Angiotensin III Induces JAK2/STAT3 Leading to IL-6 Production in Rat Vascular Smooth Muscle Cells
Abstract
:1. Introduction
2. Results
2.1. STAT3 Activation by Ang II and Ang III in Wistar VSMCs
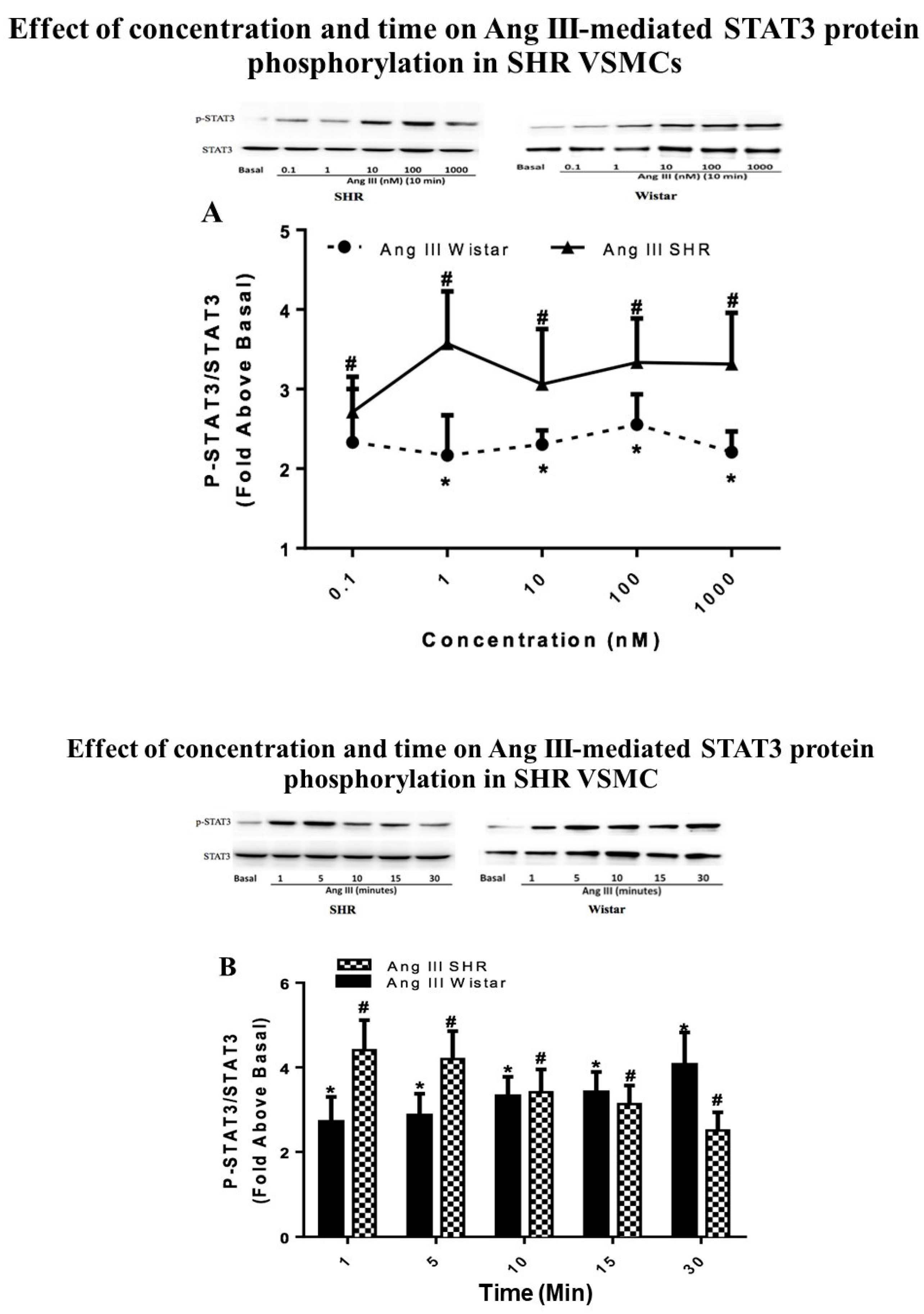
2.2. STAT3 Activation by Ang III in VSMCs from SHRs
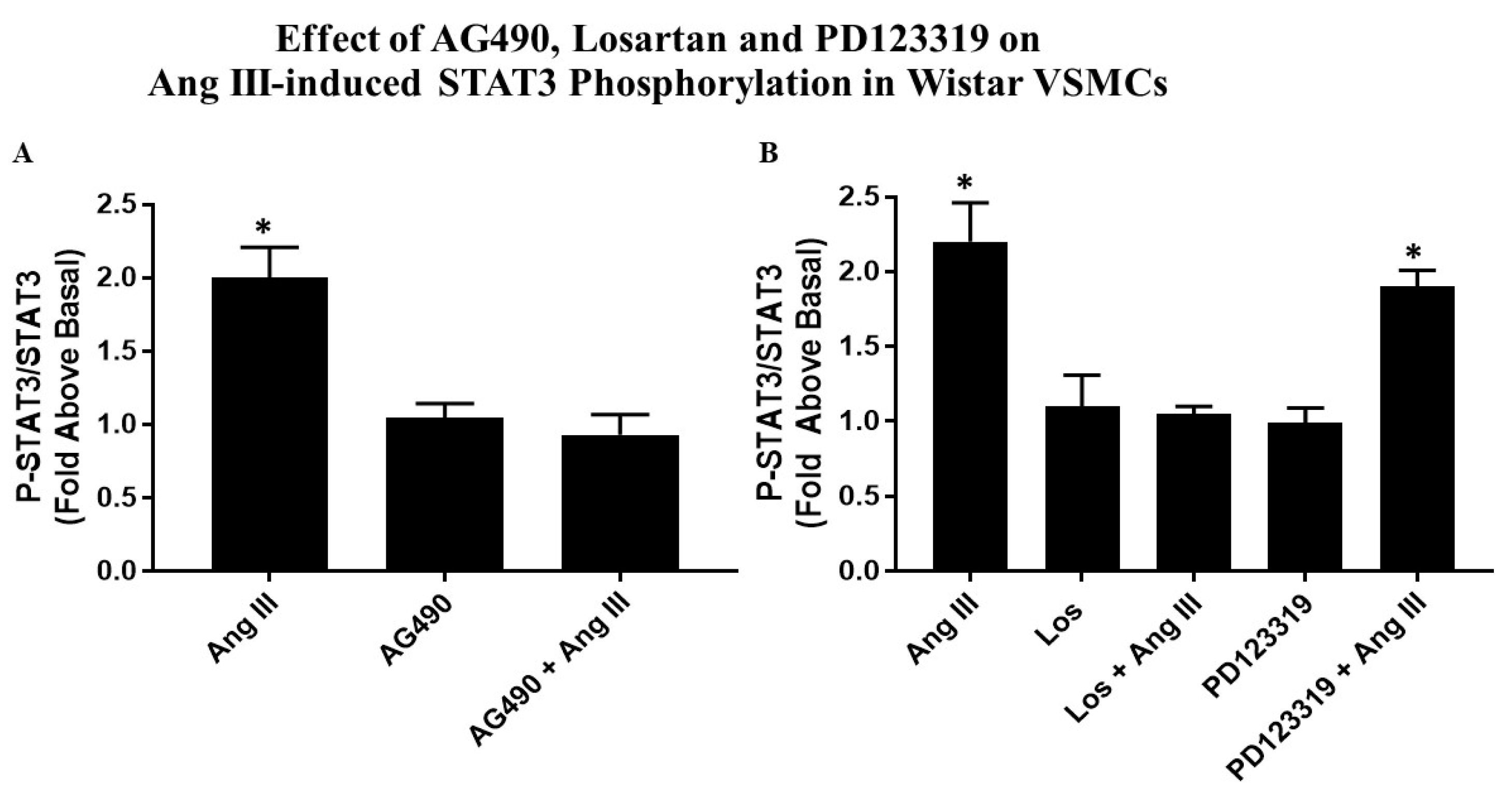
2.3. Effects of AG490 and Ang Receptor Blockers on Ang III-induced STAT3 Phosphorylation
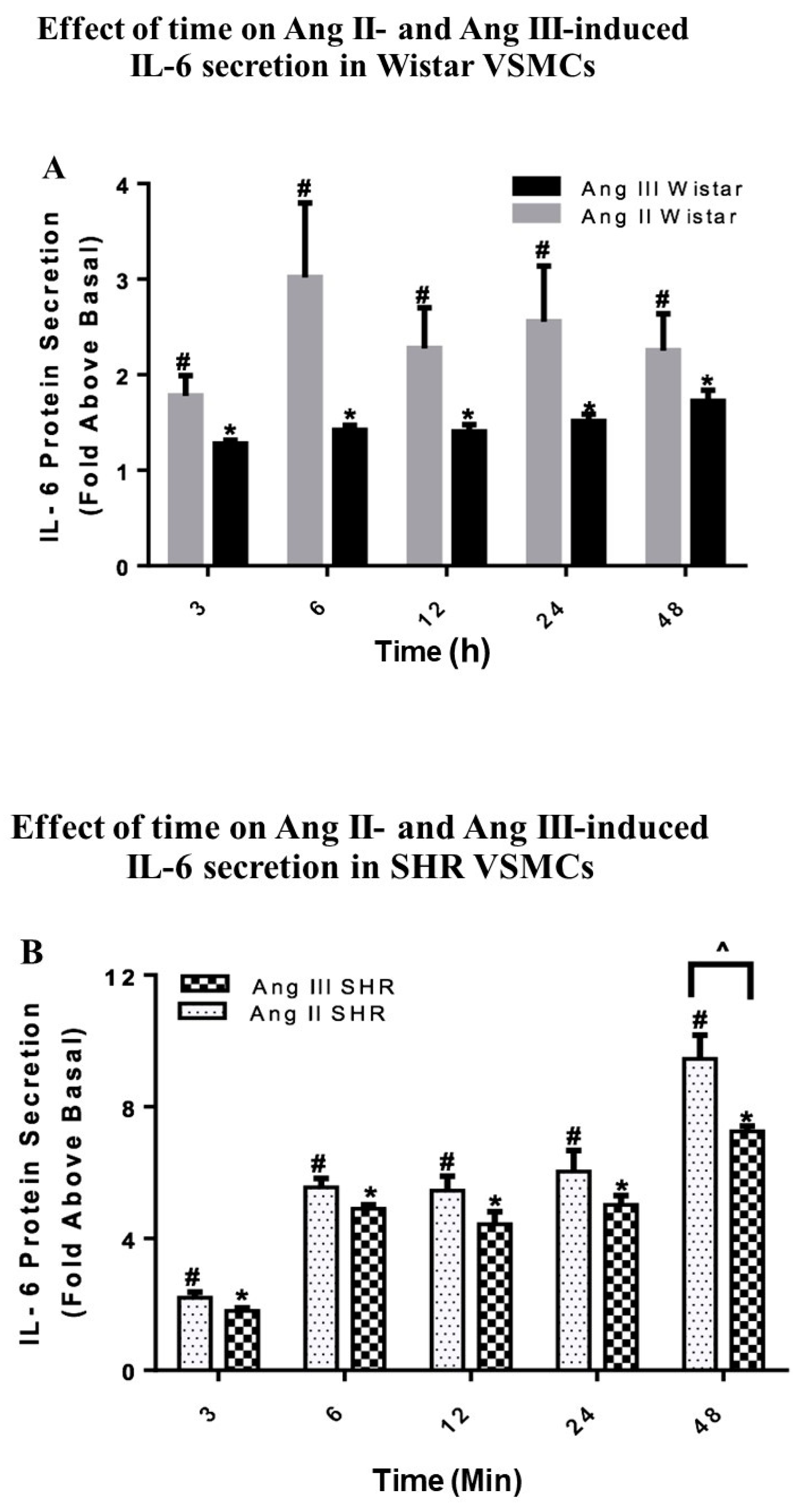
2.4. Effects of Ang II and Ang III on Wistar VSMC IL-6 Secretion
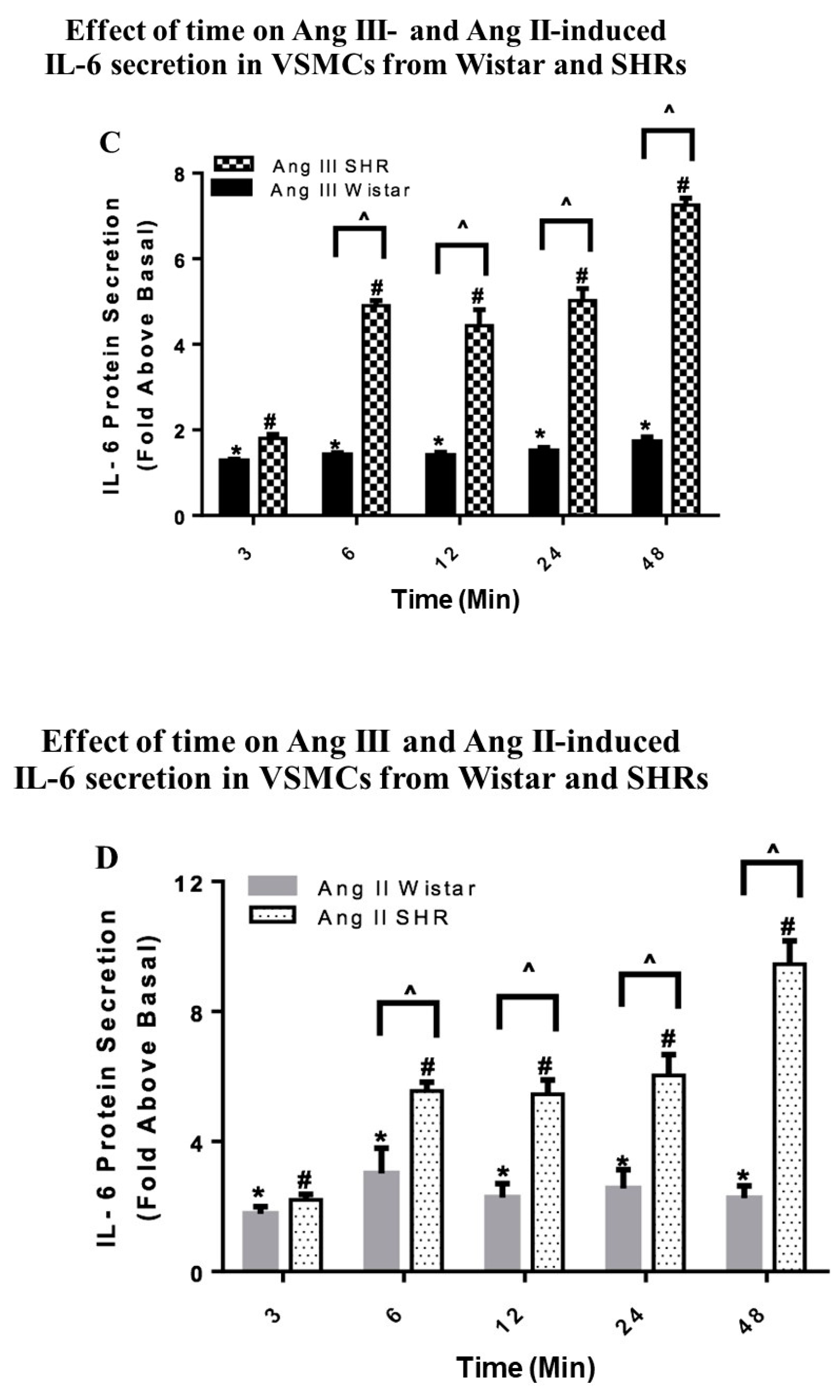
2.5. Effects of Ang II and Ang III on SHR VSMC IL-6 Secretion
2.6. Effects of AG490, Losartan and PD123319 on Ang III-induced IL-6 Secretion
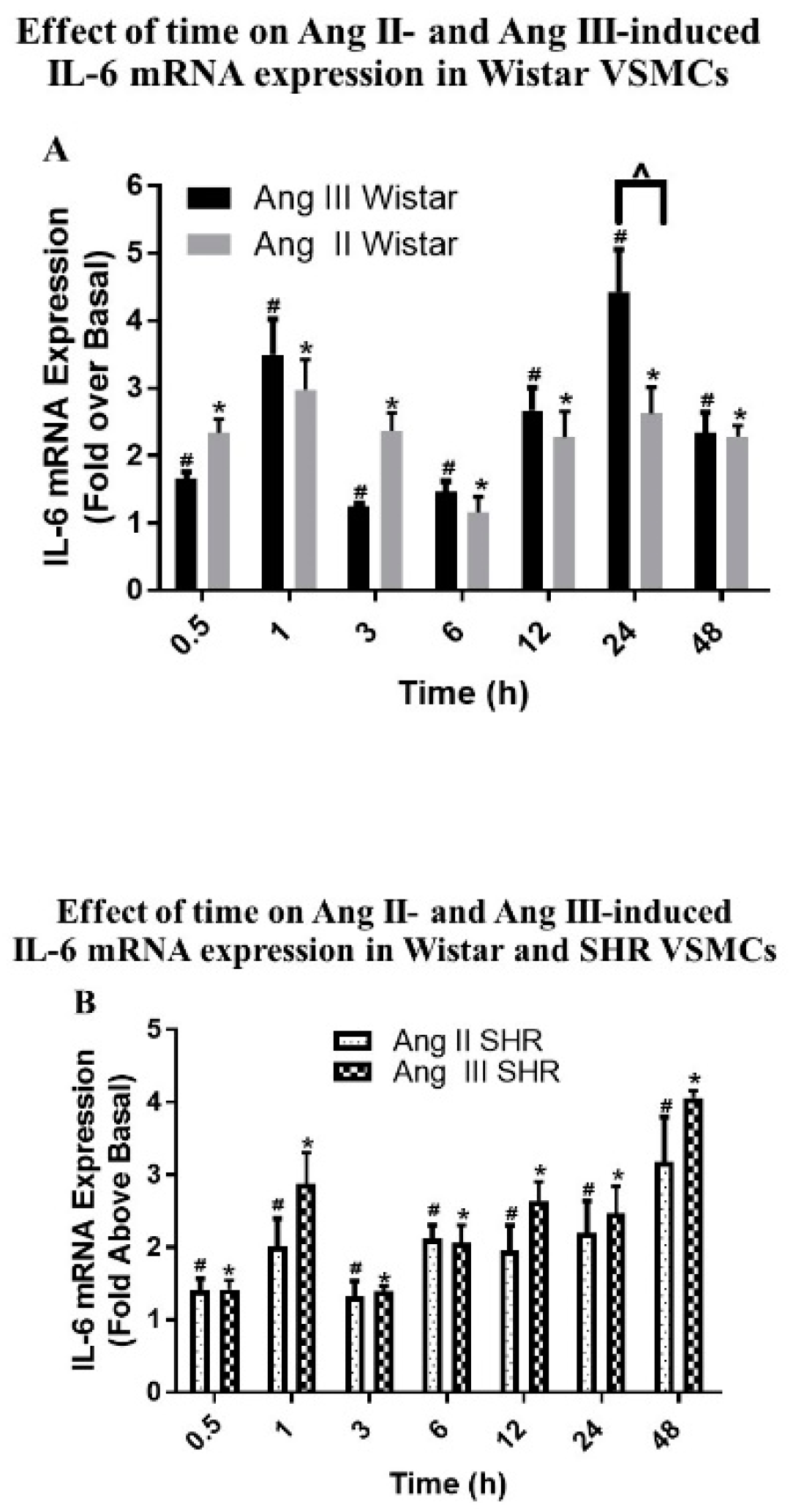
2.7. Effects of Ang II and Ang III on IL-6 mRNA Expression in Wistar VSMCs
2.8. Effects of Ang II and Ang III on IL-6 mRNA Expression in SHR VSMCs
2.9. Effects of Ang III in Wistar versus SHR VSMCs
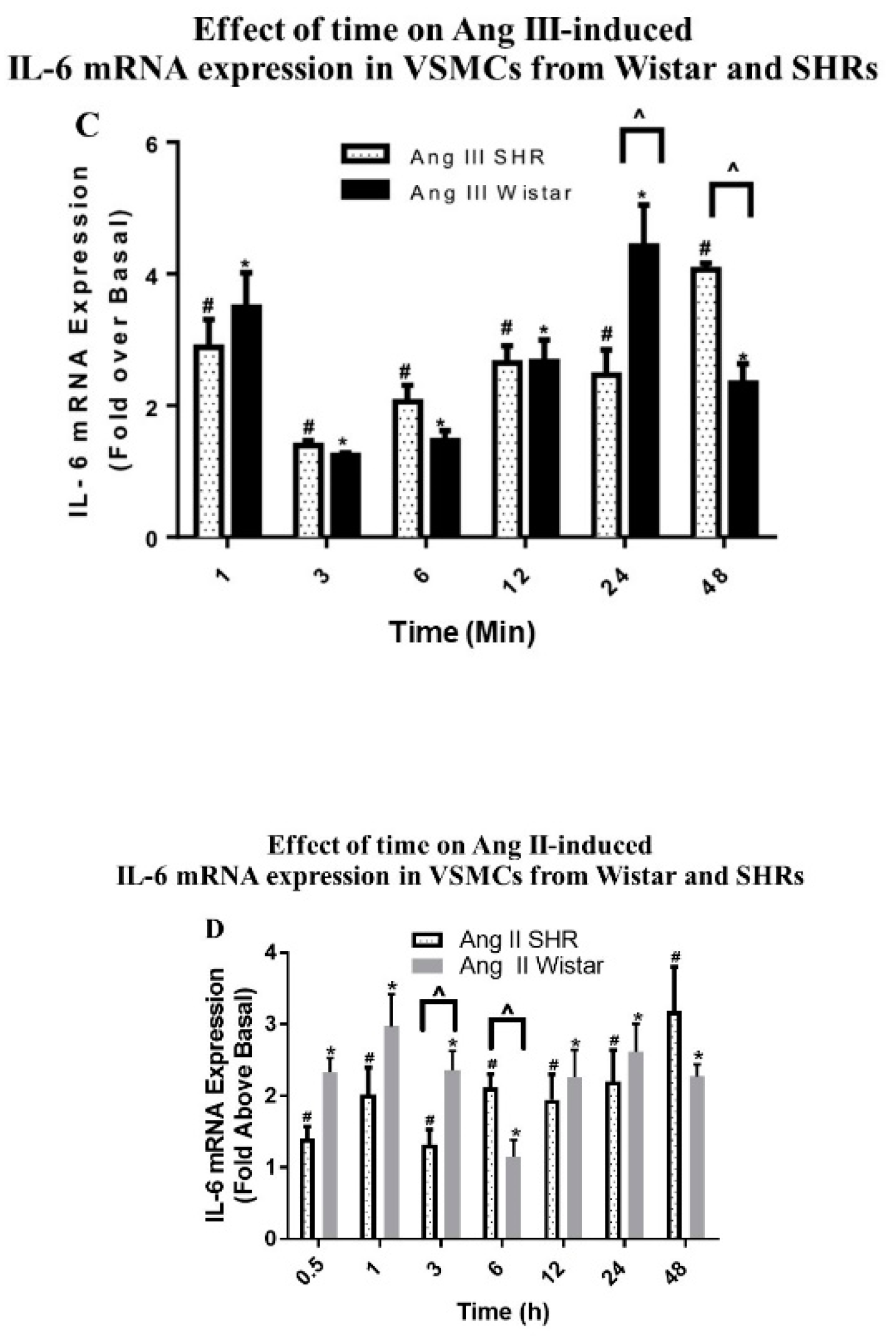
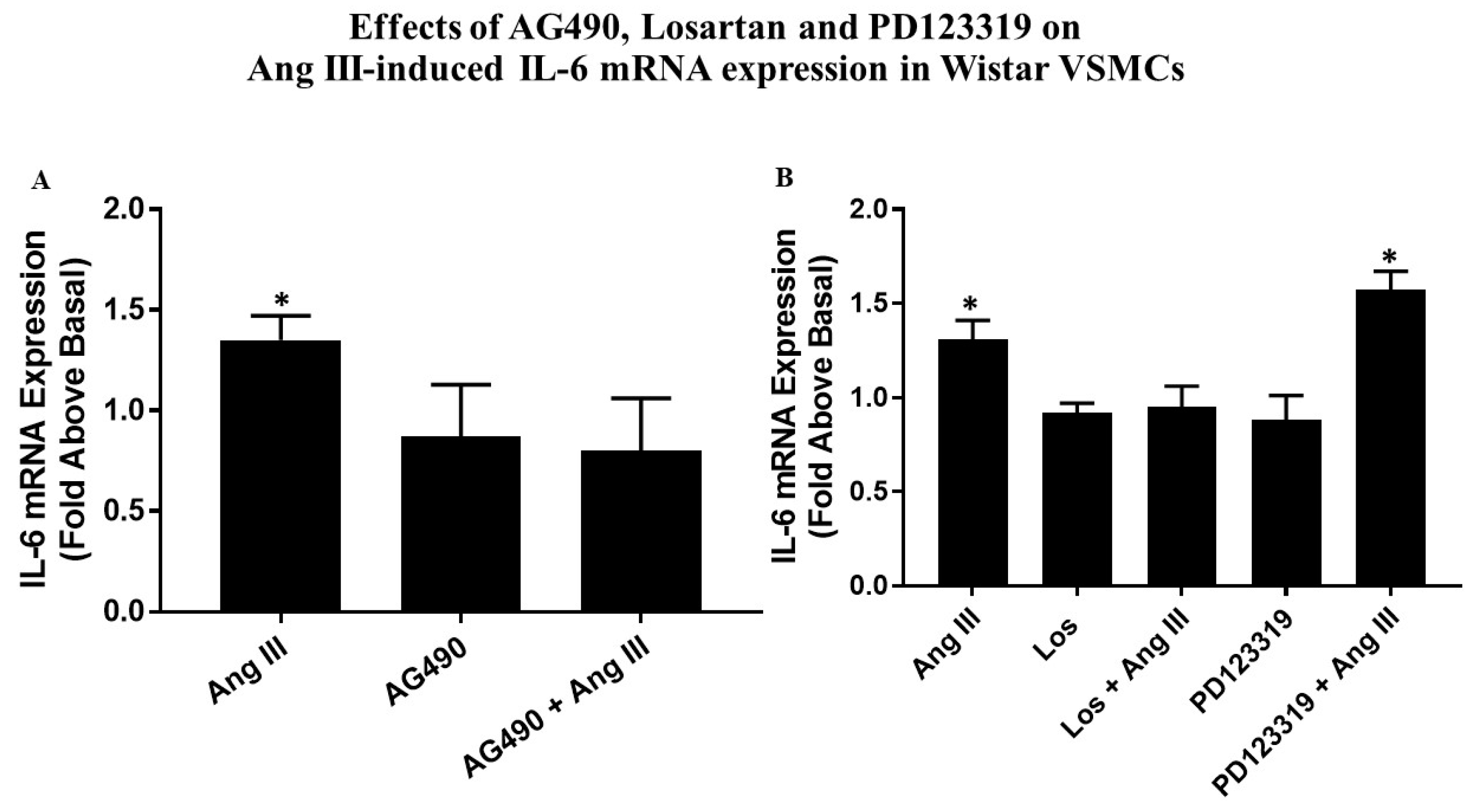
2.10. Effects of AG490, Losartan and PD123319 on Ang III-induced IL-6 mRNA Expression
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Isolation and Culture of Primary VSMCs
4.3. Cell Lysate Preparation
4.4. Western Blotting
4.5. Total RNA Extraction and Measurement of IL-6 mRNA Levels
4.6. Enzyme-Linked Immunosorbent Assay
4.7. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| MDPI | Multidisciplinary Digital Publishing Institute |
| Ang | Angiotensin |
| AT1R | angiotensin type I receptor |
| AT2R | angiotensin type 2 receptor |
| ANOVA | analysis of variance |
| BCA | bicinchoninic acid |
| DMEM/F12 | Dulbecco’s modified Eagles Medium/F12 |
| DMSO | dimethyl sulfoxide |
| ECL | enhanced chemiluminescence |
| EDTA | ethylenediamine tetraacetic acid |
| ELISA | enzyme linked immunosorbent assay |
| FBS | fetal bovine serum |
| INF | interferon |
| IL- | interleukin |
| JAK2/STAT3 | Janus kinase-2/ signal transducer and activators of transcription-3 |
| MAPK | mitogen activated protein kinase |
| PBS | phosphate buffer saline |
| qPCR | quantitative PCR |
| RAAS | renin angiotensin aldosterone system |
| SDS | sodium dodecyl sulfate |
| SHR | spontaneously hypertensive rat |
| VSMC | vascular smooth muscle cell |
References
- Atlas, S.A. The renin-angiotensin aldosterone system: Pathophysiological role and pharmacologic inhibition. J. Manag. Care Pharm. 2007, 13, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Laragh, J. Laragh’s lessons in pathophysiology and clinical pearls for treating hypertension. Am. J. Hypertens. 2001, 14, 837–854. [Google Scholar] [CrossRef]
- Mehta, P.K.; Griendling, K.K. Angiotensin II cell signaling: Physiological and pathological effects in the cardiovascular system. Am. J. Physiol Cell Physiol. 2007, 292, C82–C97. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.W.; Yamamoto, B.J.; Harding, J.W. Angiotensin receptor subtype mediated physiologies and behaviors: New discoveries and clinical targets. Prog. Neurobiol 2008, 84, 157–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, J.W.; Harding, J.W. The brain renin–angiotensin system: A diversity of functions and implications for CNS diseases. Pflüg. Arch. 2013, 46, 133–151. [Google Scholar] [CrossRef]
- Nguyen Dinh Cat, A.; Touyz, R.M. A new look at the renin-angiotensin system—focusing on the vascular system. Peptides 2011, 32, 2141–2150. [Google Scholar] [CrossRef]
- Yugandhar, V.G.; Clark, M.A. Angiotensin III: A physiological relevant peptide of the renin angiotensin system. Peptides 2013, 46, 26–32. [Google Scholar] [CrossRef]
- Kandalam, U.; Sarmiento, N.; Haspula, D.; Clark, M.A. Angiotensin III induces signal transducer and activator of transcription 3 and interleukin-6 mRNA levels in cultured rat astrocytes. J. Renin-Angiotensin Aldosterone Syst. 2014. [Google Scholar] [CrossRef]
- Aaronson, D.S.; Horvath, C.M. A road map for those who don’t know JAK-STAT. Science 2002, 296, 1653–1655. [Google Scholar] [CrossRef]
- Rawlings, J.S.; Rosler, K.M.; Harrison, D.A. The JAK/STAT signaling pathway. J. Cell Sci. 2004, 117, 1281–1283. [Google Scholar] [CrossRef] [Green Version]
- Kandalam, U.; Clark, M.A. Angiotensin II activates JAK2/STAT3 pathway and induces interleukin-6 production in cultured rat brainstem astrocytes. Regul. Pept. 2010, 159, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Kandalam, U.; Palanisamy, M.; Clark, M.A. Angiotensin II induces cell growth and IL-6 mRNA expression through the JAK2-STAT3 pathway in rat cerebellar astrocytes. Jakstat 2012, 1, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Satou, R.; Gonzalez-Villalobos, R.A. JAK-STAT and the renin-angiotensin system: The role of the JAK-STAT pathway in blood pressure and intrarenal renin-angiotensin system regulation. Jakstat 2012, 1, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Marrero, M.B.; Schieffer, B.; Paxton, W.G.; Heerdt, L.; Berk, B.C.; Delafontaine, P.; Bernstein, K.E. Direct stimulation of Jak/STAT pathway by the angiotensin II AT1 receptor. Nature 1995, 375, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Frank, G.D.; Saito, S.; Motley, E.D.; Sasaki, T.; Ohba, M.; Kuroki, T.; Inagami, T.; Eguchi, S. Requirement of Ca2+ and PKCδ for Janus kinase 2 activation by angiotensin II: Involvement of PYK2. Mol. Endocrinol. 2002, 16, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Pacurari, M.; Kafoury, R.; Tchounwou, P.B.; Ndebele, K. The Renin-Angiotensin-aldosterone system in vascular inflammation and remodeling. Int. J. Inflam. 2014. [Google Scholar] [CrossRef] [PubMed]
- Steiner, M.K.; Syrkina, O.L.; Kolliputi, N.; Mark, E.J.; Hales, C.A.; Waxman, A.B. Interleukin-6 overexpression induces pulmonary hypertension. Circ. Res. 2009, 104, 236–244. [Google Scholar] [CrossRef]
- Funakoshi, Y.; Ichiki, T.; Ito, K.; Takeshita, A. Induction of interleukin-6 expression by angiotensin II in rat vascular smooth muscle cells. Hypertension 1999, 34, 118–125. [Google Scholar] [CrossRef]
- Recinos, A.; LeJeune, W.S.; Sun, H.; Lee, C.Y.; Tieu, B.C.; Lu, M.; Hou, T.; Boldogh, I.; Tilton, R.; Brasier, A.R. Angiotensin II induces IL-6 expression and the Jak-STAT3 pathway in aortic adventitia of LDL receptor-deficient mice. Atherosclerosis 2007, 194, 125–133. [Google Scholar] [CrossRef] [Green Version]
- Clark, M.A.; Tran, H.; Nguyen, C. Angiotensin III stimulates ERK1/2 mitogen-activated protein kinases and astrocyte growth in cultured rat astrocytes. Neuropeptides 2011, 45, 329–335. [Google Scholar] [CrossRef]
- Clark, M.A.; Nguyen, C.; Tran, H. Angiotensin III induces c-Jun N-terminal kinase leading to proliferation of rat astrocytes. Neurochem. Res. 2012, 37, 1475–1481. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.A.; Nguyen, C.; Tran, H. Distinct Molecular Effects of Angiotensin II and Angiotensin III in Rat Astrocytes. Int. J. Hypertens. 2013. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, Z.A.; Patel, P.; Clark, M.A. p38 Mitogen-activated protein kinase is stimulated by both angiotensin II and angiotensin III in cultured rat astrocytes. J. Recept. Signal Transduct. Res. 2014, 34, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Guilluy, C.; Brégeon, J.; Toumaniantz, G.; Rolli-Derkinderen, M.; Retailleau, K.; Loufrani, L.; Henrion, D.; Scalbert, E.; Torres, R.M.; Offermanns, S.; et al. The Rho exchange factor Arhgef1 mediates the effects of angiotensin II on vascular tone and blood pressure. Nat. Med. 2010, 16, 183–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banes-Berceli, A.K.; Al-Azawi, H.; Proctor, D.; Qu, H.; Femminineo, D.; Hill-Pyror, C.; Webb, R.C.; Brands, M.W. Angiotensin II utilizes Janus kinase 2 in hypertension, but not in the physiological control of blood pressure, during low-salt intake. Am. J. Physiol Regul. Integr. Comp. Physiol. 2011, 301, R1169–R1176. [Google Scholar] [CrossRef] [Green Version]
- Kirabo, A.; Kearns, P.N.; Jarajapu, Y.P.; Sasser, J.M.; Oh, S.P.; Grant, M.B.; Kasahara, H.; Cardounel, A.J.; Baylis, C.; Wagner, K.U.; et al. Vascular smooth muscle Jak2 mediates angiotensin II-induced hypertension via increased levels of reactive oxygen species. Cardiovas. Res. 2011, 91, 171–179. [Google Scholar] [CrossRef] [Green Version]
- Banes, A.K.; Shaw, S.; Jenkins, J.; Redd, H.; Amiri, F.; Pollock, D.M.; Marrero, M.B. Angiotensin II blockade prevents hyperglycemia-induced activation of JAK and STAT proteins in diabetic rat kidney glomeruli. Am. J. Physiol. Ren. Physiol. 2004, 286, F653–F659. [Google Scholar] [CrossRef] [Green Version]
- Han, J.; Ye, S.; Zou, C.; Chen, T.; Wang, J.; Li, J.; Xu, L.; Huang, W.; Wang, Y.; Liang, G. Angiotensin II causes biphasic STAT3 activation through TLR4 to initiate cardiac remodeling. Hypertension 2018, 72, 1301–1311. [Google Scholar] [CrossRef]
- Griendling, K.K.; Ushio-Fukai, M.; Lassègue, B.; Alexander, R.W. Angiotensin II signaling in vascular smooth muscle. Hypertension 1997, 29, 366–370. [Google Scholar] [CrossRef]
- Yamada, T.; Kondo, T.; Numaguchi, Y.; Tsuzuki, M.; Matsubara, T.; Manabe, I.; Sata, M.; Nagai, R.; Murohara, T. Angiotensin II receptor blocker inhibits neointimal hyperplasia through regulation of smooth muscle–like progenitor cells. Arter. Thromb. Vasc. Biol. 2007, 27, 2363–2369. [Google Scholar] [CrossRef]
- Han, Y.; Runge, M.S.; Brasier, A.R. Angiotensin II induces interleukin-6 transcription in vascular smooth muscle cells through pleiotropic activation of nuclear factor-κB transcription factors. Circ. Res. 1999, 84, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Loppnow, H.; Libby, P. Proliferating or interleukin 1-activated human vascular smooth muscle cells secrete copious interleukin 6. J. Clin. Invest. 1990, 85, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Szallasi, Z. Genetic network analysis in light of massivelyparallel biological data acquisition. Pac. Symp. Biocomput. 1999, 4, 5–16. [Google Scholar]
- Baldi, P.; Long, A.D. A Bayesian framework for the analysisof microarray expression data: Regularized t-test and statisticalinferences of gene changes. Bioinformatics 2001, 17, 509–519. [Google Scholar] [CrossRef]
- Greenbaum, D.; Colangelo, C.; Williams, K.; Gerstein, M. Comparing protein abundance and mRNA expression levels on agenomic scale. Genome Biol. 2003, 4, 117. [Google Scholar] [CrossRef]
- Ross, R. The smooth muscle cell. II. Growth of smooth muscle in culture and formation of elastic fibers. J. Cell Biol. 1971, 50, 172–186. [Google Scholar] [CrossRef]
- Battle, T.; Arnal, J.F.; Challah, M.; Michel, J.B. Selective isolation of rat aortic wall layers and their cell types in culture—Application to converting enzyme activity measurement. Tissue Cell 1994, 26, 943–955. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef] [PubMed]


© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanazi, A.Z.; Clark, M.A. Angiotensin III Induces JAK2/STAT3 Leading to IL-6 Production in Rat Vascular Smooth Muscle Cells. Int. J. Mol. Sci. 2019, 20, 5551. https://doi.org/10.3390/ijms20225551
Alanazi AZ, Clark MA. Angiotensin III Induces JAK2/STAT3 Leading to IL-6 Production in Rat Vascular Smooth Muscle Cells. International Journal of Molecular Sciences. 2019; 20(22):5551. https://doi.org/10.3390/ijms20225551
Chicago/Turabian StyleAlanazi, Ahmed Z., and Michelle A. Clark. 2019. "Angiotensin III Induces JAK2/STAT3 Leading to IL-6 Production in Rat Vascular Smooth Muscle Cells" International Journal of Molecular Sciences 20, no. 22: 5551. https://doi.org/10.3390/ijms20225551



