From Messengers to Receptors in Psoriasis: The Role of IL-17RA in Disease and Treatment
Abstract
:1. Psoriasis Pathogenesis in Context
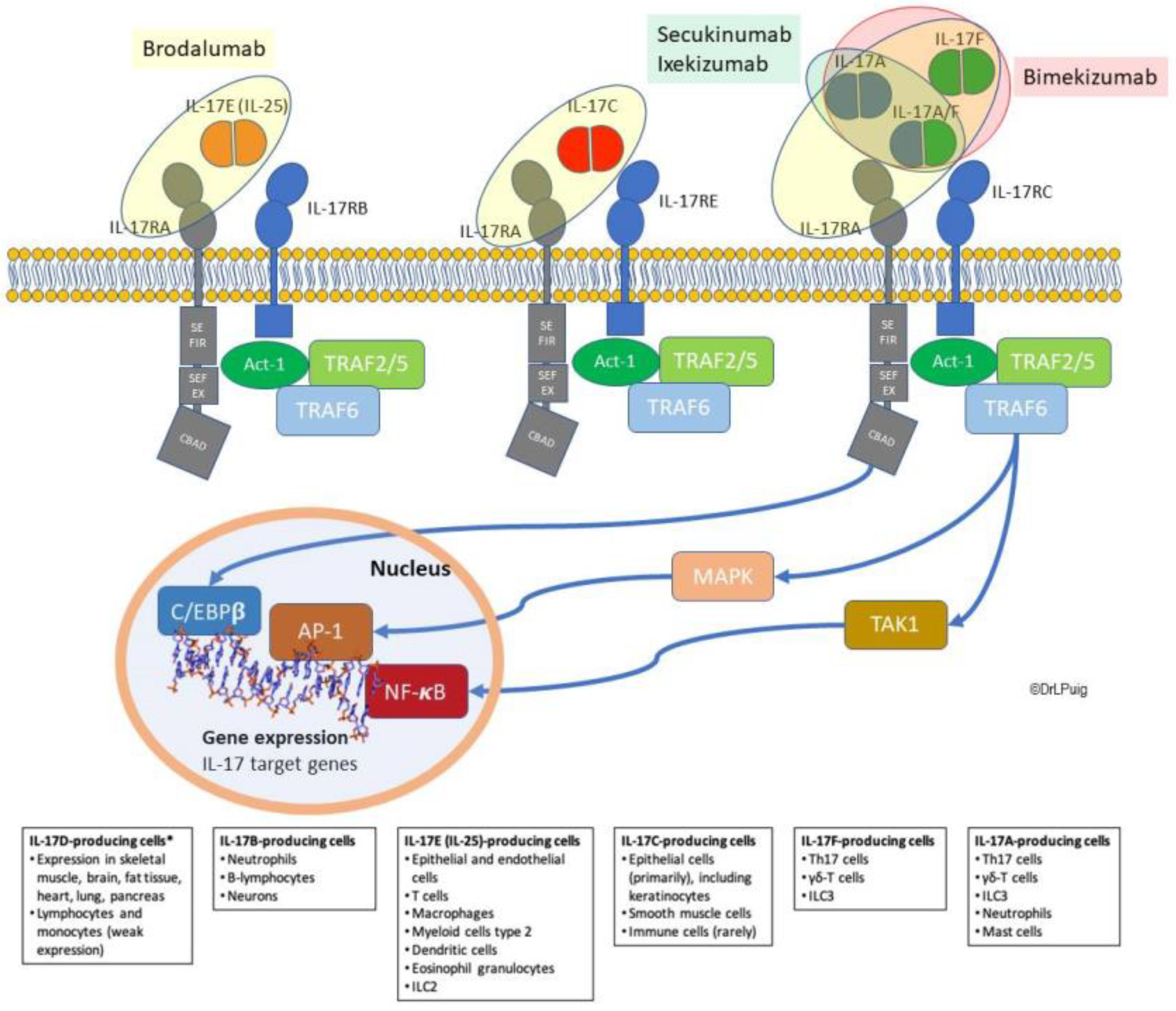
2. The IL-17 Pathogenic Route in Psoriasis
2.1. IL-17 Family Overview
2.2. IL-17 Isoforms and Their Roles in Psoriasis
2.2.1. IL-17A
2.2.2. IL-17F
2.2.3. IL-17C
2.2.4. IL-17E
2.2.5. IL-17B
2.2.6. IL-17D
2.3. IL-17 Isoforms beyond Psoriasis
2.4. IL-17R as Unique Receptors in Cytokine Signaling: Focus on IL-17RA
3. Targeting IL-17 Pathway in Psoriasis Treatment
3.1. Treatments Acting by Ligand Inhibition
3.1.1. Secukinumab
3.1.2. Ixekizumab
3.1.3. Bimekizumab
3.2. Treatments Acting by Receptor Blockade
Brodalumab
3.3. Potential Role of IL-17A/IL-17RA Blockade in Psoriasis Comorbid Conditions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CBAD | C/EBPβ-activation domain |
| C/EBP | CCAAT/enhancer-binding protein |
| CTLA8 | Cytotoxic T lymphocyte-associated antigen 8 |
| CV | Cardiovascular |
| DC | Dendritic cells |
| DEFB4 | β-defensin 4 |
| EGFR | Epidermal growth factor receptor |
| IGA mod 2011 | 2011 modified Investigator’s Global Assessment |
| ILC3 | Group 3 innate lymphoid cells |
| JNK | c-Jun N-terminal kinase |
| LSS | Lesion Severity Score |
| NAFLD | Non-alcoholic fatty liver disease |
| PASI | Psoriasis Area and Severity Index |
| PGA | Physician´s Global Assessment |
| RORC | RAR-related orphan receptor |
| SEFIR | SEF (similar expression to fibroblast growth factor genes)/IL-17 receptor |
| TIR | Toll/IL-1 receptor |
| TLR | Toll-like receptor |
| TNF | Tumor necrosis factor |
| TRAF6 | TNFR-associated factor 6 |
| VEGF | Vascular endothelial growth factor |
References
- Parisi, R.; Iskandar, I.Y.K.; Kontopantelis, E.; Augustin, M.; Griffiths, C.E.M.; Ashcroft, D.M. Global Psoriasis Atlas National, Regional, and Worldwide Epidemiology of Psoriasis: Systematic Analysis and Modelling Study. BMJ 2020, 369, m1590. [Google Scholar] [CrossRef] [PubMed]
- Rendon, A.; Schäkel, K. Psoriasis Pathogenesis and Treatment. Int. J. Mol. Sci. 2019, 20, 1475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armstrong, A.W.; Read, C. Pathophysiology, Clinical Presentation, and Treatment of Psoriasis: A Review. JAMA 2020, 323, 1945–1960. [Google Scholar] [CrossRef]
- Shuster, S. Research into Psoriasis—The Last Decade. Br. Med. J. 1971, 3, 236–239. [Google Scholar] [CrossRef] [Green Version]
- Bjerke, J.R. In Situ Characterization and Counting of Mononuclear Cells in Lesions of Different Clinical Forms of Psoriasis. Acta Derm Venereol. 1982, 62, 93–100. [Google Scholar] [PubMed]
- Bjerke, J.R. Subpopulations of Mononuclear Cells in Lesions of Psoriasis, Lichen Planus and Discoid Lupus Erythematosus Studied Using Monoclonal Antibodies. Acta Derm. Venereol. 1982, 62, 477–483. [Google Scholar]
- Hammar, H.; Gu, S.Q.; Johannesson, A.; Sundkvist, K.G.; Biberfeld, P. Subpopulations of Mononuclear Cells in Microscopic Lesions of Psoriatic Patients. Selective Accumulation of Suppressor/Cytotoxic T Cells in Epidermis during the Evolution of the Lesion. J. Invest. Derm. 1984, 83, 416–420. [Google Scholar] [CrossRef] [Green Version]
- Mueller, W.; Herrmann, B. Cyclosporin A for Psoriasis. N. Engl. J. Med. 1979, 301, 555. [Google Scholar] [CrossRef]
- Ellis, C.N.; Gorsulowsky, D.C.; Hamilton, T.A.; Billings, J.K.; Brown, M.D.; Headington, J.T.; Cooper, K.D.; Baadsgaard, O.; Duell, E.A.; Annesley, T.M. Cyclosporine Improves Psoriasis in a Double-Blind Study. JAMA 1986, 256, 3110–3116. [Google Scholar] [CrossRef]
- Jegasothy, B.V.; Ackerman, C.D.; Todo, S.; Fung, J.J.; Abu-Elmagd, K.; Starzl, T.E. Tacrolimus (FK 506)—A New Therapeutic Agent for Severe Recalcitrant Psoriasis. Arch. Derm. 1992, 128, 781–785. [Google Scholar] [CrossRef] [Green Version]
- Gottlieb, S.L.; Gilleaudeau, P.; Johnson, R.; Estes, L.; Woodworth, T.G.; Gottlieb, A.B.; Krueger, J.G. Response of Psoriasis to a Lymphocyte-Selective Toxin (DAB389IL-2) Suggests a Primary Immune, but Not Keratinocyte, Pathogenic Basis. Nat. Med. 1995, 1, 442–447. [Google Scholar] [CrossRef]
- Mosmann, T.R.; Cherwinski, H.; Bond, M.W.; Giedlin, M.A.; Coffman, R.L. Two Types of Murine Helper T Cell Clone. I. Definition According to Profiles of Lymphokine Activities and Secreted Proteins. J. Immunol. 1986, 136, 2348–2357. [Google Scholar] [PubMed]
- Yawalkar, N.; Karlen, S.; Hunger, R.; Brand, C.U.; Braathen, L.R. Expression of Interleukin-12 Is Increased in Psoriatic Skin. J. Invest. Derm. 1998, 111, 1053–1057. [Google Scholar] [CrossRef]
- Mease, P.J.; Goffe, B.S.; Metz, J.; VanderStoep, A.; Finck, B.; Burge, D.J. Etanercept in the Treatment of Psoriatic Arthritis and Psoriasis: A Randomised Trial. Lancet 2000, 356, 385–390. [Google Scholar] [CrossRef]
- Chaudhari, U.; Romano, P.; Mulcahy, L.D.; Dooley, L.T.; Baker, D.G.; Gottlieb, A.B. Efficacy and Safety of Infliximab Monotherapy for Plaque-Type Psoriasis: A Randomised Trial. Lancet 2001, 357, 1842–1847. [Google Scholar] [CrossRef]
- Papoutsaki, M.; Chimenti, M.-S.; Costanzo, A.; Talamonti, M.; Zangrilli, A.; Giunta, A.; Bianchi, L.; Chimenti, S. Adalimumab for Severe Psoriasis and Psoriatic Arthritis: An Open-Label Study in 30 Patients Previously Treated with Other Biologics. J. Am. Acad. Derm. 2007, 57, 269–275. [Google Scholar] [CrossRef]
- Oppmann, B.; Lesley, R.; Blom, B.; Timans, J.C.; Xu, Y.; Hunte, B.; Vega, F.; Yu, N.; Wang, J.; Singh, K.; et al. Novel P19 Protein Engages IL-12p40 to Form a Cytokine, IL-23, with Biological Activities Similar as Well as Distinct from IL. Immunity 2000, 13, 715–725. [Google Scholar] [CrossRef] [Green Version]
- Aggarwal, S.; Ghilardi, N.; Xie, M.-H.; de Sauvage, F.J.; Gurney, A.L. Interleukin-23 Promotes a Distinct CD4 T Cell Activation State Characterized by the Production of Interleukin. J. Biol. Chem. 2003, 278, 1910–1914. [Google Scholar] [CrossRef] [Green Version]
- Wilson, N.J.; Boniface, K.; Chan, J.R.; McKenzie, B.S.; Blumenschein, W.M.; Mattson, J.D.; Basham, B.; Smith, K.; Chen, T.; Morel, F.; et al. Development, Cytokine Profile and Function of Human Interleukin 17-Producing Helper T Cells. Nat. Immunol. 2007, 8, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Langrish, C.L.; Chen, Y.; Blumenschein, W.M.; Mattson, J.; Basham, B.; Sedgwick, J.D.; McClanahan, T.; Kastelein, R.A.; Cua, D.J. IL-23 Drives a Pathogenic T Cell Population That Induces Autoimmune Inflammation. J. Exp. Med. 2005, 201, 233–240. [Google Scholar] [CrossRef] [Green Version]
- Louten, J.; Boniface, K.; de Waal Malefyt, R. Development and Function of TH17 Cells in Health and Disease. J. Allergy Clin. Immunol. 2009, 123, 1004–1011. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Trepicchio, W.L.; Oestreicher, J.L.; Pittman, D.; Wang, F.; Chamian, F.; Dhodapkar, M.; Krueger, J.G. Increased Expression of Interleukin 23 P19 and P40 in Lesional Skin of Patients with Psoriasis Vulgaris. J. Exp. Med. 2004, 199, 125–130. [Google Scholar] [CrossRef]
- Chen, X.; Tan, Z.; Yue, Q.; Liu, H.; Liu, Z.; Li, J. The Expression of Interleukin-23 (P19/P40) and Interleukin-12 (P35/P40) in Psoriasis Skin. J. Huazhong Univ. Sci. Technol. Med. Sci. 2006, 26, 750–752. [Google Scholar] [CrossRef] [PubMed]
- Piskin, G.; Sylva-Steenland, R.M.R.; Bos, J.D.; Teunissen, M.B.M. In Vitro and in Situ Expression of IL-23 by Keratinocytes in Healthy Skin and Psoriasis Lesions: Enhanced Expression in Psoriatic Skin. J. Immunol. 2006, 176, 1908–1915. [Google Scholar] [CrossRef] [PubMed]
- Schön, M.P.; Erpenbeck, L. The Interleukin-23/Interleukin-17 Axis Links Adaptive and Innate Immunity in Psoriasis. Front. Immunol. 2018, 9, 1323. [Google Scholar] [CrossRef] [Green Version]
- Lauffer, F.; Eyerich, K.; Boehncke, W.-H.; Asadullah, K.; Beissert, S.; Ghoreschi, K.; Schön, M.P. Cytokines of the IL-17 Family in Psoriasis. J. Dtsch. Derm. Ges. 2020, 18, 675–681. [Google Scholar] [CrossRef]
- Gaffen, S.L. Structure and Signalling in the IL-17 Receptor Family. Nat. Rev. Immunol. 2009, 9, 556–567. [Google Scholar] [CrossRef] [Green Version]
- Kolls, J.K.; Lindén, A. Interleukin-17 Family Members and Inflammation. Immunity 2004, 21, 467–476. [Google Scholar] [CrossRef] [Green Version]
- Rouvier, E.; Luciani, M.F.; Mattéi, M.G.; Denizot, F.; Golstein, P. CTLA-8, Cloned from an Activated T Cell, Bearing AU-Rich Messenger RNA Instability Sequences, and Homologous to a Herpesvirus Saimiri Gene. J. Immunol. 1993, 150, 5445–5456. [Google Scholar]
- McGeachy, M.J.; Cua, D.J.; Gaffen, S.L. The IL-17 Family of Cytokines in Health and Disease. Immunity 2019, 50, 892–906. [Google Scholar] [CrossRef]
- Hymowitz, S.G.; Filvaroff, E.H.; Yin, J.P.; Lee, J.; Cai, L.; Risser, P.; Maruoka, M.; Mao, W.; Foster, J.; Kelley, R.F.; et al. IL-17s Adopt a Cystine Knot Fold: Structure and Activity of a Novel Cytokine, IL-17F, and Implications for Receptor Binding. Embo J. 2001, 20, 5332–5341. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Song, X.; Chrunyk, B.A.; Shanker, S.; Hoth, L.R.; Marr, E.S.; Griffor, M.C. Crystal Structures of Interleukin 17A and Its Complex with IL-17 Receptor, A. Nat. Commun. 2013, 4, 1888. [Google Scholar] [CrossRef] [PubMed]
- Brembilla, N.C.; Senra, L.; Boehncke, W.-H. The IL-17 Family of Cytokines in Psoriasis: IL-17A and Beyond. Front. Immunol. 2018, 9, 1682. [Google Scholar] [CrossRef] [Green Version]
- Monin, L.; Gaffen, S.L. Interleukin 17 Family Cytokines: Signaling Mechanisms, Biological Activities, and Therapeutic Implications. Cold Spring Harb. Perspect. Biol. 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Ramirez-Carrozzi, V.; Ota, N.; Sambandam, A.; Wong, K.; Hackney, J.; Martinez-Martin, N.; Ouyang, W.; Pappu, R. Cutting Edge: IL-17B Uses IL-17RA and IL-17RB to Induce Type 2 Inflammation from Human Lymphocytes. J. Immunol. 2019, 202, 1935–1941. [Google Scholar] [CrossRef] [Green Version]
- Swaidani, S.; Liu, C.; Zhao, J.; Bulek, K.; Li, X. TRAF Regulation of IL-17 Cytokine Signaling. Front. Immunol. 2019, 10, 1293. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.; Kolls, J.K. Interleukin-17A (IL17A). Gene 2017, 614, 8–14. [Google Scholar] [CrossRef] [Green Version]
- Beringer, A.; Noack, M.; Miossec, P. IL-17 in Chronic Inflammation: From Discovery to Targeting. Trends Mol. Med. 2016, 22, 230–241. [Google Scholar] [CrossRef]
- Furue, M.; Furue, K.; Tsuji, G.; Nakahara, T. Interleukin-17A and Keratinocytes in Psoriasis. Int. J. Mol. Sci. 2020, 21, 1275. [Google Scholar] [CrossRef] [Green Version]
- Heidenreich, R.; Röcken, M.; Ghoreschi, K. Angiogenesis Drives Psoriasis Pathogenesis. Int. J. Exp. Pathol. 2009, 90, 232–248. [Google Scholar] [CrossRef]
- Numasaki, M.; Tsukamoto, H.; Tomioka, Y.; Nishioka, Y.; Ohrui, T. A Heterodimeric Cytokine, Consisting of IL-17A and IL-17F, Promotes Migration and Capillary-Like Tube Formation of Human Vascular Endothelial Cells. Tohoku J. Exp. Med. 2016, 240, 47–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ishigame, H.; Kakuta, S.; Nagai, T.; Kadoki, M.; Nambu, A.; Komiyama, Y.; Fujikado, N.; Tanahashi, Y.; Akitsu, A.; Kotaki, H.; et al. Differential Roles of Interleukin-17A and -17F in Host Defense against Mucoepithelial Bacterial Infection and Allergic Responses. Immunity 2009, 30, 108–119. [Google Scholar] [CrossRef] [Green Version]
- Burns, L.A.; Maroof, A.; Marshall, D.; Steel, K.J.A.; Lalnunhlimi, S.; Cole, S.; Catrina, A.; Kirkham, B.; Taams, L.S. Presence, Function, and Regulation of IL-17F-Expressing Human CD4+ T Cells. Eur J. Immunol. 2020, 50, 568–580. [Google Scholar] [CrossRef] [Green Version]
- Johansen, C.; Usher, P.A.; Kjellerup, R.B.; Lundsgaard, D.; Iversen, L.; Kragballe, K. Characterization of the Interleukin-17 Isoforms and Receptors in Lesional Psoriatic Skin. Br. J. Dermatol. 2009, 160, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Soderstrom, C.; Berstein, G.; Zhang, W.; Valdez, H.; Fitz, L.; Kuhn, M.; Fraser, S. Ultra-Sensitive Measurement of IL-17A and IL-17F in Psoriasis Patient Serum and Skin. AAPS J. 2017, 19, 1218–1222. [Google Scholar] [CrossRef] [PubMed]
- Pantelyushin, S.; Haak, S.; Ingold, B.; Kulig, P.; Heppner, F.L.; Navarini, A.A.; Becher, B. Rorγt+ Innate Lymphocytes and Γδ T Cells Initiate Psoriasiform Plaque Formation in Mice. J. Clin. Invest. 2012, 122, 2252–2256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramirez-Carrozzi, V.; Sambandam, A.; Luis, E.; Lin, Z.; Jeet, S.; Lesch, J.; Hackney, J.; Kim, J.; Zhou, M.; Lai, J.; et al. IL-17C Regulates the Innate Immune Function of Epithelial Cells in an Autocrine Manner. Nat. Immunol. 2011, 12, 1159–1166. [Google Scholar] [CrossRef]
- Butcher, M.J.; Waseem, T.C.; Galkina, E.V. Smooth Muscle Cell-Derived Interleukin-17C Plays an Atherogenic Role via the Recruitment of Proinflammatory Interleukin-17A+ T Cells to the Aorta. Arter. Thromb Vasc. Biol. 2016, 36, 1496–1506. [Google Scholar] [CrossRef] [Green Version]
- Nies, J.F.; Panzer, U. IL-17C/IL-17RE: Emergence of a Unique Axis in TH17 Biology. Front. Immunol. 2020, 11, 341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnston, A.; Fritz, Y.; Dawes, S.M.; Diaconu, D.; Al-Attar, P.M.; Guzman, A.M.; Chen, C.S.; Fu, W.; Gudjonsson, J.E.; McCormick, T.S.; et al. Keratinocyte Overexpression of IL-17C Promotes Psoriasiform Skin Inflammation. J. Immunol. 2013, 190, 2252–2262. [Google Scholar] [CrossRef] [Green Version]
- Vandeghinste, N.; Klattig, J.; Jagerschmidt, C.; Lavazais, S.; Marsais, F.; Haas, J.D.; Auberval, M.; Lauffer, F.; Moran, T.; Ongenaert, M.; et al. Neutralization of IL-17C Reduces Skin Inflammation in Mouse Models of Psoriasis and Atopic Dermatitis. J. Invest. Derm. 2018, 138, 1555–1563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borowczyk, J.; Shutova, M.; Brembilla, N.C.; Boehncke, W.-H. IL-25 (IL-17E) in Epithelial Immunology and Pathophysiology. J. Allergy Clin. Immunol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Lu, H.; Lee, Y.-H.; Wu, Y.; Liu, K.; Shi, Y.; An, H.; Zhang, J.; Wang, X.; Lai, Y.; et al. An Interleukin-25-Mediated Autoregulatory Circuit in Keratinocytes Plays a Pivotal Role in Psoriatic Skin Inflammation. Immunity 2018, 48, 787–798.e4. [Google Scholar] [CrossRef] [Green Version]
- Senra, L.; Stalder, R.; Martinez, D.A.; Chizzolini, C.; Boehncke, W.-H.; Brembilla, N.C. Keratinocyte-Derived IL-17E Contributes to Inflammation in Psoriasis. J. Invest. Derm. 2016, 136, 1970–1980. [Google Scholar] [CrossRef] [Green Version]
- Senra, L.; Mylonas, A.; Kavanagh, R.D.; Fallon, P.G.; Conrad, C.; Borowczyk-Michalowska, J.; Wrobel, L.J.; Kaya, G.; Yawalkar, N.; Boehncke, W.-H.; et al. IL-17E (IL-25) Enhances Innate Immune Responses during Skin Inflammation. J. Invest. Derm. 2019, 139, 1732–1742.e17. [Google Scholar] [CrossRef] [PubMed]
- Bie, Q.; Jin, C.; Zhang, B.; Dong, H. IL-17B: A New Area of Study in the IL-17 Family. Mol. Immunol. 2017, 90, 50–56. [Google Scholar] [CrossRef]
- Kouri, V.-P.; Olkkonen, J.; Ainola, M.; Li, T.-F.; Björkman, L.; Konttinen, Y.T.; Mandelin, J. Neutrophils Produce Interleukin-17B in Rheumatoid Synovial Tissue. Rheumatology 2014, 53, 39–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Sun, S.; Liu, D. IL-17D: A Less Studied Cytokine of IL-17 Family. Int Arch. Allergy Immunol. 2020, 181, 618–623. [Google Scholar] [CrossRef]
- Boehncke, W.-H.; Schön, M.P. Psoriasis. Lancet 2015, 386, 983–994. [Google Scholar] [CrossRef]
- Boehncke, W.-H. Systemic Inflammation and Cardiovascular Comorbidity in Psoriasis Patients: Causes and Consequences. Front. Immunol. 2018, 9, 579. [Google Scholar] [CrossRef] [PubMed]
- Karbach, S.; Hobohm, L.; Wild, J.; Münzel, T.; Gori, T.; Wegner, J.; Steinbrink, K.; Wenzel, P.; Keller, K. Impact of Psoriasis on Mortality Rate and Outcome in Myocardial Infarction. J. Am. Heart Assoc. 2020, 9, e016956. [Google Scholar] [CrossRef]
- Menter, A.; Krueger, G.G.; Paek, S.Y.; Kivelevitch, D.; Adamopoulos, I.E.; Langley, R.G. Interleukin-17 and Interleukin-23: A Narrative Review of Mechanisms of Action in Psoriasis and Associated Comorbidities. Dermatology 2021. [Google Scholar] [CrossRef]
- Nordlohne, J.; von Vietinghoff, S. Interleukin 17A in Atherosclerosis—Regulation and Pathophysiologic Effector Function. Cytokine 2019, 122, 154089. [Google Scholar] [CrossRef] [PubMed]
- von Stebut, E.; Boehncke, W.-H.; Ghoreschi, K.; Gori, T.; Kaya, Z.; Thaci, D.; Schäffler, A. IL-17A in Psoriasis and Beyond: Cardiovascular and Metabolic Implications. Front. Immunol. 2019, 10, 3096. [Google Scholar] [CrossRef] [Green Version]
- Karbach, S.; Croxford, A.L.; Oelze, M.; Schüler, R.; Minwegen, D.; Wegner, J.; Koukes, L.; Yogev, N.; Nikolaev, A.; Reißig, S.; et al. Interleukin 17 Drives Vascular Inflammation, Endothelial Dysfunction, and Arterial Hypertension in Psoriasis-like Skin Disease. Arter. Thromb. Vasc. Biol. 2014, 34, 2658–2668. [Google Scholar] [CrossRef] [Green Version]
- Malecic, N.; Young, H.S. Excessive Angiogenesis Associated with Psoriasis as a Cause for Cardiovascular Ischaemia. Exp. Derm. 2017, 26, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Mercurio, L.; Failla, C.M.; Capriotti, L.; Scarponi, C.; Facchiano, F.; Morelli, M.; Rossi, S.; Pagnanelli, G.; Albanesi, C.; Cavani, A.; et al. Interleukin (IL)-17/IL-36 Axis Participates to the Crosstalk between Endothelial Cells and Keratinocytes during Inflammatory Skin Responses. PLoS ONE 2020, 15, e0222969. [Google Scholar] [CrossRef] [PubMed]
- Schüler, R.; Brand, A.; Klebow, S.; Wild, J.; Veras, F.P.; Ullmann, E.; Roohani, S.; Kolbinger, F.; Kossmann, S.; Wohn, C.; et al. Antagonization of IL-17A Attenuates Skin Inflammation and Vascular Dysfunction in Mouse Models of Psoriasis. J. Invest. Derm. 2019, 139, 638–647. [Google Scholar] [CrossRef] [Green Version]
- Makavos, G.; Ikonomidis, I.; Andreadou, I.; Varoudi, M.; Kapniari, I.; Loukeri, E.; Theodoropoulos, K.; Pavlidis, G.; Triantafyllidi, H.; Thymis, J.; et al. Effects of Interleukin 17A Inhibition on Myocardial Deformation and Vascular Function in Psoriasis. Can. J. Cardiol. 2020, 36, 100–111. [Google Scholar] [CrossRef]
- Kotronen, A.; Yki-Järvinen, H. Fatty Liver: A Novel Component of the Metabolic Syndrome. Arter. Thromb Vasc Biol. 2008, 28, 27–38. [Google Scholar] [CrossRef]
- Mantovani, A.; Gisondi, P.; Lonardo, A.; Targher, G. Relationship between Non-Alcoholic Fatty Liver Disease and Psoriasis: A Novel Hepato-Dermal Axis? Int. J. Mol. Sci. 2016, 17, 217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carrascosa, J.M.; Bonanad, C.; Dauden, E.; Botella, R.; Olveira-Martín, A. En nombre del Grupo de Trabajo en Inflamación Sistémica en Psoriasis Psoriasis and Nonalcoholic Fatty Liver Disease. Actas Dermosifiliogr. 2017, 108, 506–514. [Google Scholar] [CrossRef] [PubMed]
- Candia, R.; Ruiz, A.; Torres-Robles, R.; Chávez-Tapia, N.; Méndez-Sánchez, N.; Arrese, M. Risk of Non-Alcoholic Fatty Liver Disease in Patients with Psoriasis: A Systematic Review and Meta-Analysis. J. Eur. Acad. Derm. Venereol. 2015, 29, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Romero-Pérez, D.; Belinchón-Romero, I.; Bellot, P.; Francés, R.; Marco, F.; Ramos-Rincón, J.M. Nonalcoholic Fatty Liver Disease Puts Patients with Psoriasis at Greater Cardiovascular Risk. Australas J. Derm. 2019, 60, e304–e310. [Google Scholar] [CrossRef]
- Rau, M.; Schilling, A.-K.; Meertens, J.; Hering, I.; Weiss, J.; Jurowich, C.; Kudlich, T.; Hermanns, H.M.; Bantel, H.; Beyersdorf, N.; et al. Progression from Nonalcoholic Fatty Liver to Nonalcoholic Steatohepatitis Is Marked by a Higher Frequency of Th17 Cells in the Liver and an Increased Th17/Resting Regulatory T Cell Ratio in Peripheral Blood and in the Liver. J. Immunol. 2016, 196, 97–105. [Google Scholar] [CrossRef]
- Harley, I.T.W.; Stankiewicz, T.E.; Giles, D.A.; Softic, S.; Flick, L.M.; Cappelletti, M.; Sheridan, R.; Xanthakos, S.A.; Steinbrecher, K.A.; Sartor, R.B.; et al. IL-17 Signaling Accelerates the Progression of Nonalcoholic Fatty Liver Disease in Mice. Hepatology 2014, 59, 1830–1839. [Google Scholar] [CrossRef]
- Giles, D.A.; Moreno-Fernandez, M.E.; Divanovic, S. IL-17 Axis Driven Inflammation in Non-Alcoholic Fatty Liver Disease Progression. Curr. Drug Targets 2015, 16, 1315–1323. [Google Scholar] [CrossRef] [Green Version]
- Su, Y.; Huang, J.; Zhao, X.; Lu, H.; Wang, W.; Yang, X.O.; Shi, Y.; Wang, X.; Lai, Y.; Dong, C. Interleukin-17 Receptor D Constitutes an Alternative Receptor for Interleukin-17A Important in Psoriasis-like Skin Inflammation. Sci. Immunol. 2019, 4. [Google Scholar] [CrossRef]
- Goepfert, A.; Lehmann, S.; Blank, J.; Kolbinger, F.; Rondeau, J.-M. Structural Analysis Reveals That the Cytokine IL-17F Forms a Homodimeric Complex with Receptor IL-17RC to Drive IL-17RA-Independent Signaling. Immunity 2020, 52, 499–512.e5. [Google Scholar] [CrossRef]
- Ely, L.K.; Fischer, S.; Garcia, K.C. Structural Basis of Receptor Sharing by Interleukin 17 Cytokines. Nat. Immunol. 2009, 10, 1245–1251. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Swaidani, S.; Qian, W.; Kang, Z.; Sun, P.; Han, Y.; Wang, C.; Gulen, M.F.; Yin, W.; Zhang, C.; et al. A CC’ Loop Decoy Peptide Blocks the Interaction between Act1 and IL-17RA to Attenuate IL-17- and IL-25-Induced Inflammation. Sci. Signal. 2011, 4, ra72. [Google Scholar] [CrossRef] [Green Version]
- Qian, Y.; Liu, C.; Hartupee, J.; Altuntas, C.Z.; Gulen, M.F.; Jane-Wit, D.; Xiao, J.; Lu, Y.; Giltiay, N.; Liu, J.; et al. The Adaptor Act1 Is Required for Interleukin 17-Dependent Signaling Associated with Autoimmune and Inflammatory Disease. Nat. Immunol. 2007, 8, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Zepp, J.A.; Qian, W.; Martin, B.N.; Ouyang, W.; Yin, W.; Bunting, K.D.; Aronica, M.; Erzurum, S.; Li, X. A Novel IL-25 Signaling Pathway through Stat5. J. Immunol. 2015, 194, 4528–4534. [Google Scholar] [CrossRef] [Green Version]
- Chiricozzi, A.; Guttman-Yassky, E.; Suárez-Fariñas, M.; Nograles, K.E.; Tian, S.; Cardinale, I.; Chimenti, S.; Krueger, J.G. Integrative Responses to IL-17 and TNF-α in Human Keratinocytes Account for Key Inflammatory Pathogenic Circuits in Psoriasis. J. Invest. Derm. 2011, 131, 677–687. [Google Scholar] [CrossRef]
- Krueger, J.G.; Brunner, P.M. Interleukin-17 Alters the Biology of Many Cell Types Involved in the Genesis of Psoriasis, Systemic Inflammation and Associated Comorbidities. Exp. Dermatol. 2018, 27, 115–123. [Google Scholar] [CrossRef] [Green Version]
- Guo, L.; Louis, I.V.-S.; Bohjanen, P.R. Post-Transcriptional Regulation of Cytokine Expression and Signaling. Curr. Trends Immunol. 2018, 19, 33–40. [Google Scholar] [PubMed]
- Herjan, T.; Hong, L.; Bubenik, J.; Bulek, K.; Qian, W.; Liu, C.; Li, X.; Chen, X.; Yang, H.; Ouyang, S.; et al. IL-17 Receptor-Associated Adaptor Act1 Directly Stabilizes MRNAs to Mediate IL-17 Inflammatory Signaling. Nat. Immunol. 2018, 19, 354–365. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Cai, G.; Liu, C.; Zhao, J.; Gu, C.; Wu, L.; Hamilton, T.A.; Zhang, C.; Ko, J.; Zhu, L.; et al. IL-17R–EGFR Axis Links Wound Healing to Tumorigenesis in Lrig1+ Stem Cells. J. Exp. Med. 2018, 216, 195–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurte, M.; Luz-Crawford, P.; Vega-Letter, A.M.; Contreras, R.A.; Tejedor, G.; Elizondo-Vega, R.; Martinez-Viola, L.; Fernández-O’Ryan, C.; Figueroa, F.E.; Jorgensen, C.; et al. IL17/IL17RA as a Novel Signaling Axis Driving Mesenchymal Stem Cell Therapeutic Function in Experimental Autoimmune Encephalomyelitis. Front. Immunol. 2018, 9, 802. [Google Scholar] [CrossRef]
- Shen, F.; Hu, Z.; Goswami, J.; Gaffen, S.L. Identification of Common Transcriptional Regulatory Elements in Interleukin-17 Target Genes. J. Biol. Chem. 2006, 281, 24138–24148. [Google Scholar] [CrossRef] [Green Version]
- Yao, Z.; Fanslow, W.C.; Seldin, M.F.; Rousseau, A.-M.; Painter, S.L.; Comeau, M.R.; Cohen, J.I.; Spriggs, M.K. Herpesvirus Saimiri Encodes a New Cytokine, IL-17, Which Binds to a Novel Cytokine Receptor. J. Immunol. 2011, 187, 4392–4402. [Google Scholar] [CrossRef] [Green Version]
- Lindemann, M.J.; Hu, Z.; Benczik, M.; Liu, K.D.; Gaffen, S.L. Differential Regulation of the IL-17 Receptor by Gammac Cytokines: Inhibitory Signaling by the Phosphatidylinositol 3-Kinase Pathway. J. Biol. Chem. 2008, 283, 14100–14108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, L.; Hu, Y.; Xu, J.; Guo, J.; Tu, J.; Yin, Z. Ultraviolet B Inhibits IL-17A/TNF-α-Stimulated Activation of Human Dermal Fibroblasts by Decreasing the Expression of IL-17RA and IL-17RC on Fibroblasts. Front. Immunol. 2017, 8. [Google Scholar] [CrossRef] [Green Version]
- European Medicines Agency (EMA). Cosentyx (Secukinumab). European Public Assessment Report (EPAR); EMA: Brussels, Belgium, 2015. [Google Scholar]
- Hueber, W.; Patel, D.D.; Dryja, T.; Wright, A.M.; Koroleva, I.; Bruin, G.; Antoni, C.; Draelos, Z.; Gold, M.H.; Psoriasis Study Group; et al. Effects of AIN457, a Fully Human Antibody to Interleukin-17A, on Psoriasis, Rheumatoid Arthritis, and Uveitis. Sci. Transl. Med. 2010, 2, 52ra72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaleel, T.; Elmets, C.; Weinkle, A.; Kassira, S.; Elewski, B. Secukinumab (AIN-457) for the Treatment of Psoriasis. Expert Rev. Clin. Pharm. 2016, 9, 187–202. [Google Scholar] [CrossRef]
- Ly, K.; Smith, M.P.; Thibodeaux, Q.; Reddy, V.; Liao, W.; Bhutani, T. Anti IL-17 in Psoriasis. Expert Rev. Clin. Immunol. 2019, 15, 1185–1194. [Google Scholar] [CrossRef] [PubMed]
- Langley, R.G.; Elewski, B.E.; Lebwohl, M.; Reich, K.; Griffiths, C.E.M.; Papp, K.; Puig, L.; Nakagawa, H.; Spelman, L.; Sigurgeirsson, B.; et al. Secukinumab in Plaque Psoriasis—Results of Two Phase 3 Trials. N. Engl. J. Med. 2014, 371, 326–338. [Google Scholar] [CrossRef] [Green Version]
- Napolitano, M.; Megna, M.; Fabbrocini, G.; Nisticò, S.P.; Balato, N.; Dastoli, S.; Patruno, C. Eczematous Eruption during Anti-Interleukin 17 Treatment of Psoriasis: An Emerging Condition. Br. J. Dermatol. 2019, 181, 604–606. [Google Scholar] [CrossRef] [PubMed]
- Caldarola, G.; Pirro, F.; Stefani, A.D.; Talamonti, M.; Galluzzo, M.; D’Adamio, S.; Magnano, M.; Bernardini, N.; Malagoli, P.; Bardazzi, F.; et al. Clinical and Histopathological Characterization of Eczematous Eruptions Occurring in Course of Anti IL-17 Treatment: A Case Series and Review of the Literature. Expert Opin. Biol. Ther. 2020, 20, 665–672. [Google Scholar] [CrossRef] [PubMed]
- European Medicines Agency (EMA). Taltz (Ixezumab). European Public Assessment Report (EPAR); EMA: Brussels, Belgium, 2016. [Google Scholar]
- Krueger, J.G.; Fretzin, S.; Suárez-Fariñas, M.; Haslett, P.A.; Phipps, K.M.; Cameron, G.S.; McColm, J.; Katcherian, A.; Cueto, I.; White, T.; et al. IL-17A Is Essential for Cell Activation and Inflammatory Gene Circuits in Subjects with Psoriasis. J. Allergy Clin. Immunol. 2012, 130, 145–154.e9. [Google Scholar] [CrossRef] [Green Version]
- Craig, S.; Warren, R.B. Ixekizumab for the Treatment of Psoriasis: Up-to-Date. Expert Opin. Biol. 2020, 20, 549–557. [Google Scholar] [CrossRef]
- Langley, R.G.; Kimball, A.B.; Nak, H.; Xu, W.; Pangallo, B.; Osuntokun, O.O.; Agada, N.; Reich, K. Long-Term Safety Profile of Ixekizumab in Patients with Moderate-to-Severe Plaque Psoriasis: An Integrated Analysis from 11 Clinical Trials. J. Eur Acad Derm. Venereol. 2019, 33, 333–339. [Google Scholar] [CrossRef]
- Glatt, S.; Helmer, E.; Haier, B.; Strimenopoulou, F.; Price, G.; Vajjah, P.; Harari, O.A.; Lambert, J.; Shaw, S. First-in-Human Randomized Study of Bimekizumab, a Humanized Monoclonal Antibody and Selective Dual Inhibitor of IL-17A and IL-17F, in Mild Psoriasis. Br. J. Clin. Pharm. 2017, 83, 991–1001. [Google Scholar] [CrossRef] [PubMed]
- Glatt, S.; Baeten, D.; Baker, T.; Griffiths, M.; Ionescu, L.; Lawson, A.D.G.; Maroof, A.; Oliver, R.; Popa, S.; Strimenopoulou, F.; et al. Dual IL-17A and IL-17F Neutralisation by Bimekizumab in Psoriatic Arthritis: Evidence from Preclinical Experiments and a Randomised Placebo-Controlled Clinical Trial That IL-17F Contributes to Human Chronic Tissue Inflammation. Ann. Rheum. Dis. 2018, 77, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Papp, K.A.; Merola, J.F.; Gottlieb, A.B.; Griffiths, C.E.M.; Cross, N.; Peterson, L.; Cioffi, C.; Blauvelt, A. Dual Neutralization of Both Interleukin 17A and Interleukin 17F with Bimekizumab in Patients with Psoriasis: Results from BE ABLE 1, a 12-Week Randomized, Double-Blinded, Placebo-Controlled Phase 2b Trial. J. Am. Acad Derm. 2018, 79, 277–286.e10. [Google Scholar] [CrossRef] [Green Version]
- Warren, R.B.; Blauvelt, A.; Bagel, J.; Papp, K.A.; Yamauchi, P.; Armstrong, A.; Langley, R.G.; Vanvoorden, V.; De Cuyper, D.; Cioffi, C.; et al. Bimekizumab versus Adalimumab in Plaque Psoriasis. N. Engl. J. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Reich, K.; Papp, K.A.; Blauvelt, A.; Langley, R.G.; Armstrong, A.; Warren, R.B.; Gordon, K.B.; Merola, J.F.; Okubo, Y.; Madden, C.; et al. Bimekizumab versus Ustekinumab for the Treatment of Moderate to Severe Plaque Psoriasis (BE VIVID): Efficacy and Safety from a 52-Week, Multicentre, Double-Blind, Active Comparator and Placebo Controlled Phase 3 Trial. Lancet 2021, 397, 487–498. [Google Scholar] [CrossRef]
- Reich, K.; Warren, R.B.; Lebwohl, M.; Gooderham, M.; Strober, B.; Langley, R.G.; Paul, C.; De Cuyper, D.; Vanvoorden, V.; Madden, C.; et al. Bimekizumab versus Secukinumab in Plaque Psoriasis. N. Engl. J. Med. 2021. [Google Scholar] [CrossRef]
- European Medicines Agency (EMA). Kyntheum (Brodalumab). European Public-Assessment Report (EPAR); EMA: Brussels, Belgium, 2017. [Google Scholar]
- Papp, K.A.; Reid, C.; Foley, P.; Sinclair, R.; Salinger, D.H.; Williams, G.; Dong, H.; Krueger, J.G.; Russell, C.B.; Martin, D.A. Anti-IL-17 Receptor Antibody AMG 827 Leads to Rapid Clinical Response in Subjects with Moderate to Severe Psoriasis: Results from a Phase I, Randomized, Placebo-Controlled Trial. J. Invest. Derm. 2012, 132, 2466–2469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papp, K.A.; Leonardi, C.; Menter, A.; Ortonne, J.-P.; Krueger, J.G.; Kricorian, G.; Aras, G.; Li, J.; Russell, C.B.; Thompson, E.H.Z.; et al. Brodalumab, an Anti-Interleukin-17-Receptor Antibody for Psoriasis. N. Engl. J. Med. 2012, 366, 1181–1189. [Google Scholar] [CrossRef]
- Papp, K.A.; Reich, K.; Paul, C.; Blauvelt, A.; Baran, W.; Bolduc, C.; Toth, D.; Langley, R.G.; Cather, J.; Gottlieb, A.B.; et al. A Prospective Phase III, Randomized, Double-Blind, Placebo-Controlled Study of Brodalumab in Patients with Moderate-to-Severe Plaque Psoriasis. Br. J. Dermatol. 2016, 175, 273–286. [Google Scholar] [CrossRef]
- Tomalin, L.E.; Russell, C.B.; Garcet, S.; Ewald, D.A.; Klekotka, P.; Nirula, A.; Norsgaard, H.; Suàrez-Fariñas, M.; Krueger, J.G. Short-Term Transcriptional Response to IL-17 Receptor-A Antagonism in the Treatment of Psoriasis. J. Allergy Clin. Immunol. 2020, 145, 922–932. [Google Scholar] [CrossRef] [Green Version]
- Foulkes, A.C.; Warren, R.B. Brodalumab in Psoriasis: Evidence to Date and Clinical Potential. Drugs Context 2019, 8, 212570. [Google Scholar] [CrossRef]
- Kim, H.J.; Lebwohl, M.G. Biologics and Psoriasis: The Beat Goes On. Derm. Clin. 2019, 37, 29–36. [Google Scholar] [CrossRef]
- Sawyer, L.M.; Cornic, L.; Levin, L.Å.; Gibbons, C.; Møller, A.H.; Jemec, G.B. Long-Term Efficacy of Novel Therapies in Moderate-to-Severe Plaque Psoriasis: A Systematic Review and Network Meta-Analysis of PASI Response. J. Eur. Acad. Derm. Venereol. 2019, 33, 355–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.P.; Wu, K.K.; Lee, E.B.; Wu, J.J. Risk for Deep Fungal Infections during IL-17 and IL-23 Inhibitor Therapy for Psoriasis. Cutis 2020, 106, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Rusta-Sallehy, S.; Gooderham, M.; Papp, K. Brodalumab: A Review of Safety. Ski. Ther. Lett. 2018, 23, 1–3. [Google Scholar]
- Iznardo, H.; Puig, L. The Safety of Brodalumab for the Treatment of Psoriasis. Expert Opin. Drug Saf. 2020, 19, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Torres, T.; Raposo, I.; Selores, M. IL-17 Blockade in Psoriasis: Friend or Foe in Cardiovascular Risk? Am. J. Clin. Derm. 2016, 17, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Von Stebut, E.; Reich, K.; Thaçi, D.; Koenig, W.; Pinter, A.; Körber, A.; Rassaf, T.; Waisman, A.; Mani, V.; Yates, D.; et al. Impact of Secukinumab on Endothelial Dysfunction and Other Cardiovascular Disease Parameters in Psoriasis Patients over 52 Weeks. J. Invest. Derm. 2019, 139, 1054–1062. [Google Scholar] [CrossRef] [Green Version]
- Egeberg, A.; Wu, J.J.; Korman, N.; Solomon, J.A.; Goldblum, O.; Zhao, F.; Mallbris, L. Ixekizumab Treatment Shows a Neutral Impact on Cardiovascular Parameters in Patients with Moderate-to-Severe Plaque Psoriasis: Results from UNCOVER-1, UNCOVER-2, and UNCOVER. J. Am. Acad Derm. 2018, 79, 104–109.e8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, R.; Tao, A.; Zhang, S.; Zhang, M. Neutralization of Interleukin-17 Attenuates High Fat Diet-Induced Non-Alcoholic Fatty Liver Disease in Mice. Acta Biochim. Biophys Sin. 2013, 45, 726–733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, W.; Zhu, Q.; Gu, J.; Liu, X.; Lu, L.; Qian, X.; Shen, J.; Zhang, F.; Li, G. Anti-IL-17 Antibody Improves Hepatic Steatosis by Suppressing Interleukin-17-Related Fatty Acid Synthesis and Metabolism. Clin. Dev. Immunol. 2013, 2013, 253046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| IL-17 Subtype | Length | Chromosomal Location | Effect on Other Cells | Association with Diseases |
|---|---|---|---|---|
| IL-17A | 155 | 6p12 | Proinflammatory effect on epithelial cells Synergy with IL-17F | Psoriasis Atopic eczema Multiple sclerosis Rheumatoid arthritis Psoriatic arthritis Chronic inflammatory bowel diseases Inflammation with acute coronary syndrome |
| IL-17F | 153 | 6p12 | Proinflammatory effect on epithelial cells | Psoriasis |
| Synergy with IL-17A | Atopic eczema | |||
| Multiple sclerosis | ||||
| Rheumatoid arthritis | ||||
| Psoriatic arthritis | ||||
| Chronic inflammatory bowel diseases | ||||
| IL-17C | 197 | 16q24 | Autocrine stimulation of epithelial cells | Psoriasis |
| Proinflammatory effect on epithelial cells via the expression of cytokines, chemokines, and antimicrobial peptides Synergy with TNF | Atopic eczema Rheumatoid arthritis Chronic inflammatory bowel diseases | |||
| IL-17E (IL-25) | 161 | 14q11.2 | Induces the loss of cellular barrier function Modulation of proinflammatory cytokines (e.g., IL-8, CCL-5, and GM-CSF) Reduced IL-17E expression in chronic inflammatory intestinal diseases | Psoriasis Atopic eczema Allergic contact dermatitis Bronchial asthma Rheumatoid arthritis Chronic inflammatory bowel diseases |
| IL-17B | 180 | 5q32-34 | Increase in TNF-α production by fibroblasts | Rheumatoid arthritis |
| Poor prognosis in breast and stomach cancer | ||||
| IL-17D | 202 | 13q12.11 | Modulation of cytokine production by endothelial cells | Rheumatoid arthritis |
| Release of proinflammatory cytokines (e.g., IL-6, IL-8, GM-CSF) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vidal, S.; Puig, L.; Carrascosa-Carrillo, J.-M.; González-Cantero, Á.; Ruiz-Carrascosa, J.-C.; Velasco-Pastor, A.-M. From Messengers to Receptors in Psoriasis: The Role of IL-17RA in Disease and Treatment. Int. J. Mol. Sci. 2021, 22, 6740. https://doi.org/10.3390/ijms22136740
Vidal S, Puig L, Carrascosa-Carrillo J-M, González-Cantero Á, Ruiz-Carrascosa J-C, Velasco-Pastor A-M. From Messengers to Receptors in Psoriasis: The Role of IL-17RA in Disease and Treatment. International Journal of Molecular Sciences. 2021; 22(13):6740. https://doi.org/10.3390/ijms22136740
Chicago/Turabian StyleVidal, Silvia, Lluís Puig, José-Manuel Carrascosa-Carrillo, Álvaro González-Cantero, José-Carlos Ruiz-Carrascosa, and Antonio-Manuel Velasco-Pastor. 2021. "From Messengers to Receptors in Psoriasis: The Role of IL-17RA in Disease and Treatment" International Journal of Molecular Sciences 22, no. 13: 6740. https://doi.org/10.3390/ijms22136740






