Establishment of a New Device for Electrical Stimulation of Non-Degenerative Cartilage Cells In Vitro
Abstract
:1. Introduction
2. Results
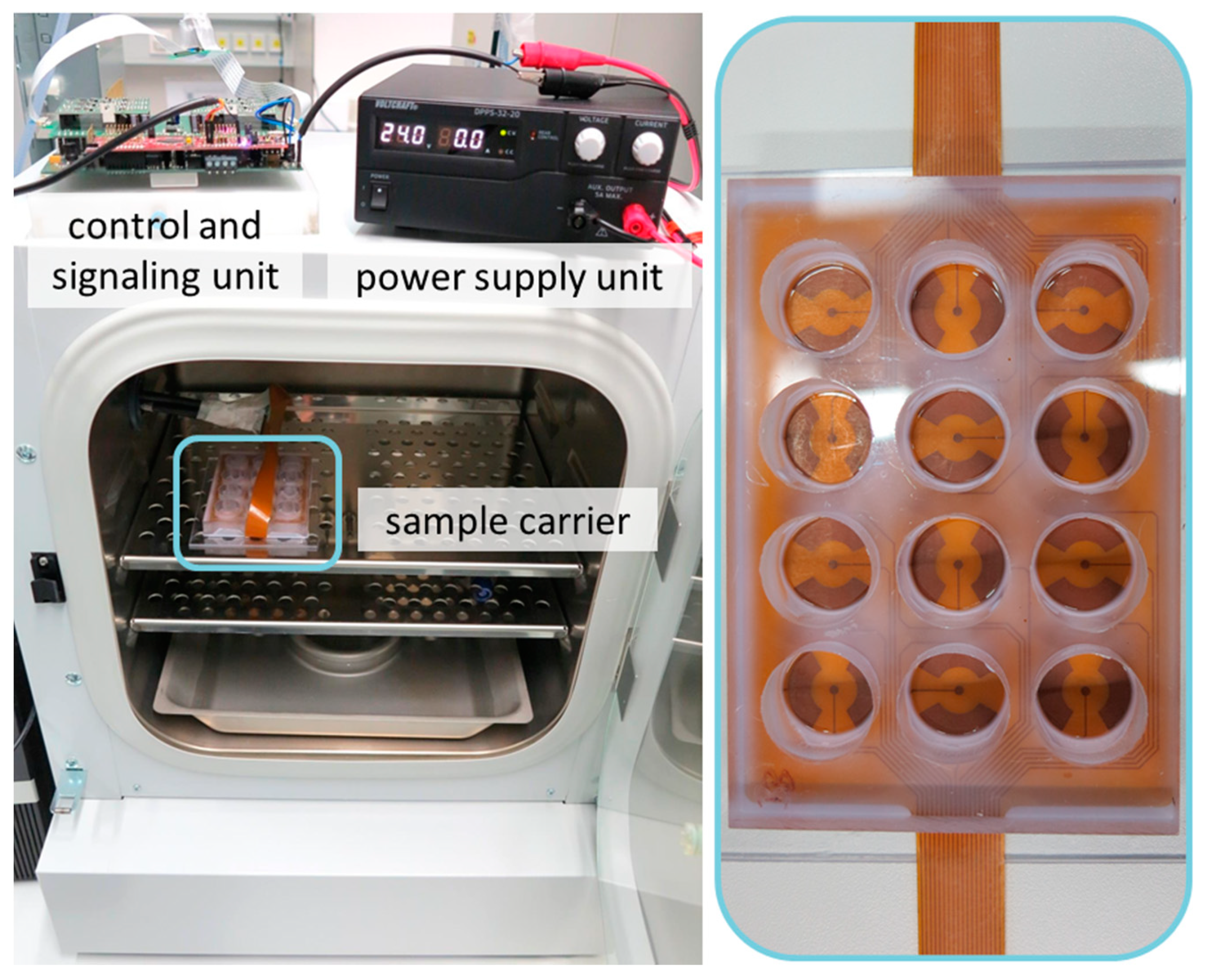
2.1. Stimulation Device
2.1.1. Control Software and User Interface
2.1.2. Control and Signal Unit
2.1.3. Sample Carrier
2.2. Biocompatibility Testing of System Components
2.3. Investigation of Stimulation Parameter
3. Discussion
4. Materials and Methods
4.1. Concept of Electrical Stimulation Device
4.2. Numerical Simulations of Electric Fields Distribution
4.3. Biocompatibiltiy Testing of Stimulation Device Components
4.4. Initial Parameter Analyses
4.4.1. Cellular Activity
4.4.2. Gene Expression Analyses
4.4.3. Protein Synthesis
4.5. Statistics and Data Illustration
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hunziker, E.B.; Quinn, T.M.; Häuselmann, H.-J. Quantitative structural organization of normal adult human articular cartilage. Osteoarthr. Cartil. 2002, 10, 564–572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, S.A.J.; Bedi, A.; Rodeo, S.A. The basic science of articular cartilage: Structure, composition, and function. Sports Health 2009, 1, 461–468. [Google Scholar] [CrossRef]
- Boettcher, K.; Kienle, S.; Nachtsheim, J.; Burgkart, R.; Hugel, T.; Lieleg, O. The structure and mechanical properties of articular cartilage are highly resilient towards transient dehydration. Acta Biomater. 2016, 29, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Buckwalter, J.A.; Mankin, H.J. Articular cartilage: Tissue design and chondrocyte-matrix interactions. Instr. Course Lect. 1998, 47, 477–486. [Google Scholar]
- Van Mow, C.; Guo, X.E. Mechano-electrochemical properties of articular cartilage: Their inhomogeneities and anisotropies. Annu. Rev. Biomed. Eng. 2002, 4, 175–209. [Google Scholar] [CrossRef]
- Carballo, C.B.; Nakagawa, Y.; Sekiya, I.; Rodeo, S.A. Basic Science of Articular Cartilage. Clin. Sports Med. 2017, 36, 413–425. [Google Scholar] [CrossRef]
- Pan, J.; Zhou, X.; Li, W.; Novotny, J.E.; Doty, S.B.; Wang, L. In situ measurement of transport between subchondral bone and articular cartilage. J. Orthop. Res. 2009, 27, 1347–1352. [Google Scholar] [CrossRef] [Green Version]
- Schmidt-Rohlfing, B.; Schneider, U.; Goost, H.; Silny, J. Mechanically induced electrical potentials of articular cartilage. J. Biomech. 2002, 35, 475–482. [Google Scholar] [CrossRef]
- Mow, V.C.; Wang, C.C.; Hung, C.T. The extracellular matrix, interstitial fluid and ions as a mechanical signal transducer in articular cartilage. Osteoarthr. Cartil. 1999, 7, 41–58. [Google Scholar] [CrossRef] [Green Version]
- Wan, L.Q.; Miller, C.; Guo, X.E.; van Mow, C. Fixed electrical charges and mobile ions affect the measurable mechano-electrochemical properties of charged-hydrated biological tissues: The articular cartilage paradigm. Mech. Chem. Biosyst. 2004, 1, 81–99. [Google Scholar]
- Xu, J.; Wang, W.; Clark, C.C.; Brighton, C.T. Signal transduction in electrically stimulated articular chondrocytes involves translocation of extracellular calcium through voltage-gated channels. Osteoarthr. Cartil. 2009, 17, 397–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, X.L.; Wan, L.Q.; Guo, X.E.; van Mow, C. A linearized formulation of triphasic mixture theory for articular cartilage, and its application to indentation analysis. J. Biomech. 2010, 43, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Vaca-González, J.J.; Guevara, J.M.; Moncayo, M.A.; Castro-Abril, H.; Hata, Y.; Garzón-Alvarado, D.A. Biophysical Stimuli: A Review of Electrical and Mechanical Stimulation in Hyaline Cartilage. Cartilage 2017, 1947603517730637. [Google Scholar] [CrossRef] [PubMed]
- Brighton, C.T.; Jensen, L.; Pollack, S.R.; Tolin, B.S.; Clark, C.C. Proliferative and synthetic response of bovine growth plate chondrocytes to various capacitively coupled electrical fields. J. Orthop. Res. 1989, 7, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Brighton, C.T.; Wang, W.; Clark, C.C. Up-regulation of matrix in bovine articular cartilage explants by electric fields. Biochem. Biophys. Res. Commun. 2006, 342, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Brighton, C.T.; Wang, W.; Clark, C.C. The effect of electrical fields on gene and protein expression in human osteoarthritic cartilage explants. J. Bone Joint Surg. Am. 2008, 90, 833–848. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.C.; Wang, W.; Brighton, C.T. Up-regulation of expression of selected genes in human bone cells with specific capacitively coupled electric fields. J. Orthop. Res. 2014, 32, 894–903. [Google Scholar] [CrossRef]
- Vaca-González, J.J.; Escobar, J.F.; Guevara, J.M.; Hata, Y.A.; Gallego Ferrer, G.; Garzón-Alvarado, D.A. Capacitively coupled electrical stimulation of rat chondroepiphysis explants: A histomorphometric analysis. Bioelectrochemistry 2019, 126, 1–11. [Google Scholar] [CrossRef]
- Chao, P.H.; Roy, R.; Mauck, R.L.; Liu, W.; Valhmu, W.B.; Hung, C.T. Chondrocyte translocation response to direct current electric fields. J. Biomech. Eng. 2000, 122, 261–267. [Google Scholar] [CrossRef]
- Rohde, M.; Ziebart, J.; Kirschstein, T.; Sellmann, T.; Porath, K.; Kühl, F.; Delenda, B.; Bahls, C.; van Rienen, U.; Bader, R.; et al. Human Osteoblast Migration in DC Electrical Fields Depends on Store Operated Ca2+-Release and Is Correlated to Upregulation of Stretch-Activated TRPM7 Channels. Front. Bioeng. Biotechnol. 2019, 7, 422. [Google Scholar] [CrossRef] [Green Version]
- Buckwalter, J.A.; Roughley, P.J.; Rosenberg, L.C. Age-related changes in cartilage proteoglycans: Quantitative electron microscopic studies. Microsc. Res. Tech. 1994, 28, 398–408. [Google Scholar] [CrossRef]
- Mollon, B.; Kandel, R.; Chahal, J.; Theodoropoulos, J. The clinical status of cartilage tissue regeneration in humans. Osteoarthr. Cartil. 2013, 21, 1824–1833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makris, E.A.; Gomoll, A.H.; Malizos, K.N.; Hu, J.C.; Athanasiou, K.A. Repair and tissue engineering techniques for articular cartilage. Nat. Rev. Rheumatol. 2015, 11, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.J.; Hu, J.C.; Athanasiou, K.A. Cell-based tissue engineering strategies used in the clinical repair of articular cartilage. Biomaterials 2016, 98, 1–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brittberg, M.; Lindahl, A.; Nilsson, A.; Ohlsson, C.; Isaksson, O.; Peterson, L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N. Engl. J. Med. 1994, 331, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Moreira-Teixeira, L.S.; Georgi, N.; Leijten, J.; Wu, L.; Karperien, M. Cartilage tissue engineering. Endocr. Dev. 2011, 21, 102–115. [Google Scholar] [CrossRef]
- Gomoll, A.H.; Minas, T. The quality of healing: Articular cartilage. Wound Repair Regen. 2014, 22 (Suppl. 1), 30–38. [Google Scholar] [CrossRef]
- Huey, D.J.; Hu, J.C.; Athanasiou, K.A. Unlike bone, cartilage regeneration remains elusive. Science 2012, 338, 917–921. [Google Scholar] [CrossRef] [Green Version]
- Armiento, A.R.; Alini, M.; Stoddart, M.J. Articular fibrocartilage—Why does hyaline cartilage fail to repair? Adv. Drug Deliv. Rev. 2019, 146, 289–305. [Google Scholar] [CrossRef]
- Huang, X.; Das, R.; Patel, A.; Nguyen, T.D. Physical Stimulations for Bone and Cartilage Regeneration. Regen. Eng. Transl. Med. 2018, 4, 216–237. [Google Scholar] [CrossRef]
- Wang, W.; Wang, Z.; Zhang, G.; Clark, C.C.; Brighton, C.T. Up-regulation of chondrocyte matrix genes and products by electric fields. Clin. Orthop. Relat. Res. 2004, S163–S173. [Google Scholar] [CrossRef] [PubMed]
- Balint, R.; Cassidy, N.J.; Cartmell, S.H. Electrical stimulation: A novel tool for tissue engineering. Tissue Eng. Part B Rev. 2013, 19, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Vaca-González, J.J.; Guevara, J.M.; Vega, J.F.; Garzón-Alvarado, D.A. An In Vitro Chondrocyte Electrical Stimulation Framework: A Methodology to Calculate Electric Fields and Modulate Proliferation, Cell Death and Glycosaminoglycan Synthesis. Cel. Mol. Bioeng. 2016, 9, 116–126. [Google Scholar] [CrossRef]
- Vavken, P.; Arrich, F.; Schuhfried, O.; Dorotka, R. Effectiveness of pulsed electromagnetic field therapy in the management of osteoarthritis of the knee: A meta-analysis of randomized controlled trials. J. Rehabil. Med. 2009, 41, 406–411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fioravanti, A.; Nerucci, F.; Collodel, G.; Markoll, R.; Marcolongo, R. Biochemical and morphological study of human articular chondrocytes cultivated in the presence of pulsed signal therapy. Ann. Rheum. Dis. 2002, 61, 1032–1033. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ongaro, A.; Pellati, A.; Masieri, F.F.; Caruso, A.; Setti, S.; Cadossi, R.; Biscione, R.; Massari, L.; Fini, M.; de Mattei, M. Chondroprotective effects of pulsed electromagnetic fields on human cartilage explants. Bioelectromagnetics 2011, 32, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Thrivikraman, G.; Boda, S.K.; Basu, B. Unraveling the mechanistic effects of electric field stimulation towards directing stem cell fate and function: A tissue engineering perspective. Biomaterials 2018, 150, 60–86. [Google Scholar] [CrossRef]
- Krueger, S.; Achilles, S.; Zimmermann, J.; Tischer, T.; Bader, R.; Jonitz-Heincke, A. Re-Differentiation Capacity of Human Chondrocytes in Vitro Following Electrical Stimulation with Capacitively Coupled Fields. J. Clin. Med. 2019, 8, 1771. [Google Scholar] [CrossRef] [Green Version]
- Hiemer, B.; Krogull, M.; Bender, T.; Ziebart, J.; Krueger, S.; Bader, R.; Jonitz-Heincke, A. Effect of electric stimulation on human chondrocytes and mesenchymal stem cells under normoxia and hypoxia. Mol. Med. Rep. 2018, 18, 2133–2141. [Google Scholar] [CrossRef] [Green Version]
- Taghian, T.; Narmoneva, D.A.; Kogan, A.B. Modulation of cell function by electric field: A high-resolution analysis. J. R. Soc. Interface 2015, 12. [Google Scholar] [CrossRef]
- Armstrong, P.F.; Brighton, C.T.; Star, A.M. Capacitively coupled electrical stimulation of bovine growth plate chondrocytes grown in pellet form. J. Orthop. Res. 1988, 6, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Brighton, C.T.; Unger, A.S.; Stambough, J.L. In vitro growth of bovine articular cartilage chondrocytes in various capacitively coupled electrical fields. J. Orthop. Res. 1984, 2, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Brighton, C.T.; Townsend, P.F. Increased cAMP production after short-term capacitively coupled stimulation in bovine growth plate chondrocytes. J. Orthop. Res. 1988, 6, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Bader, R.; Bender, T.; Jonitz-Heincke, A.; Seitz, H.; Lieberwirth, C.; Riess, A. Vorrichtung zur Elektrischen und Mechanischen Stimulation von Gewebeproben. Published patent application DE 10 2018 114 019 A1, 12 December 2019. [Google Scholar]
- Foldager, C.B.; Nielsen, A.B.; Munir, S.; Ulrich-Vinther, M.; Søballe, K.; Bünger, C.; Lind, M. Combined 3D and hypoxic culture improves cartilage-specific gene expression in human chondrocytes. Acta Orthop. 2011, 82, 234–240. [Google Scholar] [CrossRef]
- Hiemer, B.; Ziebart, J.; Jonitz-Heincke, A.; Grunert, P.C.; Su, Y.; Hansmann, D.; Bader, R. Magnetically induced electrostimulation of human osteoblasts results in enhanced cell viability and osteogenic differentiation. Int. J. Mol. Med. 2016, 38, 57–64. [Google Scholar] [CrossRef]
- Blume, G.; Müller-Wichards, W.; Goepfert, C.; Pörtner, R.; Müller, J. Electrical Stimulation of NIH-3T3 Cells with Platinum-PEDOT-Electrodes Integrated in a Bioreactor. Open Biomed. Eng. J. 2013, 7, 125–132. [Google Scholar] [CrossRef] [Green Version]
- He, X.; Li, L.; Tang, M.; Zeng, Y.; Li, H.; Yu, X. Biomimetic electrical stimulation induces rat bone marrow mesenchymal stem cells to differentiate into cardiomyocyte-like cells via TGF-beta 1 in vitro. Prog. Biophys. Mol. Biol. 2019, 148, 47–53. [Google Scholar] [CrossRef]
- Mobini, S.; Leppik, L.; Thottakkattumana Parameswaran, V.; Barker, J.H. In vitro effect of direct current electrical stimulation on rat mesenchymal stem cells. PeerJ 2017, 5, e2821. [Google Scholar] [CrossRef] [Green Version]
- Yow, S.-Z.; Lim, T.H.; Yim, E.K.F.; Lim, C.T.; Leong, K.W. A 3D Electroactive Polypyrrole-Collagen Fibrous Scaffold for Tissue Engineering. Polymers 2011, 3, 527–544. [Google Scholar] [CrossRef] [Green Version]
- Marotta, M.; Bragós, R.; Gómez-Foix, A.M. Design and performance of an electrical stimulator for long-term contraction of cultured muscle cells. Biotechniques 2004, 36, 68–73. [Google Scholar] [CrossRef] [Green Version]
- Benya, P.D.; Shaffer, J.D. Dedifferentiated chondrocytes reexpress the differentiated collagen phenotype when cultured in agarose gels. Cell 1982, 30, 215–224. [Google Scholar] [CrossRef]
- Lin, Z.; Fitzgerald, J.B.; Xu, J.; Willers, C.; Wood, D.; Grodzinsky, A.J.; Zheng, M.H. Gene expression profiles of human chondrocytes during passaged monolayer cultivation. J. Orthop. Res. 2008, 26, 1230–1237. [Google Scholar] [CrossRef] [PubMed]
- Tuan, R.S.; Chen, A.F.; Klatt, B.A. Cartilage regeneration. J. Am. Acad. Orthop. Surg. 2013, 21, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Niemeyer, P.; Albrecht, D.; Andereya, S.; Angele, P.; Ateschrang, A.; Aurich, M.; Baumann, M.; Bosch, U.; Erggelet, C.; Fickert, S.; et al. Autologous chondrocyte implantation (ACI) for cartilage defects of the knee: A guideline by the working group "Clinical Tissue Regeneration" of the German Society of Orthopaedics and Trauma (DGOU). Knee 2016, 23, 426–435. [Google Scholar] [CrossRef] [Green Version]
- Brighton, C.T.; Okereke, E.; Pollack, S.R.; Clark, C.C. In vitro bone-cell response to a capacitively coupled electrical field. The role of field strength, pulse pattern, and duty cycle. Clin. Orthop. Relat. Res. 1992, 285, 255–262. [Google Scholar]
- Vázquez-Portalatı, N.N.; Kilmer, C.E.; Panitch, A.; Liu, J.C. Characterization of Collagen Type I and II Blended Hydrogels for Articular Cartilage Tissue Engineering. Biomacromolecules 2016, 17, 3145–3152. [Google Scholar] [CrossRef] [Green Version]
- Tiruvannamalai Annamalai, R.; Mertz, D.R.; Daley, E.L.H.; Stegemann, J.P. Collagen Type II enhances chondrogenic differentiation in agarose-based modular microtissues. Cytotherapy 2016, 18, 263–277. [Google Scholar] [CrossRef] [Green Version]
- Barbero, A.; Ploegert, S.; Heberer, M.; Martin, I. Plasticity of clonal populations of dedifferentiated adult human articular chondrocytes. Arthritis Rheum. 2003, 48, 1315–1325. [Google Scholar] [CrossRef]
- Leijten, J.C.H.; Georgi, N.; Wu, L.; van Blitterswijk, C.A.; Karperien, M. Cell sources for articular cartilage repair strategies: Shifting from monocultures to cocultures. Tissue Eng. Part B Rev. 2013, 19, 31–40. [Google Scholar] [CrossRef]
- Deszcz, I.; Lis-Nawara, A.; Grelewski, P.; Dragan, S.; Bar, J. Utility of direct 3D co-culture model for chondrogenic differentiation of mesenchymal stem cells on hyaluronan scaffold (Hyaff-11). Regen. Biomater. 2020. [Google Scholar] [CrossRef]
- Mardani, M.; Roshankhah, S.; Hashemibeni, B.; Salahshoor, M.; Naghsh, E.; Esfandiari, E. Induction of chondrogenic differentiation of human adipose-derived stem cells by low frequency electric field. Adv. Biomed. Res. 2016, 5, 97. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.J.; Lee, G.S.; Chun, H. Electrical stimulation drives chondrogenesis of mesenchymal stem cells in the absence of exogenous growth factors. Sci. Rep. 2016, 6, 39302. [Google Scholar] [CrossRef] [PubMed]





| Metabolic Activity (OD) | Col1A1 (%) | CICP Protein (ng/mg) | Sox9 (%) | CIICP Protein (ng/mg) | ||
|---|---|---|---|---|---|---|
| control | 0.457 ± 0.123 | 101.3 ± 15.9 | 766.1 ± 184.2 | 101.1 ± 16.2 | 105.1 ± 29.7 | |
| 5 Vpp | 1 kHz | 0.416 ± 0.124 | 90.7 ± 16.9 | 485.7 ± 47.5 # | 88.8 ± 7.4 | 86.5 ± 36.2 |
| 60 kHz | 0.427 ± 0.044 | 114.0 ± 17.8 | 867.0 ± 340.3 | 108.0 ± 18.6 | 79.2 ± 21.7 | |
| 10 Vpp | 1 kHz | 0.342 ± 0.097 | 85.7 ± 3.3 | 481.3 ± 75.1 * | 90.2 ± 25.1 | 91.3 ± 25.1 |
| 60 kHz | 0.401 ± 0.052 | 99.0 ± 13.5 | 752.7 ± 173.0 | 98.8 ± 14.9 | 107.8 ± 28.6 | |
| 20 Vpp | 1 kHz | 0.324 ± 0.116 | 92.7 ± 23.3 | 492.4 ± 47.2 # | 98.2 ± 10.8 | 82.0 ± 29.3 |
| 60 kHz | 0.383 ± 0.038 | 101.0 ± 16.6 | 881.0 ± 243.4 | 109.2 ± 24.9 | 78.9 ± 32.5 | |
| 30 Vpp | 1 kHz | 0.357 ± 0.107 | 92.2 ± 21.9 | 566.5 ± 83.9 | 104.0 ± 11.5 | 96.7 ± 17.5 |
| 60 kHz | 0.450 ± 0.063 | 89.2 ± 15.2 | 899.1 ± 125.2 | 93.2 ± 21.8 | 93.3 ± 17.9 | |
| Material | Conductivity [S/m] σ | Relative Permittivity ε |
|---|---|---|
| Air | 10 × 10−15 | 1 |
| Cell medium | 1.5 | 80 |
| Electrodes (copper) | 5.998 × 107 | 1 |
| Insulation layer (polyimide) | 1 × 10−10 | 3.4 |
| Applied Frequency (kHz) | Applied Voltage (Vpp) | Electric Field Affecting Cells (Approximately) (V/m) |
|---|---|---|
| 1 | 5 | 0.004–0.006 |
| 1 | 10 | 0.010–0.012 |
| 1 | 20 | 0.022–0.026 |
| 1 | 30 | 0.032–0.040 |
| 60 | 5 | 0.3–0.4 |
| 60 | 10 | 0.6–0.8 |
| 60 | 20 | 1.3–1.6 |
| 60 | 30 | 2.0–2.5 |
| Gene | Primer Sequence | Description/Function | |
|---|---|---|---|
| β-Actin (ACTB) | forward | 5′-CTTCCTGGGCATGGAGTC-3′ | Housekeeping gene |
| reverse | 5′-AGCACTGTGTTGGCGTACAG-3′ | ||
| Collagen I (Col1A1) | forward | 5′-ACGAAGACATCCCACCAATC-3′ | De-differentiation marker |
| reverse | 5′-ACGAAGACATCCCACCAATC-3′ | ||
| Collagen II (Col2A1) | forward | 5′-AATGGTGGCTTCCATTCAG-3′ | Main macromolecule of the ECM of cartilaginous tissue |
| reverse | 5′-GTGATGTTCTGGGAGCCTTC-3′ | ||
| SRY-box 9 (Sox9) | forward | 5′-AGTACCCGCACCTGCACAAC-3′ | Transcriptional factor mediating chondrocytes phenotype and cartilage homeostasis |
| reverse | 5′-CGCTTCTCGCTCTCGTTCAG-3′ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krueger, S.; Riess, A.; Jonitz-Heincke, A.; Weizel, A.; Seyfarth, A.; Seitz, H.; Bader, R. Establishment of a New Device for Electrical Stimulation of Non-Degenerative Cartilage Cells In Vitro. Int. J. Mol. Sci. 2021, 22, 394. https://doi.org/10.3390/ijms22010394
Krueger S, Riess A, Jonitz-Heincke A, Weizel A, Seyfarth A, Seitz H, Bader R. Establishment of a New Device for Electrical Stimulation of Non-Degenerative Cartilage Cells In Vitro. International Journal of Molecular Sciences. 2021; 22(1):394. https://doi.org/10.3390/ijms22010394
Chicago/Turabian StyleKrueger, Simone, Alexander Riess, Anika Jonitz-Heincke, Alina Weizel, Anika Seyfarth, Hermann Seitz, and Rainer Bader. 2021. "Establishment of a New Device for Electrical Stimulation of Non-Degenerative Cartilage Cells In Vitro" International Journal of Molecular Sciences 22, no. 1: 394. https://doi.org/10.3390/ijms22010394
APA StyleKrueger, S., Riess, A., Jonitz-Heincke, A., Weizel, A., Seyfarth, A., Seitz, H., & Bader, R. (2021). Establishment of a New Device for Electrical Stimulation of Non-Degenerative Cartilage Cells In Vitro. International Journal of Molecular Sciences, 22(1), 394. https://doi.org/10.3390/ijms22010394






