The Role of Amino Acids in Neurotransmission and Fluorescent Tools for Their Detection
Abstract
:1. Introduction
- Presence of the molecule in neurons,
- Stored in synaptic vesicles and released in a Ca2+-dependent manner from neurons as a result of depolarization,
- Exogenous application of the molecule must elicit the same response from postsynaptic neurons as endogenously-released molecules due to binding to specific receptors, and
- The molecule must have a mechanism for its removal from the synapse.
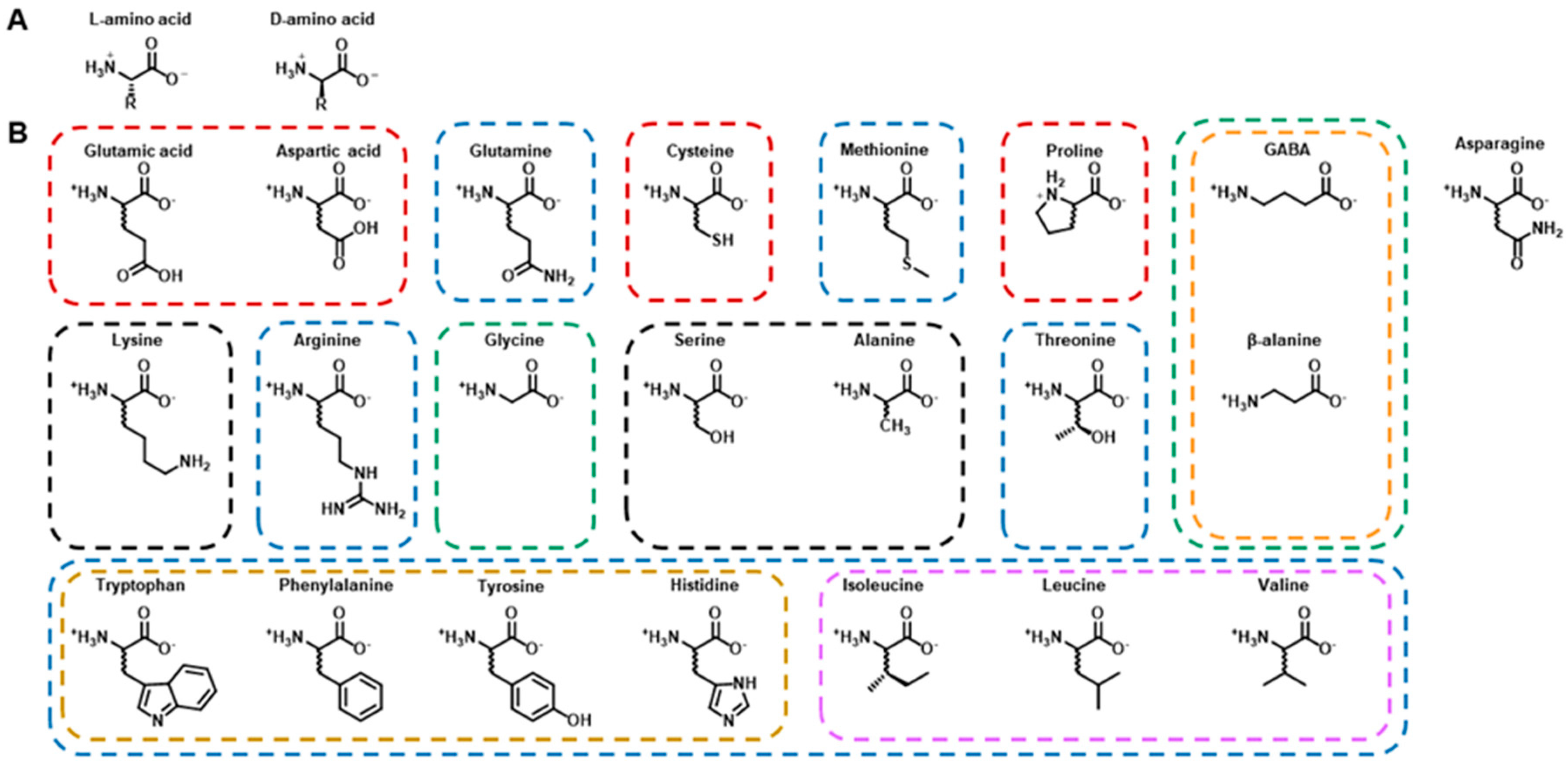
2. Amino Acids
2.1. Glutamic Acid
2.2. Aspartic Acid
2.3. Glutamine
2.4. Cysteine and Methionine: Sulfur-Containing Amino Acids
2.5. Proline
2.6. Asparagine
2.7. γ-Aminobutyric Acid
2.8. Lysine
2.9. Arginine
2.10. Glycine
2.11. Serine
2.12. Alanine
2.13. Threonine
2.14. β-Alanine
2.15. Aromatic Amino Acids
2.16. Branched-Chain Amino Acids
3. Fluorescence Imaging
3.1. Synthetic Dye-Based Indicators (Excluding FRET-Based Sensors)
3.2. Genetically Encoded Single FP-Based Indicators
3.3. Nanostructures (Excluding FRET-Based Sensors)
3.3.1. Quantum Dots
3.3.2. Carbon Nanotubes
3.4. Hybrid Strategies (Excluding FRET-Based Sensors)
3.5. FRET-Based Sensors
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AMPA | α-amino-3-hydroxy-5-methyl-4-isoxazoleproprionic acid |
| Asp | Aspartic acid |
| BBB | Blood–brain barrier |
| BCAAs | Branched-chain amino acids |
| CNS | Central nervous system |
| EAAT1 | Excitatory amino acid transporter 1 |
| FP | Fluorescent protein |
| FRET | Förster Resonance Energy Transfer |
| GABA | γ-Aminobutyric acid |
| GPCR | G protein-coupled receptors |
| GLAST-1 | Glutamate aspartate transporter 1 |
| GFP | Green fluorescent protein |
| mGluR5 | Metabotropic glutamate receptor 5 |
| MWCNT | Multiwalled carbon nanotubes |
| NMDA | N-methyl-d-aspartate |
| NIR | Near-infrared |
| NOx | Nitric oxide |
| PNS | Peripheral nervous system |
| PBP | Periplasmic binding protein |
| PA | Pipecolic acid |
| QD | Quantum dot |
| 5-HT | Serotonin |
| SWCNT | Single-walled carbon nanotubes |
| Snifit | SNAP tag-based indicator proteins with a fluorescent intramolecular tether |
| VGAT | Vesicular GABA transporter |
References
- Werman, R. A review—critical for idenctification of a central nervous system transmitter. Comp. Biochem. Physiol. 1966, 18, 745–766. [Google Scholar] [CrossRef]
- Wu, G. Amino acids: Metabolism, functions, and nutrition. Amino Acids 2009, 37, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Kehr, J.; Yoshitake, T. Monitoring molecules in neuroscience: Historical overview and current advancements. Front. Biosci. 2013, 5, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Nadler, J.V. Plasticity of Glutamate Synaptic Mechanisms. In Jasper’s Basic Mechanisms of the Epilepsies [Internet], 4th ed.; National Center for Biotechnology Information (US): Bethesda, MD, USA, 2012. [Google Scholar]
- Hassel, B.; Dingledine, R. Glutamate. In Basic Neurochemistry: Molecular, Cellular, and Medical Aspects, 7th ed.; Academic Press: San Diego, CA, USA, 2006; pp. 267–290. [Google Scholar]
- Curtis, D.; Watkins, J. The excitation and depression of spinal neurones by structurally related amino acids. J. Neurochem. 1960, 6, 117–141. [Google Scholar] [CrossRef]
- Curtis, D.; Phillis, J.; Watkins, J. The chemical excitation of spinal neurones by certain acidic amino acids. J. Physiol. 1960, 150, 656–682. [Google Scholar] [CrossRef] [PubMed]
- Curtis, D.; Watkins, J. Acidic amino acids with strong excitatory actions on mammalian neurones. J. Physiol. 1963, 166, 1–14. [Google Scholar] [CrossRef]
- Featherstone, D.E. Intercellular glutamate signaling in the nervous system and beyond. ACS Chem. Neurosci. 2010, 1, 4–12. [Google Scholar] [CrossRef] [Green Version]
- Bak, L.K.; Schousboe, A.; Waagepetersen, H.S. The glutamate/GABA-glutamine cycle: Aspects of transport, neurotransmitter homeostasis and ammonia transfer. J. Neurochem. 2006, 98, 641–653. [Google Scholar] [CrossRef]
- Meldrum, B.S. Glutamate as a neurotransmitter in the brain: Review of physiology and pathology. J. Nutr. 2000, 130, 1007S–1015S. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Danbolt, N.C. Glutamate as a neurotransmitter in the healthy brain. J. Neural Transm. 2014, 121, 799–817. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Fathali, H.; Mishra, D.; Olsson, T.; Keighron, J.D.; Skibicka, K.P.; Cans, A.-S. Counting the Number of Glutamate Molecules in Single Synaptic Vesicles. J. Am. Chem. Soc. 2019, 141, 17507–17511. [Google Scholar] [CrossRef] [PubMed]
- Clements, J.D. Transmitter timecourse in the synaptic cleft: Its role in central synaptic function. Trends Neurosci. 1996, 19, 163–171. [Google Scholar] [CrossRef]
- Clements, J.D.; Lester, R.; Tong, G.; Jahr, C.E.; Westbrook, G.L. The time course of glutamate in the synaptic cleft. Science 1992, 258, 1498–1501. [Google Scholar] [CrossRef] [PubMed]
- Kleckner, N.W.; Dingledine, R. Requirement for glycine in activation of NMDA-receptors expressed in Xenopus oocytes. Science 1988, 241, 835–837. [Google Scholar] [CrossRef] [PubMed]
- Mayer, M.L.; Westbrook, G.L.; Guthrie, P.B. Voltage-dependent block by Mg2+ of NMDA responses in spinal cord neurones. Nature 1984, 309, 261–263. [Google Scholar] [CrossRef]
- Morris, R.G.M. NMDA receptors and memory encoding. Neuropharmacology 2013, 74, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Nestler, E.J. The neural rejuvenation hypothesis of cocaine addiction. Trends Pharmacol. Sci. 2014, 35, 374–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.; Chang, L.; Song, Y.; Li, H.; Wu, Y. The role of NMDA receptors in Alzheimer’s disease. Front. Neurosci. 2019, 13. [Google Scholar] [CrossRef] [Green Version]
- Lau, A.; Tymianski, M. Glutamate receptors, neurotoxicity and neurodegeneration. Pflüg. Arch. Eur. J. Physiol. 2010, 460, 525–542. [Google Scholar] [CrossRef]
- Kullmann, D.M.; Asztely, F. Extrasynaptic glutamate spillover in the hippocampus: Evidence and implications. Trends Neurosci. 1998, 21, 8–14. [Google Scholar] [CrossRef]
- Hires, S.A.; Zhu, Y.; Tsien, R.Y. Optical measurement of synaptic glutamate spillover and reuptake by linker optimized glutamate-sensitive fluorescent reporters. Proc. Natl. Acad. Sci. USA 2008, 105, 4411–4416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parsons, M.P.; Raymond, L.A. Extrasynaptic NMDA receptor involvement in central nervous system disorders. Neuron 2014, 82, 279–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleck, M.; Henze, D.; Barrionuevo, G.; Palmer, A. Aspartate and glutamate mediate excitatory synaptic transmission in area CA1 of the hippocampus. J. Neurosci. 1993, 13, 3944–3955. [Google Scholar] [CrossRef] [PubMed]
- Docherty, M.; Bradford, H.; Wu, J.-Y. Co-release of glutamate and aspartate from cholinergic and GABAergic synaptosomes. Nature 1987, 330, 64–66. [Google Scholar] [CrossRef]
- Gundersen, V.; Holten, A.T.; Storm-Mathisen, J. GABAergic synapses in hippocampus exocytose aspartate on to NMDA receptors: Quantitative immunogold evidence for co-transmission. Mol. Cell. Neurosci. 2004, 26, 156–165. [Google Scholar] [CrossRef]
- Herring, B.E.; Silm, K.; Edwards, R.H.; Nicoll, R.A. Is aspartate an excitatory neurotransmitter? J. Neurosci. 2015, 35, 10168–10171. [Google Scholar] [CrossRef] [PubMed]
- Nadler, J.V. Aspartate release and signalling in the hippocampus. Neurochem. Res. 2011, 36, 668–676. [Google Scholar] [CrossRef]
- Chantranupong, L.; Saulnier, J.L.; Wang, W.; Jones, D.R.; Pacold, M.E.; Sabatini, B.L. Rapid purification and metabolomic profiling of synaptic vesicles from mammalian brain. bioRxiv 2020. [Google Scholar] [CrossRef]
- Baughman, R.W.; Gilbert, C.D. Aspartate and glutamate as possible neurotransmitters in the visual cortex. J. Neurosci. 1981, 1, 427–439. [Google Scholar] [CrossRef] [Green Version]
- Bradford, S.; Nadler, J. Aspartate release from rat hippocampal synaptosomes. Neuroscience 2004, 128, 751–765. [Google Scholar] [CrossRef]
- Nadler, J.V.; Vaca, K.W.; White, W.F.; Lynch, G.S.; Cotman, C.W. Aspartate and glutamate as possible transmitters of excitatory hippocampal afferents. Nature 1976, 260, 538–540. [Google Scholar] [CrossRef] [PubMed]
- Wiklund, L.; Toggenburger, G.; Cuénod, M. Aspartate: Possible neurotransmitter in cerebellar climbing fibers. Science 1982, 216, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, A.; Nishikawa, T.; Oka, T.; Takahashi, K.; Hayashi, T. Determination of free amino acid enantiomers in rat brain and serum by high-performance liquid chromatography after derivatization with N-tert.-butyloxycarbonyl-L-cysteine and o-phthaldialdehyde. J. Chromatogr. B Biomed. Sci. Appl. 1992, 582, 41–48. [Google Scholar] [CrossRef]
- Horio, M.; Ishima, T.; Fujita, Y.; Inoue, R.; Mori, H.; Hashimoto, K. Decreased levels of free d-aspartic acid in the forebrain of serine racemase (Srr) knock-out mice. Neurochem. Int. 2013, 62, 843–847. [Google Scholar] [CrossRef]
- Storck, T.; Schulte, S.; Hofmann, K.; Stoffel, W. Structure, expression, and functional analysis of a Na (+)-dependent glutamate/aspartate transporter from rat brain. Proc. Natl. Acad. Sci. USA 1992, 89, 10955–10959. [Google Scholar] [CrossRef] [Green Version]
- Reimer, R.J.; Edwards, R.H. Organic anion transport is the primary function of the SLC17/type I phosphate transporter family. Pflüg. Arch. Eur. J. Physiol. 2004, 447, 629–635. [Google Scholar] [CrossRef]
- Miyaji, T.; Echigo, N.; Hiasa, M.; Senoh, S.; Omote, H.; Moriyama, Y. Identification of a vesicular aspartate transporter. Proc. Natl. Acad. Sci. USA 2008, 105, 11720–11724. [Google Scholar] [CrossRef] [Green Version]
- Morland, C.; Nordengen, K.; Larsson, M.; Prolo, L.M.; Farzampour, Z.; Reimer, R.J.; Gundersen, V. Vesicular uptake and exocytosis of L-aspartate is independent of sialin. FASEB J. 2013, 27, 1264–1274. [Google Scholar] [CrossRef] [Green Version]
- Richards, D.S.; Griffith, R.W.; Romer, S.H.; Alvarez, F.J. Motor axon synapses on renshaw cells contain higher levels of aspartate than glutamate. PLoS ONE 2014, 9, e97240. [Google Scholar] [CrossRef] [Green Version]
- D’Aniello, S.; Somorjai, I.; Garcia-Fernàndez, J.; Topo, E.; D’Aniello, A. D-Aspartic acid is a novel endogenous neurotransmitter. FASEB J. 2011, 25, 1014–1027. [Google Scholar] [CrossRef] [Green Version]
- Ota, N.; Shi, T.; Sweedler, J.V. D-Aspartate acts as a signaling molecule in nervous and neuroendocrine systems. Amino Acids 2012, 43, 1873–1886. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Aniello, A.; Di Fiore, M.M.; Fisher, G.H.; Milone, A.; Seleni, A.; D’Aniello, S.; Perna, A.F.; Ingrosso, D. Occurrence of D-aspartic acid and N-methyl-D-aspartic acid in rat neuroendocrine tissues and their role in the modulation of luteinizing hormone and growth hormone release. FASEB J. 2000, 14, 699–714. [Google Scholar] [CrossRef] [PubMed]
- Kim, P.M.; Duan, X.; Huang, A.S.; Liu, C.Y.; Ming, G.-l.; Song, H.; Snyder, S.H. Aspartate racemase, generating neuronal D-aspartate, regulates adult neurogenesis. Proc. Natl. Acad. Sci. USA 2010, 107, 3175–3179. [Google Scholar] [CrossRef] [Green Version]
- Wolosker, H.; D’Aniello, A.; Snyder, S.H. D-aspartate disposition in neuronal and endocrine tissues: Ontogeny, biosynthesis and release. Neuroscience 2000, 100, 183–189. [Google Scholar] [CrossRef]
- Sakai, K.; Homma, H.; Lee, J.-A.; Fukushima, T.; Santa, T.; Tashiro, K.; Iwatsubo, T.; Imai, K. Emergence of D-aspartic acid in the differentiating neurons of the rat central nervous system. Brain Res. 1998, 808, 65–71. [Google Scholar] [CrossRef]
- D’Aniello, G.; Tolino, A.; D’aniello, A.; Errico, F.; Fisher, G.H.; Di Fiore, M.M. The role of D-aspartic acid and N-methyl-D-aspartic acid in the regulation of prolactin release. Endocrinology 2000, 141, 3862–3870. [Google Scholar] [CrossRef] [PubMed]
- D’Aniello, A. D-Aspartic acid: An endogenous amino acid with an important neuroendocrine role. Brain Res. Rev. 2007, 53, 215–234. [Google Scholar] [CrossRef] [PubMed]
- Errico, F.; Napolitano, F.; Nisticò, R.; Usiello, A. New insights on the role of free d-aspartate in the mammalian brain. Amino Acids 2012, 43, 1861–1871. [Google Scholar] [CrossRef]
- Molinaro, G.; Pietracupa, S.; Di Menna, L.; Pescatori, L.; Usiello, A.; Battaglia, G.; Nicoletti, F.; Bruno, V. d-Aspartate activates mGlu receptors coupled to polyphosphoinositide hydrolysis in neonate rat brain slices. Neurosci. Lett. 2010, 478, 128–130. [Google Scholar] [CrossRef]
- Ito, T.; Hayashida, M.; Kobayashi, S.; Muto, N.; Hayashi, A.; Yoshimura, T.; Mori, H. Serine racemase is involved in d-aspartate biosynthesis. J. Biochem. 2016, 160, 345–353. [Google Scholar] [CrossRef]
- Matsuda, S.; Katane, M.; Maeda, K.; Kaneko, Y.; Saitoh, Y.; Miyamoto, T.; Sekine, M.; Homma, H. Biosynthesis of d-aspartate in mammals: The rat and human homologs of mouse aspartate racemase are not responsible for the biosynthesis of d-aspartate. Amino Acids 2015, 47, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Tanaka-Hayashi, A.; Hayashi, S.; Inoue, R.; Ito, T.; Konno, K.; Yoshida, T.; Watanabe, M.; Yoshimura, T.; Mori, H. Is d-aspartate produced by glutamic-oxaloacetic transaminase-1 like 1 (Got1l1): A putative aspartate racemase? Amino Acids 2015, 47, 79–86. [Google Scholar] [CrossRef] [Green Version]
- Albrecht, J.; Sidoryk-Wegrzynowicz, M.; Zielinska, M.; Aschner, M. Roles of glutamine in neurotransmission. Neuron Glia Biol. 2010, 6, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Horio, M.; Kohno, M.; Fujita, Y.; Ishima, T.; Inoue, R.; Mori, H.; Hashimoto, K. Levels of d-serine in the brain and peripheral organs of serine racemase (Srr) knock-out mice. Neurochem. Int. 2011, 59, 853–859. [Google Scholar] [CrossRef]
- Kosenko, E.; Llansola, M.; Montoliu, C.; Monfort, P.; Rodrigo, R.; Hernandez-Viadel, M.; Erceg, S.; Sánchez-Perez, A.M.; Felipo, V. Glutamine synthetase activity and glutamine content in brain: Modulation by NMDA receptors and nitric oxide. Neurochem. Int. 2003, 43, 493–499. [Google Scholar] [CrossRef]
- Eid, T.; Tu, N.; Lee, T.-S.W.; Lai, J.C.K. Regulation of astrocyte glutamine synthetase in epilepsy. Neurochem. Int. 2013, 63, 670–681. [Google Scholar] [CrossRef] [Green Version]
- Rajkowska, G.; Stockmeier, C.A. Astrocyte pathology in major depressive disorder: Insights from human postmortem brain tissue. Curr. Drug Targets 2013, 14, 1225–1236. [Google Scholar] [CrossRef] [Green Version]
- Bernstein, H.-G.; Tausch, A.; Wagner, R.; Steiner, J.; Seeleke, P.; Walter, M.; Dobrowolny, H.; Bogerts, B. Disruption of glutamate-glutamine-GABA cycle significantly impacts on suicidal behaviour: Survey of the literature and own findings on glutamine synthetase. CNS Neurol. Disord. Drug Targets 2013, 12, 900–913. [Google Scholar] [CrossRef]
- Skowrońska, M.; Albrecht, J. Oxidative and nitrosative stress in ammonia neurotoxicity. Neurochem. Int. 2013, 62, 731–737. [Google Scholar] [CrossRef]
- Norenberg, M.D.; Rao, K.V.R.; Jayakumar, A.R. Signaling factors in the mechanism of ammonia neurotoxicity. Metab. Brain Dis. 2009, 24, 103–117. [Google Scholar] [CrossRef]
- Albrecht, J.; Norenberg, M.D. Glutamine: A Trojan horse in ammonia neurotoxicity. Hepatology 2006, 44, 788–794. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, J.; Zielińska, M.; Norenberg, M.D. Glutamine as a mediator of ammonia neurotoxicity: A critical appraisal. Biochem. Pharmacol. 2010, 80, 1303–1308. [Google Scholar] [CrossRef] [Green Version]
- Kolbaev, S.; Draguhn, A. Glutamine-induced membrane currents in cultured rat hippocampal neurons. Eur. J. Neurosci. 2008, 28, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Luengo, J.G.; Muñoz, M.-D.; Álvarez-Merz, I.; Herranz, A.S.; González, J.C.; del Río, R.M.; Hernández-Guijo, J.M.; Solís, J.M. Intracellular accumulation of amino acids increases synaptic potentials in rat hippocampal slices. Amino Acids 2019, 51, 1337–1351. [Google Scholar] [CrossRef]
- Dringen, R. Metabolism and functions of glutathione in brain. Prog. Neurobiol. 2000, 62, 649–671. [Google Scholar] [CrossRef]
- Dringen, R.; Gutterer, J.M.; Hirrlinger, J. Glutathione metabolism in brain: Metabolic interaction between astrocytes and neurons in the defense against reactive oxygen species. Eur. J. Biochem. 2000, 267, 4912–4916. [Google Scholar] [CrossRef]
- Dringen, R.; Hirrlinger, J. Glutathione pathways in the brain. Biol. Chem. 2003, 384, 505–516. [Google Scholar] [CrossRef]
- Keller, H.J.; Do, K.Q.; Zollinger, M.; Winterhalter, K.H.; Cuenod, M. Cysteine: Depolarization-induced release from rat brain in vitro. J. Neurochem. 1989, 52, 1801–1806. [Google Scholar] [CrossRef]
- Olney, J.W.; Zorumski, C.; Price, M.T.; Labruyere, J. L-Cysteine, a bicarbonate-sensitive endogenous excitotoxin. Science 1990, 248, 596–599. [Google Scholar] [CrossRef]
- Sagara, J.I.; Miura, K.; Bannai, S. Maintenance of neuronal glutathione by glial cells. J. Neurochem. 1993, 61, 1672–1676. [Google Scholar] [CrossRef]
- Janáky, R.; Varga, V.; Hermann, A.; Saransaari, P.; Oja, S.S. Mechanisms of L-cysteine neurotoxicity. Neurochem. Res. 2000, 25, 1397–1405. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, A.N.B.; Vicentini, F.; Calvo, D.J. Negative modulation of the GABA(A)rho 1 receptor function by L-cysteine. J. Neurochem. 2018, 144, 50–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peana, A.T.; Assaretti, A.R.; Muggironi, G.; Enrico, P.; Diana, M. Reduction of ethanol-derived acetaldehyde-induced motivational properties by L-cysteine. Alcohol. Clin. Exp. Res. 2009, 33, 43–48. [Google Scholar] [CrossRef]
- Peana, A.T.; Muggironi, G.; Calvisi, G.; Enrico, P.; Mereu, M.; Nieddu, M.; Boatto, G.; Diana, M. L-Cysteine reduces oral ethanol self-administration and reinstatement of ethanol-drinking behavior in rats. Pharmacol. Biochem. Behav. 2010, 94, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Peana, A.T.; Muggironi, G.; Fois, G.R.; Zinellu, M.; Sirca, D.; Diana, M. Effect of L-cysteine on acetaldehyde self-administration. Alcohol 2012, 46, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Sirca, D.; Enrico, P.; Mereu, M.; Peana, A.T.; Diana, M. L-cysteine prevents ethanol-induced stimulation of mesolimbic dopamine transmission. Alcohol. Clin. Exp. Res. 2011, 35, 862–869. [Google Scholar] [CrossRef]
- Lewerenz, J.; Hewett, S.J.; Huang, Y.; Lambros, M.; Gout, P.W.; Kalivas, P.W.; Massie, A.; Smolders, I.; Methner, A.; Pergande, M.; et al. The cystine/glutamate antiporter system x(c)(-) in health and disease: From molecular mechanisms to novel therapeutic opportunities. Antioxid. Redox Signal. 2013, 18, 522–555. [Google Scholar] [CrossRef] [Green Version]
- Soria, F.N.; Pérez-Samartín, A.; Martin, A.; Gona, K.B.; Llop, J.; Szczupak, B.; Chara, J.C.; Matute, C.; Domercq, M. Extrasynaptic glutamate release through cystine/glutamate antiporter contributes to ischemic damage. J. Clin. Investig. 2014, 124, 3645–3655. [Google Scholar] [CrossRef] [Green Version]
- McBean, G. Sulfur-Containing Amino Acids. In Handbook of Neurochemistry and Molecular Neurobiology: Amino Acids and Peptides in the Nervous System; Springer: Berlin/Heidelberg, Germany, 2007; pp. 133–154. [Google Scholar] [CrossRef]
- Qu, K.; Lee, S.; Bian, J.; Low, C.-M.; Wong, P.-H. Hydrogen sulfide: Neurochemistry and neurobiology. Neurochem. Int. 2008, 52, 155–165. [Google Scholar] [CrossRef]
- Zhang, X.; Bian, J.-S. Hydrogen sulfide: A neuromodulator and neuroprotectant in the central nervous system. ACS Chem. Neurosci. 2014, 5, 876–883. [Google Scholar] [CrossRef]
- Huxtable, R.J. Taurine in the central nervous system and the mammalian actions of taurine. Prog. Neurobiol. 1989, 32, 471–533. [Google Scholar] [CrossRef]
- Horikoshi, T.; Asanuma, A.; Yanagisawa, K.; Anzai, K.; Goto, S. Taurine and β-alanine act on both GABA and glycine receptors in Xenopus oocyte injected with mouse brain messenger RNA. Mol. Brain Res. 1988, 4, 97–105. [Google Scholar] [CrossRef]
- Davison, A.N.; Kaczmarek, L.K. Taurine—A possible neurotransmitter? Nature 1971, 234, 107–108. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, L.; Davison, A. Uptake and release of taurine from rat brain slices. J. Neurochem. 1972, 19, 2355–2362. [Google Scholar] [CrossRef]
- Oja, S.S.; Saransaari, P. Pharmacology of taurine. Proc. West. Pharmacol. Soc. 2007, 50, 8–15. [Google Scholar]
- Ochoa-de la Paz, L.; Martinez-Davila, I.; Miledi, R.; Martinez-Torres, A. Modulation of human GABAρ1 receptors by taurine. J. Neurosci. Res. 2008, 61, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Galarreta, M.; Bustamante, J.; del Rio, R.M.; Solis, J.M. Taurine induces a long-lasting increase of synaptic efficacy and axon excitability in the hippocampus. J. Neurosci. 1996, 16, 92–102. [Google Scholar] [CrossRef] [Green Version]
- Dominy, J., Jr.; Thinschmidt, J.S.; Peris, J.; Dawson, R., Jr.; Papke, R.L. Taurine-induced long-lasting potentiation in the rat hippocampus shows a partial dissociation from total hippocampal taurine content and independence from activation of known taurine transporters. J. Neurochem. 2004, 89, 1195–1205. [Google Scholar] [CrossRef]
- Hawkins, R.A.; O’Kane, R.L.; Simpson, I.A.; Vina, J.R. Structure of the blood–brain barrier and its role in the transport of amino acids. J. Nutr. 2006, 136, 218S–226S. [Google Scholar] [CrossRef]
- Bröer, A.; Tietze, N.; Kowalczuk, S.; Chubb, S.; Munzinger, M.; Bak, L.K.; Bröer, S. The orphan transporter v7-3 (slc6a15) is a Na+-dependent neutral amino acid transporter (B(0)AT2). Biochem. J. 2006, 393, 421–430. [Google Scholar] [CrossRef] [Green Version]
- Lipton, S.A.; Kim, W.-K.; Choi, Y.-B.; Kumar, S.; D’Emilia, D.M.; Rayudu, P.V.; Arnelle, D.R.; Stamler, J.S. Neurotoxicity associated with dual actions of homocysteine at the N-methyl-D-aspartate receptor. Proc. Natl. Acad. Sci. USA 1997, 94, 5923–5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poddar, R.; Paul, S. Homocysteine-NMDA receptor-mediated activation of extracellular signal-regulated kinase leads to neuronal cell death. J. Neurochem. 2009, 110, 1095–1106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brosnan, J.T.; Brosnan, M.E. The sulfur-containing amino acids: An overview. J. Nutr. 2006, 136, 1636S–1640S. [Google Scholar] [CrossRef] [Green Version]
- Ganguly, P.K.; Maddaford, T.G.; Edel, A.L.; Karmin, O.; Smeda, J.S.; Pierce, G.N. Increased homocysteine-induced release of excitatory amino acids in the striatum of spontaneously hypertensive stroke-prone rats. Brain Res. 2008, 1226, 192–198. [Google Scholar] [CrossRef]
- Hrncic, D.; Mikić, J.; Rasic-Markovic, A.; Velimirović, M.; Stojković, T.; Obrenović, R.; Rankov-Petrović, B.; Šušić, V.; Djuric, D.; Petronijević, N.; et al. Anxiety-related behavior in hyperhomocysteinemia induced by methionine nutritional overload in rats: Role of the brain oxidative stress. Can. J. Physiol. Pharmacol. 2016, 94, 1074–1082. [Google Scholar] [CrossRef]
- Bleich, S.; Spilker, K.; Kurth, C.; Degner, D.; Quintela-Schneider, M.; Javaheripour, K.; Rüther, E.; Kornhuber, J.; Wiltfang, J. Oxidative stress and an altered methionine metabolism in alcoholism. Neurosci. Lett. 2000, 293, 171–174. [Google Scholar] [CrossRef]
- Ho, P.I.; Collins, S.C.; Dhitavat, S.; Ortiz, D.; Ashline, D.; Rogers, E.; Shea, T.B. Homocysteine potentiates β-amyloid neurotoxicity: Role of oxidative stress. J. Neurochem. 2001, 78, 249–253. [Google Scholar] [CrossRef]
- Susser, E.; Brown, A.S.; Klonowski, E.; Allen, R.H.; Lindenbaum, J. Schizophrenia and impaired homocysteine metabolism: A possible association. Biol. Psychiatry 1998, 44, 141–143. [Google Scholar] [CrossRef]
- Johnson, J.L.; Roberts, E. Proline, glutamate and glutamine metabolism in mouse brain synaptosomes. Brain Res. 1984, 323, 247–256. [Google Scholar] [CrossRef]
- Clelland, C.L.; Read, L.L.; Baraldi, A.N.; Bart, C.P.; Pappas, C.A.; Panek, L.J.; Nadrich, R.H.; Clelland, J.D. Evidence for association of hyperprolinemia with schizophrenia and a measure of clinical outcome. Schizophr. Res. 2011, 131, 139–145. [Google Scholar] [CrossRef] [Green Version]
- Roussos, P.; Giakoumaki, S.G.; Bitsios, P. A risk PRODH haplotype affects sensorimotor gating, memory, schizotypy, and anxiety in healthy male subjects. Biol. Psychiatry 2009, 65, 1063–1070. [Google Scholar] [CrossRef] [PubMed]
- Paterlini, M.; Zakharenko, S.S.; Lai, W.-S.; Qin, J.; Zhang, H.; Mukai, J.; Westphal, K.G.; Olivier, B.; Sulzer, D.; Pavlidis, P. Transcriptional and behavioral interaction between 22q11. 2 orthologs modulates schizophrenia-related phenotypes in mice. Nat. Neurosci. 2005, 8, 1586–1594. [Google Scholar] [CrossRef] [PubMed]
- Takemoto, Y.; Semba, R. Immunohistochemical evidence for the localization of neurons containing the putative transmitter L-proline in rat brain. Brain Res. 2006, 1073, 311–315. [Google Scholar] [CrossRef] [Green Version]
- Mulder, A.H.; Snyder, S.H. Potassium-induced release of amino acids from cerebral cortex and spinal cord slices of the rat. Brain Res. 1974, 76, 297–308. [Google Scholar] [CrossRef]
- Nickolson, V.J. “On” and “Off” Responses of K+-Induced Synaptosomal Proline Release: Involvement of the Sodium Pump. J. Neurochem. 1982, 38, 289–292. [Google Scholar] [CrossRef] [PubMed]
- Parra, L.A.; Baust, T.; El Mestikawy, S.; Quiroz, M.; Hoffman, B.; Haflett, J.M.; Yao, J.K.; Torres, G.E. The orphan transporter Rxt1/NTT4 (SLC6A17) functions as a synaptic vesicle amino acid transporter selective for proline, glycine, leucine, and alanine. Mol. Pharmacol. 2008, 74, 1521–1532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henzi, V.; Reichling, D.B.; Helm, S.W.; Macdermott, A.B. L-Proline activates glutamate and glycine receptors in cultured rat dorsal horn neurons. Mol. Pharmacol. 1992, 41, 793–801. [Google Scholar]
- Crump, F.T.; Fremeau, R.T.; Craig, A.M. Localization of the brain-specific high-affinity L-proline transporter in cultured hippocampal neurons: Molecular heterogeneity of synaptic terminals. Mol. Cell. Neurosci. 1999, 13, 25–39. [Google Scholar] [CrossRef]
- Renick, S.E.; Kleven, D.T.; Chan, J.; Stenius, K.; Milner, T.A.; Pickel, V.M.; Fremeau, R.T. The mammalian brain high-affinity L-proline transporter is enriched preferentially in synaptic vesicles in a subpopulation of excitatory nerve terminals in rat forebrain. J. Neurosci. 1999, 19, 21–33. [Google Scholar] [CrossRef]
- Cohen, S.M.; Nadler, J.V. Proline-induced inhibition of glutamate release in hippocampal area CA1. Brain Res. 1997, 769, 333–339. [Google Scholar] [CrossRef]
- Cohen, S.M.; Nadler, J.V. Proline-induced potentiation of glutamate transmission. Brain Res. 1997, 761, 271–282. [Google Scholar] [CrossRef]
- Nadler, J.V.; Wang, A.; Hakim, A. Toxicity of L-proline toward rat hippocampal neurons. Brain Res. 1988, 456, 168–172. [Google Scholar] [CrossRef]
- Hamasu, K.; Shigemi, K.; Tsuneyoshi, Y.; Yamane, H.; Sato, H.; Denbow, D.M.; Furuse, M. Intracerebroventricular injection of L-proline and D-proline induces sedative and hypnotic effects by different mechanisms under an acute stressful condition in chicks. Amino Acids 2010, 38, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Hamasu, K.; Shigemi, K.; Kabuki, Y.; Tomonaga, S.; Denbow, D.M.; Furuse, M. Central L-proline attenuates stress-induced dopamine and serotonin metabolism in the chick forebrain. Neurosci. Lett. 2009, 460, 78–81. [Google Scholar] [CrossRef]
- Kandasamy, P.; Gyimesi, G.; Kanai, Y.; Hediger, M.A. Amino acid transporters revisited: New views in health and disease. Trends Biochem. Sci. 2018, 43, 752–789. [Google Scholar] [CrossRef] [PubMed]
- Fremeau, R.T.; Caron, M.G.; Blakely, R.D. Molecular cloning and expression of a high-affinity L-proline transporter expressed in putative glutamatergic pathways of rat brain. Neuron 1992, 8, 915–926. [Google Scholar] [CrossRef]
- Fremeau, R.T.; Velaz-Faircloth, M.; Miller, J.W.; Henzi, V.A.; Cohen, S.M.; Nadler, J.V.; Shafqat, S.; Blakely, R.D.; Domin, B. A novel nonopioid action of enkephalins: Competitive inhibition of the mammalian brain high affinity L-proline transporter. Mol. Pharmacol. 1996, 49, 1033–1041. [Google Scholar]
- Velaz-Faircloth, M.; Guadanoferraz, A.; Henzi, V.A.; Fremeau, R.T. Mammalian brain-specific L-proline transporter. J. Biol. Chem. 1995, 270, 15755–15761. [Google Scholar] [CrossRef] [Green Version]
- Schulz, D.; Morschel, J.; Schuster, S.; Eulenburg, V.; Gomeza, J. Inactivation of the mouse L-proline transporter PROT alters glutamatergic synapse biochemistry and perturbs behaviors required to respond to environmental changes. Front. Mol. Neurosci. 2018, 11, 279. [Google Scholar] [CrossRef] [Green Version]
- O’Brien, R.J.; Kamboj, S.; Ehlers, M.D.; Rosen, K.R.; Fischbach, G.D.; Huganir, R.L. Activity-dependent modulation of synaptic AMPA receptor accumulation. Neuron 1998, 21, 1067–1078. [Google Scholar] [CrossRef] [Green Version]
- Zalcman, G.; Federman, N.; Romano, A. CaMKII isoforms in learning and memory: Localization and function. Front. Mol. Neurosci. 2018, 11. [Google Scholar] [CrossRef] [PubMed]
- Delwing, D.; Bavaresco, C.S.; Wannmacher, C.M.; Wajner, M.; Dutra-Filho, C.S.; Wyse, A.T. Proline induces oxidative stress in cerebral cortex of rats. Int. J. Dev. Neurosci. 2003, 21, 105–110. [Google Scholar] [CrossRef]
- Delwing, D.; Chiarani, F.; Delwing, D.; Bavaresco, C.S.; Wannmacher, C.M.; Wajner, M.; Wyse, A.T. Proline reduces acetylcholinesterase activity in cerebral cortex of rats. Metab. Brain Dis. 2003, 18, 79–86. [Google Scholar] [CrossRef]
- Franzon, R.; Lamers, M.L.; Stefanello, F.M.; Wannmacher, C.M.; Wajner, M.; Wyse, A.T. Evidence that oxidative stress is involved in the inhibitory effect of proline on Na+, K+-ATPase activity in synaptic plasma membrane of rat hippocampus. Int. J. Dev. Neurosci. 2003, 21, 303–307. [Google Scholar] [CrossRef]
- Dieterich, D.C.; Landwehr, M.; Reissner, C.; Smalla, K.-H.; Richter, K.; Wolf, G.; Böckers, T.M.; Gundelfinger, E.D.; Kreutz, M.R. Gliap—A novel untypical l-asparaginase localized to rat brain astrocytes. J. Neurochem. 2003, 85, 1117–1125. [Google Scholar] [CrossRef] [PubMed]
- Ruzzo, E.K.; Capo-Chichi, J.-M.; Ben-Zeev, B.; Chitayat, D.; Mao, H.; Pappas, A.L.; Hitomi, Y.; Lu, Y.-F.; Yao, X.; Hamdan, F.F.; et al. Deficiency of asparagine synthetase causes congenital microcephaly and a progressive form of encephalopathy. Neuron 2013, 80, 429–441. [Google Scholar] [CrossRef] [Green Version]
- Palmer, E.E.; Hayner, J.; Sachdev, R.; Cardamone, M.; Kandula, T.; Morris, P.; Dias, K.-R.; Tao, J.; Miller, D.; Zhu, Y. Asparagine synthetase deficiency causes reduced proliferation of cells under conditions of limited asparagine. Mol. Genet. Metab. 2015, 116, 178–186. [Google Scholar] [CrossRef]
- Butterworth, R.F.; Landreville, F.; Hamel, E.; Merkel, A.; Giguere, F.; Barbeau, A. Effect of asparagine, glutamine and insulin on cerebral amino acid neurotransmitters. Can. J. Neurol. Sci. 1980, 7, 447–450. [Google Scholar] [CrossRef]
- Li, Y.; Sun, H.; Chen, Z.; Xu, H.; Bu, G.; Zheng, H. Implications of GABAergic neurotransmission in Alzheimer’s disease. Front. Aging Neurosci. 2016, 8, 31. [Google Scholar] [CrossRef] [Green Version]
- Li, K.; Xu, E. The role and the mechanism of gamma-aminobutyric acid during central nervous system development. Neurosci. Bull. 2008, 24, 195–200. [Google Scholar] [CrossRef] [Green Version]
- Wong, C.G.T.; Bottiglieri, T.; Snead, O.C., III. GABA, γ-hydroxybutyric acid, and neurological disease. Ann. Neurol. 2003, 54, S3–S12. [Google Scholar] [CrossRef]
- Garret, M.; Du, Z.; Chazalon, M.; Cho, Y.H.; Baufreton, J. Alteration of GABAergic neurotransmission in Huntington’s disease. CNS Neurosci. Ther. 2018, 24, 292–300. [Google Scholar] [CrossRef]
- Hallen, A.; Jamie, J.F.; Cooper, A.J.L. Lysine metabolism in mammalian brain: An update on the importance of recent discoveries. Amino Acids 2013, 45, 1249–1272. [Google Scholar] [CrossRef] [Green Version]
- Posset, R.; Opp, S.; Struys, E.A.; Völkl, A.; Mohr, H.; Hoffmann, G.F.; Kölker, S.; Sauer, S.W.; Okun, J.G. Understanding cerebral L-lysine metabolism: The role of L-pipecolate metabolism in Gcdh-deficient mice as a model for glutaric aciduria type I. J. Inherit. Metab. Dis. 2015, 38, 265–272. [Google Scholar] [CrossRef]
- Papes, F.; Surpili, M.J.; Langone, F.; Trigo, J.R.; Arruda, P. The essential amino acid lysine acts as precursor of glutamate in the mammalian central nervous system. FEBS Lett. 2001, 488, 34–38. [Google Scholar] [CrossRef] [Green Version]
- Struys, E.A.; Jansen, E.E.W.; Salomons, G.S. Human pyrroline-5-carboxylate reductase (PYCR1) acts on Δ1-piperideine-6-carboxylate generating L-pipecolic acid. J. Inherit. Metab. Dis. 2014, 37, 327–332. [Google Scholar] [CrossRef]
- Struys, E.A.; Jakobs, C. Metabolism of lysine in α-aminoadipic semialdehyde dehydrogenase-deficient fibroblasts: Evidence for an alternative pathway of pipecolic acid formation. FEBS Lett. 2010, 584, 181–186. [Google Scholar] [CrossRef] [Green Version]
- Pena, I.A.; Marques, L.A.; Laranjeira, Â.B.; Yunes, J.A.; Eberlin, M.N.; MacKenzie, A.; Arruda, P. Mouse lysine catabolism to aminoadipate occurs primarily through the saccharopine pathway; implications for pyridoxine dependent epilepsy (PDE). Biochim. Biophys. Acta 2017, 1863, 121–128. [Google Scholar] [CrossRef]
- Crowther, L.M.; Mathis, D.; Poms, M.; Plecko, B. New insights into human lysine degradation pathways with relevance to pyridoxine-dependent epilepsy due to antiquitin deficiency. J. Inherit. Metab. Dis. 2019, 42, 620–628. [Google Scholar] [CrossRef] [Green Version]
- Chang, Y.-F.; Myslinski, N.R. Effects of L-lysine and its metabolites on pentylenetetrazol-induced seizures. Neurosci. Lett. 1985, 59, 79–84. [Google Scholar] [CrossRef]
- Gao, X.-M.; Chang, Y.-F. Enhancement of benzodiazepine receptor binding by L-lysine is chloride-dependent and due to increase in binding affinity. Eur. J. Pharmacol. 1989, 173, 197–200. [Google Scholar] [CrossRef]
- Chang, Y.-F.; Gao, X.-M. L-lysine is a barbiturate-like anticonvulsant and modulator of the benzodiazepine receptor. Neurochem. Res. 1995, 20, 931–937. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.F.; Wang, Y.; Cauley, R.K.; Gao, X.M. Chronic L-lysine develops anti-pentylenetetrazol tolerance and reduces synaptic GABAergic sensitivity. Eur. J. Biochem. 1993, 233, 209–217. [Google Scholar] [CrossRef]
- Ebrahimi, H.A.; Ebrahimi, S. Evaluation of the effects of charged amino acids on uncontrolled seizures. Neurol. Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smriga, M.; Torii, K. Prolonged treatment with l-lysine and l-arginine reduces stress-induced anxiety in an elevated plus maze. Nutr. Neurosci. 2003, 6, 125–128. [Google Scholar] [CrossRef]
- Smriga, M.; Torii, K. L-Lysine acts like a partial serotonin receptor 4 antagonist and inhibits serotonin-mediated intestinal pathologies and anxiety in rats. Proc. Natl. Acad. Sci. USA 2003, 100, 15370–15375. [Google Scholar] [CrossRef] [Green Version]
- Clemmensen, C.; Smajilovic, S.; Wellendorph, P.; Bräuner-Osborne, H. The GPCR, class C, group 6, subtype A (GPRC6A) receptor: From cloning to physiological function. Br. J. Pharmacol. 2014, 171, 1129–1141. [Google Scholar] [CrossRef] [Green Version]
- Kondoh, T.; Kameishi, M.; Mallick, H.; Ono, T.; Torii, K. Lysine and arginine reduce the effects of cerebral ischemic insults and inhibit glutamate-induced neuronal activity in rats. Front. Integr. Neurosci. 2010, 4. [Google Scholar] [CrossRef] [Green Version]
- Severyanova, L.A.; Lazarenko, V.A.; Plotnikov, D.V.; Dolgintsev, M.E.; Kriukov, A.A. L-Lysine as the molecule influencing selective brain activity in pain-induced behavior of rats. Int. J. Mol. Sci. 2019, 20, 1899. [Google Scholar] [CrossRef] [Green Version]
- Bae, S.; Xu, Q.; Hutchinson, D.; Colton, C. Y+ and y+ L arginine transporters in neuronal cells expressing tyrosine hydroxylase. Biochim. Biophys. Acta 2005, 1745, 65–73. [Google Scholar] [CrossRef] [Green Version]
- Whitfield, J.H.; Zhang, W.H.; Herde, M.K.; Clifton, B.E.; Radziejewski, J.; Janovjak, H.; Henneberger, C.; Jackson, C.J. Construction of a robust and sensitive arginine biosensor through ancestral protein reconstruction. Protein Sci. 2015, 24, 1412–1422. [Google Scholar] [CrossRef] [Green Version]
- Wiesinger, H. Arginine, Citrulline, and Ornithine. In Handbook of Neurochemistry and Molecular Neurobiology: Amino Acids and Peptides in the Nervous System; Lajtha, A., Oja, S.S., Schousboe, A., Saransaari, P., Eds.; Springer: Boston, MA, USA, 2007; pp. 99–115. [Google Scholar] [CrossRef]
- Wiesinger, H. Arginine metabolism and the synthesis of nitric oxide in the nervous system. Prog. Neurobiol. 2001, 64, 365–391. [Google Scholar] [CrossRef]
- Contestabile, A. Roles of NMDA receptor activity and nitric oxide production in brain development. Brain Res. Rev. 2000, 32, 476–509. [Google Scholar] [CrossRef]
- Cherian, L.; Hlatky, R.; Robertson, C.S. Nitric oxide in traumatic brain injury. Brain Pathol. 2004, 14, 195–201. [Google Scholar] [CrossRef]
- Mysliveček, J.; Hassmannová, J.; Barcal, J.; Šafanda, J.; Žalud, V. Inhibitory learning and memory in newborn rats influenced by nitric oxide. Neuroscience 1996, 71, 299–312. [Google Scholar] [CrossRef]
- Susswein, A.J.; Katzoff, A.; Miller, N.; Hurwitz, I. Nitric oxide and memory. Neuroscientist 2004, 10, 153–162. [Google Scholar] [CrossRef]
- Kumar, A.; Chanana, P. Role of nitric oxide in stress-induced anxiety: From pathophysiology to therapeutic target. Vitam. Horm. 2017, 103, 147–167. [Google Scholar] [CrossRef]
- Suenaga, R.; Yamane, H.; Tomonaga, S.; Asechi, M.; Adachi, N.; Tsuneyoshi, Y.; Kurauchi, I.; Sato, H.; Denbow, D.M.; Furuse, M. Central L-arginine reduced stress responses are mediated by L-ornithine in neonatal chicks. Amino Acids 2008, 35, 107–113. [Google Scholar] [CrossRef]
- Kurata, K.; Nagasawa, M.; Tomonaga, S.; Aoki, M.; Morishita, K.; Denbow, D.M.; Furuse, M. Orally administered L-ornithine elevates brain L-ornithine levels and has an anxiolytic-like effect in mice. Nutr. Neurosci. 2011, 14, 243–248. [Google Scholar] [CrossRef]
- Miyake, M.; Kirisako, T.; Kokubo, T.; Miura, Y.; Morishita, K.; Okamura, H.; Tsuda, A. Randomised controlled trial of the effects of L-ornithine on stress markers and sleep quality in healthy workers. Nutr. J. 2014, 13, 53. [Google Scholar] [CrossRef] [Green Version]
- Schulze, A. Creatine Deficiency Syndromes. In Guanidino Compounds in Biology and Medicine; Springer: New York, NY, USA, 2003; pp. 143–150. [Google Scholar]
- de Koning, T.J.; Fuchs, S.A.; Klomp, L.W.J. Serine, Glycine, and Threonine. In Handbook of Neurochemistry and Molecular Neurobiology: Amino Acids and Peptides in the Nervous System; Lajtha, A., Oja, S.S., Schousboe, A., Saransaari, P., Eds.; Springer: Boston, MA, USA, 2007; pp. 23–45. [Google Scholar] [CrossRef]
- Curtis, D.; Hösli, L.; Johnston, G. Inhibition of spinal neurones by glycine. Nature 1967, 215, 1502–1503. [Google Scholar] [CrossRef]
- Zafra, F.; Aragon, C.; Olivares, L.; Danbolt, N.C.; Gimenez, C.; Storm-Mathisen, J. Glycine transporters are differentially expressed among CNS cells. J. Neurosci. 1995, 15, 3952–3969. [Google Scholar] [CrossRef] [PubMed]
- Dutertre, S.; Becker, C.-M.; Betz, H. Inhibitory glycine receptors: An update. J. Biol. Chem. 2012, 287, 40216–40223. [Google Scholar] [CrossRef] [Green Version]
- Jonas, P.; Bischofberger, J.; Sandkühler, J. Corelease of two fast neurotransmitters at a central synapse. Science 1998, 281, 419–424. [Google Scholar] [CrossRef] [Green Version]
- Aubrey, K.R.; Supplisson, S. Heterogeneous signaling at GABA and glycine co-releasing terminals. Front. Synaptic Neurosci. 2018, 10, 40. [Google Scholar] [CrossRef] [Green Version]
- Russier, M.; Kopysova, I.L.; Ankri, N.; Ferrand, N.; Debanne, D. GABA and glycine co-release optimizes functional inhibition in rat brainstem motoneurons in vitro. J. Physiol. 2002, 541, 123–137. [Google Scholar] [CrossRef]
- Apostolides, P.F.; Trussell, L.O. Rapid, activity-independent turnover of vesicular transmitter content at a mixed glycine/GABA synapse. J. Neurosci. 2013, 33, 4768–4781. [Google Scholar] [CrossRef]
- López-Corcuera, B.; Geerlings, A.; Aragón, C. Glycine neurotransmitter transporters: An update. Mol. Membr. Biol. 2001, 18, 13–20. [Google Scholar] [CrossRef]
- Harsing, L.G., Jr.; Matyus, P. Mechanisms of glycine release, which build up synaptic and extrasynaptic glycine levels: The role of synaptic and non-synaptic glycine transporters. Brain Res. Bull. 2013, 93, 110–119. [Google Scholar] [CrossRef]
- Miraucourt, L.S.; Dallel, R.; Voisin, D.L. Glycine inhibitory dysfunction turns touch into pain through PKCgamma interneurons. PLoS ONE 2007, 2. [Google Scholar] [CrossRef]
- Rajendra, S.; Lynch, J.W.; Schofield, P.R. The glycine receptor. Pharmacol. Ther. 1997, 73, 121–146. [Google Scholar] [CrossRef]
- Lynch, J.W. Native glycine receptor subtypes and their physiological roles. Neuropharmacology 2009, 56, 303–309. [Google Scholar] [CrossRef] [Green Version]
- Avila, A.; Nguyen, L.; Rigo, J.-M. Glycine receptors and brain development. Front. Cell. Neurosci. 2013, 7, 184. [Google Scholar] [CrossRef] [Green Version]
- Flint, A.C.; Liu, X.; Kriegstein, A.R. Nonsynaptic glycine receptor activation during early neocortical development. Neuron 1998, 20, 43–53. [Google Scholar] [CrossRef] [Green Version]
- Avila, A.; Vidal, P.M.; Dear, T.N.; Harvey, R.J.; Rigo, J.-M.; Nguyen, L. Glycine receptor α2 subunit activation promotes cortical interneuron migration. Cell Rep. 2013, 4, 738–750. [Google Scholar] [CrossRef]
- Papouin, T.; Ladépêche, L.; Ruel, J.; Sacchi, S.; Labasque, M.; Hanini, M.; Groc, L.; Pollegioni, L.; Mothet, J.-P.; Oliet, S.H.R. Synaptic and extrasynaptic NMDA receptors are gated by different endogenous coagonists. Cell 2012, 150, 633–646. [Google Scholar] [CrossRef] [Green Version]
- Ahmadi, S.; Muth-Selbach, U.; Lauterbach, A.; Lipfert, P.; Neuhuber, W.L.; Zeilhofer, H.U. Facilitation of spinal NMDA receptor currents by spillover of synaptically released glycine. Science 2003, 300, 2094–2097. [Google Scholar] [CrossRef] [Green Version]
- Jaeken, J.; Detheux, M.; Fryns, J.P.; Collet, J.F.; Alliet, P.; Van Schaftingen, E. Phosphoserine phosphatase deficiency in a patient with Williams syndrome. J. Med. Genet. 1997, 34, 594–596. [Google Scholar] [CrossRef] [Green Version]
- Tabatabaie, L.; Klomp, L.; Berger, R.; De Koning, T. L-serine synthesis in the central nervous system: A review on serine deficiency disorders. Mol. Genet. Metab. 2010, 99, 256–262. [Google Scholar] [CrossRef]
- Quackenbush, E.J.; Kraemer, K.H.; Gahl, W.A.; Schirch, V.; Whiteman, D.A.; Levine, K.; Levy, H.L. Hypoglycinaemia and psychomotor delay in a child with xeroderma pigmentosum. J. Inherit. Metab. Dis. 1999, 22, 915–924. [Google Scholar] [CrossRef]
- Buratta, S.; Hamberger, A.; Ryberg, H.; Nyström, B.; Sandberg, M.; Mozzi, R. Effect of serine and ethanolamine administration on phospholipid-related compounds and neurotransmitter amino acids in the rabbit hippocampus. J. Neurochem. 1998, 71, 2145–2150. [Google Scholar] [CrossRef]
- Furuya, S.; Tabata, T.; Mitoma, J.; Yamada, K.; Yamasaki, M.; Makino, A.; Yamamoto, T.; Watanabe, M.; Kano, M.; Hirabayashi, Y. L-Serine and glycine serve as major astroglia-derived trophic factors for cerebellar Purkinje neurons. Proc. Natl. Acad. Sci. USA 2000, 97, 11528–11533. [Google Scholar] [CrossRef] [Green Version]
- Mitoma, J.; Furuya, S.; Hirabayashi, Y. A novel metabolic communication between neurons and astrocytes: Non-essential amino acid l-serine released from astrocytes is essential for developing hippocampal neurons. Neurosci. Res. 1998, 30, 195–199. [Google Scholar] [CrossRef]
- De Miranda, J.; Santoro, A.; Engelender, S.; Wolosker, H. Human serine racemase: Moleular cloning, genomic organization and functional analysis. Gene 2000, 256, 183–188. [Google Scholar] [CrossRef]
- Wolosker, H.; Blackshaw, S.; Snyder, S.H. Serine racemase: A glial enzyme synthesizing D-serine to regulate glutamate-N-methyl-D-aspartate neurotransmission. Proc. Natl. Acad. Sci. USA 1999, 96, 13409–13414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miya, K.; Inoue, R.; Takata, Y.; Abe, M.; Natsume, R.; Sakimura, K.; Hongou, K.; Miyawaki, T.; Mori, H. Serine racemase is predominantly localized in neurons in mouse brain. J. Comp. Neurol. 2008, 510, 641–654. [Google Scholar] [CrossRef]
- Kartvelishvily, E.; Shleper, M.; Balan, L.; Dumin, E.; Wolosker, H. Neuron-derived D-serine release provides a novel means to activate N-methyl-D-aspartate receptors. J. Biol. Chem. 2006, 281, 14151–14162. [Google Scholar] [CrossRef] [Green Version]
- Mustafa, A.K.; Kim, P.M.; Snyder, S.H. D-Serine as a putative glial neurotransmitter. Neuron Glia Biol. 2004, 1, 275–281. [Google Scholar] [CrossRef] [Green Version]
- Van Horn, M.R.; Sild, M.; Ruthazer, E.S. D-serine as a gliotransmitter and its roles in brain development and disease. Front. Cell. Neurosci. 2013, 7, 39. [Google Scholar] [CrossRef] [Green Version]
- Lin, C.H.; Yang, H.T.; Lane, H.Y. D-Glutamate, D-serine, and D-alanine differ in their roles in cognitive decline in patients with Alzheimer’s disease or mild cognitive impairment. Pharmacol. Biochem. Behav. 2019, 185. [Google Scholar] [CrossRef]
- Wegner, S.A.; Hu, B.; Sergio, T.D.O.; Darevsky, D.; Kwok, C.C.-Y.; Lei, K.; Hopf, F.W. A novel NMDA receptor-based intervention to suppress compulsion-like alcohol drinking. Neuropharmacology 2019, 157, 107681. [Google Scholar] [CrossRef] [PubMed]
- Wolosker, H. D-serine regulation of NMDA receptor activity. Sci. STKE 2006, 2006, pe41. [Google Scholar] [CrossRef] [Green Version]
- Morikawa, A.; Hamase, K.; Zaitsu, K. Determination of D-alanine in the rat central nervous system and periphery using column-switching high-performance liquid chromatography. Anal. Biochem. 2003, 312, 66–72. [Google Scholar] [CrossRef]
- Konno, R.; Niwa, A.; Yasumura, Y. Intestinal bacterial origin of D-alanine in urine of mutant mice lacking D-amino-acid oxidase. Biochem. J. 1990, 268, 263. [Google Scholar] [CrossRef] [PubMed]
- Mehdi, S. Antibiotic-induced psychosis: A link to D-alanine? Med. Hypotheses 2010, 75, 676–677. [Google Scholar] [CrossRef]
- Oldendorf, W.H. Stereospecificity of blood-brain barrier permeability to amino acids. Am. J. Physiol. Leg. Content 1973, 224, 967–969. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, A.; Nishikawa, T.; Konno, R.; Niwa, A.; Yasumura, Y.; Oka, T.; Takahashi, K. Free D-serine, D-aspartate and D-alanine in central nervous system and serum in mutant mice lacking D-amino acid oxidase. Neurosci. Lett. 1993, 152, 33–36. [Google Scholar] [CrossRef]
- Iversen, S.D.; Wilkinson, S.; Simpson, B. Enhanced amphetamine responses after frontal cortex lesions in the rat. Eur. J. Pharmacol. 1971, 13, 387–390. [Google Scholar] [CrossRef]
- Atsushi, H.; Toru, N.; Takae, O.; Kiyohisa, T. D-Alanine inhibits methamphetamine-induced hyperactivity in rats. Eur. J. Pharmacol. 1991, 202, 105–107. [Google Scholar] [CrossRef]
- Leriche, L.; Schwartz, J.-C.; Sokoloff, P. The dopamine D3 receptor mediates locomotor hyperactivity induced by NMDA receptor blockade. Neuropharmacology 2003, 45, 174–181. [Google Scholar] [CrossRef]
- Jones, C.A.; Watson, D.J.G.; Fone, K.C.F. Animal models of schizophrenia. Br. J. Pharmacol. 2011, 164, 1162–1194. [Google Scholar] [CrossRef] [PubMed]
- Olney, J.W.; Newcomer, J.W.; Farber, N.B. NMDA receptor hypofunction model of schizophrenia. J. Psychiatr. Res. 1999, 33, 523–533. [Google Scholar] [CrossRef]
- Hashimoto, K. The NMDA receptor hypofunction hypothesis for schizophrenia and glycine modulatory sites on the NMDA receptors as potential therapeutic drugs. Clin. Psychopharmacol. Neurosci. 2006, 4, 3–10. [Google Scholar]
- Tsai, G.E.; Yang, P.; Chang, Y.-C.; Chong, M.-Y. D-alanine added to antipsychotics for the treatment of schizophrenia. Biol. Psychiatry 2006, 59, 230–234. [Google Scholar] [CrossRef]
- Horio, M.; Fujita, Y.; Ishima, T.; Iyo, M.; Ferraris, D.; Tsukamoto, T.; Hashimoto, K. Effects of D-amino acid oxidase inhibitor on the extracellular D-alanine levels and the efficacy of D-alanine on dizocilpine-induced prepulse inhibition deficits in mice. Open Clin. Chem. J. 2009, 2. [Google Scholar] [CrossRef] [Green Version]
- Bird, M.I.; Nunn, P.B.; Lord, L.A.J. Formation of glycine and aminoacetone from l-threonine by rat liver mitochondria. Biochim. Biophys. Acta 1984, 802, 229–236. [Google Scholar] [CrossRef]
- Maher, T.J.; Wurtman, R.J. L-Threonine administration increases glycine concentrations in the rat central nervous system. Life Sci. 1980, 26, 1283–1286. [Google Scholar] [CrossRef]
- Lee, A.; Patterson, V. A double-blind study of L-threonine in patients with spinal spasticity. Acta Neurol. Scand. 1993, 88, 334–338. [Google Scholar] [CrossRef]
- Paisley, S.; Beard, S.; Hunn, A.; Wight, J. Clinical effectiveness of oral treatments for spasticity in multiple sclerosis: A systematic review. Mult. Scler. 2002, 8, 319–329. [Google Scholar] [CrossRef]
- Tiedje, K.E.; Stevens, K.; Barnes, S.; Weaver, D.F. β-Alanine as a small molecule neurotransmitter. Neurochem. Int. 2010, 57, 177–188. [Google Scholar] [CrossRef]
- Juge, N.; Omote, H.; Moriyama, Y. Vesicular GABA transporter (VGAT) transports β-alanine. J. Neurochem. 2013, 127, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, T.; Harada, M.; Ogi, K.; Maruyama, M.; Fujii, R.; Tanaka, H.; Fukusumi, S.; Komatsu, H.; Hosoya, M.; Noguchi, Y. Identification of a G protein-coupled receptor specifically responsive to β-alanine. J. Biol. Chem. 2004, 279, 23559–23564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dong, X.; Han, S.-k.; Zylka, M.J.; Simon, M.I.; Anderson, D.J. A diverse family of GPCRs expressed in specific subsets of nociceptive sensory neurons. Cell 2001, 106, 619–632. [Google Scholar] [CrossRef] [Green Version]
- Curtis, D.; Phillis, J.; Watkins, J. The depression of spinal neurones by γ-amino-n-butyric acid and β-alanine. J. Physiol. 1959, 146, 185–203. [Google Scholar] [CrossRef] [PubMed]
- Zylka, M.J.; Dong, X.; Southwell, A.L.; Anderson, D.J. Atypical expansion in mice of the sensory neuron-specific Mrg G protein-coupled receptor family. Proc. Natl. Acad. Sci. USA 2003, 100, 10043–10048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavanaugh, D.J.; Lee, H.; Lo, L.; Shields, S.D.; Zylka, M.J.; Basbaum, A.I.; Anderson, D.J. Distinct subsets of unmyelinated primary sensory fibers mediate behavioral responses to noxious thermal and mechanical stimuli. Proc. Natl. Acad. Sci. USA 2009, 106, 9075–9080. [Google Scholar] [CrossRef] [Green Version]
- Crozier, R.A.; Ajit, S.K.; Kaftan, E.J.; Pausch, M.H. MrgD activation inhibits KCNQ/M-currents and contributes to enhanced neuronal excitability. J. Neurosci. 2007, 27, 4492–4496. [Google Scholar] [CrossRef]
- Zhuo, R.G.; Ma, X.Y.; Zhou, P.L.; Liu, X.Y.; Zhang, K.; Wei, X.L.; Yan, H.T.; Xu, J.P.; Zheng, J.Q. Mas-related G protein-coupled receptor D is coupled to endogenous calcium-activated chloride channel in Xenopus oocytes. J. Physiol. Biochem. 2014, 70, 185–191. [Google Scholar] [CrossRef]
- Wang, C.; Gu, L.; Ruan, Y.; Geng, X.; Xu, M.; Yang, N.; Yu, L.; Jiang, Y.; Zhu, C.; Yang, Y.; et al. Facilitation of MrgprD by TRP-A1 promotes neuropathic pain. FASEB J. 2019, 33, 1360–1373. [Google Scholar] [CrossRef]
- Liu, Q.; Sikand, P.; Ma, C.; Tang, Z.; Han, L.; Li, Z.; Sun, S.; LaMotte, R.H.; Dong, X. Mechanisms of itch evoked by β-alanine. J. Neurosci. 2012, 32, 14532–14537. [Google Scholar] [CrossRef]
- Fernstrom, J.D. Branched-chain amino acids and brain function. J. Nutr. 2005, 135, 1539S–1546S. [Google Scholar] [CrossRef] [PubMed]
- Pardridge, W.M. Brain metabolism: A perspective from the blood-brain barrier. Physiol. Rev. 1983, 63, 1481–1535. [Google Scholar] [CrossRef] [PubMed]
- Fernstrom, J.D. Aromatic amino acids and monoamine synthesis in the central nervous system: Influence of the diet. J. Nutr. Biochem. 1990, 1, 508–517. [Google Scholar] [CrossRef]
- Jenkins, T.A.; Nguyen, J.C.D.; Polglaze, K.E.; Bertrand, P.P. Influence of tryptophan and serotonin on mood and cognition with a possible role of the gut-brain axis. Nutrients 2016, 8, 56. [Google Scholar] [CrossRef]
- Snedden, W.; Mellor, C.S.; Martin, J.R. Familial hypertryptophanemia, tryptophanuria and indoleketonuria. Clin. Chim. Acta 1983, 131, 247–256. [Google Scholar] [CrossRef]
- Fernstrom, J.D.; Fernstrom, M.H. Tyrosine, phenylalanine, and catecholamine synthesis and function in the brain. J. Nutr. 2007, 137, 1539S–1547S. [Google Scholar] [CrossRef]
- Katz, I.; Lloyd, T.; Kaufman, S. Studies on phenylalanine and tyrosine hydroxylation by rat brain tyrosine hydroxylase. Biochim. Biophys. Acta 1976, 445, 567–578. [Google Scholar] [CrossRef]
- Roiser, J.P.; McLean, A.; Ogilvie, A.D.; Blackwell, A.D.; Bamber, D.J.; Goodyer, I.; Jones, P.B.; Sahakian, B.J. The subjective and cognitive effects of acute phenylalanine and tyrosine depletion in patients recovered from depression. Neuropsychopharmacology 2005, 30, 775–785. [Google Scholar] [CrossRef]
- McLean, A.; Rubinsztein, J.S.; Robbins, T.W.; Sahakian, B.J. The effects of tyrosine depletion in normal healthy volunteers: Implications for unipolar depression. Psychopharmacology 2004, 171, 286–297. [Google Scholar] [CrossRef]
- Grevet, E.H.; Tietzmann, M.R.; Shansis, F.M.; Hastenpflug, C.; Santana, L.C.; Forster, L.; Kapczinski, F.; Izquierdo, I. Behavioural effects of acute phenylalanine and tyrosine depletion in healthy male volunteers. J. Psychopharm. 2002, 16, 51–55. [Google Scholar] [CrossRef]
- Van Ginkel, W.G.; Jahja, R.; Huijbregts, S.C.J.; Daly, A.; MacDonald, A.; De Laet, C.; Cassiman, D.; Eyskens, F.; Körver-Keularts, I.M.L.W.; Goyens, P.J.; et al. Neurocognitive outcome in tyrosinemia type 1 patients compared to healthy controls. Orphanet J. Rare Dis. 2016, 11, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gassió, R.; Artuch, R.; Vilaseca, M.A.; Fusté, E.; Boix, C.; Sans, A.; Campistol, J. Cognitive functions in classic phenylketonuria and mild hyperphenyl-alaninaemia: Experience in a paediatric population. Dev. Med. Child Neurol. 2005, 47, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Haas, H.L.; Sergeeva, O.A.; Selbach, O. Histamine in the nervous system. Physiol. Rev. 2008, 88, 1183–1241. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, T.; Nakamura, T.; Shibakusa, T.; Sugita, M.; Naganuma, F.; Iida, T.; Miura, Y.; Mohsen, A.; Harada, R.; Yanai, K. Insufficient intake of L-histidine reduces brain histamine and causes anxiety-like behaviors in male mice. J. Nutr. 2014, 144, 1637–1641. [Google Scholar] [CrossRef]
- Van Ruitenbeek, P.; Sambeth, A.; Vermeeren, A.; Young, S.; Riedel, W. Effects of L-histidine depletion and L-tyrosine/L-phenylalanine depletion on sensory and motor processes in healthy volunteers. Br. J. Pharmacol. 2009, 157, 92–103. [Google Scholar] [CrossRef] [Green Version]
- Coppola, A.; Wenner, B.R.; Ilkayeva, O.; Stevens, R.D.; Maggioni, M.; Slotkin, T.A.; Levin, E.D.; Newgard, C.B. Branched-chain amino acids alter neurobehavioral function in rats. Am. J. Physiol. Endocrinol. Metabol. 2013, 304, E4051–E4130. [Google Scholar] [CrossRef] [Green Version]
- Meeusen, R.; Watson, P.; Hasegawa, H.; Roelands, B.; Piacentini, M.F. Central fatigue: The serotonin hypothesis and beyond. Sports Med. 2006, 36, 881–909. [Google Scholar] [CrossRef]
- Newsholme, E.A.; Blomstrand, E. Branched-chain amino acids and central fatigue. J. Nutr. 2006, 136, 274S–276S. [Google Scholar] [CrossRef]
- Yudkoff, M. Interactions in the metabolism of glutamate and the branched-chain amino acids and ketoacids in the CNS. Neurochem. Res. 2017, 42, 10–18. [Google Scholar] [CrossRef] [Green Version]
- LaNoue, K.F.; Berkich, D.A.; Conway, M.; Barber, A.J.; Hu, L.-Y.; Taylor, C.; Hutson, S. Role of specific aminotransferases in de novo glutamate synthesis and redox shuttling in the retina. J. Neurosci. Res. 2001, 66, 914–922. [Google Scholar] [CrossRef]
- García-Espinosa, M.A.; Wallin, R.; Hutson, S.M.; Sweatt, A.J. Widespread neuronal expression of branched-chain aminotransferase in the CNS: Implications for leucine/glutamate metabolism and for signaling by amino acids. J. Neurochem. 2007, 100, 1458–1468. [Google Scholar] [CrossRef] [PubMed]
- Contrusciere, V.; Paradisi, S.; Matteucci, A.; Malchiodi-Albedi, F. Branched-chain amino acids induce neurotoxicity in rat cortical cultures. Neurotox. Res. 2010, 17, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Caioli, S.; Candelotti, E.; Pedersen, J.Z.; Saba, L.; Antonini, A.; Incerpi, S.; Zona, C. Baicalein reverts L-valine-induced persistent sodium current up-modulation in primary cortical neurons. Biochim. Biophys. Acta 2016, 1862, 566–575. [Google Scholar] [CrossRef] [PubMed]
- Bridi, R.; Araldi, J.n.; Sgarbi, M.B.; Testa, C.G.; Durigon, K.; Wajner, M.; Dutra-Filho, C.S. Induction of oxidative stress in rat brain by the metabolites accumulating in maple syrup urine disease. Int. J. Dev. Neurosci. 2003, 21, 327–332. [Google Scholar] [CrossRef]
- Singh, S.; Sharma, M.P.; Ahmad, A. Construction and characterization of protein-based cysteine nanosensor for the real time measurement of cysteine level in living cells. Int. J. Biol. Macromol. 2020, 143, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Sharma, M.P.; Alqarawi, A.A.; Hashem, A.; Abd_Allah, E.F.; Ahmad, A. Real-time optical detection of isoleucine in living cells through a genetically-encoded nanosensor. Sensors 2020, 20, 146. [Google Scholar] [CrossRef] [Green Version]
- Mohsin, M.; Abdin, M.; Nischal, L.; Kardam, H.; Ahmad, A. Genetically encoded FRET-based nanosensor for in vivo measurement of leucine. Biosens. Bioelectron. 2013, 50, 72–77. [Google Scholar] [CrossRef]
- Ameen, S.; Ahmad, M.; Mohsin, M.; Qureshi, M.I.; Ibrahim, M.M.; Abdin, M.Z.; Ahmad, A. Designing, construction and characterization of genetically encoded FRET-based nanosensor for real time monitoring of lysine flux in living cells. J. Nanobiotechnol. 2016, 14, 49. [Google Scholar] [CrossRef] [Green Version]
- Mohsin, M.; Ahmad, A. Genetically-encoded nanosensor for quantitative monitoring of methionine in bacterial and yeast cells. Biosens. Bioelectron. 2014, 59, 358–364. [Google Scholar] [CrossRef]
- Guria, S.; Ghosh, A.; Manna, K.; Pal, A.; Adhikary, A.; Adhikari, S. Rapid detection of aspartic acid and glutamic acid in water by BODIPY-Based fluorescent probe: Live-cell imaging and DFT studies. Dyes Pigm. 2019, 168, 111–122. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, X.; Bai, X.; Li, P.; Su, D.; Zhang, W.; Zhang, W.; Tang, B. Highly Specific Cys Fluorescence Probe for Living Mouse Brain Imaging via Evading Reaction with Other Biothiols. Anal. Chem. 2019, 91, 8591–8594. [Google Scholar] [CrossRef]
- Yue, Y.; Huo, F.; Ning, P.; Zhang, Y.; Chao, J.; Meng, X.; Yin, C. Dual-Site Fluorescent Probe for Visualizing the Metabolism of Cys in Living Cells. J. Am. Chem. Soc. 2017, 139, 3181–3185. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Liu, C.; Cai, X.; Tian, B.; Zhu, H.; Chen, Y.; Sheng, W.; Jia, P.; Li, Z.; Yu, Y.; et al. A highly specific Golgi-targetable fluorescent probe for tracking cysteine generation during the Golgi stress response. Sensors Actuators B: Chem. 2020, 310, 127820. [Google Scholar] [CrossRef]
- Duan, Z.; Zhu, Y.; Yang, Y.; He, Z.; Liu, J.; Li, P.; Wang, H.; Tang, B. Fluorescent imaging for cysteine detection in vivo with high selectivity. ChemistryOpen 2019, 8, 316–320. [Google Scholar] [CrossRef] [Green Version]
- Hou, J.Q.; Cai, P.F.; Wang, C.Y.; Shen, Y.J. A novel fluorescent probe with a large stokes shift for cysteine based on dicyanoisophorone. Tetrahedron Lett. 2018, 59, 2581–2585. [Google Scholar] [CrossRef]
- Li, S.J.; Song, D.; Huang, W.J.; Li, Z.; Liu, Z.H. In situ imaging of cysteine in the brains of mice with epilepsy by a near-infrared emissive fluorescent probe. Anal. Chem. 2020, 92, 2802–2808. [Google Scholar] [CrossRef]
- Yu, Y.W.; Xu, H.P.; Zhang, W.; Han, Q.R.; Wang, B.X.; Jiang, Y.L. A novel near-infrared fluorescent probe for cysteine in living cells based on a push-pull dicyanoisophorone system. J. Photochem. Photobiol. A Chem. 2017, 346, 215–220. [Google Scholar] [CrossRef]
- Carter, K.P.; Young, A.M.; Palmer, A.E. Fluorescent sensors for measuring metal ions in living systems. Chem. Rev. 2014, 114, 4564–4601. [Google Scholar] [CrossRef]
- Domaille, D.W.; Que, E.L.; Chang, C.J. Synthetic fluorescent sensors for studying the cell biology of metals. Nat. Chem. Biol. 2008, 4, 168–175. [Google Scholar] [CrossRef]
- Snowden, T.S.; Anslyn, E.V. Anion recognition: Synthetic receptors for anions and their application in sensors. Curr. Opin. Chem. Biol. 1999, 3, 740–746. [Google Scholar] [CrossRef]
- Martínez-Máñez, R.; Sancenón, F. Fluorogenic and Chromogenic Chemosensors and Reagents for Anions. Chem. Rev. 2003, 103, 4419–4476. [Google Scholar] [CrossRef] [PubMed]
- Maity, D.; Schmuck, C. Synthetic Receptors for Amino Acids and Peptides. In Synthetic Receptors for Biomolecules: Design Principles and Applications; The Royal Society of Chemistry: Cambridge, UK, 2015; pp. 326–368. [Google Scholar] [CrossRef]
- Wu, W.; Tian, Z.; Li, A.D.Q. Fluorescent Nanoparticles for Biological Imaging. In Comprehensive Biomaterials II; Ducheyne, P., Ed.; Elsevier: Oxford, UK, 2017; pp. 535–548. [Google Scholar] [CrossRef]
- Resch-Genger, U.; Grabolle, M.; Cavaliere-Jaricot, S.; Nitschke, R.; Nann, T. Quantum dots versus organic dyes as fluorescent labels. Nat. Methods 2008, 5, 763. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.X.; Li, X.; Ma, Q.J.; Liang, B.B.; Ma, Z.Y. A highly selective and sensitive fluorescent probe for thiols based on a benzothiazole derivative. Anal. Methods 2016, 8, 6832–6839. [Google Scholar] [CrossRef]
- Chen, S.; Hou, P.; Wang, J.; Fu, S.; Liu, L. A simple but effective fluorescent probe with large stokes shift for specific detection of cysteine in living cells. J. Photochem. Photobiol. A Chem. 2018, 363, 7–12. [Google Scholar] [CrossRef]
- Yang, L.; Su, Y.; Geng, Y.; Zhang, Y.; Ren, X.; He, L.; Song, X. A Triple-Emission Fluorescent Probe for Discriminatory Detection of Cysteine/Homocysteine, Glutathione/Hydrogen Sulfide, and Thiophenol in Living Cells. ACS Sens. 2018, 3, 1863–1869. [Google Scholar] [CrossRef]
- Dong, B.; Lu, Y.; Zhang, N.; Song, W.; Lin, W. Ratiometric Imaging of Cysteine Level Changes in Endoplasmic Reticulum during H2O2-Induced Redox Imbalance. Anal. Chem. 2019, 91, 5513–5516. [Google Scholar] [CrossRef] [Green Version]
- Niu, H.; Zhang, Y.; Zhao, F.; Mo, S.; Cao, W.; Ye, Y.; Zhao, Y. Reductive stress imaging in the endoplasmic reticulum by using living cells and zebrafish. Chem. Commun. 2019, 55, 9629–9632. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, C.; Chen, Y.; Cai, X.; Sheng, W.; Zhu, H.; Jia, P.; Li, Z.; Huang, S.; Zhu, B. Visualization of the cysteine level during Golgi stress using a novel Golgi-targeting highly specific fluorescent probe. Chem. Commun. 2020, 56, 1807–1810. [Google Scholar] [CrossRef]
- Yue, Y.; Huo, F.; Yue, P.; Meng, X.; Salamanca, J.C.; Escobedo, J.O.; Strongin, R.M.; Yin, C. In Situ Lysosomal Cysteine-Specific Targeting and Imaging during Dexamethasone-Induced Apoptosis. Anal. Chem. 2018, 90, 7018–7024. [Google Scholar] [CrossRef]
- Chen, K.; Zhang, M.; Qi, Y.; Fan, J.; Ma, X.; Zhu, H.L.; Qian, Y. Imaging dynamic changes of an intracellular cysteine pool that responds to the stimulation of external oxidative stress. Analyst 2019, 144, 2320–2326. [Google Scholar] [CrossRef]
- Shen, Y.; Zhang, X.; Zhang, Y.; Zhang, C.; Jin, J.; Li, H. A new simple phthalimide-based fluorescent probe for highly selective cysteine and bioimaging for living cells. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2017, 185, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Duan, C.; Hu, Q.; Zhang, Y.; Qin, C.Q.; Zeng, L.T. A dual-channel responsive near-infrared fluorescent probe for multicolour imaging of cysteine in living cells. J. Mater. Chem. B 2017, 5, 3600–3606. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.T.; Liu, D.; Han, X.; Sheng, X.L.; Xu, Z.G.; Liu, S.H.; Zeng, L.T.; Yin, J. A hemicyanine-based colorimetric and ratiometric fluorescent probe for selective detection of cysteine and bioimaging in living cell. Talanta 2017, 170, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Fan, J.; Sun, W.; Du, J.; Peng, X. Mitochondria-Anchored Colorimetric and Ratiometric Fluorescent Chemosensor for Visualizing Cysteine/Homocysteine in Living Cells and Daphnia magna Model. Anal. Chem. 2019, 91, 12531–12537. [Google Scholar] [CrossRef]
- Wang, Q.; Wei, X.D.; Li, C.J.; Xie, Y.S. A novel p-aminophenylthio- and cyano-substituted BODIPY as a fluorescence turn-on probe for distinguishing cysteine and homocysteine from glutathione. Dyes Pigm. 2018, 148, 212–218. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, J.; Liu, J.; Ning, L.; Zhu, X.; Yu, B.; Liu, X.; Yao, X.; Zhang, H. Near-infrared and naked-eye fluorescence probe for direct and highly selective detection of cysteine and its application in living cells. Anal. Chem. 2015, 87, 4856–4863. [Google Scholar] [CrossRef]
- Zhang, H.; Yan, C.; Li, H.; Shi, L.; Wang, R.; Guo, Z.; Zhu, W.-H. Rational Design of Near-Infrared Cyanine-Based Fluorescent Probes for Rapid In Vivo Sensing Cysteine. ACS Appl. Bio Mater. 2020. [Google Scholar] [CrossRef]
- Han, C.; Yang, H.; Chen, M.; Su, Q.; Feng, W.; Li, F. Mitochondria-targeted near-infrared fluorescent off–on probe for selective detection of cysteine in living cells and in vivo. ACS Appl. Mater. Interfaces 2015, 7, 27968–27975. [Google Scholar] [CrossRef]
- Zhang, W.; Liu, J.; Yu, Y.W.; Han, Q.R.; Cheng, T.; Shen, J.; Wang, B.X.; Jiang, Y.L. A novel near-infrared fluorescent probe for highly selective detection of cysteine and its application in living cells. Talanta 2018, 185, 477–482. [Google Scholar] [CrossRef]
- Qi, Y.; Huang, Y.; Li, B.W.; Zeng, F.; Wu, S.Z. Real-time monitoring of endogenous cysteine levels in vivo by near-infrared turn-on fluorescent probe with large Stokes shift. Anal. Chem. 2018, 90, 1014–1020. [Google Scholar] [CrossRef]
- You, Q.-H.; Lee, A.W.-M.; Chan, W.-H.; Zhu, X.-M.; Leung, K.C.-F. A coumarin-based fluorescent probe for recognition of Cu2+ and fast detection of histidine in hard-to-transfect cells by a sensing ensemble approach. Chem. Commun. 2014, 50, 6207–6210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Un, H.-I.; Wu, S.; Huang, C.-B.; Xu, Z.; Xu, L. A naphthalimide-based fluorescent probe for highly selective detection of histidine in aqueous solution and its application in in vivo imaging. Chem. Commun. 2015, 51, 3143–3146. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.; Jia, H.; Gao, X.; Wang, Y.; Zhang, R.; Wang, R.; Zhang, Z. Reversible and selective fluorescence detection of histidine using a naphthalimide-based chemosensing ensemble. Chem. Asian J. 2015, 10, 2411–2418. [Google Scholar] [CrossRef] [PubMed]
- Elamathi, C.; Butcher, R.J.; Mohankumar, A.; Sundararaj, P.; Madankumar, A.; Kalaivani, P.; Prabhakaran, R. A quinoline-based probe for effective and selective sensing of aspartic acid in aqueous medium: In vitro and in vivo live cell imaging. Inorg. Chem. Front. 2019, 6, 3237–3244. [Google Scholar] [CrossRef]
- Marvin, J.S.; Borghuis, B.G.; Tian, L.; Cichon, J.; Harnett, M.T.; Akerboom, J.; Gordus, A.; Renninger, S.L.; Chen, T.-W.; Bargmann, C.I.; et al. An optimized fluorescent probe for visualizing glutamate neurotransmission. Nat. Methods 2013, 10, 162–170. [Google Scholar] [CrossRef] [Green Version]
- Marvin, J.S.; Scholl, B.; Wilson, D.E.; Podgorski, K.; Kazemipour, A.; Mueller, J.A.; Schoch, S.; Quiroz, F.J.U.; Rebola, N.; Bao, H. Stability, affinity, and chromatic variants of the glutamate sensor iGluSnFR. Nat. Methods 2018, 15, 936–939. [Google Scholar] [CrossRef]
- Wu, J.; Abdelfattah, A.S.; Zhou, H.; Ruangkittisakul, A.; Qian, Y.; Ballanyi, K.; Campbell, R.E. Genetically-encoded glutamate indicators with altered color and topology. ACS Chem. Biol. 2018. [Google Scholar] [CrossRef]
- Helassa, N.; Dürst, C.D.; Coates, C.; Kerruth, S.; Arif, U.; Schulze, C.; Wiegert, J.S.; Geeves, M.; Oertner, T.G.; Török, K. Ultrafast glutamate sensors resolve high-frequency release at Schaffer collateral synapses. Proc. Natl. Acad. Sci. USA 2018, 115, 5594–5599. [Google Scholar] [CrossRef] [Green Version]
- Coates, C.; Kerruth, S.; Helassa, N.; Török, K. Kinetic Mechanisms of Fast Glutamate Sensing by Fluorescent Protein Probes. Biophys. J. 2020, 118, 117–127. [Google Scholar] [CrossRef] [Green Version]
- Marvin, J.S.; Shimoda, Y.; Magloire, V.; Leite, M.; Kawashima, T.; Jensen, T.P.; Kolb, I.; Knott, E.L.; Novak, O.; Podgorski, K.; et al. A genetically encoded fluorescent sensor for in vivo imaging of GABA. Nat. Methods 2019. [Google Scholar] [CrossRef] [Green Version]
- Hu, H.; Gu, Y.; Xu, L.; Zou, Y.; Wang, A.; Tao, R.; Chen, X.; Zhao, Y.; Yang, Y. A genetically encoded toolkit for tracking live-cell histidine dynamics in space and time. Sci. Rep. 2017, 7, 43479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, N.; He, Y.; Su, Y.; Li, X.; Huang, Q.; Wang, H.; Zhang, X.; Tai, R.; Fan, C. The cytotoxicity of cadmium-based quantum dots. Biomaterials 2012, 33, 1238–1244. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Shi, F.; Chen, L.; Su, X. Tyrosine-functionalized CuInS 2 quantum dots as a fluorescence probe for the determination of biothiols, histidine and threonine. Analyst 2013, 138, 5819–5825. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Jiao, Y.; Gao, Y.; Qiao, J.; Mozneb, M.; Shuang, S.; Dong, C.; Li, C.-Z. Bright yellow fluorescent carbon dots as a multifunctional sensing platform for the label-free detection of fluoroquinolones and histidine. ACS Appl. Mater. Interfaces 2018, 10, 42915–42924. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Tabakman, S.; Welsher, K.; Dai, H. Carbon nanotubes in biology and medicine: In vitro and in vivo detection, imaging and drug delivery. Nano Res. 2009, 2, 85–120. [Google Scholar] [CrossRef] [Green Version]
- Kruss, S.; Hilmer, A.J.; Zhang, J.; Reuel, N.F.; Mu, B.; Strano, M.S. Carbon nanotubes as optical biomedical sensors. Adv. Drug Del. Rev. 2013, 65, 1933–1950. [Google Scholar] [CrossRef]
- Yang, N.; Chen, X.; Ren, T.; Zhang, P.; Yang, D. Carbon nanotube based biosensors. Sens. Actuators B Chem. 2015, 207, 690–715. [Google Scholar] [CrossRef]
- O’Connell, M.J.; Bachilo, S.M.; Huffman, C.B.; Moore, V.C.; Strano, M.S.; Haroz, E.H.; Rialon, K.L.; Boul, P.J.; Noon, W.H.; Kittrell, C. Band gap fluorescence from individual single-walled carbon nanotubes. Science 2002, 297, 593–596. [Google Scholar] [CrossRef] [Green Version]
- Smith, A.M.; Mancini, M.C.; Nie, S. Second window for in vivo imaging. Nat. Nanotechnol. 2009, 4, 710–711. [Google Scholar] [CrossRef] [Green Version]
- Hong, G.; Diao, S.; Chang, J.; Antaris, A.L.; Chen, C.; Zhang, B.; Zhao, S.; Atochin, D.N.; Huang, P.L.; Andreasson, K.I.; et al. Through-skull fluorescence imaging of the brain in a new near-infrared window. Nat. Photonics 2014, 8, 723–730. [Google Scholar] [CrossRef]
- Kruss, S.; Landry, M.P.; Ende, E.V.; Lima, B.M.; Reuel, N.F.; Zhang, J.; Nelson, J.; Mu, B.; Hilmer, A.; Strano, M. Neurotransmitter detection using corona phase molecular recognition on fluorescent single-walled carbon nanotube sensors. J. Am. Chem. Soc. 2014, 136, 713–724. [Google Scholar] [CrossRef] [Green Version]
- Beyene, A.G.; Alizadehmojarad, A.A.; Dorlhiac, G.; Goh, N.; Streets, A.M.; Král, P.; Vuković, L.; Landry, M.P. Ultralarge modulation of fluorescence by neuromodulators in carbon nanotubes functionalized with self-assembled oligonucleotide rings. Nano Lett. 2018, 18, 6995–7003. [Google Scholar] [CrossRef] [PubMed]
- Mann, F.A.; Herrmann, N.; Meyer, D.; Kruss, S. Tuning selectivity of fluorescent carbon nanotube-based neurotransmitter sensors. Sensors 2017, 17, 1521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Namiki, S.; Sakamoto, H.; Iinuma, S.; Iino, M.; Hirose, K. Optical glutamate sensor for spatiotemporal analysis of synaptic transmission. Eur. J. Neurosci. 2007, 25, 2249–2259. [Google Scholar] [CrossRef] [PubMed]
- Okubo, Y.; Sekiya, H.; Namiki, S.; Sakamoto, H.; Iinuma, S.; Yamasaki, M.; Watanabe, M.; Hirose, K.; Iino, M. Imaging extrasynaptic glutamate dynamics in the brain. Proc. Natl. Acad. Sci. USA 2010, 107, 6526–6531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takikawa, K.; Asanuma, D.; Namiki, S.; Sakamoto, H.; Ariyoshi, T.; Kimpara, N.; Hirose, K. High-throughput development of a hybrid-type fluorescent glutamate sensor for analysis of synaptic transmission. Angew. Chem. Int. Ed. 2014, 53, 13439–13443. [Google Scholar] [CrossRef]
- Okumoto, S.; Looger, L.L.; Micheva, K.D.; Reimer, R.J.; Smith, S.J.; Frommer, W.B. Detection of glutamate release from neurons by genetically encoded surface-displayed FRET nanosensors. Proc. Natl. Acad. Sci. USA 2005, 102, 8740–8745. [Google Scholar] [CrossRef] [Green Version]
- Zhang, W.H.; Herde, M.K.; Mitchell, J.A.; Whitfield, J.H.; Wulff, A.B.; Vongsouthi, V.; Sanchez-Romero, I.; Gulakova, P.E.; Minge, D.; Breithausen, B.; et al. Monitoring hippocampal glycine with the computationally designed optical sensor GlyFS. Nat. Chem. Biol. 2018. [Google Scholar] [CrossRef]
- Okada, S.; Ota, K.; Ito, T. Circular permutation of ligand-binding module improves dynamic range of genetically encoded FRET-based nanosensor. Protein Sci. 2009, 18, 2518–2527. [Google Scholar] [CrossRef] [Green Version]
- Steffen, V.; Otten, J.; Engelmann, S.; Radek, A.; Limberg, M.; Koenig, B.W.; Noack, S.; Wiechert, W.; Pohl, M. A toolbox of genetically encoded FRET-based biosensors for rapid l-lysine analysis. Sensors 2016, 16, 1604. [Google Scholar] [CrossRef] [Green Version]
- Gruenwald, K.; Holland, J.T.; Stromberg, V.; Ahmad, A.; Watcharakichkorn, D.; Okumoto, S. Visualization of glutamine transporter activities in living cells using genetically encoded glutamine sensors. PLoS ONE 2012, 7. [Google Scholar] [CrossRef]
- Bogner, M.; Ludewig, U. Visualization of arginine influx into plant cells using a specific FRET sensor. J. Fluoresc. 2007, 17, 350–360. [Google Scholar] [CrossRef]
- Kaper, T.; Looger, L.L.; Takanaga, H.; Platten, M.; Steinman, L.; Frommer, W.B. Nanosensor detection of an immunoregulatory tryptophan influx/kynurenine efflux cycle. PLoS Biol. 2007, 5. [Google Scholar] [CrossRef]
- Yoshida, T.; Nakajima, H.; Takahashi, S.; Kakizuka, A.; Imamura, H. OLIVe: A genetically-encoded fluorescent biosensor for quantitative imaging of branched-chain amino acid levels inside single living cells. ACS Sens. 2019, 4, 3333–3342. [Google Scholar] [CrossRef] [Green Version]
- Ko, W.; Kim, S.; Lee, S.; Jo, K.; Lee, H.S. Genetically encoded FRET sensors using a fluorescent unnatural amino acid as a FRET donor. RSC Adv. 2016, 6, 78661–78668. [Google Scholar] [CrossRef]
- Ko, W.; Lee, H.S. Development of specific l-methionine sensors by FRET-based protein engineering. RSC Adv. 2019, 9, 15648–15656. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.; Guo, C.; Li, Y.; Guo, J.; Xiao, J.; Qing, Z.; Li, J.; Yang, R. A ratiometric two-photon fluorescent cysteine probe with well-resolved dual emissions based on intramolecular charge transfer-mediated two-photon-FRET integration mechanism. ACS Sen. 2018, 3, 2415–2422. [Google Scholar] [CrossRef]
- Bai, Y.; Wu, M.X.; Ma, Q.J.; Wang, C.Y.; Sun, J.G.; Tian, M.J.; Li, J.S. A FRET-based ratiometric fluorescent probe for highly selective detection of cysteine based on a coumarin-rhodol derivative. New J. Chem. 2019, 43, 14763–14771. [Google Scholar] [CrossRef]
- Brun, M.A.; Tan, K.-T.; Griss, R.; Kielkowska, A.; Reymond, L.; Johnsson, K. A semisynthetic fluorescent sensor protein for glutamate. J. Am. Chem. Soc. 2012, 134, 7676–7678. [Google Scholar] [CrossRef]
- Masharina, A.; Reymond, L.; Maurel, D.; Umezawa, K.; Johnsson, K. A fluorescent sensor for GABA and synthetic GABAB receptor ligands. J. Am. Chem. Soc. 2012, 134, 19026–19034. [Google Scholar] [CrossRef]
- Shen, Y.; Nasu, Y.; Shkolnikov, I.; Kim, A.; Campbell, R.E. Engineering genetically encoded fluorescent indicators for imaging of neuronal activity: Progress and prospects. Neurosci. Res. 2020, 152, 3–14. [Google Scholar] [CrossRef]
- Shivange, A.V.; Borden, P.M.; Muthusamy, A.K.; Nichols, A.L.; Bera, K.; Bao, H.; Bishara, I.; Jeon, J.; Mulcahy, M.J.; Cohen, B.; et al. Determining the pharmacokinetics of nicotinic drugs in the endoplasmic reticulum using biosensors. J. Gen. Physiol. 2019, 151, 738–757. [Google Scholar] [CrossRef]

| Amino Acid | Excitatory or Inhibitory | Neurotransmitter, Neuromodulator, or Precursor | Receptor | Function |
|---|---|---|---|---|
| Glutamic acid (Glu) | Excitatory | Neurotransmitter | Ionotropic (AMPA, NMDA, and kainate) metabotropic glutamate receptors | Main excitatory neurotransmitter in CNS [9,11,12]. Can spill over for extrasynaptic activation [22,23,24]. Excesses can cause excitotoxicity [21]. |
| Aspartic acid (Asp) | Excitatory | Neuromodulator, neurotransmitter | NMDA and mGluR5 (d-asp only) [51] | l-Asp—neuromodulator (proposed neurotransmitter) [28,29]. d-Asp—neuromodulator (proposed neurotransmitter) [42,43]; involved in hormone release, neurogenesis, learning and memory [49,50]. |
| Glutamine (Gln) | N/A | Precursor | Ionotropic glutamate receptors (but requires millimolar concentrations) [65,66] | Generation of glutamate, GABA, and aspartate [10,55]. Involved in regulating ammonia homeostasis [63,64]. Unclear physiological relevance of glutamine-induced activation of ionotropic glutamate receptors. |
| Cysteine (Cys) | Excitatory | Neurotransmitter, precursor | NMDA [71,73] | Physiological relevance of NMDAR activation is unclear. Excitotoxin—unknown mechanism [73]. Precursor to glutathione, taurine, l-cysteine sulfuric acid, l-cysteic acid and hydrogen sulfide [81,82,83,84]. |
| Methionine (Met) | N/A | Precursor | N/A | Precursor to homocysteine, which is an excitatory neuromodulator that binds to NMDA receptors [94,95,96]. |
| Proline (Pro) | Excitatory | Neuromodulator | Glycine, NMDA, and AMPA/Kainate [110] | Excess leads to hyperprolinemia (seizures, hyperlocomotion, learning and other cognitive deficits) [103,104,105]. Stress response [116,117]. |
| Asparagine (Asn) | N/A | Precursor | N/A | Precursor to aspartate [36,128]. Deficiencies in synthesis leads to structural abnormalities in brain and cognitive deficits [129,130]. |
| GABA | Inhibitory (adult); excitatory (developing) | Neurotransmitter | Ionotropic (GABAA) and metabotropic (GABAB) | Major inhibitory neurotransmitter in the brain. Co-released with glycine in some synapses [170,171,172,173]. |
| Lysine (Lys) | Inhibitory | Neuromodulator, precursor | GABAA and GPRC6A [150] | Precursor for l-glutamate [138]. Modulator of GABAergic transmission [143,144,145,146]. Indirect regulation of d-serine [136]. Stress response and pain [148,149]. |
| Arginine (Arg) | N/A | Precursor | N/A | Precursor to NOx species and creatine [155,156]. Reduces stress-induced anxiety [148,161,162,163,164]. |
| Glycine (Gly) | Inhibitory | Neurotransmitter | Glycine receptors and NMDA | Main inhibitory neurotransmitter in the spinal cord [6,167,168,169]. Co-released with GABA in some synapses [170,171,172,173]. Co-agonist of (extrasynaptic) NMDA receptors [16,182]. Involved in cell migration and synaptogenesis [179]. |
| Serine (Ser) | Both | Precursor, neurotransmitter | NMDA and glycine (d-ser) | l-Ser—precursor to glycine and d-serine [56,166,190,191]; facilitate release of glutamate and aspartate [187]. d-Ser—co-agonist for glycine and NMDA receptors [16,182]; involved in Alzheimer’s disease and alcohol addiction [196,197]. |
| Alanine (Ala) | Both | Neuromodulator | Glycine and NMDA | d-Ala—weaker agonist for glycine receptors and co-agonist for NMDA receptors [6,16]. |
| Threonine (Thr) | N/A | Precursor | N/A | Precursor to glycine [212,213]. |
| β-alanine (β-Ala) | Inhibitory | Neurotransmitter, precursor | MrgprD [218], NMDA, GABAA/C, and glycine [216] | Rate-limiting precursor to carnosine. Pain modulation [219,222,225]. Histamine-independent itch mechanisms [226]. |
| Aromatic amino acids (phenylalanine (Phe), tryptophan (Trp), tyrosine (Tyr) and histidine (His)) | N/A | Precursors | N/A | Precursor to catecholamines, serotonin and histamine [229,232,239]. |
| BCAAs (isoleucine (Ile), leucine (Leu) and valine (Val)) | N/A | Precursor | N/A | Competes with aromatic amino acid transport, indirectly modulating synthesis of catecholamines, serotonin and histamine [227,242]. Precursor for glutamate [246,247]. |
| Ligand | Type | Name | Multiple Variants | Color | ∆F/Fmin or ∆R/Rmin | Response In Vitro a | Ref. |
|---|---|---|---|---|---|---|---|
| Glu | Synthetic | N,N-SP-BPY | No | Green | ∆F/Fmin | ~8.8 b,c | [256] |
| Genetically encoded (GE) | iGluSnFR | Green | ∆F/Fmin | 4.5 | [293] | ||
| iGluf andiGluu | Yes | 3.0 | [296] | ||||
| sf-iGluSnFR | Blue to green | 4.5 | [294] | ||||
| R-iGluSnFR | Green and red | 3.9 | [295] | ||||
| iGlul,m,h | Yes | Green | 2.4 | [297] | |||
| FRET (GE) | FLIPE | Yes | Cyan/yellow | ∆R/Rmin | 0.27 | [315] | |
| SuperGluSnFR | No | 0.44 | [23] | ||||
| FLIP-cpGltI210 | 0.31 | [317] | |||||
| Hybrid | EOS | No | Green | ∆F/Fmin | 0.37 | [312] | |
| EOS-K716A and EOS-L401C | Yes | 0.48 | [313] | ||||
| eEOS | No | 24 | [314] | ||||
| Fl-GluBP | No | 1.9 | [297] | ||||
| Hybrid FRET | Snifit-iGluR5 | No | Green/far red | ∆R/Rmin | 0.93 | [327] | |
| Asp | Synthetic | 8MPS | No | Green | ∆F/Fmin | ~30 c | [292] |
| N,N-SP-BPY | ~8.8 b,c | [256] | |||||
| FRET (GE) | FLIP-cpGltI210 | No | Cyan/yellow | ∆R/Rmin | 0.31 | [317] | |
| Gln | FRET (GE) | FLIP-cpGlnH183 | No | Cyan/yellow | ∆R/Rmin | 0.13 | [317] |
| FLIPQ | Yes | 0.26 | [319] | ||||
| EGFP-10-GlnBP-N138CouA | No | Blue/green | 0.89 | [323] | |||
| Cys | Synthetic | Probe 1 | Blue | ∆F/Fmin | 66 | [271] | |
| Probe 1 | Blue | ~120 c | [272] | ||||
| NCQ | Blue/green | ~4.7, 3 c | [273] | ||||
| Nap-Cys | ∆R/Rmin | 22 | [274] | ||||
| TCS | Cyan | ∆F/Fmin | 25 b | [257] | |||
| Probe 1 | Green | 130 b | [258] | ||||
| GT-Cys | ∆F/Fmin | 110 b | [259] | ||||
| NPCC | 13 | [275] | |||||
| Gol-Cys | 20 | [276] | |||||
| Ly-1 | 8.8 | [277] | |||||
| CyP | ~33 c | [278] | |||||
| Compound 1 | ~9 c | [279] | |||||
| BDY-NBD | Green/NIR | ~7400, 9.8 c,d,e | [280] | ||||
| hCy-A | Green/red | ∆R/Rmin | ~8 c | [281] | |||
| PYR | ∆R/Rmin | 163 | [282] | ||||
| XCN | Red | ∆F/Fmin | 1081 | [283] | |||
| P-Cy | 3 | [260] | |||||
| DCIP | ~5 b,c | [261] | |||||
| CyA | NIR | ~6.5 c | [284] | ||||
| Cy-S-diOMe | 250 | [285] | |||||
| NFL1 | ~20 c | [286] | |||||
| DDNA | 31 f | [287] | |||||
| CP-NIR | 40 | [288] | |||||
| Mito-CP | 12 b | [262] | |||||
| DP-NIR | 7.5 b | [263] | |||||
| QDs | T-CuInS2 QDs | No | Red | ∆F/Fmin | 0.72 | [301] | |
| FRET (GE) | Cys-FS | Yes | Cyan/yellow | ∆R/Rmin | 0.42 b | [251] | |
| FRET (Synthetic) | TP-Ratio-Cys | No | Blue/yellow | ∆R/Rmin | 36 | [325] | |
| Probe 1 | No | Blue/green | 50 | [326] | |||
| Met | FRET (GE) | FLIPM | Yes | Cyan/yellow | ∆R/Rmin | 0.42 b | [255] |
| YFP-MetQ-R189CouA | Blue/yellow | 1.7 | [324] | ||||
| GABA | GE | iGABASnFR | Yes | Green | ∆F/Fmin | 4.5 | [298] |
| Hybrid | Pf622.V278C-JF585 | No | Red | ∆F/Fmin | ~0.7 | [298] | |
| GABA-Snifit | Yes | Green/far red | ∆R/Rmin | 0.8 | [328] | ||
| Lys | FRET (GE) | ECFP-cpLAO-BP-Citrine | Yes | Cyan/yellow | ∆R/Rmin | ~0.83 | [318] |
| FLIPK | ~0.26 b,c | [254] | |||||
| Arg | FRET (GE) | QBP/Citrine/ECFP | Yes | Cyan/yellow | ∆R/Rmin | ~0.25 | [320] |
| FLIP-cpArgT194 | No | 0.54 | [317] | ||||
| cpFLIPR | 0.35 | [154] | |||||
| Gly | FRET (GE) | GlyFS | No | Cyan/yellow | ∆R/Rmin | 0.28 | [316] |
| Thr | QDs | T-CuInS2 QDs | No | Red | ∆F/Fmin | 0.37 | [301] |
| Trp | FRET (GE) | FLIPW-CTYT | No | Cyan/yellow | ∆R/Rmin | 0.35 | [321] |
| His | Synthetic | CAQA | No | Blue | ∆F/Fmin | ~18 c | [289] |
| NPC | Green | ∆F/Fmin | 6 | [290] | |||
| NCH-Cu2+ | Green | 10 c | [291] | ||||
| GE | FHisJ | Yes | Yellow | ∆F/Fmin | 5.2 | [299] | |
| QDs | T-CuInS2 QDs | No | Red | ∆F/Fmin | 0.46 | [301] | |
| Y-CDs | Yellow | 4.5 | [302] | ||||
| FRET | FLIP-cpHisJ194 | No | Cyan/yellow | ∆R/Rmin | 0.63 | [317] | |
| Ile | FRET | FLIP-cpLivJ261 | Yes | Cyan/yellow | ∆R/Rmin | 0.25 | [317] |
| GEII | Yes | 0.44 b | [252] | ||||
| OLIVe | No | 1.05 | [322] | ||||
| Leu | FRET | FLIP-cpLivJ261 | Yes | Cyan/yellow | ∆R/Rmin | 0.25 | [317] |
| FLIP-Leu | ~0.7 b | [253] | |||||
| OLIVe | No | 1.05 | [322] | ||||
| Val | FRET | FLIP-cpLivJ261 | No | Cyan/yellow | ∆R/Rmin | 0.25 | [317] |
| OLIVe | ~0.9 | [322] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dalangin, R.; Kim, A.; Campbell, R.E. The Role of Amino Acids in Neurotransmission and Fluorescent Tools for Their Detection. Int. J. Mol. Sci. 2020, 21, 6197. https://doi.org/10.3390/ijms21176197
Dalangin R, Kim A, Campbell RE. The Role of Amino Acids in Neurotransmission and Fluorescent Tools for Their Detection. International Journal of Molecular Sciences. 2020; 21(17):6197. https://doi.org/10.3390/ijms21176197
Chicago/Turabian StyleDalangin, Rochelin, Anna Kim, and Robert E. Campbell. 2020. "The Role of Amino Acids in Neurotransmission and Fluorescent Tools for Their Detection" International Journal of Molecular Sciences 21, no. 17: 6197. https://doi.org/10.3390/ijms21176197
APA StyleDalangin, R., Kim, A., & Campbell, R. E. (2020). The Role of Amino Acids in Neurotransmission and Fluorescent Tools for Their Detection. International Journal of Molecular Sciences, 21(17), 6197. https://doi.org/10.3390/ijms21176197





