SpeS: A Novel Superantigen and Its Potential as a Vaccine Adjuvant against Strangles
Abstract
:1. Introduction
2. Results
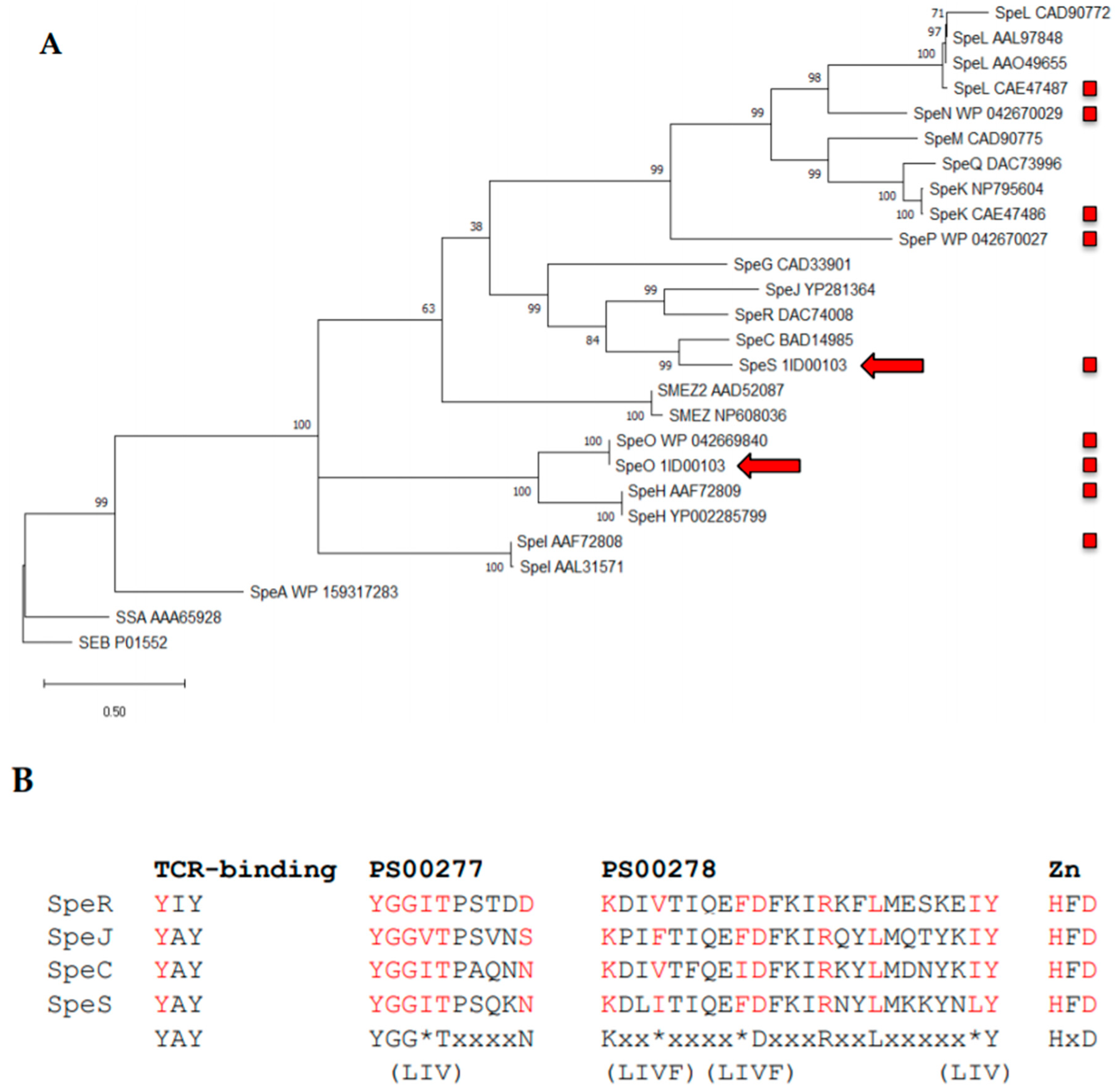
2.1. Identification of SpeS in Streptococcus equi Subspecies Zooepidemicus Strain 1ID00103
2.2. Disruption of the TCR-Binding Site in SpeS Impairs T Cell Proliferation In Vitro While Retaining Binding to MHC Class II Molecules
2.3. S. equi Surface Proteins Fused to SpeSY39I Are Devoid of Mitogenic Activity In Vitro
2.4. S. equi proteins Fused to SpeS Retain Their Ability To Bind to MHC Class II Molecules
2.5. Expression of IFNγ Decreased In Vitro After Stimulation with S. equi Surface Proteins Fused SpeSY39I
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains and DNA Extraction
4.2. Cloning and Purification of speS and Recombinant Fusion Proteins
4.3. Stimulation of Peripheal Blood Mononuclear Cells and Thymmidine Incorporation Assay
4.4. Fluorescein Isothiocyanate (FITC) Labelled Recombinant Fusion Proteins and Detection of MHC Class II Binding
4.5. Measurement of IFNγ, TNFα, IL-10 and IL-6 Expression by qPCR
4.6. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Webb, K.; Jolley, K.A.; Mitchell, Z.; Robinson, C.; Newton, J.R.; Maiden, M.C.J.; Waller, A. Development of an unambiguous and discriminatory multilocus sequence typing scheme for the Streptococcus zooepidemicus group. Microbiology 2008, 154, 3016–3024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jorm, L.R.; Love, D.N.; Bailey, G.D.; McKay, G.M.; Briscoe, D.A. Genetic structure of populations of beta-haemolytic Lancefield group C streptococci from horses and their association with disease. Res. Vet. Sci. 1994, 57, 292–299. [Google Scholar] [CrossRef]
- Waller, A.S. Strangles: A pathogenic legacy of the war horse. Vet. Rec. 2016, 178, 91–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waller, A.S. New perspectives for the diagnosis, control, treatment, and prevention of strangles in horses. Vet. Clin. North Am. Equine Pract. 2014, 30, 591–607. [Google Scholar] [CrossRef] [PubMed]
- Holden, M.T.; Heather, Z.; Paillot, R.; Steward, K.F.; Webb, K.; Ainslie, F.; Jourdan, T.; Bason, N.C.; Holroyd, N.E.; Mungall, K.; et al. Genomic evidence for the evolution of Streptococcus equi: Host restriction, increased virulence, and genetic exchange with human pathogens. PloS Pathog. 2009, 5, e1000346. [Google Scholar] [CrossRef] [Green Version]
- Waller, A.S.; Robinson, C. Streptococcus zooepidemicus and Streptococcus equi evolution: The role of CRISPRs. Biochem. Soc. Trans. 2013, 41, 1437–1443. [Google Scholar] [CrossRef]
- Fraser, J.D.; Proft, T. The bacterial superantigen and superantigen-like proteins. Immunol. Rev. 2008, 225, 226–243. [Google Scholar] [CrossRef]
- Bette, M.; Schafer, M.K.; van Rooijen, N.; Weihe, E.; Fleischer, B. Distribution and kinetics of superantigen-induced cytokine gene expression in mouse spleen. J. Exp. Med. 1993, 178, 1531–1539. [Google Scholar] [CrossRef] [Green Version]
- Miethke, T.; Wahl, C.; Heeg, K.; Echtenacher, B.; Krammer, P.H.; Wagner, H. T cell-mediated lethal shock triggered in mice by the superantigen staphylococcal enterotoxin B: Critical role of tumor necrosis factor. J. Exp. Med. 1992, 175, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Fast, D.J.; Schlievert, P.M.; Nelson, R.D. Toxic shock syndrome-associated staphylococcal and streptococcal pyrogenic toxins are potent inducers of tumor necrosis factor production. Infect. Immun. 1989, 57, 291–294. [Google Scholar] [CrossRef] [Green Version]
- Fraser, J.D. Clarifying the mechanism of superantigen toxicity. PLoS Biol. 2011, 9, e1001145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLean, R.; Rash, N.L.; Robinson, C.; Waller, A.S.; Paillot, R. Localised mitogenic activity in horses following infection with Streptococcus equi. Res. Vet. Sci. 2015, 100, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Commons, R.J.; Smeesters, P.R.; Proft, T.; Fraser, J.D.; Robins-Browne, R.; Curtis, N. Streptococcal superantigens: Categorization and clinical associations. Trends Mol. Med. 2014, 20, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Rash, N.L.; Robinson, C.; DeSouza, N.; Nair, S.; Hodgson, H.; Steward, K.; Waller, A.S.; Paillot, R. Prevalence and disease associations of superantigens szeF, szeN and szeP in the S. zooepidemicus population and possible functional redundancy of szeF. Res. Vet. Sci. 2014, 97, 481–487. [Google Scholar] [CrossRef]
- Paillot, R.; Robinson, C.; Steward, K.; Wright, N.; Jourdan, T.; Butcher, N.; Heather, Z.; Waller, A.S. Contribution of each of four Superantigens to Streptococcus equi-induced mitogenicity, gamma interferon synthesis, and immunity. Infect. Immun. 2010, 78, 1728–1739. [Google Scholar] [CrossRef] [Green Version]
- Paillot, R.; Darby, A.C.; Robinson, C.; Wright, N.L.; Steward, K.F.; Anderson, E.; Webb, K.; Holden, M.T.; Efstratiou, A.; Broughton, K.; et al. Identification of three novel superantigen-encoding genes in Streptococcus equi subsp. zooepidemicus, szeF, szeN, and szeP. Infect. Immun. 2010, 78, 4817–4827. [Google Scholar] [CrossRef] [Green Version]
- Alber, J.; El-Sayed, A.; Estoepangestie, S.; LammLer, C.; Zschock, M. Dissemination of the superantigen encoding genes seeL, seeM, szeL and szeM in Streptococcus equi subsp. equi and Streptococcus equi subsp. zooepidemicus. Vet. Microbiol. 2005, 109, 135–141. [Google Scholar] [CrossRef]
- Proft, T.; Webb, P.D.; Handley, V.; Fraser, J.D. Two novel superantigens found in both group A and group C Streptococcus. Infect. Immun. 2003, 71, 1361–1369. [Google Scholar] [CrossRef] [Green Version]
- Sundberg, E.J.; Li, H.; Llera, A.S.; McCormick, J.K.; Tormo, J.; Schlievert, P.M.; Karjalainen, K.; Mariuzza, R.A. Structures of two streptococcal superantigens bound to TCR beta chains reveal diversity in the architecture of T cell signaling complexes. Structure 2002, 10, 687–699. [Google Scholar] [CrossRef] [Green Version]
- Yamaoka, J.; Nakamura, E.; Takeda, Y.; Imamura, S.; Minato, N. Mutational analysis of superantigen activity responsible for the induction of skin erythema by streptococcal pyrogenic exotoxin C. Infect. Immun. 1998, 66, 5020–5026. [Google Scholar] [CrossRef] [Green Version]
- Petersen, T.N.; Brunak, S.; von Heijne, G.; Nielsen, H. SignalP 4.0: Discriminating signal peptides from transmembrane regions. Nat. Methods 2011, 8, 785–786. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Stecher, G.; Li, M.; Knyaz, C.; Tamura, K. MEGA X: Molecular Evolutionary Genetics Analysis across Computing Platforms. Mol. Biol. Evol. 2018, 35, 1547–1549. [Google Scholar] [CrossRef] [PubMed]
- Proft, T.; Fraser, J.D. Bacterial superantigens. Clin. Exp. Immunol. 2003, 133, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Norrby-Teglund, A.; Chatellier, S.; Low, D.E.; McGeer, A.; Green, K.; Kotb, M. Host variation in cytokine responses to superantigens determine the severity of invasive group A streptococcal infection. Eur. J. Immunol. 2000, 30, 3247–3255. [Google Scholar] [CrossRef]
- Norrby-Teglund, A.; Lustig, R.; Kotb, M. Differential induction of Th1 versus Th2 cytokines by group A streptococcal toxic shock syndrome isolates. Infect. Immun. 1997, 65, 5209–5215. [Google Scholar] [CrossRef] [Green Version]
- Norrby-Teglund, A.; Norgren, M.; Holm, S.E.; Andersson, U.; Andersson, J. Similar cytokine induction profiles of a novel streptococcal exotoxin, MF, and pyrogenic exotoxins A and B. Infect. Immun. 1994, 62, 3731–3738. [Google Scholar] [CrossRef] [Green Version]
- Miethke, T.; Wahl, C.; Regele, D.; Gaus, H.; Heeg, K.; Wagner, H. Superantigen mediated shock: A cytokine release syndrome. Immunobiology 1993, 189, 270–284. [Google Scholar] [CrossRef]
- Anzai, T.; Sheoran, A.S.; Kuwamoto, Y.; Kondo, T.; Wada, R.; Inoue, T.; Timoney, J.F. Streptococcus equi but not Streptococcus zooepidemicus produces potent mitogenic responses from equine peripheral blood mononuclear cells. Vet. Immunol. Immunopathol. 1999, 67, 235–246. [Google Scholar] [CrossRef]
- Zeppa, J.J.; Kasper, K.J.; Mohorovic, I.; Mazzuca, D.M.; Haeryfar, S.M.M.; McCormick, J.K. Nasopharyngeal infection by Streptococcus pyogenes requires superantigen-responsive Vbeta-specific T cells. Proc. Natl. Acad. Sci. USA. 2017, 114, 10226–10231. [Google Scholar] [CrossRef] [Green Version]
- Ulrich, R.G. Vaccine based on a ubiquitous cysteinyl protease and streptococcal pyrogenic exotoxin A protects against Streptococcus pyogenes sepsis and toxic shock. J. Immune Based Ther. Vaccines 2008, 6, 8. [Google Scholar] [CrossRef] [Green Version]
- Roggiani, M.; Stoehr, J.A.; Olmsted, S.B.; Matsuka, Y.V.; Pillai, S.; Ohlendorf, D.H.; Schlievert, P.M. Toxoids of streptococcal pyrogenic exotoxin A are protective in rabbit models of streptococcal toxic shock syndrome. Infect. Immun. 2000, 68, 5011–5017. [Google Scholar] [CrossRef] [Green Version]
- Radcliff, F.J.; Loh, J.M.; Ha, B.; Schuhbauer, D.; McCluskey, J.; Fraser, J.D. Antigen targeting to major histocompatibility complex class II with streptococcal mitogenic exotoxin Z-2 M1, a superantigen-based vaccine carrier. Clin. Vaccine Immunol. 2012, 19, 574–586. [Google Scholar] [CrossRef] [PubMed]
- Dickgreber, N.; Stoitzner, P.; Bai, Y.; Price, K.M.; Farrand, K.J.; Manning, K.; Angel, C.E.; Dunbar, P.R.; Ronchese, F.; Fraser, J.D.; et al. Targeting antigen to MHC class II molecules promotes efficient cross-presentation and enhances immunotherapy. J. Immunol. 2009, 182, 1260–1269. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, J.D.; Manning, K.; Chokshi, S.; Naoumov, N.V.; Fraser, J.D.; Dunbar, P.R.; Taylor, J.A. An engineered non-toxic superantigen increases cross presentation of hepatitis B virus nucleocapsids by human dendritic cells. PLoS ONE 2014, 9, e93598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, C.; Frykberg, L.; Flock, M.; Guss, B.; Waller, A.S.; Flock, J.I. Strangvac: A recombinant fusion protein vaccine that protects against strangles, caused by Streptococcus equi. Vaccine 2018, 36, 1484–1490. [Google Scholar] [CrossRef]
- Guss, B.; Flock, M.; Frykberg, L.; Waller, A.S.; Robinson, C.; Smith, K.C.; Flock, J.I. Getting to grips with strangles: An effective multi-component recombinant vaccine for the protection of horses from Streptococcus equi infection. PLoS Pathog. 2009, 5, e1000584. [Google Scholar] [CrossRef] [Green Version]
- Waller, A.; Flock, M.; Smith, K.; Robinson, C.; Mitchell, Z.; Karlstrom, A.; Lannergard, J.; Bergman, R.; Guss, B.; Flock, J.I. Vaccination of horses against strangles using recombinant antigens from Streptococcus equi. Vaccine 2007, 25, 3629–3635. [Google Scholar] [CrossRef]
- Li, Y.; Li, H.; Dimasi, N.; McCormick, J.K.; Martin, R.; Schuck, P.; Schlievert, P.M.; Mariuzza, R.A. Crystal structure of a superantigen bound to the high-affinity, zinc-dependent site on MHC class II. Immunity 2001, 14, 93–104. [Google Scholar] [CrossRef] [Green Version]
- Robinson, C.; Steward, K.F.; Potts, N.; Barker, C.; Hammond, T.A.; Pierce, K.; Gunnarsson, E.; Svansson, V.; Slater, J.; Newton, J.R.; et al. Combining two serological assays optimises sensitivity and specificity for the identification of Streptococcus equi subsp. equi exposure. Vet. J. 2013, 197, 188–191. [Google Scholar] [CrossRef] [Green Version]
- Argos, P. An investigation of oligopeptides linking domains in protein tertiary structures and possible candidates for general gene fusion. J. Mol. Biol. 1990, 211, 943–958. [Google Scholar] [CrossRef]
- Klein, J.S.; Jiang, S.; Galimidi, R.P.; Keeffe, J.R.; Bjorkman, P.J. Design and characterization of structured protein linkers with differing flexibilities. Protein Eng. Des. Sel. 2014, 27, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Cherni, I.; Yu, H.; Fromme, R.; Doran, J.D.; Grotjohann, I.; Mittman, M.; Basu, S.; Deb, A.; Dorner, K.; et al. Expression, purification and crystallization of CTB-MPR, a candidate mucosal vaccine component against HIV-1. IUCrJ 2014, 1, 305–317. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zaro, J.L.; Shen, W.C. Fusion protein linkers: Property, design and functionality. Adv. Drug Deliv. Rev. 2013, 65, 1357–1369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, J.; Nagy, S.; Bjork, L.; Abrams, J.; Holm, S.; Andersson, U. Bacterial toxin-induced cytokine production studied at the single-cell level. Immunol. Rev. 1992, 127, 69–96. [Google Scholar] [CrossRef]
- Faulkner, L.; Cooper, A.; Fantino, C.; Altmann, D.M.; Sriskandan, S. The mechanism of superantigen-mediated toxic shock= not a simple Th1 cytokine storm. J. Immunol. 2005, 175, 6870–6877. [Google Scholar] [CrossRef]
- Marmur, J. A procedure for the isolation of deoxyribonucleic acid from micro-organisms. J. Mol. Biol. 1961, 3, 208–218. [Google Scholar] [CrossRef]
- Hormanski, C.E.; Truax, R.; Pourciau, S.S.; Folsom, R.W.; Horohov, D.W. Induction of lymphokine-activated killer cells of equine origin: Specificity for equine target cells. Vet. Immunol. Immunopathol. 1992, 32, 25–36. [Google Scholar] [CrossRef]
- Castillo-Olivares, J.; Tearle, J.P.; Montesso, F.; Westcott, D.; Kydd, J.H.; Davis-Poynter, N.J.; Hannant, D. Detection of equine arteritis virus (EAV)-specific cytotoxic CD8+ T lymphocyte precursors from EAV-infected ponies. J. Gen Virol. 2003, 84, 2745–2753. [Google Scholar] [CrossRef]




© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dominguez-Medina, C.C.; Rash, N.L.; Robillard, S.; Robinson, C.; Efstratiou, A.; Broughton, K.; Parkhill, J.; Holden, M.T.G.; Lopez-Alvarez, M.R.; Paillot, R.; et al. SpeS: A Novel Superantigen and Its Potential as a Vaccine Adjuvant against Strangles. Int. J. Mol. Sci. 2020, 21, 4467. https://doi.org/10.3390/ijms21124467
Dominguez-Medina CC, Rash NL, Robillard S, Robinson C, Efstratiou A, Broughton K, Parkhill J, Holden MTG, Lopez-Alvarez MR, Paillot R, et al. SpeS: A Novel Superantigen and Its Potential as a Vaccine Adjuvant against Strangles. International Journal of Molecular Sciences. 2020; 21(12):4467. https://doi.org/10.3390/ijms21124467
Chicago/Turabian StyleDominguez-Medina, C. Coral, Nicola L. Rash, Sylvain Robillard, Carl Robinson, Androulla Efstratiou, Karen Broughton, Julian Parkhill, Matthew T.G. Holden, Maria R. Lopez-Alvarez, Romain Paillot, and et al. 2020. "SpeS: A Novel Superantigen and Its Potential as a Vaccine Adjuvant against Strangles" International Journal of Molecular Sciences 21, no. 12: 4467. https://doi.org/10.3390/ijms21124467




