Mental Health in Multiple Sclerosis Patients without Limitation of Physical Function: The Role of Physical Activity
Abstract
:1. Introduction
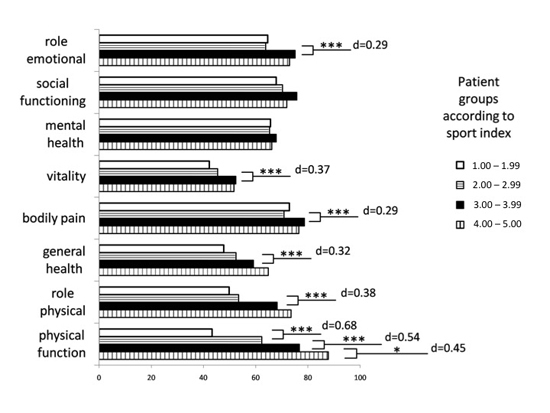
2. Results
| SF-36 | Physical Function | Role Physical | Bodily Pain | General Health | Vitality | Social Function | Role Emotional | Mental Health | |
|---|---|---|---|---|---|---|---|---|---|
| Study sample | mean | 65.24 | 58.90 | 74.09 | 54.63 | 47.47 | 71.62 | 68.2 | 66.23 |
| SD | 29.73 | 40.67 | 28.6 | 21.3 | 19.87 | 26.28 | 40.56 | 18.49 | |
| German healthy controls | mean | 83.57 | 80.0 | 77.1 | 66.05 | 61.75 | 87.66 | 87.74 | 72.79 |
| SD | 23.8 | 34.5 | 28.4 | 21.1 | 19.2 | 19.45 | 28.9 | 17.37 | |
| Group differences | significance | p < 0.001 | p < 0.001 | p = 0.014 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 |
| Effect size (Cohen’s d) | 0.68 | 0.59 | 0.11 | 0.54 | 0.74 | 0.77 | 0.62 | 0.37 |

| Activity | N (Male; Female) | EDSS | MS Duration | Age | BMI | Sport Index | Leisure Index | Work Index | BDI Score | |
|---|---|---|---|---|---|---|---|---|---|---|
| Inactive | 66 (m:16; f:50) | mean | 1.8 | 7.3 | 37.8 | 23.3 | 2.1 | 3.1 | 2.5 | 7.1 |
| SD | 1.0 | 6.0 | 10.4 | 4.0 | 0.4 | 0.9 | 0.7 | 4.4 | ||
| Less active | 66 (m:14; f52) | mean | 1.6 | 8.7 | 40.2 | 23.6 | 2.8 | 3.3 | 2.4 | 7.1 |
| SD | 0.9 | 7.4 | 10.1 | 4.3 | 0.1 | 0.8 | 0.6 | 4.5 | ||
| Active | 67 (m:11; f:56) | mean | 1.8 | 7.7 | 39.3 | 23.5 | 3.3 | 3.5 | 2.4 | 7.0 |
| SD | 1.0 | 6.4 | 8.4 | 3.5 | 0.2 | 0.8 | 0.6 | 4.4 | ||
| Very active | 66 (m:27; f:39) | mean | 1.4 | 7.4 | 40.2 | 22.5 | 4.0 | 3.7 | 2.3 | 6.2 |
| SD | 0.9 | 5.3 | 7.7 | 3.7 | 0.4 | 0.8 | 0.6 | 4.6 | ||

3. Discussion
4. Experimental Section
4.1. Physical Activity
4.2. Health-Related Quality of Life
4.3. Depression
4.4. Analysis and Statistics
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Noseworthy, J.H.; Lucchinetti, C.; Rodriguez, M.; Weinshenker, B.G. Multiple sclerosis. N. Engl. J. Med. 2000, 343, 938–952. [Google Scholar] [CrossRef]
- Motl, R.W.; Gosney, J.L. Effect of exercise training on quality of life in multiple sclerosis: A meta-analysis. Mult. Scler. 2008, 14, 129–135. [Google Scholar] [CrossRef]
- Rudick, R.A.; Miller, D.M. Health-related quality of life in multiple sclerosis: Current evidence, measurement and effects of disease severity and treatment. CNS Drugs 2008, 22, 827–839. [Google Scholar] [CrossRef]
- Sandroff, B.M.; Dlugonski, D.; Weikert, M.; Suh, Y.; Balantrapu, S.; Motl, R.W. Physical activity and multiple sclerosis: New insights regarding inactivity. Acta Neurol. Scand. 2012, 126, 256–262. [Google Scholar] [CrossRef]
- Snook, E.M.; Motl, R.W. Effect of exercise training on walking mobility in multiple sclerosis: A meta-analysis. Neurorehabil. Neural Repair 2008, 23, 108–116. [Google Scholar] [CrossRef]
- Dalgas, U.; Stenager, E. Exercise and disease progression in multiple sclerosis: Can exercise slow down the progression of multiple sclerosis? Ther. Adv. Neurol. Disord. 2012, 5, 81–95. [Google Scholar] [CrossRef]
- Dalgas, U.; Stenager, E.; Ingemann-Hansen, T. Multiple sclerosis and physical exercise: Recommendations for the application of resistance-, endurance- and combined training. Mult. Scler. 2007, 14, 35–53. [Google Scholar] [CrossRef]
- World Health Organization. Promoting Mental Health: Concepts, Emerging evidence, Practice: A report of the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- McCabe, M.P.; McKern, S. Quality of life and multiple sclerosis: Comparison between people with multiple sclerosis and people from the general population. J. Clin. Psychol. Med. Settings 2002, 9, 287–295. [Google Scholar] [CrossRef]
- Montel, S.R.; Bungener, C. Coping and quality of life in one hundred and thirty five subjects with multiple sclerosis. Mult. Scler. 2007, 13, 393–401. [Google Scholar] [CrossRef]
- Morales-Gonzales, J.M.; Benito-Leon, J.; Rivera-Navarro, J.; Mitchell, A.J. A systematic approach to analyse health-related quality of life in multiple sclerosis: The GEDMA study. Mult. Scler. 2004, 10, 47–54. [Google Scholar] [CrossRef]
- Bullinger, M.; Kirchberger, I. Der SF-36 Fragebogen zum Gesundheitszustand; Göttingen Bern Toronto Seattle: Hogrefe, Germany, 1998. [Google Scholar]
- Zwibel, H. Health and quality of life in patients with relapsing multiple sclerosis: Making the intangible tangible. J. Neurol. Sci. 2009, 287, S11–S16. [Google Scholar] [CrossRef]
- Benito-Leon, J.; Morales, J.M.; Rivera-Navarro, J.; Mitchell, A.J. A review about the impact of multiple sclerosis on health-related quality of life. Disabil. Rehabil. 2003, 25, 1291–1303. [Google Scholar] [CrossRef]
- Benito-Leon, J.; Morales, J.M.; Rivera-Navarro, J. Health-related quality of life and its relationship to cognitive and emotional functioning in multiple sclerosis patients. Eur. J. Neurol. 2002, 9, 497–502. [Google Scholar] [CrossRef]
- Glanz, B.I.; Healy, B.C.; Rintell, D.J.; Jaffin, S.K.; Bakshi, R.; Weiner, H.L. The association between cognitive impairment and quality of life in patients with early multiple sclerosis. J. Neurol. Sci. 2010, 290, 75–79. [Google Scholar] [CrossRef]
- Tepavcevic, D.K.; Kostic, J.; Basuroski, I.D.; Stojsavljevic, N.; Pekmezovic, T.; Drulovic, J. The impact of sexual dysfunction on the quality of life measured by MSQoL-54 in patients with multiple sclerosis. Mult. Scler. 2008, 14, 1131–1136. [Google Scholar] [CrossRef]
- Wynia, K.; Middel, B.; van Dijk, J.P.; de Keyser, J.H.; Reijneveld, S.A. The impact of disabilities on quality of life in people with multiple sclerosis. Mult. Scler. 2008, 14, 972–980. [Google Scholar] [CrossRef]
- Motl, R.W.; Suh, Y.; Weikert, M. Symptom cluster and quality of life in multiple sclerosis. J. Pain Symptom Manag. 2010, 39, 1025–1032. [Google Scholar] [CrossRef]
- Goretti, B.; Portaccio, E.; Zipoli, V.; Hakiki, B.; Siracusa, G.; Sorbi, S.; Amato, M.P. Coping strategies, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol. Sci. 2009, 30, 15–20. [Google Scholar] [CrossRef]
- Motl, R.W.; Snook, E.M.; McAuley, E.; Gliottoni, R.C. Symptoms, self-efficacy, and physical activity among individuals with multiple sclerosis. Res. Nurs. Health 2006, 29, 597–606. [Google Scholar] [CrossRef]
- Stuifbergen, A.K.; Blozis, S.A.; Harrison, T.C.; Becker, H.A. Exercise, functional limitations, and quality of life: A longitudinal study of persons with multiple sclerosis. Arch. Phys. Med. Rehabil. 2006, 87, 935–943. [Google Scholar] [CrossRef]
- Motl, R.W.; Snook, E.M.; McAuley, E.; Scott, J.A.; Gliottoni, R.C. Are physical activity and symptoms correlates of functional limitations and disability in multiple sclerosis? Rehabil. Psychol. 2007, 52, 463–469. [Google Scholar] [CrossRef]
- Heesen, C.; Böhm, J.; Reich, C.; Kasper, J.; Goebel, M.; Gold, S.M. Patient perception of bodily functions in multiple sclerosis: Gait and visual function are the most valuable. Mult. Scler. 2008, 14, 988–991. [Google Scholar] [CrossRef]
- Tallner, A.; Waschbisch, A.; Wenny, I.; Schwab, S.; Hentschke, C.; Pfeifer, K.; Mäurer, M. Multiple sclerosis relapses are not associated with exercise. Mult. Scler. 2012, 18, 232–235. [Google Scholar] [CrossRef]
- Van Poppel, M.N.; Chinapaw, M.J.; Mokkink, L.B.; van Mechelen, W.; Terwee, C.B. Physical activity questionnaires for adults: A systematic review of measurement properties. Sports Med. 2010, 40, 565–600. [Google Scholar] [CrossRef]
- Wagner, P.; Singer, R.; Woll, A.; Tittlbach, S.; Bös, K. Der Zusammenhang von habitueller körperlicher Aktivität und Gesundheit: Dargestellt an zwei Feldstudien. Z. Gesundheitspsychol. 2004, 12, 139–147. [Google Scholar] [CrossRef]
- Tallner, A. Körperliche Aktivität und körperliche Funktionsfähigkeit—Erfassung und Wechselwirkung bei Personen mit Multipler Sklerose. Ph.D Dissertation, Friedrich Alexander-Universität Erlangen-Nürnberg, Erlangen, Germany, 2012. [Google Scholar]
- Mostert, S.; Kesselring, J. Effects of a short-term exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult. Scler. 2002, 8, 161–168. [Google Scholar] [CrossRef]
- Wagner, P.; Singer, R. Ein Fragebogen zur Erfassung der habituellen körperlichen Aktivität verschiedener Bevölkerungsgruppen. Sportwissenschaft 2003, 33, 383–397. [Google Scholar]
- Baecke, J.A.H.; Burema, J.; Frijters, J.E.R. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am. J. Clin. Nutr. 1982, 36, 936–942. [Google Scholar]
- Singer, R.; Wagner, P. Überprüfung eines (Kurz-)Fragebogens zur Erfassung der habituellen körperlichen Aktivität. In Festschrift für Dieter Voigt; Voight, D., Meck, S., Klussmann, P.G., Eds.; LIT: Münster, Germany, 2001; pp. 359–388. [Google Scholar]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Bullinger, M. German translation and psychometric testing of the SF-36 Health Survey: Preliminary results from the IQOLA project. Soc. Sci. Med. 1995, 41, 1359–1366. [Google Scholar] [CrossRef]
- Dallmeijer, A.J.; Dekker, J.; Knol, D.L.; Kalmijn, S.; Schepers, V.P.M.; de Groot, V.; Lindeman, E.; Beelen, A.; Lankhorst, G.J.; FuPro Study Group. Dimensional structure of the SF-36 in neurological patients. J. Clin. Epidemiol. 2006, 59, 541–543. [Google Scholar] [CrossRef]
- Hobart, J.; Freeman, J.; Lamping, D.; Fitzpatrick, R.; Thompson, A. The SF-36 in multiple sclerosis: Why basic assumptions must be tested. J. Neurol. Neurosurg. Psychiatry 2001, 71, 363–370. [Google Scholar] [CrossRef]
- Hautzinger, M.; Bailer, M.; Worall, H.; Keller, F. Beck Depressionsinventar (BDI); Huber: Bern, Switzerland, 1995. [Google Scholar]
- Levy, S.S.; Li, K.-K.; Cardinal, B.J.; Maddalozzo, G.F. Transitional shifts in exercise behavior among women with multiple sclerosis. Disabil. Health J. 2009, 2, 216–223. [Google Scholar] [CrossRef]
- Neill, J.; Belan, I.; Ried, K. Effectiveness of non-pharmacological interventions for fatigue in adults with multiple sclerosis, rheumatoid arthritis, or systemic lupus erythematosus: A systematic review. J. Adv. Nurs. 2006, 56, 617–635. [Google Scholar] [CrossRef]
- Oken, B.S.; Kishiyama, S.; Zajdel, D.; Bourdette, D.; Carlsen, J.; Haas, M.; Hugos, C.; Kraemer, D.F.; Lawrence, J.; Mass, M. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology 2004, 62, 2058–2064. [Google Scholar] [CrossRef]
- White, L.; Dressendorfer, R. Exercise and multiple sclerosis. Sports Med. 2004, 34, 1077–1100. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tallner, A.; Waschbisch, A.; Hentschke, C.; Pfeifer, K.; Mäurer, M. Mental Health in Multiple Sclerosis Patients without Limitation of Physical Function: The Role of Physical Activity. Int. J. Mol. Sci. 2015, 16, 14901-14911. https://doi.org/10.3390/ijms160714901
Tallner A, Waschbisch A, Hentschke C, Pfeifer K, Mäurer M. Mental Health in Multiple Sclerosis Patients without Limitation of Physical Function: The Role of Physical Activity. International Journal of Molecular Sciences. 2015; 16(7):14901-14911. https://doi.org/10.3390/ijms160714901
Chicago/Turabian StyleTallner, Alexander, Anne Waschbisch, Christian Hentschke, Klaus Pfeifer, and Mathias Mäurer. 2015. "Mental Health in Multiple Sclerosis Patients without Limitation of Physical Function: The Role of Physical Activity" International Journal of Molecular Sciences 16, no. 7: 14901-14911. https://doi.org/10.3390/ijms160714901
APA StyleTallner, A., Waschbisch, A., Hentschke, C., Pfeifer, K., & Mäurer, M. (2015). Mental Health in Multiple Sclerosis Patients without Limitation of Physical Function: The Role of Physical Activity. International Journal of Molecular Sciences, 16(7), 14901-14911. https://doi.org/10.3390/ijms160714901