Accurate Molecular Diagnosis of Gaucher Disease Using Clinical Exome Sequencing as a First-Tier Test
Abstract
1. Introduction
2. Results
2.1. Clinical Exome Sequencing (CES) and Variant Identification
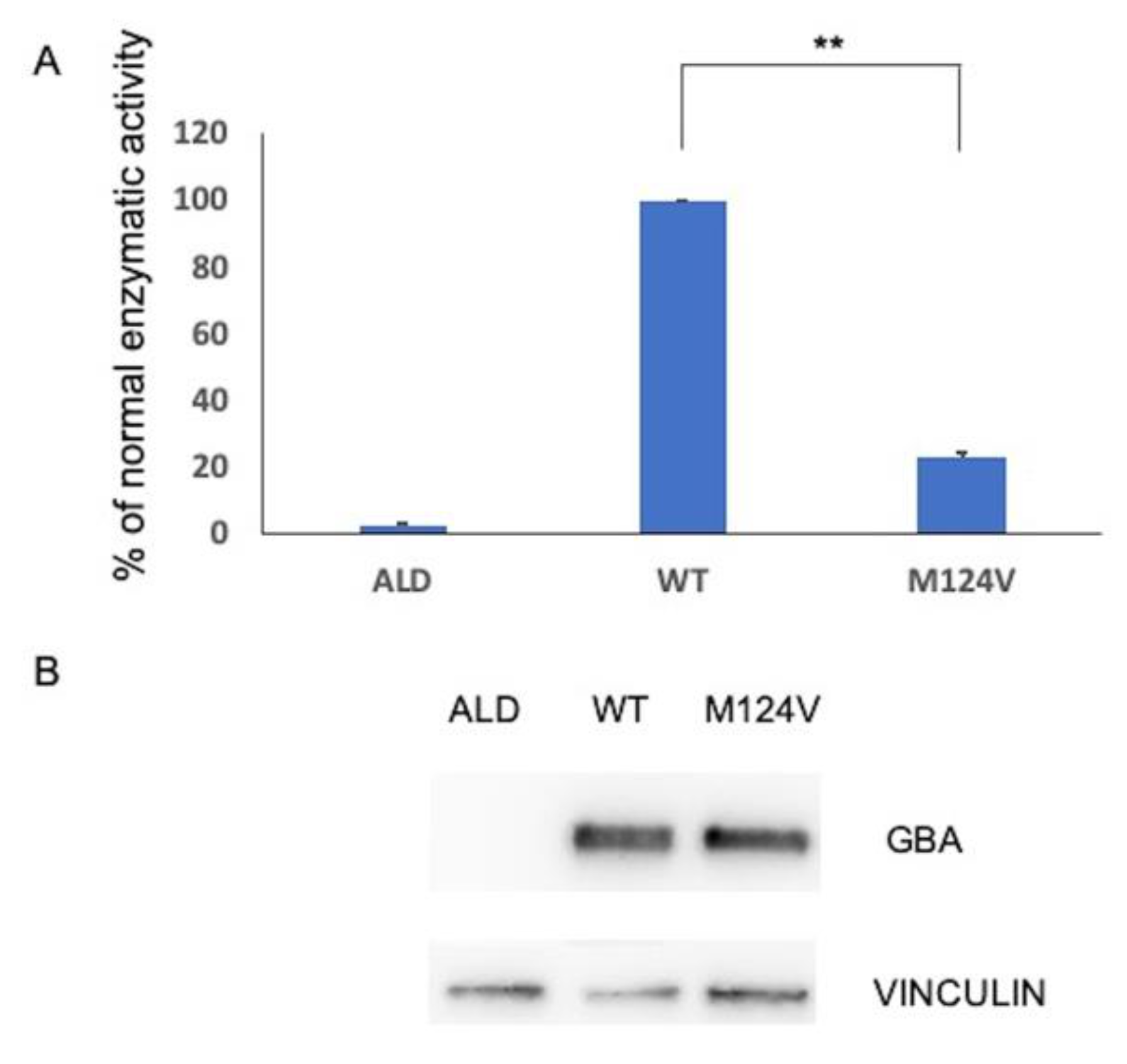
2.2. Functional Analysis of p.M124V (M85V) Variant
3. Discussion
4. Materials and Methods
4.1. Samples
4.2. Molecular Analysis
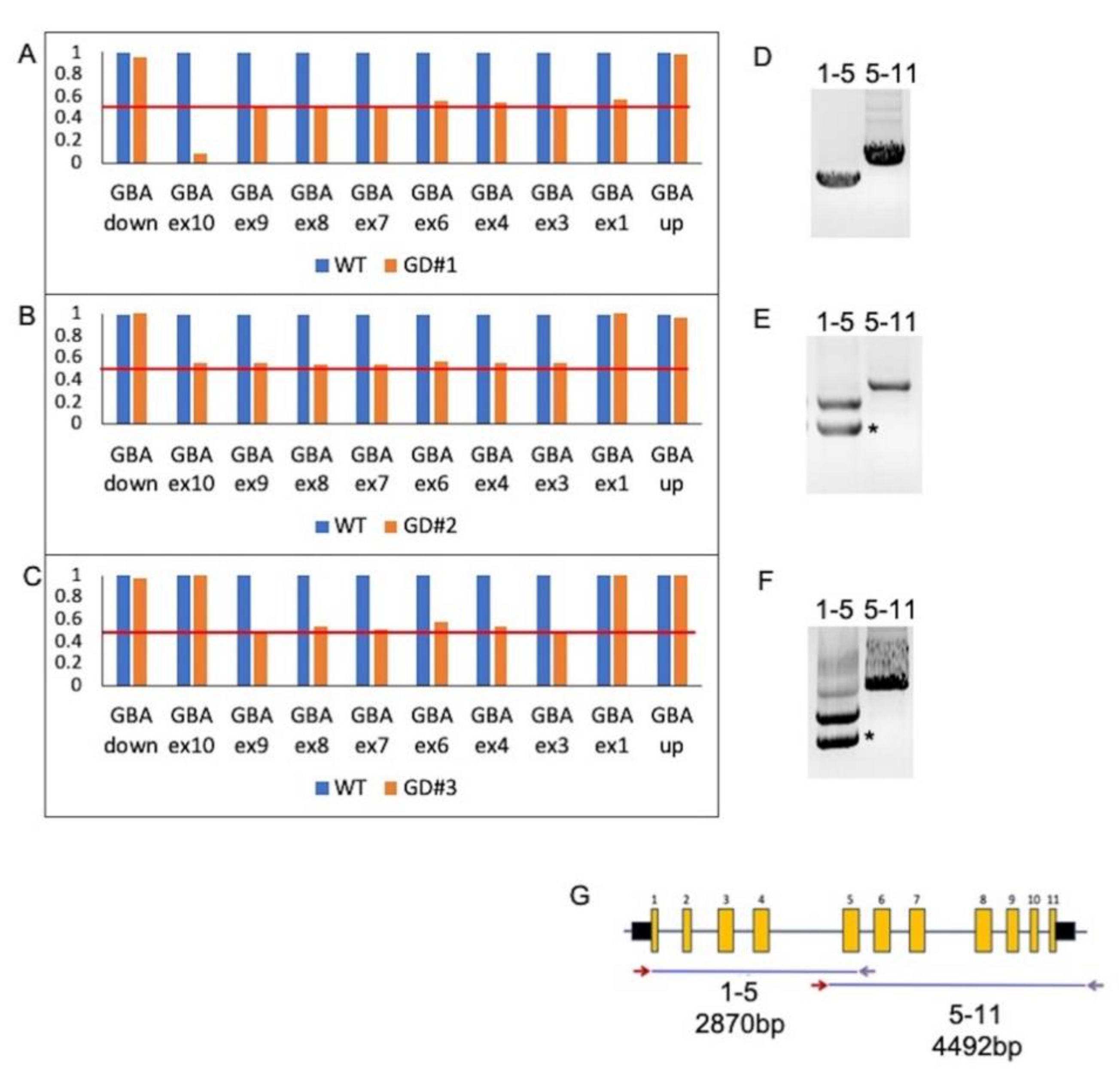
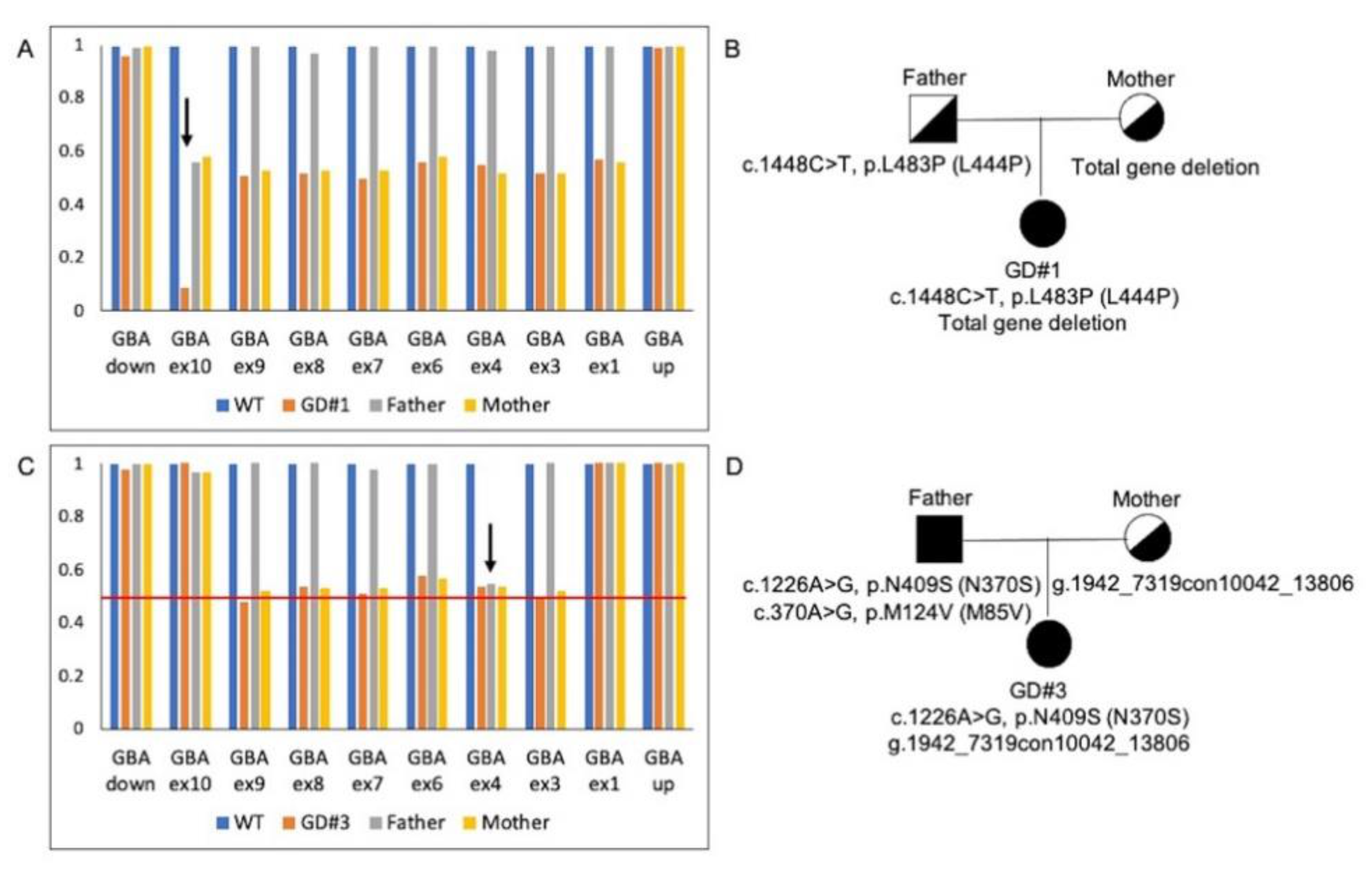
4.3. Multiplex Ligation-Dependent Probe Amplification (MLPA) Analysis of GBA Gene
4.4. Mutation Nomenclature
4.5. Site-Directed Mutagenesis
4.6. Cell Culture and Transient Transfection
4.7. Enzyme Activity Assay
4.8. Western Blotting Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Beutler, E.; Grabowski, G.A. Gaucher disease. In The Metabolic and Molecular Basis of Inherited Disease; Scriver, C.R., Beaudet, A.L., Valle, D., Sly, W.S., Eds.; McGraw-Hill: New York, NY, USA, 2001; pp. 3635–3668. [Google Scholar]
- Eblan, M.J.; Walker, J.M.; Sidransky, E. The glucocerebrosidase gene and Parkinson’s disease in Ashkenazi Jews. N. Engl. J. Med. 2005, 352, 728–731. [Google Scholar] [PubMed]
- Sato, C.; Morgan, A.; Lang, A.E.; Salehi-Rad, S.; Kawarai, T.; Meng, Y.; Ray, P.N.; Farrer, L.A.; St George-Hyslop, P.; Rogaeva, E. Analysis of the glucocerebrosidase gene in Parkinson’s disease. Mov. Disord. 2005, 20, 367–370. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.N.; Ross, B.M.; Wang, Y.; Mejia-Santana, H.; Harris, J.; Louis, E.D.; Cote, L.J.; Andrews, H.; Fahn, S.; Waters, C.; et al. Mutations in the glucocerebrosidase gene are associated with early-onset Parkinson disease. Neurology 2007, 69, 1270–1277. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.R.; Chen, C.M.; Chao, C.Y.; Ro, L.S.; Lyu, R.K.; Chang, K.H.; Lee-Chen, G.J. Glucocerebrosidase gene mutation is a risk factor for early onset of Parkinson disease among Taiwanese. J. Neurol. Neurosurg. Psychiatry 2007, 78, 977–979. [Google Scholar] [CrossRef]
- Gan-Or, Z.; Giladi, N.; Rozovski, U.; Shifrin, C.; Rosner, S.; Gurevich, T.; Bar-Shira, A.; Orr-Urtreger, A. Genotype–phenotype correlations between GBA mutations and Parkinson disease risk and onset. Neurology 2008, 70, 2277–2283. [Google Scholar] [CrossRef]
- Ryan, E.; Seehra, G.; Sharma, P.; Sidransky, E. GBA1-associated parkinsonism: New insights and therapeutic opportunities. Curr. Opin. Neurol. 2019, 32, 589–596. [Google Scholar] [CrossRef]
- Winfield, S.L.; Tayebi, N.; Martin, B.M.; Ginns, E.I.; Sidransky, E. Identification of three additional genes contiguous to the glucocerebrosidase locus on chromosome 1q21: Implications for Gaucher disease. Genome Res. 1997, 7, 1020–1026. [Google Scholar] [CrossRef][Green Version]
- Long, G.L.; Winfield, S.; Adolph, K.W.; Ginns, E.I.; Bornstein, P. Structure and organization of the human metaxin gene (MTX) and pseudogene. Genomics 1996, 33, 177–184. [Google Scholar] [CrossRef]
- Horowitz, M.; Wilder, S.; Horowitz, Z.; Reiner, O.; Gelbart, T.; Beutler, E. The human glucocerebrosidase gene and pseudogene: Structure and evolution. Genomics 1989, 4, 87e96. [Google Scholar] [CrossRef]
- Hong, C.M.; Ohashi, T.; Yu, X.J.; Weiler, S.; Barranger, J.A. Sequence of two alleles responsible for Gaucher disease. DNA Cell Biol. 1990, 9, 233e241. [Google Scholar] [CrossRef]
- Latham, T.E.; Theophilus, B.D.; Grabowski, G.A.; Smith, F.I. Heterogeneity of mutations in the acid beta-glucosidase gene of Gaucher disease patients. DNA Cell Biol. 1991, 10, 15e21. [Google Scholar] [CrossRef]
- Eyal, N.; Wilder, S.; Horowitz, M. Prevalent and rare mutations among Gaucher patients. Gene 1990, 96, 277–283. [Google Scholar] [CrossRef]
- Torralba, M.A.; Alfonso, P.; Pérez-Calvo, J.I.; Cenarro, A.; Pastores, G.M.; Giraldo, P.; Civeira, F.; Pocoví, M. High prevalence of the 55-bp deletion (c.1263del55) in exon 9 of the glucocerebrosidase gene causing misdiagnosis (for homozygous N370S (c.1226A>G) mutation) in Spanish Gaucher disease patients. Blood Cells Mol. Dis. 2002, 29, 35e40. [Google Scholar] [CrossRef]
- Filocamo, M.; Mazzotti, R.; Stroppiano, M.; Seri, M.; Giona, F.; Parenti, G.; Regis, S.; Corsolini, F.; Zoboli, S.; Gatti, R. Analysis of the glucocerebrosidase gene and mutation profile in 144 Italian gaucher patients. Hum. Mutat. 2002, 20, 234–235. [Google Scholar] [CrossRef]
- Beutler, E.; Gelbart, T. Erroneous assignment of Gaucher disease genotype as a consequence of a complete gene deletion. Hum. Mutat. 1994, 4, 212–216. [Google Scholar] [CrossRef]
- Cozar, M.; Bembi, B.; Dominissini, S.; Zampieri, S.; Vilageliu, L.; Grinberg, D.; Dardis, A. Molecular characterization of a new deletion of the GBA1 gene due to an inter Alu recombination event. Mol. Genet. Metab. 2011, 102, 226–228. [Google Scholar] [CrossRef]
- Ichinose, Y.; Ishiura, H.; Tanaka, M.; Yoshimura, J.; Doi, K.; Umeda, T.; Yamauchi, H.; Tsuchiya, M.; Koh, K.; Yamashiro, N.; et al. Neuroimaging, genetic, and enzymatic study in a Japanese family with a GBA gross deletion. Parkinsonism Relat. Disord. 2019, 61, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Deignan, J.L.; Dorrani, N.; Strom, S.P.; Kantarci, S.; Quintero-Rivera, F.; Das, K.; Toy, T.; Harry, B.; Yourshaw, M.; et al. Clinical exome sequencing for genetic identification of rare Mendelian disorders. JAMA 2014, 312, 1880–1887. [Google Scholar] [CrossRef]
- Coonrod, E.M.; Durtschi, J.D.; Margraf, R.L.; Voelkerding, K.V. Developing genome and exome sequencing for candidate gene identification in inherited disorders: An integrated technical and bioinformatics approach. Arch. Pathol. Lab. Med. 2013, 137, 415–433. [Google Scholar] [CrossRef]
- Zampieri, S.; Cattarossi, S.; Bembi, B.; Dardis, A. GBA Analysis in Next-Generation Era: Pitfalls, Challenges, and Possible Solutions. J. Mol. Diagn. 2017, 19, 33–741. [Google Scholar] [CrossRef]
- Lee, C.Y.; Yen, H.Y.; Zhong, A.W.; Gao, H. Resolving misalignment interference for NGS-based clinical diagnostics. Hum. Genet. 2021, 140, 477–492. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Dai, H.; Feng, Y.; Tang, J.; Chen, S.; Tian, X.; Gorman, E.; Schmitt, E.S.; Hansen, T.A.; Wang, J.; et al. A Comprehensive Strategy for Accurate Mutation Detection of the Highly Homologous PMS2. J. Mol. Diagn. 2015, 17, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Miocic, S.; Filocamo, M.; Dominissini, S.; Montalvo, A.L.; Vlahovicek, K.; Deganuto, M.; Mazzotti, R.; Cariati, R.; Bembi, B.; Pittis, M.G. Identification and functional characterization of five novel mutant alleles in 58 Italian patients with Gaucher disease type 1. Hum. Mutat. 2005, 25, 100. [Google Scholar] [CrossRef] [PubMed]
- Amico, G.; Grossi, S.; Vijzelaar, R.; Lanza, F.; Mazzotti, R.; Corsolini, F.; Ketema, M.; Filocamo, M. MLPA-based approach for initial and simultaneous detection of GBA deletions and recombinant alleles in patients affected by Gaucher Disease. Mol. Genet. Metab. 2016, 119, 329–337. [Google Scholar] [CrossRef]
- Pavan, E.; Ormazabal, M.; Peruzzo, P.; Vaena, E.; Rozenfeld, P.; Dardis, A. CRISPR/Cas9 Editing for Gaucher Disease Modelling. Int. J. Mol. Sci. 2020, 21, 3268. [Google Scholar] [CrossRef]
- Boot, R.G.; Renkema, G.H.; Verhoek, M.; Strijland, A.; Bliek, J.; de Meulemeester, T.M.; Mannens, M.M.; Aerts, J.M. The human chitotriosidase gene. Nature of inherited enzyme deficiency. J. Biol. Chem. 1998, 273, 25680–25685. [Google Scholar] [CrossRef]
- Koprivica, V.; Stone, D.L.; Park, J.K.; Callahan, M.; Frisch, A.; Cohen, I.J.; Tayebi, N.; Sidransky, E. Analysis and classification of 304 mutant alleles in patients with type 1 and type 3 Gaucher disease. Am. J. Hum. Genet. 2000, 66, 1777–1786. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.Y.; Kim, S.J.; Yang, J.A.; Hong, J.H.; Lee, S.J.; Kim, H.J. Identification of a novel recombinant mutation in Korean patients with Gaucher disease using a long-range PCR approach. J. Hum. Genet. 2011, 56, 469–471. [Google Scholar] [CrossRef]
- Siebert, M.; Bock, H.; Michelin-Tirelli, K.; Coelho, J.C.; Giugliani, R.; Saraiva-Pereira, M.L. Novel mutations in the glucocerebrosidase gene of brazilian patients with Gaucher disease. JIMD Rep. 2013, 9, 7–16. [Google Scholar]
- Yoshida, S.; Kido, J.; Matsumoto, S.; Momosaki, K.; Mitsubuchi, H.; Shimazu, T.; Sugawara, K.; Endo, F.; Nakamura, K. Prenatal diagnosis of Gaucher disease using next-generation sequencing. Pediatr. Int. 2016, 58, 946–949. [Google Scholar] [CrossRef]
- Fogel, B.L.; Satya-Murti, S.; Cohen, B.H. Clinical exome sequencing in neurologic disease. Neurol. Clin. Pract. 2016, 6, 164–176. [Google Scholar] [CrossRef]
- Riboldi, G.M.; Di Fonzo, A.B. GBA, Gaucher Disease, and Parkinson’s Disease: From Genetic to Clinic to New Therapeutic Approaches. Cells 2019, 8, 364. [Google Scholar] [CrossRef]
- Geiger, J.T.; Ding, J.; Crain, B.; Pletnikova, O.; Letson, C.; Dawson, T.M.; Rosenthal, L.S.; Pantelyat, A.; Gibbs, J.R.; Albert, M.S.; et al. Next-generation sequencing reveals substantial genetic contribution to dementia with Lewy bodies. Neurobiol. Dis. 2016, 94, 55–62. [Google Scholar] [CrossRef]
- Muñoz, G.; García-Seisdedos, D.; Ciubotariu, C.; Piris-Villaespesa, M.; Gandía, M.; Martín-Moro, F.; Gutiérrez-Solana, L.G.; Morado, M.; López-Jiménez, J.; Sánchez-Herranz, A.; et al. Early detection of lysosomal diseases by screening of cases of idiopathic splenomegaly and/or thrombocytopenia with a next-generation sequencing gene panel. JIMD Rep. 2019, 51, 53–61. [Google Scholar] [CrossRef]
- Almazni, I.; Stapley, R.J.; Khan, A.O.; Morgan, N.V. A comprehensive bioinformatic analysis of 126 patients with an inherited platelet disorder to identify both sequence and copy number genetic variants. Hum. Mutat. 2020, 41, 1848–1865. [Google Scholar] [CrossRef]
- den Dunnen, J.T.; Antonarakis, S.E. Mutation nomenclature extensions and suggestions to describe complex mutations: A discussion. Hum. Mutat. 2000, 15, 7–12. [Google Scholar] [CrossRef]
- den Dunnen, J.T.; Paalman, M.H. Standardizing mutation nomenclature: Why bother? Hum. Mutat. 2003, 22, 181e–182. [Google Scholar] [CrossRef]
| Patient | Allele 1 | Allele 2 |
|---|---|---|
| GD#1 | c.1448T>C, p.L483P (L444P) | Total gene deletion |
| GD#2 | c.1226A>G, p.N409S (N370S) | AH006907.2:g.2094con10194 |
| GD#3 | c.1226A>G, p.N409S (N370S) | AH006907.2:g.1942_7319con100042_13806 |
| GD#4 | c.1049A>G, p.H350R (H311R) | c.1226A>G, p.N409S (N370S) |
| GD#5 | c.413delC, p.P138Lfs*62 (P99Lfs*62) | c.1226A>G, p.N409S (N370S) |
| GD#6 | c.1226A>G, p.N409S (N370S) | c.1448T>C, p.L483P (L444P) |
| GD#7 | c.475C>T, p.159W (R120W) | c.1226A>G, p.N409S (N370S) |
| GD#8 | c.508C>T, p.R170C (R131C) | c.1448T>C, p.L483P (L444P) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zampieri, S.; Cattarossi, S.; Pavan, E.; Barbato, A.; Fiumara, A.; Peruzzo, P.; Scarpa, M.; Ciana, G.; Dardis, A. Accurate Molecular Diagnosis of Gaucher Disease Using Clinical Exome Sequencing as a First-Tier Test. Int. J. Mol. Sci. 2021, 22, 5538. https://doi.org/10.3390/ijms22115538
Zampieri S, Cattarossi S, Pavan E, Barbato A, Fiumara A, Peruzzo P, Scarpa M, Ciana G, Dardis A. Accurate Molecular Diagnosis of Gaucher Disease Using Clinical Exome Sequencing as a First-Tier Test. International Journal of Molecular Sciences. 2021; 22(11):5538. https://doi.org/10.3390/ijms22115538
Chicago/Turabian StyleZampieri, Stefania, Silvia Cattarossi, Eleonora Pavan, Antonio Barbato, Agata Fiumara, Paolo Peruzzo, Maurizio Scarpa, Giovanni Ciana, and Andrea Dardis. 2021. "Accurate Molecular Diagnosis of Gaucher Disease Using Clinical Exome Sequencing as a First-Tier Test" International Journal of Molecular Sciences 22, no. 11: 5538. https://doi.org/10.3390/ijms22115538
APA StyleZampieri, S., Cattarossi, S., Pavan, E., Barbato, A., Fiumara, A., Peruzzo, P., Scarpa, M., Ciana, G., & Dardis, A. (2021). Accurate Molecular Diagnosis of Gaucher Disease Using Clinical Exome Sequencing as a First-Tier Test. International Journal of Molecular Sciences, 22(11), 5538. https://doi.org/10.3390/ijms22115538







