GRPEL2 Knockdown Exerts Redox Regulation in Glioblastoma
Abstract
1. Introduction
2. Results
2.1. GRPEL2 Expression Correlated with Tumor Grade and Overall Survival in Glioma
2.2. GRPEL2 Expression Correlated with Oligodendroglial Differentiation and IDH Wide-Type Phenotypes
2.3. GRPEL2-Stained Microarray Correlated with WHO Grade and Oligodendroglial Differentiation in Glioma Tissues
2.4. GRPEL2 Expression Highly Correlated with TERT Rather Than ATRX Expression
2.5. GRPEL2 Enhanced Expression in Glioma Cell Lines and Its Downregulation Decreased Cell Growth
2.6. siGRPEL2-Induced Cell Growth Decrease Does Not Involve Apoptosis
2.7. GRPEL2 Knockdown Decreased the Oxygen Consumption Rate (OCR) of Glioma Cells
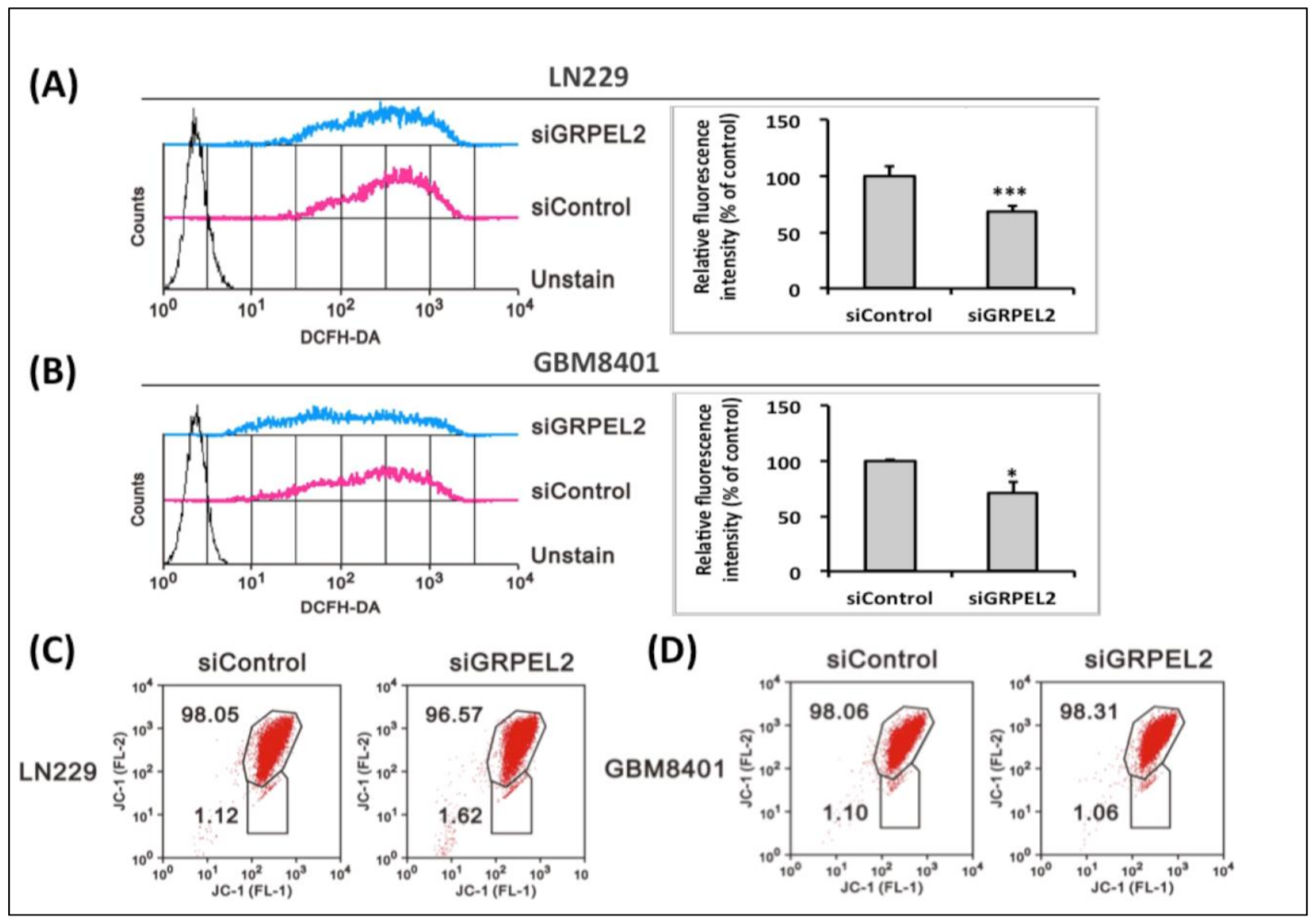
2.8. GRPEL2 Knockdown Reduced Intracellular ROS Activity without Disrupting the Mitochondrial Membrane Potential
2.9. siGRPEL2 Increased Autophagy and Senescence in Glioma Cells
3. Discussion
3.1. Impact of IDH/TERT Phenotype on GRPEL2 Expression
3.2. siGRPEL2 Suppressed Non-Mitochondrial Respiration Alternating ROS
3.3. Role of siGRPEL2 in the Regulation of Mitochondrial ROS
3.4. siGRPEL2 Enhanced Autophagy and Senescence Expressions, Impacting on the Bioenergetics of Mitochondria
4. Conclusions
5. Materials and Methods
5.1. Analysis of Data from the TCGA and CGGA Databases
5.2. Tissue Microarray Slide Preparation, Immunohistochemistry, and Scoring
5.3. Statistical Analysis of the Association between GRPEL2 Expression and Other Factors
5.4. Human Glioma Cell Lines and Lysate Preparation
5.5. Transfection of siGRPEL2 and siControl into Glioma Cell Lines and Cell Proliferation Assays
5.6. RNA Isolation and Real-Time Reverse Transcription-PCR (RT-PCR)
5.7. Western Blot Analysis (Lysate Preparation Was Referred to in 4.4)
5.8. Cell Cycle Assessment
5.9. Measurement of Oxygen Consumption Rate (OCR)
5.10. Intracellular ROS, Senescence, and Autophagy Determination
5.11. Measurement of Mitochondrial Membrane Potential
5.12. Flow Cytometry Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CGGA | Chinese Glioma Genome Atlas |
| GBM | Glioblastoma multiforme |
| GRPEL2 | GrpE protein homolog-2 |
| IHC | Immunohistochemistry |
| NEF | Nucleotide exchange factor |
| PAM | Pre-sequence-Associated Motor |
| ROS | Reactive Oxygen Species |
| TCGA | The Cancer Gene Atlas |
| WHO | World Health Organization |
References
- Corinne, E.G.; Claudia, R.O. Bioenergetics pathways and therapeutic resistance in gliomas: Emerging role of mitochondria. Curr. Pharm. Des. 2011, 17, 2421–2427. [Google Scholar] [CrossRef]
- Guerra, F.; Arbini, A.A.; Moro, L. Mitochondria and cancer chemoresistance. Biochim. Biophys. Acta BBA Bioenerg. 2017, 1858, 686–699. [Google Scholar] [CrossRef]
- Ohgaki, H.; Dessen, P.; Jourde, B.; Horstmann, S.; Nishikawa, T.; Di Patre, P.-L.; Burkhard, C.; Schüler, D.; Probst-Hensch, N.M.; Maiorka, P.C.; et al. Genetic pathways to glioblastoma- a population-based study. Cancer Res. 2004, 64, 6892–6899. [Google Scholar] [CrossRef] [PubMed]
- Franco, D.; Moretti, I.; Marie, S. Mitochondria transcription factor a: A putative target for the effect of melatonin on u87mg malignant glioma cell line. Molecules 2018, 23, 1129. [Google Scholar] [CrossRef]
- Lee, H.; Park, J.; Tran, Q.; Kim, D.; Hong, Y.; Cho, H.; Kwon, S.H.; Brazil, D.; Kim, S.-H.; Park, J. Mitochondrial transcription factor a (TFAM) is upregulated in glioma. Mol. Med. Rep. 2017, 15, 3781–3786. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, S.; Savanur, M.A.; Sinha, D.; Birje, A.; Vigneshwaran, R.; Saha, P.P.; D’Silva, P. Regulation of mitochondrial protein import by the nucleotide exchange factors grpel1 and grpel2 in human cells. J. Biol. Chem. 2017, 292, 18075–18090. [Google Scholar] [CrossRef] [PubMed]
- Jain, K.K. A critical overview of targeted therapy for glioblastoma. Front. Oncol. 2018, 8, 419. [Google Scholar] [CrossRef] [PubMed]
- Buruiană, A.; Florian, Ș.I.; Florian, A.I.; Timiș, T.L.; Mihu, C.M.; Miclăuș, M.; Oșan, S.; Hrapșa, I.; Cataniciu, R.C.; Farcaș, M.; et al. The roles of miRNA in glioblastoma tumor cell communication: Diplomatic and aggressive negotiations. Int. J. Mol. Sci. 2020, 21, 1950. [Google Scholar] [CrossRef] [PubMed]
- Maiuthed, A.; Prakhongcheep, O.; Chanvorachote, P. Microarray-based analysis of genes, transcription factors, and epigenetic modifications in lung cancer exposed to nitric oxide. Cancer Genom. Proteom. 2020, 17, 401–415. [Google Scholar] [CrossRef] [PubMed]
- Warburg, O.H.; Dickens, F. The metabolism of tumours: Investigations from the Kaiser Wilhelm institute for biology. JAMA 1931, 96, 1982. [Google Scholar] [CrossRef]
- Zhou, W.; Wahl, D.R. Metabolic abnormalities in glioblastoma and metabolic strategies to overcome treatment resistance. Cancers 2019, 11, 1231. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Ma, J.; Lu, W. The significance of mitochondrial dysfunction in cancer. Int. J. Mol. Sci. 2020, 21, 5598. [Google Scholar] [CrossRef]
- Westermann, B.; Prip-Buus, C.; Neupert, W.; Schwarz, E. The role of the GrpE homologue, Mgelp, in mediating protein import and protein folding in mitochondria. EMBO J. 1995, 14, 3452–3460. [Google Scholar] [CrossRef]
- Grimshaw, J.P.A.; Jelesarov, I.; Schönfeld, H.-J.; Christen, P. Reversible thermal transition in GrpE, the nucleotide exchange factor of the DnaK heat-shock system. J. Biol. Chem. 2001, 276, 6098–6104. [Google Scholar] [CrossRef] [PubMed]
- Brehmer, D.; Rüdiger, S.; Gässler, C.S.; Klostermeier, D.; Packschies, L.; Reinstein, J.; Mayer, M.P.; Bukau, B. Tuning of chaperone activity of Hsp70 proteins by modulation of nucleotide exchange. Nat. Struct. Biol. 2001, 8, 427–432. [Google Scholar] [CrossRef]
- Konovalova, S.; Liu, X.; Manjunath, P.; Baral, S.; Neupane, N.; Hilander, T.; Yang, Y.; Balboa, D.; Terzioglu, M.; Euro, L.; et al. Redox regulation of GRPEL2 nucleotide exchange factor for mitochondrial HSP70 chaperone. Redox Biol. 2018, 19, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Spaas, J.; van Veggel, L.; Schepers, M.; Tiane, A.; van Horssen, J.; Wilson, D.M.; Moya, P.R.; Piccart, E.; Hellings, N.; Eijnde, B.O.; et al. Oxidative stress and impaired oligodendrocyte precursor cell differentiation in neurological disorders. Cell. Mol. Life Sci. 2021, 78, 4615–4637. [Google Scholar] [CrossRef] [PubMed]
- Rüdiger, S.; Buchberger, A.B. Bernd Interaction of Hsp70 chaperones with substrates. Nat. Struct. Biol. 1997, 4, 342–349. [Google Scholar] [CrossRef]
- Oliveira, C.L.P.; Borges, J.C.; Torriani, I.L.; Ramos, C.H.I. Low resolution structure and stability studies of human GrpE#2, a mitochondrial nucleotide exchange factor. Arch. Biochem. Biophys. 2006, 449, 77–86. [Google Scholar] [CrossRef]
- Koppenol, W.H.; Bounds, P.L.; Dang, C.V. Otto warburg’s contribution to current concept of cancer metabolism. Nat. Rev. Cancer 2011, 11, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Leu, J.I.-J.; Barnoud, T.; Zhang, G.; Tian, T.; Wei, Z.; Herlyn, M.; Murphy, M.E.; George, D. Inhibition of stress-inducible HSP70 impairs mitochondrial proteostasis and function. Oncotarget 2017, 8, 45656–45669. [Google Scholar] [CrossRef] [PubMed]
- Laloraya, S.; Dekker, P.J.T.; Voos, W.; Craig, E.A.; Pfanner, N. Mitochondrial GrpE modulates the function of matrix Hsp70 in translocation and maturation of preproteins. Mol. Cell. Biol. 1995, 15, 7089–7105. [Google Scholar] [CrossRef] [PubMed]
- Panuzzo, C.; Jovanovski, A.; Pergolizzi, B.; Pironi, L.; Stanga, S.; Fava, C.; Cilloni, D. Mitochondria: A galaxy in the hematopoietic and leukemic stem cell universe. Int. J. Mol. Sci. 2020, 21, 3928. [Google Scholar] [CrossRef] [PubMed]
- Hide, T.; Shibahara, I.; Kumabe, T. Novel concept of the border niche: Glioblastoma cells use oligodendrocytes progenitor cells (GAOs) and microglia to acquire stem cell-like features. Brain Tumor Pathol. 2019, 36, 63–73. [Google Scholar] [CrossRef]
- Guntuku, L.; Naidu, V.G.M.; Yerra, V.G. Mitochondrial dysfunction in gliomas: Pharmacotherapeutic potential of natural compound. Curr. Neuropharmacol. 2016, 14, 567–583. [Google Scholar] [CrossRef]
- Gilbert, M.R.; Dignam, J.J.; Armstrong, T.S.; Wefel, J.S.; Blumenthal, D.T.; Vogelbaum, M.A.; Colman, H.; Chakravarti, A.; Pugh, S.; Won, M.; et al. A randomized trial of bevacizumab for newly diagnosed glioblastoma. N. Engl. J. Med. 2014, 370, 699–708. [Google Scholar] [CrossRef] [PubMed]
- Masui, K.; Komori, T.; Kato, Y.; Masutomi, K.; Ichimura, K.; Ogasawara, S.; Kaneko, M.K.; Oki, H.; Suzuki, H.; Nitta, M.; et al. Elevated TERT expression in TERT-wildtype adult diffuse gliomas: Histological evaluation with a novel tert-specific antibody. BioMed Res. Int. 2018, 2018, 7945845. [Google Scholar] [CrossRef] [PubMed]
- Nabors, L.B.; Portnow, J.; Ahluwalia, M.; Baehring, J.; Brem, H.; Brem, S.; Butowski, N.; Campian, J.L.; Clark, S.W.; Fabiano, A.J.; et al. Central nervous system cancers, version 3.2020, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2020, 18, 1537–1570. [Google Scholar] [CrossRef]
- Amen, A.M.; Fellmann, C.; Soczek, K.M.; Ren, S.M.; Lew, R.J.; Knott, G.J.; Park, J.E.; McKinney, A.M.; Mancini, A.; Doudna, J.A.; et al. Cancer-specific loss of TERT activation sensitizes glioblastoma to DNA damage. Proc. Natl. Acad. Sci. USA 2021, 118, e2008772118. [Google Scholar] [CrossRef]
- Henson, J.D.; Hannay, J.A.; McCarthy, S.W.; Royds, J.A.; Yeager, T.R.; Robinson, R.A.; Wharton, S.B.; Jellinek, D.A.; Arbuckle, S.M.; Yoo, J.; et al. A robust assay for alternative lengthening of telomeres in tumors shows the significance of alternative lengthening of telomeres in sarcomas and astrocytomas. Clin. Cancer Res. 2005, 11, 217–225. [Google Scholar]
- Leão, R.; Apolónio, J.D.; Lee, D.; Figueiredo, A.; Tabori, U.; Castelo-Branco, P. Mechanisms of human telomerase reverse transcriptase (hTERT) regulation: Clinical impacts in cancer. J. Biomed. Sci. 2018, 25, 22. [Google Scholar] [CrossRef]
- Yuan, X.; Larsson, C.; Xu, D. Mechanisms underlying the activation of TERT transcription and telomerase activity in human cancer: Old actors and new players. Oncogene 2019, 38, 6172–6183. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Aoki, K.; Chiba, K.; Sato, Y.; Shiozawa, Y.; Shiraishi, Y.; Shimamura, T.; Niida, A.; Motomura, K.; Ohka, F.; et al. Mutational landscape and clonal architecture in grade II and III gliomas. Nat. Genet. 2015, 47, 458–468. [Google Scholar] [CrossRef]
- Wolf, A.; Agnihotri, S.; Guha, A. Targeting metabolic remodeling in glioblastoma multiforme. Oncotarget 2010, 1, 552–562. [Google Scholar] [CrossRef] [PubMed]
- Voos, W.; Gambill, D.; Laloraya, S.; Ang, D.; Craig, E.A.; Pfanneri, N. Mitochondrial GrpE is present in a complex with hsp7o and preproteins in transit across membranes. Mol. Cell. Biol. 1994, 14, 6627–6634. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ordys, B.B.; Launay, S.; Deighton, R.F.; McCulloch, J.; Whittle, I.R. The role of mitochondria in glioma pathophysiology. Mol. Neurobiol. 2010, 42, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Perillo, B.; Di Donato, M.; Pezone, A.; Di Zazzo, E.; Giovannelli, P.; Galasso, G.; Castoria, G.; Migliaccio, A. Ros in cancer therapy: The bright side of the moon. Exp. Mol. Med. 2020, 52, 192–203. [Google Scholar] [CrossRef] [PubMed]
- Poteet, E.; Choudhury, G.R.; Winters, A.; Li, W.; Ryou, M.-G.; Liu, R.; Tang, L.; Ghorpade, A.; Wen, Y.; Yuan, F.; et al. Reversing the Warburg effect as a treatment for glioblastoma. J. Biol. Chem. 2013, 288, 9153–9164. [Google Scholar] [CrossRef]
- Morrish, F.; Hockenbery, D. Myc and mitochondrial biogenesis. Cold Spring Harb. Perspect. Med. 2014, 4, a014225. [Google Scholar] [CrossRef]
- Hartl, F.U. Molecular chaperones in cellular protein folding. Nature 1996, 381, 571–580. [Google Scholar] [CrossRef]
- Brennan, C.; Momota, H.; Hambardzumyan, D.; Ozawa, T.; Tandon, A.; Pedraza, A.; Holland, E. Glioblastoma subclasses can be defined by activity among signal transduction pathways and associated genomic alterations. PLoS ONE 2009, 4, e7752. [Google Scholar] [CrossRef]
- Louis, D.N.; Ohgaki, H.; Wiestler, O.D.; Cavenee, W.K.; Burger, P.C.; Jouvet, A.; Scheithauer, B.W.; Kleihues, P. The 2007 who classification of tumours of the central nervous system. Acta Neuropathol. 2007, 114, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Louis, D.N.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, W.K.; Ohgaki, H.; Wiestler, O.D.; Kleihues, P.; Ellison, D.W. The 2016 world health organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016, 131, 803–820. [Google Scholar] [CrossRef]
- Gordon, D.M.; Santos, J.H. The emerging role of telomerase reverse transcriptase in mitochondrial DNA metabolism. J. Nucleic Acids 2010, 2010, 390791. [Google Scholar] [CrossRef] [PubMed]
- Rosen, J.; Jakobs, P.; Ale-Agha, N.; Altschmied, J.; Haendeler, J. Non-canonical functions of telomerase reverse transcriptase—Impact on redox homeostasis. Redox Biol. 2020, 34, 101543. [Google Scholar] [CrossRef]
- Indran, I.R.; Hande, M.P.; Pervaiz, S. hTERT overexpression alleviates intracellular ROS production, improves mitochondrial function, and inhibits ros-mediated apoptosis in cancer cells. Cancer Res. 2011, 71, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Asslaber, M.; Schauer, S.; Gogg-Kamerer, M.; Bernhart, E.; Quehenberger, F.; Haybaeck, J. Native oligodendrocytes in astrocytomas might inhibit tumor proliferation by WIF1 expression. J. Neuropathol. Exp. Neurol. 2017, 76, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Rahme, G.J.; Chatterjee, P.D.; Havrda, M.C.; Israel, M.A. ID2 promotes survival of glioblastoma cells during metabolic stress by regulating mitochondrial function. Cell Death Dis. 2017, 8, e2615. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, S.; Corsinovi, D.; Lessi, F.; Tantillo, E.; Aretini, P.; Menicagli, M.; Scopelliti, C.; Civita, P.; Pasqualetti, F.; Naccarato, A.G.; et al. Mitochondrial enzyme GLUD2 plays a critical role in glioblastoma progression. EBioMedicine 2018, 37, 56–67. [Google Scholar] [CrossRef]
- May, J.L.; Kouri, F.M.; Hurley, L.A.; Liu, J.; Tommasini-Ghelfi, S.; Ji, Y.; Gao, P.; Calvert, A.E.; Lee, A.; Chandel, N.S.; et al. IDH3α regulates one-carbon metabolism in glioblastoma. Sci. Adv. 2019, 5, eaat0456. [Google Scholar] [CrossRef] [PubMed]
- Poillet-Perez, L.; Despouy, G.; Delage-Mourroux, R.; Boyer-Guittaut, M. Interplay between ROS and autophagy in cancer cells, from tumor initiation to cancer therapy. Redox Biol. 2015, 4, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Yang, J.; Wang, Z.; Wu, G.; Liu, F.E.I. TFAM is directly regulated by miR-23b in glioma. Oncol. Rep. 2013, 30, 2105–2110. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Xu, Z.; Chen, X.; Wang, X.; Zeng, S.; Zhao, Z.; Qian, L.; Li, Z.; Wei, J.; Huo, L.; et al. Novel function of lncRNA ADAMTS9-AS2 in promoting temozolomide resistance in glioblastoma via upregulating the FUS/MDM2 ubiquitination axis. Front. Cell Dev. Biol. 2019, 7, 217. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.F.; Tsai, W.C.; Chou, C.H.; Huang, L.C.; Huang, S.M.; Hueng, D.Y.; Tsai, C.K. CKAP2L Knockdown Exerts Antitumor Effects by Increasing miR-4496 in Glioblastoma Cell Lines. Int. J. Mol. Sci. 2020, 22, 197. [Google Scholar] [CrossRef]
- Li, Y.F.; Scerif, F.; Picker, S.R.; Stone, T.J.; Pickles, J.C.; Moulding, D.A.; Avery, A.; Virasami, A.; Fairchild, A.R.; Tisdall, M.; et al. Identifying cellular signalling molecules in developmental disorders of the brain: Evidence from focal cortical dysplasia and tuberous sclerosis. Neuropathol. Appl. Neurobiol. 2021, 47, 781–795. [Google Scholar] [CrossRef] [PubMed]







| Multivariate Analysis | |||
|---|---|---|---|
| Parameters | Numbers | Pearson Correlation (r) | Significance (2-Tailed) |
| TERT expression | 688 | 0.705 | 1.52 × 10−104 * |
| Tumor grade | 686 | 0.456 | 1.30 × 10−36 * |
| ATRX expression | 688 | 0.454 | 3.24 × 10−36 * |
| Patients age | 686 | 0.446 | 6.59 × 10−35 * |
| IDH1 expression | 688 | 0.326 | 1.72 × 10−18 * |
| TP53 expression | 688 | 0.270 | 5.98 × 10−13 * |
| EGFR expression | 688 | 0.270 | 5.92 × 10−13 * |
| 1p19q status | 688 | 0.246 | 6.30 × 10−11 * |
| MKI67 expression | 688 | 0.230 | 1.10 × 10−09 * |
| OS time | 685 | −0.198 | 1.78 × 10−07 * |
| AXL expression | 688 | −0.231 | 9.36 × 10−10 * |
| PDGFRA expression | 688 | −0.239 | 2.33 × 10−10 * |
| CIC expression | 688 | −0.357 | 4.24 × 10−22 * |
| NF1 expression | 688 | −0.318 | 1.27 × 10−17 * |
| NF2 expression | 688 | −0.409 | 4.62 × 10−29 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, C.-T.; Li, Y.-F.; Chou, C.-H.; Huang, L.-C.; Huang, S.-M.; Hueng, D.-Y.; Tsai, C.-K.; Chen, Y.-H. GRPEL2 Knockdown Exerts Redox Regulation in Glioblastoma. Int. J. Mol. Sci. 2021, 22, 12705. https://doi.org/10.3390/ijms222312705
Tang C-T, Li Y-F, Chou C-H, Huang L-C, Huang S-M, Hueng D-Y, Tsai C-K, Chen Y-H. GRPEL2 Knockdown Exerts Redox Regulation in Glioblastoma. International Journal of Molecular Sciences. 2021; 22(23):12705. https://doi.org/10.3390/ijms222312705
Chicago/Turabian StyleTang, Chi-Tun, Yao-Feng Li, Chung-Hsing Chou, Li-Chun Huang, Shih-Ming Huang, Dueng-Yuan Hueng, Chia-Kuang Tsai, and Yuan-Hao Chen. 2021. "GRPEL2 Knockdown Exerts Redox Regulation in Glioblastoma" International Journal of Molecular Sciences 22, no. 23: 12705. https://doi.org/10.3390/ijms222312705
APA StyleTang, C.-T., Li, Y.-F., Chou, C.-H., Huang, L.-C., Huang, S.-M., Hueng, D.-Y., Tsai, C.-K., & Chen, Y.-H. (2021). GRPEL2 Knockdown Exerts Redox Regulation in Glioblastoma. International Journal of Molecular Sciences, 22(23), 12705. https://doi.org/10.3390/ijms222312705









