New Fast Acting Glucagon for Recovery from Hypoglycemia, a Life-Threatening Situation: Nasal Powder and Injected Stable Solutions
Abstract
:1. Introduction
1.1. Treatment of Patients with Type 1 and Type 2 Diabetes
1.2. Hypoglycemia in Patients with T1D and T2D
1.2.1. What Is Hypoglycemia, Frequency of Hypoglycemia, and Hypoglycemia Unawareness
1.2.2. Hypoglycemia as a Life-Threatening Situation
Hypoglycemia, Cardiovascular Accidents, and Risk of Death
The Link between Hypoglycemia and Cardiovascular Risk
Cognitive Impairment
Quality of Life, Accidents, and Other Impacts
1.2.3. Prevention and Treatment of Hypoglycemia
1.3. The History of Glucagon, Its Use, and Its Limitations
1.3.1. History of Glucagon
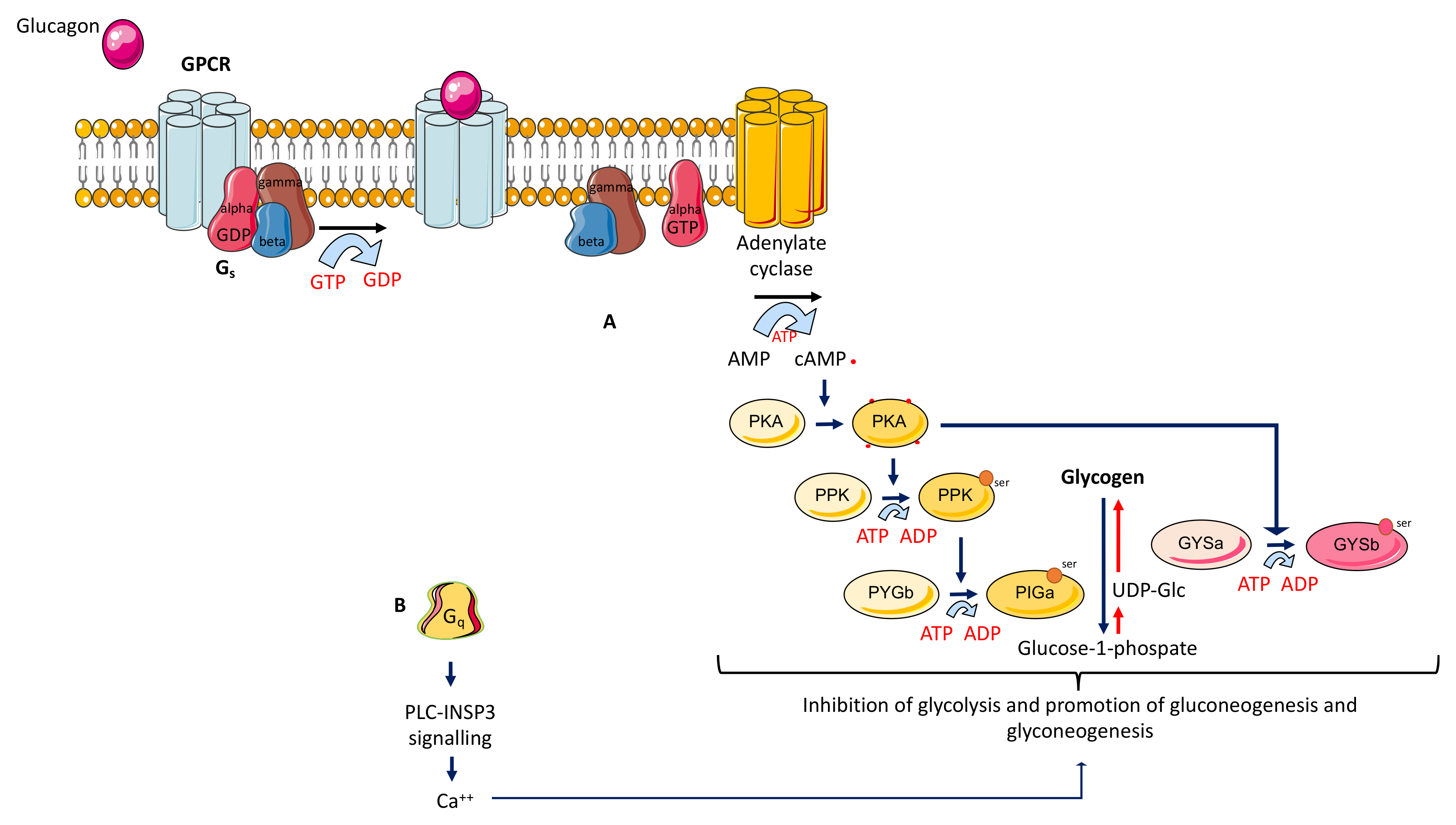
1.3.2. Actions of Glucagon
1.3.3. Indications of Glucagon
1.3.4. Limitations to the Use of Glucagon
1.4. New Fast-Acting Formulations of Glucagon
1.4.1. Nasal Glucagon
1.4.2. Glucagon Stable Solution
1.4.3. Dasiglucagon
1.5. The Future
1.5.1. The Need for Better Education and Awareness of Hypoglycemia
1.5.2. Expanding the Use of Glucagon
1.5.3. Unconscious Patients
1.5.4. Improvement of Metabolic Control and Prevention of Complications
1.5.5. Development of New Glucagon Molecules
2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Hypoglycaemia Study Group. Glucose Concentrations of Less Than 3.0 mmol/L (54 mg/dL) Should Be Reported in Clinical Trials: A Joint Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes: Table 1. Diabetes Care 2017, 40, 155–157. [Google Scholar] [CrossRef]
- Cryer, P.E.; Davis, S.N.; Shamoon, H. Hypoglycemia in diabetes. Diabetes Care 2003, 26, 1902–1912. [Google Scholar] [CrossRef] [PubMed]
- UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: Effects of treatment modalities and their duration. Diabetologia 2007, 50, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- Seaquist, E.R.; Anderson, J.; Childs, B.; Cryer, P.; Dagogo-Jack, S.; Fish, L.; Heller, S.R.; Rodriguez, H.; Rosenzweig, J.; Vigersky, R. Hypoglycemia and Diabetes: A Report of a Workgroup of the American Diabetes Association and The Endocrine Society. Diabetes Care 2013, 36, 1384–1395. [Google Scholar] [CrossRef] [PubMed]
- Beck, R.W.; Tamborlane, W.V.; Bergenstal, R.M.; Miller, K.M.; DuBose, S.N.; Hall, C.A. The T1D Exchange clinic registry. J. Clin. Endocrinol. Metab. 2012, 97, 4383–4389. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef] [PubMed]
- MacLeod, K.; Hepburn, D.; Frier, B. Frequency and Morbidity of Severe Hypoglycaemia in Insulin-treated Diabetic Patients. Diabet. Med. 1993, 10, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Leese, G.P.; Wang, J.; Broomhall, J.; Kelly, P.T.; Marsden, A.; Morrison, W.; Frier, B.M.; Morris, A.D. Frequency of Severe Hypoglycemia Requiring Emergency Treatment in Type 1 and Type 2 Diabetes: A population-based study of health service resource use. Diabetes Care 2003, 26, 1176–1180. [Google Scholar] [CrossRef]
- Geller, A.I.; Shehab, N.; Lovegrove, M.C.; Kegler, S.R.; Weidenbach, K.N.; Ryan, G.J.; Budnitz, D. National Estimates of Insulin-Related Hypoglycemia and Errors Leading to Emergency Department Visits and Hospitalizations. JAMA Intern. Med. 2014, 174, 678–686. [Google Scholar] [CrossRef]
- Pontiroli, A.E.; Miele, L.; Morabito, A. Metabolic control and risk of hypoglycaemia during the first year of intensive insulin treatment in type 2 diabetes: Systematic review and meta-analysis. Diabetes, Obes. Metab. 2011, 14, 433–446. [Google Scholar] [CrossRef]
- Misra-Hebert, A.D.; Pantalone, K.M.; Ji, X.; Milinovich, A.; Dey, T.; Chagin, K.M.; Bauman, J.M.; Kattan, M.W.; Zimmerman, R.S. Patient Characteristics Associated with Severe Hypoglycemia in a Type 2 Diabetes Cohort in a Large, Integrated Health Care System From 2006 to 2015. Diabetes Care 2018, 41, 1164–1171. [Google Scholar] [CrossRef]
- Amiel, S.A. The consequences of hypoglycaemia. Diabetologia 2021, 64, 963–970. [Google Scholar] [CrossRef]
- Goto, A.; Arah, O.; Goto, M.; Terauchi, Y.; Noda, M. Severe hypoglycaemia and cardiovascular disease: Systematic review and meta-analysis with bias analysis. BMJ 2013, 347, f4533. [Google Scholar] [CrossRef]
- Nunes, A.P.; Iglay, K.; Radican, L.; Engel, S.S.; Yang, J.; Doherty, M.C.; Dore, D. Hypoglycaemia seriousness and weight gain as determinants of cardiovascular disease outcomes among sulfonylurea users. Diabetes Obes. Metab. 2017, 19, 1425–1435. [Google Scholar] [CrossRef]
- Cryer, P.E. Mechanisms of Hypoglycemia-Associated Autonomic Failure in Diabetes. N. Engl. J. Med. 2013, 369, 362–372. [Google Scholar] [CrossRef]
- Reno, C.M.; Daphna-Iken, D.; Chen, Y.S.; VanderWeele, J.; Jethi, K.; Fisher, S.J. Severe Hypoglycemia–Induced Lethal Cardiac Arrhythmias Are Mediated by Sympathoadrenal Activation. Diabetes 2013, 62, 3570–3581. [Google Scholar] [CrossRef]
- Puente, E.C.; Silverstein, J.; Bree, A.J.; Musikantow, D.R.; Wozniak, D.F.; Maloney, S.; Daphna-Iken, R.; Fisher, S.J. Recurrent Moderate Hypoglycemia Ameliorates Brain Damage and Cognitive Dysfunction Induced by Severe Hypoglycemia. Diabetes 2010, 59, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Reno, C.M.; Tanoli, T.; Bree, A.; Daphna-Iken, D.; Cui, C.; Maloney, P.S.E.; Wozniak, D.F.; Fisher, S.J. Antecedent glycemic control reduces severe hypoglycemia-induced neuronal damage in diabetic rats. Am. J. Physiol. Metab. 2013, 304, E1331–E1337. [Google Scholar] [CrossRef] [PubMed]
- Tanenberg, R.J.; Newton, C.A.; Drake, A.J. Confirmation of Hypoglycemia in the “Dead-In-Bed” Syndrome, as Captured by a Retrospective Continuous Glucose Monitoring System. Endocr. Pract. 2010, 16, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Skrivarhaug, T.; Bangstad, H.-J.; Stene, L.C.; Sandvik, L.; Hanssen, K.F.; Joner, G. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia 2006, 49, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Reno, C.M.; VanderWeele, J.; Bayles, J.; Litvin, M.; Skinner, A.; Jordan, A.; Daphna-Iken, R.; Fisher, S.J. Severe Hypoglycemia–Induced Fatal Cardiac Arrhythmias Are Augmented by Diabetes and Attenuated by Recurrent Hypoglycemia. Diabetes 2017, 66, 3091–3097. [Google Scholar] [CrossRef]
- Pælestik, K.B.; Jespersen, N.R.; Jensen, R.V.; Johnsen, J.; Bøtker, H.E.; Kristiansen, S.B. Effects of hypoglycemia on myocardial susceptibility to ischemia-reperfusion injury and preconditioning in hearts from rats with and without type 2 diabetes. Cardiovasc. Diabetol. 2017, 16, 148. [Google Scholar] [CrossRef]
- Bedenis, R.; Price, A.H.; Robertson, C.M.; Morling, J.; Frier, B.M.; Strachan, M.W.; Price, J.F. Association Between Severe Hypoglycemia, Adverse Macrovascular Events, and Inflammation in the Edinburgh Type 2 Diabetes Study. Diabetes Care 2014, 37, 3301–3308. [Google Scholar] [CrossRef]
- ORIGIN Trial Investigators. Does hypoglycaemia increase the risk of cardiovascular events? A report from the ORIGIN trial. Eur. Heart J. 2013, 34, 3137–3144. [Google Scholar] [CrossRef]
- Soedamah-Muthu, S.S.; Chaturvedi, N.; Toeller, M.; Ferriss, B.; Reboldi, P.; Michel, G.; Manes, C.; Fuller, J.H. Risk Factors for Coronary Heart Disease in Type 1 Diabetic Patients in Europe: The EURODIAB Prospective Complications Study. Diabetes Care 2004, 27, 530–537. [Google Scholar] [CrossRef]
- La Sala, L.; Prattichizzo, F.; Ceriello, A. The link between diabetes and atherosclerosis. Eur. J. Prev. Cardiol. 2019, 26, 15–24. [Google Scholar] [CrossRef]
- Joy, N.G.; Tate, D.B.; Younk, L.M.; Davis, S.N. Effects of Acute and Antecedent Hypoglycemia on Endothelial Function and Markers of Atherothrombotic Balance in Healthy Humans. Diabetes 2015, 64, 2571–2580. [Google Scholar] [CrossRef]
- De Galan, B.E.; Zoungas, S.; Chalmers, J.; Anderson, C.; Dufouil, C.; Pillai, A.; Cooper, M.; Grobbee, D.E.; Hackett, M.; Hamet, P.; et al. Cognitive function and risks of cardiovascular disease and hypoglycaemia in patients with type 2 diabetes: The Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial. Diabetologia 2009, 52, 2328–2336. [Google Scholar] [CrossRef] [PubMed]
- Whitmer, R.A. Hypoglycemic Episodes and Risk of Dementia in Older Patients with Type 2 Diabetes Mellitus. JAMA 2009, 301, 1565–1572. [Google Scholar] [CrossRef] [PubMed]
- DeSouza, C.; Salazar, H.; Cheong, B.; Murgo, J.; Fonseca, V. Association of Hypoglycemia and Cardiac Ischemia: A study based on continuous monitoring. Diabetes Care 2003, 26, 1485–1489. [Google Scholar] [CrossRef] [PubMed]
- Bonds, D.E.; Miller, M.E.; Bergenstal, R.M.; Buse, J.; Byington, R.P.; Cutler, J.A.; Dudl, R.J.; Ismail-Beigi, F.; Kimel, A.R.; Hoogwerf, B.; et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: Retrospective epidemiological analysis of the ACCORD study. BMJ 2010, 340, b4909. [Google Scholar] [CrossRef] [PubMed]
- Zoungas, S.; Patel, A.; Chalmers, J.; De Galan, B.E.; Li, Q.; Billot, L.; Woodward, M.; Ninomiya, T.; Neal, B.; MacMahon, S.; et al. Severe Hypoglycemia and Risks of Vascular Events and Death. N. Engl. J. Med. 2010, 363, 1410–1418. [Google Scholar] [CrossRef]
- La Sala, L.; Pontiroli, A.E. Prevention of Diabetes and Cardiovascular Disease in Obesity. Int. J. Mol. Sci. 2020, 21, 8178. [Google Scholar] [CrossRef] [PubMed]
- Ceriello, A.; La Sala, L.; DE Nigris, V.; Pujadas, G.; Rondinelli, M.; Genovese, S. GLP-1 reduces metalloproteinase-9 induced by both hyperglycemia and hypoglycemia in type 1 diabetes. The possible role of oxidative stress. Ther. Clin. Risk Manag. 2015, 11, 901–903. [Google Scholar] [CrossRef]
- Hwang, J.J.; Parikh, L.; Lacadie, C.; Seo, D.; Lam, W.; Hamza, M.; Schmidt, C.; Dai, F.; Sejling, A.-S.; Belfort-DeAguiar, R.; et al. Hypoglycemia unawareness in type 1 diabetes suppresses brain responses to hypoglycemia. J. Clin. Investig. 2018, 128, 1485–1495. [Google Scholar] [CrossRef]
- Shalimova, A.; Graff, B.; Gasecki, D.; Wolf, J.; Sabisz, A.; Szurowska, E.; Jodzio, K.; Narkiewicz, K. Cognitive Dysfunction in Type 1 Diabetes Mellitus. J. Clin. Endocrinol. Metab. 2019, 104, 2239–2249. [Google Scholar] [CrossRef]
- Hansen, T.I.; Olsen, S.E.; Haferstrom, E.C.D.; Sand, T.; Frier, B.M.; Håberg, A.K.; Bjørgaas, M.R. Cognitive deficits associated with impaired awareness of hypoglycaemia in type 1 diabetes. Diabetology 2017, 60, 971–979. [Google Scholar] [CrossRef]
- McCrimmon, R.J. Consequences of recurrent hypoglycaemia on brain function in diabetes. Diabetology 2021, 64, 971–977. [Google Scholar] [CrossRef]
- Rossi, M.C.; Nicolucci, A.; Ozzello, A.; Gentile, S.; Aglialoro, A.; Chiambretti, A.; Baccetti, F.; Gentile, F.M.; Romeo, F.; Lucisano, G.; et al. Impact of severe and symptomatic hypoglycemia on quality of life and fear of hypoglycemia in type 1 and type 2 diabetes. Results of the Hypos-1 observational study. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 736–743. [Google Scholar] [CrossRef] [PubMed]
- Berra, C.; De Fazio, F.; Azzolini, E.; Albini, M.; Zangrandi, F.; Mirani, M.; Garbossa, S.; Guardado-Mendoza, R.; Condorelli, G.; Folli, F. Hypoglycemia and hyperglycemia are risk factors for falls in the hospital population. Acta Diabetol. 2019, 56, 931–938. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 13. Children and Adolescents: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019, 42, S148–S164. [Google Scholar] [CrossRef] [PubMed]
- Lucidi, P.; Porcellati, F.; Bolli, G.B.; Fanelli, C.G. Prevention and Management of Severe Hypoglycemia and Hypoglycemia Unawareness: Incorporating Sensor Technology. Curr. Diabetes Rep. 2018, 18, 83. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, L.; Freckmann, G.; Ehrmann, D.; Faber-Heinemann, G.; Guerra, S.; Waldenmaier, D.; Hermanns, N. Real-time continuous glucose monitoring in adults with type 1 diabetes and impaired hypoglycaemia awareness or severe hypoglycaemia treated with multiple daily insulin injections (HypoDE): A multicentre, randomised controlled trial. Lancet 2018, 391, 1367–1377. [Google Scholar] [CrossRef]
- Beato-Víbora, P.I.; Arroyo-Díez, F.J. New uses and formulations of glucagon for hypoglycaemia. Drugs Context 2019, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Foa, P.P.; Weinstein, H.R.; Smith, J.A. Secretion of insulin and of a hyperglycemic substance studied by means of pancreatic-femoral cross-circulation experiments. Am. J. Physiol. 1949, 157, 197–204. [Google Scholar] [CrossRef]
- Staub, A.; Sinn, L.; Behrens, O.K. Purification and crystallization of glucagon. J. Biol. Chem. 1955, 214, 619–632. [Google Scholar] [CrossRef]
- Bromer, W.W.; Sinn, L.G.; Staub, A.; Behrens, O.K. The Amino Acid Sequence of Glucagon. Diabetes 1957, 6, 234–238. [Google Scholar] [CrossRef]
- Kulina, G.R.; Rayfield, E.J. The Role of Glucagon in the Pathophysiology and Management of Diabetes. Endocr. Pract. 2016, 22, 612–621. [Google Scholar] [CrossRef]
- Hager, J.; Hansen, L.; Vaisse, C.; Vionnet, N.; Philippi, A.; Poller, W.; Velho, G.; Carcassi, C.; Contu, L.; Julier, C.; et al. A missense mutation in the glucagon receptor gene is associated with non–insulin–dependent diabetes mellitus. Nat. Genet. 1995, 9, 299–304. [Google Scholar] [CrossRef]
- Blauw, H.; Wendl, I.; DeVries, J.H.; Heise, T.; Jax, T.; on behalf of the PCDIAB consortium. Pharmacokinetics and pharmacodynamics of various glucagon dosages at different blood glucose levels. Diabetes Obes. Metab. 2016, 18, 34–39. [Google Scholar] [CrossRef]
- Haymond, M.W.; DuBose, S.N.; Rickels, M.; Wolpert, H.; Shah, V.N.; Sherr, J.; Weinstock, R.S.; Agarwal, S.; Verdejo, A.S.; Cummins, M.J.; et al. Efficacy and Safety of Mini-Dose Glucagon for Treatment of Nonsevere Hypoglycemia in Adults with Type 1 Diabetes. J. Clin. Endocrinol. Metab. 2017, 102, 2994–3001. [Google Scholar] [CrossRef]
- Tinti, D.; Rabbone, I. Mini-doses of glucagon to prevent hypoglycemia in children with type 1 diabetes refusing food: A case series. Acta Diabetol. 2020, 57, 359–365. [Google Scholar] [CrossRef]
- Pacchioni, M.; Orena, C.; Panizza, P.; Cucchi, E.; Del Maschio, A.; Pontiroli, A.E. The hypotonic effect of intranasal and intravenous glucagon in gastrointestinal radiology. Abdom. Imaging 1995, 20, 44–46. [Google Scholar] [CrossRef]
- White, C.M. A review of potential cardiovascular uses of intravenous glucagon administration. J. Clin. Pharmacol. 1999, 39, 442–447. [Google Scholar] [CrossRef]
- Boido, A.; Ceriani, V.; Pontiroli, A.E. Glucagon for hypoglycemic episodes in insulin-treated diabetic patients: A systematic review and meta-analysis with a comparison of glucagon with dextrose and of different glucagon formulations. Acta Diabetol. 2014, 52, 405–412. [Google Scholar] [CrossRef]
- Murata, T.; Okazaki, K.; Yanagisawa, K.; Yamada, K.; Kuribayashi, N.; Totsuka, Y.; Hiyoshi, T.; Naka, M.; Sugimoto, M.; Aoki, Y.; et al. Glucagon Underutilized Among Type 1 Diabetes Mellitus Patients in Japan. Diabetes Technol. Ther. 2013, 15, 748–750. [Google Scholar] [CrossRef]
- Mitchell, B.D.; He, X.; Sturdy, I.M.; Cagle, A.P.; Settles, J.A. Glucagon Prescription Patterns in Patients with Either Type 1 Or 2 Diabetes with Newly Prescribed Insulin. Endocr. Pract. 2016, 22, 123–135. [Google Scholar] [CrossRef]
- Pedersen, J. The Nature of Amyloid-like Glucagon Fibrils. J. Diabetes Sci. Technol. 2010, 4, 1357–1367. [Google Scholar] [CrossRef]
- Driscoll, K.A.; Volkening, L.K.; Haro, H.; Ocean, G.; Wang, Y.; Jackson, C.C.; Clougherty, M.; Hale, D.E.; Klingensmith, G.J.; Laffel, L.; et al. Are children with type 1 diabetes safe at school? Examining parent perceptions. Pediatr. Diabetes 2015, 16, 613–620. [Google Scholar] [CrossRef]
- Pontiroli, A.E.; Alberetto, M.; Pozza, G. Intranasal glucagon raises blood glucose concentrations in healthy volunteers. BMJ 1983, 287, 462–463. [Google Scholar] [CrossRef]
- Pontiroli, A.E.; Alberetto, M.; Calderara, A.; Pajetta, E.; Pozza, G. Nasal administration of glucagon and human calcitonin to healthy subjects: A comparison of powders and spray solutions and of different enhancing agents. Eur. J. Clin. Pharmacol. 1989, 37, 427–430. [Google Scholar] [CrossRef]
- Slama, G.; Alamowitch, C.; Desplanque, N.; Letanoux, M.; Zirinis, P. A new non-invasive method for treating insulin-reaction: Intranasal lyophylized glucagon. Diabetology 1990, 33, 671–674. [Google Scholar] [CrossRef]
- Teshima, D.; Yamauchi, A.; Makino, K.; Kataoka, Y.; Arita, Y.; Nawata, H.; Oishi, R. Nasal glucagon delivery using microcrystalline cellulose in healthy volunteers. Int. J. Pharm. 2002, 233, 61–66. [Google Scholar] [CrossRef]
- Pontiroli, A.E.; Calderara, A.; Pajetta, E.; Alberetto, M.; Pozza, G. Intranasal Glucagon as Remedy for Hypoglycemia: Studies in Healthy Subjects and Type I Diabetic Patients. Diabetes Care 1989, 12, 604–609. [Google Scholar] [CrossRef]
- Rickels, M.R.; Ruedy, K.J.; Foster, N.C.; Piché, C.A.; Dulude, H.; Sherr, J.L.; Tamborlane, W.V.; Bethin, K.E.; DiMeglio, L.A.; Wadwa, R.P.; et al. Intranasal Glucagon for Treatment of Insulin-Induced Hypoglycemia in Adults with Type 1 Diabetes: A Randomized Crossover Noninferiority Study. Diabetes Care 2016, 39, 264–270. [Google Scholar] [CrossRef]
- Sherr, J.; Ruedy, K.J.; Foster, N.C.; Piché, C.A.; Dulude, H.; Rickels, M.; Tamborlane, W.V.; Bethin, K.E.; DiMeglio, L.A.; Fox, L.; et al. Glucagon Nasal Powder: A Promising Alternative to Intramuscular Glucagon in Youth with Type 1 Diabetes. Diabetes Care 2016, 39, 555–562. [Google Scholar] [CrossRef]
- Yale, J.-F.; Dulude, H.; Egeth, M.; Piché, C.A.; Lafontaine, M.; Carballo, D.; Margolies, R.; Dissinger, E.; Shames, A.R.; Kaplowitz, N.; et al. Faster Use and Fewer Failures with Needle-Free Nasal Glucagon Versus Injectable Glucagon in Severe Hypoglycemia Rescue: A Simulation Study. Diabetes Technol. Ther. 2017, 19, 423–432. [Google Scholar] [CrossRef]
- Seaquist, E.R.; Dulude, H.; Zhang, X.M.; Rabasa-Lhoret, R.; Tsoukas, G.M.; Conway, J.R.; Weisnagel, S.J.; Gerety, G.; Woo, V.C.; Zhang, S.; et al. Prospective study evaluating the use of nasal glucagon for the treatment of moderate to severe hypoglycaemia in adults with type 1 diabetes in a real-world setting. Diabetes Obes. Metab. 2018, 20, 1316–1320. [Google Scholar] [CrossRef]
- Guzman, C.B.; Dulude, H.; Piché, C.; Rufiange, M.; Sadoune, A.A.; Rampakakis, E.; Carballo, D.; Triest, M.; Zhang, M.X.; Zhang, S.; et al. Effects of common cold and concomitant administration of nasal decongestant on the pharmacokinetics and pharmacodynamics of nasal glucagon in otherwise healthy participants: A randomized clinical trial. Diabetes Obes. Metab. 2017, 20, 646–653. [Google Scholar] [CrossRef]
- Reno, F.E.; Normand, P.; McInally, K.; Silo, S.; Stotland, P.; Triest, M.; Carballo, D.; Piché, C. A novel nasal powder formulation of glucagon: Toxicology studies in animal models. BMC Pharmacol. Toxicol. 2015, 16, 29. [Google Scholar] [CrossRef]
- Reno, F.E.; Edwards, C.N.; Jensen, M.B.; Török-Bathó, M.; Esdaile, D.J.; Piché, C.; Triest, M.; Carballo, D. Needle-free nasal delivery of glucagon for treatment of diabetes-related severe hypoglycemia: Toxicology of polypropylene resin used in delivery device. Cutan. Ocul. Toxicol. 2016, 35, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Newswanger, B.; Ammons, S.; Phadnis, N.; Ward, W.K.; Castle, J.; Campbell, R.W.; Prestrelski, S.J. Development of a Highly Stable, Nonaqueous Glucagon Formulation for Delivery via Infusion Pump Systems. J. Diabetes Sci. Technol. 2014, 9, 24–33. [Google Scholar] [CrossRef]
- Pohl, R.; Li, M.; Krasner, A.; De Souza, E. Development of Stable Liquid Glucagon Formulations for Use in Artificial Pancreas. J. Diabetes Sci. Technol. 2014, 9, 8–16. [Google Scholar] [CrossRef]
- Haymond, M.W.; Redondo, M.J.; McKay, S.; Cummins, M.J.; Newswanger, B.; Kinzell, J.; Prestrelski, S. Nonaqueous, Mini-Dose Glucagon for Treatment of Mild Hypoglycemia in Adults with Type 1 Diabetes: A Dose-Seeking Study. Diabetes Care 2016, 39, 465–468. [Google Scholar] [CrossRef]
- Valentine, V.; Newswanger, B.; Prestrelski, S.; Andre, A.D.; Garibaldi, M. Human Factors Usability and Validation Studies of a Glucagon Autoinjector in a Simulated Severe Hypoglycemia Rescue Situation. Diabetes Technol. Ther. 2019, 21, 522–530. [Google Scholar] [CrossRef]
- Newswanger, B.; Prestrelski, S.; Andre, A.D. Human factors studies of a prefilled syringe with stable liquid glucagon in a simulated severe hypoglycemia rescue situation. Expert Opin. Drug Deliv. 2019, 16, 1015–1025. [Google Scholar] [CrossRef]
- Hövelmann, U.; Bysted, B.V.; Mouritzen, U.; Macchi, F.; Lamers, D.; Kronshage, B.; Møller, D.V.; Heise, T. Pharmacokinetic and Pharmacodynamic Characteristics of Dasiglucagon, a Novel Soluble and Stable Glucagon Analog. Diabetes Care 2017, 41, 531–537. [Google Scholar] [CrossRef]
- Pieber, T.R.; Aronson, R.; Hövelmann, U.; Willard, J.; Plum-Mörschel, L.; Knudsen, K.M.; Bandak, B.; Tehranchi, R. Dasiglucagon—A Next-Generation Glucagon Analog for Rapid and Effective Treatment of Severe Hypoglycemia: Results of Phase 3 Randomized Double-Blind Clinical Trial. Diabetes Care 2021, 44, 1361–1367. [Google Scholar] [CrossRef]
- Blair, H.A. Dasiglucagon: First Approval. Drugs 2021, 81, 1115–1120. [Google Scholar] [CrossRef]
- Bajpai, S.K.; Cambron-Mellott, M.J.; Peck, E.; Poon, J.L.; Wang, Q.; Mitchell, B.D.; Babrowicz, J.; Child, C.; Raibulet, N.K.; Beusterien, K. Perceptions About Glucagon Delivery Devices for Severe Hypoglycemia: Qualitative Research with Patients, Caregivers, and Acquaintances. Clin. Ther. 2019, 41, 2073–2089.e6. [Google Scholar] [CrossRef]
- Leinwand, B.; Johnsrud, M.; Nguyen, A.; Meyer, J.; Johnson, K. A ready-to-use liquid glucagon for treatment of severe hypoglycemia demonstrates reduced healthcare payer costs in a budget impact model. J. Med. Econ. 2020, 23, 744–750. [Google Scholar] [CrossRef]
- Cherubini, V.; Rabbone, I.; Lombardo, F.; Mossetto, G.; Orsini Federici, M.; Nicolucci, A. Incidence of severe hypoglycemia and possible associated factors in pediatric patients with type 1 diabetes in the real-life, post-Diabetes Control and Complications Trial setting: A systematic review. Pediatr Diabetes 2019, 20, 678–692. [Google Scholar] [CrossRef]
- Wang, J.; Geiss, L.S.; Williams, D.E.; Gregg, E.W. Trends in Emergency Department Visit Rates for Hypoglycemia and Hyperglycemic Crisis among Adults with Diabetes, United States, 2006–2011. PLoS ONE 2015, 10, e0134917. [Google Scholar] [CrossRef]
- Bechara, G.M.; Branco, F.C.; Rodrigues, A.; Chinnici, D.; Chaney, D.; Calliari, L.E.P.; Franco, D.R. “KiDS and Diabetes in Schools” project: Experience with an international educational intervention among parents and school professionals. Pediatr. Diabetes 2018, 19, 756–760. [Google Scholar] [CrossRef]
- Beverly, E.A.; Ritholz, M.D.; Rennie, R.G.; Mort, S. A brief interactive training with medical students improves their diabetes knowledge about hypoglycemia. BMC Med Educ. 2019, 19, 171. [Google Scholar] [CrossRef]
- Dixe, M.D.A.C.R.; Gordo, C.M.G.D.O.; Catarino, H.P.; Kraus, T.; Menino, E.P.D.S.G. Effects of an education program on knowledge and self-perception of school personnel in preparing to care for type 1 diabetes students. Einstein 2020, 18, eAO5101. [Google Scholar] [CrossRef]
- Rabbone, I.; Missineo, A.; Zanetta, S.; Salzano, G.; Schiaffini, R.; Scaramuzza, A.E.; Lombardo, F. Parent and patient knowledge of nasal glucagon use and efficacy in a large cohort of Italian children and adolescents with type 1 diabetes. Diabetes Obes. Metab. 2021, 23, 2004–2005. [Google Scholar] [CrossRef]
- Deeb, L.C.; Dulude, H.; Guzman, C.B.; Zhang, S.; Reiner, B.J.; Piché, C.A.; Pradhan, S.; Zhang, X.M. A phase 3 multicenter, open-label, prospective study designed to evaluate the effectiveness and ease of use of nasal glucagon in the treatment of moderate and severe hypoglycemia in children and adolescents with type 1 diabetes in the home or school setting. Pediatr. Diabetes 2018, 19, 1007–1013. [Google Scholar]
- Hawkes, C.P.; De Leon, D.D.; Rickels, M.R. Novel Preparations of Glucagon for the Prevention and Treatment of Hypoglycemia. Curr. Diab. Rep. 2019, 19, 97. [Google Scholar] [CrossRef]
- Rabinovich, A.; Priefer, R. Glucagon delivery—An overview of current and future devices. Diabetes Metab. Syndr. 2021, 15, 102155. [Google Scholar] [CrossRef]
- Thieu, V.T.; Mitchell, B.D.; Varnado, O.J.; Frier, B.M. Treatment and prevention of severe hypoglycaemia in people with diabetes: Current and new formulations of glucagon. Diabetes Obes. Metab. 2020, 22, 469–479. [Google Scholar] [CrossRef]
| Preparation | Intranasal Glucagon | Subcutaneous Glucagon | Subcutaneous Dasiglucagon | Traditional Intramuscular/Subcutaneous Glucagon Emergency Kits |
|---|---|---|---|---|
| Molecule | glucagon | glucagon | 7 substitutions in glucagon | glucagon |
| Formulation | Dry powder | Stable non acqueous solution | Stable acqueous solution | Acqueous solution to be reconstituted before use |
| Dose suggested adults | 3 mg | 1 mg | 0.6 mg | 1 mg |
| Dose suggested infants | 3 mg | 0.5 mg * | 0.6 mg ** | 0.5 mg *** |
| Pharmacokinetics (PK) § | ||||
| c-max | 3155 pg/mL | 2481 pg/mL | 1570 pmol/L (5444 pg/mL) # | 6900 pg/mL |
| t-max | 15 min | 50 min | 35 min | 13 min |
| T ½ | 38 min | 32 min | 30 min | 26 min |
| Pharmacodynamics (PD) § | ||||
| Time to BG increase °° | 5 min | 9 min | 6–10 min | 6–10 min |
| Increase of BG °° | +102–140 mg/dL | +123–145 mg/dL | +120–140 mg/dL | +132–138 mg/dL |
| -Duration of BG increase °° | >90 min | >90 min | >90 min | >90 min |
| Repeat dose in the case of failure during the first 15 min | + | + | + | + |
| Real world studies | Performed | Performed | Performed | Not performed |
| Side effects | Nausea and vomiting, head and facial discomfort, increased lacrimation, nasal discomfort | Nausea and vomiting, headache | Nausea and vomiting, headache | Nausea and vomiting, headache |
| Contraindications | As for glucagon §§ | As for glucagon §§ | As for glucagon §§ | §§ |
| Approval and date | FDA, 2019 EMA, 2019 | FDA, 2020 (EMA, application 2021) | FDA, 2021 | FDA 1998, EMA 1991 °°° |
| Approved indication | Severe hypoglycemia | Severe hypoglycemia | Severe hypoglycemia | Severe hypoglycemia |
| Commercial name | Baqsimi | Gvoke Hypopen, (Ogluo) | Zegalogue | Glucagon GlucaGen HypoKit |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Sala, L.; Pontiroli, A.E. New Fast Acting Glucagon for Recovery from Hypoglycemia, a Life-Threatening Situation: Nasal Powder and Injected Stable Solutions. Int. J. Mol. Sci. 2021, 22, 10643. https://doi.org/10.3390/ijms221910643
La Sala L, Pontiroli AE. New Fast Acting Glucagon for Recovery from Hypoglycemia, a Life-Threatening Situation: Nasal Powder and Injected Stable Solutions. International Journal of Molecular Sciences. 2021; 22(19):10643. https://doi.org/10.3390/ijms221910643
Chicago/Turabian StyleLa Sala, Lucia, and Antonio E. Pontiroli. 2021. "New Fast Acting Glucagon for Recovery from Hypoglycemia, a Life-Threatening Situation: Nasal Powder and Injected Stable Solutions" International Journal of Molecular Sciences 22, no. 19: 10643. https://doi.org/10.3390/ijms221910643
APA StyleLa Sala, L., & Pontiroli, A. E. (2021). New Fast Acting Glucagon for Recovery from Hypoglycemia, a Life-Threatening Situation: Nasal Powder and Injected Stable Solutions. International Journal of Molecular Sciences, 22(19), 10643. https://doi.org/10.3390/ijms221910643







