Imaging Diagnostics and Pathology in SARS-CoV-2-Related Diseases
Abstract
:1. SARS-CoV-2 Pandemic
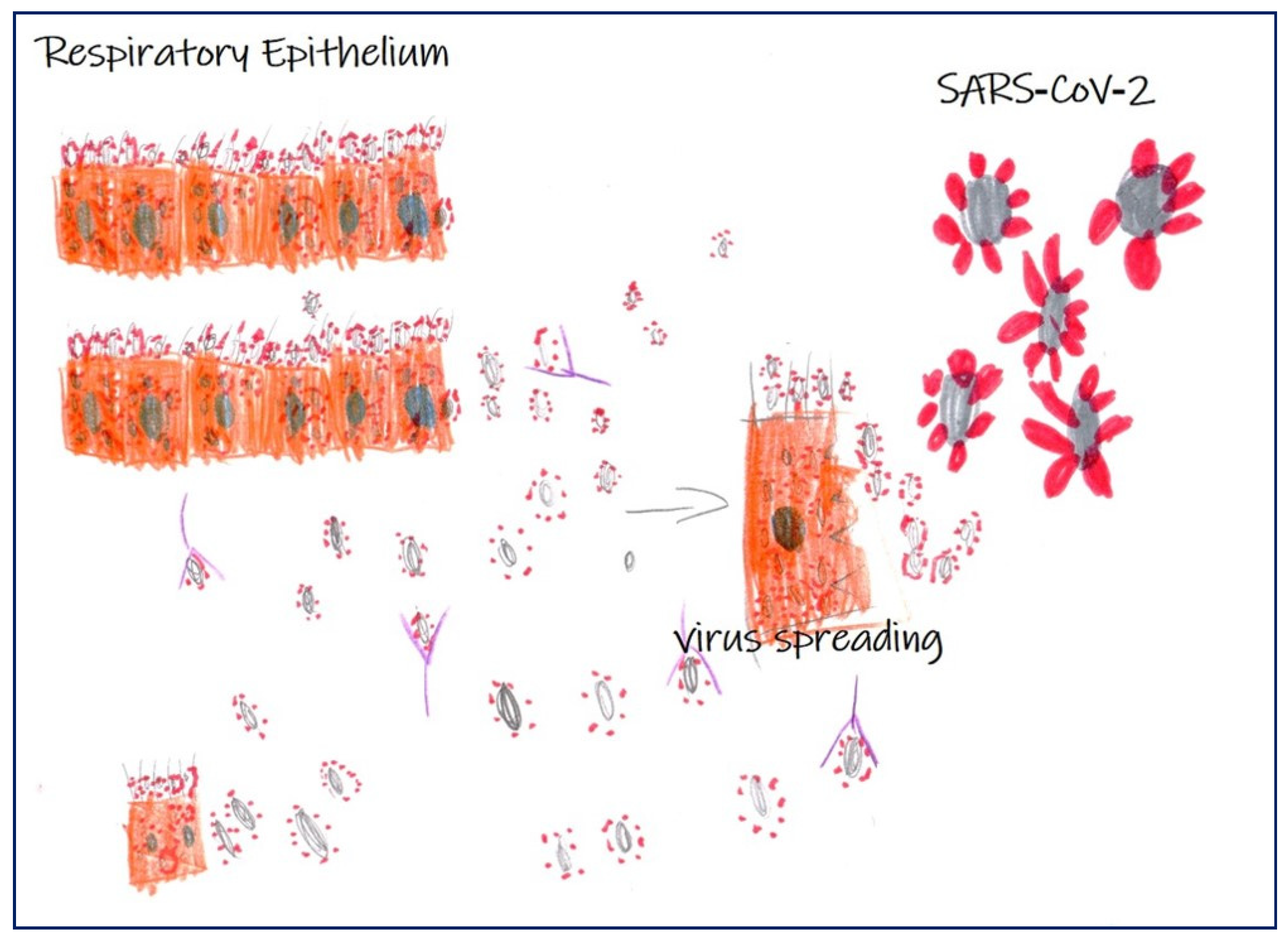
2. From Pathology to Imaging Diagnostic
3. Histological Characteristics of SARS-CoV-2 Infection
4. Lung Pathology
5. Heart Pathology
6. Renal Pathology
7. Skin Pathology
8. Central Nervous System
9. Other Organs
10. Radiological Aspects of SARS-CoV-2-Related Diseases
11. The Role of Nuclear Medicine in SARS-CoV-2-Related Diseases
12. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Yan, F.; Gao, Y.; Pang, X.; Xu, X.; Zhu, N.; Chan, H.; Hu, G.; Wu, M.; Yuan, Y.; Li, H.; et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. J. Exp. Bot. 2020, 63, 457–460. [Google Scholar] [CrossRef] [Green Version]
- Park, S.E. Epidemiology, virology, and clinical features of severe acute respiratory syndrome -coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin. Exp. Pediatr. 2020, 63, 119–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, M.Y.; Li, L.; Zhang, Y.; Wang, X.S. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect. Dis Poverty 2020, 9, 45. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.Y.; Xu, X.X.; Yin, H.S.; Hu, Q.M.; Xiong, T.; Tang, Y.Y.; Yang, A.Y.; Yu, B.P.; Huang, Z.P. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: A retrospective study. BMC Infect. Dis. 2020, 20, 311. [Google Scholar] [CrossRef] [PubMed]
- Bustin, S.A.; Nolan, T. RT-qPCR Testing of SARS-CoV-2: A Primer. Int. J. Mol. Sci. 2020, 21, 3004. [Google Scholar] [CrossRef]
- Xu, X.; Yu, C.; Qu, J.; Zhang, L.; Jiang, S.; Huang, D.; Chen, B.; Zhang, Z.; Guan, W.; Ling, Z.; et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1275–1280. [Google Scholar] [CrossRef] [Green Version]
- Ciotti, M.; Angeletti, S.; Minieri, M.; Giovannetti, M.; Benvenuto, D.; Pascarella, S.; Sagnelli, C.; Bianchi, M.; Bernardini, S.; Ciccozzi, M. SARS-COV-2 Outbreak: An Overview. Chemotherapy 2019, 64, 215–223. [Google Scholar] [CrossRef]
- Urbano, N.; Scimeca, M.; Bonanno, E.; Schillaci, O. Nuclear medicine and anatomic pathology in personalized medicine: A challenging alliance. Pers. Med. 2018, 15, 457–459. [Google Scholar] [CrossRef]
- Scimeca, M.; Urbano, N.; Bonfiglio, R.; Schillaci, O.; Bonanno, E. Management of oncological patients in the digital era: Anatomic pathology and nuclear medicine teamwork. Future Oncol. 2018, 14, 1013–1015. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with SARS-COV-2 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Shi, Y.; Wang, Y.; Shao, C.; Huang, J.; Gan, J.; Huang, X.; Bucci, E.; Piacentini, M.; Ippolito, G.; Melino, G. SARS-COV-2 infection: The perspectives on immune responses. Cell Death Differ. 2020, 27, 1451–1454. [Google Scholar] [CrossRef] [Green Version]
- Bosmuller, H.; Traxler, S.; Bitzer, M.; Häberle, H.; Raiser, W.; Nann, D.; Frauenfeld, L.; Vogelsberg, A.; Klingel, K.; Fend, F. The evolution of pulmonary pathology in fatal SARS-COV-2 disease: An autopsy study with clinical correlation. Virchows Arch. 2020, 477, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in SARS-CoV-2. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in SARS-COV-2. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Yan, R.; Zhang, Y.; Li, Y.; Xia, L.; Guo, Y.; Zhou, Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 2020, 367, 1444–1448. [Google Scholar] [CrossRef] [Green Version]
- Magro, C.; Mulvey, J.J.; Berlin, D.; Nuovo, G.; Salvatore, S.; Harp, J.; Baxter-Stoltzfus, A.; Laurence, J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe SARS-COV-2 infection: A report of five cases. Transl. Res. 2020, 220, 1–13. [Google Scholar] [CrossRef]
- Lax, S.F.; Skok, K.; Zechner, P.; Kessler, H.H.; Kaufmann, N.; Koelblinger, C.; Vander, K.; Bargfrieder, U.; Trauner, M. Pulmonary Arterial Thrombosis in SARS-COV-2 with Fatal Outcome: Results from a Prospective, Single-Center, Clinicopathologic Case Series. Ann. Intern. Med. 2020, 173, 350–361. [Google Scholar] [CrossRef]
- Wichmann, D.; Sperhake, J.-P.; Lütgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Heinrich, F.; Mushumba, H.; Kniep, I.; Schröder, A.S.; et al. Autopsy Findings and Venous Thromboembolism in Patients With SARS-COV-2. Ann. Intern. Med. 2020, 173, 350–361. [Google Scholar] [CrossRef]
- Giannis, D.; Ziogas, I.A.; Gianni, P. Coagulation disorders in coronavirus infected patients: SARS-COV-2, SARS-CoV-1, MERS-CoV and lessons from the past. J. Clin. Virol. 2020, 127, 104362. [Google Scholar] [CrossRef]
- Ishiguro, T.; Kobayashi, Y.; Uozumi, R.; Takata, N.; Takaku, Y.; Kagiyama, N.; Kanauchi, T.; Shimizu, Y.; Takayanagi, N. Viral Pneumonia Requiring Differentiation from Acute and Progressive Diffuse Interstitial Lung Diseases. Intern. Med. 2019, 58, 3509–3519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konopka, K.E.; Nguyen, T.; Jentzen, J.M.; Rayes, O.; Schmidt, C.J.; Wilson, A.M.; Farver, C.F.; Myers, J.L. Diffuse Alveolar Damage (DAD) from Coronavirus Disease 2019 Infection is Morphologically Indistinguishable from Other Causes of DAD. Histopathology 2020, 77, 570–578. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients with SARS-COV-2 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [Green Version]
- Sala, S.; Peretto, G.; Gramegna, M.; Palmisano, A.; Villatore, A.; Vignale, D.; De Cobelli, F.; Tresoldi, M.; Cappelletti, A.M.; Basso, C.; et al. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV-2 respiratory infection. Eur. Heart J. 2020, 41, 1861–1862. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhou, Y.; Wang, D.W. SARS-CoV-2: A potential novel etiology of fulminant myocarditis. Herz 2020, 45, 230–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, L.; Mir, M.; Sanchez, P.; Beg, M.; Peters, J.; Enriquez, O.; Gilbert, A. Autopsy Report with Clinical Pathological Correlation. Arch. Pathol. Lab. Med. 2020. [Google Scholar] [CrossRef]
- Tavazzi, G.; Pellegrini, C.; Maurelli, M.; Belliato, M.; Sciutti, F.; Bottazzi, A.; Sepe, P.A.; Resasco, T.; Camporotondo, R.; Bruno, R.; et al. Myocardial localization of coronavirus in SARS-COV-2 cardiogenic shock. Eur. J. Heart Fail 2020, 22, 911–915. [Google Scholar] [CrossRef] [Green Version]
- Craver, R.; Huber, S.; Sandomirsky, M.; McKenna, D.; Schieffelin, J.; Finger, L. Fatal Eosinophilic Myocarditis in a Healthy 17-Year-Old Male with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2c). Fetal Pediatr. Pathol. 2020, 39, 263–268. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Farkash, E.A.; Wilson, A.M.; Jentzen, J.M. Ultrastructural Evidence for Direct Renal Infection with SARS-CoV-2. J. Am. Soc. Nephrol. 2020, 31, 1683–1687. [Google Scholar] [CrossRef] [PubMed]
- Gianotti, R.; Recalcati, S.; Fantini, F.; Riva, C.; Milani, M.; Dainese, E.; Boggio, F. Histopathological Study of a Broad Spectrum of Skin Dermatoses in Patients Affected or Highly Suspected of Infection by SARS-COV-2 in the Northern Part of Italy: Analysis of the Many Faces of the Viral-Induced Skin Diseases in Previous and New Reported Cases. Am. J. Dermatopathol. 2020, 42, 564–570. [Google Scholar]
- Gianotti, R.; Zerbi, P.; Dodiuk-Gad, R.P. Clinical and histopathological study of skin dermatoses in patients affected by SARS-COV-2 infection in the Northern part of Italy. J. Dermatol. Sci. 2020, 98, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Zengarini, C.; Orioni, G.; Cascavilla, A.; Horna Solera, C.; Fulgaro, C.; Misciali, C.; Patrizi, A.; Gaspari, V. Histological pattern in SARS-COV-2-induced viral rash. J Eur Acad Dermatol Venereol. 2020, 2. [Google Scholar] [CrossRef]
- Llamas-Velasco, M.; Munoz-Hernandez, P.; Lazaro-Gonzalez, J.; Reolid-Pérez, A.; Abad-Santamaría, B.; Fraga, J.; Daudén-Tello, E. Thrombotic occlusive vasculopathy in a skin biopsy from a livedoid lesion of a patient with SARS-COV-2. Br. J. Dermatol. 2020, 183, 591–593. [Google Scholar]
- Verdoni, L.; Mazza, A.; Gervasoni, A.; Martelli, L.; Ruggeri, M.; Ciuffreda, M.; Bonanomi, E.; D’Antiga, L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study. Lancet 2020, 395, 1771–1778. [Google Scholar] [CrossRef]
- Viner, R.M.; Whittaker, E. Kawasaki-like disease: Emerging complication during the SARS-COV-2 pandemic. Lancet 2020, 395, 1741–1743. [Google Scholar] [CrossRef]
- Kobayashi, M.; Matsumoto, Y.; Ohya, M.; Harada, K.; Kanno, H. Histologic and Immunohistochemical Evaluation of Infiltrating Inflammatory Cells in Kawasaki Disease Arteritis Lesions. Appl. Immunohistochem. Mol. Morphol. 2020. [Google Scholar] [CrossRef]
- Maino, A.; Rossio, R.; Cugno, M.; Marzano, A.V.; Tedeschi, A. Hypereosinophilic syndrome, Churg-Strauss syndrome and parasitic diseases: Possible links between eosinophilia and thrombosis. Curr. Vasc. Pharmacol. 2012, 10, 670–675. [Google Scholar] [CrossRef]
- Solomon, I.H.; Normandin, E.; Bhattacharyya, S.; Mukerji, S.S.; Keller, K.; Ali, A.S.; Adams, G.; Hornick, J.L.; Padera, R.F., Jr.; Sabeti, P. Neuropathological Features of SARS-CoV-2. N. Engl. J. Med. 2020, 383, 989–992. [Google Scholar] [CrossRef] [PubMed]
- Iuga, A.C.; Marboe, C.C.; Yilmaz, M.M.; Lefkowitch, J.H.; Gauran, C.; Lagana, S.M. Adrenal Vascular Changes in SARS-COV-2 Autopsies. Arch. Pathol. Lab. Med. 2020. Available online: https://www.unboundmedicine.com/medline/citation/32579380/Adrenal_Vascular_Changes_in_COVID-19_Autopsies (accessed on 21 September 2020).
- Yang, M.; Chen, S.; Huang, B.; Zhong, J.M.; Su, H.; Chen, Y.J.; Cao, Q.; Ma, L.; He, J.; Li, X.F.; et al. Pathological Findings in the Testes of SARS-COV-2 Patients: Clinical Implications. Eur. Urol. Focus. 2020, 6, 1124–1129. [Google Scholar] [CrossRef] [PubMed]
- Awulachew, E.; Diriba, K.; Anja, A.; Getu, E.; Belayneh, F. Computed Tomography (CT) Imaging Features of Patients with COVID-19: Systematic Review and Meta-Analysis. Radiol. Res. Pr. 2020, 2020, 1023506. [Google Scholar]
- Bernheim, A.; Mei, X.; Huang, M.; Yang, Y.; Fayad, Z.A.; Zhang, N.; Diao, K.; Lin, B.; Zhu, X.; Li, K.; et al. Chest CT findings in coronavirus disease-19 (SARS-COV-2): Relationship to duration of infection. Radiology 2020, 295, 200463. [Google Scholar] [CrossRef] [Green Version]
- Pan, F.; Ye, T.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L.; et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (SARS-COV-2) pneumonia. Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef] [Green Version]
- Shi, H.; Han, X.; Jiang, N.; Cao, Y.; Alwalid, O.; Gu, J.; Fan, Y.; Zheng, C. Radiological findings from 81 patients with SARS-COV-2 pneumonia in Wuhan, China: A descriptive study. Lancet Infect. Dis. 2020, 20, 425–434. [Google Scholar] [CrossRef]
- Fang, Y.; Zhang, H.; Xie, J.; Lin, M.; Ying, L.; Pang, P.; Ji, W. Sensitivity of chest CT for SARS-COV-2: Comparison to RT-PCR. Radiology 2020, 19, 200432. [Google Scholar]
- Kim, H. Outbreak of novel coronavirus (SARS-COV-2): What is the role of radiologist? Eur. Radiol. 2020, 30, 3266–3267. [Google Scholar] [CrossRef] [Green Version]
- Yoon, S.H.; Lee, K.H.; Kim, J.Y.; Lee, Y.K.; Ko, H.; Kim, K.H.; Park, C.M.; Kim, Y.H. Chest radiographic and CT findings of the 2019 novel coronavirus disease (SARS-COV-2): Analysis of nine patients treated in Korea. Korean J. Radiol. 2020, 21, 494–500. [Google Scholar] [CrossRef]
- Li, Y.; Xia, L. Coronavirus disease 2019 (SARS-COV-2): Role of chest CT in diagnosis and management. AJR Am. J. Roentgenol. 2020, 215, 1–7. [Google Scholar] [CrossRef]
- Wei, J.; Xu, H.; Xiong, J.; Shen, Q.; Fan, B.; Ye, C.; Dong, W.; Hu, F. 2019 novel coronavirus (SARS-COV-2) pneumonia: Serial computed tomography findings. Korean J. Radiol. 2020, 21, 501–504. [Google Scholar] [CrossRef]
- Hu, Z.; Song, C.; Xu, C.; Jin, G.; Chen, Y.; Xu, X.; Ma, H.; Chen, W.; Lin, Y.; Zheng, Y.; et al. Clinical characteristics of 24 asymptomatic infections with SARS-COV-2 screened among close contacts in Nanjing, China. Sci. China Life Sci. 2020, 63, 706–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Z.; Fan, H.; Cai, J.; Li, Y.; Wu, B.; Hou, Y.; Xu, S.; Zhou, F.; Liu, Y.; Xuan, W.; et al. High-resolution computed tomography manifestations of SARS-COV-2 infections in patients of different ages. Eur. J. Radiol. 2020, 126, 108972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryu, S.; Chun, B.C. Epidemiological characteristics of 2019 novel coronavirus: An interim review. Epidemiol. Health 2020, 42, e2020006. [Google Scholar] [CrossRef] [Green Version]
- Chung, M.; Bernheim, A.; Mei, X.; Zhang, N.; Huang, M.; Zeng, X.; Cui, J.; Xu, W.; Yang, Y.; Fayad, Z.A.; et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 2020, 295, 202–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanne, J.P. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: Key points for the radiologist. Radiology 2020, 295, 16–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, F.; Shi, N.; Shan, F.; Zhang, Z.; Shen, J.; Lu, H.; Ling, Y.; Jiang, Y.; Shi, Y. Emerging coronavirus 2019—nCoV pneumonia. Radiology 2020, 295, 210–217. [Google Scholar] [CrossRef] [Green Version]
- Ai, T.; Yang, Z.; Hou, H.; Zhan, C.; Chen, C.; Lv, W.; Tao, Q.; Sun, Z.; Xia, L. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (SARS-COV-2) in China: A Report of 1014 Cases. Radiology 2020, 26, 200642. [Google Scholar]
- Borghesi, A.; Maroldi, R. SARS-COV-2 outbreak in Italy: Experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol. Med. 2020, 125, 509–513. [Google Scholar] [CrossRef]
- Ng, M.-Y.; Lee, E.Y.; Yang, J.; Yang, F.; Li, X.; Wang, H.; Lui, M.M.-S.; Lo, C.S.-Y.; Leung, B.; Khong, P.L.; et al. Imaging profile of the SARS-COV-2 infection: Radiologic findings and literature review. Radiol. Cardiothorac. Imaging 2020, 2, e200034. [Google Scholar] [CrossRef] [Green Version]
- Bai, H.X.; Wang, R.; Xiong, Z.; Hsieh, B.; Chang, K.; Halsey, K.; Tran, T.M.L.; Choi, J.W.; Wang, D.C.; Shi, L.B.; et al. AI Augmentation of Radiologist Performance in Distinguishing SARS-COV-2 from Pneumonia of Other Etiology on Chest CT. Radiology 2020, 27, 201491. [Google Scholar]
- Romann, M.; Fuchslocher, J. Validation of digit-length ratio (2D:4D) assessments on the basis of DXA-derived hand scans. BMC Med. Imaging 2015, 15, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, Q.Y.; Wang, X.T.; Zhang, L.N.; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020, 46, 849–850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pang, T.; Guo, S.; Zhang, X.; Zhao, L. Automatic Lung Segmentation Based on Texture and Deep Features of HRCT Images with Interstitial Lung Disease. BioMed Res. Int. 2019, 2019, 2045432. [Google Scholar] [CrossRef]
- Onishi, Y.; Teramoto, A.; Tsujimoto, M.; Tsukamoto, T.; Saito, K.; Toyama, H.; Imaizumi, K.; Fujita, H. Multiplanar analysis for pulmonary nodule classification in CT images using deep convolutional neural network and generative adversarial networks. Int. J. Comput. Assist. Radiol. Surg. 2020, 15, 173–178. [Google Scholar] [CrossRef]
- Christe, A.; Peters, A.A.; Drakopoulos, D.; Heverhagen, J.T.; Geiser, T.; Stathopoulou, T.; Christodoulidis, S.; Anthimopoulos, M.; Mougiakakou, S.G.; Ebner, L. Computer-Aided Diagnosis of Pulmonary Fibrosis Using Deep Learning and CT Images. Investig. Radiol. 2019, 54, 627–632. [Google Scholar] [CrossRef] [Green Version]
- Fischer, A.M.; Varga-Szemes, A.; Martin, S.S.; Sperl, J.I.; Sahbaee, P.; Neumann, D.; Gawlitza, J.; Henzler, T.; Johnson, C.M.; Nance, J.W.; et al. Artificial Intelligence-based Fully Automated Per Lobe Segmentation and Emphysema-quantification Based on Chest Computed Tomography Compared With Global Initiative for Chronic Obstructive Lung Disease Severity of Smokers. J. Thorac. Imaging 2020, 35 (Suppl. 1), S28–S34. [Google Scholar] [CrossRef]
- Neri, E.; Coppola, F.; Miele, V.; Bibbolino, C.; Grassi, R. Artificial intelligence: Who is responsible for the diagnosis? Radiol. Med. 2020, 125, 517–521. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Qin, L.; Xu, Z.; Yin, Y.; Wang, X.; Kong, B.; Bai, J.; Lu, Y.; Fang, Z.; Song, Q.; et al. Artificial Intelligence Distinguishes SARS-COV-2 from Community Acquired Pneumonia on Chest CT. Radiology 2020, 19, 200905. [Google Scholar]
- Stern, E.J.; Bernheim, A.; Chung, M. SARS-COV-2 compatible chest CT pattern. Am. Coll. Radiol. 2020. Available online: www.acrdsi.org/DSI-Services/Define-AI/Use-Cases/SARS-COV-2-Compatible-Chest-CT-Pattern (accessed on 21 September 2020).
- Mei, X.; Lee, H.C.; Diao, K.Y.; Huang, M.; Lin, B.; Liu, C.; Xie, Z.; Ma, Y.; Robson, P.M.; Chung, M.; et al. Artificial intelligence-enabled rapid diagnosis of patients with SARS-COV-2. Nat. Med. 2020. [Google Scholar] [CrossRef]
- Esfandiarei, M.; McManus, B.M. Molecular biology and pathogenesis of viral myocarditis. Annu. Rev. Pathol. 2008, 3, 127–155. [Google Scholar] [CrossRef] [PubMed]
- Riski, H.; Hovi, T.; Frick, M.H. Carditis associated with coronavirus infection. Lancet 1980, 2, 100–101. [Google Scholar] [CrossRef]
- Alhogbani, T. Acute myocarditis associated with novel Middle east respiratory syndrome coronavirus. Ann. Saudi Med. 2016, 36, 78–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agrawal, A.S.; Garron, T.; Tao, X.; Peng, B.H.; Wakamiya, M.; Chan, T.S.; Couch, R.B.; Tseng, C.T. Generation of a transgenic mouse model of Middle East respiratory syndrome coronavirus infection and disease. J. Virol. 2015, 89, 3659–3670. [Google Scholar] [CrossRef] [Green Version]
- Schaecher, S.R.; Stabenow, J.; Oberle, C.; Schriewer, J.; Buller, R.M.; Sagartz, J.E.; Pekosz, A. An immunosuppressed Syrian golden hamster model for SARS-CoV infection. Version 2. Virology 2008, 380, 312–321. [Google Scholar] [CrossRef] [Green Version]
- Siripanthong, B.; Nazarian, S.; Muser, D.; Deo, R.; Santangeli, P.; Khanji, M.Y.; Cooper, L.T.J.; Chahal, C.A.A. Recognizing SARS-COV-2-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020. [Google Scholar] [CrossRef]
- Kociol, R.D.; Cooper, L.T.; Fang, J.C.; Moslehi, J.J.; Pang, P.S.; Sabe, M.A.; Shah, R.V.; Sims, D.B.; Thiene, G.; Vardeny, O.; et al. Recognition and Initial Management of Fulminant Myocarditis: A Scientific Statement from the American Heart Association. Circulation 2020, 141, e69–e92. [Google Scholar] [CrossRef]
- Inciardi, R.M.; Lupi, L.; Zaccone, G.; Italia, L.; Raffo, M.; Tomasoni, D.; Cani, D.S.; Cerini, M.; Farina, D.; Gavazzi, E.; et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (SARS-COV-2). JAMA Cardiol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Kim, I.C.; Kim, J.Y.; Kim, H.A.; Han, S. SARS-COV-2-related myocarditis in a 21-year-old female patient. Eur. Heart J. 2020, 41, 1859. [Google Scholar] [CrossRef]
- Avula, A.; Nalleballe, K.; Narula, N.; Sapozhnikov, S.; Dandu, V.; Toom, S.; Glaser, A.; Elsayegh, D. SARS-COV-2 presenting as stroke. Brain Behav. Immun. 2020, 87, 115–119. [Google Scholar] [CrossRef]
- Valderrama, E.V.; Humbert, K.; Lord, A.; Frontera, J.; Yaghi, S. Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Ischemic Stroke. Stroke 2020, 51, 120030153. [Google Scholar] [CrossRef] [PubMed]
- Ye, M.; Ren, Y.; Lv, T. Encephalitis as a clinical manifestation of SARS-COV-2. Brain Behav. Immun. 2020, 88, 945–946. [Google Scholar] [CrossRef] [PubMed]
- Panciani, P.P.; Saraceno, G.; Zanin, L.; Renisi, G.; Signorini, L.; Battaglia, L.; Fontanella, M.M. SARS-CoV-2: “Three-steps” infection model and CSF diagnostic implication. Brain Behav. Immun. 2020, 87, 128–129. [Google Scholar] [CrossRef] [PubMed]
- Zanin, L.; Saraceno, G.; Panciani, P.P.; Renisi, G.; Signorini, L.; Migliorati, K.; Fontanella, M.M. SARS-CoV-2 can induce brain and spine demyelinating lesions. Acta Neurochir. 2020, 162, 1491–1494. [Google Scholar] [CrossRef]
- Filippi, L.; Schillaci, O. SPECT/CT with a hybrid camera: A new imaging modality for the functional anatomical mapping of infections. Expert Rev. Med. Devices. 2006, 3, 699–703. [Google Scholar] [CrossRef]
- Vaidyanathan, S.; Patel, C.; Scarsbrook, A.; Chowdhury, F.U. FDG PET/CT in infection and inflammation--current and emerging clinical applications. Clin. Radiol. 2015, 70, 787–800. [Google Scholar] [CrossRef]
- Schillaci, O. Use of dual-point fluorodeoxyglucose imaging to enhance sensitivity and specificity. Semin. Nucl. Med. 2012, 42, 267–280. [Google Scholar] [CrossRef] [Green Version]
- Schillaci, O.; Urbano, N. Digital PET/CT: A new intriguing chance for clinical nuclear medicine and personalized molecular imaging. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1222–1225. [Google Scholar] [CrossRef] [Green Version]
- Capitanio, S.; Nordin, A.J.; Noraini, A.R.; Rossetti, C. PET/CT in nononcological lung diseases: Current applications and future perspectives. Eur. Respir. Rev. 2016, 25, 247–258. [Google Scholar] [CrossRef]
- Qin, C.; Liu, F.; Yen, T.C.; Lan, X. 18F-FDG PET/CT findings of SARS-COV-2: A series of four highly suspected cases. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1281–1286. [Google Scholar] [CrossRef] [Green Version]
- Setti, L.; Kirienko, M.; Dalto, S.C.; Bonacina, M.; Bombardieri, E. FDG-PET/CT findings highly suspicious for SARS-COV-2 in an Italian case series of asymptomatic patients. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 1649–1656. [Google Scholar] [CrossRef]
- Polverari, G.; Arena, V.; Ceci, F.; Pelosi, E.; Ianniello, A.; Poli, E.; Sandri, A.; Penna, D. 18F-Fluorodeoxyglucose Uptake in Patient With Asymptomatic Severe Acute Respiratory Syndrome Coronavirus 2 (Coronavirus Disease 2019) Referred to Positron Emission Tomography/Computed Tomography for NSCLC Restaging. J. Thorac. Oncol. 2020, 15, 1078–1080. [Google Scholar] [CrossRef] [PubMed]
- Colandrea, M.; Gilardi, L.; Travaini, L.L.; Fracassi, S.L.V.; Funicelli, L.; Grana, C.M. (18)F-FDG PET/CT in asymptomatic patients with SARS-COV-2: The submerged iceberg surfaces. Jpn. J. Radiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Habouzit, V.; Sanchez, A.; Dehbi, S.; Prevot, N.; Bonnefoy, P.B. Incidental Finding of SARS-COV-2 Lung Infection in 18F-FDG PET/CT: What Should We Do? Clin. Nucl. Med. 2020. [Google Scholar] [CrossRef]
- Zou, S.; Zhu, X. FDG PET/CT of SARS-COV-2. Radiology 2020, 296, E118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Czernin, J.; Fanti, S.; Meyer, P.T.; Allen-Auerbach, M.; Hacker, M.; Sathekge, M.; Hicks, R.; Scott, A.M.; Hatazawa, J.; Yun, M.; et al. Imaging clinic operations in the times of SARS-COV-2: Strategies, Precautions and Experiences. J. Nucl. Med. 2020, 61, 626–629. [Google Scholar] [CrossRef] [Green Version]
- Das, K.M.; Lee, E.Y.; Singh, R.; Enani, M.A.; Al Dossari, K.; Van Gorkom, K.; Larsson, S.G.; Langer, R.D. Follow-up chest radiographic findings in patients with MERS-CoV after recovery. Indian J. Radiol. Imaging 2017, 27, 342–349. [Google Scholar] [CrossRef]
- Chefer, S.; Thomasson, D.; Seidel, J.; Reba, R.C.; Bohannon, J.K.; Lackemeyer, M.G.; Bartos, C.; Sayre, P.J.; Bollinger, L.; Hensley, L.E.; et al. Modeling [18F]-FDG lymphoid tissue kinetics to characterize nonhuman primate immune response to Middle East respiratory syndrome-coronavirus aerosol challenge. EJNMMI Res. 2015, 5, 65. [Google Scholar] [CrossRef] [Green Version]
- Yuan, H.; Wilks, M.Q.; Normandin, M.D.; El Fakhri, G.; Kaittanis, C.; Josephson, L. Heat-induced radiolabeling and fluorescence labeling of Feraheme nanoparticles for PET/SPECT imaging and flow cytometry. Nat. Protoc. 2018, 13, 392–412. [Google Scholar] [CrossRef] [Green Version]
- Muehe, A.M.; Siedek, F.; Theruvath, A.J.; Seekins, J.; Spunt, S.L.; Pribnow, A.; Hazard, F.K.; Liang, T.; Daldrup-Link, H. Differentiation of benign and malignant lymph nodes in pediatric patients on ferumoxytol-enhanced PET/MRI. Theranostics 2020, 10, 3612–3621. [Google Scholar] [CrossRef]
- Wallace, M.; Pyzalski, R.; Horejsh, D.; Brown, C.; Djavani, M.; Lu, Y.; Hanson, J.M.; Mitchen, J.L.; Perlman, S.B.; Pauza, C.D. Whole body positron emission tomography imaging of activated lymphoid tissues during acute simian-human immunodeficiency virus 89.6PD infection in rhesus macaques. Virology 2000, 274, 255–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, Q.Y.; Chen, Y.X.; Fang, J.Y. 2019 Novel coronavirus infection and gastrointestinal tract. J. Dig. Dis. 2020, 21, 125–126. [Google Scholar] [CrossRef] [Green Version]
- Akhmerov, A.; Marbán, E. SARS-COV-2 and the Heart. Circ. Res. 2020, 126, 1443–1455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahid, Z.; Kalayanamitra, R.; McClafferty, B.; Kepko, D.; Ramgobin, D.; Patel, R.; Aggarwal, C.S.; Vunnam, R.; Sahu, N.; Bhatt, D.; et al. SARS-COV-2 and Older Adults: What We Know. J. Am. Geriatr. Soc. 2020, 68, 926–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karimi-Galougahi, M.; Yousefi-Koma, A.; Bakhshayeshkaram, M.; Raad, N.; Haseli, S. 18FDG PET/CT Scan Reveals Hypoactive Orbitofrontal Cortex in Anosmia of SARS-COV-2. Acad. Radiol. 2020, 27, 1042–1043. [Google Scholar] [CrossRef]
- Vaira, L.A.; Salzano, G.; Deiana, G.; De Riu, G. Anosmia and ageusia: Common findings in SARS-COV-2 patients. Laryngoscope 2020, 130, 1787. [Google Scholar] [CrossRef] [Green Version]
- Bellani, G.; Messa, C.; Guerra, L.; Spagnolli, E.; Foti, G.; Patroniti, N.; Fumagalli, R.; Musch, G.; Fazio, F.; Pesenti, A. Lungs of patients with acute respiratory distress syndrome show diffuse inflammation in normally aerated regions: A [18F]-fluoro-2-deoxy-d-glucose PET/CT study. Crit. Care Med. 2009, 37, 2216–2222. [Google Scholar] [CrossRef]
- Juengling, F.D.; Maldonado, A.; Wuest, F.; Schindler, T.H. The role of Nuclear Medicine for SARS-COV-2—Time to act now. J. Nucl. Med. 2020, 61, 781–782. [Google Scholar] [CrossRef]
- Bhardwaj, A.; Kaur, J.; Wuest, M.; Wuest, F. In situ click chemistry generation of cyclooxygenase-2 inhibitors. Nat. Commun. 2017, 8, 1. [Google Scholar] [CrossRef] [Green Version]
- Tian, X.; Xie, G.; Xiao, H.; Ding, F.; Bao, W.; Zhang, M. CXCR4 knockdown prevents inflammatory cytokine expression in macrophages by suppressing activation of MAPK and NF-κB signaling pathways. Cell Biosci. 2019, 9, 55. [Google Scholar] [CrossRef] [Green Version]
- Linares, A.; Couling, L.E.; Carrera, E.J.; Speth, R.C. Receptor Autoradiography Protocol for the Localized Visualization of Angiotensin II Receptors. J. Vis. Exp. 2016, 112, 1–15. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | SARS-CoV-2 Infection |
|---|---|
| Gross Pathology |
|
| Microscopic examination |
|
| Pathogenesis | Combination of direct virus-induced cytopathic effects, immunologic injury, and microvascular damage induced by cytokines |
| Lung | References |
| Diffuse alveolar damage (histological hallmark of SARS-CoV-2 infection) | [15,16,17,18,19,20,21,22,23,24] |
| Focal vasculitis and capillaritis associated to microthrombosis as direct viral effect | |
| Thrombosis of large and medium-size pulmonary, related to SARS-COV-2-associated coagulopathy (likely secondary to an endothelial damage related to direct viral infection of the endothelial cells) or deriving from the deep veins of the lower extremities. Superimposed bronchopneumonia as result of bacterial superinfection | |
| Heart | |
| Myocardial damage and myocarditis associated with increase in troponin levels, related to (a) direct myocardial infection by SARS-CoV-2 (b) hypoxemia due to respiratory failure and (c) inflammatory response correlated to the severe systemic inflammation status. Acute vasculitis of the intramyocardial vessels | [25,26,27,28,29,30] |
| Kidney | |
| Acute tubular injury involving mainly the proximal tubules, probably related to direct infection of kidney by SARS-CoV-2 | [30,32] |
| Skin | |
| Urticarial rashes and papulovesicular exanthems (cause not yet known) | [33,34,35,36,37,38,39,40] |
| Livedoid purple lesions and acrocyanosis | |
| Kawasaki disease | |
| Central Nervous System | |
| Aspecific acute hypoxic damage in the brain and cerebellum (molecular test in sections of brain tissue were positive for the virus, but not immunohistochemistry) | [41] |
| Liver | |
| Sinusoidal dilatation with lymphocytic infiltration and steatosis (cause not yet known) | [20] |
| Adrenal | |
| Acute fibrinoid necrosis of arterioles (cause not yet known) | [42] |
| Testis | |
| Seminiferous tubular injury, mild lymphocytic inflammation (cause not yet known) | [43] |
| Patients | Sex | Age (mean) | Type of Study | References | |
|---|---|---|---|---|---|
| Bernheim A et al. | 121 | 61 M; 60 W | 45 ± 16 | R | [45] |
| Pan F et al. | 21 | 6 M; 15 W | 40 ± 9 | R | [46] |
| Shi H et al. | 81 | 42 M; 39 W | 49.5 ± 11 | R | [47] |
| Fang Y et al. | 51 | 29 M; 22 W | 45 | R | [48] |
| Yoon SH et al. | 9 | 4 M; 5 W | 54 | R | [50] |
| Li Y et al. | 53 | 29 M; 24 W | 58 ± 17 | R | [51] |
| Wei J et al. | 1 | 1 W | 40 | CR | [52] |
| Hu Z et al. | 24 | / | / | R | [53] |
| Chen Z et al. | 98 | M 52; W 46 | 43 ± 17.2 | R | [54] |
| Chen N et al. | 99 | M 67; W 32 | 55.5 ± 13.1 | R | [31] |
| Huang C et al. | 41 | M 30; W 11 | 49 | R | [11] |
| Wang D et al. | 138 | M 75; 63 W | / | R | [12] |
| Chung M et al. | 21 | M 13: W 8 | 51 ± 14 | R | [56] |
| Song F et al. | 51 | M 25; W 26 | 49 ± 16 | R | [58] |
| Ai T et al. | 1014 | M 467; W 547 | 51 ± 15 | R | [59] |
| Ng MY et al. | 18 | M 13; W 8 | 56 | R | [61] |
| CT Findings | Number of Studies | Number of Patients (%) |
|---|---|---|
| Patterns of the lesion | ||
| Ground-glass opacity with consolidation | 60 | 768 (18%) |
| Ground-glass opacity | 60 | 2482 (65%) |
| Consolidation | 60 | 1259 (22%) |
| Crazy paving pattern | 24 | 575 (12%) |
| Reversed halo sign | 24 | 146 (1%) |
| Other signs in the lesion | ||
| Interlobular septal thickening | 23 | 691 (27%) |
| Air bronchogram sign | 23 | 531 (18%) |
| Distribution | ||
| Bilateral | 48 | 3952 (80%) |
| Unilateral | 48 | 641 (20%) |
| Right lung | 8 | 48 (62%) |
| Left lung | 8 | 29 (38%) |
| Number of lobes involved | ||
| One lobe | 13 | 278 (14%) |
| Two lobes | 13 | 299 (11%) |
| Three lobes | 13 | 250 (13%) |
| Four lobes | 13 | 212 (15%) |
| Five lobes | 14 | 384 (34%) |
| More than one lobe | 14 | 1145 (76%) |
| Lobe of lesion distribution | ||
| Left upper lobe | 14 | 731 (74%) |
| Left lower lobe | 20 | 504 (46%) |
| Right upper lobe | 19 | 455 (40%) |
| Right middle lobe | 15 | 326 (38%) |
| Right lower lobe | 17 | 784 (74%) |
| Other findings | ||
| Pleural effusion | 60 | 94 (1.6%) |
| Lymphadenopathy | 60 | 21 (0.7%) |
| Pulmonary nodules | 22 | 262 (9%) |
| SARS-CoV-2 Positive | Imaging Analysis | Type of Study | Reference | |
|---|---|---|---|---|
| Qin et al. | 4 | 18F-FDG PET/CT | R | [92] |
| Setti et al. | 13 | 18F-FDG PET/CT | P | [93] |
| Polverari et al. | 1 | 18F-FDG PET/CT | CR | [94] |
| Colandrea et al. | 5 | 18F-FDG PET/CT | CS | [95] |
| Habouzit et al. | 1 | 18F-FDG PET/CT | CR | [96] |
| Zou et al. | 1 | 18F-FDG PET/CT | CR | [97] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scimeca, M.; Urbano, N.; Bonfiglio, R.; Montanaro, M.; Bonanno, E.; Schillaci, O.; Mauriello, A. Imaging Diagnostics and Pathology in SARS-CoV-2-Related Diseases. Int. J. Mol. Sci. 2020, 21, 6960. https://doi.org/10.3390/ijms21186960
Scimeca M, Urbano N, Bonfiglio R, Montanaro M, Bonanno E, Schillaci O, Mauriello A. Imaging Diagnostics and Pathology in SARS-CoV-2-Related Diseases. International Journal of Molecular Sciences. 2020; 21(18):6960. https://doi.org/10.3390/ijms21186960
Chicago/Turabian StyleScimeca, Manuel, Nicoletta Urbano, Rita Bonfiglio, Manuela Montanaro, Elena Bonanno, Orazio Schillaci, and Alessandro Mauriello. 2020. "Imaging Diagnostics and Pathology in SARS-CoV-2-Related Diseases" International Journal of Molecular Sciences 21, no. 18: 6960. https://doi.org/10.3390/ijms21186960
APA StyleScimeca, M., Urbano, N., Bonfiglio, R., Montanaro, M., Bonanno, E., Schillaci, O., & Mauriello, A. (2020). Imaging Diagnostics and Pathology in SARS-CoV-2-Related Diseases. International Journal of Molecular Sciences, 21(18), 6960. https://doi.org/10.3390/ijms21186960








