Bone Marrow Failure Syndromes, Overlapping Diseases with a Common Cytokine Signature
Abstract
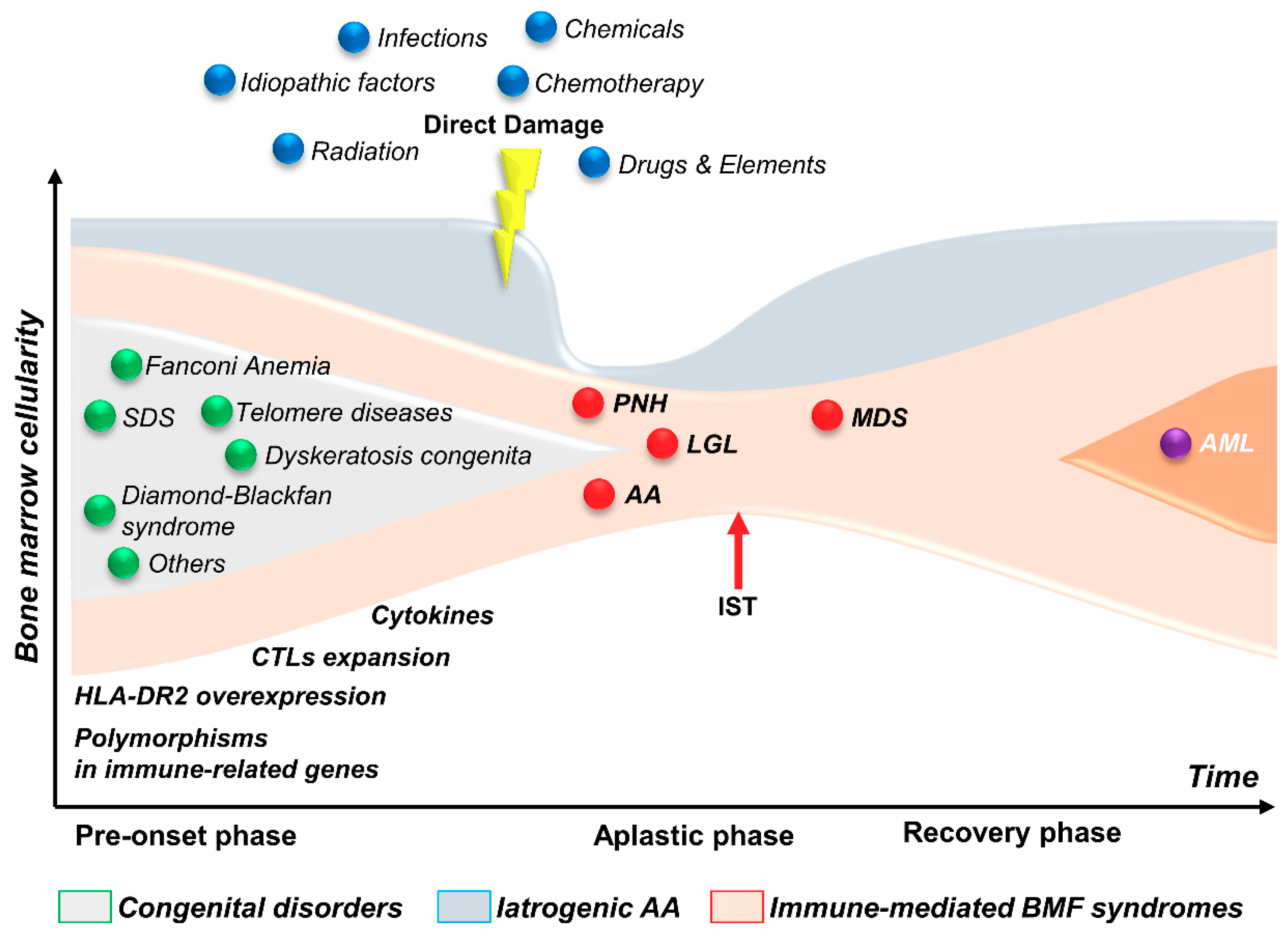
:1. Introduction
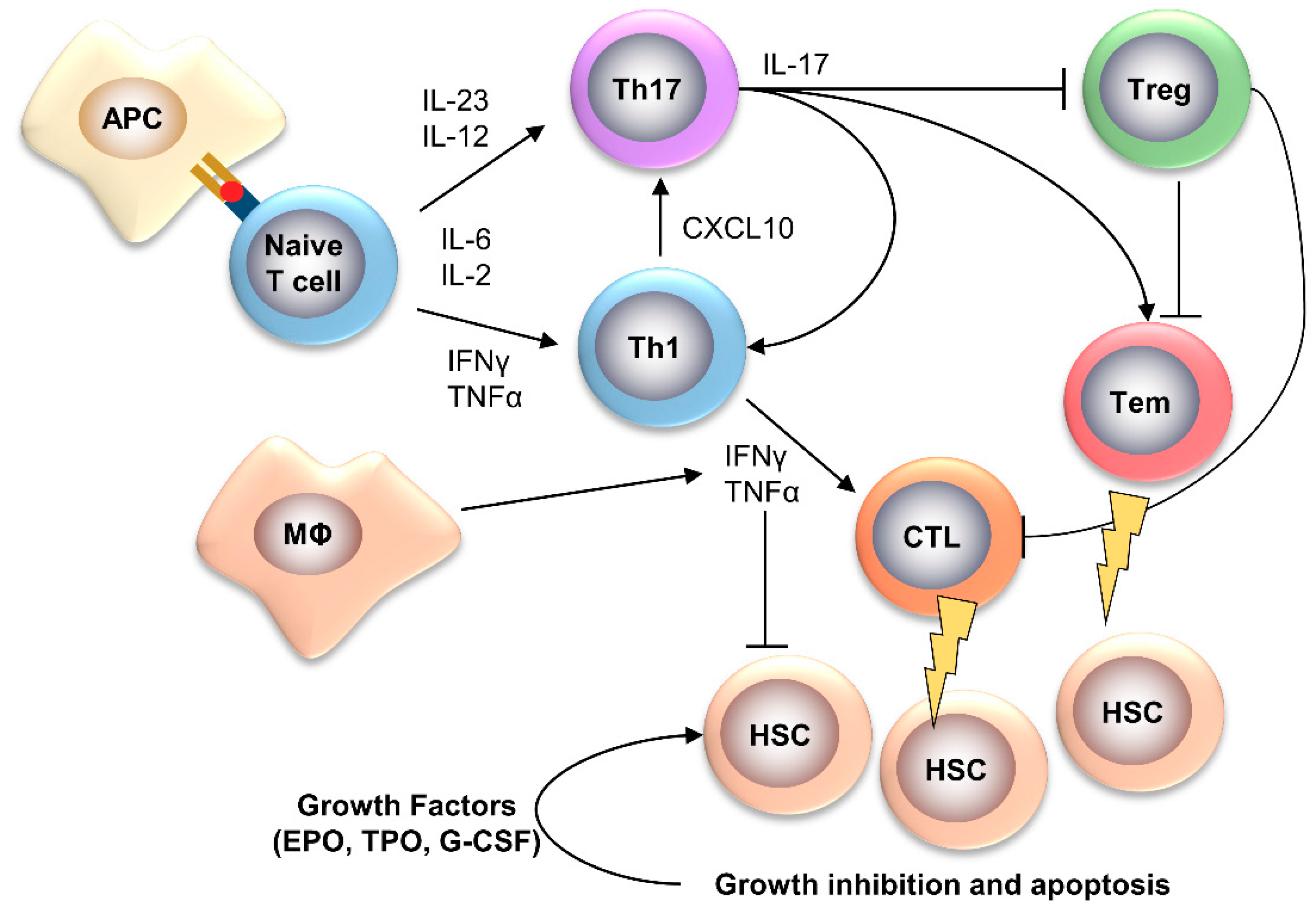
2. Acquired Aplastic Anemia
2.1. Th1 Cytokines
2.2. Th17 Cytokines
2.3. Growth Factors
2.4. BM Environment
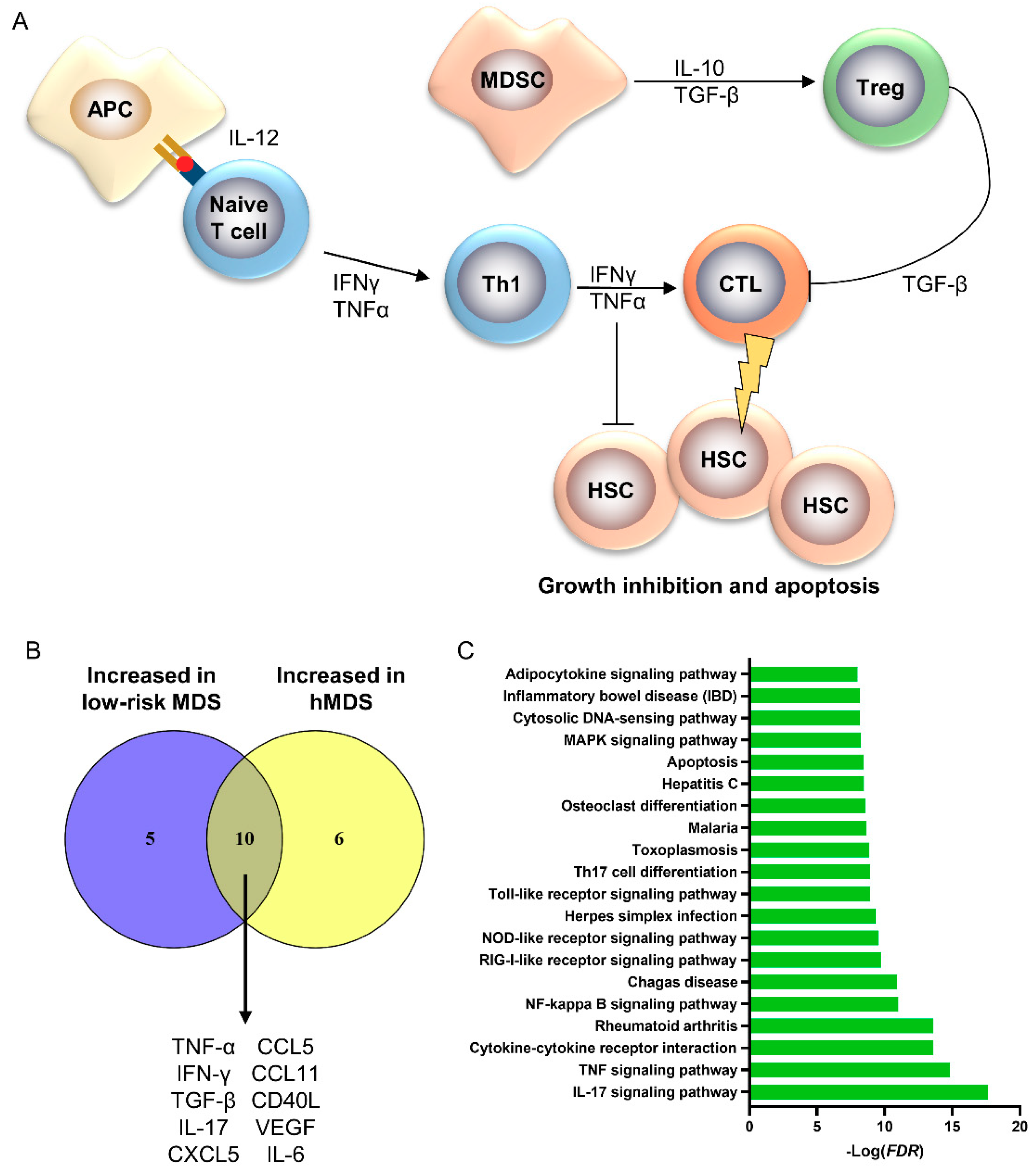
3. hMDS
4. Large Granular Lymphocyte Leukemia
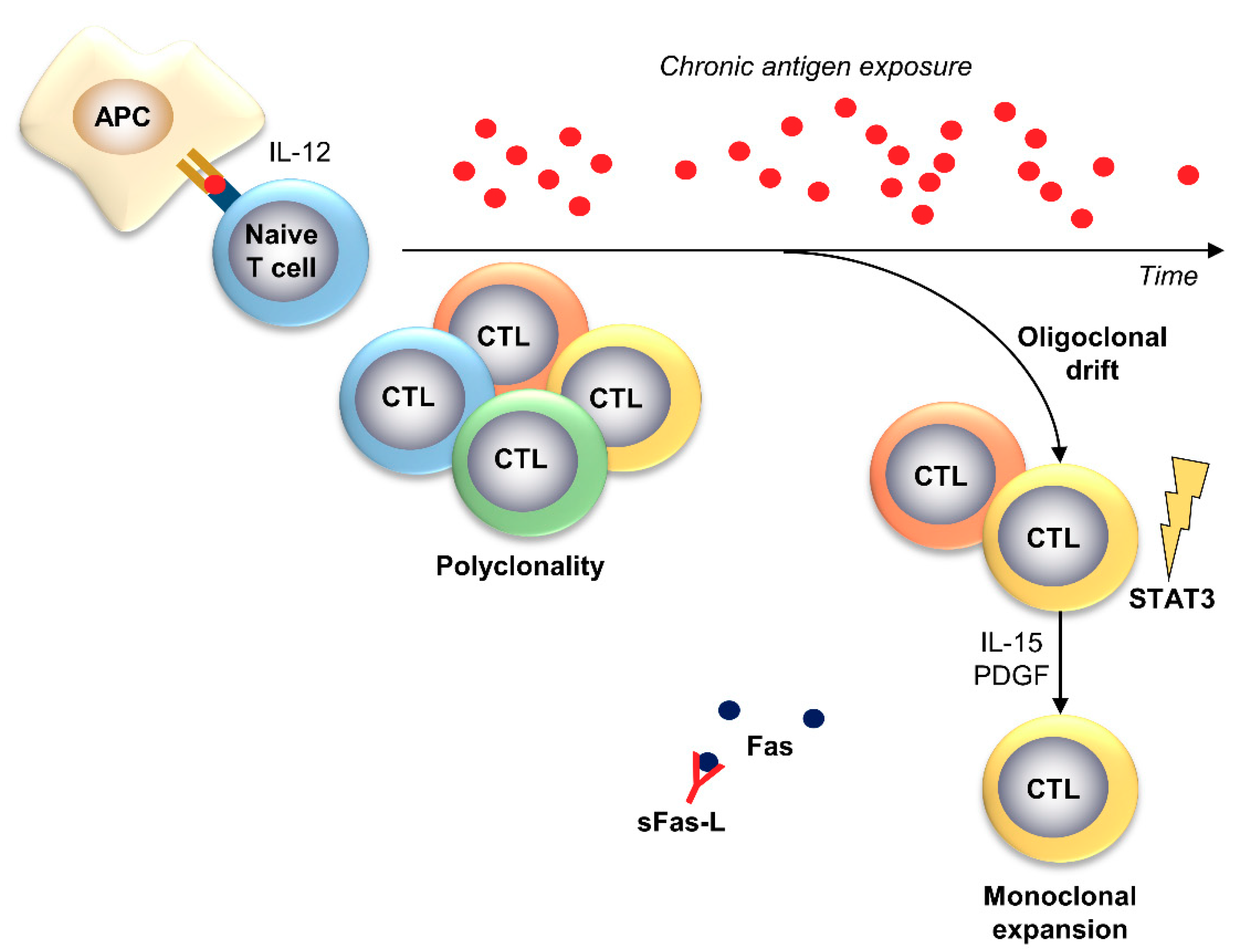
5. Paroxysmal Nocturnal Hemoglobinuria
6. Inherited BMF Syndromes
6.1. Fanconi Anemia
6.2. Diamond–Blackfan Anemia
6.3. Dyskeratosis Congenita
7. Therapy-Related MDS
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rodgers, G.P.; Young, N.S. The Bethesda Handbook of Clinical Hematology (English Edition), 4th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Young, N.S. Aplastic Anemia. N. Engl. J. Med. 2018, 379, 1643–1656. [Google Scholar] [CrossRef] [PubMed]
- Young, N.S.; Calado, R.T.; Scheinberg, P. Current concepts in the pathophysiology and treatment of aplastic anemia. Blood 2006, 108, 2509–2519. [Google Scholar] [CrossRef] [PubMed]
- Young, N.S. Current concepts in the pathophysiology and treatment of aplastic anemia. Hematol. Am. Soc. Hematol. Educ. Program. 2013, 2013, 76–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, M.; Park, C.J.; Cho, Y.W.; Jang, S.; Lee, J.H.; Lee, J.H.; Lee, K.H.; Lee, Y.H. Alterations in the bone marrow microenvironment may elicit defective hematopoiesis: A comparison of aplastic anemia, chronic myeloid leukemia, and normal bone marrow. Exp. Hematol. 2017, 45, 56–63. [Google Scholar] [CrossRef]
- Sloand, E.; Kim, S.; Maciejewski, J.P.; Tisdale, J.; Follmann, D.; Young, N.S. Intracellular interferon-gamma in circulating and marrow T cells detected by flow cytometry and the response to immunosuppressive therapy in patients with aplastic anemia. Blood 2002, 100, 1185–1191. [Google Scholar] [CrossRef] [Green Version]
- Maciejewski, J.P.; Selleri, C.; Anderson, S.; Young, N.S. Fas antigen expression on CD34+ human marrow cells is induced by interferon-gamma and tumor necrosis factor-alpha and potentiates cytokine-mediated hematopoietic suppression in vitro. Blood 1995, 85, 3183–3190. [Google Scholar] [CrossRef]
- Selleri, C.; Maciejewski, J.P.; Sato, T.; Young, N.S. Interferon-γ constitutively expressed in the stromal microenviroment of human marrow cultures mediates potent hematopoietic inhibition. Blood 1996, 87, 4149–4157. [Google Scholar] [CrossRef] [Green Version]
- Giudice, V.; Feng, X.; Lin, Z.; Hu, W.; Zhang, F.; Qiao, W.; Ibanez, M.; Rios, O.; Young, N.S. Deep sequencing and flow cytometric characterization of expanded effector memory CD8+CD57+ T cells frequently reveals T-cell receptor Vβ oligoclonality and CDR3 homology in acquired aplastic anemia. Haematologica 2018, 103, 759–769. [Google Scholar] [CrossRef] [Green Version]
- Risitano, A.M.; Maciejewski, J.P.; Green, S.; Plasilova, M.; Zeng, W.; Young, N.S. In-vivo dominant immune responses in aplastic anaemia: Molecular tracking of putatively pathogenetic T-cell clones by TCR beta-CDR3 sequencing. Lancet 2004, 364, 355–364. [Google Scholar] [CrossRef]
- Risitano, A.M.; Kook, H.; Zeng, W.; Chen, G.; Young, N.S.; Maciejewski, J.P. Oligoclonal and polyclonal CD4 and CD8 lymphocytes in aplastic anemia and paroxysmal nocturnal hemoglobinuria measured by V beta CDR3 spectratyping and flow cytometry. Blood 2002, 100, 178–183. [Google Scholar] [CrossRef] [Green Version]
- De Latour, R.P.; Visconte, V.; Takaku, T.; Wu, C.; Erie, A.J.; Sarcon, A.K.; Desierto, M.J.; Scheinberg, P.; Keyvanfar, K.; Nunez, O.; et al. Th17 immune responses contribute to the pathophysiology of aplastic anemia. Blood 2010, 116, 4175–4184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.; Liu, H. Pathogenesis of aplastic anemia. Hematology 2019, 24, 559–566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, Y.; Zhang, J.; Peng, J.; Hu, X.; Xu, C. Elevated expression of IL-12 and IL-23 in patients with aplastic anemia. Int. J. Lab. Hematol. 2009, 31, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Ghilardi, N.; Kljavin, N.; Chen, Q.; Lucas, S.; Gurney, A.L.; De Sauvage, F.J. Compromised humoral and delayed type hypersensitivity responses in IL-23-deficient mice. J. Immunol. 2004, 172, 2827–2833. [Google Scholar] [CrossRef] [Green Version]
- Oppmann, B.; Lesley, R.; Blom, B.; Timans, J.C.; Xu, Y.; Hunte, B.; Vega, F.; Yu, N.; Wang, J.; Singh, K.; et al. Novel p19 protein engages IL-12p40 to form a cytokine, IL-23, with biological activities similar as well as distinct from IL-12. Immunity 2000, 13, 715–725. [Google Scholar] [CrossRef] [Green Version]
- Hoeve, M.A.; Savage, N.D.; de Boer, T.; Langenberg, D.M.; de Waal Malefyt, R.; Ottenhoff, T.H.; Verreck, F.A. Divergent effects of IL-12 and IL-23 on the production of IL-17 by human T cells. Eur. J. Immunol. 2006, 36, 661–670. [Google Scholar] [CrossRef]
- Parham, C.; Chirica, M.; Timans, J.; Vaisberg, E.; Travis, M.; Cheung, J.; Pflanz, S.; Zhang, R.; Singh, K.P.; Vega, F.; et al. A receptor for the heterodimeric cytokine IL-23 is composed of IL-12Rbeta1 and a novel cytokine receptor subunit, IL-23R. J. Immunol. 2002, 168, 5699–5708. [Google Scholar] [CrossRef] [Green Version]
- Okamura, H.; Tsutsi, H.; Komatsu, T.; Yutsudo, M.; Hakura, A.; Tanimoto, T.; Torigoe, K.; Okura, T.; Nukada, Y.; Hattori, K.; et al. Cloning of a new cytokine that induces IFN-gamma production by T cells. Nature 1995, 378, 88–91. [Google Scholar] [CrossRef]
- Fehniger, T.A.; Shah, M.H.; Turner, M.J.; VanDeusen, J.B.; Whitman, S.P.; Cooper, M.A.; Suzuki, K.; Wechser, M.; Goodsaid, F.; Caligiuri, M.A. Differential cytokine and chemokine gene expression by human NK cells following activation with IL-18 or IL-15 in combination with IL-12: Implications for the innate immune response. J. Immunol. 1999, 162, 4511–4520. [Google Scholar]
- Dinarello, C.A.; Novick, D.; Kim, S.; Kaplanski, G. Interleukin-18 and IL-18 binding protein. Front. Immunol. 2013, 4, 289. [Google Scholar] [CrossRef] [Green Version]
- Novick, D.; Kim, S.H.; Fantuzzi, G.; Reznikov, L.L.; Dinarello, C.A.; Rubinstein, M. Interleukin-18 binding protein: A novel modulator of the Th1 cytokine response. Immunity 1999, 10, 127–136. [Google Scholar] [CrossRef] [Green Version]
- Wu, Z.; Giudice, V.; Chen, J.; Sun, W.; Lin, Z.; Keyvanfar, K.; Talasani, N.; Kajigaya, S.; Feng, X.; Young, N.S. Interleukin-18 plays a dispensable role in murine and likely also human bone marrow failure. Exp. Hematol. 2019, 69, 54–64.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De, R.; Dutta, A.; Dolai, T.K.; Ghosh, K.; Halder, A. Comparative study of bone marrow and blood plasma levels of IL-2 in aplastic anaemia and their relationship with disease severity. Hematology 2019, 24, 84–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubey, S.; Shukla, P.; Nityanand, S. Expression of interferon-gamma and tumor necrosis factor-alpha in bone marrow T cells and their levels in bone marrow plasma in patients with aplastic anemia. Ann. Hematol. 2005, 84, 572–577. [Google Scholar] [CrossRef]
- Feng, X.; Scheinberg, P.; Wu, C.O.; Samsel, L.; Nunez, O.; Prince, C.; Ganetzky, R.D.; McCoy, J.P., Jr.; Maciejewski, J.P.; Young, N.S. Cytokine signature profiles in acquired aplastic anemia and myelodysplastic syndromes. Haematologica 2011, 96, 602–606. [Google Scholar] [CrossRef] [Green Version]
- Selleri, C.; Sato, T.; Anderson, S.; Young, N.S.; Maciejewski, J.P. Interferon-gamma and tumor necrosis factor-alpha suppress both early and late stages of hematopoiesis and induce programmed cell death. J. Cell Physiol. 1995, 165, 538–546. [Google Scholar] [CrossRef]
- de Bruin, A.M.; Voermans, C.; Nolte, M.A. Impact of interferon-γ on hematopoiesis. Blood 2014, 124, 2479–2486. [Google Scholar] [CrossRef] [Green Version]
- Morales-Mantilla, D.E.; King, K.Y. The Role of Interferon-Gamma in Hematopoietic Stem Cell Development, Homeostasis, and Disease. Curr. Stem Cell. Rep. 2018, 4, 264–271. [Google Scholar] [CrossRef] [Green Version]
- Maciejewski, J.P.; Selleri, C.; Sato, T.; Cho, H.J.; Keefer, L.K.; Nathan, C.F.; Young, N.S. Nitric oxide suppression of human hematopoiesis in vitro. Contribution to inhibitory action of interferon-gamma and tumor necrosis factor-alpha. J. Clin. Investig. 1995, 96, 1085–1092. [Google Scholar] [CrossRef] [Green Version]
- Mullarky, I.K.; Szaba, F.M.; Kummer, L.W.; Wilhelm, L.B.; Parent, M.A.; Johnson, L.L.; Smiley, S.T. Gamma interferon suppresses erythropoiesis via interleukin-15. Infect. Immun. 2007, 75, 2630–2633. [Google Scholar] [CrossRef] [Green Version]
- Ho, C.H.; You, J.Y.; Chau, W.K.; Hsu, H.C.; Gau, J.P.; Chen, C.C.; Yu, T.J. Diagnostic value of serum transferrin receptor and glycosylated hemoglobin on hemolytic anemia. Ann. Hematol. 2003, 82, 228–230. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Wu, Z.; Lin, Z.; Hollinger, M.; Chen, J.; Feng, X.; Young, N.S. Macrophage TNF-α licenses donor T cells in murine bone marrow failure and can be implicated in human aplastic anemia. Blood 2018, 132, 2730–2743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dufour, C.; Ferretti, E.; Bagnasco, F.; Burlando, O.; Lanciotti, M.; Ramenghi, U.; Saracco, P.; Van Lint, M.T.; Longoni, D.; Torelli, G.F.; et al. Changes in cytokine profile pre- and post-immunosuppression in acquired aplastic anemia. Haematologica 2009, 94, 1743–1747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hara, T.; Ando, K.; Tsurumi, H.; Moriwaki, H. Excessive production of tumor necrosis factor-alpha by bone marrow T lymphocytes is essential in causing bone marrow failure in patients with aplastic anemia. Eur. J. Haematol. 2004, 73, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Ge, M.; Lu, S.; Shi, J.; Li, X.; Wang, M.; Huang, J.; Shao, Y.; Huang, Z.; Zhang, J.; et al. Pro-inflammatory effects of the Th1 chemokine CXCL10 in acquired aplastic anaemia. Cytokine 2017, 94, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Niu, Q.; Zhou, Q.; Liu, Y.; Jiang, H. Expression of CXCR4 on T-cell subsets and Plasma IL-17 Concentrations in Patients with Aplastic Anaemia. Sci. Rep. 2017, 7, 9075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Wu, Q.; Shi, J.; Ge, M.; Li, X.; Shao, Y.; Yao, J.; Zheng, Y. Involvement of interleukin-21 in the pathophysiology of aplastic anemia. Eur. J. Haematol. 2015, 95, 44–51. [Google Scholar] [CrossRef]
- Ge, M.; Zheng, Y.; Li, X.; Lu, S.; Li, H.; Chen, F.; Chen, D.; Shao, Y.; Shi, J.; Feng, S. Differential expression profile of Th1/Th17/Th2-related chemokines and their receptors in patients with acquired bone marrow failure syndromes. Hum. Immunol. 2013, 74, 176–180. [Google Scholar] [CrossRef]
- Yu, W.; Ge, M.; Lu, S.; Shi, J.; Li, X.; Zhang, J.; Wang, M.; Huang, J.; Shao, Y.; Huang, Z.; et al. Anti-inflammatory effects of interleukin-35 in acquired aplastic anemia. Cytokine 2015, 76, 409–416. [Google Scholar] [CrossRef]
- Niedbala, W.; Wei, X.Q.; Cai, B.; Hueber, A.J.; Leung, B.P.; McInnes, I.B.; Liew, F.Y. IL-35 is a novel cytokine with therapeutic effects against collagen-induced arthritis through the expansion of regulatory T cells and suppression of Th17 cells. Eur. J. Immunol. 2007, 37, 3021–3029. [Google Scholar] [CrossRef]
- Collison, L.W.; Chaturvedi, V.; Henderson, A.L.; Giacomin, P.R.; Guy, C.; Bankoti, J.; Finkelstein, D.; Forbes, K.; Workman, C.J.; Brown, S.A.; et al. IL-35-mediated induction of a potent regulatory T cell population. Nat. Immunol. 2010, 11, 1093–1101. [Google Scholar] [CrossRef] [Green Version]
- Wang, R.X.; Yu, C.R.; Dambuza, I.M.; Mahdi, R.M.; Dolinska, M.B.; Sergeev, Y.V.; Wingfield, P.T.; Kim, S.H.; Egwuagu, C.E. Interleukin-35 induces regulatory B cells that suppress autoimmune disease. Nat. Med. 2014, 20, 633–641. [Google Scholar] [CrossRef]
- Huang, Z.; Tong, H.; Li, Y.; Zhou, H.; Qian, J.; Wang, J.; Ruan, J. Post-therapeutic recovery of serum interleukin-35 level might predict positive response to immunosuppressive therapy in pediatric aplastic anemia. Hematology 2017, 22, 430–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, X.; Feng, X.; Wu, Z.; Winkler, T.; Desmond, R.; Olnes, M.; Dumitriu, B.; Townsley, D.M.; Dunbar, C.E.; Young, N.S. Persistent elevation of plasma thrombopoietin levels after treatment in severe aplastic anemia. Exp. Hematol. 2018, 58, 39–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fielder, P.J.; Gurney, A.L.; Stefanich, E.; Marian, M.; Moore, M.W.; Carver-Moore, K.; de Sauvage, F.J. Regulation of thrombopoietin levels by c-mpl-mediated binding to platelets. Blood 1996, 87, 2154–2161. [Google Scholar] [CrossRef] [Green Version]
- Qian, H.; Buza-Vidas, N.; Hyland, C.D.; Jensen, C.T.; Antonchuk, J.; Månsson, R.; Thoren, L.A.; Ekblom, M.; Alexander, W.S.; Jacobsen, S.E. Critical role of thrombopoietin in maintaining adult quiescent hematopoietic stem cells. Cell Stem Cell 2007, 1, 671–684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarado, L.J.; Huntsman, H.D.; Cheng, H.; Townsley, D.M.; Winkler, T.; Feng, X.; Dunbar, C.E.; Young, N.S.; Larochelle, A. Eltrombopag maintains human hematopoietic stem and progenitor cells under inflammatory conditions mediated by IFN-γ. Blood 2019, 133, 2043–2055. [Google Scholar] [CrossRef]
- Giudice, V.; Biancotto, A.; Wu, Z.; Cheung, F.; Candia, J.; Fantoni, G.; Kajigaya, S.; Rios, O.; Townsley, D.; Feng, X.; et al. Aptamer-based proteomics of serum and plasma in acquired aplastic anemia. Exp. Hematol. 2018, 68, 38–50. [Google Scholar] [CrossRef]
- Shao, Y.; Wang, H.; Liu, C.; Cao, Q.; Fu, R.; Wang, H.; Wang, T.; Qi, W.; Shao, Z. Transforming growth factor 15 increased in severe aplastic anemia patients. Hematology 2017, 22, 548–553. [Google Scholar] [CrossRef] [Green Version]
- Wenxin, L.; Jinxiang, F.; Yong, W.; Wenxiang, L.; Wenbiao, S.; Xueguang, Z. Expression of membrane-bound IL-15 by bone marrow fibroblast-like stromal cells in aplastic anemia. Int. Immunol. 2005, 17, 429–437. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Lu, S.; Yang, S.; Xing, W.; Feng, J.; Li, W.; Zhao, Q.; Wu, H.; Ge, M.; Ma, F.; et al. Impaired immunomodulatory ability of bone marrow mesenchymal stem cells on CD4(+) T cells in aplastic anemia. Results Immunol. 2012, 2, 142–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzaga, V.F.; Wenceslau, C.V.; Lisboa, G.S.; Frare, E.O.; Kerkis, I. Mesenchymal Stem Cell Benefits Observed in Bone Marrow Failure and Acquired Aplastic Anemia. Stem Cells Int. 2017, 2017, 8076529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shallis, R.M.; Ahmad, R.; Zeidan, A.M. Aplastic anemia: Etiology, molecular pathogenesis, and emerging concepts. Eur. J. Haematol. 2018, 101, 711–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, B.; Shao, Y.; Liu, Z.; Liu, C.; Zhang, T.; Fu, R. Bone Marrow Plasma Cytokine Signature Profiles in Severe Aplastic Anemia. Biomed. Res. Int. 2020, 2020, 8789275. [Google Scholar] [CrossRef] [Green Version]
- Medinger, M.; Drexler, B.; Lengerke, C.; Passweg, J. Pathogenesis of Acquired Aplastic Anemia and the Role of the Bone Marrow Microenvironment. Front. Oncol. 2018, 8, 587. [Google Scholar] [CrossRef] [Green Version]
- Huo, J.; Zhang, L.; Ren, X.; Li, C.; Li, X.; Dong, P.; Zheng, X.; Huang, J.; Shao, Y.; Ge, M.; et al. Multifaceted characterization of the signatures and efficacy of mesenchymal stem/stromal cells in acquired aplastic anemia. Stem Cell Res. Ther. 2020, 11, 59. [Google Scholar] [CrossRef] [Green Version]
- Shipounova, I.N.; Petrova, T.V.; Svinareva, D.A.; Momotuk, K.S.; Mikhailova, E.A.; Drize, N.I. Alterations in hematopoietic microenvironment in patients with aplastic anemia. Clin. Transl. Sci. 2009, 2, 67–74. [Google Scholar] [CrossRef] [Green Version]
- DeZern, A.E.; Sekeres, M.A. The challenging world of cytopenias: Distinguishing myelodysplastic syndromes from other disorders of marrow failure. Oncologist 2014, 19, 735–745. [Google Scholar] [CrossRef] [Green Version]
- Huang, T.C.; Ko, B.S.; Tang, J.L.; Hsu, C.; Chen, C.Y.; Tsay, W.; Huang, S.Y.; Yao, M.; Chen, Y.C.; Shen, M.C.; et al. Comparison of hypoplastic myelodysplastic syndrome (MDS) with normo-/hypercellular MDS by International Prognostic Scoring System, cytogenetic and genetic studies. Leukemia 2008, 22, 544–550. [Google Scholar] [CrossRef] [Green Version]
- Serio, B.; Risitano, A.; Giudice, V.; Montuori, N.; Selleri, C. Immunological derangement in hypocellular myelodysplastic syndromes. Transl. Med. UniSa 2014, 8, 31–42. [Google Scholar]
- Bono, E.; McLornan, D.; Travaglino, E.; Gandhi, S.; Gallì, A.; Khan, A.A.; Kulasekararaj, A.G.; Boveri, E.; Raj, K.; Elena, C.; et al. Clinical, histopathological and molecular characterization of hypoplastic myelodysplastic syndrome. Leukemia 2019, 33, 2495–2505. [Google Scholar] [CrossRef] [PubMed]
- Maciejewski, J.P.; O’Keefe, C.; Gondek, L.; Tiu, R. Immune-mediated bone marrow failure syndromes of progenitor and stem cells: Molecular analysis of cytotoxic T cell clones. Folia Histochem. Cytobiol. 2007, 45, 5–14. [Google Scholar] [PubMed]
- Wlodarski, M.W.; Gondek, L.P.; Nearman, Z.P.; Plasilova, M.; Kalaycio, M.; His, E.D.; Maciejewski, J.P. Molecular strategies for detection and quantitation of clonal cytotoxic T-cell responses in aplastic anemia and myelodysplastic syndrome. Blood 2006, 108, 2632–2641. [Google Scholar] [CrossRef] [PubMed]
- Kochenderfer, J.N.; Kobayashi, S.; Wieder, E.D.; Su, C.; Molldrem, J.J. Loss of T-lymphocyte clonal dominance in patients with myelodysplastic syndrome responsive to immunosuppression. Blood 2002, 100, 3639–3645. [Google Scholar] [CrossRef] [Green Version]
- Barrett, A.J.; Sloand, E. Autoimmune mechanisms in the pathophysiology of myelodysplastic syndromes and their clinical relevance. Haematologica 2009, 94, 449–451. [Google Scholar] [CrossRef]
- Sloand, E.M.; Pfannes, L.; Chen, G.; Shah, S.; Solomou, E.E.; Barrett, J.; Young, N.S. CD34 cells from patients with trisomy 8 myelodysplastic syndrome (MDS) express early apoptotic markers but avoid programmed cell death by up-regulation of antiapoptotic proteins. Blood 2007, 109, 2399–2405. [Google Scholar] [CrossRef] [Green Version]
- Sloand, E.M.; Mainwaring, L.; Fuhrer, M.; Ramkissoon, S.; Risitano, A.M.; Keyvanafar, K.; Lu, J.; Basu, A.; Barrett, A.J.; Young, N.S. Preferential suppression of trisomy 8 compared with normal hematopoietic cell growth by autologous lymphocytes in patients with trisomy 8 myelodysplastic syndrome. Blood 2005, 106, 841–851. [Google Scholar] [CrossRef]
- Sloand, E.M.; Kim, S.; Fuhrer, M.; Risitano, A.M.; Nakamura, R.; Maciejewski, J.P.; Barrett, A.J.; Young, N.S. Fas-mediated apoptosis is important in regulating cell replication and death in trisomy 8 hematopoietic cells but not in cells with other cytogenetic abnormalities. Blood 2002, 100, 4427–4432. [Google Scholar] [CrossRef]
- Shao, L.L.; Zhang, L.; Hou, Y.; Yu, S.; Liu, X.G.; Huang, X.Y.; Sun, Y.X.; Tian, T.; He, N.; Ma, D.X.; et al. Th22 cells as well as Th17 cells expand differentially in patients with early-stage and late-stage myelodysplastic syndrome. PLoS ONE 2012, 7, e51339. [Google Scholar] [CrossRef]
- Fozza, C.; Longinotti, M. The role of T-cells in the pathogenesis of myelodysplastic syndromes: Passengers and drivers. Leuk. Res. 2013, 37, 201–203. [Google Scholar] [CrossRef]
- Ghiringhelli, F.; Ménard, C.; Terme, M.; Flament, C.; Taieb, J.; Chaput, N.; Puig, P.E.; Novault, S.; Escudier, B.; Vivier, E.; et al. CD4+CD25+ regulatory T cells inhibit natural killer cell functions in a transforming growth factor-beta-dependent manner. J. Exp. Med. 2005, 202, 1075–1085. [Google Scholar] [CrossRef] [PubMed]
- Ralainirina, N.; Poli, A.; Michel, T.; Poos, L.; Andrès, E.; Hentges, F.; Zimmer, J. Control of NK cell functions by CD4+CD25+ regulatory T cells. J. Leukoc. Biol. 2007, 81, 144–153. [Google Scholar] [CrossRef] [Green Version]
- Bontkes, H.J.; Ruben, J.M.; Alhan, C.; Westers, T.M.; Ossenkoppele, G.J.; van de Loosdrecht, A.A. Azacitidine differentially affects CD4(pos) T-cell polarization in vitro and in vivo in high risk myelodysplastic syndromes. Leuk Res. 2012, 36, 921–930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mailloux, A.W.; Sugimori, C.; Komrokji, R.S.; Yang, L.; Maciejewski, J.P.; Sekeres, M.A.; Paquette, R.; Loughran, T.P., Jr.; List, A.F.; Epling-Burnette, P.K. Expansion of effector memory regulatory T cells represents a novel prognostic factor in lower risk myelodysplastic syndrome. J. Immunol. 2012, 189, 3198–3208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allampallam, K.; Shetty, V.T.; Raza, A. Cytokines and MDS. Cancer Treat. Res. 2001, 108, 93–100. [Google Scholar]
- Kitagawa, M.; Saito, I.; Kuwata, T.; Yoshida, S.; Yamaguchi, S.; Takahashi, M.; Tanizawa, T.; Kamiyama, R.; Hirokawa, K. Overexpression of tumor necrosis factor (TNF)-alpha and interferon (IFN)-gamma by bone marrow cells from patients with myelodysplastic syndromes. Leukemia 1997, 11, 2049–2054. [Google Scholar] [CrossRef] [Green Version]
- Stifter, G.; Heiss, S.; Gastl, G.; Tzankov, A.; Stauder, R. Over-expression of tumor necrosis factor-alpha in bone marrow biopsies from patients with myelodysplastic syndromes: Relationship to anemia and prognosis. Eur. J. Haematol. 2005, 75, 485–491. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, X.; Guo, J.; Xu, F.; He, Q.; Zhao, Y.; Yang, Y.; Gu, S.; Zhang, Y.; Wu, L.; et al. Interleukin-17 enhances the production of interferon-γ and tumour necrosis factor-α by bone marrow T lymphocytes from patients with lower risk myelodysplastic syndromes. Eur. J. Haematol. 2013, 90, 375–384. [Google Scholar] [CrossRef]
- Calado, R.T. Immunologic aspects of hypoplastic myelodysplastic syndrome. Semin. Oncol. 2011, 38, 667–672. [Google Scholar] [CrossRef] [Green Version]
- Shi, X.; Zheng, Y.; Xu, L.; Cao, C.; Dong, B.; Chen, X. The inflammatory cytokine profile of myelodysplastic syndromes: A meta-analysis. Medicine 2019, 98, e15844. [Google Scholar] [CrossRef]
- Aggarwal, S.; van de Loosdrecht, A.A.; Alhan, C.; Ossenkoppele, G.J.; Westers, T.M.; Bontkes, H.J. Role of immune responses in the pathogenesis of low-risk MDS and high-risk MDS: Implications for immunotherapy. Br. J. Haematol. 2011, 153, 568–581. [Google Scholar] [CrossRef] [PubMed]
- Giudice, V.; Wu, Z.; Kajigaya, S.; Fernandez Ibanez, M.; Rios, O.; Cheung, F.; Ito, S.; Young, N.S. Circulating S100A8 and S100A9 protein levels in plasma of patients with acquired aplastic anemia and myelodysplastic syndromes. Cytokine 2019, 113, 462–465. [Google Scholar] [CrossRef]
- Moudra, A.; Hubackova, S.; Machalova, V.; Vancurova, M.; Bartek, J.; Reinis, M.; Hodny, Z.; Jonasova, A. Dynamic alterations of bone marrow cytokine landscape of myelodysplastic syndromes patients treated with 5-azacytidine. Oncoimmunology 2016, 5, e1183860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kittang, A.O.; Sand, K.; Brenner, A.K.; Rye, K.P.; Bruserud, Ø. The Systemic Profile of Soluble Immune Mediators in Patients with Myelodysplastic Syndromes. Int. J. Mol. Sci. 2016, 17, 1080. [Google Scholar] [CrossRef]
- Jassal, B.; Matthews, L.; Viteri, G.; Gong, C.; Lorente, P.; Fabregat, A.; Sidiropoulos, K.; Cook, J.; Gillespie, M.; Haw, R.; et al. The reactome pathway knowledgebase. Nucleic Acids Res. 2020, 48, D498–D503. [Google Scholar] [CrossRef] [PubMed]
- Szklarczyk, D.; Morris, J.H.; Cook, H.; Kuhn, M.; Wyder, S.; Simonovic, M.; Santos, A.; Doncheva, N.T.; Roth, A.; Bork, P.; et al. The STRING database in 2017: Quality-controlled protein-protein association networks, made broadly accessible. Nucleic Acids Res. 2017, 45, D362–D368. [Google Scholar] [CrossRef] [PubMed]
- Lamy, T.; Moignet, A.; Loughran, T.P., Jr. LGL leukemia: From pathogenesis to treatment. Blood 2017, 129, 1082–1094. [Google Scholar] [CrossRef]
- Zambello, R.; Semenzato, G. Large granular lymphocyte disorders: New etiopathogenetic clues as a rationale for innovative therapeutic approaches. Haematologica 2009, 94, 1341–1345. [Google Scholar] [CrossRef]
- Zhang, R.; Shah, M.V.; Yang, J.; Nyland, S.B.; Liu, X.; Yun, J.K.; Albert, R.; Loughran, T.P., Jr. Network model of survival signaling in large granular lymphocyte leukemia. Proc. Natl. Acad. Sci. USA 2008, 105, 16308–16313. [Google Scholar] [CrossRef] [Green Version]
- Moignet, A.; Lamy, T. Latest Advances in the Diagnosis and Treatment of Large Granular Lymphocytic Leukemia. American Society of Clinical Oncology educational book. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 616–625. [Google Scholar] [CrossRef]
- Clemente, M.J.; Wlodarski, M.W.; Makishima, H.; Viny, A.D.; Bretschneider, I.; Shaik, M.; Bejanyan, N.; Lichtin, A.E.; Hsi, E.D.; Paquette, R.L.; et al. Clonal drift demonstrates unexpected dynamics of the T-cell repertoire in T-large granular lymphocyte leukemia. Blood 2011, 118, 4384–4393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clemente, M.J.; Przychodzen, B.; Jerez, A.; Dienes, B.E.; Afable, M.G.; Husseinzadeh, H.; Rajala, H.L.; Wlodarski, M.W.; Mustjoki, S.; Maciejewski, J.P. Deep sequencing of the T-cell receptor repertoire in CD8+ T-large granular lymphocyte leukemia identifies signature landscapes. Blood 2013, 122, 4077–4085. [Google Scholar] [CrossRef] [PubMed]
- Dubois, S.; Mariner, J.; Waldmann, T.A.; Tagaya, Y. IL-15Ralpha recycles and presents IL-15 In trans to neighboring cells. Immunity 2002, 17, 537–547. [Google Scholar] [CrossRef] [Green Version]
- Bamford, R.N.; Grant, A.J.; Burton, J.D.; Peters, C.; Kurys, G.; Goldman, C.K.; Brennan, J.; Roessler, E.; Waldmann, T.A. The interleukin (IL) 2 receptor beta chain is shared by IL-2 and a cytokine, provisionally designated IL-T, that stimulates T-cell proliferation and the induction of lymphokine-activated killer cells. Proc. Natl. Acad. Sci. USA 1994, 91, 4940–4944. [Google Scholar] [CrossRef] [Green Version]
- Grabstein, K.H.; Eisenman, J.; Shanebeck, K.; Rauch, C.; Srinivasan, S.; Fung, V.; Beers, C.; Richardson, J.; Schoenborn, M.A.; Ahdieh, M. Cloning of a T cell growth factor that interacts with the beta chain of the interleukin-2 receptor. Science 1994, 264, 965–968. [Google Scholar] [CrossRef]
- Mishra, A.; Liu, S.; Sams, G.H.; Curphey, D.P.; Santhanam, R.; Rush, L.J.; Schaefer, D.; Falkenberg, L.G.; Sullivan, L.; Jaroncyk, L.; et al. Aberrant overexpression of IL-15 initiates large granular lymphocyte leukemia through chromosomal instability and DNA hypermethylation. Cancer Cell. 2012, 22, 645–655. [Google Scholar] [CrossRef] [Green Version]
- Kallemeijn, M.J.; de Ridder, D.; Schilperoord-Vermeulen, J.; van der Klift, M.Y.; Sandberg, Y.; van Dongen, J.J.; Langerak, A.W. Dysregulated signaling, proliferation and apoptosis impact on the pathogenesis of TCRγδ+ T cell large granular lymphocyte leukemia. PLoS ONE 2017, 12, e0175670. [Google Scholar] [CrossRef]
- Lamy, T.; Liu, J.H.; Landowski, T.H.; Dalton, W.S.; Loughran, T.P., Jr. Dysregulation of CD95/CD95 ligand-apoptotic pathway in CD3(1) large granular lymphocyte leukemia. Blood 1998, 92, 4771–4777. [Google Scholar] [CrossRef]
- Liu, J.H.; Wei, S.; Lamy, T.; Li, Y.; Epling-Burnette, P.K.; Djeu, J.Y.; Loughran, T.P., Jr. Blockade of Fas dependent apoptosis by soluble Fas in LGL leukemia. Blood 2002, 100, 1449–1453. [Google Scholar] [CrossRef] [Green Version]
- Kothapalli, R.; Nyland, S.B.; Kusmartseva, I.; Bailey, R.D.; McKeown, T.M.; Loughran, T.P., Jr. Constitutive production of proinflammatory cytokines RANTES, MIP-1beta and IL-18 characterizes LGL leukemia. Int. J. Oncol. 2005, 26, 529–535. [Google Scholar]
- Schade, A.E.; Wlodarski, M.W.; Maciejewski, J.P. Pathophysiology defined by altered signal transduction pathways: The role of JAK-STAT and PI3K signaling in leukemic large granular lymphocytes. Cell Cycle 2006, 5, 2571–2574. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; LeBlanc, F.R.; Dighe, S.A.; Hamele, C.E.; Olson, T.L.; Feith, D.J.; Loughran, T.P., Jr. TRAIL mediates and sustains constitutive NF-κB activation in LGL leukemia. Blood 2018, 131, 2803–2815. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Petrus, M.; Bamford, R.; Shih, J.H.; Morris, J.C.; Janik, J.E.; Waldmann, T.A. Increased serum soluble IL-15Rα levels in T-cell large granular lymphocyte leukemia. Blood 2012, 119, 137–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gentile, T.C.; Loughran, T.P., Jr. Interleukin-12 is a costimulatory cytokine for leukemic CD3+ large granular lymphocytes. Cell Immunol. 1995, 166, 158–161. [Google Scholar] [CrossRef] [PubMed]
- Risitano, A.M.; Rotoli, B. Paroxysmal nocturnal hemoglobinuria: Pathophysiology, natural history and treatment options in the era of biological agents. Biologics 2008, 2, 205–222. [Google Scholar] [CrossRef] [Green Version]
- Devalet, B.; Mullier, F.; Chatelain, B.; Dogné, J.M.; Chatelain, C. Pathophysiology, diagnosis, and treatment of paroxysmal nocturnal hemoglobinuria: A review. Eur. J. Haematol. 2015, 95, 190–198. [Google Scholar] [CrossRef]
- Bessler, M.; Hiken, J. The pathophysiology of disease in patients with paroxysmal nocturnal hemoglobinuria. Hematology Am. Soc. Hematol. Educ. Program. 2008, 2008, 104–110. [Google Scholar] [CrossRef] [Green Version]
- Hu, R.; Mukhina, G.L.; Piantadosi, S.; Barber, J.P.; Jones, R.J.; Brodsky, R.A. PIG-A mutations in normal hematopoiesis. Blood 2005, 105, 3848–3854. [Google Scholar] [CrossRef]
- Wang, S.Y.; Yang, X.J.; Yang, S.S.; Wang, W.; Tian, Y.Y.; Cao, F.L.; Zhou, J. Association analysis of cytokine polymorphisms and plasma level in Northern Chinese Han patients with paroxysmal nocturnal hemoglobinuria. Chin. Med. J. 2012, 125, 1576–1580. [Google Scholar]
- Coluzzi, S.; Biffoni, M.; Pasqualetti, D.; Perrone, M.P.; Vaglio, S.; Rahimi, H.; Arista, M.C.; Laurenti, L.; Cerretti, R.; Girelli, G. Production of interferon-gamma by lymphocytes from paroxysmal nocturnal haemoglobinuria patients: Relationship with clinical status. Br. J. Haematol. 2004, 124, 685–690. [Google Scholar] [CrossRef]
- Maciejewski, J.P.; Hibbs, J.R.; Anderson, S.; Katevas, P.; Young, N.S. Bone marrow and peripheral blood lymphocyte phenotype in patients with bone marrow failure. Exp. Hematol. 1994, 22, 1102–1110. [Google Scholar] [PubMed]
- Dufour, C.; Corcione, A.; Svahn, J.; Haupt, R.; Battilana, N.; Pistoia, V. Interferon gamma and tumour necrosis factor alpha are overexpressed in bone marrow T lymphocytes from paedriatic patients with aplastic anaemia. Br. J. Haematol. 2001, 115, 1023–1031. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, K.; Kajigaya, S.; Keyvanfar, K.; Qiao, W.; Xie, Y.; Townsley, D.M.; Feng, X.; Young, N.S. T Cell Transcriptomes from Paroxysmal Nocturnal Hemoglobinuria Patients Reveal Novel Signaling Pathways. J. Immunol. 2017, 199, 477–488. [Google Scholar] [CrossRef] [PubMed]
- Gargiulo, L.; Zaimoku, Y.; Scappini, B.; Maruyama, H.; Ohumi, R.; Luzzatto, L.; Nakao, S.; Notaro, R. Glycosylphosphatidylinositol-specific T cells, IFN-γ-producing T cells, and pathogenesis of idiopathic aplastic anemia. Blood 2017, 129, 388–392. [Google Scholar] [CrossRef] [Green Version]
- Shimamura, A.; Alter, B.P. Pathophysiology and management of inherited bone marrow failure syndromes. Blood Rev. 2010, 24, 101–122. [Google Scholar] [CrossRef] [Green Version]
- Risitano, A.M.; Maciejewski, J.P.; Selleri, C.; Rotoli, B. Function and malfunction of hematopoietic stem cells in primary bone marrow failure syndromes. Curr. Stem Cell Res. Ther. 2007, 2, 39–52. [Google Scholar] [CrossRef] [Green Version]
- Matsui, K.; Giri, N.; Alter, B.P.; Pinto, L.A. Cytokine production by bone marrow mononuclear cells in inherited bone marrow failure syndromes. Br. J. Haematol. 2013, 163, 81–92. [Google Scholar] [CrossRef] [Green Version]
- Adam, S.; Melguizo Sanchis, D.; El-Kamah, G.; Samarasinghe, S.; Alharthi, S.; Armstrong, L.; Lako, M. Concise Review: Getting to the Core of Inherited Bone Marrow Failures. Stem Cells 2017, 35, 284–298. [Google Scholar] [CrossRef]
- Notaro, R.; Montuori, N.; di Grazia, C.; Formisano, S.; Rotoli, B.; Selleri, C. Fanconi’s anemia cells are relatively resistant to H2O2-induced damage. Haematologica 1998, 83, 868–874. [Google Scholar]
- Zatterale, A.; Calzone, R.; Renda, S.; Catalano, L.; Selleri, C.; Notaro, R.; Rotoli, B. Identification and treatment of late onset Fanconi’s anemia. Haematologica 1995, 80, 535–538. [Google Scholar]
- Parikh, S.; Bessler, M. Recent insights into inherited bone marrow failure syndromes. Curr. Opin. Pediatr. 2012, 24, 23–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenberg, P.S.; Greene, M.H.; Alter, B.P. Cancer incidence in persons with Fanconi anemia. Blood 2003, 101, 822–826. [Google Scholar] [CrossRef] [PubMed]
- Garaycoechea, J.I.; Patel, K.J. Why does the bone marrow fail in Fanconi anemia? Blood 2014, 123, 26–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carreau, M.; Gan, O.I.; Liu, L.; Doedens, M.; McKerlie, C.; Dick, J.E.; Buchwald, M. Bone marrow failure in the Fanconi anemia group C mouse model after DNA damage. Blood 1998, 91, 2737–2744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langevin, F.; Crossan, G.P.; Rosado, I.V.; Arends, M.J.; Patel, K.J. Fancd2 counteracts the toxic effects of naturally produced aldehydes in mice. Nature 2011, 475, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Giri, N.; Alter, B.P.; Penrose, K.; Falk, R.T.; Pan, Y.; Savage, S.A.; Williams, M.; Kemp, T.J.; Pinto, L.A. Immune status of patients with inherited bone marrow failure syndromes. Am. J. Hematol. 2015, 90, 702–708. [Google Scholar] [CrossRef] [Green Version]
- Korthof, E.T.; Svahn, J.; de Latour, R.P.; Terranova, P.; Moins-Teisserenc, H.; Socié, G.; Soulier, J.; Kok, M.; Bredius, R.G.; van Tol, M.; et al. Immunological profile of Fanconi anemia: A multicentric retrospective analysis of 61 patients. Am. J. Hematol. 2013, 88, 472–476. [Google Scholar] [CrossRef]
- Myers, K.C.; Bleesing, J.J.; Davies, S.M.; Zhang, X.; Martin, L.J.; Mueller, R.; Harris, R.E.; Filipovich, A.H.; Kovacic, M.B.; Wells, S.I.; et al. Impaired immune function in children with Fanconi anaemia. Br. J. Haematol. 2011, 154, 234–240. [Google Scholar] [CrossRef] [Green Version]
- Justo, G.A.; Bitencourt, M.A.; Pasquini, R.; Castelo-Branco, M.T.; Rumjanek, V.M. Increased IL10 plasmatic levels in Fanconi anemia patients. Cytokine 2013, 64, 486–489. [Google Scholar] [CrossRef]
- Dufour, C.; Corcione, A.; Svahn, J.; Haupt, R.; Poggi, V.; Beka’ssy, A.N.; Scime, R.; Pistorio, A.; Pistoia, V. TNF-alpha and IFNgamma are overexpressed in the bone marrow of Fanconi anemia patients and TNF-alpha suppresses erythropoiesis in vitro. Blood 2003, 102, 2053–2059. [Google Scholar] [CrossRef]
- Alter, B.P. Diagnosis, genetics, and management of inherited bone marrow failure syndromes. Hematology Am. Soc. Hematol. Educ. Program. 2007, 2007, 29–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsson, H.; Davey, E.J.; Fröjmark, A.S.; Miyake, K.; Utsugisawa, T.; Flygare, J.; Zahou, E.; Byman, I.; Landin, B.; Ronquist, G.; et al. Erythropoiesis in the Rps19 disrupted mouse: Analysis of erythropoietin response and biochemical markers for Diamond-Blackfan anemia. Blood Cells Mol. Dis. 2006, 36, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Schneider, R.K.; Schenone, M.; Ferreira, M.V.; Kramann, R.; Joyce, C.E.; Hartigan, C.; Beier, F.; Brümmendorf, T.H.; Germing, U.; Platzbecker, U.; et al. Rps14 haploinsufficiency causes a block in erythroid differentiation mediated by S100A8 and S100A9. Nat. Med. 2016, 22, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Pereboom, T.C.; van Weele, L.J.; Bondt, A.; MacInnes, A.W. A zebrafish model of dyskeratosis congenita reveals hematopoietic stem cell formation failure resulting from ribosomal protein-mediated p53 stabilization. Blood 2011, 118, 5458–5465. [Google Scholar] [CrossRef]
- Armanios, M.; Blackburn, E.H. The telomere syndromes. Nat. Rev. Genet. 2012, 13, 693–704. [Google Scholar] [CrossRef]
- Townsley, D.M.; Dumitriu, B.; Young, N.S. Bone marrow failure and the telomeropathies. Blood 2014, 124, 2775–2783. [Google Scholar] [CrossRef]
- Corey, S.J.; Minden, M.D.; Barber, D.L.; Kantarjian, H.; Wang, J.C.; Schimmer, A.D. Myelodysplastic syndromes: The complexity of stem-cell diseases. Nat. Rev. Cancer. 2007, 7, 118–129. [Google Scholar] [CrossRef]
- Bhatia, S. Therapy-related myelodysplasia and acute myeloid leukemia. Semin. Oncol. 2013, 40, 666–675. [Google Scholar] [CrossRef] [Green Version]
- Bhatia, R.; Deeg, H.J. Treatment-related myelodysplastic syndrome: Molecular characteristics and therapy. Curr. Opin. Hematol. 2011, 18, 77–82. [Google Scholar] [CrossRef]
- Gruschkus, S.K.; Lairson, D.; Dunn, J.K.; Risser, J.; Du, X.L. Use of white blood cell growth factors and risk of acute myeloid leukemia or myelodysplastic syndrome among elderly patients with non-Hodgkin lymphoma. Cancer 2010, 116, 5279–5289. [Google Scholar] [CrossRef]
- Stirewalt, D.L.; Mhyre, A.J.; Marcondes, M.; Pogosova-Agadjanyan, E.; Abbasi, N.; Radich, J.P.; Deeg, H.J. Tumour necrosis factor-induced gene expression in human marrow stroma: Clues to the pathophysiology of MDS? Br. J. Haematol. 2008, 140, 444–453. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, M.; Sun, C.L.; Sabado, M.D.; Francisco, L.; McDonald, T.; Chang, K.L.; Wang, S.; Radich, J.; Zhao, L.P.; et al. Gene Expression Changes in CD34+ Cells Precede Development of Therapy-Related Leukemia (t-MDS/AML) after Autologous Hematopoietic Cell Transplantation (aHCT) for Hodgkin (HL) or Non-Hodgkin Lymphoma (NHL). Blood 2009, 114, 677. [Google Scholar] [CrossRef]
- Risitano, A.M. Immunosuppressive therapies in the management of immune-mediated marrow failures in adults: Where we stand and where we are going. Br. J. Haematol. 2011, 152, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Kapralova, K.; Jahoda, O.; Koralkova, P.; Gursky, J.; Lanikova, L.; Pospisilova, D.; Divoky, V.; Horvathova, M. Oxidative DNA Damage, Inflammatory Signature, and Altered Erythrocytes Properties in Diamond-Blackfan Anemia. Int. J. Mol. Sci. 2020, 21, 9652. [Google Scholar] [CrossRef]
- Hubackova, S.; Kucerova, A.; Michlits, G.; Kyjacova, L.; Reinis, M.; Korolov, O.; Bartek, J.; Hodny, Z. IFNγ induces oxidative stress, DNA damage and tumor cell senescence via TGFβ/SMAD signaling-dependent induction of Nox4 and suppression of ANT2. Oncogene 2016, 35, 1236–1249. [Google Scholar] [CrossRef]
- Kang, T.W.; Yevsa, T.; Woller, N.; Hoenicke, L.; Wuestefeld, T.; Dauch, D.; Hohmeyer, A.; Gereke, M.; Rudalska, R.; Potapova, A.; et al. Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature 2011, 479, 547–551. [Google Scholar] [CrossRef]
- Braumüller, H.; Wieder, T.; Brenner, E.; Aßmann, S.; Hahn, M.; Alkhaled, M.; Schilbach, K.; Essmann, F.; Kneilling, M.; Griessinger, C.; et al. T-helper-1-cell cytokines drive cancer into senescence. Nature 2013, 494, 361–365. [Google Scholar] [CrossRef] [Green Version]
| ILs | Chemokines | IFNs/TNFs | Growth Factors | Others | |
|---|---|---|---|---|---|
| Increased | IL-2 | CXCL10 CCL20 | IFN-γ TNFα | G-CSF TPO EPO | GDF-15 sST2 |
| IL-8 | |||||
| IL-12 | |||||
| IL-17A | |||||
| IL-18 | |||||
| IL-21 | |||||
| IL-23 | |||||
| Decreased | IL-33 IL-35 | CCL5 | EGF VEGF | CD40L | |
| CCL11 | SELL | ||||
| CCL17 | DKK1 | ||||
| CXCL5 | c-Mpl | ||||
| CXCL11 | Hepcidin | ||||
| No changes | IL-1Ra IL-6 | CCL2 | HGF (or slightly reduced) | ||
| CCL3 | S100A8 | ||||
| CCL4 | S100A9 | ||||
| CXCL9 | S100A8/A9 | ||||
| CXCL11 |
| ILs | Chemokines | IFNs/TNFs | Growth Factors | Others | |
|---|---|---|---|---|---|
| Increased | CCL3 | VEGF | |||
| IL-1ra | CCL4 | IFN-γ | CD40L | ||
| IL-6 | CCL5 | TNFα | TGF-β | ||
| IL-17 | CCL11 | TRAIL | FLIP | ||
| CXCL5 | |||||
| CXCL11 | |||||
| Decreased | IL-10 | TPO |
| ILs | Chemokines | IFNs/TNFs | Growth Factors | Others | |
|---|---|---|---|---|---|
| Increased | IL-1β | CCL2 | IFN-γ IFN-α2 | PDGF EGF | |
| IL-1ra | |||||
| IL-6 | RANTES | ||||
| IL-8 | MIP-1α | ||||
| IL-10 | MIP-1β | ||||
| IL-12p35 | sFas-L | ||||
| IL-15 | B2M | ||||
| sIL-15Rα | |||||
| IL-18 | |||||
| Decreased | FLIP |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giudice, V.; Cardamone, C.; Triggiani, M.; Selleri, C. Bone Marrow Failure Syndromes, Overlapping Diseases with a Common Cytokine Signature. Int. J. Mol. Sci. 2021, 22, 705. https://doi.org/10.3390/ijms22020705
Giudice V, Cardamone C, Triggiani M, Selleri C. Bone Marrow Failure Syndromes, Overlapping Diseases with a Common Cytokine Signature. International Journal of Molecular Sciences. 2021; 22(2):705. https://doi.org/10.3390/ijms22020705
Chicago/Turabian StyleGiudice, Valentina, Chiara Cardamone, Massimo Triggiani, and Carmine Selleri. 2021. "Bone Marrow Failure Syndromes, Overlapping Diseases with a Common Cytokine Signature" International Journal of Molecular Sciences 22, no. 2: 705. https://doi.org/10.3390/ijms22020705
APA StyleGiudice, V., Cardamone, C., Triggiani, M., & Selleri, C. (2021). Bone Marrow Failure Syndromes, Overlapping Diseases with a Common Cytokine Signature. International Journal of Molecular Sciences, 22(2), 705. https://doi.org/10.3390/ijms22020705






