Evaluation of the Skin-Sensitizing Potential of Brazilian Green Propolis
Abstract
:1. Introduction
2. Results and Discussion
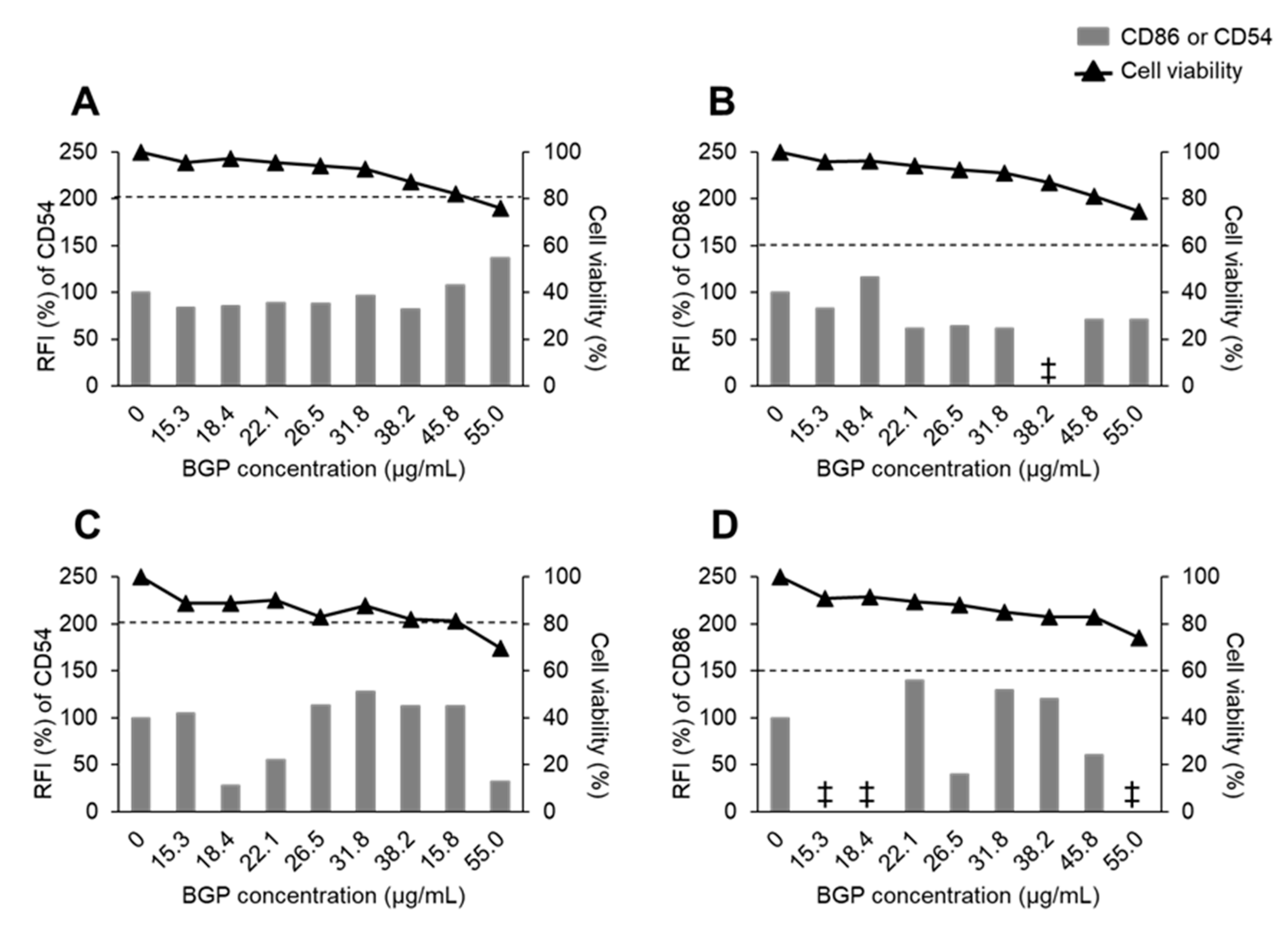
2.1. Sensitization Potency of BGP in h-CLAT
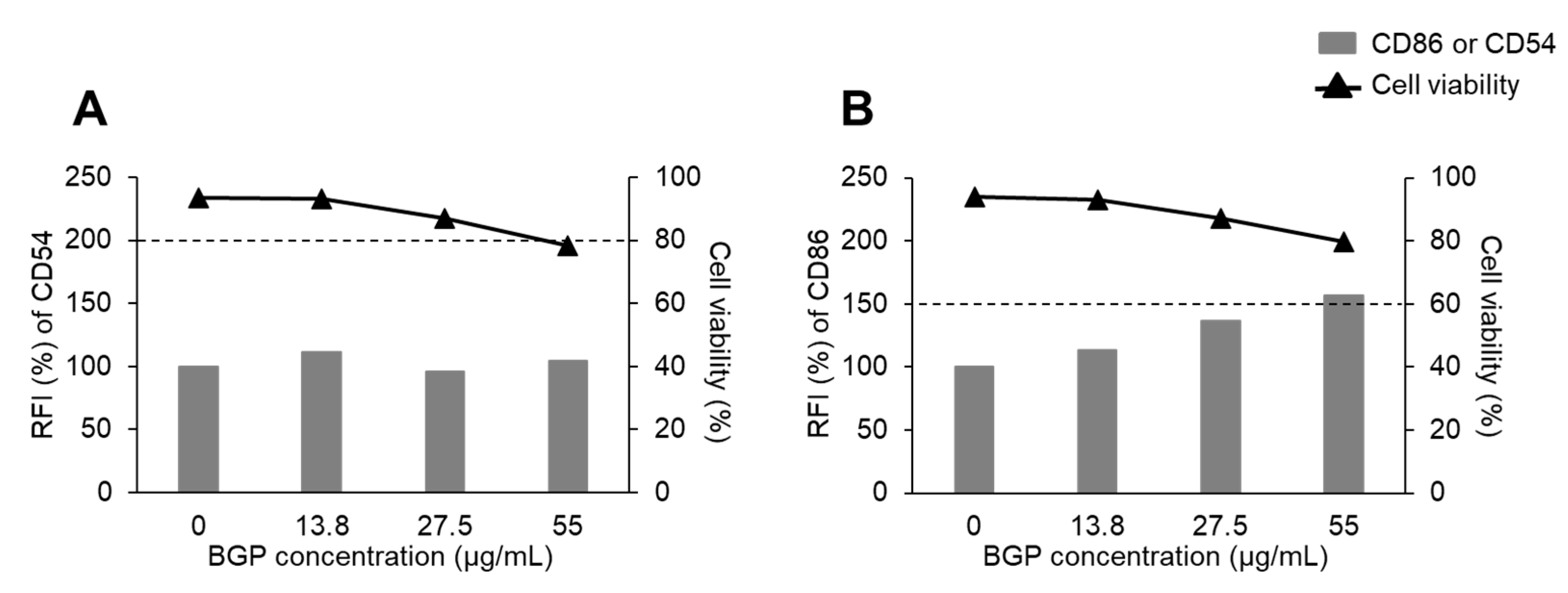
2.2. Sensitization Potency of BGP in a Modified In Vitro Test Using DC2.4 Cells
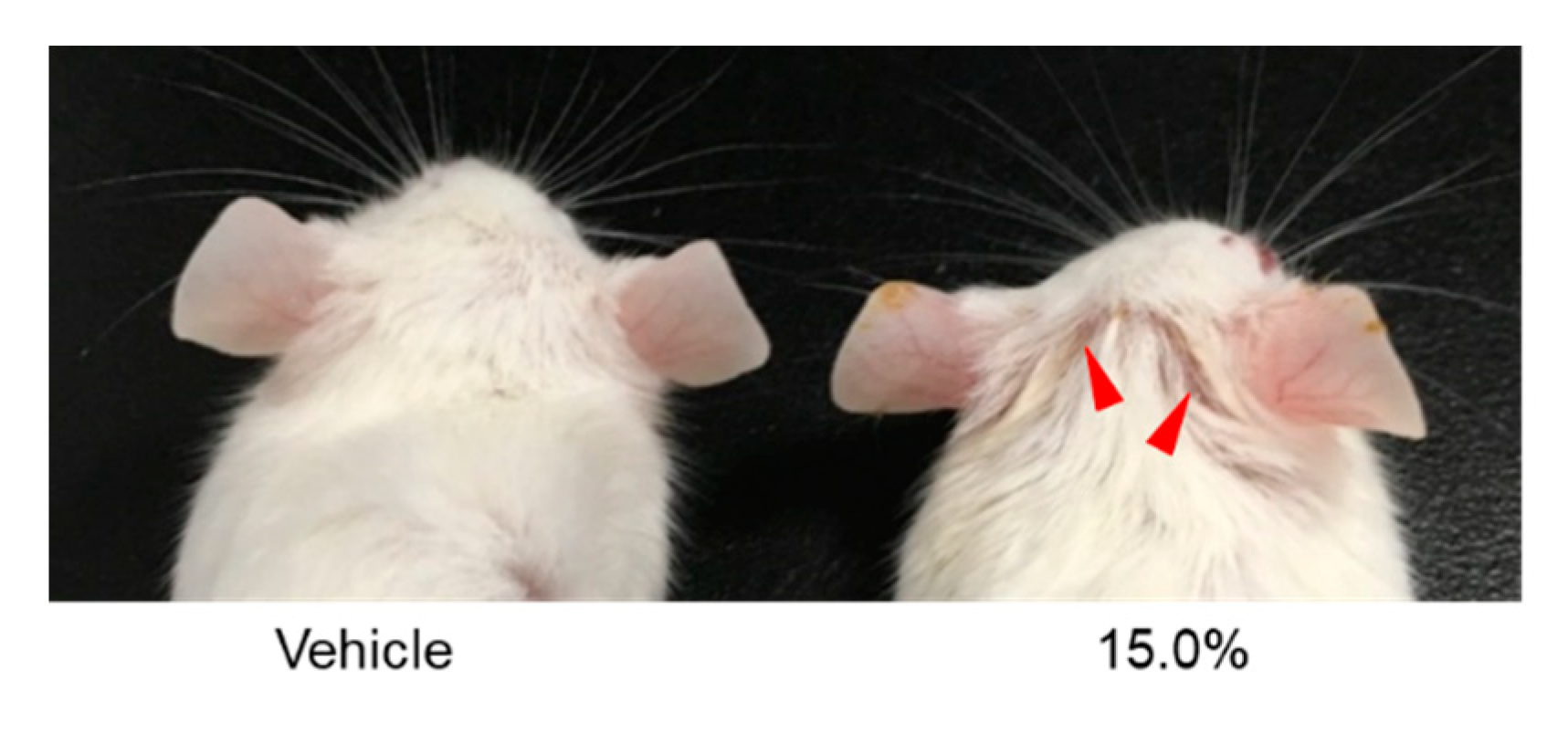
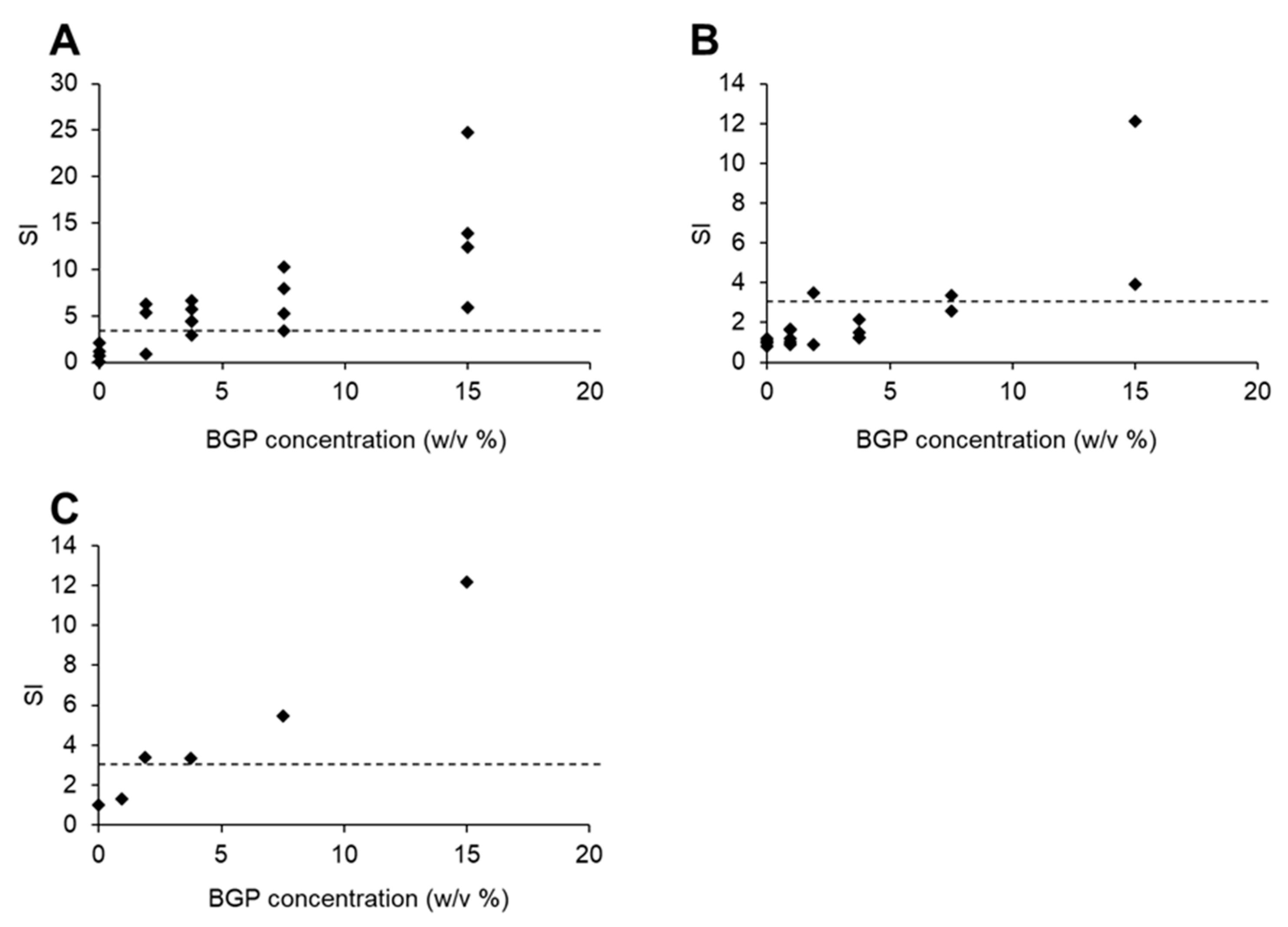
2.3. Evaluation of Skin Sensitization Potency of BGP by LLNA
3. Materials and Methods
3.1. Test Substances
3.2. Cell Cultures
3.3. Animals
3.4. Detection of Cell Viability
3.5. In Vitro Antigenicity Test
3.6. LLNA
3.7. Estimation of Skin Sensitization Potency from LLNA Results
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wagh, V.D. Propolis: A wonder bees product and its pharmacological potentials. Adv. Pharmacol. Sci. 2013, 2013, 308249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burdock, G.A. Review of the biological properties and toxicity of bee propolis (propolis). Food Chem. Toxicol. 1998, 36, 347–363. [Google Scholar] [CrossRef]
- Huang, S.; Zhang, C.P.; Wang, K.; Li, G.Q.; Hu, F.L. Recent advances in the chemical composition of propolis. Molecules 2014, 19, 19610–19632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasiotis, K.M.; Anastasiadou, P.; Papadopoulos, A.; Machera, K. Revisiting Greek Propolis: Chromatographic Analysis and Antioxidant Activity Study. PLoS ONE 2017, 12, e0170077. [Google Scholar] [CrossRef] [Green Version]
- Silva-Beltrán, N.P.; Balderrama-Carmona, A.P.; Umsza-Guez, M.A.; Souza Machado, B.A. Antiviral effects of Brazilian green and red propolis extracts on Enterovirus surrogates. Environ. Sci. Pollut. Res. Int. 2020, 27, 28510–28517. [Google Scholar] [CrossRef]
- Bankova, V. Recent trends and important developments in propolis research. Evid.-Based Complement. Alternat. Med. 2005, 2, 29–32. [Google Scholar] [CrossRef] [Green Version]
- Sforcin, J.M.; Bankova, V. Propolis: Is there a potential for the development of new drugs? J. Ethnopharmacol. 2011, 133, 253–260. [Google Scholar] [CrossRef]
- Gardana, C.; Simonetti, P. Evaluation of allergens in propolis by ultra-performance liquid chromatography/tandem mass spectrometry. Rapid Commun. Mass Spectrom. 2011, 25, 1675–1682. [Google Scholar] [CrossRef]
- De Groot, A.C. Propolis: A review of properties, applications, chemical composition, contact allergy, and other adverse effects. Dermatitis 2013, 24, 263–282. [Google Scholar] [CrossRef]
- Berretta, A.A.; Arruda, C.; Miguel, F.G.; Baptista, N.; Nascimento, A.P.; Marquele-Oliveira, F.; Hori, J.I.; Barud, H.; Damaso, B.; Ramos, C.; et al. Functional Properties of Brazilian Propolis: From Chemical Composition until the Market; IntechOpen: London, UK, 2017; Volume 4, pp. 55–96. [Google Scholar] [CrossRef] [Green Version]
- Talas, Z.S.; Gulhan, M.F.; Erdogan, K.; Orun, I. Antioxidant effects of propolis on carp Cyprinus carpio exposed to arsenic: Biochemical and histopathologic findings. Dis. Aquat. Organ. 2014, 108, 241–249. [Google Scholar] [CrossRef]
- Machado, B.A.S.; de Abreu Barreto, G.; Costa, A.S.; Costa, S.S.; Silva, R.P.D.; da Silva, D.F.; Brandão, H.N.; da Rocha, J.L.C.; Nunes, S.B.; Umsza-Guez, M.A.; et al. Determination of Parameters for the Supercritical Extraction of Antioxidant Compounds from Green Propolis Using Carbon Dioxide and Ethanol as Co-Solvent. PLoS ONE 2015, 10, e0134489. [Google Scholar] [CrossRef] [PubMed]
- Devequi-Nunes, D.; Machado, B.A.S.; de Abreu Barreto, G.; Rebouças Silva, J.; da Silva, D.F.; da Rocha, J.L.C.; Brandão, H.N.; Borges, V.M.; Umsza-Guez, M.A. Chemical characterization and biological activity of six different extracts of propolis through conventional methods and supercritical extraction. PLoS ONE 2018, 13, e0207676. [Google Scholar] [CrossRef]
- Badr, G.; Sayed, E.A.; Waly, H.; Hassan, K.A.H.; Mahmoud, M.H.; Selamoglu, Z. The Therapeutic Mechanisms of Propolis Against CCl4-Mediated Liver Injury by Mediating Apoptosis of Activated Hepatic Stellate Cells and Improving the Hepatic Architecture through PI3K/AKT/mTOR, TGF-β/Smad2, Bcl2/BAX/P53 and iNOS Signaling Pathways. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2019, 53, 301–322. [Google Scholar] [CrossRef]
- Walgrave, S.E.; Warshaw, E.M.; Glesne, L.A. Allergic contact dermatitis from propolis. Dermatitis 2005, 16, 209–215. [Google Scholar] [CrossRef]
- Uter, W.; Bauer, A.; Belloni, A.F.; Bircher, A.J.; Brans, R.; Buhl, T.; Cooper, S.M. Patch Test Results with the European Baseline Series and Additions Thereof in the ESSCA Network, 2015–2018. Contact Dermat. 2021, 84, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Petersen, H.O. Hypersensitivity to propolis. Contact Dermat. 1977, 3, 278–279. [Google Scholar] [CrossRef] [PubMed]
- Hausen, B.M.; Wollenweber, E.; Senff, H.; Post, B. Propolis allergy. (II). The sensitizing properties of 1,1-dimethylallyl caffeic acid ester. Contact Dermat. 1987, 17, 171–177. [Google Scholar] [CrossRef]
- Hausen, B.M.; Evers, P.; Stüwe, H.-T.; König, W.A.; W7ollenweber, E. Propolis Allergy (IV). Studies with Further Sensitizers from Propolis and Constituents Common to Propolis, Poplar Buds and Balsam of Peru. Contact Dermat. 1992, 26, 34–44. [Google Scholar] [CrossRef]
- Uter, W.; Gefeller, O.; Mahler, V.; Geier, J. Trends and Current Spectrum of Contact Allergy in Central Europe: Results of the Information Network of Departments of Dermatology (IVDK) 2007–2018. Br. J. Dermatol. 2020, 183, 857–865. [Google Scholar] [CrossRef]
- DeKoven, J.G.; Silverberg, J.I.; Warshaw, E.M.; Atwater, A.R.; Reeder, M.J.; Sasseville, D.; Taylor, J.S.; Zug, K.A.; Belsito, D.V.; Maibach, H.I.; et al. North American Contact Dermatitis Group Patch Test Results: 2017–2018. Dermatitis 2021, 32, 111–123. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Luo, L.; Zhang, H.; Yang, X.; Lv, Y.; Song, H. Common aroma-active components of propolis from 23 regions of China. J. Sci. Food Agric. 2010, 90, 1268–1282. [Google Scholar] [CrossRef]
- Bogdanov, S. Propolis: Biological properties and medical applications. In The Propolis Book; Bee Product Science: Muehlethurnen, Switzerland, 2017; Chapter 2. [Google Scholar]
- Nukada, Y.; Ashikaga, T.; Miyazawa, M.; Hirota, M.; Sakaguchi, H.; Sasa, H.; Nishiyama, N. Prediction of skin sensitization potency of chemicals by human Cell Line Activation Test (h-CLAT) and an attempt at classifying skin sensitization potency. Toxicol. Vitr. 2012, 26, 1150–1160. [Google Scholar] [CrossRef]
- Berges, C.; Naujokat, C.; Tinapp, S.; Wieczorek, H.; Hoeh, A.; Sadeghi, M.; Opelz, G.; Daniel, V. A cell line model for the differentiation of human dendritic cells. Biochem. Biophys. Res. Commun. 2005, 333, 896–907. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, E.; Ido, A.; Hiromori, Y.; Tanaka, K.; Kimura, T.; Nagase, H.; Nakanishi, T. Utility of Murine Dendritic Cell Line DC2.4 for in Vitro Assay of Skin-Sensitization Potential. Fundam. Toxicol. Sci. 2017, 4, 121–126. [Google Scholar] [CrossRef] [Green Version]
- Fang, F.; Wang, Y.; Li, R.; Zhao, Y.; Guo, Y.; Jiang, M.; Sun, J.; Ma, Y.; Ren, Z.; Tian, Z.; et al. Transcription Factor E2F1 Suppresses Dendritic Cell Maturation. J. Immunol. 2010, 184, 6084–6091. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, A.; Wakita, H.; Yoshikawa, T.; Nakanishi, T.; Tsutsumi, Y.; Mayumi, T.; Mukai, Y.; Yoshioka, Y.; Okada, N.; Nakagawa, S. A strategy for efficient cross-presentation of CTL-epitope peptides leading to enhanced induction of in vivo tumor immunity. J. Control. Release 2007, 117, 11–19. [Google Scholar] [CrossRef]
- Kato, S.; Koizumi, K.; Yamada, M.; Inujima, A.; Takeno, N.; Nakanishi, T.; Sakurai, H.; Nakagawa, S.; Saiki, I. A phagocytotic inducer from herbal constituent, pentagalloylglucose enhances lipoplex-mediated gene transfection in dendritic cells. Biol. Pharm. Bull. 2010, 33, 1878–1885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, N.; Tsujino, M.; Hagiwara, Y.; Tada, A.; Tamura, Y.; Mori, K.; Saito, T.; Nakagawa, S.; Mayumi, T.; Fujita, T.; et al. Administration route-dependent vaccine efficiency of murine dendritic cells pulsed with antigens. Br. J. Cancer 2001, 84, 1564–1570. [Google Scholar] [CrossRef] [Green Version]
- Takekoshi, T.; Tada, Y.; Watanabe, T.; Sugaya, M.; Hoashi, T.; Komine, M.; Kawashima, T.; Shimizu, T.; Hau, C.S.; Asahina, A.; et al. Identification of a Novel Marker for Dendritic Cell Maturation, Mouse Transmembrane Protein 123. J. Biol. Chem. 2010, 285, 31876–31884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angers-Loustau, A.; Tosti, L.; Casati, S. The Regulatory Use of the Local Lymph Node Assay for the Notification of New Chemicals in Europe. Regul. Toxicol. Pharmacol. 2011, 60, 300–307. [Google Scholar] [CrossRef]
- Woolhiser, M.R.; Munson, A.E.; Meade, B.J. Comparison of mouse strains using the local lymph node assay. Toxicology 2000, 146, 221–227. [Google Scholar] [CrossRef]
- Nishijo, T.; Miyazawa, K.; Saito, Y.; Otsubo, H.; Mizumachi, H.; Sakaguchi, H. Sensitivity of KeratinoSens™ and H-CLAT for Detecting Minute Amounts of Sensitizers to Evaluate Botanical Extract. J. Toxicol. Sci. 2019, 44, 13–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takenouchi, O.; Miyazawa, M.; Saito, K.; Ashikaga, T.; Sakaguchi, H. Predictive performance of the human Cell Line Activation Test (h-CLAT) for lipophilic chemicals with high octanol-water partition coefficients. J. Toxicol. Sci. 2013, 38, 599–609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, Z.; Reznikoff, G.; Dranoff, G.; Rock, K.L.G. Cloned Dendritic Cells Can Present Exogenous Antigens on Both MHC Class I and Class II Molecules. J. Immunol. 1997, 158, 2723–2730. [Google Scholar] [PubMed]
- Basketter, D.A.; Lea, L.J.; Dickens, A.; Briggs, D.; Pate, I.; Dearman, R.J.; Kimber, I. A Comparison of Statistical Approaches to the Derivation of EC3 Values from Local Lymph Node Assay Dose Responses. J. Appl. Toxicol. 1999, 19, 261–266. [Google Scholar] [CrossRef]
- Kimber, I.; Basketter, D.A.; Berthold, K.; Butler, M.; Garrigue, J.L.; Lea, L.; Newsome, C.; Roggeband, R.; Steiling, W.; Stropp, G.; et al. FORUM Skin Sensitization Testing in Potency and Risk Assessment. Toxicol. Sci. 2001, 59, 198–208. [Google Scholar] [CrossRef] [Green Version]

| Experiment | Concentration % (w/v) | DPM a (Mean or Mean ± 1 S.D.) | Number of Animals Used |
|---|---|---|---|
| Exp. 1 | 0.00 | 328.7 ± 276.5 | 4 |
| 1.88 | 1377.2 ± 939.8 | 3 | |
| 3.75 | 1587.2 ± 467.5 | 5 | |
| 7.50 | 2208.0 ± 983.4 | 4 | |
| 15.00 | 4685.4 ± 2574.1 | 4 | |
| Exp. 2 | 0.00 | 329.8 ± 55.3 | 4 |
| 0.94 | 422.8 ± 113.1 | 5 | |
| 1.88 | 720.9 | 2 | |
| 3.75 | 501.3 ± 143.7 | 4 | |
| 7.50 | 983.8 | 2 | |
| 15.00 | 2644.9 | 2 |
| Component Classification | Compound Name | Structure | Content (mg/g) a |
|---|---|---|---|
| Cinnamic acid derivatives | Artepillin C | 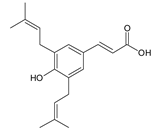 | 163.87 |
| Baccharin |  | 47.31 | |
| Drupanin |  | 19.89 | |
| p-Coumaric acid | 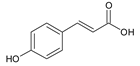 | 21.95 | |
| Flavonoids | Kaempferide |  | 27.79 |
| Dihydrokaempferide | 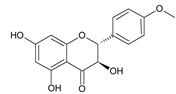 | 16.41 | |
| Betuletol | 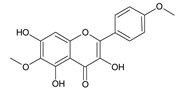 | 16.44 | |
| Isosakuranetin | 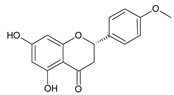 | 4.83 | |
| Kaempferol | 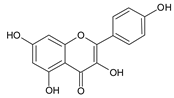 | 2.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shiraishi, E.; Ishida, K.; Matsumaru, D.; Ido, A.; Hiromori, Y.; Nagase, H.; Nakanishi, T. Evaluation of the Skin-Sensitizing Potential of Brazilian Green Propolis. Int. J. Mol. Sci. 2021, 22, 13538. https://doi.org/10.3390/ijms222413538
Shiraishi E, Ishida K, Matsumaru D, Ido A, Hiromori Y, Nagase H, Nakanishi T. Evaluation of the Skin-Sensitizing Potential of Brazilian Green Propolis. International Journal of Molecular Sciences. 2021; 22(24):13538. https://doi.org/10.3390/ijms222413538
Chicago/Turabian StyleShiraishi, Erina, Keishi Ishida, Daisuke Matsumaru, Akiko Ido, Youhei Hiromori, Hisamitsu Nagase, and Tsuyoshi Nakanishi. 2021. "Evaluation of the Skin-Sensitizing Potential of Brazilian Green Propolis" International Journal of Molecular Sciences 22, no. 24: 13538. https://doi.org/10.3390/ijms222413538






