1. Introduction
Chronic kidney disease (CKD) is highly prevalent for both adults and children [
1,
2]. Cardiovascular disease (CVD) is the leading cause of morbidity and mortality among patients with CKD [
3,
4]. Unlike adults, overt features of CVD are rarely present in children. Hypertension is the most important risk factor for premature CVD [
5]. More than 50% of children with early stages of CKD exhibited blood pressure (BP) abnormalities on 24 h ambulatory BP monitoring (ABPM) [
6,
7]. Additionally, several surrogate markers have been applied to stratify the cardiovascular risk in CKD children, including left ventricular (LV) mass, LV mass index (LVMI), and ambulatory arterial stiffness index (AASI) [
8].
Acrylamide, an industrially produced α, β-unsaturated carbonyl-containing volatile organic compound, is one of the most common toxins in food [
9,
10]. It occurs in food containing high concentrations of hydrocarbons subjected to high temperature, like breads, potato chips, and coffee [
10]. Once absorbed, acrylamide can be converted to glycidamide or conjugated with glutathione (GSH). Acrylamide and glycidamide have a short half-life. The majority of absorbed acrylamide is eliminated via the urine after conversion to mercapturic acid derivatives. GSH conjugates of acrylamide and glycidamide are further converted to mercapturic acid derivatives, N-acetyl-S-(2-carbamoylethyl)-cysteine (AAMA), and N-acetyl-S-(2-carbamoyl-2-hydroxyethyl)-cysteine (GAMA), respectively [
11]. Accordingly, urinary AAMA and GAMA levels have become widely accepted internal biomarkers of acrylamide exposure [
11]. Acrylamide has raised much concern for its negative health effects, such as carcinogenicity, neurotoxicity, reproductive toxicity, and induction of oxidative stress [
10]. However, study of the effect of acrylamide exposure on hypertension and CVD is limited, especially in pediatric population. Our previous report demonstrated that in CKD children, abnormal BP was associated with an impaired nitric oxide (NO) pathway [
6]. The interplay between NO and oxidative stress has been linked to hypertension and CKD [
12,
13], whereas whether acrylamide exposure affects the NO pathway and relates to the CV risk in CKD children is largely unknown. We, therefore, aimed to estimate the associations of urinary acrylamide metabolites with BP and CV risk markers in children with CKD. We also investigated the mediating roles of the NO pathway in the relationships between urinary acrylamide metabolites and CV outcomes to identify the potential mechanistic link.
3. Discussion
To our knowledge, this is the first study describing the association of urinary acrylamide metabolites with cardiovascular risk markers in a pediatric CKD population. Our study shows (1) children with CKD stage G2–G4 had a lower urinary acrylamide level, but a higher AAMA-to-GAMA ratio than those with CKD stage G1; (2) urinary acrylamide level was negatively associated with high SBP and DBP load on ABPM and plasma Cr level; (3) LV mass had a negative correlation with urinary acrylamide, AAMA, and GAMA levels, but a positive correlation with the AAMA-to-GAMA ratio; and (4) GAMA is superior to AAMA related to NO-related parameters, mainly citrulline and SDMA, in CKD children.
In keeping with previous studies, certain markers of CV risk tend to present in children with CKD, even in an early stage, such as ABPM abnormalities [
4,
6,
7,
16], uric acid [
17], and AASI [
18]. In the current study, up to 47.9% of children with CKD stage G1 displayed abnormal ABPM profiles. Our data support the notion that children in early stages of CKD are frequently masked by office BP measurements, and ABPM is recommended for the diagnosis of hypertension, especially in children at high cardiovascular risk [
7,
8,
19].
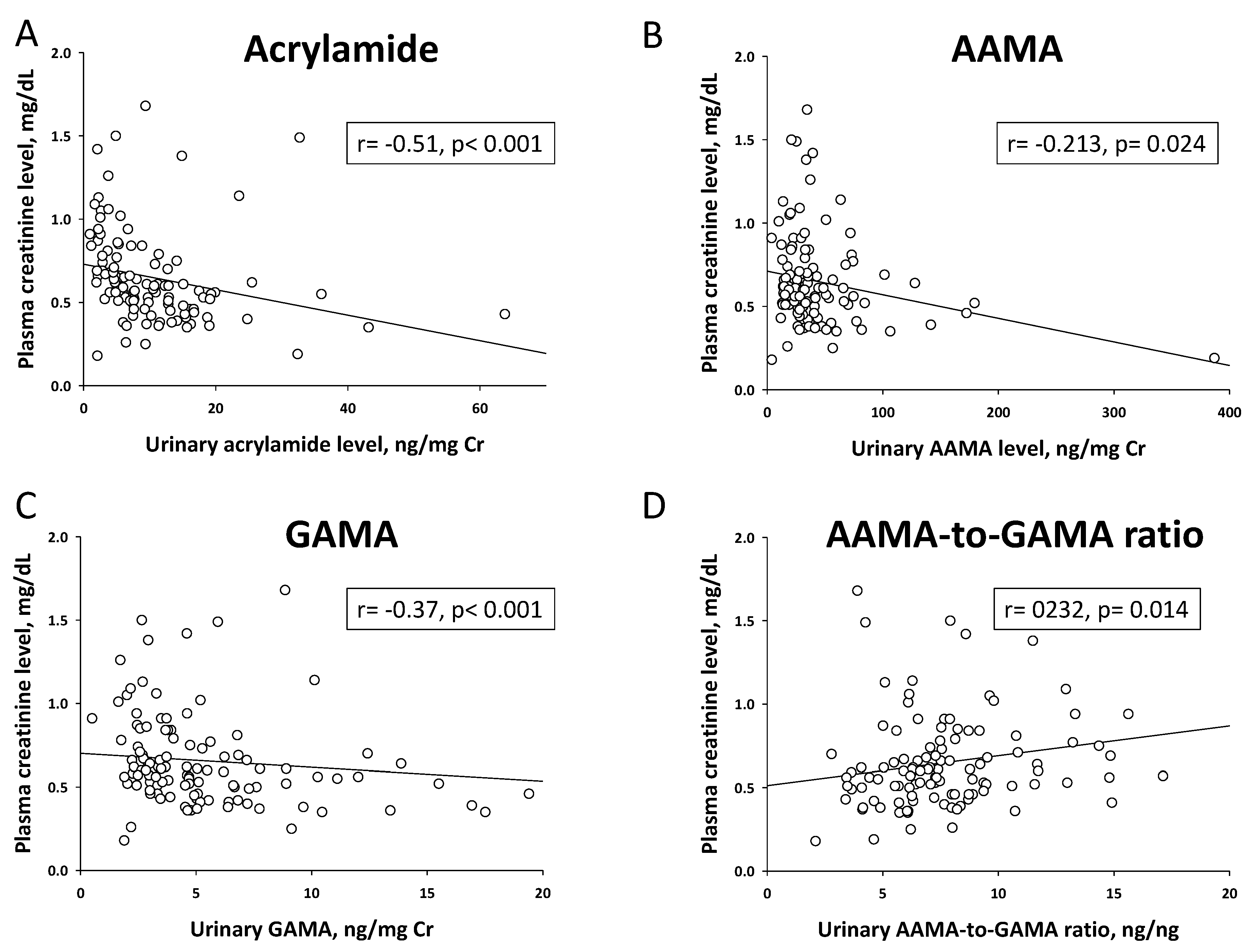
Children were reported to have a higher acrylamide intake than adults [
9]. In line with a previous study showing median urinary levels of AAMA and GAMA were 36.0 and 13.4 μg/L in children [
20], our results showed AAMA was 26.8 and GAMA was 4.1 μg/L (before normalization by Cr) in children and adolescents with CKD. Interestingly, urinary levels of acrylamide, AAMA, and GAMA were negatively correlated with plasma Cr level in the current study. It is presumably due to lower excretion of acrylamide metabolites in children with more advanced CKD. Additionally, we found only urinary acrylamide, but not AAMA and GAMA, levels were inversely associated with SBP and DBP load on ABPM. These findings suggest CKD children have a lower acrylamide conversion capacity or a lower excretion rate, leading to a higher internal exposure which may increase the risk of developing high BP.
Consistent with previous studies of pediatric CKD [
7,
21,
22], our data support the finding that left ventricular hypertrophy (LVH) is common and is associated with ABPM abnormalities in children with CKD, even in an early stage. In the current study, urinary acrylamide, AAMA and GAMA levels were negatively correlated with LV mass. Acrylamide exposure was reported to induce cardiotoxicity in animal studies [
23,
24], thus low urinary levels of acrylamide metabolites related to LVH in CKD children is likely to reflect decreased acrylamide excretion, or conversion may be a risk factor for adverse CV outcome. AASI is an index of arterial stiffness, which related to abnormal ABPM profile and LV mass in CKD children, tying well with our previous studies [
6,
22]. As expected, the severity of CKD is associated with high AASI and LV mass in the current study.
Notably, the positive associations between CV risk markers, LV mass, AASI, and the AAMA-to-GAMA ratio were observed in our study. The urinary AAMA-to-GAMA ratio is a measure of the extent of conversion of acrylamide to glycidamide and a high ratio reflects more acrylamide is conjugated with GSH than converted to glycidamide [
25]. It seems likely that acrylamide rather than glycidamide may be the substantial contributor to CV risk in CKD children. Since the toxicity of acrylamide is related to reducing GSH and provoking oxidative stress [
26], and GSH is beneficial in reducing CV risk in CKD [
27], whether this ratio may reflect the redox status and correlate with other oxidative stress markers in CKD children awaits further clarification.
In line with our previous studies [
6,
28], which showed that NO-related parameters correlated with ABPM abnormalities and CV risk markers, this present study further extends their associations with acrylamide metabolites in CKD children. Our data demonstrated that plasma citrulline level was associated with urinary levels of AAMA and GAMA, and the AAMA-to-GAMA ratio. Besides, urinary GAMA level was correlated with plasma SDMA level. In CKD, renal citrulline uptake is diminished, the amount of citrulline converted to arginine in the kidney is reduced, and plasma citrulline levels and turnover are elevated [
29]. SDMA is an endogenous NOS inhibitor and its level is elevated in advanced CKD [
30]. Accordingly, high citrulline and SDMA levels represent reduced NO bioavailability in favor of elevating BPs. Our data support the impaired NO pathway as possibly the major factor contributing to hypertension and CV risk in children with CKD. Noteworthy, the association of citrulline and SDMA with GAMA were found to be stronger than with AAMA, suggesting a probably stronger oxidative stress potency of glycidamide toward the impaired NO pathway than acrylamide. Because this study is the first to report the association between acrylamide metabolites and NO parameters, more studies are warranted to elucidate the mechanisms underlying acrylamide-induced impairment of NO-dependent CV risk in patients with CKD.
Our study has some limitations. First, we did not recruit non-CKD controls because we examined the difference of CV risk markers between two levels of renal function (i.e., CKD stage G1 vs. stage G2–G4). That is, children with CKD stage G1 were served as the controls in the present study. Although urinary levels of acrylamide metabolites determined in the present study are comparable to those previously published in children [
20], whether exposure levels of acrylamide are different between children with and without CKD remains to be determined. Second, we used ABPM reference from a different ethnic group [
31]. Although several indices of CV risk markers we used in the current study have been examined in children, their age-specific reference ranges are still lacking [
8]. Thus, our results may not be applicable to other ethnic populations until further reproducibility studies are conducted. Last, statistical comparisons were performed in a small cohort from one hospital and would not be representative of an entire population. Future multicenter studies with large sample sizes may be required to detect the true relationship.