Knee Osteoarthritis Progression Is Delayed in Silent Information Regulator 2 Ortholog 1 Knock-in Mice
Abstract
:1. Introduction
2. Results
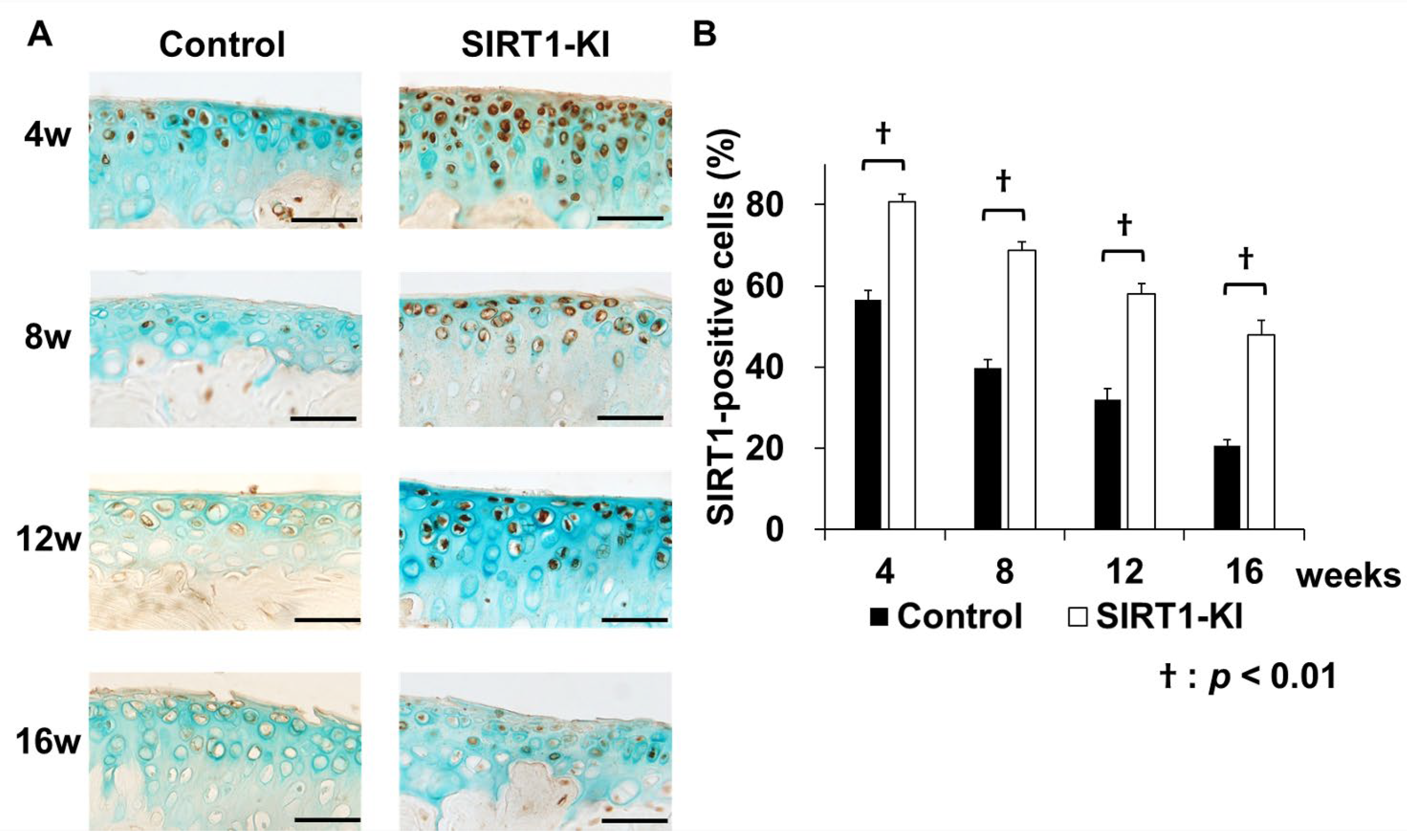
2.1. Features of SIRT1-KI Mice
2.2. Reduced Severity of Cartilage Loss in SIRT-KI Mice after Destabilization via Medial Meniscus Surgery
2.3. SIRT-KI Mice Showed Lower Levels of Cartilage Matrix-Degrading Enzymes, Apoptosis, and Inflammatory Cytokines than Those in Control Mice after OA Induction via Destabilization of Medial Meniscus
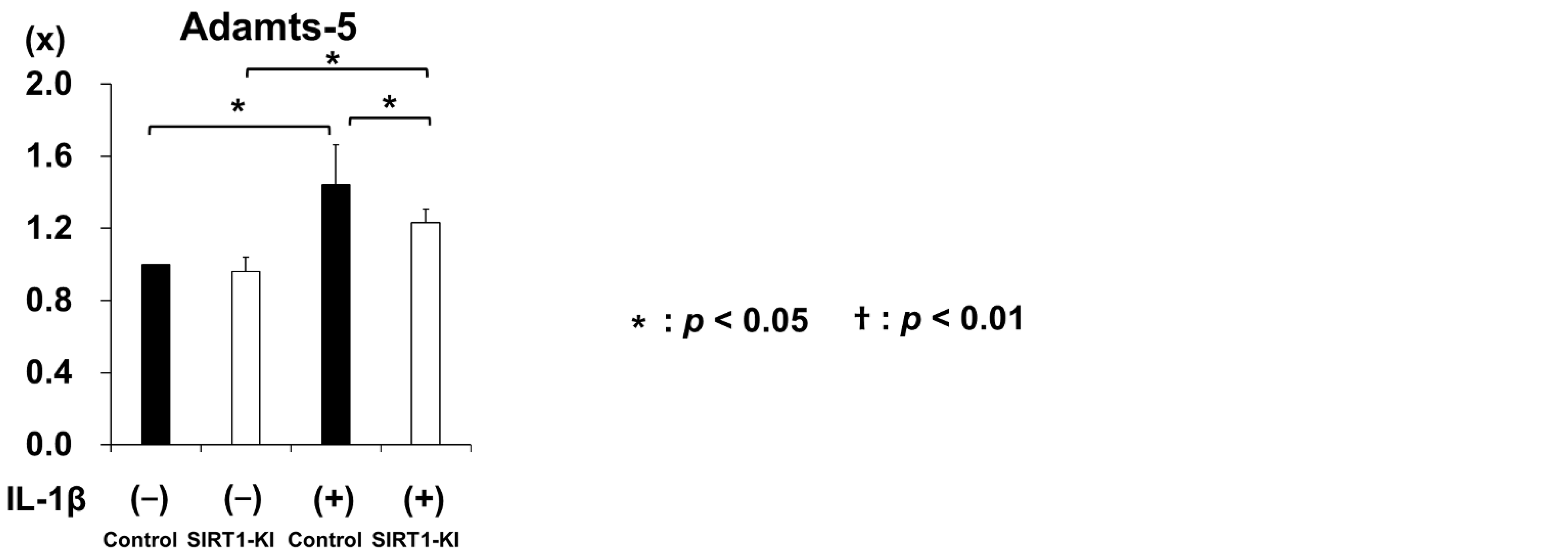
2.4. SIRT1-KI Chondrocytes Showed Higher Expression of Extracellular Matrix Genes than That in the Control Group, whereas Cartilage Degrading Enzyme Genes Were Downregulated
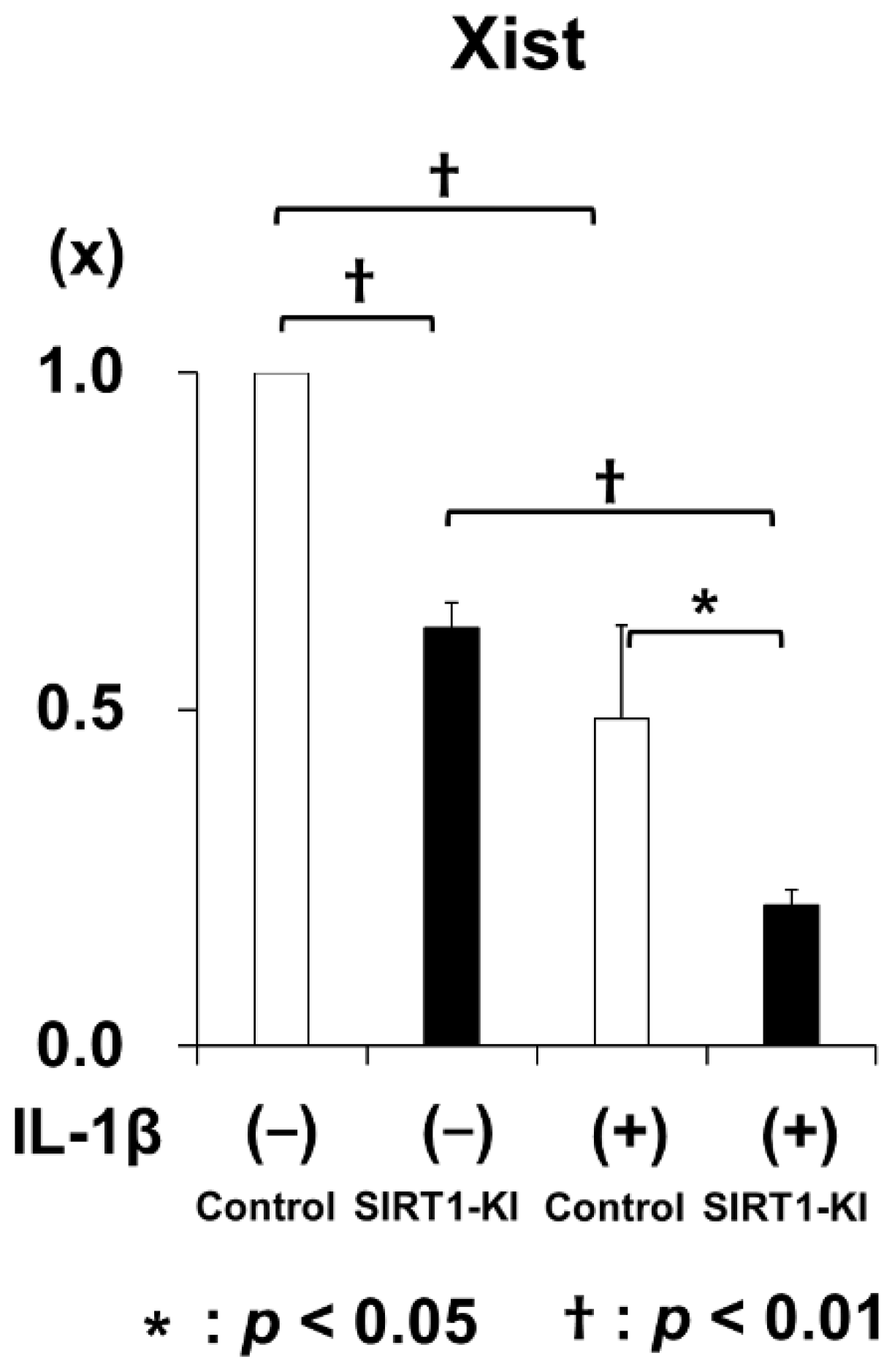
2.5. Microarray Analysis Identified 21 Genes Associated with SIRT1 Overexpression
3. Discussion
4. Materials and Methods
4.1. Mice
4.2. Genotyping
4.3. Skeletal Preparation and Body Weight Analysis
4.4. Sirt1 Expression in Control and SIRT1-KI Mice
4.5. OA Model
4.6. Cell Culture and Real-Time PCR Analysis
4.7. Histological Analysis
4.8. Immunohistochemistry
4.9. Microarray Analysis
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Felson, D.T.; Neogi, T. Osteoarthritis: Is It a Disease of Cartilage or of Bone? Arthritis Rheum. 2004, 50, 341–344. [Google Scholar] [CrossRef]
- Cai, X.; Yuan, S.; Zeng, Y.; Wang, C.; Yu, N.; Ding, C. New Trends in Pharmacological Treatments for Osteoarthritis. Front. Pharmacol. 2021, 12, 1–16. [Google Scholar] [CrossRef]
- Latourte, A.; Kloppenburg, M.; Richette, P. Emerging pharmaceutical therapies for osteoarthritis. Nat. Rev. Rheumatol. 2020, 16, 673–688. [Google Scholar] [CrossRef]
- Deng, Z.; Li, Y.; Liu, H.; Xiao, S.; Li, L.; Tian, J.; Cheng, C.; Zhang, G.; Zhang, F. The role of sirtuin 1 and its activator, resveratrol in osteoarthritis. Biosci. Rep. 2019, 39, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Hubbard, B.P.; Sinclair, D.A. Small molecule SIRT1 activators for the treatment of aging and age-related diseases. Trends Pharmacol. Sci. 2014, 35, 146–154. [Google Scholar] [CrossRef] [Green Version]
- Gagarina, V.; Gabay, O.; Dvir-Ginzberg, M.; Lee, E.J.; Brady, J.K.; Quon, M.J.; Hall, D.J. SirT1 enhances survival of human osteoarthritic chondrocytes by repressing protein tyrosine phosphatase 1B and activating the insulin-like growth factor receptor pathway. Arthritis Rheum. 2010, 62, 1383–1392. [Google Scholar] [CrossRef] [Green Version]
- Takayama, K.; Ishida, K.; Matsushita, T.; Fujita, N.; Hayashi, S.; Sasaki, K.; Tei, K.; Kubo, S.; Matsumoto, T.; Fujioka, H.; et al. SIRT1 regulation of apoptosis of human chondrocytes. Arthritis Rheum. 2009, 60, 2731–2740. [Google Scholar] [CrossRef] [PubMed]
- Dvir-Ginzberg, M.; Gagarina, V.; Lee, E.J.; Hall, D.J. Regulation of cartilage-specific gene expression in human chondrocytes by SirT1 and nicotinamide phosphoribosyltransferase. J. Biol. Chem. 2008, 283, 36300–36310. [Google Scholar] [CrossRef] [Green Version]
- Fujita, N.; Matsushita, T.; Ishida, K.; Kubo, S.; Matsumoto, T.; Takayama, K.; Kurosaka, M.; Kuroda, R. Potential involvement of SIRT1 in the pathogenesis of osteoarthritis through the modulation of chondrocyte gene expressions. J. Orthop. Res. 2011, 29, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Gabay, O.; Sanchez, C.; Dvir-Ginzberg, M.; Gagarina, V.; Zaal, K.J.; Song, Y.; He, X.H.; McBurney, M.W. Sirtuin 1 enzymatic activity is required for cartilage homeostasis in vivo in a mouse model. Arthritis Rheum. 2013, 65, 159–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gabay, O.; Oppenheimer, H.; Meir, H.; Zaal, K.; Sanchez, C.; Dvir-Ginzberg, M. Increased apoptotic chondrocytes in articular cartilage from adult heterozygous SirT1 mice. Ann. Rheum. Dis. 2012, 71, 613–616. [Google Scholar] [CrossRef]
- Matsuzaki, T.; Matsushita, T.; Takayama, K.; Matsumoto, T.; Nishida, K.; Kuroda, R.; Kurosaka, M. Disruption of Sirt1 in chondrocytes causes accelerated progression of osteoarthritis under mechanical stress and during ageing in mice. Ann. Rheum. Dis. 2014, 73, 1397–1404. [Google Scholar] [CrossRef]
- Villalba, J.M.; Alcaín, F.J. Sirtuin activators and inhibitors. BioFactors 2012, 38, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Nishida, K.; Matsushita, T.; Takayama, K.; Tanaka, T.; Miyaji, N.; Ibaraki, K.; Araki, D.; Kanzaki, N.; Matsumoto, T.; Kuroda, R. Intraperitoneal injection of the SIRT1 activator SRT1720 attenuates the progression of experimental osteoarthritis in mice. Bone Jt. Res. 2018, 7, 252–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miyaji, N.; Nishida, K.; Tanaka, T.; Araki, D.; Kanzaki, N.; Hoshino, Y.; Kuroda, R.; Matsushita, T. Inhibition of Knee Osteoarthritis Progression in Mice by Administering SRT2014, an Activator of Silent Information Regulator 2 Ortholog 1. Cartilage 2020, 1–11. [Google Scholar] [CrossRef]
- Bordone, L.; Cohen, D.; Robinson, A.; Motta, M.C.; Van Veen, E.; Czopik, A.; Steele, A.D.; Crowe, H.; Marmor, S.; Luo, J.; et al. SIRT1 transgenic mice show phenotypes resembling calorie restriction. Aging Cell 2007, 6, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Machin, D.R.; Auduong, Y.; Gogulamudi, V.R.; Liu, Y.; Islam, M.T.; Lesniewski, L.A.; Donato, A.J. Lifelong SIRT-1 overexpression attenuates large artery stiffening with advancing age. Aging 2020, 12, 11314–11324. [Google Scholar] [CrossRef] [PubMed]
- Long, G.Y.; Yang, J.Y.; Xu, J.J.; Ni, Y.H.; Zhou, X.L.; Ma, J.Y.; Fu, Y.C.; Luo, L.L. SIRT1 knock-in mice preserve ovarian reserve resembling caloric restriction. Gene 2019, 686, 194–202. [Google Scholar] [CrossRef]
- Pacholec, M.; Bleasdale, J.E.; Chrunyk, B.; Cunningham, D.; Flynn, D.; Garofalo, R.S.; Griffith, D.; Griffor, M.; Loulakis, P.; Pabst, B.; et al. SRT1720, SRT2183, SRT1460, and resveratrol are not direct activators of SIRT1. J. Biol. Chem. 2010, 285, 8340–8351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, J.; Nikolaev, A.Y.; Imai, S.I.; Chen, D.; Su, F.; Shiloh, A.; Guarente, L.; Gu, W. Negative control of p53 by Sir2α promotes cell survival under stress. Cell 2001, 107, 137–148. [Google Scholar] [CrossRef] [Green Version]
- Oppenheimer, H.; Gabay, O.; Meir, H.; Haze, A.; Kandel, L.; Liebergall, M.; Gagarina, V.; Lee, E.J.; Dvir-Ginzberg, M. 75-Kd Sirtuin 1 Blocks Tumor Necrosis Factor A-Mediated Apoptosis in Human Osteoarthritic Chondrocytes. Arthritis Rheum. 2012, 64, 718–728. [Google Scholar] [CrossRef]
- Bar Oz, M.; Kumar, A.; Elayyan, J.; Reich, E.; Binyamin, M.; Kandel, L.; Liebergall, M.; Steinmeyer, J.; Lefebvre, V.; Dvir-Ginzberg, M. Acetylation reduces SOX9 nuclear entry and ACAN gene transactivation in human chondrocytes. Aging Cell 2016, 15, 499–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oppenheimer, H.; Kumar, A.; Meir, H.; Schwartz, I.; Zini, A.; Haze, A.; Kandel, L.; Mattan, Y.; Liebergall, M.; Dvir-Ginzberg, M. Set7/9 impacts col2a1 expression through binding and repression of sirT1 histone deacetylation. J. Bone Miner. Res. 2014, 29, 348–360. [Google Scholar] [CrossRef]
- Yurube, T.; Takada, T.; Hirata, H.; Kakutani, K.; Maeno, K.; Zhang, Z.; Yamamoto, J.; Doita, M.; Kurosaka, M.; Nishida, K. Modified house-keeping gene expression in a rat tail compression loading-induced disc degeneration model. J. Orthop. Res. 2011, 29, 1284–1290. [Google Scholar] [CrossRef] [PubMed]
- Roman-Blas, J.A.; Jimenez, S.A. NF-κB as a potential therapeutic target in osteoarthritis and rheumatoid arthritis. Osteoarthr. Cartil. 2006, 14, 839–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saklatvala, J. Inflammatory Signaling in Cartilage: MAPK and NF-κ B Pathways in Chondrocytes and the Use of Inhibitors for Research into Pathogenesis and Therapy of Osteoarthritis. Curr. Drug Targets 2007, 8, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Goldring, M.B.; Marcu, K.B. Cartilage homeostasis in health and rheumatic diseases. Arthritis Res. Ther. 2009, 11, 224. [Google Scholar] [CrossRef] [Green Version]
- Grall, F.; Gu, X.; Tan, L.; Cho, J.Y.; Inan, M.S.; Pettit, A.R.; Thamrongsak, U.; Choy, B.K.; Manning, C.; Akbarali, Y.; et al. Responses to the proinflammatory cytokines interleukin-1 and tumor necrosis factor α in cells derived from rheumatoid synovium and other joint tissues involve nuclear factor κB-mediated induction of the Ets transcription factor ESE-1. Arthritis Rheum. 2003, 48, 1249–1260. [Google Scholar] [CrossRef]
- Yeung, F.; Hoberg, J.E.; Ramsey, C.S.; Keller, M.D.; Jones, D.R.; Frye, R.A.; Mayo, M.W. Modulation of NF-κB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J. 2004, 23, 2369–2380. [Google Scholar] [CrossRef] [Green Version]
- Matsushita, T.; Sasaki, H.; Takayama, K.; Ishida, K.; Matsumoto, T.; Kubo, S.; Matsuzaki, T.; Nishida, K.; Kurosaka, M.; Kuroda, R. The overexpression of SIRT1 inhibited osteoarthritic gene expression changes induced by interleukin-1β in human chondrocytes. J. Orthop. Res. 2013, 31, 531–537. [Google Scholar] [CrossRef]
- Elayyan, J.; Lee, E.J.; Gabay, O.; Smith, C.A.; Qiq, O.; Reich, E.; Mobasheri, A.; Henrotin, Y.; Kimber, S.J.; Dvir-Ginzberg, M. LEF1-mediated MMP13 gene expression is repressed by SIRT1 in human chondrocytes. FASEB J. 2017, 31, 3116–3125. [Google Scholar] [CrossRef] [Green Version]
- He, D.S.; Hu, X.J.; Yan, Y.Q.; Liu, H. Underlying mechanism of Sirt1 on apoptosis and extracellular matrix degradation of osteoarthritis chondrocytes. Mol. Med. Rep. 2017, 16, 845–850. [Google Scholar] [CrossRef] [Green Version]
- Park, S.Y.; Lee, S.W.; Lee, S.Y.; Hong, K.W.; Bae, S.S.; Kim, K.; Kim, C.D. SIRT1/Adenosine monophosphate-activated protein Kinase α signaling enhances macrophage polarization to an anti-inflammatory phenotype in rheumatoid arthritis. Front. Immunol. 2017, 8, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.K.; Yu, X.H.; Yang, W.; Wang, C.; He, W.S.; Yan, Y.G.; Zhang, J.; Wang, W.J. lncRNAs: Novel players in intervertebral disc degeneration and osteoarthritis. Cell Prolif. 2017, 50, 1–12. [Google Scholar] [CrossRef]
- Díaz-Prado, S.; Cicione, C.; Muiños-López, E.; Hermida-Gómez, T.; Oreiro, N.; Fernández-López, C.; Blanco, F.J. Characterization of microRNA expression profiles in normal and osteoarthritic human chondrocytes. BMC Musculoskelet. Disord. 2012, 13, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Lv, G.; Wang, B.; Kuang, L. XIST/miR-376c-5p/OPN axis modulates the influence of proinflammatory M1 macrophages on osteoarthritis chondrocyte apoptosis. J. Cell. Physiol. 2020, 235, 281–293. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, K.; Tang, C.; Shi, Z.; Jing, K.; Zheng, J. Long non-coding RNA XIST contributes to osteoarthritis progression via miR-149-5p/DNMT3A axis. Biomed. Pharmacother. 2020, 128, 110349. [Google Scholar] [CrossRef] [PubMed]
- Glasson, S.S.; Blanchet, T.J.; Morris, E.A. The surgical destabilization of the medial meniscus (DMM) model of osteoarthritis in the 129/SvEv mouse. Osteoarthr. Cartil. 2007, 15, 1061–1069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pritzker, K.P.H.; Gay, S.; Jimenez, S.A.; Ostergaard, K.; Pelletier, J.P.; Revell, K.; Salter, D.; van den Berg, W.B. Osteoarthritis cartilage histopathology: Grading and staging. Osteoarthr. Cartil. 2006, 14, 13–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| No. | Genes | Log Ratio |
|---|---|---|
| 1 | Sirt1 | 3.484823 |
| 2 | Acta2 | 2.169581 |
| 3 | Aspn | 1.389573 |
| 4 | Postn | 1.343505 |
| 5 | Actg2 | 1.302517 |
| 6 | Ccdc3 | 1.214218 |
| 7 | Myl9 | 1.189704 |
| 8 | Tagln | 1.168344 |
| 9 | Sfrp2 | 1.061471 |
| 10 | Pi15 | 1.019975 |
| 11 | Cfh | 1.001788 |
| 12 | Gm24405 | −1.001405 |
| 13 | Gm23604 | −1.026104 |
| 14 | Chil1 | −1.117696 |
| 15 | Serpina3c | −1.196805 |
| 16 | Gm11979 | −1.22567 |
| 17 | Mrpl32 | −1.343651 |
| 18 | Xist | −1.368057 |
| 19 | Gm24445 | −1.382748 |
| 20 | Gm23335 | −1.61242 |
| 21 | Snora69 | −1.69543 |
| Gene | Assay ID |
|---|---|
| Gapdh | Mm99999915_g1 |
| Sirt1 | Mm01168521_m1 |
| Col2a1 | Mm01309565_m1 |
| Col10a1 | Mm00487041_m1 |
| Mmp-3 | Mm00440295_m1 |
| Mmp-13 | Mm00439491_m1 |
| Acan | Mm00545807_m1 |
| Adamts-5 | Mm00478620_m1 |
| Xist | Mm01232884_m1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, T.; Miyaji, N.; Kataoka, K.; Nishida, K.; Nagai, K.; Kanzaki, N.; Hoshino, Y.; Kuroda, R.; Matsushita, T. Knee Osteoarthritis Progression Is Delayed in Silent Information Regulator 2 Ortholog 1 Knock-in Mice. Int. J. Mol. Sci. 2021, 22, 10685. https://doi.org/10.3390/ijms221910685
Yamamoto T, Miyaji N, Kataoka K, Nishida K, Nagai K, Kanzaki N, Hoshino Y, Kuroda R, Matsushita T. Knee Osteoarthritis Progression Is Delayed in Silent Information Regulator 2 Ortholog 1 Knock-in Mice. International Journal of Molecular Sciences. 2021; 22(19):10685. https://doi.org/10.3390/ijms221910685
Chicago/Turabian StyleYamamoto, Tetsuya, Nobuaki Miyaji, Kiminari Kataoka, Kyohei Nishida, Kanto Nagai, Noriyuki Kanzaki, Yuichi Hoshino, Ryosuke Kuroda, and Takehiko Matsushita. 2021. "Knee Osteoarthritis Progression Is Delayed in Silent Information Regulator 2 Ortholog 1 Knock-in Mice" International Journal of Molecular Sciences 22, no. 19: 10685. https://doi.org/10.3390/ijms221910685






