The Emerging Roles of Chromogranins and Derived Polypeptides in Atherosclerosis, Diabetes, and Coronary Heart Disease
Abstract
:1. Introduction
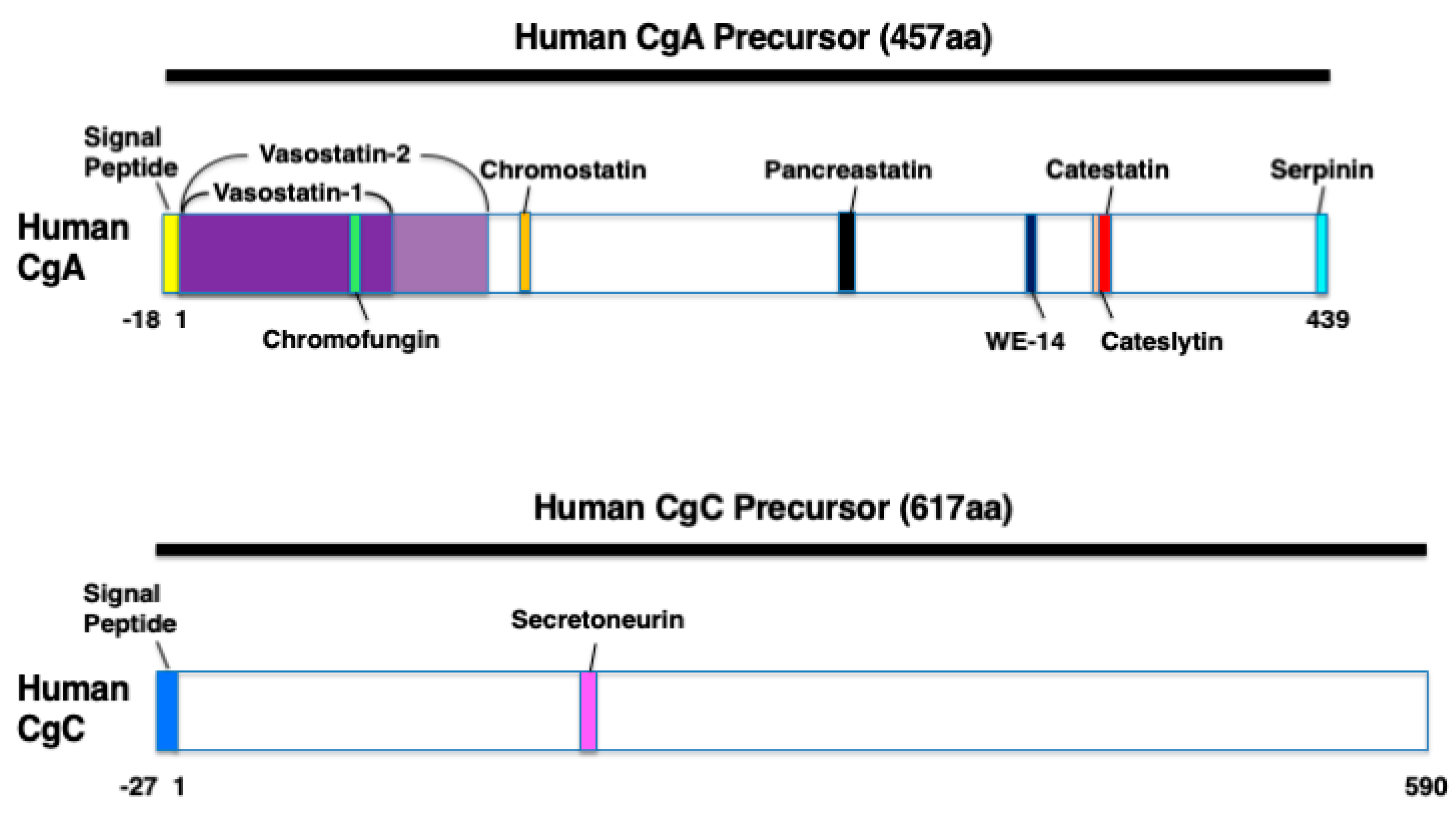
2. Characteristics of CgA, CgB, and CgC
3. Cgs-Derived Polypeptides
4. Biomarker for Diabetes, Metabolic Syndrome, and Cardiovascular Disease
5. Cardiovascular Effects
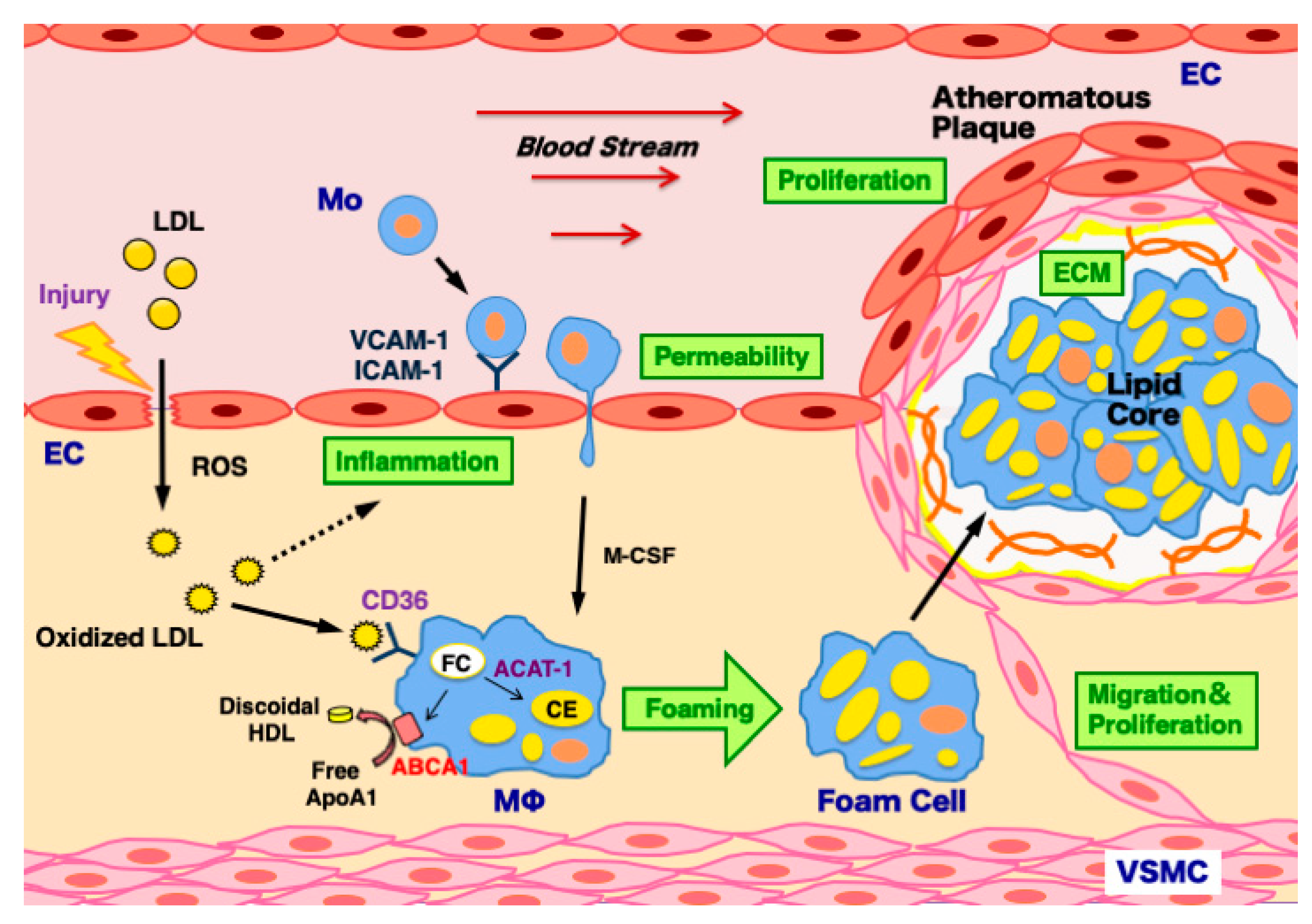
6. Atherosclerosis
6.1. ECs
6.2. Macrophages
6.3. VSMCs
6.4. Murine Models of Atherosclerosis
7. Myocardial Ischemia/Reperfusion Injury, Hind Limb Ischemia, and Stroke
8. Diabetes
9. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ABCA1 | ATP-binding cassette transporter A1 |
| ACAT-1 | Acyl coenzyme A: cholesterol acyltransferase-1 |
| AMPK | AMP-activated protein kinase |
| Cg | Chromogranin |
| CAD | Coronary artery disease |
| CE | Cholesterol ester |
| EC | Endothelial cell |
| ECM | Extracellular matrix |
| FC | Free cholesterol |
| ICAM-1 | Intercellular adhesion molecule-1 |
| LDL | Low-density lipoprotein |
| LPS | lipopolysaccharide |
| MCP-1 | Monocyte chemoattractant protein-1 |
| M-CSF | Macrophage colony stimulating factor |
| NO | Nitric oxide |
| PC | Prohormone convertase |
| PSTi8 | Pancreastatin inhibitor peptide-8 |
| ROS | Reactive oxygen species |
| TNF-α | Tumor necrosis factor-α |
| VCAM-1 | Vascular cell adhesion molecule-1 |
| VEGF | Vascular endothelial growth factor |
| VIF | Vasoconstriction-inhibiting factor |
| VSMC | Vascular smooth muscle cell |
References
- Malakar, A.K.; Choudhury, D.; Halder, B.; Paul, P.; Uddin, A.; Chakraborty, S. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell. Physiol. 2019, 234, 16812–16823. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.P.; Hunziker, P. Atherosclerosis: Insights into vascular pathobiology and outlook to novel treatments. J. Cardiovasc. Transl. Res. 2020, 13, 744–757. [Google Scholar] [CrossRef]
- Bartolomucci, A.; Possenti, R.; Mahata, S.K.; Fischer-Colbrie, R.; Loh, Y.P.; Salton, S.R.J. The extended granin family: Structure, function, and biomedical implications. Endocr. Rev. 2011, 32, 755–797. [Google Scholar] [CrossRef] [Green Version]
- Cohn, D.V.; Zangerle, R.; Fischer-Colbrie, R.; Chu, L.L.; Elting, J.J.; Hamilton, J.W.; Winkler, H. Similarity of secretory protein I from parathyroid gland to chromogranin A from adrenal medulla. Proc. Natl. Acad. Sci. USA 1982, 79, 6056–6059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huh, Y.H.; Jeon, S.H.; Yoo, S.H. Chromogranin B-induced secretory granule biogenesis: Comparison with the similar role of chromogranin A. J. Biol. Chem. 2003, 278, 40581–40589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fischer-Colbrie, R.; Hagn, C.; Kilpatrick, L.; Winkler, H. Chromogranin C: A third component of the acidic proteins in chromaffin granules. J. Neurochem. 1986, 47, 318–321. [Google Scholar] [CrossRef]
- Goetze, J.P.; Hilsted, L.M.; Rehfeld, J.F. Chromogranin A in cardiovascular endocrinology. Acta Physiol. 2021, 231, e13615. [Google Scholar] [CrossRef]
- Ebert, A.; König, J.; Frommer, L.; Schuppan, D.; Kahaly, G.J. Chromogranins serves as novel biomarker of endocrine and gastric autoimmunity. J. Clin. Endocrinol. Metab. 2020, 105, dgaa288. [Google Scholar] [CrossRef] [PubMed]
- Herold, Z.; Herold, M.; Nagy, P.; Patocs, A.; Doleschall, M.; Somogyi, A. Serum chromogranin A level continuously rises with the progression of type 1diabetes, and indicates the presence of both enterochromaffin-like cell hyperplasia and autoimmune gastritis. J. Diabetes Investig. 2020, 11, 865–873. [Google Scholar] [CrossRef] [Green Version]
- Herold, Z.; Doleschall, M.; Kovesdi, A.; Patocs, A.; Somogyi, A. Chromogranin A and its role in the pathogenesis of diabetes mellitus. Endokrynol. Pol. 2018, 69, 598–610. [Google Scholar] [CrossRef] [PubMed]
- Cetin, Y.; Aunis, D.; Bader, M.F.; Galindo, E.; Jörns, A.; Bargsten, G.; Grube, D. Chromostatin, a chromogranin A-derived bioactive peptide, is present in human pancreatic insulin (β) cells. Proc. Natl. Acad. Sci. USA 1993, 90, 2360–2364. [Google Scholar] [CrossRef] [Green Version]
- Tatemoto, K.; Efendić, S.; Mutt, V.; Makk, G.; Feistner, G.J.; Barchas, J.D. Pancreastatin, a novel pancreatic peptide that inhibits insulin secretion. Nature 1986, 324, 476–478. [Google Scholar] [CrossRef] [PubMed]
- Hossain, Z.; Valicherla, G.R.; Gupta, A.P.; Syed, A.A.; Riyazuddin, M.; Chandra, S.; Siddiqi, M.I.; Gayen, J.R. Discovery of pancreastatin inhibitor PSTi8 for the treatment of insulin resistance and diabetes: Studies in rodent models of diabetes mellitus. Sci. Rep. 2018, 8, 8715. [Google Scholar] [CrossRef] [Green Version]
- Zhang, K.; Chen, Y.; Wen, G.; Mahata, M.; Rao, F.; Fung, M.M.; Vaingankar, S.; Biswas, N.; Gayen, J.R.; Friese, R.S.; et al. Catecholamine storage vesicles: Role of core protein genetic polymorphisms in hypertension. Curr. Hypertens. Rep. 2011, 13, 36–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fung, M.M.; Nguyen, C.; Mehtani, P.; Salem, R.M.; Perez, B.; Thomas, B.; Das, M.; Schork, N.J.; Mahata, S.K.; Ziegler, M.G.; et al. Genetic variation within adrenergic pathways determines in vivo effects of presynaptic stimulation in humans. Circulation 2008, 117, 517–525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, G.; Wessel, J.; Zhou, W.; Ehret, G.B.; Rao, F.; Stridsberg, M.; Mahata, S.K.; Gent, P.M.; Das, M.; Cooper, R.S.; et al. An ancestral variant of Secretogranin II confers regulation by PHOX2 transcription factors and association with hypertension. Hum. Mol. Genet. 2007, 16, 1752–1764. [Google Scholar] [CrossRef]
- Choi, Y.; Miura, M.; Nakata, Y.; Sugasawa, T.; Nissato, S.; Otsuki, T.; Sugawara, J.; Iemitsu, M.; Kawakami, Y.; Shimano, H.; et al. A common genetic variant of the chromogranin A-derived peptide catestatin is associated with atherogenesis and hypertension in a Japanese population. Endocr. J. 2015, 62, 797–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiranmayi, M.; Chirasani, V.R.; Allu, P.K.; Subramanian, L.; Martelli, E.E.; Sahu, B.S.; Vishnuprabu, D.; Kumaragurubaran, R.; Sharma, S.; Bodhini, D.; et al. Catestatin Gly364Ser variant alters systemic blood pressure and the risk for hypertension in human populations via endothelial nitric oxide pathway. Hypertension 2016, 68, 334–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kojima, M.; Ozawa, N.; Mori, Y.; Takahashi, Y.; Watanabe-Kominato, K.; Shirai, R.; Watanabe, R.; Sato, K.; Matsuyama, T.; Ishibashi-Ueda, H.; et al. Catestatin prevents macrophage-driven atherosclerosis but not arterial injury-induced neointimal hyperplasia. Thromb. Haemost. 2018, 118, 182–194. [Google Scholar] [CrossRef]
- Sato, Y.; Watanabe, R.; Uchiyama, N.; Ozawa, N.; Takahashi, Y.; Shirai, R.; Sato, K.; Mori, Y.; Matsuyama, T.; Ishibashi-Ueda, H.; et al. Inhibitory effects of vasostatin-1 against atherogenesis. Clin. Sci. 2018, 132, 2493–2507. [Google Scholar] [CrossRef]
- Xiong, W.; Wang, X.; Dai, D.; Zhang, B.; Lu, L.; Tao, R. The anti-inflammatory vasostatin-2 attenuates atherosclerosis in ApoE-/- mice and inhibits monocyte/macrophage recruitment. Thromb. Haemost. 2017, 117, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Fornero, S.; Bassino, E.; Gallo, M.P.; Ramella, R.; Levi, R.; Alloatti, G. Endothelium dependent cardiovascular effects of the chromogranin A-derived peptides vasostatin-1 and catestatin. Curr. Med. Chem. 2012, 19, 4059–4067. [Google Scholar] [CrossRef]
- Salem, S.; Jankowski, V.; Asare, Y.; Liehn, E.; Welker, P.; Raya-Bermudez, A.; Pineda-Martos, C.; Rodriguez, M.; Muñoz-Castañeda, J.R.; Bruck, H.; et al. Identification of the vasoconstriction-inhibiting factor (VIF), a potent endogenous cofactor of angiotensin II acting on the angiotensin II type 2 receptor. Circulation 2015, 131, 1426–1434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Troger, J.; Theurl, M.; Kirchmair, R.; Pasqua, T.; Tota, B.; Angelone, T.; Cerra, M.C.; Nowosielski, Y.; Mätzler, R.; Troger, J.; et al. Granin-derived peptides. Prog. Neurobiol. 2017, 154, 37–61. [Google Scholar] [CrossRef]
- Blaschko, H.; Comline, R.S.; Schneider, F.H.; Silver, M.; Smith, A.D. Secretion of a chromaffin granule protein, chromogranin, from the adrenal gland after splanchnic stimulation. Nature 1967, 215, 58–59. [Google Scholar] [CrossRef]
- Lee, R.W.; Huttner, W.B. Tyrosine-O-sulfated proteins of PC12 pheochromocytoma cells and their sulfation by a tyrosylprotein sulfotransferase. J. Biol. Chem. 1983, 258, 11326–11334. [Google Scholar] [CrossRef]
- Gerdes, H.H.; Rosa, P.; Phillips, E.; Baeuerle, P.A.; Frank, R.; Argos, P.; Huttner, W.B. The primary structure of human secretogranin II, a widespread tyrosine-sulfated secretory granule protein that exhibits low pH- and calcium-induced aggregation. J. Biol. Chem. 1989, 264, 12009–12015. [Google Scholar] [CrossRef]
- Mahata, S.K.; Kozak, C.A.; Szpirer, J.; Szpirer, C.; Modi, W.S.; Gerdes, H.H.; Huttner, W.B.; O’Connor, D.T. Dispersion of chromogranin/secretogranin secretory protein family loci in mammalian genomes. Genomics 1996, 33, 135–139. [Google Scholar] [CrossRef]
- Mouland, A.J.; Bevan, S.; White, J.H.; Hendy, G.N. Human chromogranin A gene. Molecular cloning, structural analysis, and neuroendocrine cell-specific expression. J. Biol. Chem. 1994, 269, 6918–6926. [Google Scholar] [CrossRef]
- Greenwood, T.A.; Cadman, P.E.; Stridsberg, M.; Nguyen, S.; Taupenot, L.; Schork, N.J.; O’Connor, D.T. Genome-wide linkage analysis of chromogranin B expression in the CEPH pedigrees: Implications for exocytotic sympathochromaffin secretion in humans. Physiol. Genomics 2004, 18, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Benedum, U.M.; Lamouroux, A.; Konecki, D.S.; Rosa, P.; Hille, A.; Baeuerle, P.A.; Frank, R.; Lottspeich, F.; Mallet, J.; Huttner, W.B. The primary structure of human secretogranin I (chromogranin B): Comparison with chromogranin A reveals homologous terminal domains and a large intervening variable region. EMBO J. 1987, 6, 1203–1211. [Google Scholar] [CrossRef] [PubMed]
- Scammell, J.G.; Reddy, S.; Valentine, D.L.; Coker, T.N.; Nikolopoulos, S.N.; Ross, R.A. Isolation and characterization of the human secretogranin II gene promoter. Brain Res. Mol. Brain Res. 2000, 75, 8–15. [Google Scholar] [CrossRef]
- Fargali, S.; Garcia, A.L.; Sadahiro, M.; Jiang, C.; Janssen, W.G.; Lin, W.J.; Cogliani, V.; Elste, A.; Mortillo, S.; Cero, C.; et al. The granin VGF promotes genesis of secretory vesicles, and regulatescirculating catecholamine levels and blood pressure. FASEB J. 2014, 28, 2120–2133. [Google Scholar] [CrossRef] [Green Version]
- Bearrows, S.C.; Bauchle, C.J.; Becker, M.; Haldeman, J.M.; Swaminathan, S.; Stephens, S.B. Chromogranin B regulates early-stage insulin granule trafficking from the Golgi in pancreatic islet β-cells. J. Cell Sci. 2019, 132, jcs231373. [Google Scholar] [CrossRef] [Green Version]
- Saria, A.; Troger, J.; Kirchmair, R.; Fischer-Colbrie, R.; Hogue-Angeletti, R.; Winkler, H. Secretoneurin releases dopamine from rat striatal slices: A biological effect of a peptide derived from secretogranin II (chromogranin C). Neuroscience 1993, 54, 1–4. [Google Scholar] [CrossRef]
- D’amico, M.A.; Ghinassi, B.; Izzicup, P.; Monzoli, L.; Di Baldassarre, A. Biological function and clinical relevance of chromogranin A and derived peptides. Endocr. Connect. 2014, 3, R45–R54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahata, S.K.; Corti, A. Chromogranin A and its fragments in cardiovascular, immunometabolic, and cancer regulation. Ann. N. Y. Acad. Sci. 2019, 1455, 34–58. [Google Scholar] [CrossRef] [Green Version]
- Portel-Gomes, G.M.; Grimelius, L.; Johansson, H.; Wilander, E.; Stridsberg, M. Chromogranin A in human neuroendocrine tumors: An immunohistochemical study with region-specific antibodies. Am. J. Surg. Pathol. 2001, 25, 1261–1267. [Google Scholar] [CrossRef]
- Strub, J.M.; Garcia-Sablone, P.; Lonning, K.; Taupenot, L.; Hubert, P.; Van Dorsselaer, A.; Aunis, D.; Metz-Boutigue, M.H. Processing of chromogranin B in bovine adrenal medulla. Identification of secretolytin, the endogenous C-terminal fragment of residues 614–626 with antibacterial activity. Eur. J. Biochem. 1995, 229, 356–368. [Google Scholar] [CrossRef]
- Tasiemski, A.; Hammad, H.; Vandenbulcke, F.; Breton, C.; Bilfinger, T.J.; Pestel, J.; Salzet, M. Presence of chromogranin-derived antimicrobial peptides in plasma during coronary artery bypass surgery and evidence of an immune origin of these peptides. Blood 2002, 100, 553–559. [Google Scholar] [CrossRef] [Green Version]
- Wiedermann, C.J.; Dunzendorfer, S.; Kähler, C.M.; Reinisch, N.; Schratzberger, P. Secretoneurin and neurogenic inflammation. Zhongguo Yao Li Xue Bao 1999, 20, 789–794. [Google Scholar] [PubMed]
- Røsjø, H.; Stridsberg, M.; Florholmen, G.; Stensløkken, K.O.; Ottesen, A.H.; Sjaastad, I.; Husberg, C.; Dahl, M.B.; Øie, E.; Louch, W.E.; et al. Secretogranin II; a protein increased in the myocardium and circulation in heart failure with cardioprotective properties. PLoS ONE 2012, 7, e37401. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Schgoer, W.; Beer, A.G.; Jeschke, J.; Leierer, J.; Theurl, M.; Frauscher, S.; Tepper, O.M.; Niederwanger, A.; Ritsch, A.; et al. Hypoxia up-regulates the angiogenic cytokine secretoneurin via an HIF-1α- and basic FGF-dependent pathway in muscle cells. FASEB J. 2007, 21, 2906–2917. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, D.T.; Bernstein, K.N. Radioimmunoassay of chromogranin A in plasma as a measure of exocytotic sympathoadrenal activity in normal subjects and patients with pheochromocytoma. N. Engl. J. Med. 1984, 311, 764–770. [Google Scholar] [CrossRef]
- Tota, B.; Angelone, T.; Cerra, M.C. The surging role of chromogranin A in cardiovascular homeostasis. Front. Chem. 2014, 2, 64. [Google Scholar] [CrossRef] [Green Version]
- Goetze, J.P.; Alehagen, U.; Flyvbjerg, A.; Rehfeld, J.F. Chromogranin A as a biomarker in cardiovascular disease. Biomark. Med. 2014, 8, 133–140. [Google Scholar] [CrossRef]
- Herold, Z.; Herold, M.; Rosta, K.; Doleschall, M.; Somogyi, A. Lower serum chromogranin B level is associated with type 1 diabetes and with type 2 diabetes patients with intensive conservative insulin treatment. Diabetol. Metab. Syndr. 2020, 12, 61. [Google Scholar] [CrossRef]
- O’Connor, D.T.; Cadman, P.E.; Smiley, C.; Salem, R.M.; Rao, F.; Smith, J.; Funk, S.D.; Mahata, S.K.; Mahata, M.; Wen, G.; et al. Pancreastatin: Multiple actions on human intermediary metabolism in vivo, variation in disease, and naturally occurring functional genetic polymorphism. J. Clin. Endocrinol. Metab. 2005, 90, 5414–5425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sánchez-Margalet, V.; Lobón, J.A.; González, A.; Fernández-Soto, M.L.; Escobar-Jiménez, F.; Goberna, R. Increased plasma pancreastatin-like levels in gestational diabetes: Correlation with catecholamine levels. Diabetes Care 1998, 21, 1951–1954. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Wang, Y.N.; Li, M.C.; Wang, H.B.; Pu, L.J.; Niu, W.Q.; Meng, H.; Yang, E.L.; Zhang, R.Y.; Zhang, Q.; et al. Reduced serum levels of vasostatin-2, an anti-inflammatory peptide derived from chromogranin A, are associated with the presence and severity of coronary artery disease. Eur. Heart J. 2012, 33, 2297–2306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simunovic, M.; Supe-Domic, D.; Karin, Z.; Degoricija, M.; Paradzik, M.; Bozic, J.; Unic, I.; Skrabic, V. Serum catestatin concentrations are decreased in obese children and adolescents. Pediatr. Diabetes 2019, 20, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, N.; Santoro, F.; Di Biase, L.; Di Terlizzi, V.; Vitale, E.; Barone, R.; Della Rocca, D.G.; De Leon, D.L.; Cruz, N.S.; Di Biase, M.; et al. Chromogranin-A serum levels in patients with takotsubo syndrome and ST elevation acute myocardial infarction. Int. J. Cardiol. 2020, 320, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Jansson, A.M.; Røsjø, H.; Omland, T.; Karlsson, T.; Hartford, M.; Flyvbjerg, A.; Caidahl, K. Prognostic value of circulating chromogranin A levels in acute coronary syndromes. Eur. Heart J. 2009, 30, 25–32. [Google Scholar] [CrossRef]
- Estensen, M.E.; Hognestad, A.; Syversen, U.; Squire, I.; Ng, L.; Kjekshus, J.; Dickstein, K.; Omland, T. Prognostic value of plasma chromogranin A levels in patients with complicated myocardial infarction. Am. Heart J. 2006, 152, 927.e1–927.e6. [Google Scholar] [CrossRef] [PubMed]
- Omland, T.; Dickstein, K.; Syversen, U. Association between plasma chromogranin A concentration and long-term mortality after myocardial infarction. Am. J. Med. 2003, 114, 25–30. [Google Scholar] [CrossRef]
- Bachetti, T.; Ferrari Bardile, A.; Aloi, T.L.; Colombo, B.; Assi, E.; Savino, G.; Vercelli, A.; Colombo, R.; Corti, A. Plasma levels of vasostatin-1, a chromogranin A fragment, are associated with carotid artery maximum stenosis: A pilot study. Int. J. Cardiol. 2017, 236, 438–443. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, X.; Yang, C.; Su, X.; Yang, W.; Dai, Y.; Han, H.; Jiang, J.; Lu, L.; Wang, H.; et al. Decreased circulating catestatin levels are associated with coronary artery disease: The emerging anti-inflammatory role. Atherosclerosis 2019, 281, 78–88. [Google Scholar] [CrossRef]
- Xu, W.; Yu, H.; Wu, H.; Li, S.; Chen, B.; Gao, W. Plasma catestatin in patients with acute coronary syndrome. Cardiology 2017, 136, 164–169. [Google Scholar] [CrossRef]
- Pan, W.Q.; He, Y.H.; Su, Q.; Yang, J.; Fang, Y.H.; Ding, F.H.; Yan, X.X.; Liu, Z.H.; Wang, X.Q.; Yang, K.; et al. Association of decreased serum vasostatin-2 level with ischemic chronic heart failure and with MACE in 3-year follow-up: Vasostatin-2 prevents heart failure in myocardial infarction rats. Int. J. Cardiol. 2016, 221, 1–11. [Google Scholar] [CrossRef]
- Liu, L.; Ding, W.; Zhao, F.; Shi, L.; Pang, Y.; Tang, C. Plasma levels and potential roles of catestatin in patients with coronary heart disease. Scand. Cardiovasc. J. 2013, 47, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Xie, H.; Wang, X.; Liang, Y.; Yu, H.; Gao, W. Correlation of plasma catestatin level and the prognosis of patients with acute myocardial infarction. PLoS ONE 2015, 10, e0122993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, W.; Yu, H.; Li, W.; Gao, W.; Guo, L.; Wang, G. Plasma catestatin: A useful biomarker for coronary collateral development with chronic myocardial ischemia. PLoS ONE 2016, 11, e0149062. [Google Scholar] [CrossRef] [Green Version]
- Zhu, D.; Xie, H.; Wang, X.; Liang, Y.; Yu, H.; Gao, W. Catestatin–A novel predictor of left ventricular remodeling after acute myocardial infarction. Sci. Rep. 2017, 7, 44168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, L.; Wang, J.; Ding, W.H.; Han, P.; Yang, Y.; Qi, L.T.; Zhang, B.W. Plasma catestatin level in patients with acute myocardial infarction and its correlation with ventricular remodelling. Postgrad. Med. J. 2013, 89, 193–196. [Google Scholar] [CrossRef] [Green Version]
- Takiyyuddin, M.A.; Parmer, R.J.; Kailasam, M.T.; Cervenka, J.H.; Kennedy, B.; Ziegler, M.G.; Lin, M.C.; Li, J.; Grim, C.E.; Wright, F.A. Chromogranin A in human hypertension. Influence of heredity. Hypertension 1995, 26, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Durakoğlugil, M.E.; Ayaz, T.; Kocaman, S.A.; Kırbaş, A.; Durakoğlugil, T.; Erdoğan, T.; Çetin, M.; Şahin, O.Z.; Çiçek, Y. The relationship of plasma catestatin concentrations with metabolic and vascular parameters in untreated hypertensive patients: Influence on high-density lipoprotein cholesterol. Anatol. J. Cardiol. 2015, 15, 577–585. [Google Scholar] [CrossRef]
- Sánchez-Margalet, V.; Valle, M.; Lobón, J.A.; Maldonado, A.; Escobar-Jimenez, F.; Oliván, J.; Pérez-Cano, R.; Goberna, R. Increased plasma pancreastatin-like immunoreactivity levels in non-obese patients with essential hypertension. J. Hypertens. 1995, 13, 251–258. [Google Scholar]
- Ceconi, C.; Ferrari, R.; Bachetti, T.; Opasich, C.; Volterrani, M.; Colombo, B.; Parrinello, G.; Corti, A. Chromogranin A in heart failure; a novel neurohumoral factor and a predictor for mortality. Eur. Heart J. 2002, 23, 967–974. [Google Scholar] [CrossRef] [Green Version]
- Røsjø, H.; Husberg, C.; Dahl, M.B.; Stridsberg, M.; Sjaastad, I.; Finsen, A.V.; Carlson, C.R.; Oie, E.; Omland, T.; Christensen, G. Chromogranin B in heart failure: A putative cardiac biomarker expressed in the failing myocardium. Circ. Heart Fail. 2010, 3, 503–511. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Ding, W.; Li, R.; Ye, X.; Zhao, J.; Jiang, J.; Meng, L.; Wang, J.; Chu, S.; Han, X.; et al. Plasma levels and diagnostic value of catestatin in patients with heart failure. Peptides 2013, 46, 20–25. [Google Scholar] [CrossRef]
- Dobson, R.; Burgess, M.I.; Banks, M.; Pritchard, D.M.; Vora, J.; Valle, J.W.; Wong, C.; Chadwick, C.; George, K.; Keevil, B.; et al. The association of a panel of biomarkers with the presence and severity of carcinoid heart disease: A cross-sectional study. PLoS ONE 2013, 8, e73679. [Google Scholar] [CrossRef] [Green Version]
- Pieroni, M.; Corti, A.; Tota, B.; Curnis, F.; Angelone, T.; Colombo, B.; Cerra, M.C.; Bellocci, F.; Crea, F.; Maseri, A. Myocardial production of chromogranin A in human heart: A new regulatory peptide of cardiac function. Eur. Heart J. 2007, 28, 1117–1127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tombetti, E.; Colombo, B.; Di Chio, M.C.; Sartorelli, S.; Papa, M.; Salerno, A.; Bozzolo, E.P.; Tombolini, E.; Benedetti, G.; Godi, C.; et al. Chromogranin-A production and fragmentation in patients with Takayasu arteritis. Arthritis Res. Ther. 2016, 18, 187. [Google Scholar] [CrossRef] [Green Version]
- Ottesen, A.H.; Louch, W.E.; Carlson, C.R.; Landsverk, O.J.B.; Kurola, J.; Johansen, R.F.; Moe, M.K.; Aronsen, J.M.; Høiseth, A.D.; Jarstadmarken, H.; et al. Secretoneurin is a novel prognostic cardiovascular biomarker associated with cardiomyocyte calcium handling. J. Am. Coll. Cardiol. 2015, 65, 339–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brynildsen, J.; Myhre, P.L.; Lyngbakken, M.N.; Klaeboe, L.G.; Stridsberg, M.; Christensen, G.; Edvardsen, T.; Omland, T.; Røsjø, H. Circulating secretoneurin concentrations in patients with moderate to severe aortic stenosis. Clin. Biochem. 2019, 71, 17–23. [Google Scholar] [CrossRef]
- Brynildsen, J.; Petäjä, L.; Myhre, P.L.; Lyngbakken, M.N.; Nygård, S.; Stridsberg, M.; Christensen, G.; Ottesen, A.H.; Pettilä, V.; Omland, T.; et al. Circulating secretoneurin concentrations after cardiac surgery: Data from the FINNish Acute Kidney Injury Heart Study. Crit. Care Med. 2019, 47, e412–e419. [Google Scholar] [CrossRef]
- Soell, M.; Feki, A.; Hannig, M.; Sano, H.; Pinget, M.; Selimovic, D. Chromogranin A detection in saliva of type 2 diabetes patients. Bosn. J. Basic Med. Sci. 2010, 10, 2–8. [Google Scholar] [CrossRef] [Green Version]
- Kogawa, E.M.; Grisi, D.C.; Falcão, D.P.; Amorim, I.A.; Rezende, T.M.; da Silva, I.C.; Silva, O.N.; Franco, O.L.; de Amorim, R.F. Impact of glycemic control on oral health status in type 2 diabetes individuals and its association with salivary and plasma levels of chromogranin A. Arch. Oral Biol. 2016, 62, 10–19. [Google Scholar] [CrossRef]
- Fournier, I.; Gaucher, D.; Chich, J.F.; Bach, C.; Shooshtarizadeh, P.; Picaud, S.; Bourcier, T.; Speeg-Schatz, C.; Strub, J.M.; Van Dorsselaer, A.; et al. Processing of chromogranins/secretogranin in patients with diabetic retinopathy. Regul. Pept. 2011, 167, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Mahata, S.K.; Kiranmayi, M.; Mahapatra, N.R. Catestatin: A mster regulation of cardiovascular functions. Curr. Med. Chem. 2018, 25, 1352–1374. [Google Scholar] [CrossRef] [PubMed]
- Fung, M.M.; Salem, R.M.; Mehtani, P.; Thomas, B.; Lu, C.F.; Perez, B.; Rao, F.; Stridsberg, M.; Ziegler, M.G.; Mahata, S.K.; et al. Direct vasoactive effects of the chromogranin A (CHGA) peptide catestatin in humans in vivo. Clin. Exp. Hypertens. 2010, 32, 278–287. [Google Scholar] [CrossRef] [Green Version]
- Aardal, S.; Helle, K.B.; Elsayed, S.; Reed, R.K.; Serck-Hanssen, S. Vasostatins, comprising the N-terminal domain of chromogranin A, suppress tension in isolated human blood vessel segments. J. Neuroendocrinol. 1993, 5, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Aardal, S.; Galindo, E.; Aunis, D.; Helle, K.B. Human chromostatin inhibits endothelin-1-induced contractures in human blood vessels. Regul. Pept. 1993, 47, 25–32. [Google Scholar] [CrossRef]
- González-Yanes, C.; Santos-Alvarez, J.; Sánchez-Margalet, V. Pancreastatin, a chromogranin A-derived peptide, activates Galpha(16) and phospholipase C-beta(2) by interacting with specific receptors in rat heartmembranes. Cell Signal. 2001, 13, 43–49. [Google Scholar] [CrossRef]
- Lugardon, K.; Chasserot-Golaz, S.; Kieffer, A.E.; Maget-Dana, R.; Nullans, G.; Kieffer, B.; Aunis, D.; Metz-Boutigue, M.H. Structural and biological characterization of chromofungin, the antifungal chromogranin A-(47-66)-derived peptide. J. Biol. Chem. 2001, 276, 35875–35882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strub, J.M.; Sorokine, O.; van Dorsselaer, A.; Aunis, D.; Metz-Boutigue, M.H. Phosphorylation and O-glycosylation sites of bovine chromogarnin A from adrenal medullary chromaffin granules and their relationship with biological activities. J. Biol. Chem. 1997, 272, 11928–11936. [Google Scholar] [CrossRef] [Green Version]
- Tota, B.; Gentile, S.; Pasqua, T.; Bassino, E.; Koshimizu, H.; Cawley, N.X.; Cerra, M.C.; Loh, Y.P.; Angelone, T. The novel chromogranin A-derived serpinin and pyroglutaminated serpininpeptides are positive cardiac β-adrenergic-like inotropes. FASEB J. 2012, 26, 2888–2898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rocca, C.; De Bartolo, A.; Grande, F.; Rizzuti, B.; Pasqua, T.; Giordano, F.; Granieri, M.C.; Occhiuzzi, M.A.; Garofalo, A.; Amodio, N.; et al. Cateslytin abrogates lipopolysaccharide-induced cardiomyocyte injury by reducing inflammation and oxidative stress through toll like receptor 4 interaction. Int. Immunopharmacol. 2021, 94, 107487. [Google Scholar] [CrossRef]
- Theurl, M.; Schgoer, W.; Albrecht, K.; Jeschke, J.; Egger, M.; Beer, A.G.; Vasiljevic, D.; Rong, S.; Wolf, A.M.; Bahlmann, F.H.; et al. The neuropeptide catestatin acts as a novel angiogenic cytokine via a basic fibroblast growth factor-dependent mechanism. Circ. Res. 2010, 107, 1326–1335. [Google Scholar] [CrossRef] [Green Version]
- Fischer-Colbrie, R.; Kirchmair, R.; Kähler, C.M.; Wiedermann, C.J.; Saria, A. Secretoneurin: A new player in angiogenesis and chemotaxis linking nerves, blood vessels and the immune system. Curr. Protein Pept. Sci. 2005, 6, 373–385. [Google Scholar] [CrossRef] [PubMed]
- Veschini, L.; Crippa, L.; Dondossola, E.; Doglioni, C.; Corti, A.; Ferrero, E. The vasostatin-1 fragment of chromogranin A preserves a quiescent phenotype in hypoxia-driven endothelial cells and regulates tumor neovascularization. FASEB J. 2011, 25, 3906–3914. [Google Scholar] [CrossRef] [PubMed]
- Maestroni, S.; Maestroni, A.; Ceglia, S.; Tremolada, G.; Mancino, M.; Sacchi, A.; Lattanzio, R.; Zucchiatti, I.; Corti, A.; Bandello, F.; et al. Effect of chromogranin A-derived vasostatin-1 on laser-induced choroidal neovascularization in the mouse. Acta Ophthalmol. 2015, 93, e218–e222. [Google Scholar] [CrossRef] [Green Version]
- Albrecht-Schgoer, K.; Schgoer, W.; Holfeld, J.; Theurl, M.; Wiedemann, D.; Steger, C.; Gupta, R.; Semsroth, S.; Fischer-Colbrie, R.; Beer, A.G.; et al. The angiogenic factor secretoneurin induces coronary angiogenesis in a model of myocardial infarction by stimulation of vascular endothelial growth factor signaling in endothelial cells. Circulation 2012, 126, 2491–2501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mundi, S.; Massaro, M.; Scoditti, E.; Carluccio, M.A.; van Hinsbergh, V.W.M.; Iruela-Arispe, M.L.; De Caterina, R. Endothelial permeability, LDL deposition, and cardiovascular risk factors—A review. Cardiovasc. Res. 2018, 114, 35–52. [Google Scholar] [CrossRef]
- Obikane, H.; Abiko, Y.; Ueno, H.; Kusumi, Y.; Esumi, M.; Mitsumata, M. Effect of endothelial cell proliferation on atherogenesis: A role of p21Sdi/Cip/Waf1 in monocyte adhesion to endothelial cells. Atherosclerosis 2010, 212, 116–122. [Google Scholar] [CrossRef]
- Ferreno, E.; Scabini, S.; Magni, E.; Foglieni, C.; Belloni, D.; Colombo, B.; Curnis, F.; Villa, A.; Ferrero, M.E.; Corti, A. Chromogranin A protects vessels against tumor necrosis factor α-induced vascular leakage. FASEB J. 2004, 18, 554–556. [Google Scholar] [CrossRef]
- Helle, K.B.; Metz-Boutigue, M.H.; Cerra, M.C.; Angelone, T. Chromogranins: From discovery to current times. Pflugers Arch. 2018, 470, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.; Liu, S.; Zhang, D.; Wei, F.; Gu, N.; Zeng, Y.; Chen, X.; Xu, S.; Liu, S.; Xiang, T. Chromogranin A (CGA)-derived polypeptide (CGA47-66) inhibits TNF-α-induced vascular endothelial hyper-permeability through SOC-related Ca2+ signaling. Peptides 2020, 131, 170297. [Google Scholar] [CrossRef]
- Blois, A.; Srebro, B.; Mandalà, M.; Corti, A.; Helle, K.B.; Serck-Hanssen, G. The chromogranin A peptide vasostatin-I inhibits gap formation and signal transduction mediated by inflammatory agents in cultured bovine pulmonary and coronary arterial endothelial cells. Regul. Pept. 2006, 135, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Belloni, D.; Scabini, S.; Foglieni, C.; Veschini, L.; Giazzon, A.; Colombo, B.; Fulgenzi, A.; Helle, K.B.; Ferrero, M.E.; Corti, A.; et al. The vasostatin-I fragment of chromogranin A inhibits VEGF-induced endothelial proliferation and migration. FASEB J. 2007, 21, 3052–3062. [Google Scholar] [CrossRef]
- Helle, K.B. Regulatory peptides from chromogranin A and secretogranin II: Putative modulators of cells and tissues involved in inflammatory conditions. Regul. Pept. 2010, 165, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Schgoer, W.; Theurl, M.; Jeschke, J.; Beer, A.G.; Albrecht, K.; Gander, R.; Rong, S.; Vasiljevic, D.; Egger, M.; Wolf, A.M.; et al. Gene therapy with the angiogenic cytokine secretoneurin induces therapeutic angiogenesis by a nitric oxide-dependent mechanism. Circ. Res. 2009, 105, 994–1002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kähler, C.M.; Kirchmair, R.; Kaufmann, G.; Kähler, S.T.; Reinisch, N.; Fischer-Colbrie, R.; Hongue-Angeletti, R.; Winkler, H.; Wiedermann, C.J. Inhibition of proliferation and stimulation of migration of endothelial cells by secretoneurin in vitro. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 932–939. [Google Scholar] [CrossRef] [PubMed]
- Kähler, C.M.; Kaufmann, G.; Kähler, S.T.; Wiedermann, C.J. The neuropeptide secretoneurin stimulates adhesion of human monocytes to arterial and venous endothelial cells in vitro. Regul. Pept. 2002, 110, 65–73. [Google Scholar] [CrossRef]
- Chan, C.K.; Vanhoutte, P.M. Secretoneurin facilitates endothelium-dependent relaxations in porcine coronary arteries. Am. J. Physiol. Heart Circ. Physiol. 2011, 300, H1159–H1165. [Google Scholar] [CrossRef]
- Watanabe, R.; Watanabe, H.; Takahashi, Y.; Kojima, M.; Konii, H.; Watanabe, K.; Shirai, R.; Sato, K.; Matsuyama, T.; Ishibashi-Ueda, H.; et al. Atheroprotective effects of tumor necrosis factor-stimulated gene-6. JACC Basic Transl. Sci. 2016, 6, 494–509. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Beer, A.G.; Theurl, M.; Schgoer, W.; Hotter, B.; Tatarczyk, T. Monocyte migration: A novel effect and signaling pathways of catestatin. Eur. J. Pharmacol. 2008, 598, 104–111. [Google Scholar] [CrossRef]
- Reinisch, N.; Kirchmair, R.; Kähler, C.M.; Hogue-Angeletti, R.; Fischer-Colbrie, R.; Winkler, H.; Wiedermann, C.J. Attraction of human monocytes by the neuropeptide secretoneurin. FEBS Lett. 1993, 334, 41–44. [Google Scholar] [CrossRef] [Green Version]
- Ying, W.; Tang, K.; Avolio, E.; Schilling, J.M.; Pasqua, T.; Liu, M.A.; Cheng, H.; Gao, H.; Zhang, J.; Mahata, S.; et al. Immunosuppression of macrophages underlies the cardioprotective effects of CST (Catestatin). Hypertension 2021, 77, 1670–1682. [Google Scholar] [CrossRef]
- Adiguzel, E.; Ahmad, P.J.; Franco, C.; Bendeck, M.P. Collagens in the progression and complications of atherosclerosis. Vasc. Med. 2009, 14, 73–89. [Google Scholar] [CrossRef] [Green Version]
- Wagenseil, J.E.; Mecham, R.P. Elastin in large artery stiffness and hypertension. J. Cardiovasc. Transl. Res. 2012, 5, 264–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hou, J.; Xue, X.; Li, J. Vasostatin-2 inhibits cell proliferation and adhesion in vascular smooth muscle cells, which are associated with the progression of atherosclerosis. Biochem. Biophys. Res. Commun. 2016, 469, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Zhou, C.; Sun, N. The neuropeptide catestatin promotes vascular smooth muscle cell proliferation through the Ca2+-calcineurin-NFAT signaling pathway. Biochem. Biophys. Res. Commun. 2011, 407, 807–812. [Google Scholar] [CrossRef]
- Kähler, C.M.; Schratzberger, P.; Wiedermann, C.J. Response of vascular smooth muscle cells to the neuropeptide secretoneurin. A functional role for migration and proliferation in vitro. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 2029–2035. [Google Scholar] [CrossRef]
- Liu, W.; Wang, F.; Zhao, M.; Fan, Y.; Cai, W.; Luo, M. The neuropeptide secretoneurin exerts a direct effect on arteriogenesis in vivo and in vitro. Anat. Rec. 2018, 301, 1917–1927. [Google Scholar] [CrossRef] [Green Version]
- Bourebaba, Y.; Mularczyk, M.; Marycz, K.; Bourebaba, L. Catestatin peptide of chromogranin A as a potential new target for several risk factors management in the course of metabolic syndrome. Biomed. Pharmacother. 2020, 134, 111113. [Google Scholar] [CrossRef]
- Gayen, J.R.; Saberi, M.; Schenk, S.; Biswas, N.; Vaingankar, S.M.; Cheung, W.W.; Najjar, S.M.; O’Connor, D.T.; Bandyopadhyay, G.; Mahata, S.K. A novel pathway of insulin sensistivity in chromogranin A null mice: A crucial role for pancreastatin in glucose homeostasis. J. Biol. Chem. 2009, 284, 28498–28509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandyopadhyay, G.K.; Mahata, S.K. Chromogranin A regulation of obesity and peripheral insulin sensitivity. Front. Endocrinol. 2017, 8, 20. [Google Scholar] [CrossRef] [Green Version]
- Pasqua, T.; Corti, A.; Gentile, S.; Pochini, L.; Bianco, M.; Metz-Boutigue, M.H.; Carmela, M.; Tota, B.; Angelone, T. Full-length human chromogranin-A cardioactivity: Myocardial, coronary, and stimulus-induced processing evidence in normotensive and hypertensive male rat hearts. Endocrinology 2013, 154, 3353–3365. [Google Scholar] [CrossRef] [Green Version]
- Penna, C.; Alloatti, G.; Gallo, M.P.; Cerra, M.C.; Levi, R.; Tullio, F.; Bassino, E.; Dolgetta, S.; Mahata, S.K.; Tota, B.; et al. Catestatin improves post-ischemic left ventricular function and decreases ischemia/reperfusion injury in heart. Cell. Mol. Neurobiol. 2010, 30, 1171–1179. [Google Scholar] [CrossRef] [Green Version]
- Cappello, S.; Angelone, T.; Tota, B.; Pagliaro, P.; Penna, C.; Rastaldo, R.; Corti, A.; Losano, G.; Cerra, M.C. Human recombinant chromogranin A-derived vasostatin-1 mimics preconditioning via an adenosine/nitric oxide signaling mechanism. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H719–H727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filice, E.; Pasqua, T.; Quintieri, A.M.; Cantafio, P.; Scavello, F.; Amodio, N.; Cerra, M.C.; Marban, C.; Schneider, F.; Metz-Boutigue, M.-H.; et al. Chromofungin, CgA 47-66 –derived peptide, produces basal cardiac effects and postconditioning cardioprotective action during ischemia/reperfusion injury. Peptides 2015, 71, 40–48. [Google Scholar] [CrossRef]
- Pasqua, T.; Tota, B.; Penna, C.; Corti, A.; Cerra, M.C.; Loh, Y.P.; Angelone, T. pGlu-serpinin protects the normotensive and hypertensive heart from ischemic injury. J. Endocrinol. 2015, 227, 167–178. [Google Scholar] [CrossRef] [Green Version]
- Theurl, M.; Schgoer, W.; Albrecht-Schgoer, K.; Lener, D.; Wolf, D.; Wolf, M.; Demetz, E.; Tymoszuk, P.; Tancevski, I.; Fischer-Colbrie, R.; et al. Secretoneurin gene therapy improves hind limb and cardiac ischaemia in Apo E-/- mice without influencing systemic atherosclerosis. Cardiovasc. Res. 2015, 105, 96–106. [Google Scholar] [CrossRef] [Green Version]
- Albrecht-Schgoer, K.; Barthelmes, J.; Schgoer, W.; Theurl, M.; Nardin, I.; Lener, D.; Gutmann, C.; Dünnhaupt, S.; Bernkop-Schnürch, A.; Kirchmair, R. Nanoparticular delivery system for a secretoneurin derivative induces angiogenesis in a hind limb ischemia model. J. Control. Release 2017, 250, 1–8. [Google Scholar] [CrossRef]
- Schgoer, W.; Theurl, M.; Albrecht-Schgoer, K.; Jonach, V.; Koller, B.; Lener, D.; Franz, W.M.; Kirchmair, R. Secretoneurin gene therapy improves blood flow in an ischemia model in type 1 diabetic mice by enhancing therapeutic neovascularization. PLoS ONE 2013, 8, e74029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theurl, M.; Lener, D.; Albrecht-Schgoer, K.; Beer, A.; Schgoer, W.; Liu, Y.; Stanzl, U.; Fischer-Colbrie, R.; Kirchmair, R. Gene therapy with the angiogenic neuropeptide secretoneurin ameliorates experimental diabetic neuropathy. FASEB J. 2018, 32, 4815–4823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.L.; Liu, Y.; Jiang, W.; Wang, X.X.; Yuan, G.L.; Zhao, Y.L.; Yu, C. Secretoneurin suppresses cardiac hypertrophy through suppression of oxidant stress. Eur. J. Pharmacol. 2018, 822, 13–24. [Google Scholar] [CrossRef]
- Posod, A.; Wechselberger, K.; Stanika, R.I.; Obermair, G.J.; Wegleiter, K.; Huber, E.; Urbanek, M.; Kiechl-Kohlendorfer, U.; Griesmaier, E. Administration of secretoneurin is protective in hypoxic-ischemic neonatal brain injury predominantly in the hypoxic-only hemisphere. Neuroscience 2017, 352, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Shyu, W.C.; Lin, S.Z.; Chiang, M.F.; Chen, D.C.; Su, C.Y.; Wang, H.J.; Liu, R.S.; Tsai, C.H.; Li, H. Secretoneurin promotes neuroprotection and neuronal plasticity via the Jak2/Stat3 pathway in murine models of stroke. J. Clin. Investig. 2008, 118, 133–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ying, W.; Mahata, S.; Bandyopadhyay, G.K.; Zhou, Z.; Wollam, J.; Vu, J.; Mayoral, R.; Chi, N.W.; Webster, N.J.G.; Corti, A.; et al. Catestatin inhibits obesity-induced macrophage infiltration and inflammation in the liver and suppresses hepatic glucose production, leading to improved insulin sensitivity. Diabetes 2018, 67, 841–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delong, T.; Baker, R.L.; He, J.; Barbour, G.; Bradley, B.; Haskins, K. Diabetogenic T-cell clones recognize an altered peptide of chromogranin A. Diabetes 2012, 61, 3239–3246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Zhou, L.; Li, Y.; Zhang, J.; Guo, B.; Meng, G.; Chen, X.; Zheng, Q.; Zhang, L.; Zhang, M.; et al. Identification of autoreactive CD8+ T cell responses targeting chromogranin A in humanized NOD mice and type 1 diabetes patients. Clin. Immunol. 2015, 159, 63–71. [Google Scholar] [CrossRef] [Green Version]
- Nikoopour, E.; Sandrock, C.; Huszarik, K.; Krougly, O.; Lee-Chan, E.; Masteller, E.L.; Bluestone, J.A.; Singh, B. Cutting edge: Vasostatin-1-derived peptide ChgA29-42 is an antigenic epitope of diabetogenic BDC2.5 T cells in nonobese diabetic mice. J. Immunol. 2011, 186, 3831–3835. [Google Scholar] [CrossRef] [Green Version]
- Valicherla, G.R.; Hossain, Z.; Mahata, S.K.; Gayen, J.R. Pancreastatin is an endogenous peptide that regulates glucose homeostasis. Physiol. Genomics 2013, 45, 1060–1071. [Google Scholar] [CrossRef] [Green Version]
- González-Yanes, C.; Sánchez-Magalet, V. Pancreastatin, a chromogranin-A-derived peptide, inhibits insulin-stimulated glycogen synthesis by activating GSK-3 in rat adipocytes. Biochem. Biophys. Res. Commun. 2001, 289, 282–287. [Google Scholar] [CrossRef]
- Gupta, A.P.; Syed, A.A.; Garg, R.; Goand, U.K.; Singh, P.; Riyazuddin, M.; Valicherla, G.R.; Husain, A.; Gayen, J.R. Pancreastatin inhibitor PSTi8 attenuates hyperinsulinemia induced obesity and inflammation mediated insulin resistance via MAPK/NOX3-JNK pathway. Eur. J. Pharmacol. 2019, 864, 172723. [Google Scholar] [CrossRef]
- Bandyopadhyay, G.K.; Lu, M.; Avolio, E.; Siddiqui, J.A.; Gayen, J.R.; Wollam, J.; Vu, C.U.; Chi, N.W.; O’Connor, D.T.; Mahata, S.K. Pancreastatin-dependent inflammatory signaling mediates obesity-induced insulin resistance. Diabetes 2015, 64, 104–116. [Google Scholar] [CrossRef] [Green Version]
- Zagórowicz, E.; Bak, M.; Siemińska, J.; Muszyński, J. Pancreastatin secretion stimulation in healthy volunteers. Pol. Arch. Med. Wewn. 2002, 108, 1185–1191. [Google Scholar] [PubMed]
- Cadman, P.E.; Rao, F.; Mahata, S.K.; O’Connor, D.T. Studies of the dysglycemic peptide, pancreastatin, using a human forearm model. Ann. N. Y. Acad. Sci. 2002, 971, 528–529. [Google Scholar] [CrossRef] [PubMed]
- Siegel, E.G.; Gallwitz, B.; Fölsch, U.R.; Schmidt, W.E. Effect of human pancreastatin peptide (hP-16) on oral glucose tolerance in man. Exp. Clin. Endocrinol. Diabetes 1998, 106, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Valicherla, G.R.; Gupta, A.P.; Hossain, Z.; Riyazuddin, M.; Syed, A.A.; Husain, A.; Lahiri, S.; Dave, K.M.; Gayen, J.R. Pancreastatin inhibitor, PSTi8 ameliorates metabolic health by modulating AKT/GSK-3β and PKCλ/ζ/SREBP1c pathways in high fat diet induced insulin resistance in peri-/post-menopausal rats. Peptides 2019, 120, 170147. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.P.; Garg, R.; Singh, P.; Goand, U.K.; Syed, A.A.; Valicherla, G.R.; Riyazuddin, M.; Mugale, M.N.; Gayen, J.R. Pancreastatin inhibitor PSTi8 protects the obesity associated skeletal muscle insulin resistance in diet induced streptozotocin-treated diabetic mice. Eur. J. Pharmacol. 2020, 881, 173204. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.P.; Singh, P.; Garg, R.; Valicherla, G.R.; Riyazuddin, M.; Syed, A.A.; Hossain, Z.; Gayen, J.R. Pancreastatin inhibitor activates AMPK pathway via GPR78 and ameliorates dexamethasone induced fatty liver disease in C57BL/6 mice. Biomed. Pharmacother. 2019, 116, 108959. [Google Scholar] [CrossRef] [PubMed]
| Type 1 Diabetes | Control | p Value | Ref | Type 2 Diabetes | Control | p Value | Ref | |
|---|---|---|---|---|---|---|---|---|
| CgA | 61.64 ± 55.27 ↑ | 48.03 ± 19.99 | 0.0348 | [47] | 57.80 ± 34.74 | 49.97 ± 22.29 | 0.1587 | [47] |
| CgB | 89.39 ± 34.23 ↓ | 107.38 ± 59.77 | 0.0241 | [47] | 99.72 ± 54.79 | 112.54 ± 61.68 | 0.1698 | [47] |
| Pancreastatin | NE | NE | NE | - | 0.097 ± 0.022 ↑ | 0.026 ± 0.004 | 0.009 | [48] |
| CAD | Control | p Value | Ref | Hypertension | Control | p Value | Ref | |
|---|---|---|---|---|---|---|---|---|
| CgA | 358 ± 304 ↑ | 108 ± 74 | 0.017 | [52] | 99.9 ± 6.7 ↑ | 62.8 ± 4.7 | <0.001 | [65] |
| Catestatin | 2.09 ± 1.42 ↓ | 4.05 ± 3.52 | 0.0112 | [19] | 2.27 ± 0.83 ↑ | 1.92 ± 0.49 | 0.004 | [66] |
| Vasostatin-2 | 4.45 ± 2.64 ↓ | 5.82 ± 3.22 | <0.001 | [50] | NE | NE | NE | - |
| EC | Macrophage | VSMC | ||||||
|---|---|---|---|---|---|---|---|---|
| Permeability | Proliferation | VCAM-1 | Foaming Cell | Migration | Proliferation | Collagen | Elastin | |
| CgA | ↓ | NE | NE | NE | NE | NE | NE | NE |
| Catestatin | ↓ | ↑ | ↓ | ↓ | ↓ | ↓ | ↓ (*1) | ↑ |
| Vasostatin-1 | ↓ | ↓ | ↓ | ↓ | ↓ | → | ↓ (*2) | ↑ |
| Vasostatin-2 | NE | ↑ | ↓ | NE | ↓ | ↓ | NE | NE |
| Secretoneurin | ↑ | ↑ or ↓ | ↑ | NE | NE | ↑ | NE | NE |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watanabe, T. The Emerging Roles of Chromogranins and Derived Polypeptides in Atherosclerosis, Diabetes, and Coronary Heart Disease. Int. J. Mol. Sci. 2021, 22, 6118. https://doi.org/10.3390/ijms22116118
Watanabe T. The Emerging Roles of Chromogranins and Derived Polypeptides in Atherosclerosis, Diabetes, and Coronary Heart Disease. International Journal of Molecular Sciences. 2021; 22(11):6118. https://doi.org/10.3390/ijms22116118
Chicago/Turabian StyleWatanabe, Takuya. 2021. "The Emerging Roles of Chromogranins and Derived Polypeptides in Atherosclerosis, Diabetes, and Coronary Heart Disease" International Journal of Molecular Sciences 22, no. 11: 6118. https://doi.org/10.3390/ijms22116118
APA StyleWatanabe, T. (2021). The Emerging Roles of Chromogranins and Derived Polypeptides in Atherosclerosis, Diabetes, and Coronary Heart Disease. International Journal of Molecular Sciences, 22(11), 6118. https://doi.org/10.3390/ijms22116118






