Genetic Susceptibility to Periodontal Disease in Down Syndrome: A Case-Control Study
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Groups
4.2. Collection and Processing of Saliva Samples
4.3. Association Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bull, M.J. Down Syndrome. N. Engl. J. Med. 2020, 382, 2344–2352. [Google Scholar] [CrossRef]
- Whooten, R.; Schmitt, J.; Schwartz, A. Endocrine manifestations of Down syndrome. Curr. Opin. Endocrinol. Diabetes Obes. 2018, 25, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Mubayrik, A.B. The Dental Needs and Treatment of Patients with Down Syndrome. Dent. Clin. N. Am. 2016, 60, 613–626. [Google Scholar] [CrossRef]
- Krishnan, C.; Archana, A. Evaluation of Oral Hygiene Status and Periodontal Health in Mentally Retarded Subjects with or without Down’s Syndrome in Comparison with Normal Healthy Individuals. J. Oral Health Commun. Dent. 2014, 8, 91–94. [Google Scholar] [CrossRef] [Green Version]
- Cutress, T.W. Periodontal disease and oral hygiene in trisomy 21. Arch. Oral Biol. 1971, 16, 1345–1355. [Google Scholar] [CrossRef]
- Ferreira, R.; Michel, R.C.; Greghi, S.L.A.; de Resende, M.L.R.; Sant’Ana, A.C.P.; Damante, C.A.; Zangrando, M.S. Prevention and periodontal treatment in Down syndrome patients: A systematic review. PLoS ONE 2016, 11, e0158339. [Google Scholar] [CrossRef] [Green Version]
- Amano, A.; Murakami, J.; Akiyama, S.; Morisaki, I. Etiologic factors of early-onset periodontal disease in Down syndrome. Jpn. Dent. Sci. Rev. 2008, 44, 118–127. [Google Scholar] [CrossRef] [Green Version]
- Khocht, A.; Yaskell, T.; Janal, M.; Turner, B.F.; Rams, T.E.; Haffajee, A.D.; Socranski, S.S. Subgingival microbiota in adult Down syndrome periodontitis. J. Periodontal. Res. 2012, 47, 500–507. [Google Scholar] [CrossRef] [Green Version]
- Nóvoa, L.; Sánchez, M.D.C.; Blanco, J.; Limeres, J.; Cuenca, M.; Marín, M.J.; Sanz, M.; Herrera, D.; Diz, P. The Subgingival Microbiome in Patients with Down Syndrome and Periodontitis. J. Clin. Med. 2020, 9, 2482. [Google Scholar] [CrossRef]
- Ram, G.; Chinen, J. Infections and immunodeficiency in Down syndrome. Clin. Exp. Immunol. 2011, 164, 9–16. [Google Scholar] [CrossRef]
- Nateghi Rostami, M.; Douraghi, M.; Miramin Mohammadi, A.; Nikmanesh, B. Altered serum pro-inflammatory cytokines in children with Down’s syndrome. Eur. Cytokine Netw. 2012, 23, 64–67. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Che, M.; Yuan, J.; Yu, Y.; Cao, C.; Qin, X.Y.; Cheng, Y. Aberrations in circulating inflammatory cytokine levels in patients with Down syndrome: A meta-analysis. Oncotarget 2017, 8, 84489–84496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsilingaridis, G.; Yucel-Lindberg, T.; Modéer, T. T-helper-related cytokines in gingival crevicular fluid from adolescents with Down syndrome. Clin. Oral Investig. 2012, 16, 267–273. [Google Scholar] [CrossRef]
- Taşdemir, İ.; Yılmaz, H.E.; Narin, F.; Sağlam, M. Assessment of saliva and gingival crevicular fluid soluble urokinase plasminogen activator receptor (suPAR), galectin-1, and TNF-α levels in periodontal health and disease. J. Periodontal Res. 2020, 55, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Murakami, T.; Takahata, Y.; Hata, K.; Nishimura, R. Role of interleukin-1 and inflammasomes in oral disease. J. Oral Biosci. 2020, 62, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Marcaccini, A.M.; Novaes, A.B., Jr.; Meschiari, C.A.; Souza, S.L.; Palioto, D.B.; Sorgi, C.A.; Faccioli, L.H.; Tanus-Santos, J.E.; Gerlach, R.F. Circulating matrix metalloproteinase-8 (MMP-8) and MMP-9 are increased in chronic periodontal disease and decrease after non-surgical periodontal therapy. Clin. Chim. Acta 2009, 409, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Polizzi, A.; Ronsivalle, V.; Alibrandi, A.; Palazzo, G.; Lo Giudice, A. Impact of matrix metalloproteinase-9 during periodontitis and cardiovascular diseases. Molecules 2021, 26, 1777. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Williams, R.C.; Lo Giudice, A. Analysis of galectin-3 levels as a source of coronary heart disease risk during periodontitis. J. Periodontal Res. 2021, 56, 597–605. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Williams, R.C. Periodontitis activates the nlrp3 inflammasome in serum and saliva. J. Periodontol. 2021. [Google Scholar] [CrossRef]
- De Coo, A.; Cruz, R.; Quintela, I.; Herrera, D.; Sanz, M.; Diz, P.; Rodríguez Grandío, S.; Vallcorba, N.; Ramos, I.; Oteo, A.; et al. Genome-wide association study of stage III/IV grade C periodontitis (former aggressive periodontitis) in a Spanish population. J. Clin. Periodontol. 2021. [Google Scholar] [CrossRef]
- Tsilingaridis, G.; Yucel-Lindberg, T.; Quezada, H.C.; Modéer, T. The relationship between matrix metalloproteinases (MMP-3, -8, -9) in serum and peripheral lymphocytes (CD8+, CD56+) in Down syndrome children with gingivitis. J. Periodontal Res. 2014, 49, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S162–S170. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Che, Q.; Jiang, F.Z.; Wang, H.H.; Wang, F.Y.; Liao, Y.; Wan, X.P. Piwil1 causes epigenetic alteration of PTEN gene via upregulation of DNA methyltransferase in type I endometrial cancer. Biochem. Biophys. Res. Commun. 2015, 463, 876–880. [Google Scholar] [CrossRef]
- Xie, K.; Zhang, K.; Kong, J.; Wang, C.; Gu, Y.; Liang, C.; Jiang, T.; Qin, N.; Liu, J.; Guo, X.; et al. Cancer-testis gene PIWIL1 promotes cell proliferation, migration, and invasion in lung adenocarcinoma. Cancer Med. 2018, 7, 157–166. [Google Scholar] [CrossRef] [Green Version]
- Aravin, A.A.; Hannon, G.J. Small RNA silencing pathways in germ and stem cells. Cold Spring Harb. Symp. Quant. Biol. 2008, 73, 283–290. [Google Scholar] [CrossRef] [Green Version]
- Friemel, C.; Ammerpohl, O.; Gutwein, J.; Schmutzler, A.G.; Caliebe, A.; Kautza, M.; von Otte, S.; Siebert, R.; Bens, S. Array-based DNA methylation profiling in male infertility reveals allele-specific DNA methylation in PIWIL1 and PIWIL2. Fertil. Steril. 2014, 101, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Cheung, S.; Parrella, A.; Rosenwaks, Z.; Palermo, G.D. Genetic and epigenetic profiling of the infertile male. PLoS ONE 2019, 14, e0214275. [Google Scholar] [CrossRef] [Green Version]
- Parizot, E.; Dard, R.; Janel, N.; Vialard, F. Down syndrome and infertility: What support should we provide? J. Assist. Reprod. Genet. 2021, 36, 1063–1067. [Google Scholar] [CrossRef]
- Carmona-Iragui, M.; Videla, L.; Lleó, A.; Fortea, J. Down syndrome, Alzheimer disease, and cerebral amyloid angiopathy: The complex triangle of brain amyloidosis. Dev. Neurobiol. 2019, 79, 716–737. [Google Scholar] [CrossRef]
- Villela, D.; Ramalho, R.F.; Silva, A.R.T.; Brentani, H.; Suemoto, C.K.; Pasqualucci, C.A.; Grinberg, L.T.; Krepischi, A.C.; Rosenberg, C. Differential DNA Methylation of MicroRNA Genes in Temporal Cortex from Alzheimer’s Disease Individuals. Neural Plast. 2016, 2016, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Toyono, T.; Nakashima, M.; Kuhara, S.; Akamine, A. Expression of TGF-β superfamily receptors in dental pulp. J. Dent. Res. 1997, 76, 1555–1560. [Google Scholar] [CrossRef] [PubMed]
- Fatemi, K.; Disfani, R.; Zare, R.; Moeintaghavi, A.; Ali, S.A.; Boostani, H.R. Influence of moderate to severe chronic periodontitis on dental pulp. J. Indian Soc. Periodontol. 2012, 16, 558–561. [Google Scholar]
- Song, G.; Ouyang, G.; Bao, S. The activation of Akt/PKB signaling pathway and cell survival. J. Cell Mol. Med. 2005, 9, 59–71. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, M.; Inoue, T.; Naito, M.; Nakayama, K.; Ohara, N. Attenuation of the phosphatidylinositol 3-Kinase/Akt signaling pathway by porphyromonas gingivalis gingipains RgpA, RgpB, and Kgp. J. Biol. Chem. 2015, 290, 5190–5202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakayama, M.; Ohara, N. Molecular mechanisms of Porphyromonas gingivalis-host cell interaction on periodontal diseases. Jap. Dent. Sci. Rev. 2017, 53, 134–140. [Google Scholar] [CrossRef]
- Liu, J.; Wang, X.; Zheng, M.; Luan, Q. Lipopolysaccharide from Porphyromonas gingivalis promotes autophagy of human gingival fibroblasts through the PI3K/Akt/mTOR signaling pathway. Life Sci. 2018, 211, 133–139. [Google Scholar] [CrossRef]
- McCormick, B.; Chu, J.Y.; Vermeren, S. Cross-talk between Rho GTPases and PI3K in the neutrophil. Small GTPases 2019, 10, 187–195. [Google Scholar] [CrossRef]
- Lawrence, M.S.; Stojanov, P.; Mermel, C.H.; Robinson, J.T.; Garraway, L.A.; Golub, T.R.; Meyerson, M.; Gabriel, S.B.; Lander, E.S.; Getz, G. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 2014, 505, 495–501. [Google Scholar] [CrossRef] [Green Version]
- Bortul, R.; Tazzari, P.L.; Billi, A.M.; Tabellini, G.; Mantovani, I.; Cappellini, A.; Deguelin, A. PI3K/AKT inhibitor, enhances chemosensitivity of leukaemia cells with an active PI3K/AKT pathway. Br. J. Haematol. 2005, 129, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Guarente, V.; Sportoletti, P. Lessons, Challenges and Future Therapeutic Opportunities for PI3K Inhibition in CLL. Cancers 2021, 13, 1280. [Google Scholar] [CrossRef] [PubMed]
- Whitlock, J.A. Down syndrome and acute lymphoblastic leukaemia. Br. J. Haematol. 2006, 135, 595–602. [Google Scholar] [CrossRef]
- Alsadat, S.; Khorami, H. PI3K/AKT pathway in modulating glucose homeostasis and its alteration in Diabetes. Annals Med. Biomed. Sci. 2015, 1, 46–55. [Google Scholar]
- Alexander, M.; Petri, H.; Ding, Y.; Wandel, C.; Khwaja, O.; Foskett, N. Morbidity and medication in a large population of individuals with Down syndrome compared to the general population. Dev. Med. Child Neurol. 2016, 58, 246–254. [Google Scholar] [CrossRef]
- Heras-Sandoval, D.; Pérez-Rojas, J.M.; Hernández-Damián, J.; Pedraza-Chaverri, J. The role of PI3K/AKT/mTOR pathway in the modulation of autophagy and the clearance of protein aggregates in neurodegeneration. Cell Signal. 2014, 26, 2694–2701. [Google Scholar] [CrossRef] [PubMed]
- Hartley, D.; Blumenthal, T.; Carrillo, M.; DiPaolo, G.; Esralew, L.; Gardiner, K.; Granholm, A.C.; Iqbal, K.; Krams, M.; Lemere, C.; et al. Down syndrome and Alzheimer’s disease: Common pathways, common goals. Alzheimers Dement. 2015, 11, 700–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaur, S.; Agnihotri, R. Alzheimer’s disease and chronic periodontitis: Is there an association? Geriatr. Gerontol. Int. 2015, 15, 391–404. [Google Scholar] [CrossRef] [PubMed]
- Ide, M.; Harris, M.; Stevens, A.; Sussams, R.; Hopkins, V.; Culliford, D.; Ibbett, P.; Raybould, R.; Thomas, R.; Puenter, U.; et al. Periodontitis and cognitive decline in Alzheimer’s disease. PLoS ONE 2016, 11, e0151081. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, K.D.; Lewis, H.C.; Hill, A.A.; Pandey, A.; Jackson, L.P.; Cabral, J.M.; Smith, K.P.; Liggett, L.A.; Gomez, E.B.; Galbraith, M.D.; et al. Trisomy 21 consistently activates the interferon response. eLife 2016, 5, e16220. [Google Scholar] [CrossRef]
- Sullivan, K.D.; Evans, D.; Pandey, A.; Hraha, T.H.; Smith, K.P.; Markham, N.; Rachubinski, A.L.; Wolter-Warmerdam, K.; Hickey, F.; Espinosa, J.M.; et al. Trisomy 21 causes changes in the circulating proteome indicative of chronic autoinflammation. Sci. Rep. 2017, 7, 14818. [Google Scholar] [CrossRef] [Green Version]
- Platanias, L.C. Mechanisms of type-I- and type-II-interferon-mediated signalling. Nat. Rev. Immunol. 2005, 5, 375–386. [Google Scholar] [CrossRef]
- Tanaka, M.H.; Giro, E.M.; Cavalcante, L.B.; Pires, J.R.; Apponi, L.H.; Valentini, S.R.; Spolidório, D.M.; Capela, M.V.; Rossa, C., Jr.; Scarel-Caminaga, R.M. Expression of interferon-γ, interferon-α and related genes in individuals with Down syndrome and periodontitis. Cytokine 2012, 60, 875–881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frankl, S.N.; Shiere, F.R.; Fogels, H.R. Should the parent remain with the child in the dental operatory? J. Dent. Child 1962, 29, 150–163. [Google Scholar]
- Albandar, J.M.; Susin, C.; Hughes, F.J. Manifestations of systemic diseases and conditions that affect the periodontal attachment apparatus: Case definitions and diagnostic considerations. J. Clin. Periodontol. 2018, 45, S171–S189. [Google Scholar] [CrossRef] [Green Version]
- Chapple, I.L.C.; Mealey, B.L.; Van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S74–S84. [Google Scholar] [CrossRef] [PubMed]
- Jyothy, A.; Rao, G.N.; Kumar, K.S.; Rao, V.B.; Devi, B.U.; Reddy, P.P. Translocation Down syndrome. Indian J. Med. Sci. 2002, 56, 122–126. [Google Scholar]
- Purcell, S.; Neale, B.; Todd-Brown, K.; Thomas, L.; Ferreira, M.A.R.; Bender, D.; Sham, P.C. PLINK: A Tool Set for Whole-Genome Association and Population-Based Linkage Analyses. Am. J. Hum. Genet. 2007, 81, 559–575. [Google Scholar] [CrossRef] [Green Version]
- Ionita-Laza, I.; Lee, S.; Makarov, V.; Buxbaum, J.D.; Lin, X. Sequence Kernel Association Tests for the Combined Effect of Rare and Common Variants. Am. J. Hum. Genet. 2013, 92, 841–853. [Google Scholar] [CrossRef] [Green Version]


| Marker | Gene | CHR | Minor Allele | N Total | p | OR (95% CI) | Genotypes (Dd + dd/DD) |
|---|---|---|---|---|---|---|---|
| rs4315121 | C12orf74 | 12 | T | 87 | 9.85 × 10−5 | 8.84 (3.03–25.77) | PD: 42/9 HP: 15/21 |
| rs4814890 | LOC101930064 | 20 | T | 87 | 9.61 × 10−5 | 0.13 (0.05–0.35) | PD: 18/33 HP: 29/7 |
| rs1549874 | KBTBD12 | 3 | G | 87 | 8.27 × 10−5 | 0.08 (0.02–0.29) | PD: 4/47 HP: 18/18 |
| rs11060842 | PIWIL1 | 12 | C | 86 | 7.82 × 10−5 | 9.05 (2.99–27.33) | PD: 44/7 HP: 16/19 |
| rs62030877 | C16orf82(upstr) | 16 | C | 87 | 8.92 × 10−5 | 0.14 (0.05–0.38) | PD: 10/41 HP: 23/13 |
| Gene | N Markers (Test) | p | SKAT |
|---|---|---|---|
| PIWIL1 | 47 (44) | 1.90 × 10−5 | SKAT w1 |
| MIR9-2 | 22 (22) | 3.76 × 10−5 | Burden |
| LOC101929147 | 26 (25) | 3.93 × 10−5 | SKAT w1 |
| LHCGR | 42 (35) | 1.04 × 10−4 | SKAT |
| LOC101928304 | 38 (35) | 1.33 × 10−4 | SKAT |
| TPR | 32 (15) | 1.51 × 10−4 | SKAT w1 |
| BCR | 43 (30) | 1.55 × 10−4 | Burden |
| DERL2 | 8 (3) | 1.76 × 10−4 | SKAT |
| CLRN1-AS1 | 37 (32) | 1.97 × 10−4 | Burden |
| LOC285501 | 32 (32) | 1.97 × 10−4 | SKAT |
| ACVRL1 | 14 (4) | 2.07 × 10−4 | Burden |
| PLCXD3 | 52 (49) | 2.50 × 10−4 | SKAT w1 |
| MIR15A | 7 (7) | 2.61 × 10−4 | Burden |
| AKR1D1 | 33 (24) | 3.03 × 10−4 | SKAT w1 |
| CDHR4 | 16 (6) | 3.07 × 10−4 | Burden |
| LSM8 | 28 (27) | 3.21 × 10−4 | SKAT w1 |
| CCDC60 | 96 (86) | 3.30 × 10−4 | SKAT w1 |
| CDCA2 | 76 (61) | 3.32 × 10−4 | SKAT w1 |
| GNA12 | 50 (49) | 3.34 × 10−4 | Buden |
| LOC646762 | 11 (10) | 3.57 × 10−4 | SKAT w1 |
| COA4 | 3 (3) | 3.70 × 10−4 | SKAT |
| MCHR1 | 17 (15) | 4.48 × 10−4 | SKAT |
| CACNG8 | 25 (23) | 4.91 × 10−4 | SKAT |
| BBS12 | 44 (23) | 4.92 × 10−4 | SKAT |
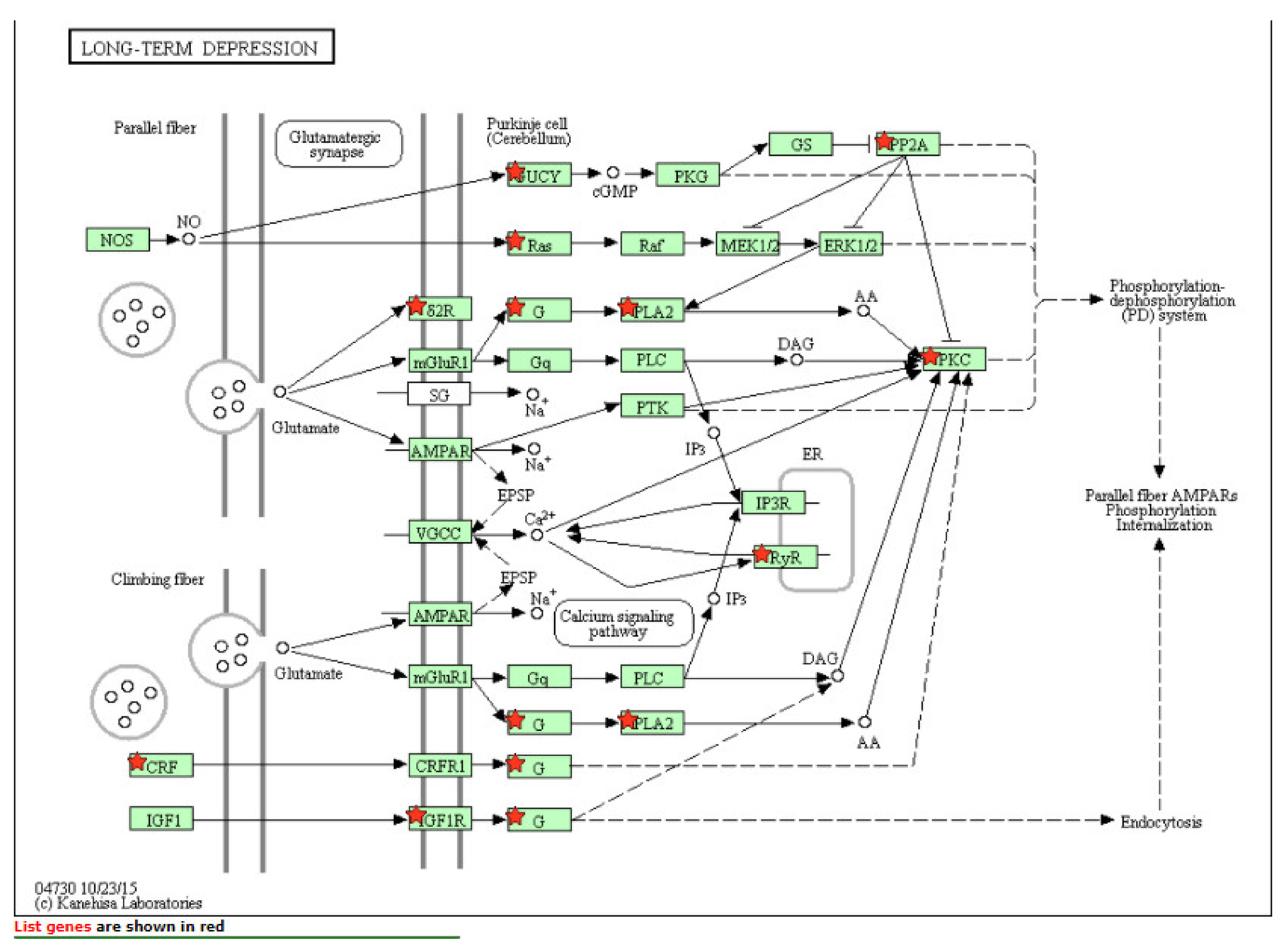
| Pathway | Genes (N) | p |
|---|---|---|
| Long-term depression pathway | 15 | 5.1 × 10−3 |
| FoxO signaling pathway | 25 | 1.2 × 10−2 |
| PI3K-Akt signaling pathway | 53 | 1.3 × 10−2 |
| Glutamatergic synapse | 22 | 1.3 × 10−2 |
| Rap1 signaling pathway | 35 | 1.5 × 10−2 |
| VEGF signaling pathway | 14 | 1.5 × 10−2 |
| Platelet activation | 24 | 1.6 × 10−2 |
| Malaria | 12 | 1.7 × 10−2 |
| Eph kinases and ephrins support platelet aggregation | 5 | 1.7 × 10−2 |
| Fat digestion and absorption | 10 | 2.4 × 10−2 |
| Ras signaling pathway | 36 | 2.5 × 10−2 |
| T-cell receptor signaling pathway | 19 | 2.6 × 10−2 |
| Hepatitis B | 25 | 2.9 × 10−2 |
| Wnt signaling pathway | 24 | 3.0 × 10−2 |
| Circadian entrainment | 18 | 3.1 × 10−2 |
| Primary bile acid biosynthesis | 6 | 3.3 × 10−2 |
| Fc epsilon RI signaling pathway | 14 | 3.4 × 10−2 |
| Signaling pathways regulating stem cell pluripotency | 24 | 3.4 × 10−2 |
| Rho-selective Guanine Exchange Factor AKAP13 Mediates Stress Fiber Formation | 5 | 3.6 × 10−2 |
| Fatty acid degradation | 10 | 3.8 × 10−2 |
| Wnt signaling pathway | 25 | 4.1 × 10−2 |
| TGF-beta signaling pathway | 16 | 4.2 × 10−2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández, M.; de Coo, A.; Quintela, I.; García, E.; Diniz-Freitas, M.; Limeres, J.; Diz, P.; Blanco, J.; Carracedo, Á.; Cruz, R. Genetic Susceptibility to Periodontal Disease in Down Syndrome: A Case-Control Study. Int. J. Mol. Sci. 2021, 22, 6274. https://doi.org/10.3390/ijms22126274
Fernández M, de Coo A, Quintela I, García E, Diniz-Freitas M, Limeres J, Diz P, Blanco J, Carracedo Á, Cruz R. Genetic Susceptibility to Periodontal Disease in Down Syndrome: A Case-Control Study. International Journal of Molecular Sciences. 2021; 22(12):6274. https://doi.org/10.3390/ijms22126274
Chicago/Turabian StyleFernández, María, Alicia de Coo, Inés Quintela, Eliane García, Márcio Diniz-Freitas, Jacobo Limeres, Pedro Diz, Juan Blanco, Ángel Carracedo, and Raquel Cruz. 2021. "Genetic Susceptibility to Periodontal Disease in Down Syndrome: A Case-Control Study" International Journal of Molecular Sciences 22, no. 12: 6274. https://doi.org/10.3390/ijms22126274
APA StyleFernández, M., de Coo, A., Quintela, I., García, E., Diniz-Freitas, M., Limeres, J., Diz, P., Blanco, J., Carracedo, Á., & Cruz, R. (2021). Genetic Susceptibility to Periodontal Disease in Down Syndrome: A Case-Control Study. International Journal of Molecular Sciences, 22(12), 6274. https://doi.org/10.3390/ijms22126274







