Sex Differences in Placental Protein Expression and Efficiency in a Rat Model of Fetal Programming Induced by Maternal Undernutrition
Abstract
1. Introduction
2. Results
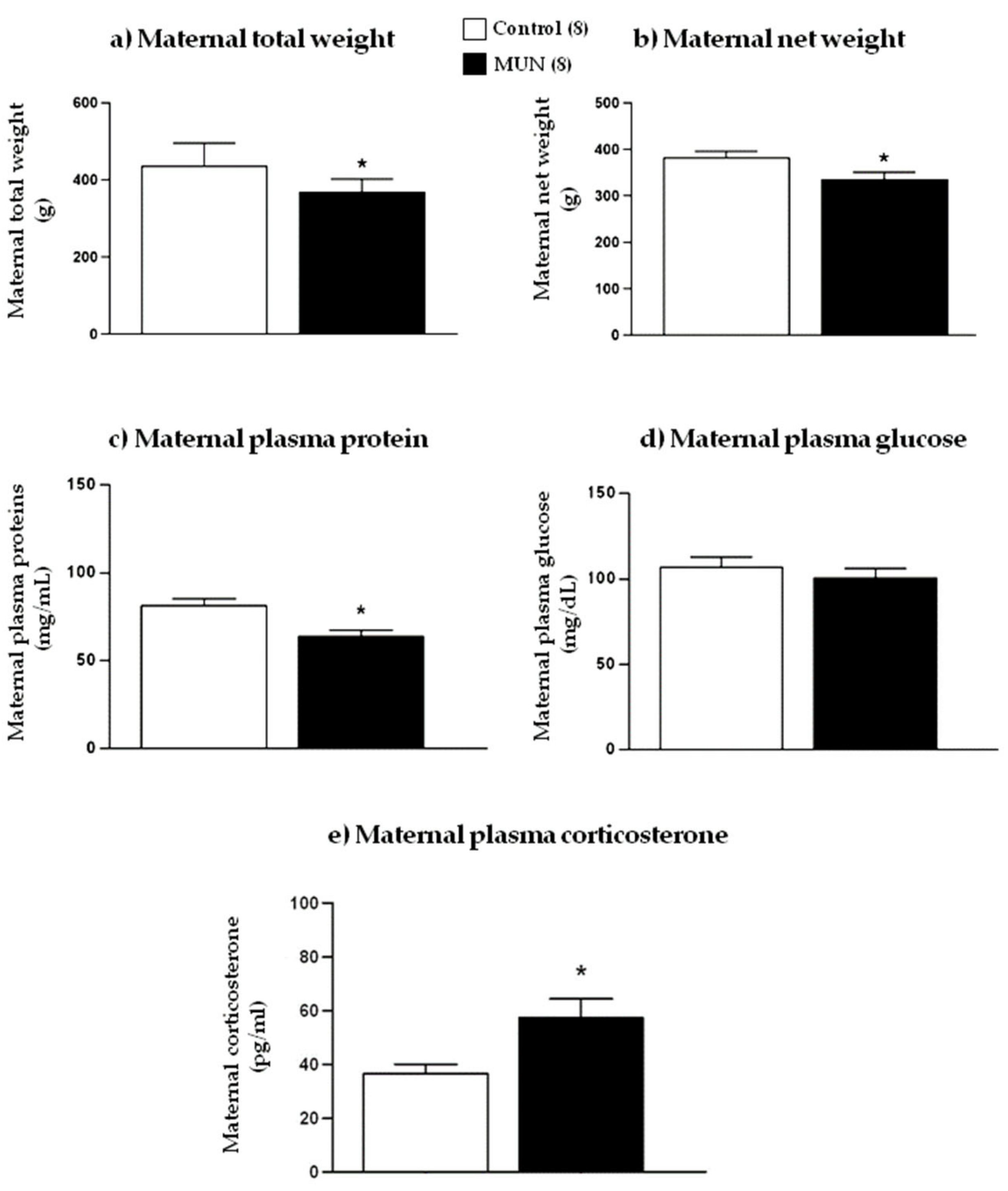
2.1. Maternal Weight and Metabolic Parameters
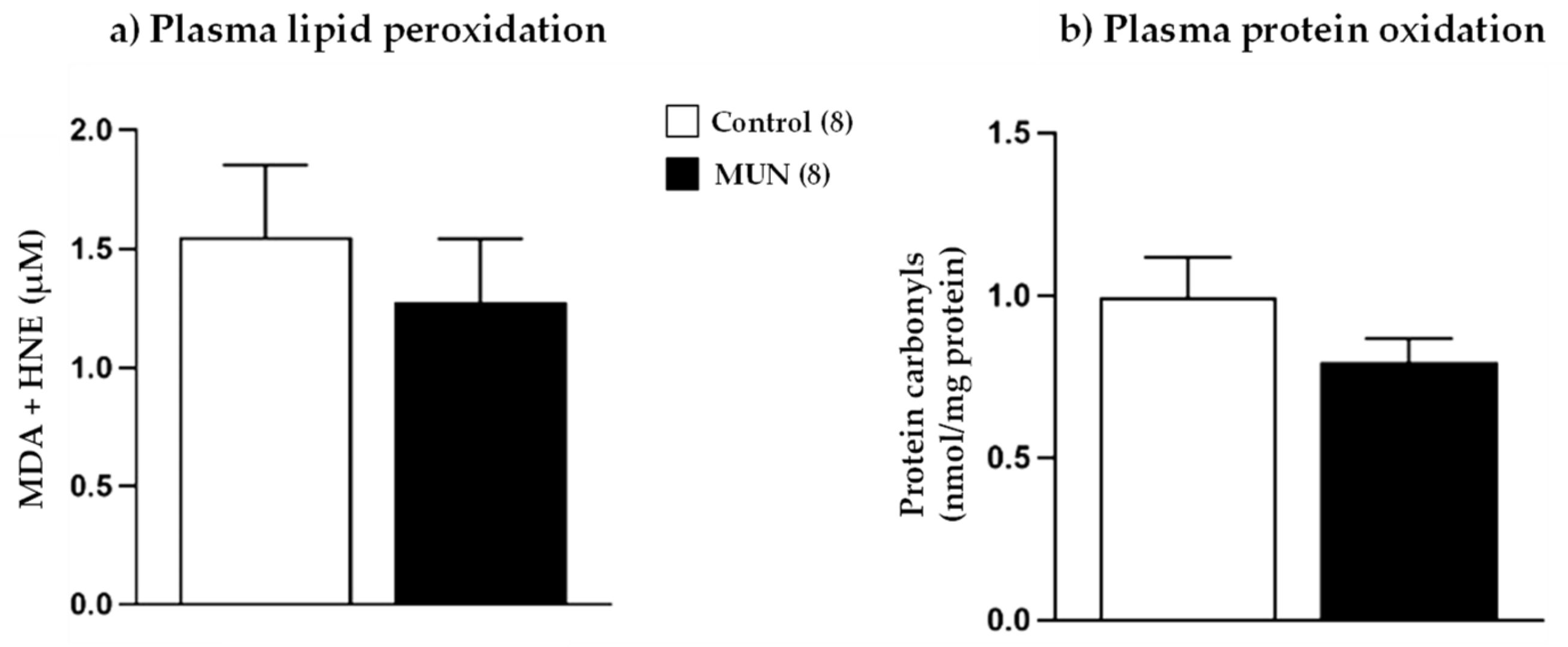
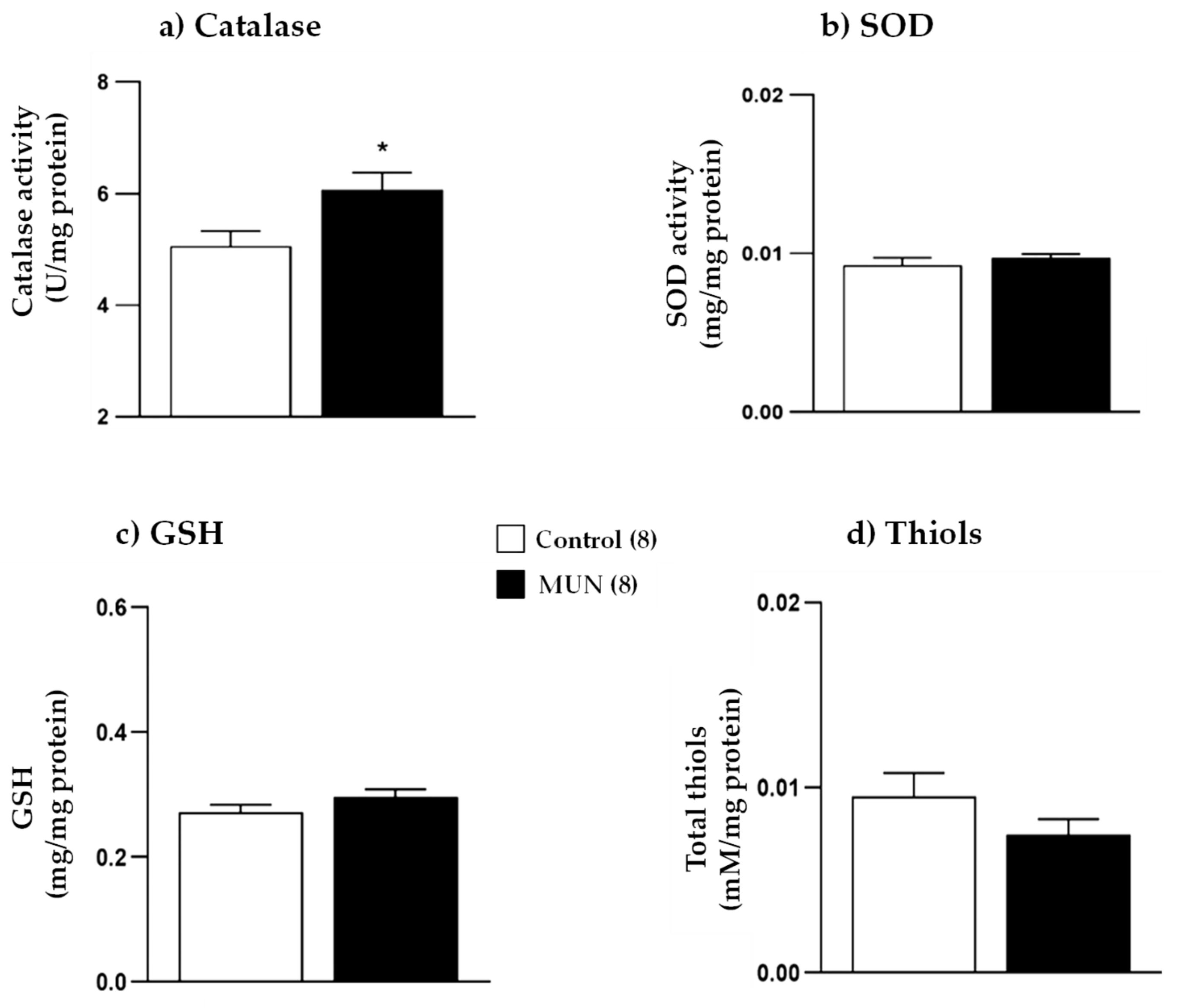
2.2. Maternal Plasma Oxidative Status
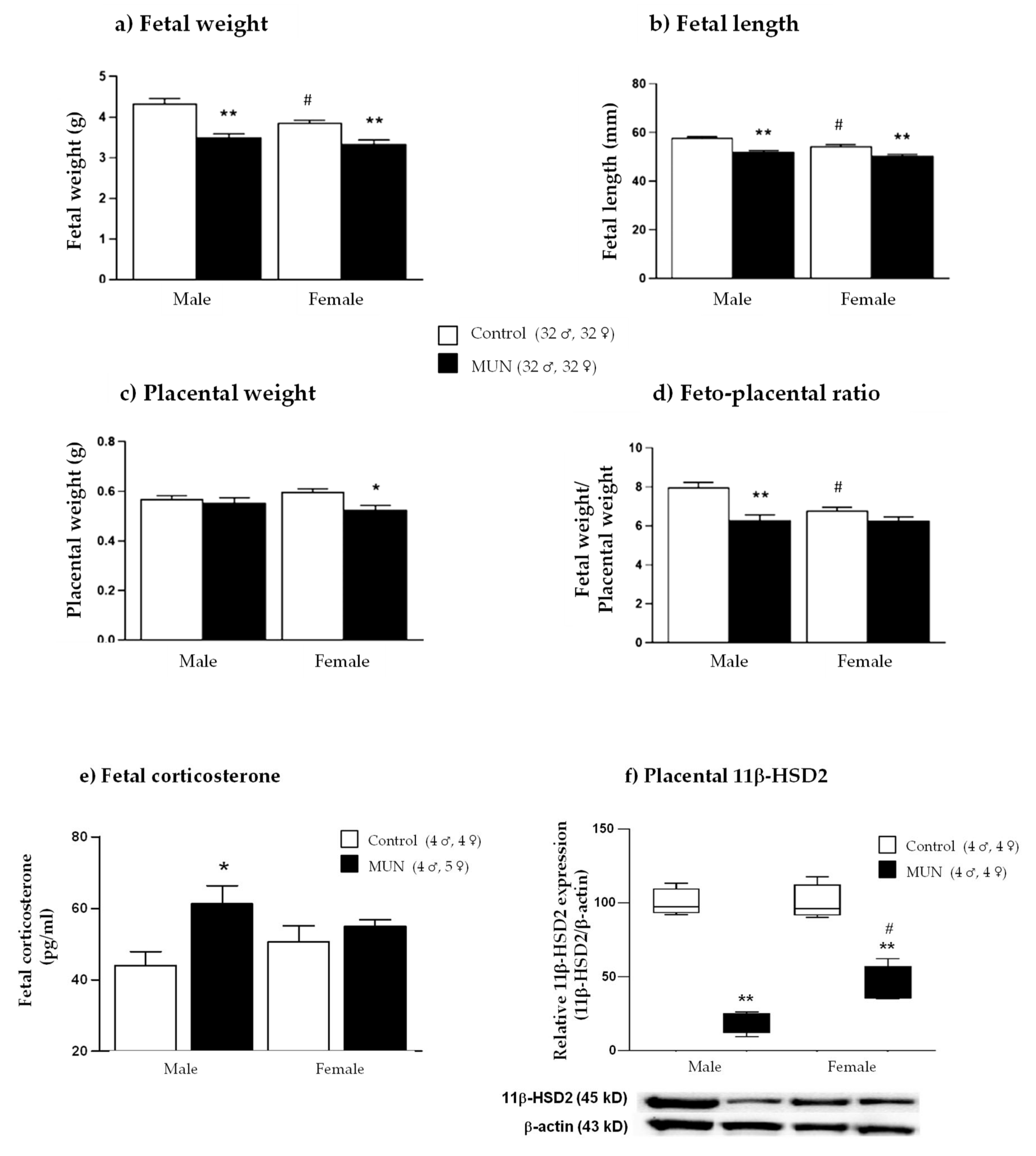
2.3. Fetal and Placental Growth Parameters
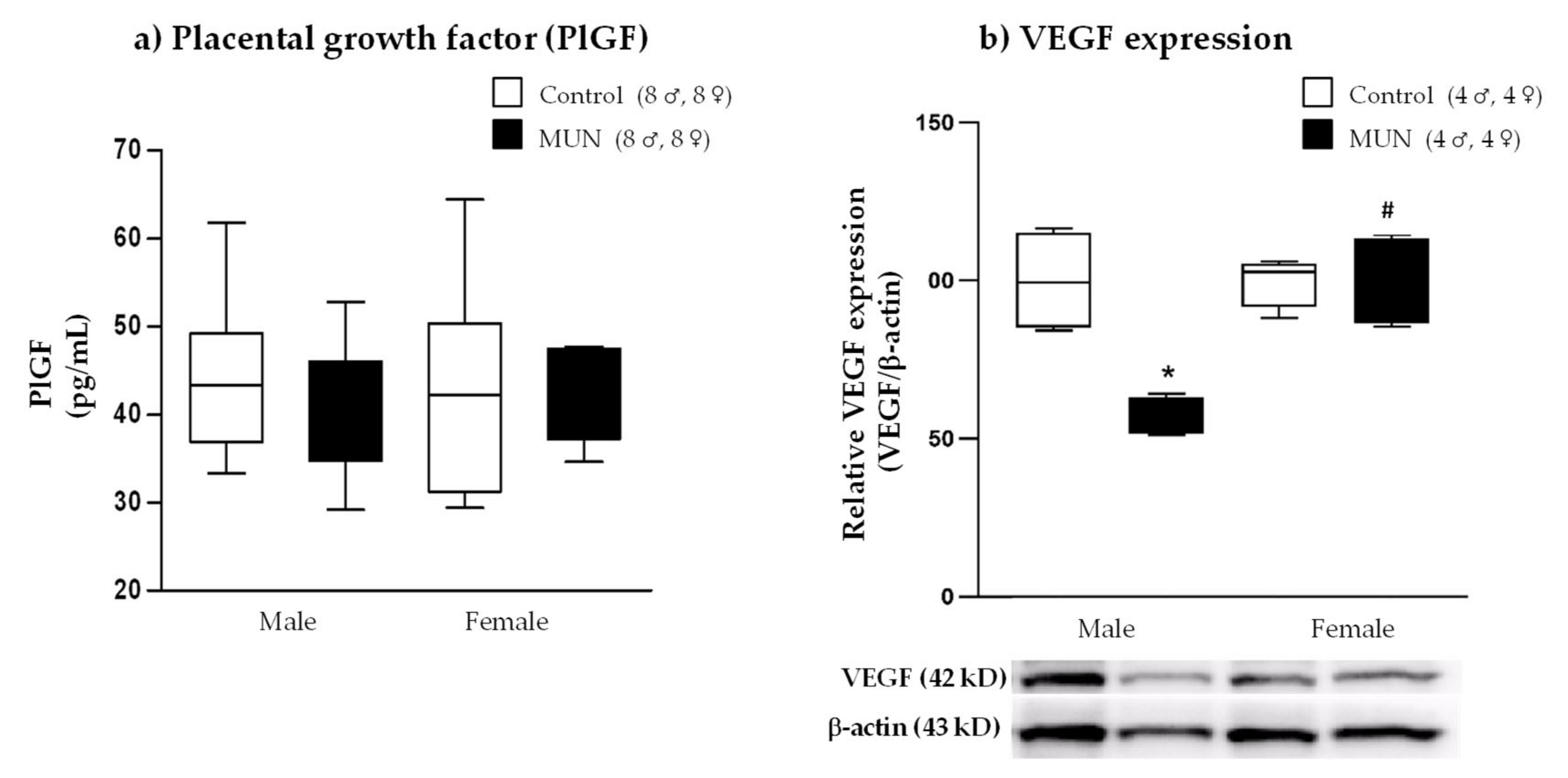
2.4. Placental Growth Factor (PlGF) and Vascular Endothelial Growth Factor (VEGF)
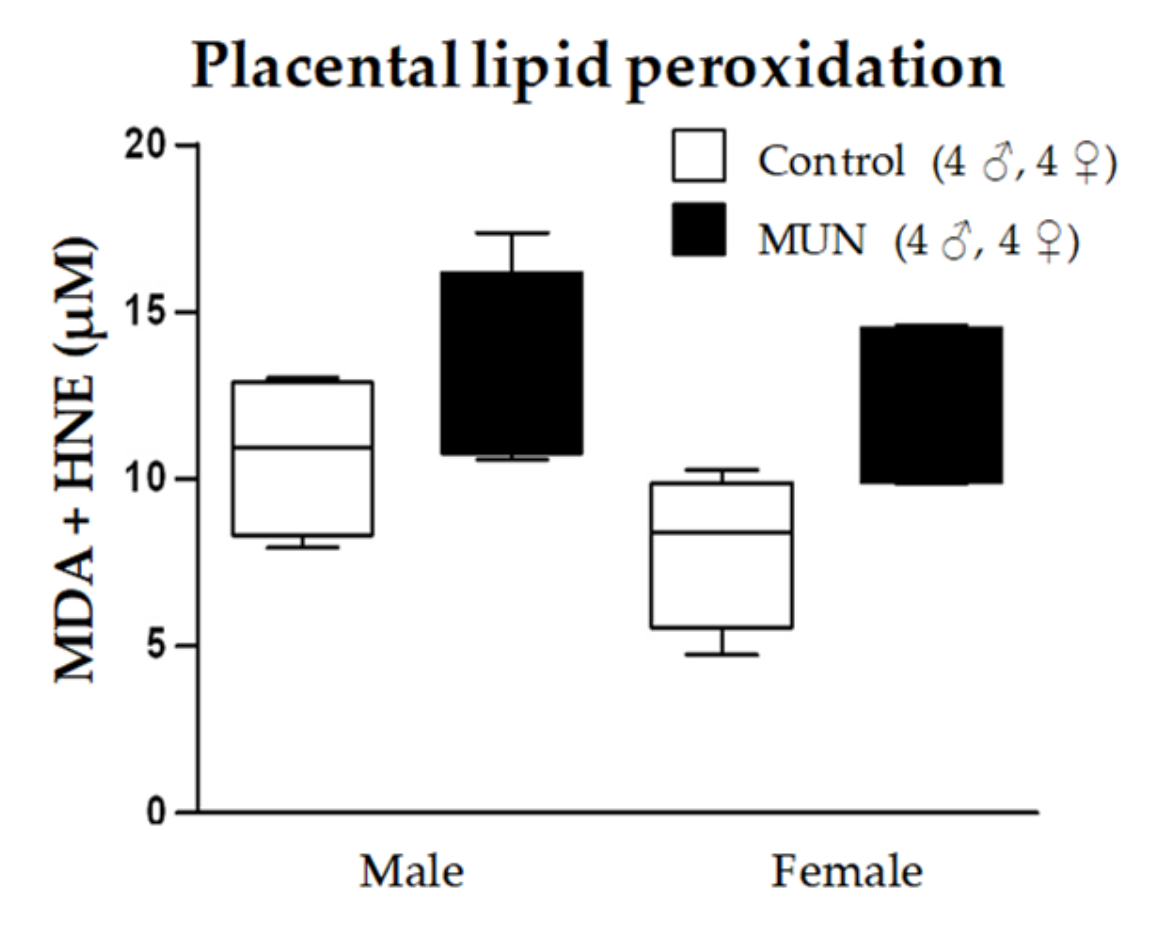
2.5. Placental Oxidative Status
2.5.1. Lipid Peroxidation
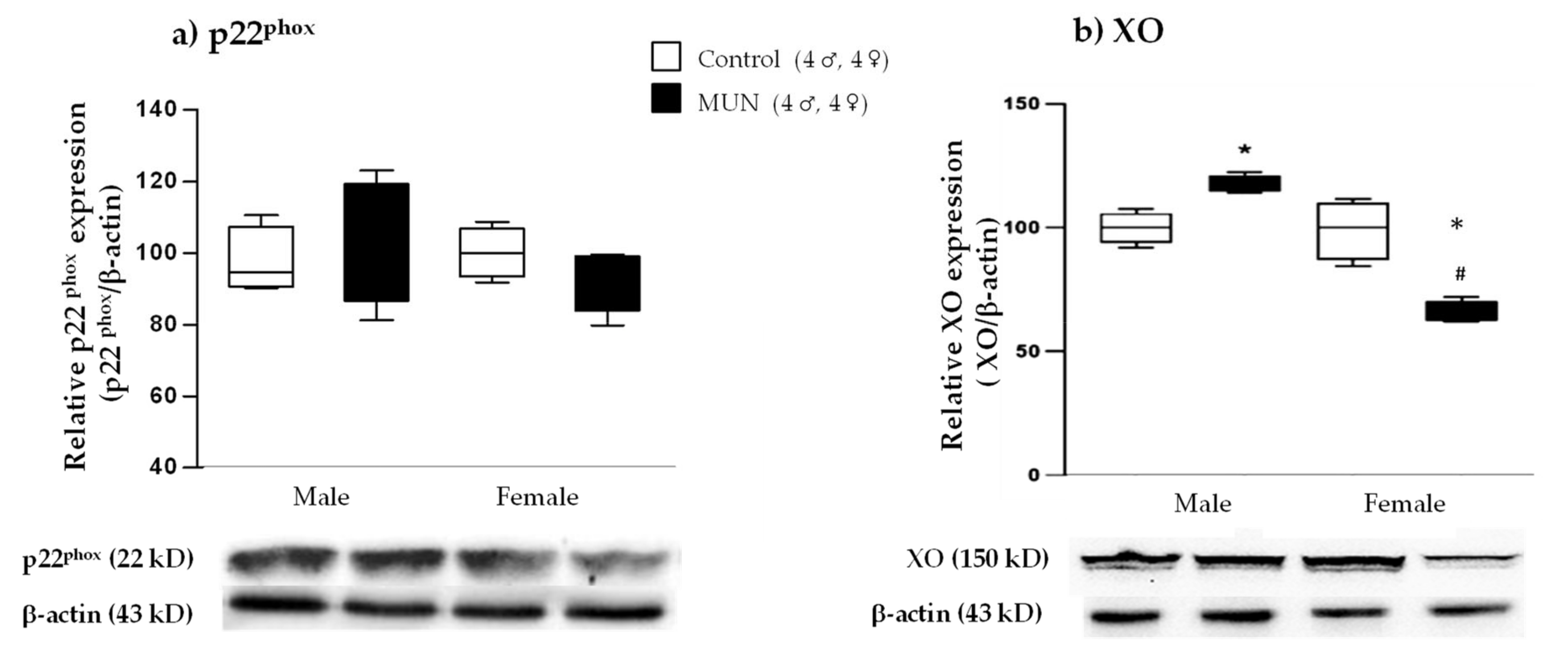
2.5.2. Expression of ROS-Producing Enzymes
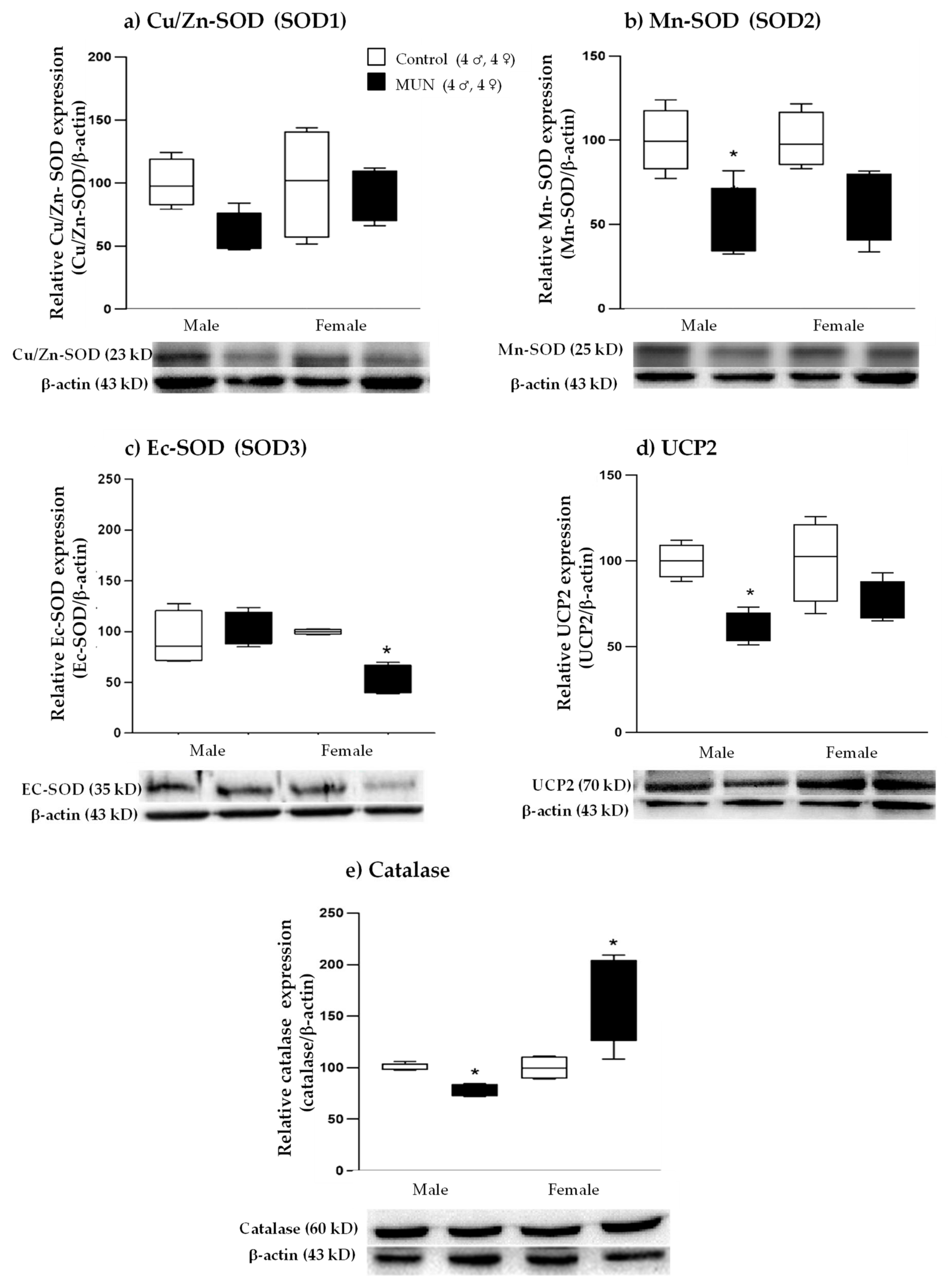
2.5.3. Expression of ROS-Degrading Enzymes
3. Discussion
4. Materials and Methods
4.1. Maternal Undernutrition (MUN) Model
4.2. Experimental Design
4.3. Oxidative Status in Plasma and Placenta
4.4. Western Blot Assay in Placental Tissue
4.5. Corticosterone Assay in Plasma
4.6. Placental Growth Factor (PlGF)
4.7. Statistical Analysis
5. Conclusions
- Suboptimal nutrition during gestation induces stress response and elevates maternal corticosterone.
- Placental adaptation to undernutrition exhibits sexual dimorphism, showing reduced efficiency in males.
- Lower efficiency in MUN male placenta may be related to excess ROS and reduced angiogenic factors and GC barrier, and may contribute to higher susceptibility to cardiovascular disease programming.
- Female placenta has better adaptive response to maternal undernutrition with moderate growth and better oxidative balance, angiogenesis, and GC barrier
- Lower GC access to female fetus can contribute to lower susceptibility to cardiovascular disease programming in response to undernutrition.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alexander, B.T.; Dasinger, J.H.; Intapad, S. Fetal programming and cardiovascular pathology. Compr. Physiol. 2015, 5, 997–1025. [Google Scholar] [CrossRef] [PubMed]
- Jaskolka, D.; Retnakaran, R.; Zinman, B.; Kramer, C.K. Sex of the baby and risk of gestational diabetes mellitus in the mother: A systematic review and meta-analysis. Diabetologia 2015, 58, 2469–2475. [Google Scholar] [CrossRef] [PubMed]
- Jaskolka, D.; Retnakaran, R.; Zinman, B.; Kramer, C.K. Fetal sex and maternal risk of pre-eclampsia/eclampsia: A systematic review and meta-analysis. Int. J. Obstet. Gynaecol. 2017, 124, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Ramiro-Cortijo, D.; de la Calle, M.; Böger, R.; Hannemann, J.; Lüneburg, N.; López-Giménez, M.R.; Rodríguez-Rodríguez, P.; Martín-Cabrejas, M.Á.; Benítez, V.; de Pablo, Á.L.L.; et al. Male fetal sex is associated with low maternal plasma anti-inflammatory cytokine profile in the first trimester of healthy pregnancies. Cytokine 2020, 136, 155290. [Google Scholar] [CrossRef]
- Tamayev, L.; Schreiber, L.; Marciano, A.; Bar, J.; Kovo, M. Are there gender-specific differences in pregnancy outcome and placental abnormalities of pregnancies complicated with small for gestational age? Arch. Gynecol. Obstet. 2020, 301, 1147–1151. [Google Scholar] [CrossRef]
- Peacock, J.L.; Marston, L.; Marlow, N.; Calvert, S.A.; Greenough, A. Neonatal and infant outcome in boys and girls born very prematurely. Pediatr. Res. 2012, 71, 305–310. [Google Scholar] [CrossRef]
- Bennet, L. Sex, drugs and rock and roll: Tales from preterm fetal life. J. Physiol. 2017, 595, 1865–1881. [Google Scholar] [CrossRef]
- Gabory, A.; Roseboom, T.J.; Moore, T.; Moore, L.G.; Junien, C. Placental contribution to the origins of sexual dimorphism in health and diseases: Sex chromosomes and epigenetics. Biol. Sex Differ. 2013, 4, 5. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, P.; Ramiro-Cortijo, D.; Reyes-Hernández, C.G.; López de Pablo, A.L.; González, M.C.; Arribas, S.M. Implication of oxidative stress in fetal programming of cardiovascular disease. Front. Physiol. 2018, 9, 602. [Google Scholar] [CrossRef]
- Bartho, L.A.; Holland, O.J.; Moritz, K.M.; Perkins, A.V.; Cuffe, J.S.M. Maternal corticosterone in the mouse alters oxidative stress markers, antioxidant function and mitochondrial content in placentas of female fetuses. J. Physiol. 2019, 597, 3053–3067. [Google Scholar] [CrossRef]
- Stark, M.J.; Hodyl, N.A.; Wright, I.M.R.; Clifton, V.L. Influence of sex and glucocorticoid exposure on preterm placental pro-oxidant-antioxidant balance. Placenta 2011, 32, 865–870. [Google Scholar] [CrossRef] [PubMed]
- Belkacemi, L.; Jelks, A.; Chen, C.-H.; Ross, M.G.; Desai, M. Altered placental development in undernourished rats: Role of maternal glucocorticoids. Reprod. Biol. Endocrinol. 2011, 9, 105. [Google Scholar] [CrossRef] [PubMed]
- Hewitt, D.P.; Mark, P.J.; Waddell, B.J. Glucocorticoids Prevent the Normal Increase in Placental Vascular Endothelial Growth Factor Expression and Placental Vascularity during Late Pregnancy in the Rat. Endocrinology 2006, 147, 5568–5574. [Google Scholar] [CrossRef] [PubMed]
- Togher, K.L.; Togher, K.L.; O’Keeffe, M.M.; O’Keeffe, M.M.; Khashan, A.S.; Khashan, A.S.; Gutierrez, H.; Gutierrez, H.; Kenny, L.C.; Kenny, L.C.; et al. Epigenetic regulation of the placental HSD11B2 barrier and its role as a critical regulator of fetal development. Epigenetics 2014, 9, 816–822. [Google Scholar] [CrossRef]
- Correia-Branco, A.; Keating, E.; Martel, F. Maternal undernutrition and fetal developmental programming of obesity. Reprod. Sci. 2014, 22, 138–145. [Google Scholar] [CrossRef]
- Diego, M.A.; Jones, N.A.; Field, T.; Hernandez-Reif, M.; Schanberg, S.; Kuhn, C.; Gonzalez-Garcia, A. Maternal psychological distress, prenatal cortisol, and fetal weight. Psychosom. Med. 2006, 68, 747–753. [Google Scholar] [CrossRef]
- Zhu, P.; Wang, W.; Zuo, R.; Sun, K. Mechanisms for establishment of the placental glucocorticoid barrier, a guard for life. Cell. Mol. Life Sci. 2018, 76, 13–26. [Google Scholar] [CrossRef]
- Stark, M.J.; Wright, I.M.R.; Clifton, V.L. Sex-specific alterations in placental 11 -hydroxysteroid dehydrogenase 2 activity and early postnatal clinical course following antenatal betamethasone. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 297, R510–R514. [Google Scholar] [CrossRef]
- Limones, M.; Sevillano, J.; Sánchez-Alonso, M.G.; Herrera, E.; Ramos-Álvarez, M.D.P. Metabolic alterations associated with maternal undernutrition during the first half of gestation lead to a diabetogenic state in the rat. Eur. J. Nutr. 2018, 58, 2521–2533. [Google Scholar] [CrossRef]
- Vaughan, O.R.; Sferruzzi-Perri, A.N.; Fowden, A.L. Maternal corticosterone regulates nutrient allocation to fetal growth in mice. J. Physiol. 2012, 590, 5529–5540. [Google Scholar] [CrossRef]
- Toumi, M.L.; Merzoug, S.; Baudin, B.; Tahraoui, A. Quercetin alleviates predator stress-induced anxiety-like and brain oxidative signs in pregnant rats and immune count disturbance in their offspring. Pharmacol. Biochem. Behav. 2013, 107, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chitra, M.; Mathangi, D.C.; Pricilla, J.; Sembulingam, P. Maternal oxidative stress and antioxidant defence during labour. IOSR-JDMS 2015, 14, 10–15. [Google Scholar]
- Kinalski, M.; Śledziewski, A.; Telejko, B.; Zarzycki, W.; Kinalska, I. Lipid peroxidation and scavenging enzyme activity in streptozotocin-induced diabetes. Acta Diabetol. 2000, 37, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, F.G.; Diniz, E.M.D.A.; Kandler, I.; Cianciarullo, M.A.; Dos Santos, N.R. Assessment of oxidative damage and enzymatic antioxidant system activity on the umbilical cord blood and saliva from preterm newborns with risk factors for early-onset neonatal sepsis. Rev. Assoc. Med. Bras. 2018, 64, 888–895. [Google Scholar] [CrossRef]
- Taravati, A.; Taiwan, T.F. Comprehensive analysis of oxidative stress markers and antioxidants status in preeclampsia. Taiwan. J. Obstet. Gynecol. 2018, 57, 779–790. [Google Scholar] [CrossRef]
- Rocha, S.; Gomes, D.; Lima, M.; Bronze-da-Rocha, E.; Sntos-Silva, A. Peroxiredoxin 2, glutathione peroxidase, and catalase in the cytosol and membrane of erythrocytes under H2O2-induced oxidative stress. Free Radic. Res. 2015, 49, 990–1003. [Google Scholar] [CrossRef]
- Fukai, T.; Ushio-Fukai, M. Superoxide dismutases: Role in redox signaling, vascular function, and diseases. Antioxid. Redox Signal. 2011, 15, 1583–1606. [Google Scholar] [CrossRef]
- Bukowski, R.; Smith, G.C.S.; Malone, F.D.; Ball, R.H.; Nyberg, D.A.; Comstock, C.H.; Hankins, G.D.V.; Berkowitz, R.L.; Gross, S.J.; Dugoff, L.; et al. Human sexual size dimorphism in early pregnancy. Am. J. Epidemiol. 2007, 165, 1216–1218. [Google Scholar] [CrossRef]
- Alur, P. Sex differences in nutrition, growth, and metabolism in preterm infants. Front. Pediatr. 2019, 7, 22. [Google Scholar] [CrossRef]
- Mandò, C.; Calabrese, S.; Mazzocco, M.I.; Novielli, C.; Anelli, G.M.; Antonazzo, P.; Cetin, I. Sex specific adaptations in placental biometry of overweight and obese women. Placenta 2016, 38, 1–7. [Google Scholar] [CrossRef]
- Eriksson, J.G.; Kajantie, E.; Osmond, C.; Thornburg, K.; Barker, D.J.P. Boys live dangerously in the womb. Am. J. Hum. Biol. 2010, 22, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Clifton, V.L. Review: Sex and the Human Placenta: Mediating Differential Strategies of Fetal Growth and Survival. Placenta 2010, 31, S33–S39. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.; Zhang, X.; Sieli, P.T.; Falduto, M.T.; Torres, K.E.; Rosenfeld, C.S. Contrasting effects of different maternal diets on sexually dimorphic gene expression in the murine placenta. Proc. Natl. Acad. Sci. USA 2010, 107, 5557–5562. [Google Scholar] [CrossRef] [PubMed]
- Makrydimas, G.; Sotiriadis, A.; Savvidou, M.D.; Spencer, K.; Nicolaides, K.H. Physiological distribution of placental growth factor and soluble Flt-1 in early pregnancy. Prenat. Diagn. 2008, 28, 175–179. [Google Scholar] [CrossRef]
- Malamitsi-Puchner, A.; Boutsikou, T.; Economou, E.; Sarandakou, A.; Makrakis, E.; Hassiakos, D.; Creatsas, G. Vascular endothelial growth factor and placenta growth factor inintrauterine growth-restricted fetuses and neonates. Mediat. Inflamm. 2005, 2005, 293–297. [Google Scholar] [CrossRef]
- Zhao, S.; Zhong, S.; Wang, F.; Wang, H.; Xu, D.; Li, G. Microcystin-LR exposure decreased the fetal weight of mice by disturbance of placental development and ROS-mediated endoplasmic reticulum stress in the placenta. Environ. Pollut. 2020, 256, 113362. [Google Scholar] [CrossRef]
- Hu, C.; Yang, Y.; Li, J.; Wang, H.; Cheng, C.; Yang, L.; Li, Q.; Deng, J.; Liang, Z.; Yin, Y.; et al. Maternal diet-Induced obesity compromises oxidative stress status and angiogenesis in the porcine placenta by upregulating Nox2 expression. Oxid. Med. Cell. Longev. 2019, 2019, 1–13. [Google Scholar] [CrossRef]
- Pereira, R.D.; De Long, N.E.; Wang, R.C.; Yazdi, F.T.; Holloway, A.C.; Raha, S. Angiogenesis in the placenta: The role of reactive oxygen species signaling. BioMed Res. Int. 2015, 2015, 814543. [Google Scholar] [CrossRef]
- Schoots, M.H.; Gordijn, S.J.; Scherjon, S.A.; van Goor, H.; Hillebrands, J.-L. Oxidative stress in placental pathology. Placenta 2018, 69, 153–161. [Google Scholar] [CrossRef]
- Myatt, L.; Cui, X. Oxidative stress in the placenta. Histochem. Cell Biol. 2004, 122, 369–382. [Google Scholar] [CrossRef]
- MacMillan-Crow, L.; Crow, J.; Thompson, J. Peroxynitrite-mediated inactivation of manganese superoxide dismutase involves nitration and oxidation of critical tyrosine residues. Biochemistry 1998, 37, 1613–1622. [Google Scholar] [CrossRef] [PubMed]
- Webster, R.P.; Roberts, V.H.J.; Myatt, L. Protein Nitration in Placenta—Functional Significance. Placenta 2008, 29, 985–994. [Google Scholar] [CrossRef] [PubMed]
- JeŽEk, P.; OlejÁR, T.; SmolkovÁ, K.; JeŽEk, J.; DlaskovÁ, A.; PlecitÁ-HlavatÁ, L.; Zelenka, J.; ŠPaČEk, T.; EngstovÁ, H.; Pajuelo Reguera, D.; et al. Antioxidant and regulatory role of mitochondrial uncoupling protein UCP2 in pancreatic β-cells. Physiol. Res. 2014, 63, S73–S91. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, E.; Aljunaidy, M.M.; Kirschenman, R.; Spaans, F.; Morton, J.S.; Phillips, T.E.J.; Case, C.P.; Cooke, C.-L.M.; Davidge, S.T. Sex-specific effects of nanoparticle-encapsulated MitoQ (nMitoQ) delivery to the placenta in a rat model of fetal hypoxia. Front. Physiol. 2019, 10, 562. [Google Scholar] [CrossRef] [PubMed]
- Aljunaidy, M.M.; Morton, J.S.; Cooke, C.-L.M.; Davidge, S.T. Prenatal hypoxia and placental oxidative stress: Linkages to developmental origins of cardiovascular disease. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2017, 313, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Vega, C.C.; Reyes-Castro, L.A.; Rodríguez-González, G.L.; Bautista, C.J.; Vázquez-Martínez, M.; Larrea, F.; Chamorro-Cevallos, G.A.; Nathanielsz, P.W.; Zambrano, E. Resveratrol partially prevents oxidative stress and metabolic dysfunction in pregnant rats fed a low protein diet and their offspring. J. Physiol. 2016, 594, 1483–1499. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Bhanu, P.T.; Loren, P.T. Sexual dimorphism of mitochondrial function in the hypoxic guinea pig placenta. Biol. Reprod. 2019, 100, 208–216. [Google Scholar]
- Tarrade, A.; Panchenko, P.; Junien, C.; Gabory, A. Placental contribution to nutritional programming of health and diseases: Epigenetics and sexual dimorphism. J. Exp. Biol. 2015, 218, 50–58. [Google Scholar] [CrossRef]
- Marsit, C.J.; Maccani, M.A.; Padbury, J.F.; Lester, B.M. Placental 11-beta hydroxysteroid dehydrogenase methylation is associated with newborn growth and a measure of neurobehavioral outcome. PLoS ONE 2012, 7, e33794. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, P.; de Pablo, A.L.L.; Condezo-Hoyos, L.; Martín-Cabrejas, M.A.; Aguilera, Y.; Ruiz-Hurtado, G.; Gutierrez-Arzapalo, P.Y.; Ramiro-Cortijo, D.; Fernández-Alfonso, M.S.; González, M.D.C.; et al. Fetal undernutrition is associated with perinatal sex-dependent alterations in oxidative status. J. Nutr. Biochem. 2015, 26, 1650–1659. [Google Scholar] [CrossRef]
- Gila-Díaz, A.; Herranz Carrillo, G.; Cañas, S.; Saenz de Pipaón, M.; Martínez-Orgado, J.A.; Rodríguez-Rodríguez, P.; López de Pablo, Á.L.; Martin-Cabrejas, M.A.; Ramiro-Cortijo, D.; Arribas, S.M. Influence of Maternal Age and Gestational Age on Breast Milk Antioxidants During the First Month of Lactation. Nutrients 2020, 12, 2569. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Phuthong, S.; Reyes-Hernández, C.G.; Rodríguez-Rodríguez, P.; Ramiro-Cortijo, D.; Gil-Ortega, M.; González-Blázquez, R.; González, M.C.; López de Pablo, A.L.; Arribas, S.M. Sex Differences in Placental Protein Expression and Efficiency in a Rat Model of Fetal Programming Induced by Maternal Undernutrition. Int. J. Mol. Sci. 2021, 22, 237. https://doi.org/10.3390/ijms22010237
Phuthong S, Reyes-Hernández CG, Rodríguez-Rodríguez P, Ramiro-Cortijo D, Gil-Ortega M, González-Blázquez R, González MC, López de Pablo AL, Arribas SM. Sex Differences in Placental Protein Expression and Efficiency in a Rat Model of Fetal Programming Induced by Maternal Undernutrition. International Journal of Molecular Sciences. 2021; 22(1):237. https://doi.org/10.3390/ijms22010237
Chicago/Turabian StylePhuthong, Sophida, Cynthia Guadalupe Reyes-Hernández, Pilar Rodríguez-Rodríguez, David Ramiro-Cortijo, Marta Gil-Ortega, Raquel González-Blázquez, M. Carmen González, Angel Luis López de Pablo, and Silvia M. Arribas. 2021. "Sex Differences in Placental Protein Expression and Efficiency in a Rat Model of Fetal Programming Induced by Maternal Undernutrition" International Journal of Molecular Sciences 22, no. 1: 237. https://doi.org/10.3390/ijms22010237
APA StylePhuthong, S., Reyes-Hernández, C. G., Rodríguez-Rodríguez, P., Ramiro-Cortijo, D., Gil-Ortega, M., González-Blázquez, R., González, M. C., López de Pablo, A. L., & Arribas, S. M. (2021). Sex Differences in Placental Protein Expression and Efficiency in a Rat Model of Fetal Programming Induced by Maternal Undernutrition. International Journal of Molecular Sciences, 22(1), 237. https://doi.org/10.3390/ijms22010237







