Role of EphA4 in Mediating Motor Neuron Death in MND
Abstract
:1. Introduction
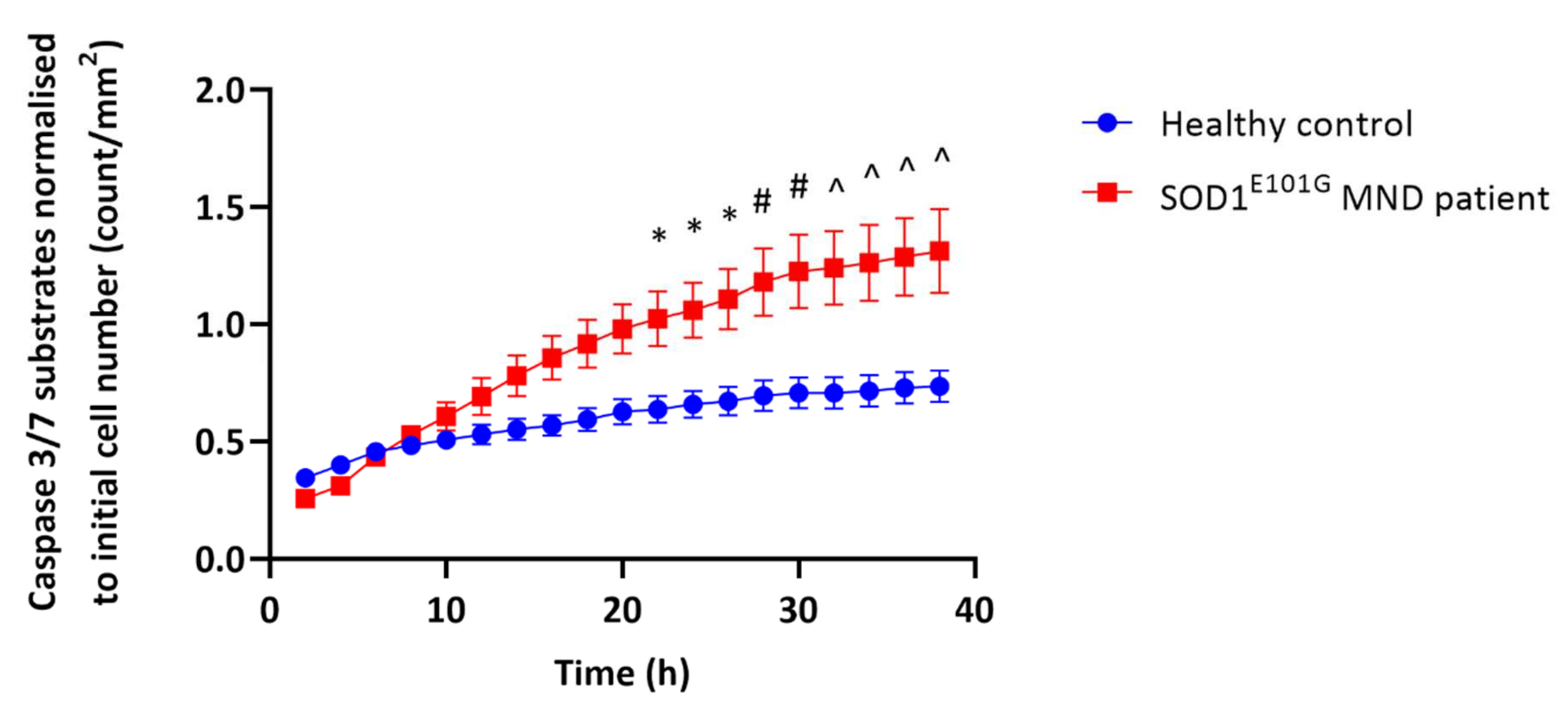
2. EphA4 Signalling Acts Directly on Motor Neurons to Cause Cell Death
3. Direct Regulation of Motor Neuron Death by EphA4
3.1. Role of Rho/Rock Signalling
3.2. Role of D-Serine-Induced NMDAR Activation
3.3. Role of Calcium Channels
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviation
| MND | Motor neuron disease |
| GPI | Glycosyl phosphatidylinositol |
| SCI | Spinal cord injury |
| EphA4-FL | Full-length EphA4 |
| mEphA4-Fc | Mutant EphA4-Fc |
| ChAT | Choline acetyltransferase |
| P5 | Postnatal day 5 |
| CNS | Central nervous system |
| NMJ | Neuromuscular junction |
| TA | Tibialis anterior |
| iPSC | Induced pluripotent stem cell |
| LDH | Lactate dehydrogenase |
| ROCK | Rho-associated coiled-coil-containing protein kinase |
| EC | Endothelial cell |
| CA-4-P | Combretastatin A-4-phosphate |
| MLC | Myosin light chain |
| MAPK | Mitogen-activated protein kinases |
| PTEN | Phosphatase and tensin homologue |
| BBB | Blood–brain barrier |
| SAH | Subarachnoid haemorrhage |
| NMDAR | N-methyl-d-aspartate receptor |
| SR | Serine racemase |
| DAO | D-amino acid oxidase |
| AMPAR | AMPA receptor |
References
- Turner, M.R.; Kiernan, M.C.; Leigh, P.N.; Talbot, K. Biomarkers in amyotrophic lateral sclerosis. Lancet Neurol. 2009, 8, 94–109. [Google Scholar] [CrossRef]
- Rowland, L.P.; Shneider, N.A. Amyotrophic lateral sclerosis. N. Engl. J. Med. 2001, 344, 1688–1700. [Google Scholar] [CrossRef]
- Yedavalli, V.S.; Patil, A.; Shah, P. Amyotrophic Lateral Sclerosis and its Mimics/Variants: A Comprehensive Review. J. Clin. Imaging Sci. 2018, 8, 53. [Google Scholar]
- Bensimon, G.; Lacomblez, L.; Meininger, V. A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N. Engl. J. Med. 1994, 330, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Hinchcliffe, M.; Smith, A. Riluzole: Real-world evidence supports significant extension of median survival times in patients with amyotrophic lateral sclerosis. Degener. Neurol. Neuromuscul. Dis. 2017, 7, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Miller, R.G.; Mitchell, J.D.; Moore, D.H. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database Syst. Rev. 2012, CD001447. [Google Scholar] [CrossRef]
- Zoing, M.C.; Burke, D.; Pamphlett, R.; Kiernan, M.C. Riluzole therapy for motor neurone disease: An early Australian experience (1996–2002). J. Clin. Neurosci. 2006, 13, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Al-Chalabi, A.; Calvo, A.; Chio, A.; Colville, S.; Ellis, C.M.; Hardiman, O.; Heverin, M.; Howard, R.S.; Huisman, M.H.; Keren, N.; et al. Analysis of amyotrophic lateral sclerosis as a multistep process: A population-based modelling study. Lancet Neurol. 2014, 13, 1108–1113. [Google Scholar] [CrossRef] [Green Version]
- Rothstein, J.D. Current hypotheses for the underlying biology of amyotrophic lateral sclerosis. Ann. Neurol. 2009, 65 (Suppl. 1), S3–S9. [Google Scholar] [CrossRef] [PubMed]
- Ragagnin, A.M.G.; Shadfar, S.; Vidal, M.; Jamali, M.S.; Atkin, J.D. Motor Neuron Susceptibility in ALS/FTD. Front. Neurosci. 2019, 13, 532. [Google Scholar] [CrossRef] [Green Version]
- Pirooznia, S.K.; Dawson, V.L.; Dawson, T.M. Motor neuron death in ALS: Programmed by astrocytes? Neuron 2014, 81, 961–963. [Google Scholar] [CrossRef] [Green Version]
- Bowden, T.A.; Aricescu, A.R.; Nettleship, J.E.; Siebold, C.; Rahman-Huq, N.; Owens, R.J.; Stuart, D.I.; Jones, E.Y. Structural plasticity of eph receptor A4 facilitates cross-class ephrin signaling. Structure 2009, 17, 1386–1397. [Google Scholar] [CrossRef] [Green Version]
- Pasquale, E.B. Eph receptors and ephrins in cancer: Bidirectional signalling and beyond. Nat. Rev. Cancer 2010, 10, 165–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lackmann, M.; Boyd, A.W. Eph, a protein family coming of age: More confusion, insight, or complexity? Sci Signal. 2008, 1, re2. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.W.; Bartlett, P.F.; Lackmann, M. Therapeutic targeting of EPH receptors and their ligands. Nat. Rev. Drug Discov. 2014, 13, 39–62. [Google Scholar] [CrossRef] [PubMed]
- Dottori, M.; Hartley, L.; Galea, M.; Paxinos, G.; Polizzotto, M.; Kilpatrick, T.; Bartlett, P.F.; Murphy, M.; Kontgen, F.; Boyd, A.W. EphA4 (Sek1) receptor tyrosine kinase is required for the development of the corticospinal tract. Proc. Natl. Acad. Sci. USA 1998, 95, 13248–13253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gatto, G.; Morales, D.; Kania, A.; Klein, R. EphA4 receptor shedding regulates spinal motor axon guidance. Curr. Biol. 2014, 24, 2355–2365. [Google Scholar] [CrossRef] [Green Version]
- Spanevello, M.D.; Tajouri, S.I.; Mirciov, C.; Kurniawan, N.; Pearse, M.J.; Fabri, L.J.; Owczarek, C.M.; Hardy, M.P.; Bradford, R.A.; Ramunno, M.L.; et al. Acute delivery of EphA4-Fc improves functional recovery after contusive spinal cord injury in rats. J. Neurotrauma 2013, 30, 1023–1034. [Google Scholar] [CrossRef] [Green Version]
- Goldshmit, Y.; Spanevello, M.D.; Tajouri, S.; Li, L.; Rogers, F.; Pearse, M.; Galea, M.; Bartlett, P.F.; Boyd, A.W.; Turnley, A.M. EphA4 blockers promote axonal regeneration and functional recovery following spinal cord injury in mice. PLoS ONE 2011, 6, e24636. [Google Scholar] [CrossRef] [Green Version]
- Goldshmit, Y.; Galea, M.P.; Wise, G.; Bartlett, P.F.; Turnley, A.M. Axonal regeneration and lack of astrocytic gliosis in EphA4-deficient mice. J. Neurosci. 2004, 24, 10064–10073. [Google Scholar] [CrossRef] [Green Version]
- Van Hoecke, A.; Schoonaert, L.; Lemmens, R.; Timmers, M.; Staats, K.A.; Laird, A.S.; Peeters, E.; Philips, T.; Goris, A.; Dubois, B.; et al. EPHA4 is a disease modifier of amyotrophic lateral sclerosis in animal models and in humans. Nat. Med. 2012, 18, 1418–1422. [Google Scholar] [CrossRef]
- Zhao, J.; Cooper, L.T.; Boyd, A.W.; Bartlett, P.F. Decreased signalling of EphA4 improves functional performance and motor neuron survival in the SOD1(G93A) ALS mouse model. Sci. Rep. 2018, 8, 11393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.; Boyd, A.W.; Bartlett, P.F. The identification of a novel isoform of EphA4 and ITS expression in SOD1G93A mice. Neuroscience 2017, 347, 11–21. [Google Scholar] [CrossRef] [Green Version]
- Wu, B.; De, S.K.; Kulinich, A.; Salem, A.F.; Koeppen, J.; Wang, R.; Barile, E.; Wang, S.; Zhang, D.; Ethell, I.; et al. Potent and Selective EphA4 Agonists for the Treatment of ALS. Cell Chem. Biol. 2017, 24, 293–305. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, K. Role of EphA4 signaling in the pathogenesis of amyotrophic lateral sclerosis and therapeutic potential of traditional Chinese medicine rhynchophylline. Psychopharmacology 2015, 232, 2873–2875. [Google Scholar] [CrossRef] [PubMed]
- Pegg, C.L.; Cooper, L.T.; Zhao, J.; Gerometta, M.; Smith, F.M.; Yeh, M.; Bartlett, P.F.; Gorman, J.J.; Boyd, A.W. Glycoengineering of EphA4 Fc leads to a unique, long-acting and broad spectrum, Eph receptor therapeutic antagonist. Sci. Rep. 2017, 7, 6519. [Google Scholar] [CrossRef] [Green Version]
- Rossi, J.; Balthasar, N.; Olson, D.; Scott, M.; Berglund, E.; Lee, C.E.; Choi, M.J.; Lauzon, D.; Lowell, B.B.; Elmquist, J.K. Melanocortin-4 receptors expressed by cholinergic neurons regulate energy balance and glucose homeostasis. Cell Metab. 2011, 13, 195–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Ortiz, E.; Yui, D.; Song, D.; Li, Y.; Rubenstein, J.L.; Reichardt, L.F.; Parada, L.F. TrkA gene ablation in basal forebrain results in dysfunction of the cholinergic circuitry. J. Neurosci. 2012, 32, 4065–4079. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bax, M.; McKenna, J.; Do-Ha, D.; Stevens, C.H.; Higginbottom, S.; Balez, R.; Cabral-da-Silva, M.E.C.; Farrawell, N.E.; Engel, M.; Poronnik, P.; et al. The ubiquitin proteasome system is a key regulator of pluripotent stem cell survival and motor neuron differentiation. Cells 2019, 8, 581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balez, R.; Steiner, N.; Engel, M.; Munoz, S.S.; Lum, J.S.; Wu, Y.; Wang, D.; Vallotton, P.; Sachdev, P.; O’Connor, M.; et al. Neuroprotective effects of apigenin against inflammation, neuronal excitability and apoptosis in an induced pluripotent stem cell model of Alzheimer’s disease. Sci. Rep. 2016, 6, 31450. [Google Scholar] [CrossRef] [Green Version]
- National Health and Medical Research Council. The National Statement on Ethical Conduct in Human Research; National Health and Medical Research Council: Canberra, Australia, 2007.
- Ben-Shushan, E.; Feldman, E.; Reubinoff, B.E. Notch signaling regulates motor neuron differentiation of human embryonic stem cells. Stem. Cells 2015, 33, 403–415. [Google Scholar] [CrossRef] [Green Version]
- Bardy, C.; van den Hurk, M.; Eames, T.; Marchand, C.; Hernandez, R.V.; Kellogg, M.; Gorris, M.; Galet, B.; Palomares, V.; Brown, J.; et al. Neuronal medium that supports basic synaptic functions and activity of human neurons in vitro. Proc. Natl. Acad. Sci. USA 2015, 112, E2725–E2734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jagannathan, L.; Cuddapah, S.; Costa, M. Oxidative stress under ambient and physiological oxygen tension in tissue culture. Curr. Pharmacol. Rep. 2016, 2, 64–72. [Google Scholar] [CrossRef] [Green Version]
- Comley, L.; Allodi, I.; Nichterwitz, S.; Nizzardo, M.; Simone, C.; Corti, S.; Hedlund, E. Motor neurons with differential vulnerability to degeneration show distinct protein signatures in health and ALS. Neuroscience 2015, 291, 216–229. [Google Scholar] [CrossRef] [Green Version]
- Royet, A.; Broutier, L.; Coissieux, M.M.; Malleval, C.; Gadot, N.; Maillet, D.; Gratadou-Hupon, L.; Bernet, A.; Nony, P.; Treilleux, I.; et al. Ephrin-B3 supports glioblastoma growth by inhibiting apoptosis induced by the dependence receptor EphA4. Oncotarget 2017, 8, 23750–23759. [Google Scholar] [CrossRef] [Green Version]
- Nelersa, C.M.; Barreras, H.; Runko, E.; Ricard, J.; Shi, Y.; Glass, S.J.; Bixby, J.L.; Lemmon, V.P.; Liebl, D.J. High-content analysis of proapoptotic EphA4 dependence receptor functions using small-molecule libraries. J. Biomol. Screen. 2012, 17, 785–795. [Google Scholar] [CrossRef] [Green Version]
- Chen, F.; Liu, Z.; Peng, W.; Gao, Z.; Ouyang, H.; Yan, T.; Ding, S.; Cai, Z.; Zhao, B.; Mao, L.; et al. Activation of EphA4 induced by EphrinA1 exacerbates disruption of the blood-brain barrier following cerebral ischemia-reperfusion via the Rho/ROCK signaling pathway. Exp. Ther. Med. 2018, 16, 2651–2658. [Google Scholar] [CrossRef]
- Xu, L.J.; Gao, F.; Cheng, S.; Zhou, Z.X.; Li, F.; Miao, Y.; Niu, W.R.; Yuan, F.; Sun, X.H.; Wang, Z. Activated ephrinA3/EphA4 forward signaling induces retinal ganglion cell apoptosis in experimental glaucoma. Neuropharmacology 2020, 178, 108228. [Google Scholar] [CrossRef]
- Chen, Y.; Hua, Y.; Li, X.; Arslan, I.M.; Zhang, W.; Meng, G. Distinct Types of Cell Death and the Implication in Diabetic Cardiomyopathy. Front. Pharmacol. 2020, 11, 42. [Google Scholar] [CrossRef] [PubMed]
- Shaw, P.J. Molecular and cellular pathways of neurodegeneration in motor neurone disease. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1046–1057. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Chen, X.; Gueydan, C.; Han, J. Plasma membrane changes during programmed cell deaths. Cell Res. 2018, 28, 9–21. [Google Scholar] [CrossRef]
- McElhinney, B.; Poynter, M.E.; Shrivastava, P.; Hazen, S.L.; Janssen-Heininger, Y.M. Eosinophil peroxidase catalyzes JNK-mediated membrane blebbing in a Rho kinase-dependent manner. J. Leukoc. Biol. 2003, 74, 897–907. [Google Scholar] [CrossRef]
- Kanthou, C.; Tozer, G.M. The tumor vascular targeting agent combretastatin A-4-phosphate induces reorganization of the actin cytoskeleton and early membrane blebbing in human endothelial cells. Blood 2002, 99, 2060–2069. [Google Scholar] [CrossRef]
- Mavria, G.; Vercoulen, Y.; Yeo, M.; Paterson, H.; Karasarides, M.; Marais, R.; Bird, D.; Marshall, C.J. ERK-MAPK signaling opposes Rho-kinase to promote endothelial cell survival and sprouting during angiogenesis. Cancer Cell 2006, 9, 33–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, J.; Xie, M.; Shah, V.R.; Schneider, M.D.; Entman, M.L.; Wei, L.; Schwartz, R.J. Activation of Rho-associated coiled-coil protein kinase 1 (ROCK-1) by caspase-3 cleavage plays an essential role in cardiac myocyte apoptosis. Proc. Natl. Acad. Sci. USA 2006, 103, 14495–14500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfrum, S.; Dendorfer, A.; Rikitake, Y.; Stalker, T.J.; Gong, Y.; Scalia, R.; Dominiak, P.; Liao, J.K. Inhibition of Rho-kinase leads to rapid activation of phosphatidylinositol 3-kinase/protein kinase Akt and cardiovascular protection. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 1842–1847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takata, M.; Tanaka, H.; Kimura, M.; Nagahara, Y.; Tanaka, K.; Kawasaki, K.; Seto, M.; Tsuruma, K.; Shimazawa, M.; Hara, H. Fasudil, a rho kinase inhibitor, limits motor neuron loss in experimental models of amyotrophic lateral sclerosis. Br. J. Pharmacol. 2013, 170, 341–351. [Google Scholar] [CrossRef] [Green Version]
- Fan, R.; Enkhjargal, B.; Camara, R.; Yan, F.; Gong, L.; ShengtaoYao Tang, J.; Chen, Y.; Zhang, J.H. Critical role of EphA4 in early brain injury after subarachnoid hemorrhage in rat. Exp. Neurol. 2017, 296, 41–48. [Google Scholar] [CrossRef]
- Lemmens, R.; Jaspers, T.; Robberecht, W.; Thijs, V.N. Modifying expression of EphA4 and its downstream targets improves functional recovery after stroke. Hum. Mol. Genet. 2013, 22, 2214–2220. [Google Scholar] [CrossRef] [PubMed]
- Gunther, R.; Saal, K.A.; Suhr, M.; Scheer, D.; Koch, J.C.; Bahr, M.; Lingor, P.; Tonges, L. The rho kinase inhibitor Y-27632 improves motor performance in male SOD1(G93A) mice. Front. Neurosci. 2014, 8, 304. [Google Scholar]
- Lingor, P.; Weber, M.; Camu, W.; Friede, T.; Hilgers, R.; Leha, A.; Neuwirth, C.; Gunther, R.; Benatar, M.; Kuzma-Kozakiewicz, M.; et al. ROCK-ALS: Protocol for a randomized, placebo-controlled, double-blind phase IIa trial of safety, tolerability and efficacy of the Rho kinase (ROCK) inhibitor Fasudil in amyotrophic lateral sclerosis. Front. Neurol. 2019, 10, 293. [Google Scholar] [CrossRef] [Green Version]
- Koch, J.C.; Kuttler, J.; Maass, F.; Lengenfeld, T.; Zielke, E.; Bahr, M.; Lingor, P. Compassionate use of the ROCK inhibitor Fasudil in three patients with amyotrophic lateral sclerosis. Front. Neurol. 2020, 11, 173. [Google Scholar] [CrossRef]
- Baudet, S.; Becret, J.; Nicol, X. Approaches to Manipulate Ephrin-A:EphA Forward Signaling Pathway. Pharmaceuticals 2020, 13, 140. [Google Scholar] [CrossRef]
- Murai, K.K.; Pasquale, E.B. Eph’ective signaling: Forward, reverse and crosstalk. J. Cell Sci. 2003, 116, 2823–2832. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Sawada, T.; Jing, X.; Yokote, H.; Yan, X.; Sakaguchi, K. Regulation of ephexin1, a guanine nucleotide exchange factor of Rho family GTPases, by fibroblast growth factor receptor-mediated tyrosine phosphorylation. J. Biol. Chem. 2007, 282, 31103–31112. [Google Scholar] [CrossRef] [Green Version]
- Iwasato, T.; Katoh, H.; Nishimaru, H.; Ishikawa, Y.; Inoue, H.; Saito, Y.M.; Ando, R.; Iwama, M.; Takahashi, R.; Negishi, M.; et al. Rac-GAP alpha-chimerin regulates motor-circuit formation as a key mediator of EphrinB3/EphA4 forward signaling. Cell 2007, 130, 742–753. [Google Scholar] [CrossRef] [Green Version]
- Winning, R.S.; Ward, E.K.; Scales, J.B.; Walker, G.K. EphA4 catalytic activity causes inhibition of RhoA GTPase in Xenopus laevis embryos. Differentiation 2002, 70, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Koch, J.C.; Tatenhorst, L.; Roser, A.E.; Saal, K.A.; Tonges, L.; Lingor, P. ROCK inhibition in models of neurodegeneration and its potential for clinical translation. Pharmacol. Ther. 2018, 189, 1–21. [Google Scholar] [CrossRef]
- Nakayama, A.Y.; Harms, M.B.; Luo, L. Small GTPases Rac and Rho in the maintenance of dendritic spines and branches in hippocampal pyramidal neurons. J. Neurosci. 2000, 20, 5329–5338. [Google Scholar] [CrossRef]
- Van Den Bosch, L.; Van Damme, P.; Bogaert, E.; Robberecht, W. The role of excitotoxicity in the pathogenesis of amyotrophic lateral sclerosis. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2006, 1762, 1068–1082. [Google Scholar] [CrossRef] [Green Version]
- Mothet, J.P.; Parent, A.T.; Wolosker, H.; Brady, R.O.; Linden, D.J., Jr.; Ferris, C.D.; Rogawski, M.A.; Snyder, S.H. D-serine is an endogenous ligand for the glycine site of the N-methyl-D-aspartate receptor. Proc. Natl. Acad. Sci. USA 2000, 97, 4926–4931. [Google Scholar] [CrossRef] [Green Version]
- Cameron, H.A.; McEwen, B.S.; Gould, E. Regulation of adult neurogenesis by excitatory input and NMDA receptor activation in the dentate gyrus. J. Neurosci. 1995, 15, 4687–4692. [Google Scholar] [CrossRef]
- Ndountse, L.T.; Chan, H.M. Role of N-methyl-D-aspartate receptors in polychlorinated biphenyl mediated neurotoxicity. Toxicol. Lett. 2009, 184, 50–55. [Google Scholar] [CrossRef]
- Kritis, A.A.; Stamoula, E.G.; Paniskaki, K.A.; Vavilis, T.D. Researching glutamate-induced cytotoxicity in different cell lines: A comparative/collective analysis/study. Front. Cell. Neurosci. 2015, 9, 91. [Google Scholar] [CrossRef] [Green Version]
- Kartvelishvily, E.; Shleper, M.; Balan, L.; Dumin, E.; Wolosker, H. Neuron-derived D-serine release provides a novel means to activate N-methyl-D-aspartate receptors. J. Biol. Chem. 2006, 281, 14151–14162. [Google Scholar] [CrossRef] [Green Version]
- Sasabe, J.; Miyoshi, Y.; Suzuki, M.; Mita, M.; Konno, R.; Matsuoka, M.; Hamase, K.; Aiso, S. D-amino acid oxidase controls motoneuron degeneration through D-serine. Proc. Natl. Acad. Sci. USA 2012, 109, 627–632. [Google Scholar] [CrossRef] [Green Version]
- Sasabe, J.; Chiba, T.; Yamada, M.; Okamoto, K.; Nishimoto, I.; Matsuoka, M.; Aiso, S. D-serine is a key determinant of glutamate toxicity in amyotrophic lateral sclerosis. EMBO J. 2007, 26, 4149–4159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, P.; de Belleroche, J. Experimental approaches for elucidating co-agonist regulation of NMDA receptor in motor neurons: Therapeutic implications for amyotrophic lateral sclerosis (ALS). J. Pharm. Biomed. Anal. 2015, 116, 2–6. [Google Scholar] [CrossRef]
- Zhuang, Z.; Yang, B.; Theus, M.H.; Sick, J.T.; Bethea, J.R.; Sick, T.J.; Liebl, D.J. EphrinBs regulate D-serine synthesis and release in astrocytes. J. Neurosci. 2010, 30, 16015–16024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.; Taylor, C.J.; Newcombe, E.A.; Spanevello, M.D.; O’Keeffe, I.; Cooper, L.T.; Jhaveri, D.J.; Boyd, A.W.; Bartlett, P.F. EphA4 Regulates Hippocampal Neural Precursor Proliferation in the Adult Mouse Brain by d-Serine Modulation of N-Methyl-d-Aspartate Receptor Signaling. Cereb. Cortex 2018, 29, 17. [Google Scholar] [CrossRef]
- Mitchell, J.; Paul, P.; Chen, H.J.; Morris, A.; Payling, M.; Falchi, M.; Habgood, J.; Panoutsou, S.; Winkler, S.; Tisato, V.; et al. Familial amyotrophic lateral sclerosis is associated with a mutation in D-amino acid oxidase. Proc. Natl. Acad. Sci. USA 2010, 107, 7556–7561. [Google Scholar] [CrossRef] [Green Version]
- Kondratskyi, A.; Kondratska, K.; Skryma, R.; Prevarskaya, N. Ion channels in the regulation of apoptosis. Biochim. Biophys. Acta (BBA) Biomembr. 2015, 1848, 2532–2546. [Google Scholar] [CrossRef] [Green Version]
- Iwai, Y.; Shibuya, K.; Misawa, S.; Sekiguchi, Y.; Watanabe, K.; Amino, H.; Kuwabara, S. Axonal Dysfunction Precedes Motor Neuronal Death in Amyotrophic Lateral Sclerosis. PLoS ONE 2016, 11, e0158596. [Google Scholar] [CrossRef]
- Martin, L.J. Mitochondrial pathobiology in ALS. J. Bioenerg. Biomembr. 2011, 43, 569–579. [Google Scholar] [CrossRef] [Green Version]
- Pieri, M.; Carunchio, I.; Curcio, L.; Mercuri, N.B.; Zona, C. Increased persistent sodium current determines cortical hyperexcitability in a genetic model of amyotrophic lateral sclerosis. Exp. Neurol. 2009, 215, 368–379. [Google Scholar] [CrossRef]
- Kanai, K.; Kuwabara, S.; Misawa, S.; Tamura, N.; Ogawara, K.; Nakata, M.; Sawai, S.; Hattori, T.; Bostock, H. Altered axonal excitability properties in amyotrophic lateral sclerosis: Impaired potassium channel function related to disease stage. Brain 2006, 129, 953–962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LoRusso, E.; Hickman, J.J.; Guo, X. Ion channel dysfunction and altered motoneuron excitability in ALS. Neurol. Disord. Epilepsy J. 2019, 3, 124. [Google Scholar]
- Spalloni, A.; Nutini, M.; Longone, P. Role of the N-methyl-d-aspartate receptors complex in amyotrophic lateral sclerosis. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2013, 1832, 312–322. [Google Scholar] [CrossRef] [Green Version]
- Platt, S.R. The role of glutamate in central nervous system health and disease—A review. Vet. J. 2007, 173, 278–286. [Google Scholar] [CrossRef]
- Tortarolo, M.; Grignaschi, G.; Calvaresi, N.; Zennaro, E.; Spaltro, G.; Colovic, M.; Fracasso, C.; Guiso, G.; Elger, B.; Schneider, H.; et al. Glutamate AMPA receptors change in motor neurons of SOD1G93A transgenic mice and their inhibition by a noncompetitive antagonist ameliorates the progression of amytrophic lateral sclerosis-like disease. J. Neurosci. Res. 2006, 83, 134–146. [Google Scholar] [CrossRef] [PubMed]
- Rembach, A.; Turner, B.J.; Bruce, S.; Cheah, I.K.; Scott, R.L.; Lopes, E.C.; Zagami, C.J.; Beart, P.M.; Cheung, N.S.; Langford, S.J.; et al. Antisense peptide nucleic acid targeting GluR3 delays disease onset and progression in the SOD1 G93A mouse model of familial ALS. J. Neurosci. Res. 2004, 77, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, B.T.; Livesey, M.R.; Zhao, C.; Gregory, J.M.; James, O.T.; Cleary, E.M.; Chouhan, A.K.; Gane, A.B.; Perkins, E.M.; Dando, O.; et al. C9ORF72 repeat expansion causes vulnerability of motor neurons to Ca2+-permeable AMPA receptor-mediated excitotoxicity. Nat. Commun. 2018, 9, 347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hideyama, T.; Yamashita, T.; Suzuki, T.; Tsuji, S.; Higuchi, M.; Seeburg, P.H.; Takahashi, R.; Misawa, H.; Kwak, S. Induced loss of ADAR2 engenders slow death of motor neurons from Q/R site-unedited GluR2. J. Neurosci. 2010, 30, 11917–11925. [Google Scholar] [CrossRef]
- Fu, A.K.; Hung, K.W.; Fu, W.Y.; Shen, C.; Chen, Y.; Xia, J.; Lai, K.O.; Ip, N.Y. APC(Cdh1) mediates EphA4-dependent downregulation of AMPA receptors in homeostatic plasticity. Nat. Neurosci. 2011, 14, 181–189. [Google Scholar] [CrossRef]
- Chen, Y.; Fu, A.K.; Ip, N.Y. Eph receptors at synapses: Implications in neurodegenerative diseases. Cell. Signal. 2012, 24, 606–611. [Google Scholar] [CrossRef] [PubMed]
- Murai, K.K.; Pasquale, E.B. Eph receptors and ephrins in neuron-astrocyte communication at synapses. Glia 2011, 59, 1567–1578. [Google Scholar] [CrossRef]
- Murai, K.K.; Nguyen, L.N.; Irie, F.; Yamaguchi, Y.; Pasquale, E.B. Control of hippocampal dendritic spine morphology through ephrin-A3/EphA4 signaling. Nat. Neurosci. 2003, 6, 153–160. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, J.; Stevens, C.H.; Boyd, A.W.; Ooi, L.; Bartlett, P.F. Role of EphA4 in Mediating Motor Neuron Death in MND. Int. J. Mol. Sci. 2021, 22, 9430. https://doi.org/10.3390/ijms22179430
Zhao J, Stevens CH, Boyd AW, Ooi L, Bartlett PF. Role of EphA4 in Mediating Motor Neuron Death in MND. International Journal of Molecular Sciences. 2021; 22(17):9430. https://doi.org/10.3390/ijms22179430
Chicago/Turabian StyleZhao, Jing, Claire H. Stevens, Andrew W. Boyd, Lezanne Ooi, and Perry F. Bartlett. 2021. "Role of EphA4 in Mediating Motor Neuron Death in MND" International Journal of Molecular Sciences 22, no. 17: 9430. https://doi.org/10.3390/ijms22179430





