Heart Failure and Atrial Fibrillation: From Basic Science to Clinical Practice
Abstract
:1. Introduction
2. Combined Heart Failure and Atrial Fibrillation: Epidemiological and Prognostic Implications
3. Common Pathophysiological Background for Heart Failure and Atrial Fibrillation
3.1. Hemodynamic Mechanisms
| Items | Pathophysiological Mechanisms |
|---|---|
| Hemodynamic | Increased left ventricle filling pressure |
| Increased resting heart rate | |
| Exaggerated heart rate response to exercise | |
| Loss of atrial contraction | |
| Reduced myocardial contractility | |
| Neuro-hormonal | Renin-angiotensin-aldosterone system activation |
| Adrenergic activation | |
| Increase of transforming growth factor-β1 | |
| Cellular | Extracellular matrix alteration |
| Intracellular calcium overload |
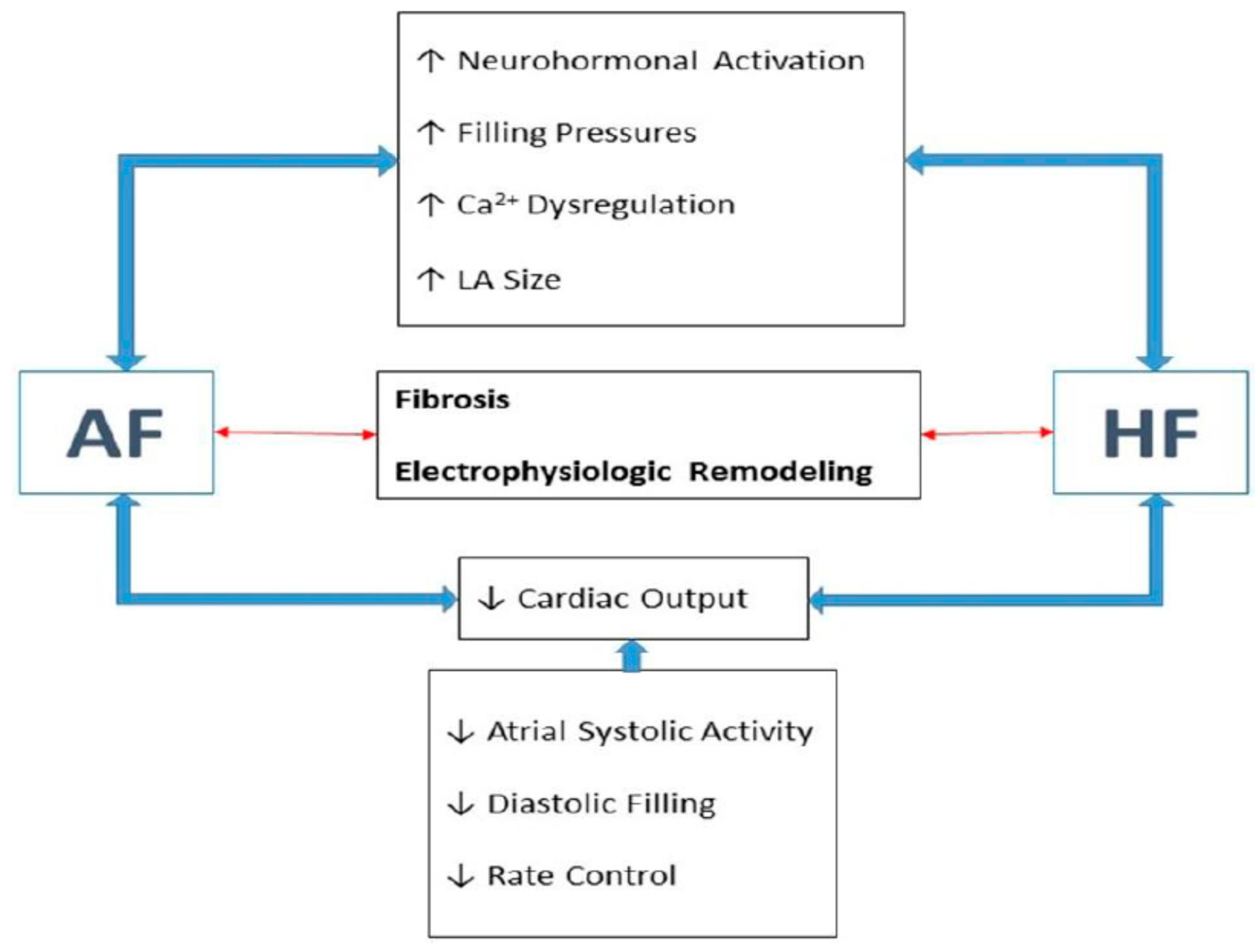
3.2. Neuro-Hormonal Mechanisms
3.3. Cellular and Intra-Cellular Mechanisms
4. Fibroblast Growth Factor-23: A Key Link between Chronic Kidney Disease, Atrial Fibrillation and Heart Failure

5. Atrial Structure and Function Influence on Thromboembolic Risk and Heart Failure
6. Obesity and Epicardial Fat Increase Atrial Arrhythmogenesis
7. Abnormal Gene Expression in Atrial Fibrillation
8. Heart Failure and Atrial Fibrillation: Treatment Implications
9. Conclusions
Author Contributions
Conflicts of Interest
References
- McMurray, J.J.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Bohm, M.; Dickstein, K.; Falk, V.; Filippatos, G.; Fonseca, C.; Gomez-Sanchez, M.A.; et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the european society of cardiology: Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail 2012, 14, 803–869. [Google Scholar] [CrossRef]
- Roubille, F.; Tardif, J.C. New therapeutic targets in cardiology: Heart failure and arrhythmia: HCN Channels. Circulation 2013, 127, 1986–1996. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Hylek, E.M.; Phillips, K.A.; Chang, Y.; Henault, L.E.; Selby, J.V.; Singer, D.E. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The anticoagulation and risk factors in atrial fibrillation (ATRIA) study. JAMA 2001, 285, 2370–2375. [Google Scholar] [CrossRef] [PubMed]
- Chugh, S.S.; Roth, G.A.; Gillum, R.F.; Mensah, G.A. Global burden of atrial fibrillation in developed and developing nations. Glob. Heart 2014, 9, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.J.; Larson, M.G.; Levy, D.; Vasan, R.S.; Leip, E.P.; Wolf, P.A.; D’Agostino, R.B.; Murabito, J.M.; Kannel, W.B.; Benjamin, E.J. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: The framingham heart study. Circulation 2003, 107, 2920–2925. [Google Scholar] [CrossRef] [PubMed]
- Carson, P.E.; Johnson, G.R.; Dunkman, W.B.; Fletcher, R.D.; Farrell, L.; Cohn, J.N. The influence of atrial fibrillation on prognosis in mild to moderate heart failure: The V-HeFT studies: The V-HeFT VA cooperative studies group. Circulation 1993, 87, VI102–VI110. [Google Scholar] [PubMed]
- Savelieva, I.; John Camm, A. Atrial fibrillation and heart failure: Natural history and pharmacological treatment. Europace 2004, 5 (Suppl. 1), S5–S19. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef]
- Stevenson, W.G.; Stevenson, L.W.; Middlekauff, H.R.; Fonarow, G.C.; Hamilton, M.A.; Woo, M.A.; Saxon, L.A.; Natterson, P.D.; Steimle, A.; Walden, J.A.; et al. Improving survival for patients with atrial fibrillation and advanced heart failure. J. Am. Coll. Cardiol. 1996, 28, 1458–1463. [Google Scholar] [CrossRef]
- Mamas, M.A.; Caldwell, J.C.; Chacko, S.; Garratt, C.J.; Fath-Ordoubadi, F.; Neyses, L. A meta-analysis of the prognostic significance of atrial fibrillation in chronic heart failure. Eur. J. Heart Fail. 2009, 11, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.M.; Redfield, M.M.; Shen, W.K.; Gersh, B.J. Atrial fibrillation and ventricular dysfunction: A vicious electromechanical cycle. Circulation 2004, 109, 2839–2843. [Google Scholar] [CrossRef] [PubMed]
- Burstein, B.; Nattel, S. Atrial fibrosis: Mechanisms and clinical relevance in atrial fibrillation. J. Am. Coll. Cardiol. 2008, 51, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Nattel, S.; Burstein, B.; Dobrev, D. Atrial remodeling and atrial fibrillation: Mechanisms and implications. Circ. Arrhythm. Electrophysiol. 2008, 1, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.T.; Lai, L.P.; Kuo, K.T.; Hwang, J.J.; Hsieh, C.S.; Hsu, K.L.; Tseng, C.D.; Tseng, Y.Z.; Chiang, F.T.; Lin, J.L. Angiotensin II activates signal transducer and activators of transcription 3 via Rac1 in atrial myocytes and fibroblasts: Implication for the therapeutic effect of statin in atrial structural remodeling. Circulation 2008, 117, 344–355. [Google Scholar] [CrossRef] [PubMed]
- Rosenkranz, S. TNF-β1 and angiotensin networking in cardiac remodeling. Cardiovasc. Res. 2004, 63, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Verheule, S.; Sato, T.; Everett, T.T.; Engle, S.K.; Otten, D.; Rubart-von der Lohe, M.; Nakajima, H.O.; Nakajima, H.; Field, L.J.; Olgin, J.E. Increased vulnerability to atrial fibrillation in transgenic mice with selective atrial fibrosis caused by overexpression of TNF-β1. Circ. Res. 2004, 94, 1458–1465. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.H.; Akazawa, H.; Tamagawa, M.; Ito, K.; Yasuda, N.; Kudo, Y.; Yamamoto, R.; Ozasa, Y.; Fujimoto, M.; Wang, P.; et al. Cardiac mast cells cause atrial fibrillation through PDGF-A-mediated fibrosis in pressure-overloaded mouse hearts. J. Clin. Investig. 2010, 120, 242–253. [Google Scholar] [CrossRef]
- Qu, Y.C.; Du, Y.M.; Wu, S.L.; Chen, Q.X.; Wu, H.L.; Zhou, S.F. Activated nuclear factor-κB and increased tumor necrosis factor-α in atrial tissue of atrial fibrillation. Scand. Cardiovasc. J. 2009, 43, 292–297. [Google Scholar] [CrossRef]
- Adam, O.; Lavall, D.; Theobald, K.; Hohl, M.; Grube, M.; Ameling, S.; Sussman, M.A.; Rosenkranz, S.; Kroemer, H.K.; Schafers, H.J.; et al. Rac1-induced connective tissue growth factor regulates connexin 43 and N-cadherin expression in atrial fibrillation. J. Am. Coll. Cardiol. 2010, 55, 469–480. [Google Scholar] [CrossRef]
- Sulciner, D.J.; Irani, K.; Yu, Z.X.; Ferrans, V.J.; Goldschmidt-Clermont, P.; Finkel, T. Rac1 regulates a cytokine-stimulated, redox-dependent pathway necessary for NF-κB activation. Mol. Cell. Biol. 1996, 16, 7115–7121. [Google Scholar] [PubMed]
- Gao, G.; Dudley, S.C., Jr. Redox regulation, NF-κb, and atrial fibrillation. Antioxid. Redox Signal. 2009, 11, 2265–2277. [Google Scholar] [CrossRef] [PubMed]
- Adam, O.; Frost, G.; Custodis, F.; Sussman, M.A.; Schafers, H.J.; Bohm, M.; Laufs, U. Role of Rac1 GTPase activation in atrial fibrillation. J. Am. Coll. Cardiol. 2007, 50, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Goette, A.; Lendeckel, U.; Klein, H.U. Signal transduction systems and atrial fibrillation. Cardiovasc. Res. 2002, 54, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Brilla, C.G.; Scheer, C.; Rupp, H. Angiotensin II and intracellular calcium of adult cardiac fibroblasts. J. Mol. Cell Cardiol. 1998, 30, 1237–1246. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.M.; Mehta, A.A. Aldosterone and angiotensin: Role in diabetes and cardiovascular diseases. Eur. J. Pharmacol. 2012, 697, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.G.; Cai, H.; Landmesser, U.; Griendling, K.K. Interactions of angiotensin II with NAD(P)H oxidase, oxidant stress and cardiovascular disease. J. Renin Angiotensin Aldosterone Syst. 2003, 4, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Teekakirikul, P.; Eminaga, S.; Toka, O.; Alcalai, R.; Wang, L.; Wakimoto, H.; Nayor, M.; Konno, T.; Gorham, J.M.; Wolf, C.M.; et al. Cardiac fibrosis in mice with hypertrophic cardiomyopathy is mediated by non-myocyte proliferation and requires TNF-β. J. Clin. Invest. 2010, 120, 3520–3529. [Google Scholar] [CrossRef]
- Takeda, N.; Manabe, I.; Uchino, Y.; Eguchi, K.; Matsumoto, S.; Nishimura, S.; Shindo, T.; Sano, M.; Otsu, K.; Snider, P.; et al. Cardiac fibroblasts are essential for the adaptive response of the murine heart to pressure overload. J. Clin. Investig. 2010, 120, 254–265. [Google Scholar] [CrossRef]
- Aleong, R.G.; Sauer, W.H.; Murphy, G.A.; Port, J.D.; Anand, I.S.; Fiuzat, M.; O’Connor, C.M.; Abraham, W.T.; Liggett, S.B.; Bristow, M.R. Prevention of atrial fibrillation by bucindolol is dependent on the β1389 Arg/Gly adrenergic receptor polymorphism. JACC Heart Fail. 2013, 1, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Kao, D.P.; Davis, G.; Aleong, R.; O'Connor, C.M.; Fiuzat, M.; Carson, P.E.; Anand, I.S.; Plehn, J.F.; Gottlieb, S.S.; Silver, M.A.; et al. Effect of bucindolol on heart failure outcomes and heart rate response in patients with reduced ejection fraction heart failure and atrial fibrillation. Eur. J. Heart Fail. 2013, 15, 324–333. [Google Scholar] [CrossRef]
- Oral, H.; Crawford, T.; Frederick, M.; Gadeela, N.; Wimmer, A.; Dey, S.; Sarrazin, J.F.; Kuhne, M.; Chalfoun, N.; Wells, D.; et al. Inducibility of paroxysmal atrial fibrillation by isoproterenol and its relation to the mode of onset of atrial fibrillation. J. Cardiovasc. Electrophysiol. 2008, 19, 466–470. [Google Scholar] [CrossRef]
- Sharifov, O.F.; Fedorov, V.V.; Beloshapko, G.G.; Glukhov, A.V.; Yushmanova, A.V.; Rosenshtraukh, L.V. Roles of adrenergic and cholinergic stimulation in spontaneous atrial fibrillation in dogs. J. Am. Coll. Cardiol. 2004, 43, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhang, Y.J.; Wang, Y.L.; Xu, Y.F.; Liu, S.; Chen, Z.Y.; Liu, L.L. Effect of dipfluzine on delayed afterdepolarizations and triggered activity induced by isoprenaline in human atrial fibers. Yao Xue Xue Bao (in Chinese) 2006, 41, 184–187. [Google Scholar]
- Van der Velden, H.M.; Ausma, J.; Rook, M.B.; Hellemons, A.J.; van Veen, T.A.; Allessie, M.A.; Jongsma, H.J. Gap junctional remodeling in relation to stabilization of atrial fibrillation in the goat. Cardiovasc. Res. 2000, 46, 476–486. [Google Scholar] [CrossRef] [PubMed]
- Satoh, T.; Zipes, D.P. Unequal atrial stretch in dogs increases dispersion of refractoriness conducive to developing atrial fibrillation. J. Cardiovasc. Electrophysiol. 1996, 7, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Allessie, M.A.; Boyden, P.A.; Camm, A.J.; Kleber, A.G.; Lab, M.J.; Legato, M.J.; Rosen, M.R.; Schwartz, P.J.; Spooner, P.M.; van Wagoner, D.R.; et al. Pathophysiology and prevention of atrial fibrillation. Circulation 2001, 103, 769–777. [Google Scholar] [CrossRef]
- Daoud, E.G.; Bogun, F.; Goyal, R.; Harvey, M.; Man, K.C.; Strickberger, S.A.; Morady, F. Effect of atrial fibrillation on atrial refractoriness in humans. Circulation 1996, 94, 1600–1606. [Google Scholar] [CrossRef] [PubMed]
- Hasenfuss, G.; Reinecke, H.; Studer, R.; Meyer, M.; Pieske, B.; Holtz, J.; Holubarsch, C.; Posival, H.; Just, H.; Drexler, H. Relation between myocardial function and expression of sarcoplasmic reticulum Ca2+-ATPase in failing and nonfailing human myocardium. Circ. Res. 1994, 75, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Voigt, N.; Li, N.; Wang, Q.; Wang, W.; Trafford, A.W.; Abu-Taha, I.; Sun, Q.; Wieland, T.; Ravens, U.; Nattel, S.; et al. Enhanced sarcoplasmic reticulum Ca2+ leak and increased Na+–Ca2+ exchanger function underlie delayed afterdepolarizations in patients with chronic atrial fibrillation. Circulation 2012, 125, 2059–2070. [Google Scholar] [CrossRef] [PubMed]
- Hove-Madsen, L.; Llach, A.; Bayes-Genis, A.; Roura, S.; Rodriguez Font, E.; Aris, A.; Cinca, J. Atrial fibrillation is associated with increased spontaneous calcium release from the sarcoplasmic reticulum in human atrial myocytes. Circulation 2004, 110, 1358–1363. [Google Scholar] [CrossRef] [PubMed]
- Neef, S.; Dybkova, N.; Sossalla, S.; Ort, K.R.; Fluschnik, N.; Neumann, K.; Seipelt, R.; Schondube, F.A.; Hasenfuss, G.; Maier, L.S. CaMKII-dependent diastolic SR Ca2+ leak and elevated diastolic Ca2+ levels in right atrial myocardium of patients with atrial fibrillation. Circ. Res. 2010, 106, 1134–1144. [Google Scholar] [CrossRef] [PubMed]
- Voigt, N.; Heijman, J.; Wang, Q.; Chiang, D.Y.; Li, N.; Karck, M.; Wehrens, X.H.; Nattel, S.; Dobrev, D. Cellular and molecular mechanisms of atrial arrhythmogenesis in patients with paroxysmal atrial fibrillation. Circulation 2014, 129, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Mathew, J.S.; Sachs, M.C.; Katz, R.; Patton, K.K.; Heckbert, S.R.; Hoofnagle, A.N.; Alonso, A.; Chonchol, M.; Deo, R.; Ix, J.H.; et al. Fibroblast growth factor-23 and incident atrial fibrillation: The multi-ethnic study of atherosclerosis (MESA) and the cardiovascular health study (CHS). Circulation 2014, 130, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, O.M.; Januzzi, J.L.; Isakova, T.; Laliberte, K.; Smith, K.; Collerone, G.; Sarwar, A.; Hoffmann, U.; Coglianese, E.; Christenson, R.; et al. Fibroblast growth factor 23 and left ventricular hypertrophy in chronic kidney disease. Circulation 2009, 119, 2545–2552. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, M.A.; Manning, W.J. Diastolic dysfunction and risk of atrial fibrillation: A mechanistic appraisal. Circulation 2012, 126, 2353–2362. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.K.; Shah, A.M.; Giugliano, R.P.; Ruff, C.T.; Antman, E.M.; Grip, L.T.; Deenadayalu, N.; Hoffman, E.; Patel, I.; Shi, M.; et al. Left atrial structure and function in atrial fibrillation: ENGAGE AF-TIMI 48. Eur. Heart J. 2014, 35, 1457–1465. [Google Scholar] [CrossRef] [PubMed]
- Stroke Risk in Atrial Fibrillation Working Group. Comparison of 12 risk stratification schemes to predict stroke in patients with nonvalvular atrial fibrillation. Stroke 2008, 39, 1901–1910. [Google Scholar]
- Dittrich, H.C.; Pearce, L.A.; Asinger, R.W.; McBride, R.; Webel, R.; Zabalgoitia, M.; Pennock, G.D.; Safford, R.E.; Rothbart, R.M.; Halperin, J.L.; et al. Left atrial diameter in nonvalvular atrial fibrillation: An echocardiographic study: Stroke prevention in atrial fibrillation investigators. Am. Heart J. 1999, 137, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Gage, B.F.; Waterman, A.D.; Shannon, W.; Boechler, M.; Rich, M.W.; Radford, M.J. Validation of clinical classification schemes for predicting stroke: Results from the national registry of atrial fibrillation. JAMA 2001, 285, 2864–2870. [Google Scholar] [CrossRef] [PubMed]
- Atrial Fibrillation Investigayors. Echocardiographic predictors of stroke in patients with atrial fibrillation: A prospective study of 1066 patients from 3 clinical trials. Arch. Intern. Med. 1998, 158, 1316–1320. [Google Scholar]
- Kenchaiah, S.; Evans, J.C.; Levy, D.; Wilson, P.W.; Benjamin, E.J.; Larson, M.G.; Kannel, W.B.; Vasan, R.S. Obesity and the risk of heart failure. N. Engl. J. Med. 2002, 347, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Morricone, L.; Malavazos, A.E.; Coman, C.; Donati, C.; Hassan, T.; Caviezel, F. Echocardiographic abnormalities in normotensive obese patients: Relationship with visceral fat. Obes. Res. 2002, 10, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Psaty, B.M.; Manolio, T.A.; Kuller, L.H.; Kronmal, R.A.; Cushman, M.; Fried, L.P.; White, R.; Furberg, C.D.; Rautaharju, P.M. Incidence of and risk factors for atrial fibrillation in older adults. Circulation 1997, 96, 2455–2461. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.K.; Chen, Y.J.; Chen, S.A. Potential atrial arrhythmogenicity of adipocytes: Implications for the genesis of atrial fibrillation. Med. Hypotheses 2010, 74, 1026–1029. [Google Scholar] [CrossRef] [PubMed]
- Nagashima, K.; Okumura, Y.; Watanabe, I.; Nakai, T.; Ohkubo, K.; Kofune, M.; Mano, H.; Sonoda, K.; Hiro, T.; Nikaido, M.; et al. Does location of epicardial adipose tissue correspond to endocardial high dominant frequency or complex fractionated atrial electrogram sites during atrial fibrillation? Circ. Arrhythm. Electrophysiol. 2012, 5, 676–683. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.S.; Turker, I. Epicardial adipose tissue and neural mechanisms of atrial fibrillation. Circ. Arrhythm. Electrophysiol. 2012, 5, 618–620. [Google Scholar] [CrossRef] [PubMed]
- Batal, O.; Schoenhagen, P.; Shao, M.; Ayyad, A.E.; van Wagoner, D.R.; Halliburton, S.S.; Tchou, P.J.; Chung, M.K. Left atrial epicardial adiposity and atrial fibrillation. Circ. Arrhythm. Electrophysiol. 2010, 3, 230–236. [Google Scholar] [CrossRef]
- Lin, Y.K.; Chen, Y.C.; Chang, S.L.; Lin, Y.J.; Chen, J.H.; Yeh, Y.H.; Chen, S.A.; Chen, Y.J. Heart failure epicardial fat increases atrial arrhythmogenesis. Int. J. Cardiol. 2013, 167, 1979–1983. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Tai, C.T.; Chiou, C.W.; Wen, Z.C.; Chan, P.; Lee, S.H.; Chen, S.A. Inducibility of atrial fibrillation during atrioventricular pacing with varying intervals: Role of atrial electrophysiology and the autonomic nervous system. J. Cardiovasc. Electrophysiol. 1999, 10, 1578–1585. [Google Scholar] [CrossRef] [PubMed]
- Aydin, H.; Toprak, A.; Deyneli, O.; Yazici, D.; Tarcin, O.; Sancak, S.; Yavuz, D.; Akalin, S. Epicardial fat tissue thickness correlates with endothelial dysfunction and other cardiovascular risk factors in patients with metabolic syndrome. Metab. Syndr. Relat. Disord. 2010, 8, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Tuttolomondo, A.; Casuccio, A.; di Raimondo, D.; di Sciacca, R.; Arnao, V.; Licata, G. Immuno-inflammatory predictors of stroke at follow-up in patients with chronic non-valvular atrial fibrillation (NVAF). Clin. Sci. (Lond.) 2009, 116, 781–789. [Google Scholar] [CrossRef]
- Acevedo, M.; Corbalan, R.; Braun, S.; Pereira, J.; Gonzalez, I.; Navarrete, C. Biochemical predictors of cardiac rhythm at 1 year follow-up in patients with non-valvular atrial fibrillation. J. Thromb. Thrombolysis 2012, 33, 383–388. [Google Scholar] [CrossRef]
- Girerd, N.; Scridon, A.; Bessiere, F.; Chauveau, S.; Geloen, A.; Boussel, L.; Morel, E.; Chevalier, P. Periatrial epicardial fat is associated with markers of endothelial dysfunction in patients with atrial fibrillation. PLoS One 2013, 8, e77167. [Google Scholar] [CrossRef] [PubMed]
- Khan, R.S.; Kato, T.S.; Chokshi, A.; Chew, M.; Yu, S.; Wu, C.; Singh, P.; Cheema, F.H.; Takayama, H.; Harris, C.; et al. Adipose tissue inflammation and adiponectin resistance in patients with advanced heart failure: Correction after ventricular assist device implantation. Circ. Heart Fail. 2012, 5, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Vela, M.E.; Torres, N.; Tovar, A.R. White adipose tissue as endocrine organ and its role in obesity. Arch. Med. Res. 2008, 39, 715–728. [Google Scholar] [CrossRef] [PubMed]
- Fei, J.; Cook, C.; Blough, E.; Santanam, N. Age and sex mediated changes in epicardial fat adipokines. Atherosclerosis 2010, 212, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O. Obesity and cardiovascular disease: Risk factor, paradox, and impact of weight loss. J. Am. Coll. Cardiol. 2009, 53, 1925–1932. [Google Scholar] [CrossRef] [PubMed]
- Fontes-Carvalho, R.; Fontes-Oliveira, M.; Sampaio, F.; Mancio, J.; Bettencourt, N.; Teixeira, M.; Rocha Goncalves, F.; Gama, V.; Leite-Moreira, A. Influence of epicardial and visceral fat on left ventricular diastolic and systolic functions in patients after myocardial infarction. Am. J. Cardiol. 2014, 114, 1663–1669. [Google Scholar] [CrossRef] [PubMed]
- Canepa, M.; Strait, J.B.; Abramov, D.; Milaneschi, Y.; AlGhatrif, M.; Moni, M.; Ramachandran, R.; Najjar, S.S.; Brunelli, C.; Abraham, T.P.; et al. Contribution of central adiposity to left ventricular diastolic function (from the baltimore longitudinal study of aging). Am. J. Cardiol. 2012, 109, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Russo, C.; Jin, Z.; Homma, S.; Rundek, T.; Elkind, M.S.; Sacco, R.L.; di Tullio, M.R. Effect of obesity and overweight on left ventricular diastolic function: A community-based study in an elderly cohort. J. Am. Coll. Cardiol. 2011, 57, 1368–1374. [Google Scholar] [CrossRef] [PubMed]
- Konishi, M.; Sugiyama, S.; Sugamura, K.; Nozaki, T.; Matsubara, J.; Akiyama, E.; Utsunomiya, D.; Matsuzawa, Y.; Yamashita, Y.; Kimura, K.; et al. Accumulation of pericardial fat correlates with left ventricular diastolic dysfunction in patients with normal ejection fraction. J. Cardiol. 2012, 59, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Chugh, S.S.; Blackshear, J.L.; Shen, W.K.; Hammill, S.C.; Gersh, B.J. Epidemiology and natural history of atrial fibrillation: Clinical implications. J. Am. Coll. Cardiol. 2001, 37, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Arnar, D.O.; Thorvaldsson, S.; Manolio, T.A.; Thorgeirsson, G.; Kristjansson, K.; Hakonarson, H.; Stefansson, K. Familial aggregation of atrial fibrillation in iceland. Eur. Heart J. 2006, 27, 708–712. [Google Scholar] [CrossRef] [PubMed]
- Ellinor, P.T.; Lunetta, K.L.; Albert, C.M.; Glazer, N.L.; Ritchie, M.D.; Smith, A.V.; Arking, D.E.; Muller-Nurasyid, M.; Krijthe, B.P.; Lubitz, S.A.; et al. Meta-analysis identifies six new susceptibility loci for atrial fibrillation. Nat. Genet. 2012, 44, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Duygu, B.; Poels, E.M.; da Costa Martins, P.A. Genetics and epigenetics of arrhythmia and heart failure. Front. Genet. 2013, 4, 219. [Google Scholar] [CrossRef] [PubMed]
- Finsterer, J.; Stollberger, C.; Keller, H. Arrhythmia-related workup in hereditary myopathies. J. Electrocardiol. 2012, 45, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Corley, S.D.; Epstein, A.E.; DiMarco, J.P.; Domanski, M.J.; Geller, N.; Greene, H.L.; Josephson, R.A.; Kellen, J.C.; Klein, R.C.; Krahn, A.D.; et al. Relationships between sinus rhythm, treatment, and survival in the atrial fibrillation follow-up investigation of rhythm management (AFFIRM) study. Circulation 2004, 109, 1509–1513. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Talajic, M.; Nattel, S.; Wyse, D.G.; Dorian, P.; Lee, K.L.; Bourassa, M.G.; Arnold, J.M.; Buxton, A.E.; Camm, A.J.; et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N. Engl. J. Med. 2008, 358, 2667–2677. [Google Scholar] [CrossRef] [PubMed]
- Shelton, R.J.; Clark, A.L.; Goode, K.; Rigby, A.S.; Houghton, T.; Kaye, G.C.; Cleland, J.G. A randomised, controlled study of rate versus rhythm control in patients with chronic atrial fibrillation and heart failure: (CAFE-II study). Heart 2009, 95, 924–930. [Google Scholar] [CrossRef] [PubMed]
- Hagens, V.E.; Ranchor, A.V.; van Sonderen, E.; Bosker, H.A.; Kamp, O.; Tijssen, J.G.; Kingma, J.H.; Crijns, H.J.; van Gelder, I.C. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation: Results from the rate control versus electrical cardioversion (RACE) study. J. Am. Coll. Cardiol. 2004, 43, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J.; Kirchhof, P.; Lip, G.Y.; Schotten, U.; Savelieva, I.; Ernst, S.; van Gelder, I.C.; Al-Attar, N.; Hindricks, G.; Prendergast, B.; et al. Guidelines for the management of atrial fibrillation: The task force for the management of atrial fibrillation of the european society of cardiology (ESC). Eur. Heart J. 2010, 31, 2369–2429. [Google Scholar] [CrossRef] [PubMed]
- Wolf, P.A.; Abbott, R.D.; Kannel, W.B. Atrial fibrillation as an independent risk factor for stroke: The framingham study. Stroke 1991, 22, 983–988. [Google Scholar] [CrossRef]
- Pedersen, O.D.; Bagger, H.; Kober, L.; Torp-Pedersen, C. Trandolapril reduces the incidence of atrial fibrillation after acute myocardial infarction in patients with left ventricular dysfunction. Circulation 1999, 100, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Ducharme, A.; Swedberg, K.; Pfeffer, M.A.; Cohen-Solal, A.; Granger, C.B.; Maggioni, A.P.; Michelson, E.L.; McMurray, J.J.; Olsson, L.; Rouleau, J.L.; et al. Prevention of atrial fibrillation in patients with symptomatic chronic heart failure by candesartan in the candesartan in heart failure: Assessment of reduction in mortality and morbidity (CHARM) program. Am. Heart J. 2006, 151, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Nasr, I.A.; Bouzamondo, A.; Hulot, J.S.; Dubourg, O.; le Heuzey, J.Y.; Lechat, P. Prevention of atrial fibrillation onset by β-blocker treatment in heart failure: A meta-analysis. Eur. Heart J. 2007, 28, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Swedberg, K.; Zannad, F.; McMurray, J.J.; Krum, H.; van Veldhuisen, D.J.; Shi, H.; Vincent, J.; Pitt, B. Eplerenone and atrial fibrillation in mild systolic heart failure: Results from the EMPHASIS-HF (eplerenone in mild patients hospitalization and survival study in heart failure) study. J. Am. Coll. Cardiol. 2012, 59, 1598–1603. [Google Scholar] [CrossRef] [PubMed]
- Wilton, S.B.; Leung, A.A.; Ghali, W.A.; Faris, P.; Exner, D.V. Outcomes of cardiac resynchronization therapy in patients with versus those without atrial fibrillation: A systematic review and meta-analysis. Heart Rhythm. 2011, 8, 1088–1094. [Google Scholar] [CrossRef] [PubMed]
- Lopes, C.; Pereira, T.; Barra, S. Cardiac resynchronization therapy in patients with atrial fibrillation: A meta-analysis. Rev. Port. Cardiol. 2014, 33, 717–725. [Google Scholar] [PubMed]
- Brignole, M.; Auricchio, A.; Baron-Esquivias, G.; Bordachar, P.; Boriani, G.; Breithardt, O.A.; Cleland, J.; Deharo, J.C.; Delgado, V.; Elliott, P.M.; et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: The task force on cardiac pacing and resynchronization therapy of the european society of cardiology (ESC): Developed in collaboration with the european heart rhythm association (EHRA). Eur. Heart J. 2013, 15, 1070–1118. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira, J.P.; Santos, M. Heart Failure and Atrial Fibrillation: From Basic Science to Clinical Practice. Int. J. Mol. Sci. 2015, 16, 3133-3147. https://doi.org/10.3390/ijms16023133
Ferreira JP, Santos M. Heart Failure and Atrial Fibrillation: From Basic Science to Clinical Practice. International Journal of Molecular Sciences. 2015; 16(2):3133-3147. https://doi.org/10.3390/ijms16023133
Chicago/Turabian StyleFerreira, João Pedro, and Mário Santos. 2015. "Heart Failure and Atrial Fibrillation: From Basic Science to Clinical Practice" International Journal of Molecular Sciences 16, no. 2: 3133-3147. https://doi.org/10.3390/ijms16023133
APA StyleFerreira, J. P., & Santos, M. (2015). Heart Failure and Atrial Fibrillation: From Basic Science to Clinical Practice. International Journal of Molecular Sciences, 16(2), 3133-3147. https://doi.org/10.3390/ijms16023133





