Sappanone A Prevents Left Ventricular Dysfunction in a Rat Myocardial Ischemia Reperfusion Injury Model
Abstract
:1. Introduction
2. Results
2.1. Experimental Design, Gross Examination, Myocardial Infarct Size, and Serum Cardiac Marker Results
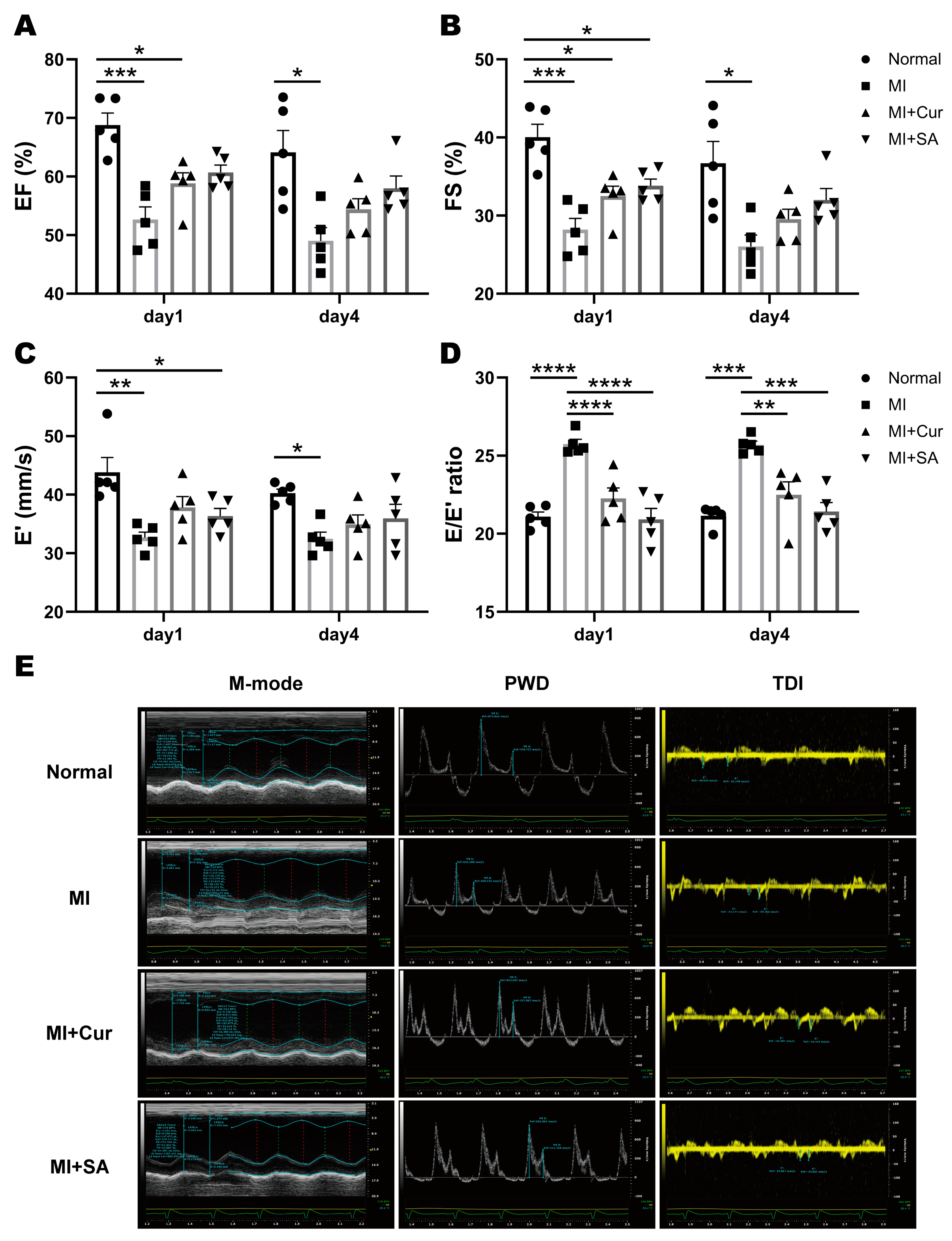
2.2. Echocardiographic Results
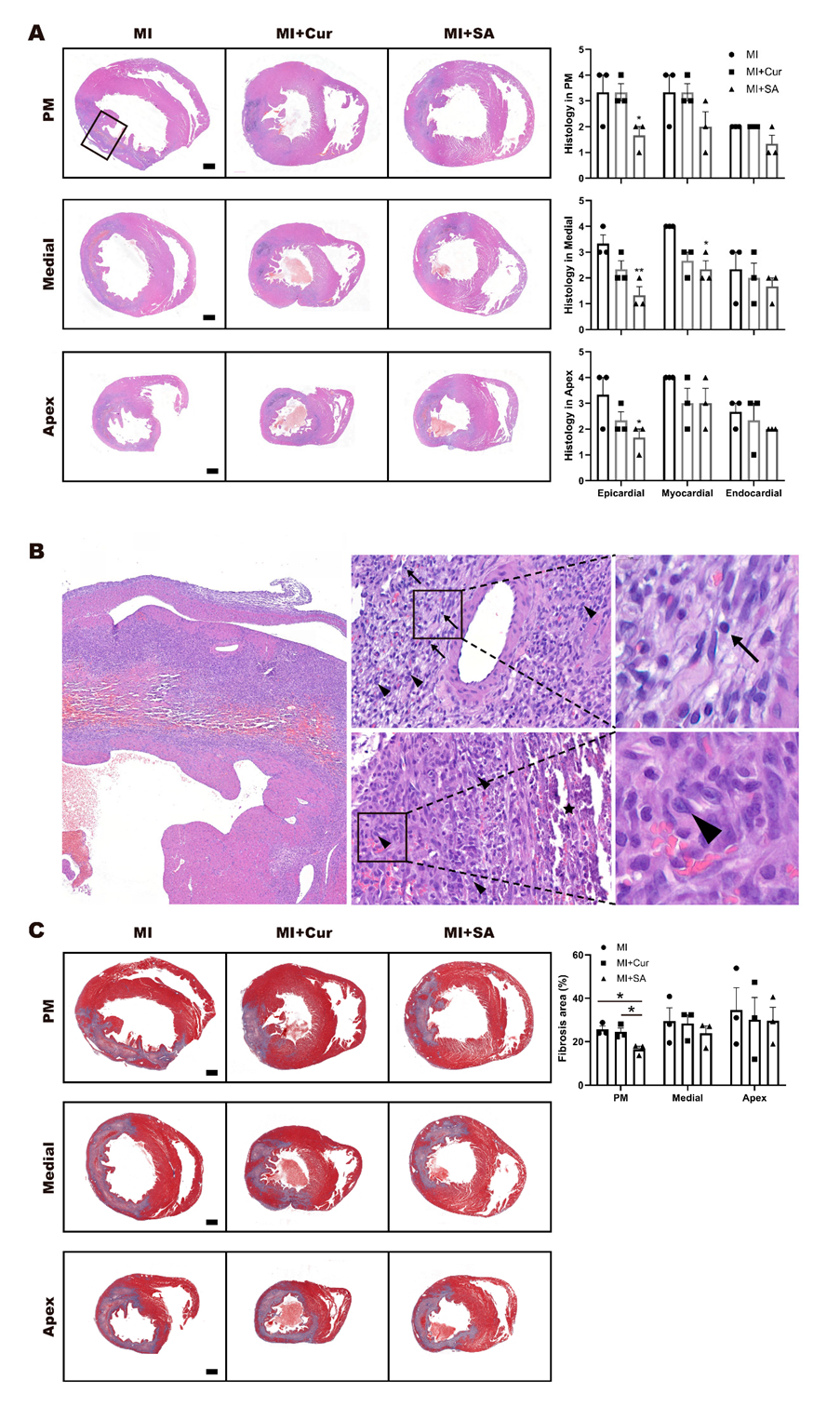
2.3. Histopathological Results
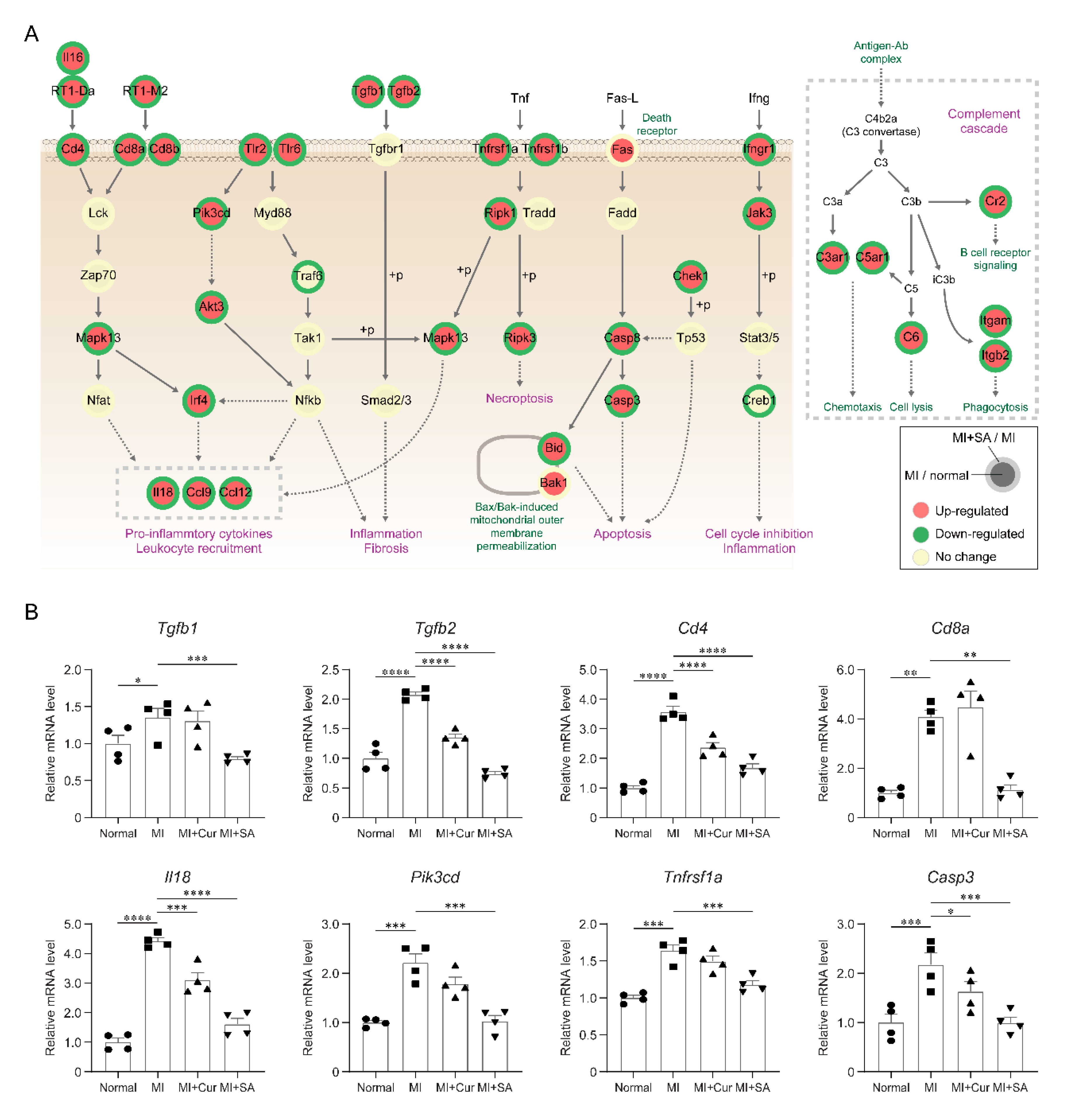
2.4. Sappanone A Treatment Results in Changes of Multiple Cellular Processes in the Rat Myocardial I/R Injury Model
2.5. Inhibitory Effects of Sappanone A on Myocardial Infarction-Related Processes
3. Discussion
4. Materials and Methods
4.1. Chemicals and Reagents
4.2. Animals, Husbandry, and Experimental Design
4.3. Induction of Myocardial I/R Injury
4.4. Echocardiographic Analysis
4.5. Myocardial Infarct Size
4.6. Serum Chemistry of CK-MB, LDH, and AST
4.7. Histopathological Analysis
4.8. mRNA Sequencing and Data Analysis
4.9. Identification of Differentially Expressed Genes (DEGs)
4.10. RT-PCR
4.11. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| LAD | left anterior descending |
| LV | left ventricular |
| MI | myocardial infarction |
| EF | ejection fraction |
| FS | fractional shortening |
| PWD | pulse wave doppler |
| TDI | tissue doppler imaging. |
| SV | stroke volume |
| CO | cardiac output |
| LVIDd | left ventricular internal diameter at diastole |
| LVIDs | left ventricular internal diameter at systole |
| IVSd | interventricular septal thickness at diastole |
| IVSs | interventricular septal thickness at systole |
| LVPWd | left ventricular posterior wall thickness at diastole |
| LVPWs | left ventricular posterior wall thickness at systole |
| DEG | differentially expressed gene |
| GOBP | gene ontology biological process |
References
- Jayaraj, J.C.; Davatyan, K.; Subramanian, S.S.; Priya, J. Epidemiology of myocardial infarction. In Myocardial Infarction; Pamukçu, B., Ed.; IntechOpen: London, UK, 2018. [Google Scholar]
- Mor-Avi, V.; Lang, R.M.; Badano, L.P.; Belohlavek, M.; Cardim, N.M.; Derumeaux, G.; Galderisi, M.; Marwick, T.; Nagueh, S.F.; Sengupta, P.P.; et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. Eur. J. Echocardiogr. 2011, 12, 167–205. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Marwick, T.H.; Cook, S.A.; Go, R.T.; Fix, J.S.; James, K.B.; Sapp, S.K.; MacIntyre, W.J.; Thomas, J.D. Prognosis of patients with left ventricular dysfunction, with and without viable myocardium after myocardial infarction. Relative efficacy of medical therapy and revascularization. Circulation 1994, 90, 2687–2694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanders, D.; Dudley, M.; Groban, L. Diastolic dysfunction, cardiovascular aging, and the anesthesiologist. Anesthesiol. Clin. 2009, 27, 497–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moller, J.E.; Pellikka, P.A.; Hillis, G.S.; Oh, J.K. Prognostic importance of diastolic function and filling pressure in patients with acute myocardial infarction. Circulation 2006, 114, 438–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, X.R.; Xu, H.J.; Wang, L.F.; Liu, C.B.; Yu, F. Mesenchymal stem cell transplantation carried in SVVYGLR modified self-assembling peptide promoted cardiac repair and angiogenesis after myocardial infarction. Biochem. Biophys. Res. Commun. 2017, 491, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Dai, Y.; Yan, S.; Shi, Y.; Han, B.; Li, J.; Cha, L.; Mu, J. Down-regulation of lncRNA KCNQ1OT1 protects against myocardial ischemia/reperfusion injury following acute myocardial infarction. Biochem. Biophys. Res. Commun. 2017, 491, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.P.; Wang, Z.F.; Tootle, S.; Philip, T.; Zhao, Z.Q. Curcumin promotes cardiac repair and ameliorates cardiac dysfunction following myocardial infarction. Br. J. Pharmacol. 2012, 167, 1550–1562. [Google Scholar] [CrossRef] [Green Version]
- Cootney, R.W. Ultrasound imaging: Principles and applications in rodent research. ILAR J. 2001, 42, 233–247. [Google Scholar] [CrossRef] [Green Version]
- Holinski, S.; Knebel, F.; Heinze, G.; Konertz, W.; Baumann, G.; Borges, A.C. Noninvasive monitoring of cardiac function in a chronic ischemic heart failure model in the rat: Assessment with tissue Doppler and non-Doppler 2D strain echocardiography. Cardiovasc. Ultrasound 2011, 9, 15. [Google Scholar] [CrossRef] [Green Version]
- Jo, W.; Lee, H.Y.; Kim, S.J.; Son, W.C.; Song, S.; Kim, H. Sustained left ventricular diastolic dysfunction following ischemia reperfusion injury in an acute myocardial infarction rat model. Jpn. J. Vet. Res. 2018, 66, 281–288. [Google Scholar]
- Jo, W.; Kang, K.K.; Chae, S.; Son, W.C. Metformin Alleviates Left Ventricular Diastolic Dysfunction in a Rat Myocardial Ischemia Reperfusion Injury Model. Int. J. Mol. Sci. 2020, 21, 1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cuong, T.D.; Hung, T.M.; Kim, J.C.; Kim, E.H.; Woo, M.H.; Choi, J.S.; Lee, J.H.; Min, B.S. Phenolic Compounds from Caesalpinia sappan Heartwood and Their Anti-inflammatory Activity. J. Nat. Prod. 2012, 75, 2069–2075. [Google Scholar] [CrossRef]
- Lee, S.; Choi, S.Y.; Choo, Y.Y.; Kim, O.; Tran, P.T.; Dao, C.T.; Min, B.S.; Lee, J.H. Sappanone A exhibits anti-inflammatory effects via modulation of Nrf2 and NF-kappaB. Int. Immunopharmacol. 2015, 28, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Choo, Y.Y.; Tran, P.T.; Min, B.S.; Kim, O.; Nguyen, H.D.; Kwon, S.H.; Lee, J.H. Sappanone A inhibits RANKL-induced osteoclastogenesis in BMMs and prevents inflammation-mediated bone loss. Int. Immunopharmacol. 2017, 52, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Aldous, S.J. Cardiac biomarkers in acute myocardial infarction. Int. J. Cardiol. 2013, 164, 282–294. [Google Scholar] [CrossRef] [PubMed]
- da Huang, W.; Sherman, B.T.; Lempicki, R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009, 4, 44–57. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Simoons, M.L.; Chaitman, B.R.; White, H.D. Task Force for the Universal Definition of Myocardial Infarction, Third universal definition of myocardial infarction. Nat. Rev. Cardiol. 2012, 9, 620–633. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Zhang, C.; Khanna, A. Wideband high-frequency echocardiography to evaluate myocardial infarct size. J. Ultrasound Med. 2009, 28, 1527–1534. [Google Scholar] [CrossRef] [Green Version]
- Feigenbaum, H. Journal of the American Society of Echocardiography: 25 Years Old. J. Am. Soc. Echocardiogr. 2012, 25, 1–2. [Google Scholar] [CrossRef]
- Cerisano, G.; Bolognese, L.; Carrabba, N.; Buonamici, P.; Santoro, G.M.; Antoniucci, D.; Santini, A.; Moschi, G.; Fazzini, P.F. Doppler-derived mitral deceleration time: An early strong predictor of left ventricular remodeling after reperfused anterior acute myocardial infarction. Circulation 1999, 99, 230–236. [Google Scholar] [CrossRef] [Green Version]
- Nagueh, S.F.; Lakkis, N.M.; Middleton, K.J.; Spencer, W.H., 3rd; Zoghbi, W.A.; Quinones, M.A. Doppler estimation of left ventricular filling pressures in patients with hypertrophic cardiomyopathy. Circulation 1999, 99, 254–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagueh, S.F.; Mikati, I.; Kopelen, H.A.; Middleton, K.J.; Quinones, M.A.; Zoghbi, W.A. Doppler estimation of left ventricular filling pressure in sinus tachycardia. A new application of tissue doppler imaging. Circulation 1998, 98, 1644–1650. [Google Scholar] [CrossRef] [PubMed]
- Kessler, E.L.; Rivaud, M.R.; Vos, M.A.; van Veen, T.A.B. Sex-specific influence on cardiac structural remodeling and therapy in cardiovascular disease. Biol. Sex Differ. 2019, 10, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, H.J.; Wang, C.H.; Qiao, Z.Y.; Xu, Y.W. Protective effect of curcumin against myocardium injury in ischemia reperfusion rats. Pharm. Biol. 2017, 55, 1144–1148. [Google Scholar] [CrossRef]
- Boarescu, P.M.; Boarescu, I.; Bocsan, I.C.; Pop, R.M.; Gheban, D.; Bulboaca, A.E.; Nicula, C.; Rajnoveanu, R.M.; Bolboaca, S.D. Curcumin Nanoparticles Protect against Isoproterenol Induced Myocardial Infarction by Alleviating Myocardial Tissue Oxidative Stress, Electrocardiogram, and Biological Changes. Molecules 2019, 24, 2802. [Google Scholar] [CrossRef] [Green Version]
- Chang, J.; Nair, V.; Luk, A.; Butany, J. Pathology of myocardial infarction. Diagn. Histopathol. 2013, 19, 7–12. [Google Scholar] [CrossRef]
- Gorcsan, J., 3rd; Tanaka, H. Echocardiographic assessment of myocardial strain. J. Am. Coll. Cardiol. 2011, 58, 1401–1413. [Google Scholar] [CrossRef] [Green Version]
- Bujak, M.; Frangogiannis, N.G. The role of TGF-beta signaling in myocardial infarction and cardiac remodeling. Cardiovasc. Res. 2007, 74, 184–195. [Google Scholar] [CrossRef] [Green Version]
- Christia, P.; Frangogiannis, N.G. Targeting inflammatory pathways in myocardial infarction. Eur. J. Clin. Investig. 2013, 43, 986–995. [Google Scholar] [CrossRef]
- Ong, S.B.; Hernandez-Resendiz, S.; Crespo-Avilan, G.E.; Mukhametshina, R.T.; Kwek, X.Y.; Cabrera-Fuentes, H.A.; Hausenloy, D.J. Inflammation following acute myocardial infarction: Multiple players, dynamic roles, and novel therapeutic opportunities. Pharmacol. Ther. 2018, 186, 73–87. [Google Scholar] [CrossRef]
- Krishnamurthy, P.; Rajasingh, J.; Lambers, E.; Qin, G.; Losordo, D.W.; Kishore, R. IL-10 inhibits inflammation and attenuates left ventricular remodeling after myocardial infarction via activation of STAT3 and suppression of HuR. Circ. Res. 2009, 104, e9–e18. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wang, H.; Li, J. Inflammation and Inflammatory Cells in Myocardial Infarction and Reperfusion Injury: A Double-Edged Sword. Clin. Med. Insights Cardiol. 2016, 10, 79–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prabhu, S.D.; Frangogiannis, N.G. The Biological Basis for Cardiac Repair After Myocardial Infarction: From Inflammation to Fibrosis. Circ. Res. 2016, 119, 91–112. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Guo, Z.; Ding, Z.; Mehta, J.L. Inflammation, Autophagy, and Apoptosis After Myocardial Infarction. J. Am. Heart Assoc. 2018, 7, e008024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trapnell, C.; Pachter, L.; Salzberg, S.L. TopHat: Discovering splice junctions with RNA-Seq. Bioinformatics 2009, 25, 1105–1111. [Google Scholar] [CrossRef]
- Anders, S.; Pyl, P.T.; Huber, W. HTSeq--a Python framework to work with high-throughput sequencing data. Bioinformatics 2015, 31, 166–169. [Google Scholar] [CrossRef]
- Robinson, M.D.; Oshlack, A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 2010, 11, R25. [Google Scholar] [CrossRef] [Green Version]
- Chae, S.; Ahn, B.Y.; Byun, K.; Cho, Y.M.; Yu, M.H.; Lee, B.; Hwang, D.; Park, K.S. A systems approach for decoding mitochondrial retrograde signaling pathways. Sci. Signal 2013, 6, rs4. [Google Scholar] [CrossRef]
- Cline, M.S.; Smoot, M.; Cerami, E.; Kuchinsky, A.; Landys, N.; Workman, C.; Christmas, R.; Avila-Campilo, I.; Creech, M.; Gross, B.; et al. Integration of biological networks and gene expression data using Cytoscape. Nat. Protoc. 2007, 2, 2366–2382. [Google Scholar] [CrossRef] [Green Version]
- Kanehisa, M.; Goto, S.; Sato, Y.; Furumichi, M.; Tanabe, M. KEGG for integration and interpretation of large-scale molecular data sets. Nucleic Acids Res. 2012, 40, D109–D114. [Google Scholar] [CrossRef] [Green Version]


| MI Area Region | MI | MI + Cur | MI + SA |
|---|---|---|---|
| Papillary muscle (PM) | 20.52 ± 11.54 | 25.68 ± 7.45 | 11.53 ± 8.35 |
| Proximal medial | 21.52 ± 2.63 | 23.19 ± 2.38 | 10.19 ± 6.31 |
| Distal medial | 33.09 ± 4.83 | 24.55 ± 3.12 | # 9.64 ± 6.22 |
| Apex | 51.46 ± 9.33 | # 25.01 ± 10.50 | ### 12.39 ± 7.64 |
| Total | 31.65 ± 2.37 | 24.61 ± 2.53 | ## 10.94 ± 5.95 |
| Cardiac Function | Day 1 | Day 4 | ||||||
|---|---|---|---|---|---|---|---|---|
| Normal | MI | MI+Cur | MI+SA | Normal | MI | MI+Cur | MI+SA | |
| EF, % | 68.79 ± 4.59 | *** 52.63 ± 4.85 | * 58.81 ± 4.12 | 60.68 ± 2.82 | 64.13 ± 8.30 | * 49.01 ± 5.06 | 54.39 ± 4.07 | 57.97 ± 4.70 |
| FS, % | 40.05 ± 3.66 | *** 28.21 ± 3.18 | * 32.48 ± 2.85 | * 33.80 ± 1.98 | 36.69 ± 6.24 | * 26.03 ± 3.28 | 29.55 ± 2.80 | 31.99 ± 3.30 |
| HR, BPM | 256.16 ± 21.28 | 302.19 ± 48.56 | 303.10 ± 20.50 | 259.16 ± 49.83 | 244.41 ± 30.13 | 263.63 ± 15.35 | 256.91 ± 38.13 | 244.75 ± 11.91 |
| SV, µL | 219.43 ± 27.86 | 182.83 ± 10.82 | 210.01 ± 23.71 | 216.28 ± 21.84 | 233.88 ± 23.15 | 206.55 ± 22.86 | 224.25 ± 28.84 | 228.74 ± 38.15 |
| CO, mL/min | 55.97 ± 6.27 | 54.97 ± 6.07 | 63.39 ± 8.80 | 62.82 ± 11.05 | 56.93 ± 7.21 | 54.23 ± 5.61 | 56.93 ± 2.95 | 55.90 ± 9.42 |
| LVIDd, mm | 7.73 ± 0.53 | 7.90 ± 0.27 | 7.96 ± 0.46 | 8.15 ± 0.52 | 8.18 ± 0.75 | 8.73 ± 0.15 | 8.63 ± 0.26 | 8.49 ± 0.71 |
| LVIDs, mm | 4.66 ± 0.53 | * 5.66 ± 0.41 | 5.37 ± 0.41 | 5.43 ± 0.52 | 5.19 ± 0.89 | 6.36 ± 0.41 | 6.13 ± 0.20 | 5.88 ± 0.73 |
| IVSd, mm | 1.52 ± 0.05 | 1.53 ± 0.16 | 1.59 ± 0.16 | 1.54 ± 0.23 | 1.48 ± 0.20 | 1.36 ± 0.07 | 1.40 ± 0.16 | 1.41 ± 0.10 |
| IVSs, mm | 2.57 ± 0.11 | 2.24 ± 0.20 | 2.55 ± 0.22 | 2.65 ± 0.27 | 2.52 ± 0.24 | 2.19 ± 0.20 | 2.22 ± 0.21 | 2.34 ± 0.23 |
| LVPWd, mm | 1.66 ± 0.15 | 1.57 ± 0.12 | 1.70 ± 0.09 | 1.98 ± 0.55 | 1.57 ± 0.17 | 1.62 ± 0.27 | 1.57 ± 0.16 | 1.66 ± 0.12 |
| LVPWs, mm | 2.65 ± 0.23 | 2.36 ± 0.28 | 2.53 ± 0.07 | 2.69 ± 0.37 | 2.42 ± 0.26 | 2.28 ± 0.26 | 2.38 ± 0.24 | 2.58 ± 0.23 |
| E′, mm/s | 43.82 ± 5.66 | ** 32.67 ± 2.14 | * 37.82 ± 4.16 | 36.33 ± 2.95 | 40.23 ± 1.62 | * 32.44 ± 2.62 | 34.93 ± 3.63 | 35.94 ± 5.40 |
| E/A ratio | 1.66 ± 0.32 | 2.10 ± 0.40 | 1.91 ± 0.37 | 1.75 ± 0.34 | 1.82 ± 0.28 | 1.95 ± 0.17 | 2.04 ± 0.50 | 2.16 ± 0.64 |
| E/E′ ratio | 21.09 ± 0.68 | **** 25.74 ± 0.68 | **** 22.26 ± 1.50 | **** 20.92 ± 1.58 | 21.14 ± 0.68 | *** 25.69 ± 0.54 | ** 22.50 ± 1.83 | *** 21.42 ± 1.29 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, W.; Min, B.S.; Yang, H.-Y.; Park, N.-H.; Kang, K.-K.; Lee, S.; Chae, S.; Ma, E.S.; Son, W.-C. Sappanone A Prevents Left Ventricular Dysfunction in a Rat Myocardial Ischemia Reperfusion Injury Model. Int. J. Mol. Sci. 2020, 21, 6935. https://doi.org/10.3390/ijms21186935
Jo W, Min BS, Yang H-Y, Park N-H, Kang K-K, Lee S, Chae S, Ma ES, Son W-C. Sappanone A Prevents Left Ventricular Dysfunction in a Rat Myocardial Ischemia Reperfusion Injury Model. International Journal of Molecular Sciences. 2020; 21(18):6935. https://doi.org/10.3390/ijms21186935
Chicago/Turabian StyleJo, Woori, Byung Sun Min, Hee-Young Yang, Na-Hye Park, Kyung-Ku Kang, Sijoon Lee, Sehyun Chae, Eun Sook Ma, and Woo-Chan Son. 2020. "Sappanone A Prevents Left Ventricular Dysfunction in a Rat Myocardial Ischemia Reperfusion Injury Model" International Journal of Molecular Sciences 21, no. 18: 6935. https://doi.org/10.3390/ijms21186935
APA StyleJo, W., Min, B. S., Yang, H.-Y., Park, N.-H., Kang, K.-K., Lee, S., Chae, S., Ma, E. S., & Son, W.-C. (2020). Sappanone A Prevents Left Ventricular Dysfunction in a Rat Myocardial Ischemia Reperfusion Injury Model. International Journal of Molecular Sciences, 21(18), 6935. https://doi.org/10.3390/ijms21186935




