Inhalations with Brine Solution from the ‘Wieliczka’ Salt Mine Diminish Airway Hyperreactivity and Inflammation in a Murine Model of Non-Atopic Asthma
Abstract
1. Introduction
2. Results
2.1. Basal Ventilatory Parameters
2.2. Airway Hyperreactivity (AHR) to Methacholine (MCh)
2.3. Cell Infiltration
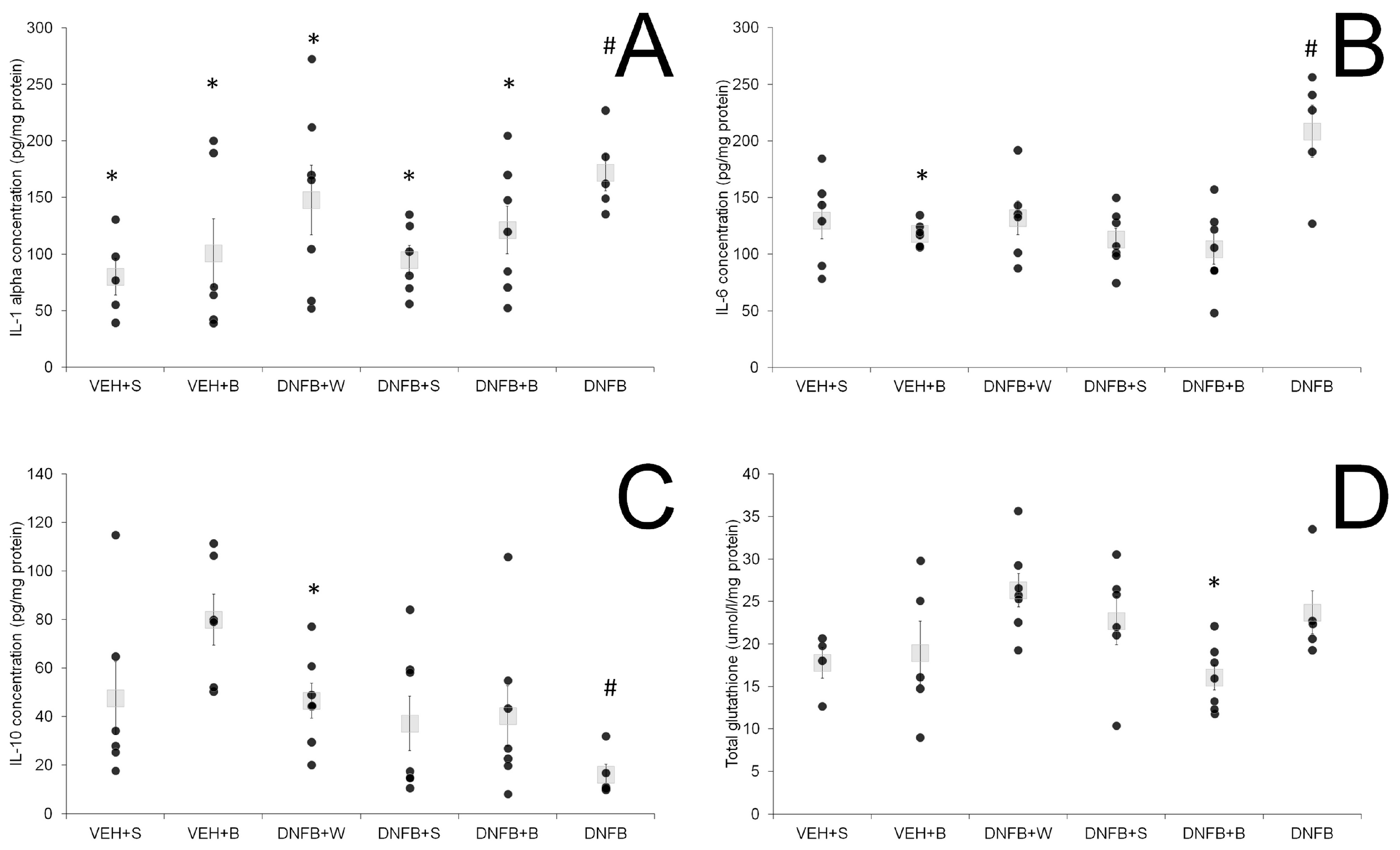
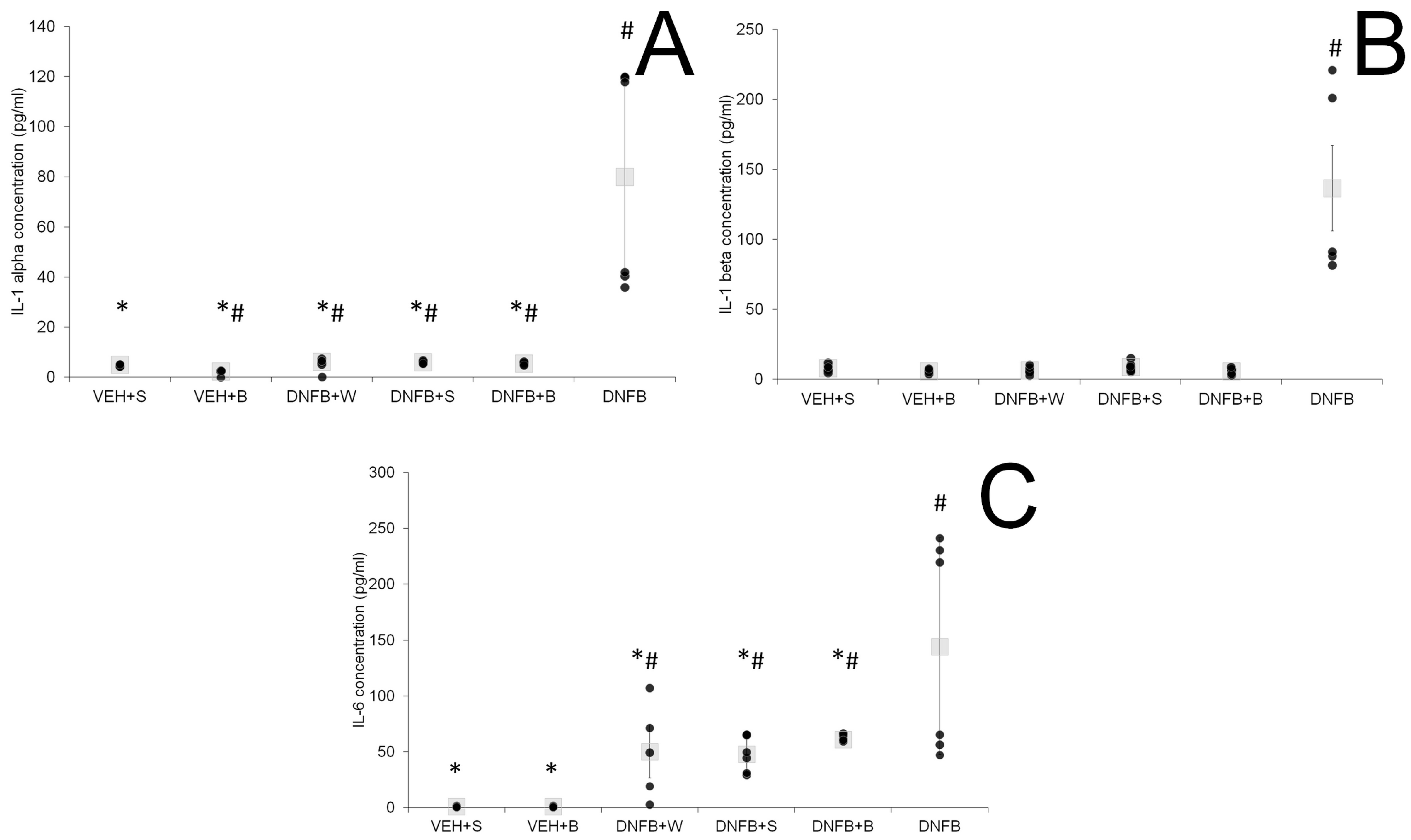
2.4. Airway Inflammation
2.5. Oxidative Stress Marker
3. Discussion
4. Materials and Methods
4.1. Drugs and Reagents Used in the Study
4.2. Experimental Procedures
4.2.1. Sensitization and Methacholine Challenge
4.2.2. Inhalations
4.2.3. BALF Collection and Cytological Analysis
4.2.4. Lung Collection and Homogenization
4.2.5. Biochemical Analyses
4.3. Statistical Analyses
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| DNFB | 1-fluoro-2, 4-dinitrobenzene (as substance) |
| DNS | dinitrobenzene sulfonic acid |
| MCh | methacholine |
| BALF | broncho-alveolar lavage fluid |
| DNFB+W | sensitized pure water inhaled animals |
| DNFB+S | sensitized saline inhaled animals |
| DNFB+B | sensitized brine inhaled animals |
| VEH+S | sham-sensitized saline-inhaled animals |
| VEH+B | sham-sensitized brine-inhaled animals |
| DNFB | sensitized non-inhaled animals (as experimental group) |
References
- Vizmanos-Lamotte, G.; Moreno-Galdo, A.; Munoz, X.; Gomez-Olles, S.; Gartner, S.; Cruz, M.J. Induced sputum cell count and cytokine profile in atopic and non-atopic children with asthma. Pediatr. Pulmonol. 2013, 48, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Berend, N.; Salome, C.M.; King, G.G. Mechanisms of airway hyperresponsiveness in asthma. Respirology 2008, 13, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Gorgojo, I.; Antolín-Amérigo, D.; Domínguez-Ortega, J.; Quirce, S. Non-eosinophilic asthma: Current perspectives. J. Asthma Allergy 2018, 11, 267–281. [Google Scholar] [CrossRef]
- Green, R.H.; Brightling, C.E.; Woltmann, G.; Parker, D.; Wardlaw, A.J.; Pavord, I.D. Analysis of induced sputum in adults with asthma: Identification of subgroup with isolated sputum neutrophilia and poor response to inhaled corticosteroids. Thorax 2002, 57, 875–879. [Google Scholar] [CrossRef]
- Turkeli, A.; Yilmaz, O.; Taneli, F.; Horasan, G.D.; Kanik, E.T.; Kizilkaya, M.; Gozukara, C.; Yuksel, H. IL-5, IL-8 and MMP -9 levels in exhaled breath condensate of atopic and nonatopic asthmatic children. Respir. Med. 2015, 109, 680–688. [Google Scholar] [CrossRef]
- GINA Global Initiative for Asthma; Global Strategy for Asthma Management and Prevention. Available online: www.ginasthma.org (accessed on 20 March 2020).
- Eberlein, B.; Huss-Marp, J.; Pfab, F.; Fischer, R.; Franz, R.; Schlich, M.; Leibl, M.; Allertseder, V.; Liptak, J.; Kriegisch, M.; et al. Influence of alpine mountain climate of Bavaria on patients with atopic diseases: Studies at the Environmental Research Station Schneefernerhaus (UFS—Zugspitze)—A pilot study. Clin. Transl. Allergy 2014, 4, 17. [Google Scholar] [CrossRef] [PubMed]
- Gaisberger, M.; Šanović, R.; Dobias, H.; Kolarž, P.; Moder, A.; Thalhamer, J.; Selimović, A.; Huttegger, I.; Ritter, M.; Hartl, A. Effects of ionized waterfall aerosol on pediatric allergic asthma. J. Asthma 2012, 498, 830–838. [Google Scholar] [CrossRef] [PubMed]
- Menger, W.; Schellhaas, J. A telemetric study of the secretolytic effect of sea-air on children with bronchial asthma (author’s transl). Prax Klin Pneumol. 1980, 34, 746–749. (In German) [Google Scholar] [PubMed]
- Gutenbrunner, C.; Bender, T.; Cantista, P.; Karagülle, Z. A proposal for a worldwide definition of health resort medicine, balneology, medical hydrology and climatology. Int. J. Biometeorol. 2010, 54, 495–507. [Google Scholar] [CrossRef]
- Tomooka, L.T.; Murphy, C.; Davidson, T.M. Clinical study and literature review of nasal irrigation. Laryngoscope 2000, 110, 1189–1193. [Google Scholar] [CrossRef]
- Wei, C.C.; Adappa, N.D.; Cohen, N.A. Use of topical nasal therapies in the management of chronic rhinosinusitis. Laryngoscope 2013, 123, 2347–2359. [Google Scholar] [CrossRef]
- Donaldson, S.H.; Bennett, W.D.; Zeman, K.L.; Knowles, M.R.; Tarran, R.; Boucher, R.C. Mucus clearance and lung function in cystic fibrosis with hypertonic saline. N. Engl. J. Med. 2006, 354, 241–250. [Google Scholar] [CrossRef]
- Elkins, M.R.; Robinson, M.; Rose, B.R.; Harbour, C.; Moriarty, C.P.; Marks, G.B.; Belousova, E.G.; Xuan, W.; Bye, P.T.P. A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis. N. Engl. J. Med. 2006, 354, 229–240. [Google Scholar] [CrossRef]
- Rassulova, M.A.; Razumov, A.N.; Aĭrapetova, N.S. Use of natural physical factors in the rehabilitative treatment of patients with chronic obstructive pulmonary diseases. Probl Tuberk Bolezn Legk 2007, 12, 10–14. (In Russian) [Google Scholar]
- Michel, O. Nasal irrigation in case of rhinosinusitis. Laryngo Rhino Otol. 2006, 85, 448–458. (In German) [Google Scholar] [CrossRef]
- Olina, M.; Aluffi Valletti, P.; Pia, F.; Toso, A.; Borello, G.; Policarpo, M.; Garavelli, P.L. Hydrological indications in the therapy of pharyngitis. Recenti Prog. Med. 2008, 99, 314–321. (In Italian) [Google Scholar]
- Passariello, A.; Di Costanzo, M.; Terrin, G.; Iannotti, A.; Buono, P.; Balestrieri, U.; Balestrieri, G.; Ascione, E.; Pedata, M.; Canani, F.B.; et al. Crenotherapy modulates the expression of pro-inflammatory cytokines and immunoregulatory peptides in nasal secretions of children with chronic rhinosinusitis. Am. J. Rhinol. Allergy 2012, 26, e15–e19. [Google Scholar] [CrossRef]
- Prandelli, C.; Parola, C.; Buizza, L.; Delbarba, A.; Marziano, M.; Salvi, V.; Zacchi, V.; Memo, M.; Sozzani, S.; Calza, S.; et al. Sulphurous thermal water increases the release of the anti-inflammatory cytokine IL-10 and modulates antioxidant enzyme activity. Int. J. Immunopathol. Pharmacol. 2013, 26, 633–646. [Google Scholar] [CrossRef]
- Kostrzon, M.; Czarnobilski, K.; Czarnobilska, E. The influence of pulmonary rehabilitation in the Wieliczka Salt Mine on asthma control-preliminary results. Przegl Lek 2015, 72, 716–720. [Google Scholar]
- Petraccia, L.; Masciullo, S.G.; Grassi, M.; Pace, A.; Lucchetta, M.C.; Valenzi, V.I.; Avino, P.; Fraioli, A. Spa and climate therapy in chronic obstructive pulmonary diseases. Clin. Ter. 2005, 156, 23–31. (In Italian) [Google Scholar]
- Chernenkov, R.A.; Chernenkova, E.A.; Zhukov, G.V. The use of an artificial microclimate chamber in the treatment of patients with chronic obstructive lung diseases. Vopr Kurortol Fizioter Lech Fiz Kult 1997, 4, 19–21. (In Russian) [Google Scholar]
- Cantone, E.; Maione, N.; Di Rubbo, V.; Esposito, F.; Iengo, M. Olfactory performance after crenotherapy in chronic rhinosinusitis in the elderly. Laryngoscope 2015, 125, 1529–1534. [Google Scholar] [CrossRef]
- Ciprandi, G.; Cristofolini, M.; Mira, E. Comano thermal water inhalations in the treatment of allergic rhinitis: Preliminary results. Eur. Ann. Allergy Clin. Immunol. 2016, 48, 220–223. [Google Scholar]
- Costantino, M.; Giuberti, G.; Caraglia, M.; Lombardi, A.; Misso, G.; Abbruzzese, A.; Ciani, F.; Lampa, E. Possible antioxidant role of SPA therapy with chlorine–sulphur– bicarbonate mineral water. Amino Acids 2009, 36, 161–165. [Google Scholar] [CrossRef]
- Passali, D.; Gabelli, G.; Passali, G.C.; Magnato, R.; Platzgummer, S.; Salerni, L.; Cunsolo, S.L.; Joos, A.; Bellussi, L.M. Radioactive Merano SPA treatment for allergic rhinitis therapy. Int. J. Otolaryngol. 2016, 2016, 2801913. [Google Scholar] [CrossRef]
- Varricchio, A.; Giuliano, M.; Capasso, M.; Del Gaizo, D.; Ascione, E.; De Lucia, A.; Avvisati, F.; Capuano, F.; De Rosa, G.; Di Mauro, F.; et al. Salso-sulphide thermal water in the prevention of recurrent respiratory infections in children. Int. J. Immunopathol. Pharmacol. 2013, 26, 941–952. [Google Scholar] [CrossRef]
- Kostrzon, M.; Sliwka, A.; Wloch, T.; Szpunar, M.; Ankowska, D.; Nowobilski, R. Subterranean pulmonary rehabilitation in chronic obstructive pulmonary disease. Adv. Exp. Med. Biol. 2019, 1176, 35–46. [Google Scholar]
- d’Obyrn, K.; Rajchel, L. Balneoterapeutyczne wykorzystanie solanek w uzdrowisku Kopalnia Soli Wieliczka. Przegl Geol. 2015, 63, 981–984. (In Polish) [Google Scholar]
- Zajac, D.; Russjan, E.; Kostrzon, M.; Kmiecki, M.; Kaczynska, K. The influence of inhalation of brine from the Wieliczka Salt Mine on inflammation and airway hyperreactivity in a murine model of non-atopic asthma. Eur. Respir. J. 2019, 54 (Suppl. 63). Available online: https://erj.ersjournals.com/content/54/suppl_63/PA4211 (accessed on 15 March 2020).
- Rubin, B.K. Aerosol medications for treatment of mucus clearance disorders. Respir. Care 2015, 60, 825–829. [Google Scholar] [CrossRef]
- Tanizaki, Y.; Kitani, H.; Okazaki, M.; Mifune, T.; Mitsunobu, F.; Honke, N. Clinical effects of complex spa therapy on patients with steroid-dependent intractable asthma (SDIA). Arerugi 1993, 42, 219–227. [Google Scholar]
- Bar-Yoseph, R.; Kugelman, N.; Livnat, G.; Gur, M.; Hakim, F.; Nir, V.; Bentur, L. Halotherapy as asthma treatment in children: A randomized, controlled, prospective pilot study. Pediatr. Pulmonol. 2017, 52, 580–587. [Google Scholar] [CrossRef]
- Maguire, C.; Cantrill, H.; Hind, D.; Bradburn, M.; Everard, M.L. Hypertonic saline (HS) for acute bronchiolitis: Systematic review and meta-analysis. BMC Pulm. Med. 2015, 15, 148. [Google Scholar] [CrossRef]
- Daviskas, E.; Anderson, S.D.; Gonda, I.; Eberl, S.; Meikle, S.; Seale, J.P.; Bautovich, G. Inhalation of hypertonic saline aerosol enhances mucociliary clearance in asthmatic and healthy subjects. Eur. Respir. J. 1996, 9, 725–732. [Google Scholar] [CrossRef]
- Fujimura, M.; Amemiya, M.; Myou, S.; Mizuguchi, M.; Matsuda, T. A guinea-pig model of ultrasonically nebulized distilled water-induced bronchoconstriction. Eur. Respir. J. 1997, 10, 2237–2242. [Google Scholar] [CrossRef]
- Kivity, S.; Poterman, R.; Schwarz, Y.; Soferman, R.; Topilsky, M. Changes in sensitivity to methacholine after inhalation with distilled water: The role of the bronchoconstrictive response. Eur. Respir. J. 1995, 8, 253–256. [Google Scholar] [CrossRef]
- Schoeffel, R.E.; Anderson, S.D.; Altounyan, R.E.C. Bronchial hyperreactivity in response to inhalation of ultrasonically nebulized solutions of distilled water and saline. Br. Med. J. 1981, 283, 1285–1287. [Google Scholar] [CrossRef]
- Kashiwabara, K.; Itonaga, K.; Moroi, T. Airborne water droplets in mist or fog affect nocturnal attacks in asthmatic children. J. Asthma 2003, 40, 405–411. [Google Scholar] [CrossRef]
- Tränkner, D.; Hahne, N.; Suginoa, K.; Hoonb, M.A.; Zukera, C. Population of sensory neurons essential for asthmatic hyperreactivity of inflamed airways. Proc. Natl. Acad. Sci. USA 2014, 111, 11515–11520. [Google Scholar] [CrossRef]
- Vanoirbeek, J.A.; Rinaldi, M.; De Vooght, V.; Haenen, S.; Bobic, S.; Gayan-Ramirez, G.; Hoet, P.H.M.; Verbeken, E.; Decramer, M.; Nemery, B.; et al. Noninvasive and invasive pulmonary function in mouse models of obstructive and restrictive respiratory diseases. Am. J. Respir. Cell Mol. Biol. 2010, 42, 96–104. [Google Scholar] [CrossRef]
- Kraneveld, A.D.; van der Kleij, H.P.M.; Kool, M.; van Houwelingen, A.H.; Weitenberg, A.C.D.; Redegeld, F.A.M.; Nijkamp, F.P. Key role for mast cells in nonatopic asthma. J. Immunol. 2002, 169, 2044–2053. [Google Scholar] [CrossRef]
- Russjan, E.; Andrzejewski, K.; Sulejczak, D.; Kleczkowska, P.; Kaczyńska, K. Endomorphin-2- and neurotensin- based chimeric peptide attenuates airway inflammation in mouse model of nonallergic asthma. Int. J. Mol. Sci. 2019, 20, 5935. [Google Scholar] [CrossRef]
- Kim, H.Y.; De Kruyff, R.H.; Umetsu, D.T. The many paths to asthma: Phenotype shaped by innate and adaptive immunity. Nat. Immunol. 2010, 11, 577–584. [Google Scholar] [CrossRef]
- Maltby, S.; Tay, H.L.; Yang, M.; Foster, P.S. Mouse models of severe asthma: Understanding the mechanisms of steroid resistance, tissue remodeling and disease exacerbation. Respirology 2017, 22, 874–885. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.-Q.; Xiang, Y.; Liu, C.; Tan, Y.-R.; Qu, F.; Peng, L.-H.; Zhu, X.-L.; Qin, L. The role of bronchial epithelial cells in airway hyperresponsiveness. Acta Physiol. Sin. 2007, 59, 454–464. [Google Scholar]
- Boshtam, M.; Asgary, S.; Kouhpayeh, S.; Shariati, L.; Khanahmad, H. Aptamers against pro- and anti-inflammatory cytokines: A review. Inflammation 2017, 40, 340–349. [Google Scholar] [CrossRef]
- Zaripova, T.N.; Antipova, I.I.; Siniagina, M.A. A new approach to the treatment of patients presenting with bronchial asthma and concomitant allergic rhinitis. Vopr Kurortol Fizioter Lech Fiz Kult 2013, 5, 23–28. (In Russian) [Google Scholar]
- Yokoyama, A.; Kohno, N.; Fujino, S.; Hamada, H.; Inoue, Y.; Fujioka, S.; Ishida, S.; Hiwada, K. Circulating interleukin-6 levels in patients with bronchial asthma. Am. J. Respir. Crit. Care Med. 1995, 151, 1354–1358. [Google Scholar] [CrossRef] [PubMed]
- Liao, Z.; Xiao, H.; Zhang, Y.; Tong, R.-S.; Zhang, L.-J.; Bian, Y.; He, X. IL-1beta: A key modulator in asthmatic airway smooth muscle hyper-reactivity. Expert Rev. Respir. Med. 2005, 9, 429–436. [Google Scholar] [CrossRef]
- Tsukagoshi, H.; Sakamoto, T.; Xu, W.; Barnes, P.; Chung, F. Effect of interleukin-1β on airway hyperresponsiveness and inflammation in sensitized and nonsensitized Brown-Norway rats. J. Allergy Clin. Immunol. 1994, 93, 464–469. [Google Scholar] [CrossRef]
- Barnes, T.C.; Anderson, M.E.; Moots, R.J. The Many Faces of Interleukin-6: The Role of IL-6 in Inflammation, Vasculopathy, and Fibrosis in Systemic Sclerosis. Int. J. Rheumat. 2011, 721608. [Google Scholar] [CrossRef] [PubMed]
- Johnson, V.J.; Yucesoy, B.; Luster, M.I. Prevention of IL-1 signaling attenuates airway hyperresponsiveness and inflammation in a murine model of toluene diisocyanate–induced asthma. J. Allergy Clin. Immunol. 2005, 116, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Ray, A.; Kolls, J.K. Neutrophilic inflammation in asthma and association with disease severity. Trends Immunol. 2017, 38, 942–954. [Google Scholar] [CrossRef]
- Krane, C.M.; Fortner, C.N.; Hand, A.R.; McGraw, D.W.; Lorenz, J.N.; Wert, S.E.; Towne, J.E.; Paul, R.J.; Whitsett, J.A.; Menon, A.G. Aquaporin 5-deficient mouse lungs are hyperresponsive to cholinergic stimulation. Proc. Natl. Acad. Sci. USA 2001, 98, 14114–14119. [Google Scholar] [CrossRef]
- Hoffert, J.D.; Leitch, V.; Agre, P.; King, L.S. Hypertonic Induction of Aquaporin-5 Expression through an ERK-dependent Pathway. J. Biol. Chem. 2000, 275, 9070–9077. [Google Scholar] [CrossRef]
- Nilsson, H.; Dragomir, A.; Ahlander, A.; Johannesson, M.; Roomans, G.M. Effects of hyperosmotic stress on cultured airway epithelial cells. Cell Tissue Res. 2007, 330, 257–269. [Google Scholar] [CrossRef] [PubMed]
- Wark, P.A.; Donald, V.M.; Jones, A.P. Nebulized hypertonic saline for cystic fibrosis. Cochrane Database Syst. Rev. 2005, CD001506. [Google Scholar] [CrossRef]
- Comhair, A.; Erzurum, S.C. Redox control of asthma: Molecular mechanisms and therapeutic opportunities. Antioxid Redox Signal 2010, 121, 93–124. [Google Scholar] [CrossRef]
- Fitzpatrick, A.M.; Teague, W.G.; Holguin, F.; Yeh, M.; Brown, L.A.S. for the Severe Asthma Research Program. Airway glutathione homeostasis is altered in children with severe asthma: Evidence for oxidant stress. J. Allergy Clin. Immunol. 2009, 123, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.J.; Houston, M.; Anderson, J. Increased levels of glutathione in bronchoalveolar lavage fluid from patients with asthma. Am. Rev. Respir. Dis. 1993, 147, 1461–1464. [Google Scholar] [CrossRef]
- Kleniewska, P.; Pawliczak, R. The participation of oxidative stress in the pathogenesis of bronchial asthma. Biomed Pharm. 2017, 94, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Wohlauer, M.; Moore, E.E.; Silliman, C.C.; Fragoso, M.; Gamboni, F.; Harr, J.; Accurso, F.; Wright, F.; Haenel, J.; Fullerton, D.; et al. Nebulized hypertonic saline attenuates acute lung injury following trauma and hemorrhagic shock. Crit. Care Med. 2012, 40, 2647–2653. [Google Scholar] [CrossRef] [PubMed]
- Wright, F.L.; Gamboni, F.; Moore, E.E.; Nydam, T.L.; Mitra, S.; Silliman, C.C.; Banerjee, A. Hyperosmolarity invokes distinct anti-inflammatory mechanisms in pulmonary epithelial cells: Evidence from signaling and transcription layers. PLoS ONE 2014, 9, e114129. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, M.; Salami, A.; Mora, F.; Casazza, A.; Sovatzis, A.; Teglia, R.; Cordone, M.P.; Mora, R. Behavior of serum IgE and IgA in patients with allergic rhinitis treated with iodine bromide thermal water. Acta Otorhinolaryngol. Ital. 2002, 22, 215–219. (In Italian) [Google Scholar] [PubMed]
- Bellometti, S.; Bertocco, E.; Galzigna, L. Changes in the intrabronchial microflora of patients with chronic bronchitis after inhaling mineral water. Vopr Kurortol Fizioter Lech Fiz Kult 1998, 5, 17–19. (In Russian) [Google Scholar]
- Matveeva, L.A.; Kuzmenko, O.V.; Kurts, I.A.; Golosova, L.O. The use of an aerosol of natural brine and of sinusoidal modulated currents in chronic pneumonias in children. Vopr Kurortol Fizioter Lech Fiz Kult 1998, 2, 12–15. (In Russian) [Google Scholar]
- Keller, S.; König, V.; Mösges, R. Thermal water applications in the treatment of upper respiratory tract diseases: A systematic review and meta-analysis. J. Allergy 2014, 943824. [Google Scholar] [CrossRef]
- Viegas, J.; Esteves, A.F.; Cardoso, E.M.; Arosa, F.A.; Vitale, M.; Taborda-Barata, L. Biological effects of thermal water-associated hydrogen sulfide on human airways and associated immune cells: Implications for respiratory diseases. Front. Public Health 2019, 7, 128. [Google Scholar] [CrossRef]
- de Baaij, J.H.F.; Hoenderop, J.G.J.; Bindels, R.J.M. Magnesium in man: Implications for health and disease. Physiol. Rev. 2015, 95, 1–46. [Google Scholar] [CrossRef]
- Emelyanov, A.; Fedoseev, G.; Barnes, P.J. Reduced intracellular magnesium concentrations in asthmatic patients. Eur. Respir. J. 1999, 13, 38–40. [Google Scholar] [CrossRef]
- Hashimoto, Y.; Nishimura, Y.; Maeda, H.; Yokoyama, M. Assessment of magnesium status in patients with bronchial asthma. J. Asthma 2000, 37, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Gilliland, F.D.; Berhane, K.T.; Li, Y.F.; Kim, D.H.; Margolis, H.G. Dietary magnesium, potassium, sodium, and children’s lung function. Am. J. Epidemiol. 2002, 155, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Hirota, N.; Martin, J.G. Mechanisms of airway remodeling. Chest 2013, 144, 1026–1032. [Google Scholar] [CrossRef]
- Okayama, H.; Aikawa, T.; Okayama, M.; Sasaki, H.; Mue, S.; Takishima, T. Bronchodilating Effect of intravenous magnesium sulfate in bronchial asthma. JAMA 1987, 257, 1076–1078. [Google Scholar] [CrossRef]
- Powell, C.V.E.; Kolamunnage-Dona, R.; Lowe, J.; Boland, A.; Petrou, S.; Doull, I.; Hood, K.; Williamson, P.R. MAGNETIC study group. MAGNEsium Trial in Children (MAGNETIC): A randomised, placebo-controlled trial and economic evaluation of nebulised magnesium sulphate in acute severe asthma in children. Health Technol. Assess. 2013, 17, 1–216. [Google Scholar] [CrossRef]
- Nakaya, M.; Dohi, M.; Okunishi, K.; Nakagome, K.; Tanaka, R.; Imamura, M.; Baba, S.; Takeuchi, N.; Yamamoto, K.; Kaga, K. Noninvasive system for evaluating allergen-induced nasal hypersensitivity in murine allergic rhinitis. Lab. Investig. 2006, 86, 917–926. [Google Scholar] [CrossRef] [PubMed]
- Niu, C.; Wang, T.; Zou, W.; Hu, J.; Ying, L.; Zhang, M.; Liu, J.; Tian, D.; Dai, J.; Luo, Z.; et al. Enhanced pause correlates with airway neutrophils and airway-epithelial injury in asthmatic mice treated with dexamethasone. J. Asthma 2019, 56, 11–20. [Google Scholar] [CrossRef]
- Vanoirbeek, J.A.; Tarkowski, M.; De Vooght, V.; Nemery, B.; Hoet, P.H. Immunological determinants in a mouse model of chemical-induced asthma after multiple exposures. Scand. J. Immunol. 2009, 70, 25–33. [Google Scholar] [CrossRef]
- Lundblad, L.K.A.; Irvin, C.G.; Hantos, Z.; Sly, P.; Mitzner, W.; Bates, J.H.T. Penh is not a measure of airway resistance! Eur. Respir. J. 2007, 30, 805–816. [Google Scholar] [CrossRef]
- Lundblad, L.K.A.; Irvin, C.G.; Adler, A.; Bates, J.H.T. A reevaluation of the validity of unrestrained plethysmography in mice. J. Appl. Physiol. 2002, 93, 1198–1207. [Google Scholar] [CrossRef]
- Zhang, Q.; Lai, K.; Xie, J.; Chen, G.; Zhong, N. Does unrestrained single-chamber plethysmography provide a valid assessment of airway responsiveness in allergic BALB/c mice? Respir. Res. 2009, 10, 61. [Google Scholar] [CrossRef]
- Hamelmann, E.; Schwarze, J.; Takeda, K.; Oshiba, A.; Larsen, G.L.; Irvin, C.G.; Gelfand, E.W. Noninvasive measurement of airway responsiveness in allergic mice using barometric plethysmography. Am. J. Respir. Crit. Care Med. 1997, 156, 766–775. [Google Scholar] [CrossRef]
- Adler, A.; Cieslewicz, G.; Irvin, C.G. Unrestrained plethysmography is an unreliable measure of airway responsiveness in BALB/c and C57BL/6 mice. J. Appl. Physiol. 2004, 97, 286–292. [Google Scholar] [CrossRef]
- Duguet, A.; Biyah, K.; Minshall, E.; Gomes, R.; Wang, C.-G.; Taoudi-Benchekroun, M.; Bates, J.H.T.; Eidelman, D.H. Bronchial responsiveness among inbred mouse strains. Role of airway smooth-muscle shortening velocity. Am. J. Respir. Crit. Care Med. 2000, 161, 839–848. [Google Scholar] [CrossRef]
- van der Kleij, H.P.M.; Kraneveld, A.D.; van Houwelingen, A.H.; Kool, M.; Weitenberg, A.C.D.; Redegeld, F.A.M.; Nijkamp, F.P. Murine model for non-IgE-mediated asthma. Inflammation 2004, 28, 115–125. [Google Scholar] [CrossRef]
- Russjan, E.; Kaczyńska, K. Beneficial effects of neurotensin in murine model of hapten-induced asthma. Int. J. Mol. Sci. 2019, 20, 5025. [Google Scholar] [CrossRef]
- Russjan, E.; Kaczyńska, K. Murine models of hapten-induced asthma. Toxicology 2018, 410, 41–48. [Google Scholar] [CrossRef]




| f (1/min) | TV (mL) | MV (mL/min) | Ti (s) | Te (s) | Penh | ||
|---|---|---|---|---|---|---|---|
| VEH+S | Before (day 7) | 457.09 ± 30.07 | 0.317 ± 0.018 | 142.06 ± 12.91 | 0.0491 ± 0.0016 | 0.1386 ± 0.0294 | 1.258 ± 0.176 |
| After (day 21) | 468.92 ± 15.76 | 0.367 ± 0.010 # | 167.34 ± 7.66 # | 0.0511 ± 0.0010 | 0.1194 ± 0.0090 | 0.898 ± 0.099 | |
| VEH+B | Before (day 7) | 484.54 ± 16.86 | 0.375 ± 0.030 | 175.20 ± 15.47 | 0.0513 ± 0.0018 | 0.0998 ± 0.0118 | 0.997 ± 0.124 |
| After (day 21) | 481.53 ± 8.11 | 0.348 ± 0.020 | 164.13 ± 10.79 | 0.0489 ± 0.0007 | 0.1239 ± 0.0121 | 1.098 ± 0.112 | |
| DNFB+W | Before (day 7) | 407.09 ± 41.93 | 0.359 ± 0.040 | 202.14 ± 20.32 | 0.0608 ± 0.0067 | 0.1219 ± 0.0200 | 1.537 ± 0.334 |
| After (day 21) | 448.06 ± 12.45 | 0.429 ± 0.037 | 187.59 ± 15.81 | 0.0561 ± 0.0029 | 0.1116 ± 0.0115 | 1.327 ± 0.256 | |
| DNFB+S | Before (day 7) | 478.83 ± 13.48 | 0.354 ± 0.035 | 165.22 ± 14.26 | 0.0505 ± 0.0023 | 0.1081 ± 0.0075 | 1.242 ± 0.171 |
| After (day 21) | 467.04 ± 9.77 | 0.421 ± 0.028 * | 191.19 ± 11.65 * | 0.0530 ± 0.0016 | 0.1082 ± 0.0104 * | 1.111 ± 0.149 | |
| DNFB+B | Before (day 7) | 428.31 ± 29.07 | 0.307 ± 0.018 | 121.03 ± 10.13 | 0.0516 ± 0.0031 | 0.1694 ± 0.0305 | 1.479 ± 0.167 |
| After (day 21) | 468.37 ± 11.76 | 0.364 ± 0.021 | 165.85 ± 9.41 # | 0.0504 ± 0.0012 | 0.1310 ± 0.0246 | 1.322 ± 0.240 | |
| DNFB | Before (day 7) | 459.94 ± 16.20 | 0.342 ± 0.013 | 149.50 ± 8.08 | 0.0509 ± 0.0016 | 0.1273 ± 0.0196 | 1.181 ± 0.118 |
| After (day 21) | 472.73 ± 9.80 | 0.344 ± 0.017 | 154.35 ± 8.18 | 0.0506 ± 0.0012 | 0.1388 ± 0.0134 | 1.702 ± 0.212 # |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zając, D.; Russjan, E.; Kostrzon, M.; Kaczyńska, K. Inhalations with Brine Solution from the ‘Wieliczka’ Salt Mine Diminish Airway Hyperreactivity and Inflammation in a Murine Model of Non-Atopic Asthma. Int. J. Mol. Sci. 2020, 21, 4798. https://doi.org/10.3390/ijms21134798
Zając D, Russjan E, Kostrzon M, Kaczyńska K. Inhalations with Brine Solution from the ‘Wieliczka’ Salt Mine Diminish Airway Hyperreactivity and Inflammation in a Murine Model of Non-Atopic Asthma. International Journal of Molecular Sciences. 2020; 21(13):4798. https://doi.org/10.3390/ijms21134798
Chicago/Turabian StyleZając, Dominika, Ewelina Russjan, Magdalena Kostrzon, and Katarzyna Kaczyńska. 2020. "Inhalations with Brine Solution from the ‘Wieliczka’ Salt Mine Diminish Airway Hyperreactivity and Inflammation in a Murine Model of Non-Atopic Asthma" International Journal of Molecular Sciences 21, no. 13: 4798. https://doi.org/10.3390/ijms21134798
APA StyleZając, D., Russjan, E., Kostrzon, M., & Kaczyńska, K. (2020). Inhalations with Brine Solution from the ‘Wieliczka’ Salt Mine Diminish Airway Hyperreactivity and Inflammation in a Murine Model of Non-Atopic Asthma. International Journal of Molecular Sciences, 21(13), 4798. https://doi.org/10.3390/ijms21134798





