Adipose-Derived Stem Cells in the Treatment of Perianal Fistulas in Crohn’s Disease: Rationale, Clinical Results and Perspectives
Abstract
:1. Introduction
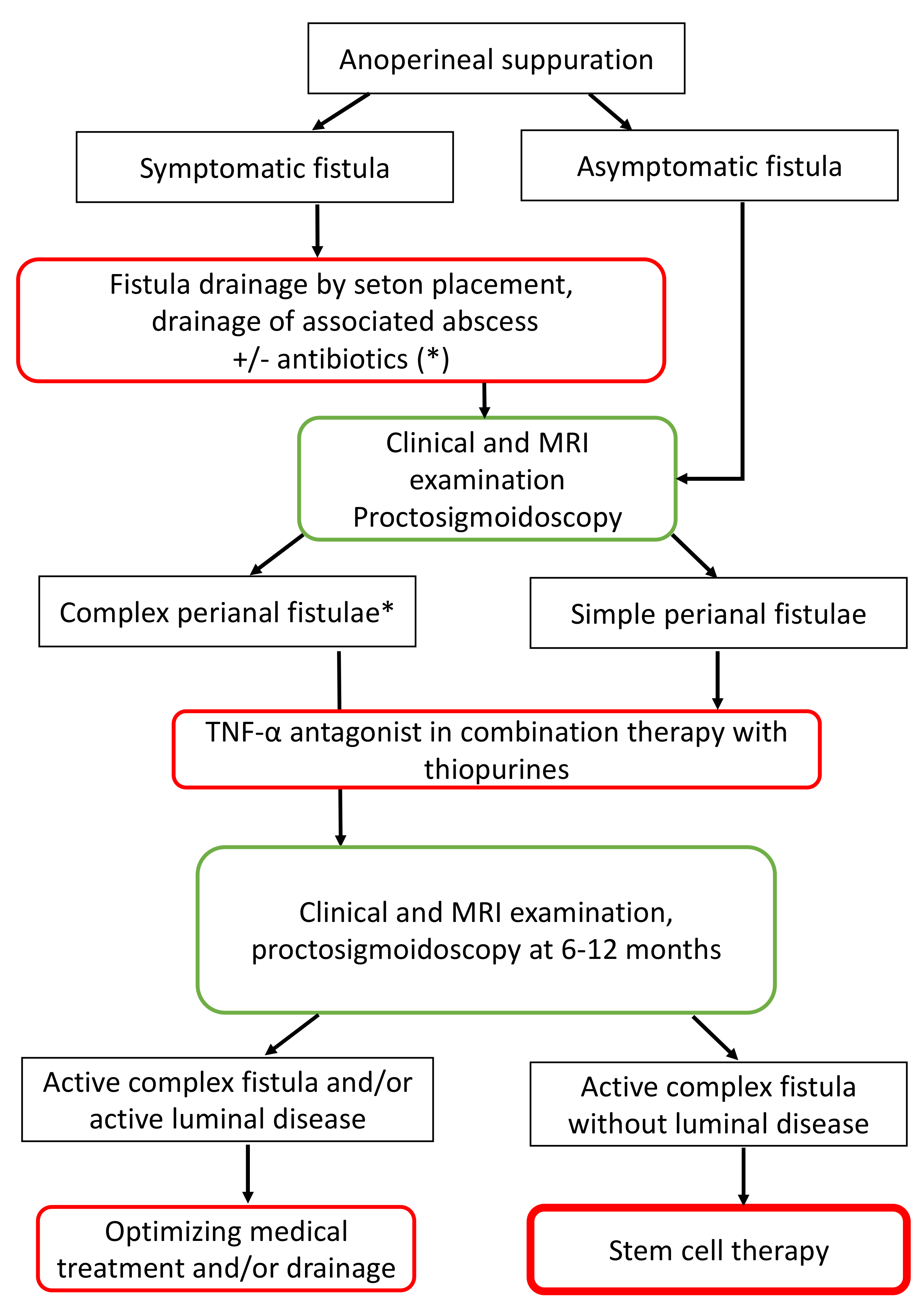
2. Treatment of Perianal Fistulizing Crohn’s Disease
3. Properties of ADSCs and Their Clinical Application
3.1. Origin and General Properties of MSCs
3.2. Isolating ADSCs
3.3. Properties and Molecular Aspects of MSCs
3.4. Advantages of ADSCs versus BM-MSCs
3.5. Autologous versus Allogenic ADSCs
3.6. Clinical Applications and Safety of ADSCs
4. Clinical Trials Using ADSCs in Perianal Fistulas in Crohn’s Disease
4.1. Published Papers
4.2. Ongoing Trials
5. Perspectives and Future Developments
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
Abbreviations
| CD | Crohn’s disease |
| MSC | Mesenchymal stem cells |
| ADSC | Adipose-derived stem cells |
| BM-MSC | Bone marrow mesenchymal stem cells |
| SVF | Serum vascular fraction |
| PBMC | Peripheral blood mononuclear cells |
| MRI | Magnetic resonance imaging. |
References
- Beaugerie, L.; Seksik, P.; Nion-Larmurier, I.; Gendre, J.-P.; Cosnes, J. Predictors of Crohn’s Disease. Gastroenterology 2006, 130, 650–656. [Google Scholar] [CrossRef]
- Brochard, C.; Siproudhis, L.; Wallenhorst, T.; Cuen, D.; d’Halluin, P.N.; Garros, A.; Bretagne, J.-F.; Bouguen, G. Anorectal Stricture in 102 Patients with Crohn’s Disease: Natural History in the Era of Biologics. Aliment. Pharmacol. Ther. 2014, 40, 796–803. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, D.A.; Loftus, E.V.; Tremaine, W.J.; Panaccione, R.; Harmsen, W.S.; Zinsmeister, A.R.; Sandborn, W.J. The Natural History of Fistulizing Crohn’s Disease in Olmsted County, Minnesota. Gastroenterology 2002, 122, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Peyrin-Biroulet, L.; Harmsen, W.S.; Tremaine, W.J.; Zinsmeister, A.R.; Sandborn, W.J.; Loftus, E.V. Cumulative Length of Bowel Resection in a Population-Based Cohort of Patients With Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2016, 14, 1439–1444. [Google Scholar] [CrossRef] [Green Version]
- Wallenhorst, T.; Brochard, C.; Le Balch, E.; Bodere, A.; Garros, A.; Merlini-l’Heritier, A.; Bouguen, G.; Siproudhis, L. Anal Ulcerations in Crohn’s Disease: Natural History in the Era of Biological Therapy. Dig. Liver Dis. 2017, 49, 1191–1195. [Google Scholar] [CrossRef] [PubMed]
- Lightner, A.L.; Ashburn, J.H.; Brar, M.S.; Carvello, M.; Chandrasinghe, P.; van Overstraeten, A.B.; Fleshner, P.R.; Gallo, G.; Kotze, P.G.; Holubar, S.D.; et al. Fistulizing Crohn’s Disease. Curr. Probl. Surg. 2020, 57, 100808. [Google Scholar] [CrossRef] [PubMed]
- Sandborn, W.J.; Fazio, V.W.; Feagan, B.G.; Hanauer, S.B. American Gastroenterological Association Clinical Practice Committee. AGA Technical Review on Perianal Crohn’s Disease. Gastroenterology 2003, 125, 1508–1530. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, I.; Nuij, V.J.A.A.; van der Meulen-de Jong, A.E.; van der Woude, C.J. Disappointing Durable Remission Rates in Complex Crohn’s Disease Fistula. Inflamm. Bowel Dis. 2014, 20, 2022–2028. [Google Scholar] [CrossRef] [Green Version]
- Kirchgesner, J.; Lemaitre, M.; Rudnichi, A.; Racine, A.; Zureik, M.; Carbonnel, F.; Dray-Spira, R. Therapeutic Management of Inflammatory Bowel Disease in Real-Life Practice in the Current Era of Anti-TNF Agents: Analysis of the French Administrative Health Databases 2009–2014. Aliment. Pharmacol. Ther. 2017, 45, 37–49. [Google Scholar] [CrossRef]
- Schwartz, D.A.; Ghazi, L.J.; Regueiro, M.; Fichera, A.; Zoccali, M.; Ong, E.M.W.; Mortelé, K.J. Crohn’s & Colitis Foundation of America, Inc. Guidelines for the Multidisciplinary Management of Crohn’s Perianal Fistulas: Summary Statement. Inflamm. Bowel Dis. 2015, 21, 723–730. [Google Scholar] [CrossRef]
- Present, D.H.; Rutgeerts, P.; Targan, S.; Hanauer, S.B.; Mayer, L.; van Hogezand, R.A.; Podolsky, D.K.; Sands, B.E.; Braakman, T.; DeWoody, K.L.; et al. Infliximab for the Treatment of Fistulas in Patients with Crohn’s Disease. N. Engl. J. Med. 1999, 340, 1398–1405. [Google Scholar] [CrossRef] [Green Version]
- Sands, B.E.; Anderson, F.H.; Bernstein, C.N.; Chey, W.Y.; Feagan, B.G.; Fedorak, R.N.; Kamm, M.A.; Korzenik, J.R.; Lashner, B.A.; Onken, J.E.; et al. Infliximab Maintenance Therapy for Fistulizing Crohn’s Disease. N. Engl. J. Med. 2004, 350, 876–885. [Google Scholar] [CrossRef] [PubMed]
- Panaccione, R.; Colombel, J.-F.; Sandborn, W.J.; D’Haens, G.; Zhou, Q.; Pollack, P.F.; Thakkar, R.B.; Robinson, A.M. Adalimumab Maintains Remission of Crohn’s Disease after up to 4 Years of Treatment: Data from CHARM and ADHERE. Aliment. Pharmacol. Ther. 2013, 38, 1236–1247. [Google Scholar] [CrossRef]
- Roumeguère, P.; Bouchard, D.; Pigot, F.; Castinel, A.; Juguet, F.; Gaye, D.; Capdepont, M.; Zerbib, F.; Laharie, D. Combined Approach with Infliximab, Surgery, and Methotrexate in Severe Fistulizing Anoperineal Crohn’s Disease: Results from a Prospective Study. Inflamm. Bowel Dis. 2011, 17, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Yarur, A.J.; Kanagala, V.; Stein, D.J.; Czul, F.; Quintero, M.A.; Agrawal, D.; Patel, A.; Best, K.; Fox, C.; Idstein, K.; et al. Higher Infliximab Trough Levels Are Associated with Perianal Fistula Healing in Patients with Crohn’s Disease. Aliment. Pharmacol. Ther. 2017, 45, 933–940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouguen, G.; Siproudhis, L.; Gizard, E.; Wallenhorst, T.; Billioud, V.; Bretagne, J.-F.; Bigard, M.-A.; Peyrin-Biroulet, L. Long-Term Outcome of Perianal Fistulizing Crohn’s Disease Treated with Infliximab. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2013, 11, 975–981. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haennig, A.; Staumont, G.; Lepage, B.; Faure, P.; Alric, L.; Buscail, L.; Bournet, B.; Moreau, J. The Results of Seton Drainage Combined with Anti-TNFα Therapy for Anal Fistula in Crohn’s Disease. Colorectal Dis. 2015, 17, 311–319. [Google Scholar] [CrossRef]
- Dibley, L.; Norton, C. Experiences of Fecal Incontinence in People with Inflammatory Bowel Disease: Self-Reported Experiences among a Community Sample. Inflamm. Bowel Dis. 2013, 19, 1450–1462. [Google Scholar] [CrossRef]
- Mahadev, S.; Young, J.M.; Selby, W.; Solomon, M.J. Quality of Life in Perianal Crohn’s Disease: What Do Patients Consider Important? Dis. Colon Rectum 2011, 54, 579–585. [Google Scholar] [CrossRef]
- Zhang, X.-M.; Zhang, Y.-J.; Wang, W.; Wei, Y.-Q.; Deng, H.-X. Mesenchymal Stem Cells to Treat Crohn’s Disease with Fistula. Hum. Gene Ther. 2017, 28, 534–540. [Google Scholar] [CrossRef]
- Grégoire, C.; Lechanteur, C.; Briquet, A.; Baudoux, É.; Baron, F.; Louis, E.; Beguin, Y. Review Article: Mesenchymal Stromal Cell Therapy for Inflammatory Bowel Diseases. Aliment. Pharmacol. Ther. 2017, 45, 205–221. [Google Scholar] [CrossRef] [Green Version]
- Qiu, Y.; Li, M.-Y.; Feng, T.; Feng, R.; Mao, R.; Chen, B.-L.; He, Y.; Zeng, Z.-R.; Zhang, S.-H.; Chen, M.-H. Systematic Review with Meta-Analysis: The Efficacy and Safety of Stem Cell Therapy for Crohn’s Disease. Stem Cell Res. Ther. 2017, 8, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lightner, A.L.; Wang, Z.; Zubair, A.C.; Dozois, E.J. A Systematic Review and Meta-Analysis of Mesenchymal Stem Cell Injections for the Treatment of Perianal Crohn’s Disease: Progress Made and Future Directions. Dis. Colon Rectum 2018, 61, 629–640. [Google Scholar] [CrossRef]
- Choi, S.; Jeon, B.G.; Chae, G.; Lee, S.-J. The Clinical Efficacy of Stem Cell Therapy for Complex Perianal Fistulas: A Meta-Analysis. Tech. Coloproctol 2019, 23, 411–427. [Google Scholar] [CrossRef]
- Gallo, G.; Tiesi, V.; Fulginiti, S.; De Paola, G.; Vescio, G.; Sammarco, G. Mesenchymal Stromal Cell Therapy in the Management of Perianal Fistulas in Crohn’s Disease: An Up-To-Date Review. Med. Kaunas Lith. 2020, 56, 563. [Google Scholar] [CrossRef]
- Bourin, P.; Bunnell, B.A.; Casteilla, L.; Dominici, M.; Katz, A.J.; March, K.L.; Redl, H.; Rubin, J.P.; Yoshimura, K.; Gimble, J.M. Stromal Cells from the Adipose Tissue-Derived Stromal Vascular Fraction and Culture Expanded Adipose Tissue-Derived Stromal/Stem Cells: A Joint Statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy 2013, 15, 641–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miana, V.V.; González, E.A.P. Adipose Tissue Stem Cells in Regenerative Medicine. Ecancermedicalscience 2018, 12, 822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carvello, M.; Lightner, A.; Yamamoto, T.; Kotze, P.G.; Spinelli, A. Mesenchymal Stem Cells for Perianal Crohn’s Disease. Cells 2019, 8, 764. [Google Scholar] [CrossRef] [Green Version]
- Lombardi, F.; Palumbo, P.; Augello, F.R.; Cifone, M.G.; Cinque, B.; Giuliani, M. Secretome of Adipose Tissue-Derived Stem Cells (ASCs) as a Novel Trend in Chronic Non-Healing Wounds: An Overview of Experimental In Vitro and In Vivo Studies and Methodological Variables. Int. J. Mol. Sci. 2019, 20, 3721. [Google Scholar] [CrossRef] [Green Version]
- Qomi, R.T.; Sheykhhasan, M. Adipose-Derived Stromal Cell in Regenerative Medicine: A Review. World J. Stem Cells 2017, 9, 107–117. [Google Scholar] [CrossRef]
- Hughes, L.E. Clinical Classification of Perianal Crohn’s Disease. Dis. Colon Rectum 1992, 35, 928–932. [Google Scholar] [CrossRef]
- Rackovsky, O.; Hirten, R.; Ungaro, R.; Colombel, J.-F. Clinical Updates on Perianal Fistulas in Crohn’s Disease. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 597–605. [Google Scholar] [CrossRef]
- Irvine, E.J. Usual Therapy Improves Perianal Crohn’s Disease as Measured by a New Disease Activity Index. McMaster IBD Study Group. J. Clin. Gastroenterol. 1995, 20, 27–32. [Google Scholar]
- Horaist, C.; de Parades, V.; Abramowitz, L.; Benfredj, P.; Bonnaud, G.; Bouchard, D.; Fathallah, N.; Sénéjoux, A.; Siproudhis, L.; Staumont, G.; et al. Elaboration and Validation of Crohn’s Disease Anoperineal Lesions Consensual Definitions. World J. Gastroenterol. 2017, 23, 5371–5378. [Google Scholar] [CrossRef]
- Vermeire, S.; Schreiber, S.; Sandborn, W.J.; Dubois, C.; Rutgeerts, P. Correlation between the Crohn’s Disease Activity and Harvey-Bradshaw Indices in Assessing Crohn’s Disease Severity. Clin. Gastroenterol. Hepatol. 2010, 8, 357–363. [Google Scholar] [CrossRef]
- Van Assche, G.; Vanbeckevoort, D.; Bielen, D.; Coremans, G.; Aerden, I.; Noman, M.; D’Hoore, A.; Penninckx, F.; Marchal, G.; Cornillie, F.; et al. Magnetic Resonance Imaging of the Effects of Infliximab on Perianal Fistulizing Crohn’s Disease. Am. J. Gastroenterol. 2003, 98, 332–339. [Google Scholar] [CrossRef]
- Garros, A.; Siproudhis, L.; Tchoundjeu, B.; Rohou, T.; Brochard, C.; Wallenhorst, T.; Bretagne, J.-F.; Bouguen, G. Magnetic Resonance Imaging and Clinical Assessments for Perianal Crohn’s Disease: Gain and Limits. Dig. Liver Dis. 2014, 46, 1072–1076. [Google Scholar] [CrossRef]
- Thomassin, L.; Armengol-Debeir, L.; Charpentier, C.; Bridoux, V.; Koning, E.; Savoye, G.; Savoye-Collet, C. Magnetic Resonance Imaging May Predict Deep Remission in Patients with Perianal Fistulizing Crohn’s Disease. World J. Gastroenterol. 2017, 23, 4285–4292. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, G.N.; Owen, H.A.; Torkington, J.; Lunniss, P.J.; Nicholls, R.J.; Cohen, C.R.G. Long-Term Outcome Following Loose-Seton Technique for External Sphincter Preservation in Complex Anal Fistula. Br. J. Surg. 2004, 91, 476–480. [Google Scholar] [CrossRef] [PubMed]
- van Koperen, P.J.; Safiruddin, F.; Bemelman, W.A.; Slors, J.F.M. Outcome of Surgical Treatment for Fistula in Ano in Crohn’s Disease. Br. J. Surg. 2009, 96, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Soltani, A.; Kaiser, A.M. Endorectal Advancement Flap for Cryptoglandular or Crohn’s Fistula-in-Ano. Dis. Colon Rectum 2010, 53, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Heywood, N.; Adegbola, S.; Tozer, P.; Sahnan, K.; Fearnhead, N.S.; Brown, S.R. ENiGMA Collaborators. Systematic Review of Surgical Interventions for Crohn’s Anal Fistula. BJS Open 2017, 1, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Grimaud, J.-C.; Munoz-Bongrand, N.; Siproudhis, L.; Abramowitz, L.; Sénéjoux, A.; Vitton, V.; Gambiez, L.; Flourié, B.; Hébuterne, X.; Louis, E.; et al. Fibrin Glue Is Effective Healing Perianal Fistulas in Patients with Crohn’s Disease. Gastroenterology 2010, 138, 2275–2281. [Google Scholar] [CrossRef]
- Senéjoux, A.; Siproudhis, L.; Abramowitz, L.; Munoz-Bongrand, N.; Desseaux, K.; Bouguen, G.; Bourreille, A.; Dewit, O.; Stefanescu, C.; Vernier, G.; et al. Fistula Plug in Fistulising Ano-Perineal Crohn’s Disease: A Randomised Controlled Trial. J. Crohns Colitis 2016, 10, 141–148. [Google Scholar] [CrossRef]
- Bondi, J.; Avdagic, J.; Karlbom, U.; Hallböök, O.; Kalman, D.; Benth, J.; Naimy, N.; Øresland, T. Randomized Clinical Trial Comparing Collagen Plug and Advancement Flap for Trans-Sphincteric Anal Fistula. Br. J. Surg. 2017, 104, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.C.; Luthra, P.; Hanauer, S.B.; Travis, S.P.; Harris, M.S.; Reinisch, W. Placebo Response Rate in Clinical Trials of Fistulizing Crohn’s Disease: Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2014, 12, 1981–1990. [Google Scholar] [CrossRef]
- Kawalec, P.; Mikrut, A.; Wiśniewska, N.; Pilc, A. Tumor Necrosis Factor-α Antibodies (Infliximab, Adalimumab and Certolizumab) in Crohn’s Disease: Systematic Review and Meta-Analysis. Arch. Med. Sci. AMS 2013, 9, 765–779. [Google Scholar] [CrossRef]
- Tougeron, D.; Savoye, G.; Savoye-Collet, C.; Koning, E.; Michot, F.; Lerebours, E. Predicting Factors of Fistula Healing and Clinical Remission after Infliximab-Based Combined Therapy for Perianal Fistulizing Crohn’s Disease. Dig. Dis. Sci. 2009, 54, 1746–1752. [Google Scholar] [CrossRef]
- Colombel, J.-F.; Schwartz, D.A.; Sandborn, W.J.; Kamm, M.A.; D’Haens, G.; Rutgeerts, P.; Enns, R.; Panaccione, R.; Schreiber, S.; Li, J.; et al. Adalimumab for the Treatment of Fistulas in Patients with Crohn’s Disease. Gut 2009, 58, 940–948. [Google Scholar] [CrossRef] [Green Version]
- Talbot, C.; Sagar, P.M.; Johnston, M.J.; Finan, P.J.; Burke, D. Infliximab in the Surgical Management of Complex Fistulating Anal Crohn’s Disease. Colorectal Dis. 2005, 7, 164–168. [Google Scholar] [CrossRef]
- Topstad, D.R.; Panaccione, R.; Heine, J.A.; Johnson, D.R.E.; MacLean, A.R.; Buie, W.D. Combined Seton Placement, Infliximab Infusion, and Maintenance Immunosuppressives Improve Healing Rate in Fistulizing Anorectal Crohn’s Disease: A Single Center Experience. Dis. Colon Rectum 2003, 46, 577–583. [Google Scholar] [CrossRef]
- Regueiro, M.; Mardini, H. Treatment of Perianal Fistulizing Crohn’s Disease with Infliximab Alone or as an Adjunct to Exam under Anesthesia with Seton Placement. Inflamm. Bowel Dis. 2003, 9, 98–103. [Google Scholar] [CrossRef]
- Hyder, S.A.; Travis, S.P.L.; Jewell, D.P.; McC Mortensen, N.J.; George, B.D. Fistulating Anal Crohn’s Disease: Results of Combined Surgical and Infliximab Treatment. Dis. Colon Rectum 2006, 49, 1837–1841. [Google Scholar] [CrossRef]
- Guidi, L.; Ratto, C.; Semeraro, S.; Roberto, I.; De Vitis, I.; Papa, A.; Marzo, M.; Parello, A.; Foglietto, G.; Doglietto, G.B.; et al. Combined Therapy with Infliximab and Seton Drainage for Perianal Fistulizing Crohn’s Disease with Anal Endosonographic Monitoring: A Single-Centre Experience. Tech. Coloproctol. 2008, 12, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, S.; Matsuo, K.; Sasaki, T.; Nakano, M.; Sakai, K.; Beppu, R.; Yamashita, Y.; Maeda, K.; Aoyagi, K. Clinical Advantages of Combined Seton Placement and Infliximab Maintenance Therapy for Perianal Fistulizing Crohn’s Disease: When and How Were the Seton Drains Removed? Hepatogastroenterology 2010, 57, 3–7. [Google Scholar] [PubMed]
- de Groof, E.J.; Sahami, S.; Lucas, C.; Ponsioen, C.Y.; Bemelman, W.A.; Buskens, C.J. Treatment of Perianal Fistula in Crohn’s Disease: A Systematic Review and Meta-Analysis Comparing Seton Drainage and Anti-Tumour Necrosis Factor Treatment. Colorectal Dis. 2016, 18, 667–675. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.J.; Parker, C.E.; Taylor, S.R.; Guizzetti, L.; Feagan, B.G.; Lobo, A.J.; Jairath, V. Efficacy of Medical Therapies for Fistulizing Crohn’s Disease: Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 1879–1892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapuis-Biron, C.; Bourrier, A.; Nachury, M.; Nancey, S.; Bouhnik, Y.; Serrero, M.; Armengol-Debeir, L.; Buisson, A.; Tran-Minh, M.-L.; Zallot, C.; et al. Vedolizumab for Perianal Crohn’s Disease: A Multicentre Cohort Study in 151 Patients. Aliment. Pharmacol. Ther. 2020, 51, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Ungar, B.; Kopylov, U. Editorial: Is Vedolizumab Effective for Perianal Crohn’s Disease? Aliment. Pharmacol. Ther. 2020, 51, 912–913. [Google Scholar] [CrossRef] [PubMed]
- Verstockt, B.; Ferrante, M.; Vermeire, S.; Van Assche, G. New Treatment Options for Inflammatory Bowel Diseases. J. Gastroenterol. 2018, 53, 585–590. [Google Scholar] [CrossRef] [Green Version]
- Dulai, P.S.; Singh, S.; Jiang, X.; Peerani, F.; Narula, N.; Chaudrey, K.; Whitehead, D.; Hudesman, D.; Lukin, D.; Swaminath, A.; et al. The Real-World Effectiveness and Safety of Vedolizumab for Moderate-Severe Crohn’s Disease: Results From the US VICTORY Consortium. Am. J. Gastroenterol. 2016, 111, 1147–1155. [Google Scholar] [CrossRef]
- Chapuis-Biron, C.; Kirchgesner, J.; Pariente, B.; Bouhnik, Y.; Amiot, A.; Viennot, S.; Serrero, M.; Fumery, M.; Allez, M.; Siproudhis, L.; et al. Ustekinumab for Perianal Crohn’s Disease: The BioLAP Multicenter Study From the GETAID. Am. J. Gastroenterol. 2020, 115, 1812–1820. [Google Scholar] [CrossRef]
- Biemans, V.B.C.; Jong, A.E.V.D.M.-D.; van der Woude, C.J.; Löwenberg, M.; Dijkstra, G.; Oldenburg, B.; de Boer, N.K.H.; van der Marel, S.; Bodelier, A.G.L.; Jansen, J.M.; et al. Ustekinumab for Crohn’s Disease: Results of the ICC Registry, a Nationwide Prospective Observational Cohort Study. J. Crohns Colitis 2020, 14, 33–45. [Google Scholar] [CrossRef]
- Corte, H.; Maggiori, L.; Treton, X.; Lefevre, J.H.; Ferron, M.; Panis, Y. Rectovaginal Fistula: What Is the Optimal Strategy?: An Analysis of 79 Patients Undergoing 286 Procedures. Ann. Surg. 2015, 262, 855–860. [Google Scholar] [CrossRef]
- Andreani, S.M.; Dang, H.H.; Grondona, P.; Khan, A.Z.; Edwards, D.P. Rectovaginal Fistula in Crohn’s Disease. Dis. Colon Rectum 2007, 50, 2215–2222. [Google Scholar] [CrossRef]
- Sands, B.E.; Blank, M.A.; Patel, K.; van Deventer, S.J. Long-Term Treatment of Rectovaginal Fistulas in Crohn’s Disease: Response to Infliximab in the ACCENT II Study. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2004, 2, 912–920. [Google Scholar] [CrossRef]
- Panés, J.; García-Olmo, D.; Van Assche, G.; Colombel, J.F.; Reinisch, W.; Baumgart, D.C.; Dignass, A.; Nachury, M.; Ferrante, M.; Kazemi-Shirazi, L.; et al. Expanded Allogeneic Adipose-Derived Mesenchymal Stem Cells (Cx601) for Complex Perianal Fistulas in Crohn’s Disease: A Phase 3 Randomised, Double-Blind Controlled Trial. Lancet 2016, 388, 1281–1290. [Google Scholar] [CrossRef]
- Panés, J.; García-Olmo, D.; Van Assche, G.; Colombel, J.F.; Reinisch, W.; Baumgart, D.C.; Dignass, A.; Nachury, M.; Ferrante, M.; Kazemi-Shirazi, L.; et al. Long-Term Efficacy and Safety of Stem Cell Therapy (Cx601) for Complex Perianal Fistulas in Patients With Crohn’s Disease. Gastroenterology 2018, 154, 1334–1342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zuk, P.A.; Zhu, M.; Mizuno, H.; Huang, J.; Futrell, J.W.; Katz, A.J.; Benhaim, P.; Lorenz, H.P.; Hedrick, M.H. Multilineage Cells from Human Adipose Tissue: Implications for Cell-Based Therapies. Tissue Eng. 2001, 7, 211–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strem, B.M.; Hicok, K.C.; Zhu, M.; Wulur, I.; Alfonso, Z.; Schreiber, R.E.; Fraser, J.K.; Hedrick, M.H. Multipotential Differentiation of Adipose Tissue-Derived Stem Cells. Keio J. Med. 2005, 54, 132–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fraser, J.K.; Schreiber, R.; Strem, B.; Zhu, M.; Alfonso, Z.; Wulur, I.; Hedrick, M.H. Plasticity of Human Adipose Stem Cells toward Endothelial Cells and Cardiomyocytes. Nat. Clin. Pract. Cardiovasc. Med. 2006, 3, S33–S37. [Google Scholar] [CrossRef]
- Charbord, P.; Casteilla, L. Human mesenchymal stem cell biology. Med. Sci. 2011, 27, 261–267. [Google Scholar] [CrossRef] [Green Version]
- Marquez-Curtis, L.A.; Janowska-Wieczorek, A.; McGann, L.E.; Elliott, J.A.W. Mesenchymal Stromal Cells Derived from Various Tissues: Biological, Clinical and Cryopreservation Aspects. Cryobiology 2015, 71, 181–197. [Google Scholar] [CrossRef] [Green Version]
- Strioga, M.; Viswanathan, S.; Darinskas, A.; Slaby, O.; Michalek, J. Same or Not the Same? Comparison of Adipose Tissue-Derived versus Bone Marrow-Derived Mesenchymal Stem and Stromal Cells. Stem Cells Dev. 2012, 21, 2724–2752. [Google Scholar] [CrossRef]
- Kern, S.; Eichler, H.; Stoeve, J.; Klüter, H.; Bieback, K. Comparative Analysis of Mesenchymal Stem Cells from Bone Marrow, Umbilical Cord Blood, or Adipose Tissue. Stem Cells Dayt. Ohio 2006, 24, 1294–1301. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, E.M.; Le Blanc, K.; Dominici, M.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.C.; Deans, R.J.; Krause, D.S.; Keating, A. Clarification of the Nomenclature for MSC: The International Society for Cellular Therapy Position Statement. Cytotherapy 2005, 7, 393–395. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal Criteria for Defining Multipotent Mesenchymal Stromal Cells. The International Society for Cellular Therapy Position Statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I. Mesenchymal Stem Cells: Time to Change the Name. Stem Cells Transl. Med. 2017, 6, 1445–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denost, Q.; Pontallier, A.; Buscail, E.; Montembault, A.; Bareille, R.; Siadous, R.; Durand, M.; Delmond, S.; David, L.; Bordenave, L. Colorectal Wall Regeneration Resulting from the Association of Chitosan Hydrogel and Stromal Vascular Fraction from Adipose Tissue. J. Biomed. Mater. Res. A 2018, 106, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Doorn, J.; Moll, G.; Le Blanc, K.; van Blitterswijk, C.; de Boer, J. Therapeutic Applications of Mesenchymal Stromal Cells: Paracrine Effects and Potential Improvements. Tissue Eng. Part B Rev. 2012, 18, 101–115. [Google Scholar] [CrossRef]
- Mitchell, J.B.; McIntosh, K.; Zvonic, S.; Garrett, S.; Floyd, Z.E.; Kloster, A.; Di Halvorsen, Y.; Storms, R.W.; Goh, B.; Kilroy, G.; et al. Immunophenotype of Human Adipose-Derived Cells: Temporal Changes in Stromal-Associated and Stem Cell-Associated Markers. Stem Cells Dayt. Ohio 2006, 24, 376–385. [Google Scholar] [CrossRef]
- Gentile, P.; Calabrese, C.; De Angelis, B.; Pizzicannella, J.; Kothari, A.; Garcovich, S. Impact of the Different Preparation Methods to Obtain Human Adipose-Derived Stromal Vascular Fraction Cells (AD-SVFs) and Human Adipose-Derived Mesenchymal Stem Cells (AD-MSCs): Enzymatic Digestion Versus Mechanical Centrifugation. Int. J. Mol. Sci. 2019, 20, 5471. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Zhou, J.; Zhang, X.; Liu, Y.; Chen, J.; Hu, B.; Song, J.; Zhang, Y. Strategies to Optimize Adult Stem Cell Therapy for Tissue Regeneration. Int. J. Mol. Sci. 2016, 17, 982. [Google Scholar] [CrossRef] [Green Version]
- Katz, A.J.; Tholpady, A.; Tholpady, S.S.; Shang, H.; Ogle, R.C. Cell Surface and Transcriptional Characterization of Human Adipose-Derived Adherent Stromal (HADAS) Cells. Stem Cells Dayt. Ohio 2005, 23, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Gronthos, S.; Franklin, D.M.; Leddy, H.A.; Robey, P.G.; Storms, R.W.; Gimble, J.M. Surface Protein Characterization of Human Adipose Tissue-Derived Stromal Cells. J. Cell. Physiol. 2001, 189, 54–63. [Google Scholar] [CrossRef]
- Lindroos, B.; Aho, K.-L.; Kuokkanen, H.; Räty, S.; Huhtala, H.; Lemponen, R.; Yli-Harja, O.; Suuronen, R.; Miettinen, S. Differential Gene Expression in Adipose Stem Cells Cultured in Allogeneic Human Serum versus Fetal Bovine Serum. Tissue Eng. Part A 2010, 16, 2281–2294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zannettino, A.C.W.; Paton, S.; Arthur, A.; Khor, F.; Itescu, S.; Gimble, J.M.; Gronthos, S. Multipotential Human Adipose-Derived Stromal Stem Cells Exhibit a Perivascular Phenotype in vitro and in vivo. J. Cell. Physiol. 2008, 214, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Lindroos, B.; Boucher, S.; Chase, L.; Kuokkanen, H.; Huhtala, H.; Haataja, R.; Vemuri, M.; Suuronen, R.; Miettinen, S. Serum-Free, Xeno-Free Culture Media Maintain the Proliferation Rate and Multipotentiality of Adipose Stem Cells in vitro. Cytotherapy 2009, 11, 958–972. [Google Scholar] [CrossRef]
- Parker, A.M.; Shang, H.; Khurgel, M.; Katz, A.J. Low Serum and Serum-Free Culture of Multipotential Human Adipose Stem Cells. Cytotherapy 2007, 9, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Qiu, G.; Zheng, G.; Ge, M.; Wang, J.; Huang, R.; Shu, Q.; Xu, J. Mesenchymal Stem Cell-Derived Extracellular Vesicles Affect Disease Outcomes via Transfer of MicroRNAs. Stem Cell Res. Ther. 2018, 9, 320. [Google Scholar] [CrossRef]
- Zheng, G.; Huang, R.; Qiu, G.; Ge, M.; Wang, J.; Shu, Q.; Xu, J. Mesenchymal Stromal Cell-Derived Extracellular Vesicles: Regenerative and Immunomodulatory Effects and Potential Applications in Sepsis. Cell Tissue Res. 2018, 374, 1–15. [Google Scholar] [CrossRef]
- Bruno, S.; Grange, C.; Deregibus, M.C.; Calogero, R.A.; Saviozzi, S.; Collino, F.; Morando, L.; Busca, A.; Falda, M.; Bussolati, B.; et al. Mesenchymal Stem Cell-Derived Microvesicles Protect against Acute Tubular Injury. J. Am. Soc. Nephrol. JASN 2009, 20, 1053–1067. [Google Scholar] [CrossRef] [Green Version]
- dos Santos, C.C.; Murthy, S.; Hu, P.; Shan, Y.; Haitsma, J.J.; Mei, S.H.J.; Stewart, D.J.; Liles, W.C. Network Analysis of Transcriptional Responses Induced by Mesenchymal Stem Cell Treatment of Experimental Sepsis. Am. J. Pathol. 2012, 181, 1681–1692. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Zhang, G.; Cheng, Z.; Yin, D.; Du, T.; Ju, G.; Miao, S.; Liu, G.; Lu, M.; Zhu, Y. Microvesicles Derived from Human Wharton’s Jelly Mesenchymal Stromal Cells Ameliorate Renal Ischemia-Reperfusion Injury in Rats by Suppressing CX3CL1. Stem Cell Res. Ther. 2014, 5, 40. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.Y.; Kim, W.K.; Oh, K.-J.; Han, B.S.; Lee, S.C.; Bae, K.-H. Recent Advances in Proteomic Studies of Adipose Tissues and Adipocytes. Int. J. Mol. Sci. 2015, 16, 4581–4599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coelho, M.; Oliveira, T.; Fernandes, R. Biochemistry of Adipose Tissue: An Endocrine Organ. Arch. Med. Sci. AMS 2013, 9, 191–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, M.V.; Morrison, T.J.; Doherty, D.F.; McAuley, D.F.; Matthay, M.A.; Kissenpfennig, A.; O’Kane, C.M.; Krasnodembskaya, A.D. Mitochondrial Transfer via Tunneling Nanotubes Is an Important Mechanism by Which Mesenchymal Stem Cells Enhance Macrophage Phagocytosis in the In Vitro and In Vivo Models of ARDS. Stem Cells Dayt. Ohio 2016, 34, 2210–2223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gnecchi, M.; Zhang, Z.; Ni, A.; Dzau, V.J. Paracrine Mechanisms in Adult Stem Cell Signaling and Therapy. Circ. Res. 2008, 103, 1204–1219. [Google Scholar] [CrossRef]
- Dubey, N.K.; Mishra, V.K.; Dubey, R.; Deng, Y.-H.; Tsai, F.-C.; Deng, W.-P. Revisiting the Advances in Isolation, Characterization and Secretome of Adipose-Derived Stromal/Stem Cells. Int. J. Mol. Sci. 2018, 19, 2200. [Google Scholar] [CrossRef] [Green Version]
- Ortiz-Virumbrales, M.; Menta, R.; Pérez, L.M.; Lucchesi, O.; Mancheño-Corvo, P.; Avivar-Valderas, Á.; Palacios, I.; Herrero-Mendez, A.; Dalemans, W.; de la Rosa, O.; et al. Human Adipose Mesenchymal Stem Cells Modulate Myeloid Cells toward an Anti-Inflammatory and Reparative Phenotype: Role of IL-6 and PGE2. Stem Cell Res. Ther. 2020, 11, 462. [Google Scholar] [CrossRef]
- Rehman, J.; Traktuev, D.; Li, J.; Merfeld-Clauss, S.; Temm-Grove, C.J.; Bovenkerk, J.E.; Pell, C.L.; Johnstone, B.H.; Considine, R.V.; March, K.L. Secretion of Angiogenic and Antiapoptotic Factors by Human Adipose Stromal Cells. Circulation 2004, 109, 1292–1298. [Google Scholar] [CrossRef]
- Tan, S.S.; Han, X.; Sivakumaran, P.; Lim, S.Y.; Morrison, W.A. Melatonin Protects Human Adipose-Derived Stem Cells from Oxidative Stress and Cell Death. Arch. Plast. Surg. 2016, 43, 237–241. [Google Scholar] [CrossRef] [Green Version]
- Mirabet, V.; Solves, P.; Miñana, M.D.; Encabo, A.; Carbonell-Uberos, F.; Blanquer, A.; Roig, R. Human Platelet Lysate Enhances the Proliferative Activity of Cultured Human Fibroblast-like Cells from Different Tissues. Cell Tissue Bank. 2008, 9, 1–10. [Google Scholar] [CrossRef]
- English, K. Mechanisms of Mesenchymal Stromal Cell Immunomodulation. Immunol. Cell Biol. 2013, 91, 19–26. [Google Scholar] [CrossRef] [Green Version]
- Ryan, J.M.; Barry, F.; Murphy, J.M.; Mahon, B.P. Interferon-Gamma Does Not Break, but Promotes the Immunosuppressive Capacity of Adult Human Mesenchymal Stem Cells. Clin. Exp. Immunol. 2007, 149, 353–363. [Google Scholar] [CrossRef]
- Ankrum, J.A.; Ong, J.F.; Karp, J.M. Mesenchymal Stem Cells: Immune Evasive, Not Immune Privileged. Nat. Biotechnol. 2014, 32, 252–260. [Google Scholar] [CrossRef] [Green Version]
- DelaRosa, O.; Sánchez-Correa, B.; Morgado, S.; Ramírez, C.; del Río, B.; Menta, R.; Lombardo, E.; Tarazona, R.; Casado, J.G. Human Adipose-Derived Stem Cells Impair Natural Killer Cell Function and Exhibit Low Susceptibility to Natural Killer-Mediated Lysis. Stem Cells Dev. 2012, 21, 1333–1343. [Google Scholar] [CrossRef] [Green Version]
- Sung, D.K.; Chang, Y.S.; Sung, S.I.; Yoo, H.S.; Ahn, S.Y.; Park, W.S. Antibacterial Effect of Mesenchymal Stem Cells against Escherichia Coli Is Mediated by Secretion of Beta- Defensin- 2 via Toll- like Receptor 4 Signalling. Cell. Microbiol. 2016, 18, 424–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, Y.-X.; Xu, J.-F.; Seeley, E.J.; Tang, X.-D.; Xu, L.-L.; Zhu, Y.-G.; Song, Y.-L.; Qu, J.-M. Adipose Tissue-Derived Mesenchymal Stem Cells Attenuate Pulmonary Infection Caused by Pseudomonas Aeruginosa via Inhibiting Overproduction of Prostaglandin E2. Stem Cells Dayt. Ohio 2015, 33, 2331–2342. [Google Scholar] [CrossRef] [PubMed]
- Zhu, P.; Liu, J.; Shi, J.; Zhou, Q.; Liu, J.; Zhang, X.; Du, Z.; Liu, Q.; Guo, Y. Melatonin Protects ADSCs from ROS and Enhances Their Therapeutic Potency in a Rat Model of Myocardial Infarction. J. Cell. Mol. Med. 2015, 19, 2232–2243. [Google Scholar] [CrossRef] [PubMed]
- Cousin, B.; Ravet, E.; Poglio, S.; De Toni, F.; Bertuzzi, M.; Lulka, H.; Touil, I.; André, M.; Grolleau, J.-L.; Péron, J.-M.; et al. Adult Stromal Cells Derived from Human Adipose Tissue Provoke Pancreatic Cancer Cell Death Both in vitro and in vivo. PLoS ONE 2009, 4, e6278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, W.; Wein, F.; Seckinger, A.; Frankhauser, M.; Wirkner, U.; Krause, U.; Blake, J.; Schwager, C.; Eckstein, V.; Ansorge, W.; et al. Comparative Characteristics of Mesenchymal Stem Cells from Human Bone Marrow, Adipose Tissue, and Umbilical Cord Blood. Exp. Hematol. 2005, 33, 1402–1416. [Google Scholar] [CrossRef]
- Izadpanah, R.; Trygg, C.; Patel, B.; Kriedt, C.; Dufour, J.; Gimble, J.M.; Bunnell, B.A. Biologic Properties of Mesenchymal Stem Cells Derived from Bone Marrow and Adipose Tissue. J. Cell. Biochem. 2006, 99, 1285–1297. [Google Scholar] [CrossRef] [Green Version]
- Barlow, S.; Brooke, G.; Chatterjee, K.; Price, G.; Pelekanos, R.; Rossetti, T.; Doody, M.; Venter, D.; Pain, S.; Gilshenan, K.; et al. Comparison of Human Placenta- and Bone Marrow-Derived Multipotent Mesenchymal Stem Cells. Stem Cells Dev. 2008, 17, 1095–1107. [Google Scholar] [CrossRef] [Green Version]
- Dufrane, D. Impact of Age on Human Adipose Stem Cells for Bone Tissue Engineering. Cell Transplant. 2017, 26, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Ertaş, G.; Ural, E.; Ural, D.; Aksoy, A.; Kozdağ, G.; Gacar, G.; Karaöz, E. Comparative Analysis of Apoptotic Resistance of Mesenchymal Stem Cells Isolated from Human Bone Marrow and Adipose Tissue. Sci. World J. 2012, 2012, 105698. [Google Scholar] [CrossRef]
- Melief, S.M.; Zwaginga, J.J.; Fibbe, W.E.; Roelofs, H. Adipose Tissue-Derived Multipotent Stromal Cells Have a Higher Immunomodulatory Capacity than Their Bone Marrow-Derived Counterparts. Stem Cells Transl. Med. 2013, 2, 455–463. [Google Scholar] [CrossRef]
- Bislenghi, G.; Wolthuis, A.; Van Assche, G.; Vermeire, S.; Ferrante, M.; D’Hoore, A. Cx601 (Darvadstrocel) for the Treatment of Perianal Fistulizing Crohn’s Disease. Expert Opin. Biol. Ther. 2019, 19, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Avivar-Valderas, A.; Martín-Martín, C.; Ramírez, C.; Del Río, B.; Menta, R.; Mancheño-Corvo, P.; Ortiz-Virumbrales, M.; Herrero-Méndez, Á.; Panés, J.; García-Olmo, D.; et al. Dissecting Allo-Sensitization After Local Administration of Human Allogeneic Adipose Mesenchymal Stem Cells in Perianal Fistulas of Crohn’s Disease Patients. Front. Immunol. 2019, 10, 1244. [Google Scholar] [CrossRef] [Green Version]
- Kastrup, J.; Haack-Sørensen, M.; Juhl, M.; Søndergaard, R.H.; Follin, B.; Lund, L.D.; Johansen, E.M.; Qayyum, A.A.; Mathiasen, A.B.; Jørgensen, E.; et al. Cryopreserved Off-the-Shelf Allogeneic Adipose-Derived Stromal Cells for Therapy in Patients with Ischemic Heart Disease and Heart Failure-A Safety Study. Stem Cells Transl. Med. 2017, 6, 1963–1971. [Google Scholar] [CrossRef] [PubMed]
- Guijarro, D.; Lebrin, M.; Lairez, O.; Bourin, P.; Piriou, N.; Pozzo, J.; Lande, G.; Berry, M.; Le Tourneau, T.; Cussac, D.; et al. Intramyocardial Transplantation of Mesenchymal Stromal Cells for Chronic Myocardial Ischemia and Impaired Left Ventricular Function: Results of the MESAMI 1 Pilot Trial. Int. J. Cardiol. 2016, 209, 258–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bura, A.; Planat-Benard, V.; Bourin, P.; Silvestre, J.-S.; Gross, F.; Grolleau, J.-L.; Saint-Lebese, B.; Peyrafitte, J.-A.; Fleury, S.; Gadelorge, M.; et al. Phase I Trial: The Use of Autologous Cultured Adipose-Derived Stroma/Stem Cells to Treat Patients with Non-Revascularizable Critical Limb Ischemia. Cytotherapy 2014, 16, 245–257. [Google Scholar] [CrossRef] [Green Version]
- Takahashi, H.; Sakata, N.; Yoshimatsu, G.; Hasegawa, S.; Kodama, S. Regenerative and Transplantation Medicine: Cellular Therapy Using Adipose Tissue-Derived Mesenchymal Stromal Cells for Type 1 Diabetes Mellitus. J. Clin. Med. 2019, 8, 249. [Google Scholar] [CrossRef] [Green Version]
- Pers, Y.-M.; Rackwitz, L.; Ferreira, R.; Pullig, O.; Delfour, C.; Barry, F.; Sensebe, L.; Casteilla, L.; Fleury, S.; Bourin, P.; et al. Adipose Mesenchymal Stromal Cell-Based Therapy for Severe Osteoarthritis of the Knee: A Phase I Dose-Escalation Trial. Stem Cells Transl. Med. 2016, 5, 847–856. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peeters, C.M.M.; Leijs, M.J.C.; Reijman, M.; van Osch, G.J.V.M.; Bos, P.K. Safety of Intra-Articular Cell-Therapy with Culture-Expanded Stem Cells in Humans: A Systematic Literature Review. Osteoarthr. Cartil. 2013, 21, 1465–1473. [Google Scholar] [CrossRef] [Green Version]
- Freitag, J.; Bates, D.; Wickham, J.; Shah, K.; Huguenin, L.; Tenen, A.; Paterson, K.; Boyd, R. Adipose-Derived Mesenchymal Stem Cell Therapy in the Treatment of Knee Osteoarthritis: A Randomized Controlled Trial. Regen. Med. 2019, 14, 213–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowles, A.C.; Wise, R.M.; Gerstein, B.Y.; Thomas, R.C.; Ogelman, R.; Manayan, R.C.; Bunnell, B.A. Adipose Stromal Vascular Fraction Attenuates TH1 Cell-Mediated Pathology in a Model of Multiple Sclerosis. J. Neuroinflam. 2018, 15, 77. [Google Scholar] [CrossRef] [Green Version]
- Kwak, K.-A.; Cho, H.-J.; Yang, J.-Y.; Park, Y.-S. Current Perspectives Regarding Stem Cell-Based Therapy for Liver Cirrhosis. Can. J. Gastroenterol. Hepatol. 2018, 2018, 4197857. [Google Scholar] [CrossRef] [PubMed]
- Jurado, M.; De La Mata, C.; Ruiz-García, A.; López-Fernández, E.; Espinosa, O.; Remigia, M.J.; Moratalla, L.; Goterris, R.; García-Martín, P.; Ruiz-Cabello, F.; et al. Adipose Tissue-Derived Mesenchymal Stromal Cells as Part of Therapy for Chronic Graft-versus-Host Disease: A Phase I/II Study. Cytotherapy 2017, 19, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Rogers, C.J.; Harman, R.J.; Bunnell, B.A.; Schreiber, M.A.; Xiang, C.; Wang, F.-S.; Santidrian, A.F.; Minev, B.R. Rationale for the Clinical Use of Adipose-Derived Mesenchymal Stem Cells for COVID-19 Patients. J. Transl. Med. 2020, 18, 203. [Google Scholar] [CrossRef] [PubMed]
- Toyserkani, N.M.; Jørgensen, M.G.; Tabatabaeifar, S.; Jensen, C.H.; Sheikh, S.P.; Sørensen, J.A. Concise Review: A Safety Assessment of Adipose-Derived Cell Therapy in Clinical Trials: A Systematic Review of Reported Adverse Events. Stem Cells Transl. Med. 2017, 6, 1786–1794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhai, Y.; Wu, W.; Xi, X.; Yu, R. Adipose-Derived Stem Cells Promote Proliferation and Invasion in Cervical Cancer by Targeting the HGF/c-MET Pathway. Cancer Manag. Res. 2020, 12, 11823–11832. [Google Scholar] [CrossRef] [PubMed]
- Scioli, M.G.; Storti, G.; D’Amico, F.; Gentile, P.; Kim, B.-S.; Cervelli, V.; Orlandi, A. Adipose-Derived Stem Cells in Cancer Progression: New Perspectives and Opportunities. Int. J. Mol. Sci. 2019, 20, 3296. [Google Scholar] [CrossRef] [Green Version]
- Sabol, R.A.; Giacomelli, P.; Beighley, A.; Bunnell, B.A. Adipose Stem Cells and Cancer: Concise Review. Stem Cells Dayt. Ohio 2019, 37, 1261–1266. [Google Scholar] [CrossRef] [Green Version]
- Ejaz, A.; Yang, K.S.; Venkatesh, K.P.; Chinnapaka, S.; Kokai, L.E.; Rubin, J.P. The Impact of Human Lipoaspirate and Adipose Tissue-Derived Stem Cells Contact Culture on Breast Cancer Cells: Implications in Breast Reconstruction. Int. J. Mol. Sci. 2020, 21, 9171. [Google Scholar] [CrossRef] [PubMed]
- Ryska, O.; Serclova, Z.; Mestak, O.; Matouskova, E.; Vesely, P.; Mrazova, I. Local Application of Adipose-Derived Mesenchymal Stem Cells Supports the Healing of Fistula: Prospective Randomised Study on Rat Model of Fistulising Crohn’s Disease. Scand. J. Gastroenterol. 2017, 52, 543–550. [Google Scholar] [CrossRef]
- Cao, Y.; Ding, Z.; Han, C.; Shi, H.; Cui, L.; Lin, R. Efficacy of Mesenchymal Stromal Cells for Fistula Treatment of Crohn’s Disease: A Systematic Review and Meta-Analysis. Dig. Dis. Sci. 2017, 62, 851–860. [Google Scholar] [CrossRef]
- Cheng, F.; Huang, Z.; Li, Z. Efficacy and Safety of Mesenchymal Stem Cells in Treatment of Complex Perianal Fistulas: A Meta-Analysis. Stem Cells Int. 2020, 2020, 8816737. [Google Scholar] [CrossRef] [PubMed]
- Aso, K.; Tsuruhara, A.; Takagaki, K.; Oki, K.; Ota, M.; Nose, Y.; Tanemura, H.; Urushihata, N.; Sasanuma, J.; Sano, M.; et al. Adipose-Derived Mesenchymal Stem Cells Restore Impaired Mucosal Immune Responses in Aged Mice. PLoS ONE 2016, 11, e0148185. [Google Scholar] [CrossRef] [Green Version]
- Flacs, M.; Collard, M.; Doblas, S.; Zappa, M.; Cazals-Hatem, D.; Maggiori, L.; Panis, Y.; Treton, X.; Ogier-Denis, E. Preclinical Model of Perianal Fistulizing Crohn’s Disease. Inflamm. Bowel Dis. 2020, 26, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Olmo, D.; Herreros, D.; Pascual, I.; Pascual, J.A.; Del-Valle, E.; Zorrilla, J.; De-La-Quintana, P.; Garcia-Arranz, M.; Pascual, M. Expanded Adipose-Derived Stem Cells for the Treatment of Complex Perianal Fistula: A Phase II Clinical Trial. Dis. Colon Rectum 2009, 52, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Guadalajara, H.; Herreros, D.; De-La-Quintana, P.; Trebol, J.; Garcia-Arranz, M.; Garcia-Olmo, D. Long-Term Follow-up of Patients Undergoing Adipose-Derived Adult Stem Cell Administration to Treat Complex Perianal Fistulas. Int. J. Colorectal Dis. 2012, 27, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.Y.; Park, K.J.; Cho, Y.B.; Yoon, S.N.; Song, K.H.; Kim, D.S.; Jung, S.H.; Kim, M.; Yoo, H.-W.; Kim, I.; et al. Autologous Adipose Tissue-Derived Stem Cells Treatment Demonstrated Favorable and Sustainable Therapeutic Effect for Crohn’s Fistula. Stem Cells Dayt. Ohio 2013, 31, 2575–2581. [Google Scholar] [CrossRef]
- de la Portilla, F.; Alba, F.; García-Olmo, D.; Herrerías, J.M.; González, F.X.; Galindo, A. Expanded Allogeneic Adipose-Derived Stem Cells (EASCs) for the Treatment of Complex Perianal Fistula in Crohn’s Disease: Results from a Multicenter Phase I/IIa Clinical Trial. Int. J. Colorectal Dis. 2013, 28, 313–323. [Google Scholar] [CrossRef]
- Cho, Y.B.; Park, K.J.; Yoon, S.N.; Song, K.H.; Kim, D.S.; Jung, S.H.; Kim, M.; Jeong, H.Y.; Yu, C.S. Long-Term Results of Adipose-Derived Stem Cell Therapy for the Treatment of Crohn’s Fistula. Stem Cells Transl. Med. 2015, 4, 532–537. [Google Scholar] [CrossRef]
- Dietz, A.B.; Dozois, E.J.; Fletcher, J.G.; Butler, G.W.; Radel, D.; Lightner, A.L.; Dave, M.; Friton, J.; Nair, A.; Camilleri, E.T.; et al. Autologous Mesenchymal Stem Cells, Applied in a Bioabsorbable Matrix, for Treatment of Perianal Fistulas in Patients With Crohn’s Disease. Gastroenterology 2017, 153, 59–62. [Google Scholar] [CrossRef]
- Dige, A.; Hougaard, H.T.; Agnholt, J.; Pedersen, B.G.; Tencerova, M.; Kassem, M.; Krogh, K.; Lundby, L. Efficacy of Injection of Freshly Collected Autologous Adipose Tissue Into Perianal Fistulas in Patients With Crohn’s Disease. Gastroenterology 2019, 156, 2208–2216. [Google Scholar] [CrossRef] [Green Version]
- Serrero, M.; Grimaud, F.; Philandrianos, C.; Visée, C.; Sabatier, F.; Grimaud, J.-C. Long-Term Safety and Efficacy of Local Microinjection Combining Autologous Microfat and Adipose-Derived Stromal Vascular Fraction for the Treatment of Refractory Perianal Fistula in Crohn’s Disease. Gastroenterology 2019, 156, 2335–2337. [Google Scholar] [CrossRef]
- Herreros, M.D.; Garcia-Olmo, D.; Guadalajara, H.; Georgiev-Hristov, T.; Brandariz, L.; Garcia-Arranz, M. Stem Cell Therapy: A Compassionate Use Program in Perianal Fistula. Stem Cells Int. 2019, 2019, 6132340. [Google Scholar] [CrossRef] [Green Version]
- Zhou, C.; Li, M.; Zhang, Y.; Ni, M.; Wang, Y.; Xu, D.; Shi, Y.; Zhang, B.; Chen, Y.; Huang, Y.; et al. Autologous Adipose-Derived Stem Cells for the Treatment of Crohn’s Fistula-in-Ano: An Open-Label, Controlled Trial. Stem Cell Res. Ther. 2020, 11, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwandner, O. Stem Cell Injection for Complex Anal Fistula in Crohn’s Disease: A Single-Center Experience. World J. Gastroenterol. 2021, 27, 3643–3653. [Google Scholar] [CrossRef] [PubMed]
- Cassinotti, A.; Annaloro, C.; Ardizzone, S.; Onida, F.; Della Volpe, A.; Clerici, M.; Usardi, P.; Greco, S.; Maconi, G.; Porro, G.B.; et al. Autologous Haematopoietic Stem Cell Transplantation without CD34+ Cell Selection in Refractory Crohn’s Disease. Gut 2008, 57, 211–217. [Google Scholar] [CrossRef]
- Gregoire, C.; Briquet, A.; Pirenne, C.; Lechanteur, C.; Louis, E.; Beguin, Y. Allogeneic Mesenchymal Stromal Cells for Refractory Luminal Crohn’s Disease: A Phase I-II Study. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2018, 50, 1251–1255. [Google Scholar] [CrossRef]
- Dave, M.; Jaiswal, P.; Cominelli, F. Mesenchymal Stem/Stromal Cell Therapy for Inflammatory Bowel Disease: An Updated Review with Maintenance of Remission. Curr. Opin. Gastroenterol. 2017, 33, 59–68. [Google Scholar] [CrossRef]
- Garcia-Arranz, M.; Garcia-Olmo, D.; Herreros, M.D.; Gracia-Solana, J.; Guadalajara, H.; de la Portilla, F.; Baixauli, J.; Garcia-Garcia, J.; Ramirez, J.M.; Sanchez-Guijo, F.; et al. Autologous Adipose-Derived Stem Cells for the Treatment of Complex Cryptoglandular Perianal Fistula: A Randomized Clinical Trial with Long-Term Follow-Up. Stem Cells Transl. Med. 2020, 9, 295–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dozois, E.J.; Lightner, A.L.; Mathis, K.L.; Chua, H.K.; Kelley, S.R.; Fletcher, J.G.; Dietz, A.B.; Friton, J.J.; Butler, G.W.; Faubion, W.A. Early Results of a Phase I Trial Using an Adipose-Derived Mesenchymal Stem Cell-Coated Fistula Plug for the Treatment of Transsphincteric Cryptoglandular Fistulas. Dis. Colon Rectum 2019, 62, 615–622. [Google Scholar] [CrossRef] [PubMed]
- García-Arranz, M.; Herreros, M.D.; González-Gómez, C.; de la Quintana, P.; Guadalajara, H.; Georgiev-Hristov, T.; Trébol, J.; Garcia-Olmo, D. Treatment of Crohn’s-Related Rectovaginal Fistula With Allogeneic Expanded-Adipose Derived Stem Cells: A Phase I-IIa Clinical Trial. Stem Cells Transl. Med. 2016, 5, 1441–1446. [Google Scholar] [CrossRef]
- Lightner, A.L.; Dozois, E.J.; Dietz, A.B.; Fletcher, J.G.; Friton, J.; Butler, G.; Faubion, W.A. Matrix-Delivered Autologous Mesenchymal Stem Cell Therapy for Refractory Rectovaginal Crohn’s Fistulas. Inflamm. Bowel Dis. 2020, 26, 670–677. [Google Scholar] [CrossRef]
- Bouchard, D.; Abramowitz, L.; Bouguen, G.; Brochard, C.; Dabadie, A.; de Parades, V.; Eléouet-Kaplan, M.; Fathallah, N.; Faucheron, J.-L.; Maggiori, L.; et al. Anoperineal Lesions in Crohn’s Disease: French Recommendations for Clinical Practice. Tech. Coloproctol. 2017, 21, 683–691. [Google Scholar] [CrossRef]
- Gionchetti, P.; Dignass, A.; Danese, S.; Dias, F.J.M.; Rogler, G.; Lakatos, P.L.; Adamina, M.; Ardizzone, S.; Buskens, C.J.; Sebastian, S.; et al. 3rd European Evidence-Based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 2: Surgical Management and Special Situations. J. Crohns Colitis 2017, 11, 135–149. [Google Scholar] [CrossRef] [Green Version]
- Park, I.-S. Enhancement of Wound Healing by Conditioned Medium of Adipose-Derived Stromal Cell with Photobiomodulation in Skin Wound. Int. J. Stem Cells 2021, 14, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhang, M.; Lu, G.-L.; Huang, B.-X.; Wang, D.-W.; Shao, Y.; Lu, M.-J. Hypoxic Preconditioning Enhances Cellular Viability and Pro-Angiogenic Paracrine Activity: The Roles of VEGF-A and SDF-1a in Rat Adipose Stem Cells. Front. Cell Dev. Biol. 2020, 8, 580131. [Google Scholar] [CrossRef] [PubMed]




| Author, Year, [ref] | Phase, Design (Patient Number) | Cell Type (Additional Procedure) | Number of Cells Injected (×107) | Concomitant Treatments | Evaluation Criteria | Time Point (Weeks) | Complete Healing | Total Follow-Up (Weeks) | Related Adverse Events |
|---|---|---|---|---|---|---|---|---|---|
| Garcia-Olmo 2009 [135] | II, prospective (49, 14 with CD) | Autologous (+fibrin glue vs. fibrin glue alone) | 2 | yes | Clinical + QoL | 8 | 71% | 48 | none |
| Guadalajara, 2012 [136] | II, retrospective, monocentre (50) | Autologous? (+fibrin glue versus fibrin glue alone) | 2 | yes | Clinical + MRI | 152 | 58% | 168 | 1 (2%) |
| Lee, 2013 [137] | I, prospective, multicentre (43) | Autologous (+fibrin glue) | 3 | yes | Clinical | 4, 6 and 8 | 79% | - | none |
| De La Portilla, 2013 [138] | I/IIa, multicentre (24) | Allogenic | 2 | yes | Clinical + MRI | 24 | 56% | - | 4 (16.5%) |
| Cho, 2015 [139] | II (43) | Autologous | 3 | yes | Clinical | 48 | 79% | 96 | none |
| Panes, 2016 [67] | III, prospective, multicentre, controlled (212) | Allogenic (*) | 12 | yes | Clinical + MRI | 24 | 50% versus 34% in placebo | 24 | 18 (17%) |
| Panes, 2018 [68] | III, prospective, multicentre, controlled (212) | Allogenic (*) | 12 | yes | Clinical + MRI | 52 | 56% versus 38% in placebo | 52 | - |
| Dietz, 2017 [140] | I, monocentre, open label single arm (12) | Autologous (+plug matrix) | 2 (twice) | yes | Clinical | 24 | 83% | 24 | none |
| Dige, 2019 [141] | I, monocentre, open label single arm (21) | Autologous SVF | - | yes | 24 | 76% | 24 | 1 (5%) | |
| Serrero, 2019 [142] | I, monocentre, open label single arm (10) | Autologous SVF (+microfat grafting) | 1 to 6 | yes | Clinical + MRI | 12 and 48 | 70 and 80% at 24 and 48 weeks respectively | 48 | 3 (30%) |
| Herreros, 2019 [143] | Monocentre, observational (45 with 18 CD) | Allogenic & Autologous SVF (**) | 0.2 to 6 | no | Clinical | 24 | 46% | 26 | none |
| Zhou, 2020 [144] | Monocentre, observational (22) | Autologous, versus surgery alone | 0.5 | yes | Clinical + MRI or EUS | 12, 24 and 48 | 90, 72 and 63% at 12, 24 and 48 weeks respectively | 48 | none |
| Schwandner, 2021 [145] | Mononcenter Observational Retrospective (12) | Allogenic (*) | 12 | yes | Clinical | 12 | 67% | 56 | 4 (33%) |
| ID Number Name Country | Phase (Number of Patients) | Protocol Design and Cells | Main Endpoints |
|---|---|---|---|
| NCT03466515 Stem Cell Treatment of Complex Crohn’s Perianal Fistula. A Pilot Study Denmark | I (20) | Injection in and around the fistula track of autologous fat tissue and ADSC from SVF (Cytori Celusion system®) | Healing (clinical + MRI), time to healing, AE |
| NCT03913572 Treatment of Perianal Disease Using Adipose-derived Stem Cells USA | Retrospective, observational (25) | Group 1: surgery + one single injection of ADSC derived from SVF (Revolve System—Acelity®) Group 2: surgery alone | Healing at 4 months Clinical + MRI Assessment of PDAI + Adverse Events |
| NCT03279081 Efficacy and Safety of Cx601, Adult Allogeneic Expanded ADSC for the Treatment of Complex Perianal Fistula(s) in Participants With Crohn’s Disease (CD) (ADMIRE-CD-II) USA | III Randomized, controlled (554) | Cx601 (Darvadstrocel, Alofisel) 12 × 107 ADSC versus placebo, single intra-fistula injection | Clinical remission, clinical response, combined response (*) Clinical + MRI evaluation at 24 and 52 weeks TRAE |
| NCT04118088 Postauthorization Safety Study of the Long-Term Safety and Efficacy of Repeat Administration of Darvadstrocel in Patients With Crohn’s Disease and Complex Perianal Fistula EU, USA | IV (50) | Observational Repeat injection in patients 12 × 107 ADSC (Cx601—Darvadstrocel—Alofisel) | Safety = TRAE |
| NCT04010526 Double-blind Randomised Placebo Controlled Study Evaluating Local Co-administration of Autologous Adipose-Derived Stromal Vascular Fraction with Microfat for Refractory Perianal Crohn’s Fistulas France | II (84) | Double-blind randomised Placebo Controlled Single injection of both ADSC from SVF and microfat tissue in the fistula track versus placebo injection | Healing at 24 weeks, clinical + MRI PDAI TRAE |
| NCT04075825 A Follow-up of a Phase 3 Study to Evaluate the Long-term Safety and Efficacy of Darvadstrocel in the Treatment of Complex Perianal Fistula in Subjects With Crohn’s Disease who have Participated in ADMIRE II Study USA | (≤554) | Participants who received a single dose of darvadstrocel (Cx601), 120 million cells, intralesionally or darvadstrocel matching placebo previously in the ADMIRE-CD II study will be observed for efficacy and safety | AE and TRAE from baseline to week 156 Clinical response and remission at weeks 104 and 156 Relapse(s) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buscail, E.; Le Cosquer, G.; Gross, F.; Lebrin, M.; Bugarel, L.; Deraison, C.; Vergnolle, N.; Bournet, B.; Gilletta, C.; Buscail, L. Adipose-Derived Stem Cells in the Treatment of Perianal Fistulas in Crohn’s Disease: Rationale, Clinical Results and Perspectives. Int. J. Mol. Sci. 2021, 22, 9967. https://doi.org/10.3390/ijms22189967
Buscail E, Le Cosquer G, Gross F, Lebrin M, Bugarel L, Deraison C, Vergnolle N, Bournet B, Gilletta C, Buscail L. Adipose-Derived Stem Cells in the Treatment of Perianal Fistulas in Crohn’s Disease: Rationale, Clinical Results and Perspectives. International Journal of Molecular Sciences. 2021; 22(18):9967. https://doi.org/10.3390/ijms22189967
Chicago/Turabian StyleBuscail, Etienne, Guillaume Le Cosquer, Fabian Gross, Marine Lebrin, Laetitia Bugarel, Céline Deraison, Nathalie Vergnolle, Barbara Bournet, Cyrielle Gilletta, and Louis Buscail. 2021. "Adipose-Derived Stem Cells in the Treatment of Perianal Fistulas in Crohn’s Disease: Rationale, Clinical Results and Perspectives" International Journal of Molecular Sciences 22, no. 18: 9967. https://doi.org/10.3390/ijms22189967
APA StyleBuscail, E., Le Cosquer, G., Gross, F., Lebrin, M., Bugarel, L., Deraison, C., Vergnolle, N., Bournet, B., Gilletta, C., & Buscail, L. (2021). Adipose-Derived Stem Cells in the Treatment of Perianal Fistulas in Crohn’s Disease: Rationale, Clinical Results and Perspectives. International Journal of Molecular Sciences, 22(18), 9967. https://doi.org/10.3390/ijms22189967







