A Review of Plant Extracts and Plant-Derived Natural Compounds in the Prevention/Treatment of Neonatal Hypoxic-Ischemic Brain Injury
Abstract
1. Introduction
2. Pathophysiology of Neonatal Hypoxic-Ischemic Brain Damage
2.1. Excitatory
2.2. Free Radical Toxicity
2.3. Inflammation
2.4. Neuronal Death
3. Potential Mechanisms for Neuroprotective Strategies
3.1. Reduction of Cellular Apoptosis and Oxidative Stress in HI
3.2. Reduction of Neurotrophic-Evoked Excitation and Inflammatory Cytokines in HI
3.3. Animal Model of HI
4. Pharmacological Evidence of Natural Plant Products in Neonatal Hypoxic-Ischemic Brain Damage
4.1. Plant Extracts
4.1.1. Grape Seed Extract
4.1.2. Grape Seed Proanthocyanidin Extract
4.1.3. Pomegranate Juice and Pomegranate Polyphenol Extract
4.1.4. Dendrobium officinale Extract
4.2. Phytochemicals
4.2.1. Verbascoside
4.2.2. Geniposide
4.2.3. Hesperidin
4.2.4. Quercetin
4.2.5. Pterostilbene
4.2.6. Vitexin
4.2.7. Oxymatrine
4.2.8. Coumestrol
4.2.9. Plastoquinone
4.2.10. Resveratrol
4.2.11. Piceatannol
4.2.12. Polydatin
4.2.13. Vanillin
4.2.14. Caffeine
4.2.15. Crocin
4.2.16. Tanshinone IIA
4.2.17. Cannabidiol
4.2.18. Huperzine A
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Kruszewski, S.P. Neonatal Brain Injury. N. Engl. J. Med. 2005, 352, 1985–1995. [Google Scholar] [CrossRef]
- Lawn, J.E.; Cousens, S.; Zupan, J. 4 Million Neonatal Deaths: When? Where? Why? Lancet 2005, 365, 891–900. [Google Scholar] [CrossRef]
- Dilenge, M.E.; Majnemer, A.; Shevell, M.I. Long-Term Developmental Outcome of Asphyxiated Term Neonates. J. Child Neurol. 2001, 16, 781–792. [Google Scholar] [CrossRef]
- Graham, E.M.; Ruis, K.A.; Hartman, A.L.; Northington, F.J.; Fox, H.E. A Systematic Review of the Role of Intrapartum Hypoxia-Ischemia in the Causation of Neonatal Encephalopathy. Am. J. Obstet. Gynecol. 2008, 199, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Kurinczuk, J.J.; White-Koning, M.; Badawi, N. Epidemiology of Neonatal Encephalopathy and Hypoxic-Ischaemic Encephalopathy. Early Hum. Dev. 2010, 86, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Airede, A.I. Birth Asphyxia and Hypoxic-Ischaemic Encephalopathy: Incidence and Severity. Ann. Trop. Paediatr. 1991, 11, 331–335. [Google Scholar] [CrossRef] [PubMed]
- De Haan, M.; Wyatt, J.S.; Roth, S.; Vargha-Khadem, F.; Gadian, D.; Mishkin, M. Brain and Cognitive-Behavioural Development after Asphyxia at Term Birth. Dev. Sci. 2006, 9, 350–358. [Google Scholar] [CrossRef]
- Roth, S.C.; Edwards, A.D.; Cady, E.B.; Delpy, D.T.; Wyatt, J.S.; Azzopardi, D.; Baudin, J.; Townsend, J.; Stewart, A.L.; Reynolds, E.O. Relation between cerebral oxidative metabolism following birth asphyxia, and neurodevelopmental outcome and brain growth at one year. Dev. Med. Child Neurol. 1992, 34, 285–295. [Google Scholar] [CrossRef]
- Gluckman, P.D.; Pinal, C.S.; Gunn, A.J. Hypoxic-Ischemic Brain Injury in the Newborn: Pathophysiology and Potential Strategies for Intervention. Semin. Neonatol. 2001, 6, 109–120. [Google Scholar] [CrossRef]
- Bunney, P.E.; Zink, A.N.; Holm, A.A.; Billington, C.J.; Kotz, C.M. Orexin activation counteracts decreases in nonexercise activity thermogenesis (NEAT) caused by high-fat diet. Physiol. Behav. 2017, 176, 139–148. [Google Scholar] [CrossRef]
- Gluckman, P.D.; Wyatt, J.S.; Azzopardi, D.; Ballard, R.; Edwards, A.D.; Ferriero, D.M.; Polin, R.A.; Robertson, C.M.; Thoresen, M.; Whitelaw, A.; et al. Selective Head Cooling with Mild Systemic Hypothermia after Neonatal Encephalopathy: Multicentre Randomised Trial. Lancet 2005, 365, 663–670. [Google Scholar] [CrossRef]
- Azzopardi, D.; Strohm, B.; Marlow, N.; Brocklehurst, P.; Deierl, A.; Eddama, O.; Goodwin, J.; Halliday, H.L.; Juszczak, E.; Kapellou, O.; et al. Effects of Hypothermia for Perinatal Asphyxia on Childhood Outcomes. N. Engl. J. Med. 2014, 371, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Shankaran, S.; Pappas, A.; McDonald, S.A.; Vohr, B.R.; Hintz, S.R.; Yolton, K.; Gustafson, K.E.; Leach, T.M.; Green, C.; Bara, R.; et al. Childhood Outcomes after Hypothermia for Neonatal Encephalopathy. Obstet. Gynecol. Surv. 2012, 67, 617–619. [Google Scholar] [CrossRef]
- Ournal, T.H.E.J.; Ediatrics, O.F.P. Neuroprotective Strategies in Neonatal Brain Injury. J. Pediatr. 2017, 192, 22–32. [Google Scholar] [CrossRef]
- Simonyi, A.; Wang, Q.; Miller, R.L.; Yusof, M.; Shelat, P.B.; Sun, A.Y.; Sun, G.Y. Polyphenols in Cerebral Ischemia: Novel Targets for Neuroprotection. Mol. Neurobiol. 2005, 31, 135–147. [Google Scholar] [CrossRef]
- Ahmad, N.; Khan, Z.; Hasan, N.; Basit, A.; Zohrameena, S. Neuroprotective Agents, Natural Plant Herbs & Drugs in Ischemic Stroke: A Review. PharmaTutor 2017, 5, 29–36. [Google Scholar]
- Costa, S.L.; Silva, V.D.A.; dos Santos Souza, C.; Santos, C.C.; Paris, I.; Muñoz, P.; Segura-Aguilar, J. Impact of Plant-Derived Flavonoids on Neurodegenerative Diseases. Neurotox. Res. 2016. [Google Scholar] [CrossRef]
- Su, S.; Hsieh, C. Anti-Inflammatory Effects of Chinese Medicinal Herbs on Cerebral Ischemia. Chin. Med. 2011, 6, 1–9. [Google Scholar] [CrossRef]
- Pohl, F.; Kong, P.; Lin, T. The Potential Use of Plant Natural Products and Plant Extracts with Antioxidant Properties for the Prevention/Treatment of Neurodegenerative Diseases: In Vitro, In Vivo and Clinical Trials. Molecules 2018, 23, 3283. [Google Scholar] [CrossRef]
- Albrecht, M.; Zitta, K.; Groenendaal, F.; Van Bel, F.; Peeters-Scholte, C. Neuroprotective Strategies Following Perinatal Hypoxia-Ischemia: Taking Aim at NOS. Free Radic. Biol. Med. 2019, 142, 123–131. [Google Scholar] [CrossRef]
- Nair, J.; Kumar, V.H.S. Current and Emerging Therapies in the Management of Hypoxic Ischemic Encephalopathy in Neonates. Children 2018, 5, 99. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Chen, W.; Sinha, B.; Tu, Y.; Manning, S.; Thomas, N.; Zhou, S.; Jiang, H.; Ma, H.; Kroessler, D.A.; et al. Neuroprotective Agents for Neonatal Hypoxic-Ischemic Brain Injury. Drug Discov. Today 2015, 20, 1372–1381. [Google Scholar] [CrossRef] [PubMed]
- Dixon, B.J.; Reis, C.; Ho, W.M.; Tang, J.; Zhang, J.H. Neuroprotective strategies after neonatal hypoxic ischemic encephalopathy. Int. J. Mol. Sci. 2015, 16, 22368–22401. [Google Scholar] [CrossRef] [PubMed]
- Grow, J.; Barks, J.D.E. Pathogenesis of Hypoxic-Ischemic Cerebral Injury in the Term Infant: Current Concepts. Clin. Perinatol. 2002, 29, 585–602. [Google Scholar] [CrossRef]
- Northington, F.J.; Graham, E.M.; Martin, L.J. Apoptosis in perinatal hypoxic-ischemic brain injury: How important is it and should it be inhibited? Brain Res. Rev. 2005, 50, 244–257. [Google Scholar] [CrossRef]
- Yin, W.; Cao, G.; Johnnides, M.J.; Signore, A.P.; Luo, Y.; Hickey, R.W.; Chen, J. TAT-Mediated Delivery of Bcl-XL Protein Is Neuroprotective against Neonatal Hypoxic-Ischemic Brain Injury via Inhibition of Caspases and AIF. Neurobiol. Dis. 2006, 21, 358–371. [Google Scholar] [CrossRef]
- Han, B.H.; Xu, D.; Choi, J.; Han, Y.; Xanthoudakis, S.; Roy, S.; Tam, J.; Vaillancourt, J.; Colucci, J.; Siman, R.; et al. Selective, reversible caspase-3 inhibitor is neuroprotective and reveals distinct pathways of cell death after neonatal hypoxic-ischemic brain injury. J. Biol. Chem. 2002, 277, 30128–30136. [Google Scholar] [CrossRef]
- Alonso-Alconada, D.; Álvarez, A.; Arteaga, O.; Martínez-Ibargüen, A.; Hilario, E. Neuroprotective Effect of Melatonin: A Novel Therapy against Perinatal Hypoxia-Ischemia. Int. J. Mol. Sci. 2013, 14, 9379–9395. [Google Scholar] [CrossRef]
- Arteaga, O.; Álvarez, A.; Revuelta, M.; Santaolalla, F.; Urtasun, A.; Hilario, E. Role of Antioxidants in Neonatal Hypoxic–Ischemic Brain Injury: New Therapeutic Approaches. Int. J. Mol. Sci. 2017, 18, 265. [Google Scholar] [CrossRef]
- Shen, H.; Hu, X.; Liu, C.; Wang, S.; Zhang, W.; Gao, H.; Stetler, R.A.; Gao, Y.; Chen, J. Ethyl Pyruvate Protects against Hypoxic-Ischemic Brain Injury via Anti-Cell Death and Anti-Inflammatory Mechanisms. Neurobiol. Dis. 2010, 37, 711–722. [Google Scholar] [CrossRef]
- Yang, D.; Sun, Y.Y.; Lin, X.; Baumann, J.M.; Dunn, R.S.; Lindquist, D.M.; Kuan, C.Y. Intranasal Delivery of Cell-Penetrating Anti-NF-κB Peptides (Tat-NBD) Alleviates Infection-Sensitized Hypoxic-Ischemic Brain Injury. Exp. Neurol. 2013, 247, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Yıldız, E.P.; Ekici, B.; Tatlı, B. Neonatal Hypoxic Ischemic Encephalopathy: An Update on Disease Pathogenesis and Treatment. Expert Rev. Neurother. 2017, 17, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Donega, V.; van Velthoven, C.T.; Nijboer, C.H.; Kavelaars, A.; Heijnen, C.J. The endogenous regenerative capacity of the damaged newborn brain: Boosting neurogenesis with mesenchymal stem cell treatment. J. Cereb. Blood Flow Metab. 2013, 33, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.I.; Xiong, L.-J.; Tong, Y.U.; Mao, M. The Neuroprotective Roles of BDNF in Hypoxic Ischemic Brain Injury. Biomed. Rep. 2013, 1, 167–176. [Google Scholar] [CrossRef]
- Yager, J.Y.; Ashwal, S. Animal models of perinatal hypoxic-ischemic brain damage. Pediatr. Neurol. 2009, 40, 156–167. [Google Scholar] [CrossRef]
- Loren, D.J.; Seeram, N.P.; Schulman, R.N.; Holtzman, D.M. Maternal Dietary Supplementation with Pomegranate Juice Is Neuroprotective in an Animal Model of Neonatal Hypoxic-Ischemic Brain Injury. Pediatr. Res. 2005, 57, 858–864. [Google Scholar] [CrossRef]
- Li, X.-L.; Hong, M. Aqueous Extract of Dendrobium Officinale Confers Neuroprotection against Hypoxic-Ischemic Brain Damage in Neonatal Rats. Kaohsiung J. Med. Sci. 2020, 36, 43–53. [Google Scholar] [CrossRef]
- Lafuente, H.; Pazos, M.R.; Alvarez, A.; Mohammed, N.; Santos, M.; Arizti, M.; Alvarez, F.J.; Martinez-Orgado, J.A.; Davidson, J. Effects of Cannabidiol and Hypothermia on Short-Term Brain Damage in New-Born Piglets after Acute Hypoxia-Ischemia. Front. Neurosci. 2016, 10, 1–11. [Google Scholar] [CrossRef]
- Yadav, M.; Jain, S.; Bhardwaj, A.; Nagpal, R.; Puniya, M.; Tomar, R.; Singh, V.; Parkash, O.; Prasad, G.B.K.S.; Marotta, F.; et al. Biological and Medicinal Properties of Grapes and Their Bioactive Constituents: An Update. J. Med. Food 2009, 12, 473–484. [Google Scholar] [CrossRef]
- Jang, M.H.; Piao, X.L.; Kim, J.M.; Kwon, S.W.; Park, J.H. Inhibition of Cholinesterase and Amyloid-β Aggregation by Resveratrol Oligomers from Vitis Amurensis. Phyther. Res. 2008, 22, 544–549. [Google Scholar] [CrossRef]
- Fine, A.M. Oligomeric Proanthocyanidin Complexes: Applications Oligomeric Proanthocyanidins. Altern. Med. Rev. 2000, 5, 144–151. [Google Scholar] [PubMed]
- Bian, J.T.; Bhargava, H.N. Protective Effects of Grape Seed Proanthocyanidins and Selected Antioxidants against TPA-Induced Hepatic and Brain Lipid Peroxidation and DNA Fragmentation, and Peritoneal Macrophage Activation in Mice. Gen. Pharmacol. 1998, 30, 771–776. [Google Scholar] [CrossRef]
- Bagchi, D.; Sen, C.K.; Ray, S.D.; Das, D.K.; Bagchi, M.; Preuss, H.G.; Vinson, J.A. Molecular Mechanisms of Cardioprotection by a Novel Grape Seed Proanthocyanidin Extract. Mutat. Res. Fundam. Mol. Mech. Mutagen. 2003, 523–524, 87–97. [Google Scholar] [CrossRef]
- Shafiee, M.; Carbonneau, M.A.; Urban, N.; Descomps, B.; Leger, C.L. Grape and Grape Seed Extract Capacities at Protecting LDL against Oxidation Generated by Cu2+, AAPH or SIN-1 and at Decreasing Superoxide THP-1 Cell Production. A Comparison to Other Extracts or Compounds. Free Radic. Res. 2003, 37, 573–584. [Google Scholar] [CrossRef]
- Balu, M.; Sangeetha, P.; Murali, G.; Panneerselvam, C. Modulatory Role of Grape Seed Extract on Age-Related Oxidative DNA Damage in Central Nervous System of Rats. Brain Res. Bull. 2006, 68, 469–473. [Google Scholar] [CrossRef]
- Ariga, T. The Antioxidative Function, Preventive Action on Disease and Utilization of Proanthocyanidins. BioFactors 2004, 21, 197–201. [Google Scholar] [CrossRef]
- Sato, M.; Bagchi, D.; Tosaki, A.; Das, D.K. Grape Seed Proanthocyanidin Reduces Cardiomyocyte Apoptosis by Inhibiting Ischemia/Reperfusion-Induced Activation of JNK-1 and C-JUN. Free Radic. Biol. Med. 2001, 31, 729–737. [Google Scholar] [CrossRef]
- Ray, S.D.; Kumar, M.A.; Bagchi, D. A novel proanthocyanidin IH636 grape seed extract increases in vivo Bcl-XL expression and prevents acetaminophen-induced programmed and unprogrammed cell death in mouse liver. Arch. Biochem. Biophys. 1999, 369, 42–58. [Google Scholar] [CrossRef]
- Sugisawa, A.; Inoue, S.; Umegaki, K. Grape Seed Extract Prevents H2O2-Induced Chromosomal Damage in Human Lymphoblastoid Cells. Biol. Pharm. Bull. 2004, 27, 1459–1461. [Google Scholar] [CrossRef]
- Baines, C.P.; Molkentin, J.D. STRESS signaling pathways that modulate cardiac myocyte apoptosis. J. Mol. Cell. Cardiol. 2005, 38, 47–62. [Google Scholar] [CrossRef]
- Hwang, I.K.; Yoo, K.Y.; Kim, D.S.; Jeong, Y.K.; Kim, J.D.; Shin, H.K.; Lim, S.S.; Yoo, I.D.; Kang, T.C.; Kim, D.W.; et al. Neuroprotective Effects of Grape Seed Extract on Neuronal Injury by Inhibiting DNA Damage in the Gerbil Hippocampus after Transient Forebrain Ischemia. Life Sci. 2004, 75, 1989–2001. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Liu, Y.M.; Fratkins, J.D.; LeBlanc, M.H. Grape Seed Extract Suppresses Lipid Peroxidation and Reduces Hypoxic Ischemic Brain Injury in Neonatal Rats. Brain Res. Bull. 2005, 66, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Liu, Y.M.; Leblanc, M.H.; Bhatt, A.J.; Rhodes, P.G. Grape Seed Extract given Three Hours after Injury Suppresses Lipid Peroxidation and Reduces Hypoxic-Ischemic Brain Injury in Neonatal Rats. Pediatr. Res. 2007, 61, 295–300. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fracassetti, D.; Costa, C.; Moulay, L.; Tomás-barberán, F.A. Ellagic Acid Derivatives, Ellagitannins, Proanthocyanidins and Other Phenolics, Vitamin C and Antioxidant Capacity of Two Powder Products from Camu-Camu Fruit (Myrciaria Dubia). Food Chem. 2013, 139, 578–588. [Google Scholar] [CrossRef] [PubMed]
- Margalef, M.; Guerrero, L.; Pons, Z.; Isabel, F.; Arola, L.; Muguerza, B.; Arola-arnal, A. A dose—Response study of the bioavailability of grape seed proanthocyanidin in rat and lipid-lowering effects of generated metabolites in HepG2 cells. Food Res. Int. 2014, 64, 500–507. [Google Scholar] [CrossRef]
- Devi, S.A.; Jolitha, A.B.; Ishii, N. Grape seed proanthocyanidin extract (GSPE) and antioxidant defense in the brain of adult rats. Med Sci. Monit. 2006, 12, BR124–BR129. [Google Scholar]
- Ferruzzi, M.G.; Lobo, J.K.; Janle, E.M.; Cooper, B.; Simon, J.E.; Wu, Q.; Welch, C.; Ho, L.; Weaver, C.; Pasinetti, G.M. Bioavailability of gallic acid and catechins from grape seed polyphenol extract is improved by repeated dosing in rats: Implications for treatment in alzheimer’s disease. J. Alzheimers Dis. 2009, 18, 113–124. [Google Scholar] [CrossRef]
- Wu, L.; Zhang, Q.L.; Zhang, X.Y.; Lv, C.; Li, J.; Yuan, Y.; Yin, F.X. Pharmacokinetics and Blood-Brain Barrier Penetration of (+)-Catechin and (-)-Epicatechin in Rats by Microdialysis Sampling Coupled to High-Performance Liquid Chromatography with Chemiluminescence Detection. J. Agric. Food Chem. 2012, 60, 9377–9383. [Google Scholar] [CrossRef]
- Kong, X.; Guan, J.; Gong, S.; Wang, R. Neuroprotective Effects of Grape Seed Procyanidin Extract on Ischemia-Reperfusion Brain Injury. Chin. Med. Sci. J. 2017, 32, 92–99. [Google Scholar] [CrossRef]
- Tu, X.; Wang, M.; Liu, Y.; Zhao, W.; Ren, X.; Li, Y.; Liu, H.; Gu, Z.; Jia, H.; Liu, J.; et al. Pretreatment of Grape Seed Proanthocyanidin Extract Exerts Neuroprotective Effect in Murine Model of Neonatal Hypoxic-Ischemic Brain Injury by Its Antiapoptotic Property. Cell. Mol. Neurobiol. 2019, 39, 953–961. [Google Scholar] [CrossRef]
- Kalaycıoğlu, Z.; Erim, F.B. Total Phenolic Contents, Antioxidant Activities, and Bioactive Ingredients of Juices from Pomegranate Cultivars Worldwide. Food Chem. 2017, 221, 496–507. [Google Scholar] [CrossRef] [PubMed]
- Venkata, C.; Prakash, S.; Prakash, I. Bioactive Chemical Constituents from Pomegranate (Punica Granatum) Juice, Seed and Peel-A Review. Int. J. Res. Chem. Environ. 2011, 1, 1–18. [Google Scholar]
- Akhtar, S.; Ismail, T.; Fraternale, D.; Sestili, P. Pomegranate Peel and Peel Extracts: Chemistry and Food Features. Food Chem. 2015, 174, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Landete, J.M. Ellagitannins, Ellagic Acid and Their Derived Metabolites: A Review about Source, Metabolism, Functions and Health. Food Res. Int. 2011, 44, 1150–1160. [Google Scholar] [CrossRef]
- Wu, P.; Fitschen, P.J.; Kistler, B.M.; Jeong, J.H.; Chung, H.R.; Aviram, M.; Phillips, S.A.; Fernhall, B.; Wilund, K.R. Effects of pomegranate extract supplementation on cardiovascular risk factors and physical function in hemodialysis patients. J. Med. Food 2015, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Ferri, C.; Giorgini, P.; Bo, S.; Nachtigal, P.; Grassi, D. Effects of Pomegranate Juice on Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pharmacol. Res. 2017, 115, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Panth, N.; Manandhar, B.; Paudel, K.R. Anticancer Activity of Punica Granatum (Pomegranate): A Review. Phyther. Res. 2017, 31, 568–578. [Google Scholar] [CrossRef]
- Article, R.; Review, G. Anti-cancer activity of pomegranate and its biophenols; general review. EC Nutr. 2016, 1, 28–52. [Google Scholar]
- Shukla, M.; Gupta, K.; Rasheed, Z.; Khan, K.A.; Haqqi, T.M. Consumption of hydrolyzable tannins-rich pomegranate extract suppresses inflammation and joint damage in rheumatoid arthritis. Nutrition 2008, 24, 733–743. [Google Scholar] [CrossRef]
- Ghavipour, M.; Sotoudeh, G.; Tavakoli, E.; Mowla, K.; Hasanzadeh, J.; Mazloom, Z. Pomegranate extract alleviates disease activity and some blood biomarkers of in fl ammation and oxidative stress in Rheumatoid Arthritis patients. Eur. J. Clin. Nutr. 2016, 71, 92–96. [Google Scholar] [CrossRef]
- Sahebkar, A.; Simental-Mendía, L.E.; Giorgini, P.; Ferri, C.; Grassi, D. Lipid Profile Changes after Pomegranate Consumption: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phytomedicine 2016. [Google Scholar] [CrossRef] [PubMed]
- Al-Muammar, M.N.; Khan, F. Obesity: The Preventive Role of the Pomegranate (Punica Granatum). Nutrition 2012, 28, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Banihani, S.; Swedan, S.; Alguraan, Z. Pomegranate and Type 2 Diabetes. Nutr. Res. 2013, 33, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Asadi, M.S.; Mirghazanfari, S.M.; Dadpay, M. Evaluation of wound healing activities of pomegranate (Punica granatum-Lythraceae) Peel and Pulp. JRMDS 2018, 6, 230–236. [Google Scholar] [CrossRef]
- Morvaridzadeh, M.; Sepidarkish, M.; Daneshzad, E.; Akbari, A.; Mobini, G.R.; Heshmati, J. The Effect of Pomegranate on Oxidative Stress Parameters: A Systematic Review and Meta-Analysis. Complement. Ther. Med. 2020, 48, 102252. [Google Scholar] [CrossRef]
- Li, Y.; Guo, C.; Yang, J.; Wei, J.; Xu, J.; Cheng, S. Evaluation of Antioxidant Properties of Pomegranate Peel Extract in Comparison with Pomegranate Pulp Extract. Food Chem. 2006, 96, 254–260. [Google Scholar] [CrossRef]
- Acker, L.E.P. Antioxidant Activities of Pomegranate Fruit Extract and Its Anthocyanidins: Delphinidin, Cyanidin, and Pelargonidin. J. Agric. Food Chem. 2002, 50, 166–171. [Google Scholar]
- Ismail, T.; Sestili, P.; Akhtar, S. Pomegranate Peel and Fruit Extracts: A Review of Potential Anti-Inflammatory and Anti-Infective Effects. J. Ethnopharmacol. 2012, 143, 397–405. [Google Scholar] [CrossRef]
- Lansky, E.P.; Newman, R.A. Punica granatum (pomegranate) and its potential for prevention and treatment of inflammation and cancer. J. Ethnopharmacol. 2007, 109, 177–206. [Google Scholar] [CrossRef]
- Singh, B.; Singh, J.P. Antimicrobial Potential of Pomegranate Peel: A Review. Int. J. Food Sci. Technol. 2018, 1–7. [Google Scholar] [CrossRef]
- Wu, Y.; Zhu, C.; Zhang, Y.; Li, Y.; Sun, J. Immunomodulatory and Antioxidant Effects of Pomegranate Peel Polysaccharides on Immunosuppressed Mice. Int. J. Biol. Macromol. 2019, 137, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Thilakarathna, S.H.; Rupasinghe, H.P.V. Anti-Atherosclerotic Effects of Fruit Bioactive Compounds: A Review of Current Scientific Evidence. Can. J. Plant Sci. 2012. [Google Scholar] [CrossRef]
- Zhou, B.; Yi, H.; Tan, J.; Wu, Y.; Liu, G.; Qiu, Z. Anti-proliferative effects of polyphenols from pomegranate rind (Punica Granatum L.) on EJ bladder cancer cells via regulation of p53/miR-34a axis. Phytother. Res. 2015, 29, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Orgil, O.; Spector, L.; Holland, D.; Mahajna, J. The anti-proliferative and anti-androgenic activity of different pomegranate accessions. J. Funct. Foods 2016, 26, 517–528. [Google Scholar] [CrossRef]
- Braidy, N.; Selvaraju, S.; Essa, M.M.; Vaishnav, R.; Al-Adawi, S.; Al-Asmi, A.; Al-Senawi, H.; Abd, A.; Alobaidy, A.; Lakhtakia, R.; et al. Neuroprotective Effects of a Variety of Pomegranate Juice Extracts against MPTP-Induced Cytotoxicity and Oxidative Stress in Human Primary Neurons. Oxid. Med. Cell. Longev. 2013, 2013, 1–12. [Google Scholar] [CrossRef]
- Al Damen, L.; Stockton, A.; Al-Dujaili, E.A. Effects on Cognition of Berry, Pomegranate, Grape and Biophenols: A General Review. JPAD 2018, 5, 1–8. [Google Scholar]
- Amri, Z.; Ghorbel, A.; Turki, M.; Akrout, F.M.; Ayadi, F.; Elfeki, A. Effect of pomegranate extracts on brain antioxidant markers and cholinesterase activity in high fat-high fructose diet induced obesity in rat model. BMC Complement. Altern. Med. 2017, 1–9. [Google Scholar] [CrossRef]
- Morzelle, M.C.; Salgado, J.M.; Telles, M.; Mourelle, D.; Bachiega, P.; Buck, H.S.; Viel, T.A. Neuroprotective effects of pomegranate peel extract after chronic infusion with amyloid-β peptide in mice. PLoS ONE 2016, 11, e0141332. [Google Scholar] [CrossRef]
- Yuan, T.; Ma, H.; Liu, W.; Niesen, D.B.; Shah, N.; Crews, R.; Rose, K.N.; Vattem, D.A.; Seeram, N.P. Pomegranate’s neuroprotective effects against Alzheimer’s disease are mediated by urolithins, its ellagitannin-gut microbial derived metabolites. ACS Chem. Neurosci. 2015, 7, 26–33. [Google Scholar] [CrossRef]
- Subash, S.; Essa, M.M.; Asmi, A.; Al-Adawi, S.; Vaishnav, R.; Braidy, N.; Manivasagam, T.; Guillemin, G.J. Pomegranate from Oman Alleviates the Brain Oxidative Damage in Transgenic Mouse Model of Alzheimer’s Disease. J. Tradit. Complement. Med. 2014, 4, 232–238. [Google Scholar] [CrossRef]
- Ahmed, M.A.E.; El Morsy, E.M.; Ahmed, A.A. Pomegranate extract protects against cerebral ischemia/reperfusion injury and preserves brain DNA integrity in rats. Life Sci. 2014. [Google Scholar] [CrossRef] [PubMed]
- Sarkaki, A.; Farbood, Y.; Hashemi, S.; Rad, M.R. Pomegranate seed hydroalcoholic extract improves memory deficits in ovariectomized rats with permanent cerebral hypoperfusion/ischemia. Avicenna J. Phytomed. 2015, 5, 43–55. [Google Scholar] [PubMed]
- Alireza, S.; Moslem, R. Improving active and passive avoidance memories deficits due to permanent cerebral ischemia by pomegranate seed extract in female rats. Malays. J. Med Sci. 2013, 20, 25–34. [Google Scholar]
- Rafieirad, M.; Abbaszadeh, H. Pomegranate Seed Extract Reduces Ischemia Induced Anxiety in Male Rats. J. Herbmed Pharmacol. 2017, 6, 85–89. [Google Scholar]
- Bellone, J.A.; Murray, J.R.; Jorge, P.; Fogel, T.G.; Kim, M.; Wallace, D.R.; Hartman, R.E.; Bellone, J.A.; Murray, J.R.; Jorge, P.; et al. Pomegranate Supplementation Improves Cognitive and Functional Recovery Following Ischemic Stroke: A Randomized Trial. Nutr. Neurosci. 2019, 22, 738–743. [Google Scholar] [CrossRef]
- West, T.; Atzeva, M.; Holtzman, D.M. Pomegranate polyphenols and resveratrol protect the neonatal brain against hypoxic-ischemic injury. Dev. Neurosci. 2007, 29, 363–372. [Google Scholar] [CrossRef]
- Basu, A.; Penugonda, K. Pomegranate Juice: A Heart-Healthy Fruit Juice. Nutr. Rev. 2009, 67, 49–56. [Google Scholar] [CrossRef]
- Gil, I.; Toma, F.A.; Hess-pierce, B.; Holcroft, D.M.; Kader, A.A. Antioxidant activity of pomegranate juice and its relationship with phenolic composition and processing. J. Agric. Food Chem. 2000, 48, 4581–4589. [Google Scholar] [CrossRef]
- Teixeira da Silva, J.A.; Ng, T.B. The Medicinal and Pharmaceutical Importance of Dendrobium Species. Appl. Microbiol. Biotechnol. 2017, 101, 2227–2239. [Google Scholar] [CrossRef]
- Ng, T.B.; Liu, J.; Wong, J.H.; Ye, X.; Wing Sze, S.C.; Tong, Y.; Zhang, K.Y. Review of Research on Dendrobium, a Prized Folk Medicine. Appl. Microbiol. Biotechnol. 2012, 93, 1795–1803. [Google Scholar] [CrossRef]
- Tang, H.; Zhao, T.; Sheng, Y.; Zheng, T.; Fu, L.; Zhang, Y. Dendrobium Officinale Kimura et Migo: A Review on Its Ethnopharmacology, Phytochemistry, Pharmacology, and Industrialization. Evid. Based Complement. Altern. Med. 2017, 2017, 7436259. [Google Scholar] [CrossRef] [PubMed]
- Koo, K.A.; Sung, S.H.; Park, J.H.; Kim, S.H.; Lee, K.Y.; Kim, Y.C. In Vitro Neuroprotective Activities of Phenylethanoid Glycosides from Callicarpa Dichotoma. Planta Med. 2005, 71, 778–780. [Google Scholar] [CrossRef] [PubMed]
- Alipieva, K.; Korkina, L.; Erdogan, I.; Georgiev, M.I. Verbascoside—A review of its occurrence, (bio) synthesis and pharmacological significance. Biotechnol. Adv. 2014, 32, 1065–1076. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.; He, J.; Hu, X.; Zeng, Y.; Li, Y.; Wu, H.; Qiu, R.; Ma, W.; Li, T.; Li, C.; et al. Advanced Research on Acteoside for Chemistry and Bioactivities. J. Asian Nat. Prod. Res. 2011, 37–41. [Google Scholar] [CrossRef]
- Imperio, M.D.; Cardinali, A.; Antuono, I.D.; Linsalata, V.; Minervini, F.; Redan, B.W.; Ferruzzi, M.G. Stability—Activity of Verbascoside, a Known Antioxidant Compound, at Different PH Conditions. Food Res. Int. 2014, 66, 373–378. [Google Scholar] [CrossRef]
- Frum, Y.; Viljoen, A.M.; Van Heerden, F.R. Verbascoside and luteolin-5-o-β-d-glucoside isolated from Halleria lucida L. exhibit antagonistic anti-oxidant properties in vitro. S. Afr. J. Bot. 2007, 73, 583–587. [Google Scholar] [CrossRef][Green Version]
- Lee, J.H.; Lee, J.Y.; Kang, H.S.; Jeong, C.H.; Moon, H.; Whang, W.K.; Kim, C.J.; Sim, S.S. The Effect of Acteoside on Histamine Release and Arachidonic Acid Release in RBL-2H3 Mast Cells. Arch. Pharmacal Res. 2006, 29, 508–513. [Google Scholar] [CrossRef]
- Speranza, L.; Franceschelli, S.; Pesce, M.; Reale, M.; Menghini, L.; Vinciguerra, I.; De Lutiis, M.A.; Felaco, M.; Grilli, A. Antiinfl Ammatory Effects in THP-1 Cells Treated with Verbascoside. Phytother. Res. 2010, 1404, 1398–1404. [Google Scholar] [CrossRef]
- Pesce, M.; Franceschelli, S.; Ferrone, A.; Anna, M.; Lutiis, D.; Patruno, A.; Grilli, A.; Felaco, M.; Speranza, L. Verbascoside Down-Regulates Some pro-Inflammatory Signal Transduction Pathways by Increasing the Activity of Tyrosine Phosphatase SHP-1 in the U937 Cell Line. J. Cell. Mol. Med. 2015, 19, 1548–1556. [Google Scholar] [CrossRef]
- Hno, T.O.; Noue, M.I.; Gihara, Y.O.; Aracoglu, I.S. Antimetastatic Activity of Acteoside, a Phenylethanoid Glycoside. Biol. Pharm. Bull. 2002, 25, 666–668. [Google Scholar]
- Zhou, L.; Feng, Y.; Jin, Y.; Liu, X.; Sui, H.; Chai, N.; Chen, X.; Liu, N.; Ji, Q.; Wang, Y.; et al. Verbascoside Promotes Apoptosis by Regulating HIPK2-P53 Signaling in Human Colorectal Cancer. BMC Cancer 2014, 14, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Wang, J.; Ma, J.; Gu, Z.; Jiang, C.; Yu, L.; Fu, X. Neuroprotective Effects of Cistanches Herba Therapy on Patients with Moderate Alzheimer ’ s Disease. Evid. Based Complement. Altern. Med. 2015, 2015, 103985. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Huang, F.X.; Wang, J.; Shi, C.C.; Fang, G.Y. Protective Effect of Liquiritin on Corticosterone-Induced Neurotoxicity in Pc12 Cells. Trop. J. Pharm. Res. 2018, 17, 2013–2017. [Google Scholar] [CrossRef]
- Yuan, J.; Ren, J.; Wang, Y.; He, X.; Zhao, Y. Acteoside Binds to Caspase-3 and Exerts Neuroprotection in the Rotenone Rat Model of Parkinson’s Disease. PLoS ONE 2016, 11, e0162696. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Lu, M.; Lan, X.; Liu, N.; Wang, H.; Du, J.; Sun, T.; Li, Y.; Yu, J. Neuroprotective Effect of Verbascoside on Hypoxic-Ischemic Brain Damage in Neonatal Rat. Neurosci. Lett. 2019, 711, 134415. [Google Scholar] [CrossRef]
- Inda, B.D.; Ebnath, S.D.; Anik, R.B. Naturally Occurring Iridoids and Secoiridoids. An Updated Review, Part 4. Chem. Pharm. Bull. 2011, 59, 803–833. [Google Scholar]
- El-Naggar, L.J.; Beal, J.L. Iridoids. A review. J. Nat. Prod. 1980, 43, 649–707. [Google Scholar] [CrossRef]
- Chou, G.; Wang, Z.; Medica, C.M.; Park, Z.H. Iridoid glycosides from Gardenia jasminoides Ellis. Helv. Chim. Acta 2008, 91, 4–10. [Google Scholar]
- Shan, M.; Yu, S.; Yan, H.; Guo, S.; Xiao, W.; Wang, Z.; Zhang, L.; Ding, A.; Wu, Q.; Fong, S.; et al. A review on the phytochemistry, pharmacology, pharmacokinetics and toxicology of geniposide, a natural product. Molecules 2017, 22, 1689. [Google Scholar] [CrossRef]
- Li, F.; Li, W.; Li, X.; Li, F.; Zhang, L.; Wang, B.; Huang, G.; Guo, X.; Wan, L.; Liu, Y.; et al. Geniposide Attenuates Inflammatory Response by Suppressing P2Y14 Receptor and Downstream ERK1/2 Signaling Pathway in Oxygen and Glucose Deprivation-Induced Brain Microvascular Endothelial Cells. J. Ethnopharmacol. 2016, 185, 77–86. [Google Scholar] [CrossRef]
- Wang, J.; Hou, J.; Zhang, P. Geniposide Reduces Inflammatory Responses of Oxygen-Glucose Deprived Rat Microglial Cells via Inhibition of the TLR4 Signaling Pathway. Neurochem. Res. 2012, 2, 2235–22480. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Xia, Z.; Gao, X.; Yin, F.; Liu, J. Glucagon-like Peptide 1 Receptor Plays a Critical Role in Geniposide-Regulated Insulin Secretion in INS-1 Cells. Acta Pharmacol. Sin. 2011, 33, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yin, F.; Zheng, X.; Jing, J.; Hu, Y. Geniposide, a Novel Agonist for GLP-1 Receptor, Prevents PC12 Cells from Oxidative Damage via MAP Kinase Pathway. Neurochem. Int. 2007, 51, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, Y.; Li, L.; Hölscher, C. Neuroprotective Effects of Geniposide in the MPTP Mouse Model of Parkinson’s Disease. Eur. J. Pharmacol. 2015, 768, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhao, C.; Lv, C.; Liu, X.; Du, S.; Li, Z.; Wang, Y.; Zhang, W. Geniposide Alleviates Amyloid-Induced Synaptic Injury by Protecting Axonal Mitochondrial Trafficking. Front. Cell. Neurosci. 2017, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lv, C.; Wang, L.; Liu, X.; Yan, S.; Yan, S.S.; Wang, Y.; Zhang, W. Multi-Faced Neuroprotective Effects of Geniposide Depending on the RAGE-Mediated Signaling in an Alzheimer Mouse Model. Neuropharmacology 2015, 89, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, D.; Hou, J.; Lei, H. Protective Effects of Geniposide and Ginsenoside Rg1 Combination Treatment on Rats Following Cerebral Ischemia Are Mediated via Microglial MicroRNA-155-5p Inhibition. Mol. Med. Rep. 2018, 17, 3186–3193. [Google Scholar] [CrossRef]
- Pan, L.; Wang, W.; Shi, F.; Zhou, J.; Zhang, M.; Zhu, H.; Zeng, M. Exploratory Pharmacokinetics of Geniposide in Rat Model of Cerebral Ischemia Orally Administered with or without Baicalin and/or Berberine. Evid. Based Complement. Altern. Med. 2013, 2013, 349531. [Google Scholar] [CrossRef]
- Huang, B.; Chen, P.; Huang, L.; Li, S.; Zhu, R.; Sheng, T.; Yu, W.; Chen, Z.; Wang, T. Geniposide Attenuates Post-Ischaemic Neurovascular Damage via GluN2A/AKT/ ERK-Dependent Mechanism. Cell. Physiol. Biochem. 2017, 43, 705–716. [Google Scholar] [CrossRef]
- Liu, F.; Wang, Y.; Yao, W.; Xue, Y.; Zhou, J.; Liu, Z. Geniposide Attenuates Neonatal Mouse Brain Injury after Hypoxic-Ischemia Involving the Activation of PI3K/Akt Signaling Pathway. J. Chem. Neuroanat. 2019, 102, 54. [Google Scholar] [CrossRef]
- Wu, G.A.; Terol, J.; Ibanez, V.; López-García, A.; Pérez-Román, E.; Borredá, C.; Domingo, C.; Tadeo, F.R.; Carbonell-caballero, J.; Alonso, R.; et al. Genomics of the Origin and Evolution of Citrus. Nature 2018. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Garg, S.; Zaneveld, L.J.D.; Singla, A.K. Chemistry and Pharmacology of the Citrus Bioflavonoid Hesperidin. Phyther. Res. 2001, 15, 655–669. [Google Scholar] [CrossRef] [PubMed]
- Elavarasan, J.; Velusamy, P.; Ganesan, T.; Ramakrishnan, S.K.; Rajasekaran, D.; Periandavan, K. Hesperidin-Mediated Expression of Nrf2 and Upregulation of Antioxidant Status in Senescent Rat Heart. J. Pharm. Pharmacol. 2012, 64, 1472–1482. [Google Scholar] [CrossRef] [PubMed]
- Cho, J. Antioxidant and Neuroprotective Effects of Hesperidin and Its Aglycone Hesperetin. Arch. Pharmacal Res. 2006, 29, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Lorzadeh, E.; Ramezani-Jolfaie, N.; Mohammadi, M. The Effect of Hesperidin Supplementation on Inflammatory Markers in Human Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Clinical Trials. Chem. Biol. Interact. 2019, 307, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Dimpfel, W. Different Anticonvulsive Effects of Hesperidin and Its Aglycone Hesperetin on Electrical Activity in the Rat Hippocampus In-Vitro. J. Pharm. Pharmacol. 2006, 58, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Rainey-smith, S.; Schroetke, L.; Bahia, P.; Fahmi, A.; Skilton, R.; Spencer, J.P.E.; Rice-evans, C.; Rattray, M.; Williams, R.J. Neuroprotective effects of hesperetin in mouse primary neurones are independent of CREB activation. Neurosci. Lett. 2008, 438, 29–33. [Google Scholar] [CrossRef]
- Huang, S.; Tsai, S.; Lin, J.; Wu, C.; Yen, G. Cytoprotective Effects of Hesperetin and Hesperidin against Amyloid β-Induced Impairment of Glucose Transport through Downregulation of Neuronal Autophagy. Mol. Nutr. Food Res. 2012, 601–609. [Google Scholar] [CrossRef]
- Menze, E.T.; Tadros, M.G.; Abdel-tawab, A.M.; Khalifa, A.E. Potential Neuroprotective Effects of Hesperidin on 3-Nitropropionic Acid-Induced Neurotoxicity in Rats. Neurotoxicology 2012, 33, 1265–1275. [Google Scholar] [CrossRef]
- Kumar, P.; Kumar, A. Protective Effect of Hesperidin and Naringin against 3-Nitropropionic Acid Induced Huntington’s like Symptoms in Rats: Possible Role of Nitric Oxide. Behav. Brain Res. 2010, 206, 38–46. [Google Scholar] [CrossRef]
- Choi, E.J.; Ahn, W.S. Neuroprotective Effects of Chronic Hesperetin Administration in Mice. Arch. Pharmacal Res. 2008, 31, 1457–1462. [Google Scholar] [CrossRef] [PubMed]
- Donato, F.; de Gomes, M.G.; Goes, A.T.R.; Borges Filho, C.; Del Fabbro, L.; Antunes, M.S.; Souza, L.C.; Boeira, S.P.; Jesseb, C.R. Hesperidin Exerts Antidepressant-like Effects in Acute and Chronic Treatments in Mice: Possible Role of l-Arginine-NO-CGMP Pathway and BDNF Levels. Brain Res. Bull. 2014, 104, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Gaur, V.; Kumar, A. Hesperidin Pre-Treatment Attenuates NO-Mediated Cerebral Ischemic Reperfusion Injury and Memory Dysfunction. Pharmacol. Rep. 2010, 62, 635–648. [Google Scholar] [CrossRef]
- Rong, Z.; Pan, R.; Xu, Y.; Zhang, C.; Cao, Y.; Liu, D. Hesperidin pretreatment protects hypoxia—Ischemic brain injury in neonatal rat. Neuroscience 2013, 255, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Lakhanpal, P.; Rai, D.K. Quercetin: A versatile flavonoid. Internet J. Med. Update 2007, 2, 22–37. [Google Scholar] [CrossRef]
- Erden Inal, M.; Kahraman, A. The Protective Effect of Flavonol Quercetin against Ultraviolet a Induced Oxidative Stress in Rats. Toxicology 2000, 154, 21–29. [Google Scholar] [CrossRef]
- Shutenko, Z.; Henry, Y.; Pinard, E.; Seylaz, J.; Potier, P.; Berthet, F.; Girard, P.; Sercombe, R. Influence of the Antioxidant Quercetin in Vivo on the Level of Nitric Oxide Determined by Electron Paramagnetic Resonance in Rat Brain during Global Ischemia and Reperfusion. Biochem. Pharmacol. 1999, 57, 199–208. [Google Scholar] [CrossRef]
- Huk, I.; Brovkovych, V.; Nanobash Vili, J.; Weigel, G.; Neumayer, C.; Partyka, L.; Patton, S.; Malinski, T. Bioflavonoid Quercetin Scavenges Superoxide and Increases Nitric Oxide Concentration in Ischaemia-Reperfusion Injury: An Experimental Study. Br. J. Surg. 1998, 85, 1080–1085. [Google Scholar] [CrossRef]
- Du, G.; Zhao, Z.; Chen, Y.; Li, Z.; Tian, Y.; Liu, Z.; Liu, B.; Song, J. Quercetin Attenuates Neuronal Autophagy and Apoptosis in Rat Traumatic Brain Injury Model via Activation of PI3K/Akt Signaling Pathway. Neurol. Res. 2016, 38, 1012–1019. [Google Scholar] [CrossRef]
- Lei, X.; Chao, H.; Zhang, Z.; Lv, J.; Li, S.; Wei, H.; Xue, R.; Li, F.; Li, Z. Neuroprotective Effects of Quercetin in a Mouse Model of Brain Ischemic/Reperfusion Injury via Anti-Apoptotic Mechanisms Based on the Akt Pathway. Mol. Med. Rep. 2015, 12, 3688–3696. [Google Scholar] [CrossRef]
- Hwang, I.K.; Lee, C.H.; Yoo, K.Y.; Choi, J.H.; Park, O.K.; Lim, S.S.; Kang, I.J.; Kwon, D.Y.; Park, J.; Yi, J.S.; et al. Neuroprotective Effects of Onion Extract and Quercetin against Ischemic Neuronal Damage in the Gerbil Hippocampus. J. Med. Food 2009, 12, 990–995. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.Q.; Yao, R.Q.; Liu, X.; Huang, J.J.; Qi, D.S.; Yang, L.H. Quercetin Protects Oligodendrocyte Precursor Cells from Oxygen/Glucose Deprivation Injury in Vitro via the Activation of the PI3K/Akt Signaling Pathway. Brain Res. Bull. 2011, 86, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.H.; Choi, Y.H.; Moon, S.K.; Kim, W.J.; Kim, G.Y. Quercetin Inhibits Lipopolysaccharide-Induced Nitric Oxide Production in BV2 Microglial Cells by Suppressing the NF-κB Pathway and Activating the Nrf2-Dependent HO-1 Pathway. Int. Immunopharmacol. 2013, 17, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Yao, R.Q.; Qi, D.S.; Yu, H.L.; Liu, J.; Yang, L.H.; Wu, X.X. Quercetin Attenuates Cell Apoptosis in Focal Cerebral Ischemia Rat Brain via Activation of BDNF-TrkB-PI3K/Akt Signaling Pathway. Neurochem. Res. 2012, 37, 2777–2786. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.; Khan, M.M.; Hoda, M.N.; Raza, S.S.; Khan, M.B.; Javed, H.; Ishrat, T.; Ashafaq, M.; Ahmad, M.E.; Safhi, M.M.; et al. Quercetin Protects against Oxidative Stress Associated Damages in a Rat Model of Transient Focal Cerebral Ischemia and Reperfusion. Neurochem. Res. 2011, 36, 1360–1371. [Google Scholar] [CrossRef]
- Cho, J.Y.; Kim, I.S.; Jang, Y.H.; Kim, A.R.; Lee, S.R. Protective Effect of Quercetin, a Natural Flavonoid against Neuronal Damage after Transient Global Cerebral Ischemia. Neurosci. Lett. 2006, 404, 330–335. [Google Scholar] [CrossRef]
- Rivera, F.; Costa, G.; Abin, A.; Urbanavicius, J.; Arruti, C.; Casanova, G.; Dajas, F. Reduction of Ischemic Brain Damage and Increase of Glutathione by a Liposomal Preparation of Quercetin in Permanent Focal Ischemia in Rats. Neurotox. Res. 2008, 13, 105–114. [Google Scholar] [CrossRef]
- Ghosh, A.; Sarkar, S.; Mandal, A.K.; Das, N. Neuroprotective Role of Nanoencapsulated Quercetin in Combating Ischemia-Reperfusion Induced Neuronal Damage in Young and Aged Rats. PLoS ONE 2013, 8, e57735. [Google Scholar] [CrossRef]
- Qu, X.; Qi, D.; Dong, F.; Wang, B.; Guo, R.; Luo, M.; Yao, R. Quercetin Improves Hypoxia-Ischemia Induced Cognitive Deficits via Promoting Remyelination in Neonatal Rat. Brain Res. 2014, 1553, 31–40. [Google Scholar] [CrossRef]
- Wu, M.; Liu, F.; Guo, Q. Quercetin Attenuates Hypoxia-Ischemia Induced Brain Injury in Neonatal Rats by Inhibiting TLR4/NF-κB Signaling Pathway. Int. Immunopharmacol. 2019, 74, 105704. [Google Scholar] [CrossRef]
- Adrian, M.; Jeandet, P.; Douillet-Breuil, A.C.; Tesson, L.; Bessis, R. Stilbene Content of Mature Vitis Vinifera Berries in Response to UV-C Elicitation. J. Agric. Food Chem. 2000, 48, 6103–6105. [Google Scholar] [CrossRef] [PubMed]
- Roupe, K.A.; Remsberg, C.M.; Yáñez, J.A.; Davies, N.M. Pharmacometrics of Stilbenes: Seguing Towards the Clinic. Curr. Clin. Pharmacol. 2006, 1, 81–101. [Google Scholar] [CrossRef] [PubMed]
- Jeandet, P.; Clément, C.; Courot, E.; Cordelier, S. Modulation of Phytoalexin Biosynthesis in Engineered Plants for Disease Resistance. Int. J. Mol. Sci. 2013, 14, 14136–14170. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Fan, C.; Yu, L.; Yang, Y.; Jiang, S.; Ma, Z.; Hu, W.; Li, T.; Yang, Z.; Tian, T.; et al. Pterostilbene Exerts an Anti-Inflammatory Effect via Regulating Endoplasmic Reticulum Stress in Endothelial Cells. Cytokine 2016, 77, 88–97. [Google Scholar] [CrossRef] [PubMed]
- McCormack, D.; McFadden, D. A Review of Pterostilbene Antioxidant Activity and Disease Modification. Oxid. Med. Cell. Longev. 2013, 2013. [Google Scholar] [CrossRef]
- Remsberg, C.M.; Yáñez, J.A.; Ohgami, Y.; Vega-villa, K.R.; Rimando, A.M.; Davies, N.M. Pharmacometrics of Pterostilbene: Preclinical Pharmacokinetics and Metabolism, Anticancer, Antiinflammatory, Antioxidant and Analgesic Activity. Phytotherapy Res. 2008, 179, 169–179. [Google Scholar] [CrossRef]
- Hou, Y.; Xie, G.; Miao, F.; Ding, L.; Mou, Y.; Wang, L.; Su, G.; Chen, G.; Yang, J.; Wu, C. Pterostilbene Attenuates Lipopolysaccharide-Induced Learning and Memory Impairment Possibly via Inhibiting Microglia Activation and Protecting Neuronal Injury in Mice. Prog. Neuropsychopharmacol. Biol. Psychiatry 2014. [Google Scholar] [CrossRef]
- Chang, J.; Rimando, A.; Pallas, M.; Camins, A.; Porquet, D.; Reeves, J.; Shukitt-hale, B.; Smith, M.A.; Joseph, J.A.; Casadesus, G. Low-Dose Pterostilbene, but Not Resveratrol, Is a Potent Neuromodulator in Aging and Alzheimer’s Disease. NBA 2012, 33, 2062–2071. [Google Scholar] [CrossRef]
- Papers, O. Anxiolytic Action of Pterostilbene: Involvement of Hippocampal ERK Phosphorylation. Planta Med. 2013, 79, 723–730. [Google Scholar]
- Yang, Y.; Wang, J.; Li, Y.; Fan, C.; Jiang, S.; Zhao, L.; Di, S.; Xin, Z.; Wang, B.; Wu, G.; et al. HO-1 Signaling Activation by Pterostilbene Treatment Attenuates Mitochondrial Oxidative Damage Induced by Cerebral Ischemia Reperfusion Injury. Mol. Neurobiol. 2015. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, X.; Ma, A.; Zhang, Y.; Chen, Y.; Zhou, H.; Li, W.; Jin, X. Orally Administrated Pterostilbene Attenuates Acute Cerebral Ischemia—Reperfusion Injury in a Dose- and Time-Dependent Manner in Mice. Pharmacol. Biochem. Behav. 2015, 135, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Song, T.; Yang, L.; Wang, X.; Yang, C.; Jiang, Y. Neuroprotective Actions of Pterostilbene on Hypoxic-Ischemic Brain Damage in Neonatal Rats through Upregulation of Heme Oxygenase-1. Int. J. Dev. Neurosci. 2016, 54, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Liu, Y.E.; Cao, J.; Zeng, G.; Shen, C.; Zhou, M.; Chen, Y.; Pu, W.; Potters, L.; Shi, E.Y. Vitexins, nature-derived lignan compounds, induce apoptosis and suppress tumor growth. Clin. Cancer 2010, 15, 5161–5169. [Google Scholar] [CrossRef] [PubMed]
- Zucolotto, S.M.; Fagundes, C.; Reginatto, F.H.; Ramos, F.A.; Castellanos, L.; Duque, C.; Schenkel, E.P. Analysis of C-Glycosyl Flavonoids from South American Passiflora Species by HPLC-DAD and HPLC-MS. Phytochem. Anal. 2012, 23, 232–239. [Google Scholar] [CrossRef]
- Zhang, J.; Yuan, K.; Zhou, W.L.; Zhou, J.; Yang, P. Studies on the Active Components and Antioxidant Activities of the Extracts of Mimosa Pudica Linn. from Southern China. Pharmacogn. Mag. 2011, 7, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Moheb, A.; Ibrahim, R.K.; Roy, R.; Sarhan, F. Changes in Wheat Leaf Phenolome in Response to Cold Acclimation. Phytochemistry 2011, 72, 2294–2307. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.Y.; Liu, R.H.; Xu, X.D.; Yu, M.Q.; Zhang, Q.; Liu, H.L. The Pharmacokinetics of C-Glycosyl Flavones of Hawthorn Leaf Flavonoids in Rat after Single Dose Oral Administration. Phytomedicine 2010, 17, 640–645. [Google Scholar] [CrossRef]
- Zhou, J.; Hu, H.; Long, J.; Wan, F.; Li, L.; Zhang, S.; Shi, Y.E.; Chen, Y. Vitexin 6, a Novel Lignan, Induces Autophagy and Apoptosis by Activating the Jun N-Terminal Kinase Pathway. Anticancer Drugs 2013, 24, 928–936. [Google Scholar] [CrossRef]
- Li, Y.L.; Ma, S.C.; Yang, Y.T.; Ye, S.M.; But, P.P.H. Antiviral Activities of Flavonoids and Organic Acid from Trollius Chinensis Bunge. J. Ethnopharmacol. 2002, 79, 365–368. [Google Scholar] [CrossRef]
- Dong, L.; Fan, Y.; Shao, X.; Chen, Z. Vitexin Protects against Myocardial Ischemia/Reperfusion Injury in Langendorff-Perfused Rat Hearts by Attenuating Inflammatory Response and Apoptosis. Food Chem. Toxicol. 2011, 49, 3211–3216. [Google Scholar] [CrossRef]
- Dong, L.Y.; Li, S.; Zhen, Y.L.; Wang, Y.N.; Shao, X.; Luo, Z.G. Cardioprotection of Vitexin on Myocardial Ischemia/Reperfusion Injury in Rat via Regulating Inflammatory Cytokines and MAPK Pathway. Am. J. Chin. Med. 2013, 41, 1251–1266. [Google Scholar] [CrossRef] [PubMed]
- Can, Ö.D.; Demir Özkay, Ü.; Üçel, U.I. Anti-Depressant-like Effect of Vitexin in BALB/c Mice and Evidence for the Involvement of Monoaminergic Mechanisms. Eur. J. Pharmacol. 2013, 699, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, E.; Nassiri-Asl, M.; Shafeei, M.; Sheikhi, M. Neuroprotective Effects of Vitexin, a Flavonoid, on Pentylenetetrazole-Induced Seizure in Rats. Chem. Biol. Drug Des. 2012, 80, 274–278. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, E.; Nassiri-Asl, M.; Sheikhi, M.; Shafiee, M. Effects of Vitexin on Scopolamine-Induced Memory Impairment in Rats. Chin. J. Physiol. 2013, 56, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Yang, Z.M.; Zhang, N.; Tian, Z.; Liu, S.B.; Zhao, M.G. Neuroprotective Effects of Vitexin by Inhibition of NMDA Receptors in Primary Cultures of Mouse Cerebral Cortical Neurons. Mol. Cell. Biochem. 2014, 386, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhen, Y.; Wu, X.; Jiang, Q.; Li, X.; Chen, Z.; Zhang, G.; Dong, L. Vitexin Protects Brain against Ischemia/Reperfusion Injury via Modulating Mitogen-Activated Protein Kinase and Apoptosis Signaling in Mice. Phytomedicine 2015, 22, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.J.; Eun, J.S.; Kim, B.G.; Kim, S.Y.; Jeon, H.; Soh, Y. Vitexin, an HIF-1α Inhibitor, Has Anti-Metastatic Potential in PC12 cells. Mol. Cells 2006, 22, 291–299. [Google Scholar]
- Min, J.W.; Hu, J.J.; He, M.; Sanchez, R.M.; Huang, W.X.; Liu, Y.Q.; Bsoul, N.B.; Han, S.; Yin, J.; Liu, W.H.; et al. Vitexin Reduces Hypoxia-Ischemia Neonatal Brain Injury by the Inhibition of HIF-1alpha in a Rat Pup Model. Neuropharmacology 2015, 99, 38–50. [Google Scholar] [CrossRef]
- Funaya, N.; Haginaka, J. Matrine- and Oxymatrine-Imprinted Monodisperse Polymers Prepared by Precipitation Polymerization and Their Applications for the Selective Extraction of Matrine-Type Alkaloids from Sophora Flavescens Aiton. J. Chromatogr. A 2012, 1248, 18–23. [Google Scholar] [CrossRef]
- Guzman, J.R.; Koo, J.S.; Goldsmith, J.R.; Mühlbauer, M.; Narula, A.; Jobin, C. Oxymatrine Prevents NF-ΚB Nuclear Translocation and Ameliorates Acute Intestinal Inflammation. Sci. Rep. 2013, 3, 1–9. [Google Scholar] [CrossRef]
- Wang, S.; Jia, J. Oxymatrine Attenuates Diabetes-Associated Cognitive Deficits in Rats. Acta Pharmacol. Sin. 2014, 35, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.J.; Li, Q.; Wang, J.B.; Zhao, Y.L.; Zhong, Y.W.; Bai, Y.F.; Wang, R.L.; Li, J.Y.; Yang, H.Y.; Zeng, L.N.; et al. Combining Oxymatrine or Matrine with Lamivudine Increased Its Antireplication Effect against the Hepatitis B Virus in Vitro. Evid. Based Complement. Altern. Med. 2013, 2013, 186573. [Google Scholar] [CrossRef] [PubMed]
- Papers, O. Protective Effects of Oxymatrine on Experimental Diabetic Nephropathy. Planta Med. 2014, 80, 269–276. [Google Scholar]
- Chai, N.L.; Fu, Q.; Shi, H.; Cai, C.H.; Wan, J.; Xu, S.P.; Wu, B.Y. Oxymatrine Liposome Attenuates Hepatic Fibrosis via Targeting Hepatic Stellate Cells. World J. Gastroenterol. 2012, 18, 4199–4206. [Google Scholar] [CrossRef]
- Xiao, T.; Wang, Y.; Zhang, Y.; Bai, C.; Shen, X. Similar to Spironolactone, Oxymatrine Is Protective in Aldosterone-Induced Cardiomyocyte Injury via Inhibition of Calpain and Apoptosis-Inducing Factor Signaling. PLoS ONE 2014, 9, e88856. [Google Scholar] [CrossRef]
- Zhang, X.; Jiang, W.; Zhou, A.L.; Zhao, M.; Jiang, D.R. Inhibitory Effect of Oxymatrine on Hepatocyte Apoptosis via TLR4/PI3K/Akt/GSK-3β Signaling Pathway. World J. Gastroenterol. 2017, 23, 3839–3849. [Google Scholar] [CrossRef]
- Liu, Y.; Xu, Y.; Ji, W.; Li, X.; Sun, B.; Gao, Q.; Su, C. Anti-Tumor Activities of Matrine and Oxymatrine: Literature Review. Tumor Biol. 2014. [Google Scholar] [CrossRef]
- Ying, X.J.; Jin, B.; Chen, X.W.; Xie, J.; Xu, H.M.; Dong, P. Oxymatrine Downregulates HPV16E7 Expression and Inhibits Cell Proliferation in Laryngeal Squamous Cell Carcinoma Hep-2 Cells in Vitro. Biomed Res. Int. 2015, 2015, 150390. [Google Scholar] [CrossRef]
- Dong, X.; Du, Q.; Yu, W.; Zhang, Z.; Zhu, Q.; Che, Z.; Chen, F.; Wang, H.; Chen, J. Anti-inflammatory effects of oxymatrine through inhibition of nuclear factor–kappa b and mitogen-activated protein kinase activation in lipopolysaccharide-induced BV2 microglia cells. Iran. J. Pharm. Res. 2013, 12, 165–174. [Google Scholar]
- Dong, X.-Q.; Yu, W.-H.; Hu, Y.-Y.; Zhang, Z.-Y.; Huang, M. Oxymatrine Reduces Neuronal Cell Apoptosis by Inhibiting Toll-like Receptor 4/Nuclear Factor Kappa-B-Dependent Inflammatory Responses in Traumatic Rat Brain Injury. Inflamm. Res. 2011, 533–539. [Google Scholar] [CrossRef]
- Cui, L.; Zhang, X.; Yang, R.; Wang, L.; Liu, L.; Li, M.; Du, W. Neuroprotection and Underlying Mechanisms of Oxymatrine in Cerebral Ischemia of Rats. Neurol. Res. 2011, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.H.; Shao, L.; Zhu, G.J. Oxymatrine Attenuates Brain Hypoxic-Ischemic Injury from Apoptosis and Oxidative Stress: Role of p-Akt/GSK3β/HO-1/Nrf-2 Signaling Pathway. Metab. Brain Dis. 2018, 33, 1869–1875. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Zhou, R.; Li, H.N.; Yao, W.X.; Qiao, H.Q.; Wang, S.J.; Niu, Y.; Sun, T.; Li, Y.X.; Yu, J.Q. Oxymatrine Attenuated Hypoxic-Ischemic Brain Damage in Neonatal Rats via Improving Antioxidant Enzyme Activities and Inhibiting Cell Death. Neurochem. Int. 2015, 89, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, H.; Liu, N.; Du, J.; Lan, X.; Qi, X.; Zhuang, C.; Sun, T.; Li, Y.; Yu, J. Oxymatrine Protects Neonatal Rat against Hypoxic-Ischemic Brain Damage via PI3K/Akt/GSK3β Pathway. Life Sci. 2020, 254. [Google Scholar] [CrossRef] [PubMed]
- Inagaki, T.; Etgen, A.M. Neuroprotective Action of Acute Estrogens: Animal Models of Brain Ischemia and Clinical Implications. Steroids 2013, 78, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Ibarreta, D.; Daxenberger, A.; Meyer, H.H. Possible health impact of phytoestrogens and xenoestrogens in food. Apmis 2001, 109, S402–S425. [Google Scholar] [CrossRef]
- Cornwell, T.; Cohick, W.; Raskin, I. Dietary phytoestrogens and health. Phytochemistry 2004, 65, 995–1016. [Google Scholar] [CrossRef]
- Stahl, S.; Chun, T.; Gray, W.G. Phytoestrogens Act as Estrogen Agonists in an Estrogen-Responsive Pituitary Cell Line. Toxicol. Appl. Pharmacol. 1998, 48, 41–48. [Google Scholar] [CrossRef]
- Zhao, L.; Chen, Q.; Brinton, R.D. Neuroprotective and Neurotrophic Efficacy of Phytoestrogens in Cultured Hippocampal Neurons. Exp. Biol. Med. 2002, 227, 509–519. [Google Scholar] [CrossRef]
- Chandsawangbhuwana, C.; Baker, M.E. 3D Models of Human ER α and ER β Complexed with Coumestrol. Steroids 2014, 80, 37–43. [Google Scholar] [CrossRef]
- Jung, E.; Zuly, L.; Kwang, J.; Seo, H.; Baeg, G.; Young, N.; Kang, G.; Ryong, T. Mass Production of Coumestrol from Soybean (Glycine Max) Adventitious Roots through Bioreactor: Effect on Collagen Production. Plant Biotechnol. Rep. 2019. [Google Scholar] [CrossRef]
- Stopper, H.; Schmitt, E.; Kobras, K. Genotoxicity of Phytoestrogens. Mutat. Res. Fundam. Mol. Mech. Mutagen. 2005, 574, 139–155. [Google Scholar] [CrossRef] [PubMed]
- Yuk, H.J.; Lee, J.H.; Curtis-Long, M.J.; Lee, J.W.; Kim, Y.S.; Ryu, H.W.; Park, C.G.; Jeong, T.S.; Park, K.H. The Most Abundant Polyphenol of Soy Leaves, Coumestrol, Displays Potent $α$-Glucosidase Inhibitory Activity. Food Chem. 2011, 126, 1057–1063. [Google Scholar] [CrossRef]
- You, J.S.; Cho, I.A.; Kang, K.R.; Oh, J.S.; Yu, S.J.; Lee, G.J.; Seo, Y.S.; Kim, S.G.; Kim, C.S.; Kim, D.K.; et al. Coumestrol Counteracts Interleukin-1β-Induced Catabolic Effects by Suppressing Inflammation in Primary Rat Chondrocytes. Inflammation 2017, 40, 79–91. [Google Scholar] [CrossRef]
- Jang, Y.J.; Son, H.J.; Ahn, J.; Jung, C.H.; Ha, T. Coumestrol Modulates Akt and Wnt/β-Catenin Signaling during the Attenuation of Adipogenesis. Food Funct. 2016, 7, 4984–4991. [Google Scholar] [CrossRef]
- Park, G.; Baek, S.; Kim, J.E.; Lim, T.G.; Lee, C.C.; Yang, H.; Kang, Y.G.; Park, J.S.; Augustin, M.; Mrosek, M.; et al. Flt3 Is a Target of Coumestrol in Protecting against UVB-Induced Skin Photoaging. Biochem. Pharmacol. 2015, 98, 473–483. [Google Scholar] [CrossRef]
- Lim, W.; Jeong, M.; Bazer, F.W.; Song, G. Coumestrol Inhibits Proliferation and Migration of Prostate Cancer Cells by Regulating AKT, ERK1/2, and JNK MAPK Cell Signaling Cascades. J. Cell. Physiol. 2017, 232, 862–871. [Google Scholar] [CrossRef]
- Zafar, A.; Singh, S.; Naseem, I. Cu(II)-Coumestrol Interaction Leads to ROS-Mediated DNA Damage and Cell Death: A Putative Mechanism for Anticancer Activity. J. Nutr. Biochem. 2016, 33, 15–27. [Google Scholar] [CrossRef]
- Lee, Y.H.; Yuk, H.J.; Park, K.H.; Bae, Y.S. Coumestrol Induces Senescence through Protein Kinase CKII Inhibition-Mediated Reactive Oxygen Species Production in Human Breast Cancer and Colon Cancer Cells. Food Chem. 2013, 141, 381–388. [Google Scholar] [CrossRef]
- Koirala, P.; Seong, S.H.; Jung, H.A.; Choi, J.S. Comparative Evaluation of the Antioxidant and Anti-Alzheimer’s Disease Potential of Coumestrol and Puerarol Isolated from Pueraria Lobata Using Molecular Modeling Studies. Molecules 2018, 23, 785. [Google Scholar] [CrossRef]
- Liu, M.; Tsuang, F.; Sheu, S.; Sun, J. The Protective Effects of Coumestrol against Lipopolysaccharide-Induced Toxicity on Mice Astrocytes. Neurol. Res. 2011, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Canal Castro, C.; Pagnussat, A.S.; Orlandi, L.; Worm, P.; Moura, N.; Etgen, A.M.; Alexandre Netto, C. Coumestrol Has Neuroprotective Effects before and after Global Cerebral Ischemia in Female Rats. Brain Res. 2012, 1474, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Castro, C.C.; Pagnussat, A.S.; Moura, N.; da Cunha, M.J.; Machado, F.R.; Wyse, A.T.S.; Netto, C.A. Coumestrol Treatment Prevents Na+, K+-ATPase Inhibition and Affords Histological Neuroprotection to Male Rats Receiving Cerebral Global Ischemia. Neurol. Res. 2014, 36, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Beatriz, J.; Anastacio, R.; Farias, E.; Nicola, F.; Odorcyk, F.; Bandeira, R.; Alexandre, C.; Biochemistry, P.P.; Federal, U.; Ufrgs, S.; et al. Phytoestrogen Coumestrol Attenuates Brain Mitochondrial Dysfunction and Long-Term Cognitive Deficits Following Neonatal Hypoxia—Ischemia. Int. J. Dev. Neurosci. 2019, 79, 86–95. [Google Scholar] [CrossRef]
- Mubarakshina, M.M.; Ivanov, B.N. The Production and Scavenging of Reactive Oxygen Species in the Plastoquinone Pool of Chloroplast Thylakoid Membranes. Physiol. Plant. 2010, 140, 103–110. [Google Scholar] [CrossRef]
- Borisova-Mubarakshina, M.M.; Vetoshkina, D.V.; Ivanov, B.N. Antioxidant and Signaling Functions of the Plastoquinone Pool in Higher Plants. Physiol. Plant 2019, 166, 181–198. [Google Scholar] [CrossRef]
- Amesz, J. The function of plastoquinone in photosynthetic electron transport. Biochim. Biophys. Acta. 1973, 301, 35–51. [Google Scholar] [CrossRef]
- Ivanov, B.; Khorobrykh, S. Participation of photosynthetic electron transport in production and scavenging of reactive oxygen species. Antioxid. Redox Signal. 2003, 5, 43–53. [Google Scholar] [CrossRef]
- Skulachev, V.P. A biochemical approach to the problem of aging: “megaproject” on membrane-penetrating ions. The first results and prospects. Biochemistry 2007, 72, 1385–1396. [Google Scholar] [CrossRef]
- Bakeeva, L.E.; Barskov, I.V.; Egorov, M.V.; Isaev, N.K.; Kapelko, V.I.; Kazachenko, A.V.; Kirpatovsky, V.I.; Kozlovsky, S.V.; Lakomkin, V.L.; Levina, S.B.; et al. Mitochondria Targeted Plastoquinone Derivatives as Tools to Interrupt Execution of the Aging Program. 2. Treatment of Some ROS and Age Related Diseases (Heart Arrhythmia, Heart Infarctions, Kidney Ischemia, and Stroke). Biochemistry 2008, 73, 1288–1299. [Google Scholar] [CrossRef]
- Jankauskas, S.S.; Andrianova, N.V.; Alieva, I.B.; Prusov, A.N.; Matsievsky, D.D.; Zorova, L.D.; Pevzner, I.B.; Savchenko, E.S.; Pirogov, Y.A.; Silachev, D.N.; et al. Dysfunction of Kidney Endothelium after Ischemia / Reperfusion and Its Prevention by Mitochondria Targeted Antioxidant. Biochemistry 2016, 81, 1538–1548. [Google Scholar] [CrossRef] [PubMed]
- Plotnikov, E.Y.; Chupyrkina, A.A.; Jankauskas, S.S.; Pevzner, I.B.; Silachev, D.N.; Skulachev, V.P.; Zorov, D.B. Biochimica et Biophysica Acta Mechanisms of Nephroprotective Effect of Mitochondria-Targeted Antioxidants under Rhabdomyolysis and Ischemia/Reperfusion. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2011, 1812, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Neroev, V.V.; Archipova, M.M.; Bakeeva, L.E.; Fursova, A.Z.; Grigorian, E.N.; Grishanova, A.Y.; Iomdina, E.N.; Ivashchenko, Z.N.; Katargina, L.A.; Maslova, I.P.K.; et al. Mitochondria Targeted Plastoquinone Derivatives as Tools to Interrupt Execution of the Aging Program. 4. Age Related Eye Disease. SkQ1 Returns Vision to Blind Animals. Biochemistry 2008, 73, 1317–1328. [Google Scholar] [CrossRef] [PubMed]
- Isaev, N.K.; Novikova, S.V.; Stelmashook, E.V.; Barskov, I.V.; Silachev, D.N.; Khaspekov, L.G.; Skulachev, V.P.; Zorov, D.B. Mitochondria Targeted Plastoquinone Antioxidant SkQR1 Decreases Trauma Induced Neurological Deficit in Rat. Biochemistry 2012, 77, 996–999. [Google Scholar] [CrossRef]
- Silachev, D.N.; Isaev, N.K.; Pevzner, I.B.; Zorova, L.D. The Mitochondria-Targeted Antioxidants and Remote Kidney Preconditioning Ameliorate Brain Damage through Kidney-to-Brain Cross-Talk. PLoS ONE 2012, 7, e51553. [Google Scholar] [CrossRef]
- Plotnikov, E.Y.; Silachev, D.N.; Chupyrkina, A.A.; Danshina, M.I.; Jankauskas, S.S.; Morosanova, M.A.; Stelmashook, E.V.; Vasileva, A.K.; Goryacheva, E.S.; Pirogov, Y.A.; et al. New Generation Skulachev Ions Exhibiting Nephroprotective and Neuroprotective Properties. Biochemistry 2010, 75, 145–150. [Google Scholar] [CrossRef]
- Ischemic, H.; Injury, B.; Silachev, D.N.; Plotnikov, E.Y.; Pevzner, I.B.; Zorova, L.D.; Balakireva, A.V.; Id, M.V.G.; Pirogov, Y.A.; Skulachev, V.P.; et al. Neuroprotective effects of mitochondria-targeted plastoquinone and thymoquinone in a rat model of brain ischemia/reperfusion injury. Molecules 2015, 20, 14487–14503. [Google Scholar] [CrossRef]
- Akinwumi, B.C.; Bordun, K.M.; Anderson, H.D. Biological Activities of Stilbenoids. Int. J. Mol. Sci. 2018, 19, 792. [Google Scholar] [CrossRef]
- Fernández-Mar, M.I.; Mateos, R.; García-parrilla, M.C.; Puertas, B.; Cantos-Villar, E. Bioactive Compounds in Wine: Resveratrol, Hydroxytyrosol and Melatonin: A Review. Food Chem. 2012, 130, 797–813. [Google Scholar] [CrossRef]
- Sovak, M. Grape Extract, Resveratrol, and Its Analogs: A Review. J. Med. Food 2001, 4, 93–105. [Google Scholar] [CrossRef]
- Smoliga, J.M.; Baur, J.A.; Hausenblas, H.A. Resveratrol and Health—A Comprehensive Review of Human Clinical Trials. Mol. Nutr. Food Res. 2011, 1129–1141. [Google Scholar] [CrossRef] [PubMed]
- Cottart, C.H.; Nivet-Antoine, V.; Beaudeux, J.L. Review of Recent Data on the Metabolism, Biological Effects, and Toxicity of Resveratrol in Humans. Mol. Nutr. Food Res. 2014, 58, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Rauf, A.; Imran, M.; Sulera, H.A.R.; Ahmad, B.; Peters, D.G.; Mubarak, M.S. A Comprehensive Review of the Health Perspectives of Resveratrol. Food Funct. 2017, 8, 4284–4305. [Google Scholar] [CrossRef] [PubMed]
- Savouret, J.F.; Quesne, M. Resveratrol and Cancer: A Review. Biomed. Pharmacother. 2002, 56, 84–87. [Google Scholar] [CrossRef]
- Meng, T.; Xiao, D.; Muhammed, A.; Deng, J.; Chen, L.; He, J. Anti-Inflammatory Action and Mechanisms of Resveratrol. Molecules 2021, 26, 229. [Google Scholar] [CrossRef]
- Neves, A.R.; Lucio, M.; LC Lima, J.; Reis, S. Resveratrol in Medicinal Chemistry: A Critical Review of Its Pharmacokinetics, Drug-Delivery, and Membrane Interactions. Curr. Med. Chem. 2012, 19, 1663–1681. [Google Scholar] [CrossRef]
- Albani, D.; Polito, L.; Signorini, A.; Forloni, G. Neuroprotective Properties of Resveratrol in Different Neurodegenerative Disorders. BioFactors 2010, 36, 370–376. [Google Scholar] [CrossRef]
- Bastianetto, S.; Ménard, C.; Quirion, R. Neuroprotective Action of Resveratrol. Biochim. Biophys. BBA Acta Mol. Basis Dis. 2015, 1852, 1195–1201. [Google Scholar] [CrossRef]
- Richard, T.; Victor, U.; Bordeau, S.; Waffo-téguo, P.; Richard, T.; Pawlus, A.D.; Igl, M.; Pedrot, E.; Waffo-teguo, P. Neuroprotective Properties of Resveratrol and Derivatives Neuroprotective Properties of Resveratrol and Derivatives. Ann. N.Y. Acad. Sci. 2011. [Google Scholar] [CrossRef]
- Tellone, E.; Galtieri, A.; Russo, A.; Giardina, B.; Ficarra, S. Resveratrol: A Focus on Several Neurodegenerative Diseases. Oxid. Med. Cell. Longev. 2015, 2015, 392169. [Google Scholar] [CrossRef]
- Pallàs, M.; Casadesús, G.; Smith, M.A.; Coto-montes, A.; Pelegri, C.; Vilaplana, J.; Camins, A. Resveratrol and Neurodegenerative Diseases: Activation of SIRT1 as the Potential Pathway towards Neuroprotection. Curr. Neurovasc. Res. 2009, 6, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Granados-Soto, V. Resveratrol: A Natural Compound with Pharmacological Potential in Neurodegenerative Diseases. CNS Neurosci. Ther. 2008, 14, 14–234. [Google Scholar] [CrossRef]
- Rege, S.D.; Geetha, T.; Griffin, G.D.; Broderick, T.L.; Babu, J.R. Neuroprotective Effects of Resveratrol in Alzheimer Disease Pathology. Front. Aging Neurosci. 2014, 6, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Gomes, Q.; Alexandre, B.; Paulo, J.; Silva, B.; Fernanda, C.; Romeiro, R.; Monteiro, S.; Rodrigues, C.A.; Gonçalves, P.R.; Sakai, J.T.; et al. Neuroprotective Mechanisms of Resveratrol in Alzheimer’s Disease: Role of SIRT1. Oxid. Med. Cell. Longev. 2018, 2018, 8152373. [Google Scholar] [CrossRef]
- Singh, N.; Agrawal, M.; Dore, S. Neuroprotective Properties and Mechanisms of Resveratrol in in Vitro and in Vivo Experimental Cerebral Stroke Models. ACS Chem. Neurosci. 2013, 4, 1151–1162. [Google Scholar] [CrossRef]
- Lopez, M.S.; Dempsey, R.J.; Vemuganti, R. Resveratrol Neuroprotection in Stroke and Traumatic CNS Injury. Neurochem. Int. 2015. [Google Scholar] [CrossRef]
- Dave, K.R.; Fazio, R.A.D.E.; Bao, Y.C.; Raval, A.P. Resveratrol pretreatment protects rat brain from cerebral ischemic damage via a sirtuin 1—Uncoupling protein 2 pathway. Neuroscience 2009, 159, 993–1002. [Google Scholar] [CrossRef]
- Dong, W.; Li, N.; Gao, D.; Zhen, H. Resveratrol Attenuates Ischemic Brain Damage in the Delayed Phase after Stroke and Induces Messenger RNA and Protein Express for Angiogenic Factors. J. Vasc. Surg. 2008, 48, 709–714. [Google Scholar] [CrossRef]
- Lei, J.R.; Tu, X.K.; Wang, Y.; Tu, D.W.; Shi, S.S. Resveratrol Downregulates the TLR4 Signaling Pathway to Reduce Brain Damage in a Rat Model of Focal Cerebral Ischemia. Exp. Ther. Med. 2019, 3215–3221. [Google Scholar] [CrossRef]
- Suo, S.; Cheng, M.; Lien, C. Resveratrol Reduction of Infarct Size in Long-Evans Rats Subjected to Focal Cerebral Ischemia. Life Sci. 2001, 69, 1057–1065. [Google Scholar]
- Li, Z.; Pang, L.; Fang, F.; Zhang, G.; Zhang, J.; Xie, M.; Wang, L. Resveratrol Attenuates Brain Damage in a Rat Model of Focal Cerebral Ischemia via Up-Regulation of Hippocampal Bcl-2. Brain Res. 2012, 1450, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Lee, H.; Lee, S. Protective effect of resveratrol against neuronal damage following transient global cerebral ischemia in mice. J. Nutr. Biochem. 2015. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Xu, J.; Rottinghaus, G.E.; Simonyi, A.; Lubahn, D.; Sun, G.Y.; Sun, A.Y. Resveratrol protects against global cerebral ischemic injury in gerbils. Brain Res. 2002, 958, 439–447. [Google Scholar] [CrossRef]
- Gao, D.; Zhang, X.; Jiang, X.; Peng, Y.; Huang, W.; Cheng, G.; Song, L. Resveratrol Reduces the Elevated Level of MMP-9 Induced by Cerebral Ischemia—Reperfusion in Mice. Life Sci. 2006, 78, 2564–2570. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Li, Z.; Wang, Y.; Hou, Y.; Li, L.; Zhao, J. Resveratrol Alleviates Cerebral Ischemia/Reperfusion Injury in Rats by Inhibiting NLRP3 Inflammasome Activation through Sirt1-Dependent Autophagy Induction. Int. Immunopharmacol. 2017, 50, 208–215. [Google Scholar] [CrossRef]
- Kizmazoglu, C.; Aydin, H.E.; Sevin, I.E.; Kalemci, O.; Yuceer, N.; Atasoy, M.A. Neuroprotective Effect of Resveratrol on Acute Brain Ischemia Reperfusion Injury by Measuring Annexin V, P53, Bcl-2 Levels in Rats. J. Korean Neurosurg. Soc. 2015, 58, 508–512. [Google Scholar] [CrossRef]
- Abdel-Aleem, G.A.; Khaleel, E.F.; Mostafa, D.G.; Elberier, L.K. Neuroprotective effect of resveratrol against brain ischemia reperfusion injury in rats entails reduction of DJ-1 protein expression and activation of PI3K/Akt/GSK3b survival pathway. Arch. Physiol. Biochem. 2016, 3455. [Google Scholar] [CrossRef]
- Kovacic, P.; Somanathan, R. Multifaceted Approach to Resveratrol Bioactivity Focus on Antioxidant Action, Cell Signaling and Safety. Oxid. Med. Cell. Longev. 2010, 3, 86–100. [Google Scholar] [CrossRef]
- Science, F. Neuroprotective Effects of Resveratrol on Cerebral Ischemia-Induced Neuron Loss Mediated by Free Radical Scavenging and Cerebral Blood Flow Elevation. J. Agric. Food Chem. 2006, 54, 3126–3131. [Google Scholar]
- Poulsen, M.M.; Fjeldborg, K.; Ornstrup, M.J.; Kjær, T.N.; Nøhr, M.K.; Pedersen, S.B. Resveratrol and Inflammation: Challenges in Translating Pre-Clinical Fi Ndings to Improved Patient Outcomes. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2015. [Google Scholar] [CrossRef]
- Zhang, F.; Liu, J.; Shi, J. Anti-Inflammatory Activities of Resveratrol in the Brain: Role of Resveratrol in Microglial Activation. Eur. J. Pharmacol. 2010, 636, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Fulda, S.; Debatin, K.M. Resveratrol Modulation of Signal Transduction in Apoptosis and Cell Survival: A Mini-Review. Cancer Detect. Prev. 2006, 30, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.Y.; Seo, M.A.; Choi, E.J.; Kim, J.K.; Seo, E.S.; Lee, J.H.; Chung, H.L.; Kim, W.T. Neuroprotective effects of resveratrol via anti-apoptosis on hypoxic-ischemic brain injury in neonatal rats. Korean J. Pediatr. 2008, 51, 1102–1111. [Google Scholar] [CrossRef]
- Karalis, F.; Soubasi, V.; Georgiou, T.; Nakas, C.T.; Simeonidou, C.; Guiba-Tziampiri, O.; Spandou, E. Resveratrol Ameliorates Hypoxia/Ischemia-Induced Behavioral Deficits and Brain Injury in the Neonatal Rat Brain. Brain Res. 2011, 1425, 98–110. [Google Scholar] [CrossRef] [PubMed]
- Arteaga, O.; Revuelta, M.; Urigüen, L.; Álvarez, A.; Montalvo, H.; Hilario, E. Pretreatment with Resveratrol Prevents Neuronal Injury and Cognitive Deficits Induced by Perinatal Hypoxia-Ischemia in Rats. PLoS ONE 2015, 10, e0142424. [Google Scholar] [CrossRef] [PubMed]
- Pan, S.; Li, S.; Hu, Y.; Zhang, H.; Liu, Y.; Jiang, H.; Fang, M.; Li, Z.; Xu, K.; Zhang, H.; et al. Resveratrol Post-Treatment Protects against Neonatal Brain Injury after Hypoxia-Ischemia. Oncotarget 2016, 7, 79247–79261. [Google Scholar] [CrossRef] [PubMed]
- Le, K.; Chibaatar Daliv, E.; Wu, S.; Qian, F.; Ali, A.I.; Yu, D.; Guo, Y. SIRT1-Regulated HMGB1 Release Is Partially Involved in TLR4 Signal Transduction: A Possible Anti-Neuroinflammatory Mechanism of Resveratrol in Neonatal Hypoxic-Ischemic Brain Injury. Int. Immunopharmacol. 2019, 75, 105779. [Google Scholar] [CrossRef]
- Matsui, Y.; Sugiyama, K.; Kamei, M.; Takahashi, T.; Suzuki, T.; Katagata, Y.; Ito, T. Extract of Passion Fruit (Passiflora Edulis) Seed Containing High Amounts of Piceatannol Inhibits Melanogenesis and Promotes Collagen Synthesis. J. Agric. Food Chem. 2010, 58, 11112–11118. [Google Scholar] [CrossRef]
- Rodríguez-Cabo, T.; Rodríguez, I.; López, P.; Ramil, M.; Cela, R. Investigation of Liquid Chromatography Quadrupole Time-of-Flight Mass Spectrometry Performance for Identification and Determination of Hydroxylated Stilbene Antioxidants in Wine. J. Chromatogr. A 2014, 1337, 162–170. [Google Scholar] [CrossRef]
- Rossi, M.; Caruso, F.; Opazo, C.; Salciccioli, J. Crystal and Molecular Structure of Piceatannol; Scavenging Features of Resveratrol and Piceatannol on Hydroxyl and Peroxyl Radicals and Docking with Transthyretin. J. Agric. Food Chem. 2008, 56, 10557–10566. [Google Scholar] [CrossRef]
- Murias, M.; Jäger, W.; Handler, N.; Erker, T.; Horvath, Z.; Szekeres, T.; Nohl, H.; Gille, L. Antioxidant, Prooxidant and Cytotoxic Activity of Hydroxylated Resveratrol Analogues: Structure-Activity Relationship. Biochem. Pharmacol. 2005, 69, 903–912. [Google Scholar] [CrossRef]
- Banik, K.; Ranaware, A.M.; Harsha, C.; Nitesh, T.; Girisa, S.; Deshpande, V.; Fan, L.; Nalawade, S.P.; Sethi, G.; Kunnumakkara, A.B. Piceatannol: A Natural Stilbene for the Prevention and Treatment of Cancer. Pharmacol. Res. 2020, 153, 104635. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Park, S.A.; Almazari, I.; Kim, E.H.; Na, H.K.; Surh, Y.J. Piceatannol Induces Heme Oxygenase-1 Expression in Human Mammary Epithelial Cells through Activation of ARE-Driven Nrf2 Signaling. Arch. Biochem. Biophys. 2010, 501, 142–150. [Google Scholar] [CrossRef]
- Gerszon, J.; Walczak, A.; Rodacka, A. Attenuation of H2O2-Induced Neuronal Cell Damage by Piceatannol. J. Funct. Foods 2017, 35, 540–548. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, L.H.; Chen, X.; Zhang, N.; Li, G. Piceatannol Attenuates Behavioral Disorder and Neurological Deficits in Aging Mice: Via Activating the Nrf2 Pathway. Food Funct. 2018, 9, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.C.; Prasad, S.; Aggarwal, B.B. Anti-Inflammatory Nutraceuticals and Chronic Diseases; Springer: New York, NY, USA, 2016; Volume 928, pp. 267–289. [Google Scholar] [CrossRef]
- Dumont, U.; Sanchez, S.; Olivier, B.; Chateil, J.F.; Pellerin, L.; Beauvieux, M.C.; Bouzier-Sore, A.K.; Roumes, H. Maternal consumption of piceatannol: A nutritional neuroprotective strategy against hypoxia-ischemia in rat neonates. Brain Res. 2019, 1717, 86–94. [Google Scholar] [CrossRef]
- Zhang, D.; Li, X.; Hao, D.; Li, G.; Xu, B.; Ma, G.; Su, Z.; Zhang, D.; Li, X.; Hao, D.; et al. Systematic purification of polydatin, resveratrol and anthraglycoside B from Polygonum cuspidatum Sieb. et Zucc. Sep. Purif. Technol. 2009, 66, 329–339. [Google Scholar] [CrossRef]
- Du, Q.; Peng, C.; Zhang, H. Polydatin: A Review of Pharmacology and Pharmacokinetics. Pharm. Biol. 2013, 0209. [Google Scholar] [CrossRef]
- Cheng, Y.; Zhang, H.; Sun, L.; Guo, S.; Ouyang, S.; Zhang, Y.; Xu, J. Involvement of Cell Adhesion Molecules in Polydatin Protection of Brain Tissues from Ischemia—Reperfusion Injury. Brain Res. 2006, 1110, 193–200. [Google Scholar] [CrossRef]
- Gao, Y.; Chen, T.; Lei, X.; Li, Y.; Dai, X.; Cao, Y.; Ding, Q.; Lei, X.; Li, T.; Lin, X. Neuroprotective Effects of Polydatin against Mitochondrial-Dependent Apoptosis in the Rat Cerebral Cortex Following Ischemia/Reperfusion Injury. Mol. Med. Rep. 2016, 5481–5488. [Google Scholar] [CrossRef]
- Sun, J.; Qu, Y.; He, H.; Fan, X.; Qin, Y.; Mao, W.; Xu, L. Protective Effect of Polydatin on Learning and Memory Impairments in Neonatal Rats with Hypoxic-ischemic Brain Injury by Up-regulating Brain-derived Neurotrophic Factor. Mol. Med. Rep. 2014, 10, 3047–3051. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rao, S.R.; Ravishankar, G.A. Review Vanilla Flavour: Production by Conventional and Biotechnological Routes. J. Sci. Food Agric. 2000, 304, 289–304. [Google Scholar]
- Anand, A.; Khurana, R.; Wahal, N.; Mahajan, S.; Mehta, M.; Satija, S.; Sharma, N.; Vyas, M.; Khurana, N. Vanillin: A comprehensive review of pharmacological activities. Plant Arch. 2019, 19, 1000–1004. [Google Scholar]
- Kim, H.J.; Hwang, I.K.; Won, M.H. Vanillin, 4-hydroxybenzyl aldehyde and 4-hydroxybenzyl alcohol prevent hippocampal CA1 cell death following global ischemia. Brain Res. 2007, 1181. [Google Scholar] [CrossRef]
- Dhanalakshmi, C.; Janakiraman, U.; Essa, M.M.; Kalandar, A. Vanillin Attenuated Behavioural Impairments, Neurochemical Deficts, Oxidative Stress and Apoptosis Against Rotenone Induced Rat Model of Parkinson’s Disease. Neurochem. Res. 2016, 41, 1899–1910. [Google Scholar] [CrossRef]
- Lan, X.; Wang, Q.; Yang, J.; Ma, L.; Zhang, W.; Zheng, P.; Sun, T. Neuroprotective e effectof Vanillin on hypoxic-ischemic brain damage in neonatal rats. Biomed. Pharmacother. 2019, 118, 109196. [Google Scholar] [CrossRef]
- Nawrot, P.; Jordan, S.; Eastwood, J.; Rotstein, J.; Hugenholtz, A.; Feeley, M.; Jordan, S.; Eastwood, J.; Rotstein, J.; Hugenholtz, A.; et al. Effects of caffeine on human health. Food Addit. Contam. 2017. [Google Scholar] [CrossRef]
- Deslandes, A.C.; Veiga, H.; Cagy, M.; Piedade, R.; Pompeu, F.; Ribeiro, P. Effects of Caffeine on the Electrophysiological, Cognitive and Motor Responses of the Central Nervous System. Braz. J. Med Biol. Res. 2005, 38, 1077–1086. [Google Scholar] [CrossRef]
- Comer, A.M.; Perry, C.M.; Figgitt, D.P.; Bhatia, J.; Neonatology, S.; College, M. Caffeine Citrate: A Review of Its Use in Apnoea of Prematurity. Paediatr Drugs. 2001, 3, 61–79. [Google Scholar] [CrossRef]
- Schmidt, B.; Roberts, R.S.; Davis, P.; Doyle, L.W.; Barrington, K.J.; Ohlsson, A.; Solimano, A.; Tin, W. Caffeine Therapy for Apnea of Prematurity. N. Engl. J. Med. 2006, 2112–2121. [Google Scholar] [CrossRef]
- Picone, S.; Bedetta, M.; Paolillo, P. Caffeine Citrate: When and for How Long. A Literature Review. J. Matern. Neonatal Med. 2012, 25, 11–14. [Google Scholar] [CrossRef]
- Back, S.A.; Craig, A.; Luo, N.L.; Ren, J.; Akundi, R.S.; Ribeiro, I.; Rivkees, S.A. Protective Effects of Caffeine on Chronic Hypoxia-Induced Perinatal White Matter Injury. Ann. Neurol. 2006, 3, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Kilicdag, H.; Daglioglu, Y.K.; Erdogan, S.; Zorludemir, S. Effects of Caffeine on Neuronal Apoptosis in Neonatal Hypoxic-Ischemic Brain Injury. Ann. Neurol. 2014, 7058, 1470–1475. [Google Scholar] [CrossRef] [PubMed]
- Hoda, S.; Hosseinzadeh, H. Bioactivity Assessment and Toxicity of Crocin: A Comprehensive Review. Food Chem. Toxicol. 2014, 64, 65–80. [Google Scholar] [CrossRef]
- Abdel-Rahman, R.F.; El Awdan, S.A.; Hegazy, R.R.; Mansour, D.F.; Ogaly, H.A.; Abdelbaset, M. Neuroprotective Effect of Crocus Sativus against Cerebral Ischemia in Rats. Metab. Brain Dis. 2020, 427–439. [Google Scholar] [CrossRef] [PubMed]
- Sarshoori, J.R.; Asadi, M.H.; Mohammadi, M.T. Neuroprotective Effects of Crocin on the Histopathological Alterations Following Brain Ischemia-Reperfusion Injury in Rat. Iran. J. Basic Med. Sci. 2014, 17, 895. [Google Scholar] [PubMed]
- Pitsikas, N.; Sakellaridis, N. Crocus sativus L. extracts antagonize memory impairments in different behavioural tasks in the rat. Behav. Brain Res. 2006, 173, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Zhang, L.; Rao, W.; Su, N.; Hui, H.; Wang, L.; Peng, C.; Tu, Y.; Zhang, S.; Fei, Z. Neuroprotective Effects of Crocin against Traumatic Brain Injury in Mice: Involvement of Notch Signaling Pathway. Neurosci. Lett. 2015, 591, 53–58. [Google Scholar] [CrossRef]
- Hassani, F.V.; Naseri, V.; Razavi, B.M.; Mehri, S.; Abnous, K. Antidepressant Effects of Crocin and Its Effects on Transcript and Protein Levels of CREB, BDNF, and VGF in Rat Hippocampus. DARU J. Pharm. Sci. 2014, 22, 1–9. [Google Scholar]
- Huang, A.; Jia, L. Crocin Enhances Hypothermia Therapy in Hypoxic Ischemia-Induced Brain Injury in Mice. Acta Neurol. Belg. 2019. [Google Scholar] [CrossRef]
- Xu, S.; Liu, P. Tanshinone II-A: New Perspectives for Old Remedies. Expert Opin. Ther. Pat. 2013, 23, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Liu, Z.; Li, H.; Little, P.J.; Liu, P.; Xu, S. Cardiovascular Actions and Therapeutic Potential of Tanshinone IIA. Atherosclerosis 2012, 220, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Shang, Q.; Xu, H.; Huang, L. Tanshinone IIA: A Promising Natural Cardioprotective Agent. Evid. Based Complement. Altern. Med. 2012, 2012, 716459. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Jiang, P.; Ye, M.; Kim, S.H.; Jiang, C.; Lü, J. Tanshinones: Sources, Pharmacokinetics and Anti-Cancer Activities. Int. J. Mol. Sci. 2012, 13, 13621–13666. [Google Scholar] [CrossRef]
- Niu, X.L.; Ichimori, K.; Yang, X.; Hirota, Y.; Hoshiai, K.; Li, M.; Nakazawa, H. Tanshinone II-A Inhibits Low Density Lipoprotein Oxidation in Vitro. Free Radic. Res. 2000, 33, 305–312. [Google Scholar] [CrossRef]
- Zhou, Z.Y.; Zhao, W.R.; Zhang, J.; Chen, X.L.; Tang, J.Y. Sodium Tanshinone IIA Sulfonate: A Review of Pharmacological Activity and Pharmacokinetics. Biomed. Pharmacother. 2019, 118, 109362. [Google Scholar] [CrossRef]
- Chen, Y.; Wu, X.; Yu, S.; Lin, X.; Wu, J.; Li, L.; Zhao, J.; Zhao, Y. Neuroprotection of Tanshinone IIA against Cerebral Ischemia/Reperfusion Injury through Inhibition of Macrophage Migration Inhibitory Factor in Rats. PLoS ONE 2012, 7, e40165. [Google Scholar] [CrossRef]
- Ren, Y.; Houghton, P.J.; Hider, R.C.; Howes, M.J.R. Novel Diterpenoid Acetylcholinesterase Inhibitors from Salvia Miltiorhiza. Planta Med. 2004, 70, 201–204. [Google Scholar] [CrossRef]
- Xia, W.J.; Yang, M.; Fok, T.F.; Li, K.; Chan, W.Y.; Ng, P.-C.; Ng, H.K.; Chik, K.W.; Wang, C.C.; Gu, G.J.S.; et al. Partial Neuroprotective Effect of Pretreatment with Tanshinone IIA on Neonatal Hypoxia-Ischemia Brain Damage. Pediatr. Res. 2005, 58, 784–790. [Google Scholar] [CrossRef]
- Fowler, C.J. Plant-derived, synthetic and endogenous cannabinoids as neuroprotective agents: Non-psychoactive cannabinoids, ‘entourage’ compounds and inhibitors of N-acyl ethanolamine breakdown as therapeutic strategies to avoid pyschotropic effects. Brain Res. Rev. 2003, 41, 26–43. [Google Scholar] [CrossRef]
- Rosenberg, E.C.; Patra, P.H.; Whalley, B.J. Therapeutic Effects of Cannabinoids in Animal Models of Seizures, Epilepsy, Epileptogenesis, and Epilepsy-Related Neuroprotection. Epilepsy Behav. 2016, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.J.; Garcia-Merino, A. Neuroprotective Agents: Cannabinoids. Clin. Immunol. 2012, 142, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Fernández-López, D.; Pazos, M.R.; Tolon, R.M.; Moro, M.A.; Romero, J.; Lizasoain, I.; Martinez-Orgado, J. The cannabinoid agonist WIN55212 reduces brain damage in an in vivo model of hypoxic-ischemic encephalopathy in newborn rats. Pediatric Res. 2007, 62, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Zuardi, A.W.; Crippa, J.A.S.; Hallak, J.E.C.; Bhattacharyya, S.; Martín-Santos, R.; Mcguire, P.K.; Guimarães, F.S. A Critical Review of the Antipsychotic Effects of Cannabidiol 30 Years of a Trans- Lational Investigation. Curr. Pharm. Des. 2012, 15, 5131–5140. [Google Scholar] [CrossRef]
- Scuderi, C.; De Filippis, D.; Iuvone, T.; Blasio, A.; Steardo, A.; Esposito, G. Cannabidiol in Medicine: A Review of Its Therapeutic Potential in CNS Disorders. Phytotherapy Res. 2009, 602, 597–602. [Google Scholar] [CrossRef]
- Millar, S.A.; Stone, N.L.; Yates, A.S.; Sullivan, S.E.O. A Systematic Review on the Pharmacokinetics of Cannabidiol in Humans. Front. Pharmacol. 2018, 9. [Google Scholar] [CrossRef]
- Burstein, S. CBD Receptor Binding Signaling Events Downstream Events. Bioorg. Med. Chem. 2015. [Google Scholar] [CrossRef]
- Alvarez, F.J.; Lafuente, H.; Rey-santano, M.C.; Mielgo, V.E.; Gastiasoro, E.; Rueda, M.; Pertwee, R.G.; Castillo, A.I.; Romero, J.; Martínez-Orgado, J. Neuroprotective Effects of the Nonpsychoactive Cannabinoid Cannabidiol in Hypoxic-Ischemic Newborn Piglets. Pediatr. Res. 2008, 64, 653–658. [Google Scholar] [CrossRef]
- Castillo, A.; Tolón, M.R.; Fernández-Ruiz, J.; Romero, J.; Martinez-Orgado, J. Neurobiology of Disease The Neuroprotective Effect of Cannabidiol in an in Vitro Model of Newborn Hypoxic—Ischemic Brain Damage in Mice Is Mediated by CB2 and Adenosine Receptors. Neurobiol. Dis. 2010, 37, 434–440. [Google Scholar] [CrossRef]
- Lafuente, H.; Alvarez, F.J.; Pazos, M.R.; Alvarez, A.; Rey-Santano, M.C.; Mielgo, V.; Murgia-Esteve, X.; Hilario, E.; Martinez-Orgado, J. Cannabidiol Reduces Brain Damage and Improves Functional Recovery after Acute Hypoxia-Ischemia in Newborn Pigs. Pediatr. Res. 2011, 70, 272–277. [Google Scholar] [CrossRef]
- Pazos, M.R.; Cinquina, V.; Gómez, A.; Layunta, R.; Santos, M.; Fernández-ruiz, J.; Martínez-orgado, J. Cannabidiol administration after hypoxia e ischemia to newborn rats reduces long-term brain injury and restores neurobehavioral function. Neuropharmacology 2012, 63, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Pazos, M.R.; Mohammed, N.; Lafuente, H.; Santos, M.; Martínez-pinilla, E.; Moreno, E.; Valdizan, E.; Romero, J.; Pazos, A.; Franco, R.; et al. Mechanisms of Cannabidiol Neuroprotection in Hypoxice Ischemic Newborn Pigs: Role of 5HT1A and CB2 Receptors. Neuropharmacology 2013, 71, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Barata, L.; Arruza, L.; Rodríguez, M.; Aleo, E.; Vierge, E.; Criado, E.; Sobrino, E.; Vargas, C.; Ceprián, M.; Gutiérrez-Rodríguez, A.; et al. Neuroprotection by Cannabidiol and Hypothermia in a Piglet Model of Newborn Hypoxic-Ischemic Brain Damage. Neuropharmacology 2019, 146, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.; Rodrigues, M.; Fortuna, A.; Falcão, A.; Alves, G. Huperzine A from Huperzia Serrata: A Review of Its Sources, Chemistry, Pharmacology and Toxicology. Phytochem. Rev. 2016, 15, 51–85. [Google Scholar] [CrossRef]
- Desilets, A.R.; Gickas, J.J.; Dunican, K.C. Role of Huperzine A in the Treatment of Alzheimer’s Disease. Ann. Pharmacother. 2009, 43. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Hm, W.; Zhou, R.L.; Liu, G.J.; Dong, B.R. Huperzine A for Alzheimer’s Disease. Cochr. Database Syst. Rev. 2009, 2. [Google Scholar] [CrossRef]
- Wang, R.; Can, X. Neuroprotective Effects of Huperzine A. Neurosignals 2005, 14, 71–82. [Google Scholar] [CrossRef]
- Damar, U.; Gersner, R.; Johnstone, J.T.; Schachter, S.; Rotenberg, A.; Gersner, R.; Johnstone, J.T.; Schachter, S.; Rotenberg, A. Expert Review of Neurotherapeutics Huperzine A as a Neuroprotective and Antiepileptic Drug: A Review of Preclinical Research. Expert Rev. Neurother. 2016, 16, 671–680. [Google Scholar] [CrossRef]
- Park, S. State Key Laboratory of Drug Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Zhangjiang Hi-Tech Park, Shanghai, P.R. China. J. Neurochem. 2008, 1594–1603. [Google Scholar] [CrossRef]
- Shuan, L.; Zhou, J.; Mei, X.; Can, X. Huperzine A Attenuates Cognitive Deficits and Brain Injury in Neonatal Rats after Hypoxia—Ischemia. Brain Res. 2002, 949, 162–170. [Google Scholar]
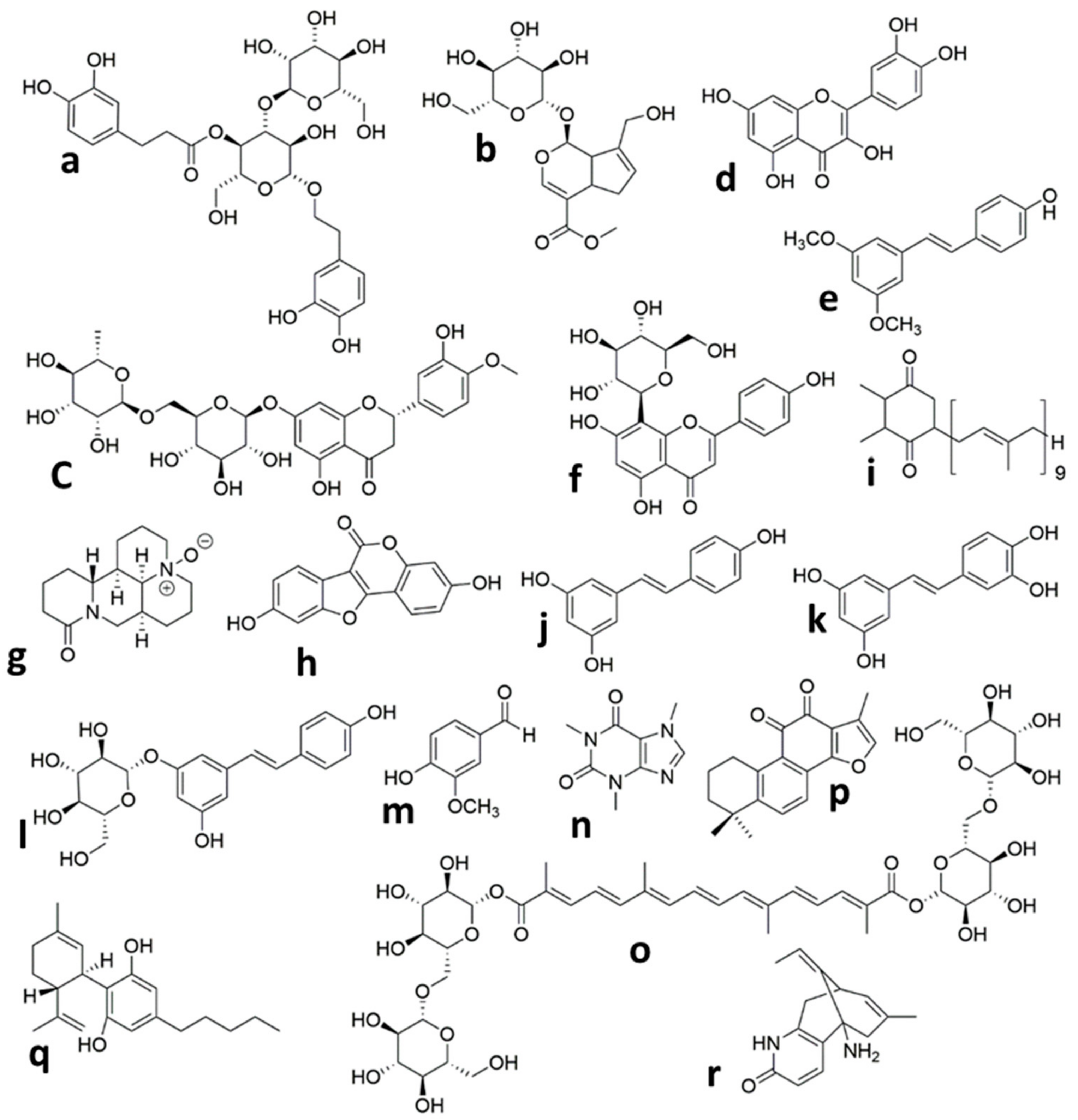

| Plant Extract/Compound | Administration Regimen | Dose | Species | Synergistic/Complementary Mechanism with/without Hypothermia | Effects/Molecular Mechanism | Reference |
|---|---|---|---|---|---|---|
| Grape seed extract | Pretreatment 5 min before HI Post-treatment 4 h after reoxygenation | 50 mg/kg intra peritoneal (i.p.) injection twice daily for 1 day | P7 neonatal rat pups | Pretreatment: Reduction of brain weight loss Improvement of histopathologic brain score Antioxidant effect: Reduction of lipid peroxidation (reduced 8-iso-PGF2α and TBARS level) Post-treatment: No protection | [52] | |
| Post-treatment 5 min to 5 h after reoxygenation | 50 mg/kg i.p. injection | P7 neonatal rat pups | Reduction of brain weight loss Antioxidant effect: Reduction of lipid peroxidation (reduced 8-iso-PGF2α level) Anti-apoptotic effect: Reduction of pro-apoptotic protein c-jun | [53] | ||
| Grape seed proanthocyanidin extract | Pretreatment 20 min before HI | 30 mg/kg i.p. injection | P7neonatal mouse pups | Reduction of infarct volume Improvement of neurobehavioral recovery Anti-apoptotic effect: Reduction of apoptotic cells number Reduction of pro-apoptotic proteins expression(bax and cleaved-caspase-3) Enhancement of anti-apoptotic (bcl-2) proteins expression and increased ratio of bcl2-to-bax | [60] | |
| Pomegranate juice | Maternal dietary supplementation | 1:60 or 1:80 or 1:320 dilutions of pj concentrate, during last third of pregnancy and litter suckling | P7 neonatal mouse pups | Reduction of brain tissue loss Anti-apoptotic effect: Reduction of caspase-3 activation | [36] | |
| Pomegranate polyphenol extract | Maternal dietary supplementation | 4.8 mg/day during pregnancy and litter suckling | P7 neonatal mouse pups | Anti-apoptotic effect Reduction of caspase-3 activation | [96] | |
| Dendribium officinale extract | Post-treatment | (75 or 150 or 300) mg/kg, intragastric administration, Daily for 14 consecutive days | P7 neonatal rat pups | Improvement of behavioral ability Reduction of CI area percentage Regulation of brain injury-related proteins’ expression (diminished HDAC1 and elevated KCC2 expression) Antioxidant effect: Diminished levels of NOS, NO, and MDA Enhancement of antioxidant capacity (increased SOD activity) Anti-apoptotic effect Downregulated caspase-3 and Bax expressionUpregulated Bcl-2 expression Anti-inflammatory effect: Regulation of neurotrophic factors expression (increased expression of BDNF, bFGF, and CNTF) Mechanism: Inhibition of HIF-1α | [37] | |
| Caffeine | Pretreatment immediately before HI, post-treatment 0, 24, 48, and 72 h after HI | 20 mg/kg | P7 neonatal rat pups | Decreased ventriculomegaly and hypomyelination More normally arranged myelinated axon orientation Enhanced proportion of immature oligodendrocytes Anti-apoptotic effectDecreased number of apoptotic cells | [303] | |
| Pterostilbene | Pretreatment 30 min before HI | 50 mg/kg i.p. injection | P7 neonatal rat pups | Enhancement of animal survival Reduction of neurological score Improvement in motor coordination, motor deficit, and working memory deficit Reduction of brain infarct volume Reduction of brain edema Anti-inflammation: (decreased TNFα, IL-1, and IL-6 expression; decreased p-65 and NF-κβ expression) Antioxidant: (decreased TBARS and ROS level; increased SOD activity) Antiapoptotic: (inhibition of programmed cell death) Mechanism: HO-1 signaling pathway (Prevention of HO-1 mRNA and protein expression) | [172] | |
| Quercetin | Pretreatment | 40 mg/kg/day Intra-gastrically injection once a day for 7 days, last administration was 2 h after HI | P7 neonatal rat pups | Anti-apoptosis: (downregulated Bax, upregulated Bcl-2, attenuated DNA-strands breaks) Anti-inflammation: (attenuated astrogliosis and microgliosis; downregulated IL-6, IL-1β, and TNF-α) Mechanism: Suppression of TLR4-mediated NF-κB signaling pathway (decreased TLR4 phosphorylation and downstream signals of p65 and p-IκBα) | [159] | |
| Post-treatment 2 h after HI to the day of rats’ scarification | 20 or 40 mg/kg Intra-gastrically injection Once a day | P3 neonatal rat pups | Improvement of myelination in the cortex through strengthening survival of oligodendrocytes | [160] | ||
| Resveratrol | Pretreatment 24 h/10 min before HI Post-treatment3 h after HI | 20 mg/kg or 200 μg/kg or 2 μg/kg i.p. injection | P7 Neonatal rat and mouse pups | Pretreatment: Protecting brain from tissue loss Preventing apoptosis and necrosis (diminished caspase-3 and calpain activation) Post-treatment: No protection | [96] | |
| Pretreatment 30 min before HI Post-treatment 30 min after HI | 30 mg/kg i.p. injection | P7 neonatal rat pups | Pretreatment: anti-apoptotic: (reduced expression level of Bax, caspase-3, and the ratio of Bax/Bcl-2) Post-treatment Not protection | [273] | ||
| Post-treatment Immediately after HI | 90 mg/kg i.p. injection | P7 neonatal rat pups | Reduced infarct volume Preserved myelination Behavioral tests (P8–P66): Improved early reflexes and sensorimotor functions Improved learning/memory function | [274] | ||
| Pretreatment 10 min before HI Post-treatment Immediately after HI | 20 mg/kg i.p. injection | P7 neonatal rat pups | Pretreatment: Reduced infarct volume Preserved myelination Minimized astroglial reactive response Improved long-term cognitive impairment Post-treatment: Not protection | [275] | ||
| Post-treatment 0 h, 8 h and 18 h after HI | 100 mg/kg i.p. injection | P7 neonatal rat pups | Anti- inflammation:(reduction of inflammatory factors expression; inhibition of microglia activation) anti-apoptosis: (regulation of Bax, Bcl-2 and caspase3 expression) | [276] | ||
| Post-treatment immediately after HI and 12 h later | 100 mg/mL i.p. injection | P7 neonatal mouse pups | Anti- inflammation: (reduced expression levels of IL-1β, IL-6, and TNF-α) Enhancement of SIRT1 levelMechanism: Inhibition of TLR4/MyD88/NF-κB signaling pathway (reduced TLR4, MyD88, NF-κB levels) | [277] | ||
| Tanshinone IIA | From 2 days before HI for 9 or 16 days | 10 mg/kg/day i.p. injection | P7 neonatal rat pups | Improved neuropathology and sensorimotor functions Improved antioxidant capacity Protect mitochondrial membrane potential | [320] | |
| Vanillin | Post- treatment Immediately after HI | 80 mg/kg, i.p. injection | P7 neonatal rat pups | Improved neurobehavioral deficits Reduced brain infract volume Reduced brain edema Reduced neuronal degeneration and necrotic cell death Preserving BBB integrity (decreased IgG leakage, reduced levels of MMPs, upregulated expression of TJ-related proteins) Inhibiting oxidative stress (increased SOD, GSH-Px, and CAT; increased T-AOC; decreased lipid peroxidation (MDA content)) | [297] | |
| Verbascoside | Post-treatment | (60 or 120 or 240) mg/kg, i.p. injection, every 12 h for two consecutive days | P7 neonatal rat pups | Reduction of prolonged reflex latencies Reduction of brain infarct volume Reduction of necrosis Reduction of degeneration and morphological damage of neurons Reduction of autophagosome formation Reverse expression level of autophagy-related proteins (Beclin-1, LC3-II/I ratio, and P62) | [115] | |
| Vitexin | Post-treatment 5 min or 3 h after HI | (30 or 45 or 60) mg/kg i.p. injection single dose | P7 neonatal rat pups | 5 min after HI:Reduction of brain infarct volume Reduction of brain edema Improvement of long-term behavioral development Attenuation of neuronal cell death and brain tissue loss Attenuation of BBB disruption: (reduction of IgG staining and brain water content) Mechanism: inhibition of HIF-1α/VEGF(decreased HIF-1α and VEGF protein levels) 3 h after HI: vitexin lost its neuroprotection | [188] | |
| Cannabidiol | Post-treatment 15 and 240 min after HI | 0.1 mg/kg i.v. injection | P3–P5 newborn piglets | Reduction of brain edema Prevention of brain seizures Reduced cell lossReduced number of degenerating neurons Cardio-protective effects | [329] | |
| Post-treatment | 100 µM | Forebrain slices from P7–P10 neonatal mouse pups | Prevention of necrotic cell death (reduced LDH efflux to the medium) Anti-apoptotic: (reduced caspase-9 level) Anti-inflammatory: (reduced IL-6 and TNF-α level; reduced COX-2 expression level) Excitotoxicity modulation: (decreased glutamate release) Antioxidant: (decreased iNOS expression) Mechanism: Activation of A2A and CBD receptors | [330] | ||
| Post-treatment 15 and 240 min after HI | 0.1 mg/kg i.v. injection | P1–P3 newborn piglets | Long follow-up study (72 h after HI): Improved neurobehavioral performance Improved brain activity Stabilized metabolic activity Reduced cell death Anti-inflammatory effect (protects astrocytes) | [331] | ||
| Post-treatment 10 min after HI | 1 mg/kg i.v. injection | P7–P10 neonatal rat pups | Long follow-up study (7 days or one month after HI): Reduced infarct volume Modulated brain excitotoxicity, oxidative stress, and inflammation 7 days after HI Improved neurobehavioral performance one month after HI | [332] | ||
| Post-treatment 30 min after HI | 1 mg/kg i.v. injection | P1–P2 newborn piglets | Modulation of excitotoxicity, oxidative stress and inflammationMechanism Involvement of CB2 and 5HT1A receptors | [333] | ||
| Post-treatment 30 min after HT Combined with hypothermia | 1 mg/kg i.v. injection | P1–P2 newborn piglets | Short follow-up study: Modulation of excitotoxicity, inflammation, oxidative stress, and cell damage was greater than either hypothermia or CBD alone | Cannabidiol treatments reduced the oxidized protein and TNFα levels | [38] | |
| Post-treatment 30 min after HT Combined with hypothermia | 1 mg/kg i.v. injection repeated 24 and 48 h after HI | P1 newborn piglets | Reverse the induction of increases in lactate/N-acetyl-aspartate, glutamate/Nacetyl-aspartate, TNFα, or apoptosis Modulate the brain excitotoxicity and inflammation More complete neuroprotection than CBD or hypothermia alone | Long follow-up study: Improved brain activity Decreased microglial activation | [334] | |
| Coumestrol | Pretreatment Immediately pre-hypoxia Post-treatment 3 h after hypoxia | 20 mg/kg i.p. injection | P7 male neonatal rat pups | Pre- and post-treatment: Preventing reference and working memory impairments Preventing late cognitive deficits in reference and working memory at P60 Reduction of brain tissue loss Reduction of late GFAP overexpression (index of late reactive astrogliosis) Pretreatment: Prevention of mitochondrial swelling Mechanism: Prevention of mitochondrial dysfunction and long-term cognitive deficits | [224] | |
| Crocin | Post-treatment Immediately or 2 h after HI | 10 mg/kg combined with hypothermia | P7 neonatal mouse pups | Reduced neurological severity score Anti-oxidative effect: (reduced levels of MDA, ROS, and NO; reduced mRNA expression of iNOS and COX-2) Anti-inflammatory effect: (reduced IL-1β and TNF-α levels) | [311] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohsenpour, H.; Pesce, M.; Patruno, A.; Bahrami, A.; Pour, P.M.; Farzaei, M.H. A Review of Plant Extracts and Plant-Derived Natural Compounds in the Prevention/Treatment of Neonatal Hypoxic-Ischemic Brain Injury. Int. J. Mol. Sci. 2021, 22, 833. https://doi.org/10.3390/ijms22020833
Mohsenpour H, Pesce M, Patruno A, Bahrami A, Pour PM, Farzaei MH. A Review of Plant Extracts and Plant-Derived Natural Compounds in the Prevention/Treatment of Neonatal Hypoxic-Ischemic Brain Injury. International Journal of Molecular Sciences. 2021; 22(2):833. https://doi.org/10.3390/ijms22020833
Chicago/Turabian StyleMohsenpour, Hadi, Mirko Pesce, Antonia Patruno, Azam Bahrami, Pardis Mohammadi Pour, and Mohammad Hosein Farzaei. 2021. "A Review of Plant Extracts and Plant-Derived Natural Compounds in the Prevention/Treatment of Neonatal Hypoxic-Ischemic Brain Injury" International Journal of Molecular Sciences 22, no. 2: 833. https://doi.org/10.3390/ijms22020833
APA StyleMohsenpour, H., Pesce, M., Patruno, A., Bahrami, A., Pour, P. M., & Farzaei, M. H. (2021). A Review of Plant Extracts and Plant-Derived Natural Compounds in the Prevention/Treatment of Neonatal Hypoxic-Ischemic Brain Injury. International Journal of Molecular Sciences, 22(2), 833. https://doi.org/10.3390/ijms22020833






