm 2011, 8, 748–757. [Google Scholar]
- Chang, S.S.; O’Keefe, D.S.; Bacich, D.J.; Reuter, V.E.; Heston, W.D.; Gaudin, P.B. Prostate-specific membrane antigen is produced in tumor-associated neovasculature. Clin. Cancer Res 1999, 5, 2674–2681. [Google Scholar]
- Bouchelouche, K.; Choyke, P.L.; Capala, J. Prostate specific membrane antigen- a target for imaging and therapy with radionuclides. Discov. Med 2010, 9, 55–61. [Google Scholar]
- Hillier, S.M.; Maresca, K.P.; Femia, F.J.; Marquis, J.C.; Foss, C.A.; Nguyen, N.; Zimmerman, C.N.; Barrett, J.A.; Eckelman, W.C.; Pomper, M.G.; et al. Preclinical evaluation of novel glutamate-urea-lysine analogues that target prostate-specific membrane antigen as molecular imaging pharmaceuticals for prostate cancer. Cancer Res 2009, 69, 6932–6940. [Google Scholar]
- Maresca, K.P.; Hillier, S.M.; Femia, F.J.; Keith, D.; Barone, C.; Joyal, J.L.; Zimmerman, C.N.; Kozikowski, A.P.; Barrett, J.A.; Eckelman, W.C.; et al. A series of halogenated heterodimeric inhibitors of prostate specific membrane antigen (PSMA) as radiolabeled probes for targeting prostate cancer. J. Med. Chem 2009, 52, 347–357. [Google Scholar]
- Kobayashi, H.; Boelte, K.C.; Lin, P.C. Endothelial cell adhesion molecules and cancer progression. Curr. Med. Chem 2007, 14, 377–386. [Google Scholar]
- Delorme, S.; Krix, M. Contrast-enhanced ultrasound for examining tumor biology. Cancer Imaging 2006, 6, 148–152. [Google Scholar]
- Qayum, N.; Im, J.; Stratford, M.R.; Bernhard, E.J.; McKenna, W.G.; Muschel, R.J. Modulation of the tumor microvasculature by phosphoinositide-3 kinase inhibition increases doxorubicin delivery in vivo. Clin. Cancer Res 2012, 18, 161–169. [Google Scholar]
- Sirsi, S.R.; Flexman, M.L.; Vlachos, F.; Huang, J.; Hernandez, S.L.; Kim, H.K.; Johung, T.B.; Gander, J.W.; Reichstein, A.R.; Lampl, B.S.; et al. Contrast ultrasound imaging for identification of early responder tumor models to anti-angiogenic therapy. Ultrasound Med. Biol 2012, 38, 1019–1029. [Google Scholar]
- Lassau, N.; Lamuraglia, M.; Chami, L.; Leclere, J.; Bonvalot, S.; Terrier, P.; Roche, A.; Le, C.A. Gastrointestinal stromal tumors treated with imatinib: Monitoring response with contrast-enhanced sonography. AJR Am. J. Roentgenol 2006, 187, 1267–1273. [Google Scholar]
- Kaufmann, B.A.; Lewis, C.; Xie, A.; Mirza-Mohd, A.; Lindner, J.R. Detection of recent myocardial ischaemia by molecular imaging of P-selectin with targeted contrast echocardiography. Eur. Heart J 2007, 28, 2011–2017. [Google Scholar]
- Weller, G.E.; Villanueva, F.S.; Klibanov, A.L.; Wagner, W.R. Modulating targeted adhesion of an ultrasound contrast agent to dysfunctional endothelium. Ann. Biomed. Eng 2002, 30, 1012–1019. [Google Scholar]



| Target | Ligand | Model System | Tumor Contrast Enhancement Compared to Non-Targeted Control MBs 1 | Other Findings | Reference |
|---|---|---|---|---|---|
| VEGFR2/KDR | Heterodimeric peptide (BR55) | Mouse Colon carcinoma xenograft LS174T | 3-fold | Video intensity corresponds to MVD and VEGFR2 expression, allowing monitoring of antiangiogenic therapy | [26] |
| VEGFR2 | Heterodimeric peptide (BR55) | Rat Mammary carcinoma 13762 MAT B III | NA | The binding specificity of microbubbles with heterodimeric peptide ligand was similar to that of microbubbles with anti-VEGFR2 antibodies | [18] |
| VEGFR2 | Heterodimeric peptide (BR55) | Mouse Breast cancer xenograft MCF-7/MDA-MB-231 | NA | 2-fold difference in VEGFR2 expression between tumor models reflected in video intensity | [27] |
| VEGFR2 | Heterodimeric peptide (BR55) | Rat Prostate adenocarcinoma G Dunning R-3327 | NA | 20-fold difference in signal intensity between prostate cancer and normal tissue. Binding similar to that of antibody-coated bubbles | [28] |
| VEGFR2 | Antibody | Mouse Breast cancer xenograft NR67 | 2.5-fold | Retention of VEGFR2-targeting bubbles correlate to VEGFR2 expression but not vascularity | [29] |
| VEGFR2 | Antibody | Mouse Pancreatic cancer xenograft MiaPaCa2/Pan02 | 1.5-fold | Reduced endothelial expression of VEGFR after treatment with gemcitabine | [30] |
| VEGFR2 | Antibody | Mouse/Rat Angiosarcoma (SVR) Glioma (C6) | 3–5 fold | Unspecific control MBs had significantly higher video intensity than unlabeled MBs (10-fold) | [31] |
| VEGFR2 | Antibody | Mouse Squamous cell carcinoma HaCaT-ras-A-5RT3 | 7.5-fold | Reduced microbubble retention after matrix metalloproteinase inhibition. No significant difference between VEGFR2- and αvβ3-targeted microbubbles | [32] |
| αvβ3 | Echistatin | Rat Glioma xenograft U87MG | 3-fold | Spatial variation in signal intensity corresponded to integrin expression | [33] |
| αvβ3 | Knottin | Mouse Ovarian cancer xenograft SK-OV-3 | 3-fold | Knottin-decorated MBs outperformed MBs conjugated with RGD or antibodies and had a 12-fold tumor-muscle ratio | [14] |
| αvβ3 | Cyclic RGD peptide | Mouse Breast cancer xenograft Met-1 | 8-fold | [9] | |
| αvβ3 | RGD | Mouse Squamous cell carcinoma HaCaT-ras-A-5RT3 | 5-fold | [32] | |
| Endoglin (CD105) | Antibody | Mouse Pancreatic cancer xenograft MiaPaCa2 | 1.5-fold | [30] | |
| VEGFR2 αvβ3 Endoglin (CD105) | Antibodies | Mouse Subcutaneous xenografts MDA-MB361 (breast) SKOV-3 (ovarian) MiaPaCa2 (pancreatic) | NA | Microbubbles targeting endoglin had up to 3-fold higher video intensity than microbubbles targeting VEGFR2 or αvβ3. In pancreatic tumors, microbubbles targeting αvβ3 had the highest video intensity | [34] |
| Unknown | RRL | Mouse Prostate cancer xenograft PC-3 | 3-fold | Spatial variation in signal intensity corresponded to vascular density | [35] |
| ICAM-1 αvβ3 | Antibody | Rat Prostate cancer xenograft AT-1 | 3-fold | Approximately 1.5-fold higher video intensity than RGD-labeled MBs | [36] |
| VEGFR2 + αvβ3 | 2 × antibody | Mouse Ovarian cancer xenograft SK-OV-3 | 4-fold (VEGFR2) 3-fold (αvβ3) 6-fold (VEGFR2 + αvβ3) | Dual-targeted microbubbles outperformed microbubbles with only one ligand | [37] |
| VEGFR2 + αvβ3 + ICAM1 | 3 × antibody | Mouse MDA-MB-231 | NA | Triple-targeted microbubbles had 1.6-fold higher signal intensity than the additive intensity of all three single-targeted microbubbles, and approximately 5-fold higher VI than any of the single-targeted microbubbles alone | [38] |
© 2012 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Moestue, S.A.; Gribbestad, I.S.; Hansen, R. Intravascular Targets for Molecular Contrast-Enhanced Ultrasound Imaging. Int. J. Mol. Sci. 2012, 13, 6679-6697. https://doi.org/10.3390/ijms13066679
Moestue SA, Gribbestad IS, Hansen R. Intravascular Targets for Molecular Contrast-Enhanced Ultrasound Imaging. International Journal of Molecular Sciences. 2012; 13(6):6679-6697. https://doi.org/10.3390/ijms13066679
Chicago/Turabian StyleMoestue, Siver A., Ingrid S. Gribbestad, and Rune Hansen. 2012. "Intravascular Targets for Molecular Contrast-Enhanced Ultrasound Imaging" International Journal of Molecular Sciences 13, no. 6: 6679-6697. https://doi.org/10.3390/ijms13066679
APA StyleMoestue, S. A., Gribbestad, I. S., & Hansen, R. (2012). Intravascular Targets for Molecular Contrast-Enhanced Ultrasound Imaging. International Journal of Molecular Sciences, 13(6), 6679-6697. https://doi.org/10.3390/ijms13066679