Selenium Compounds as Novel Potential Anticancer Agents
Abstract
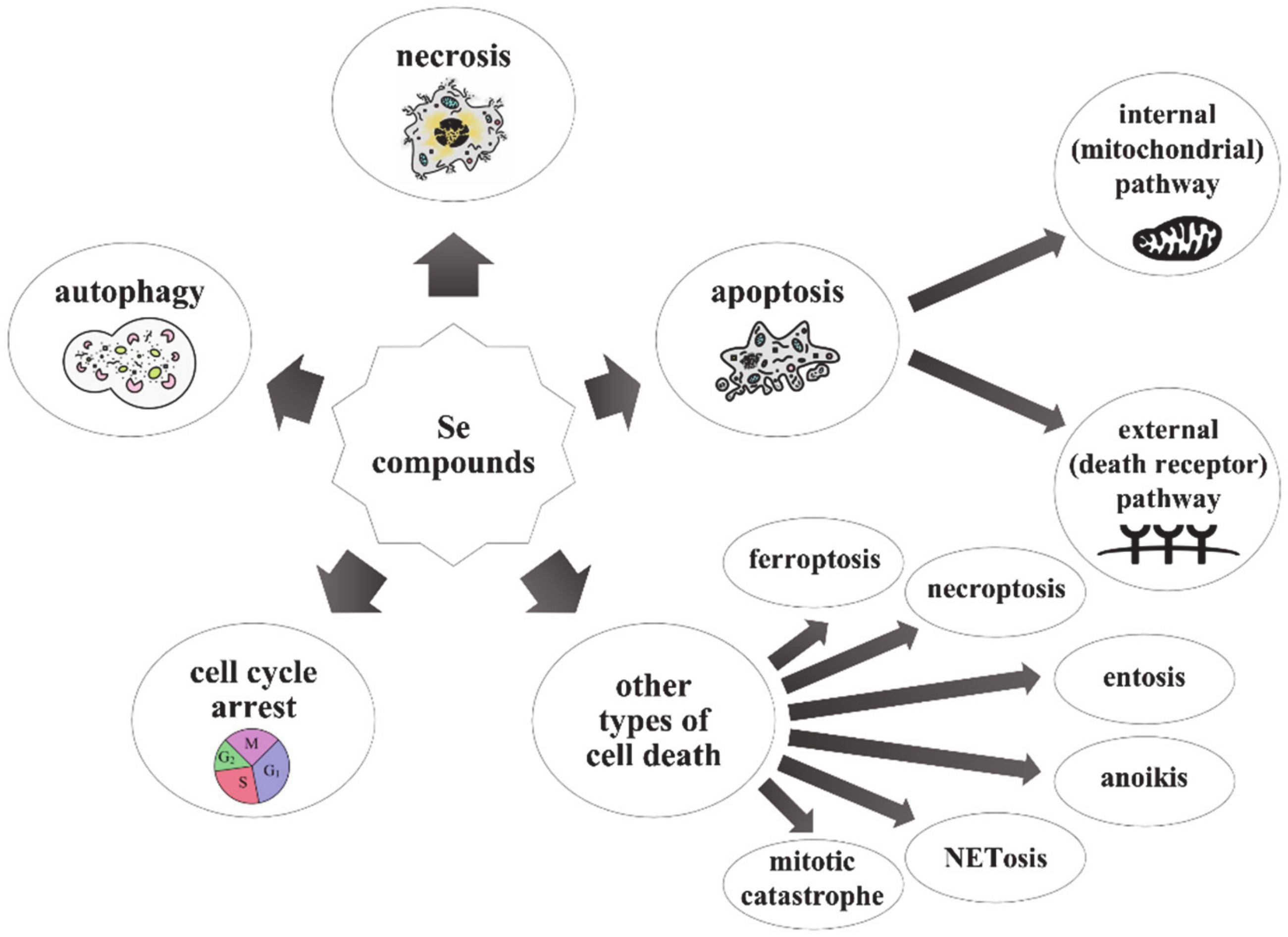
1. Introduction
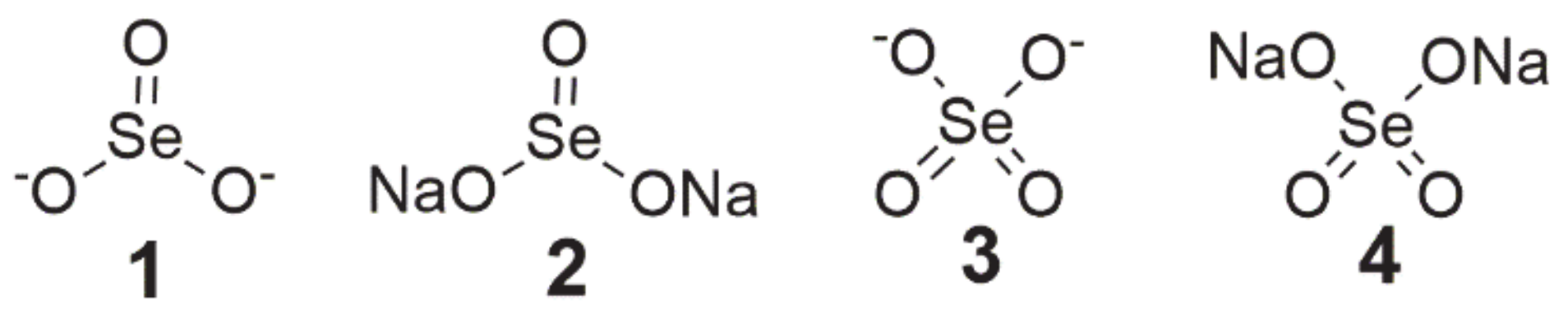
2. Inorganic Selenium Compounds
3. Organic Selenium Compounds
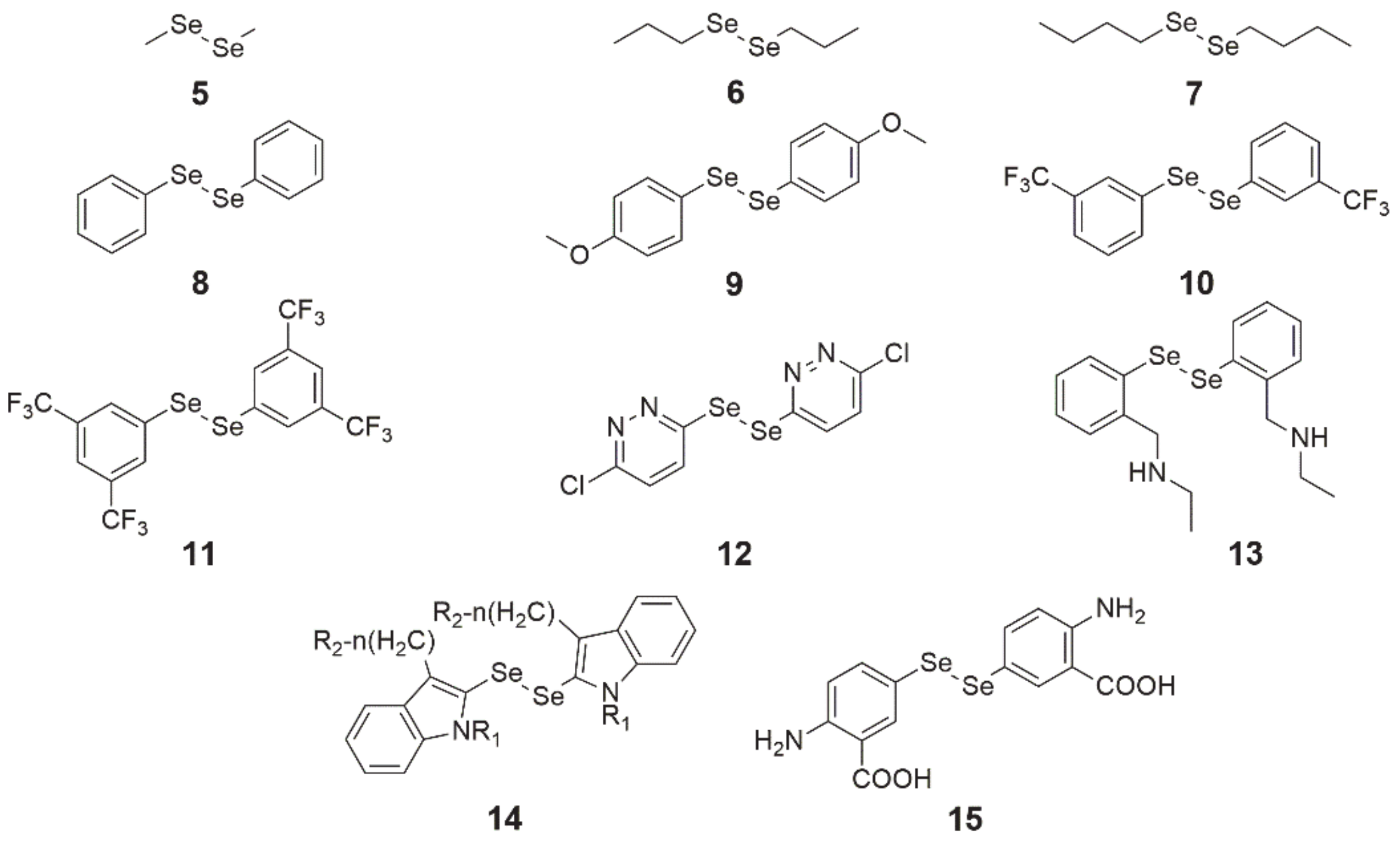
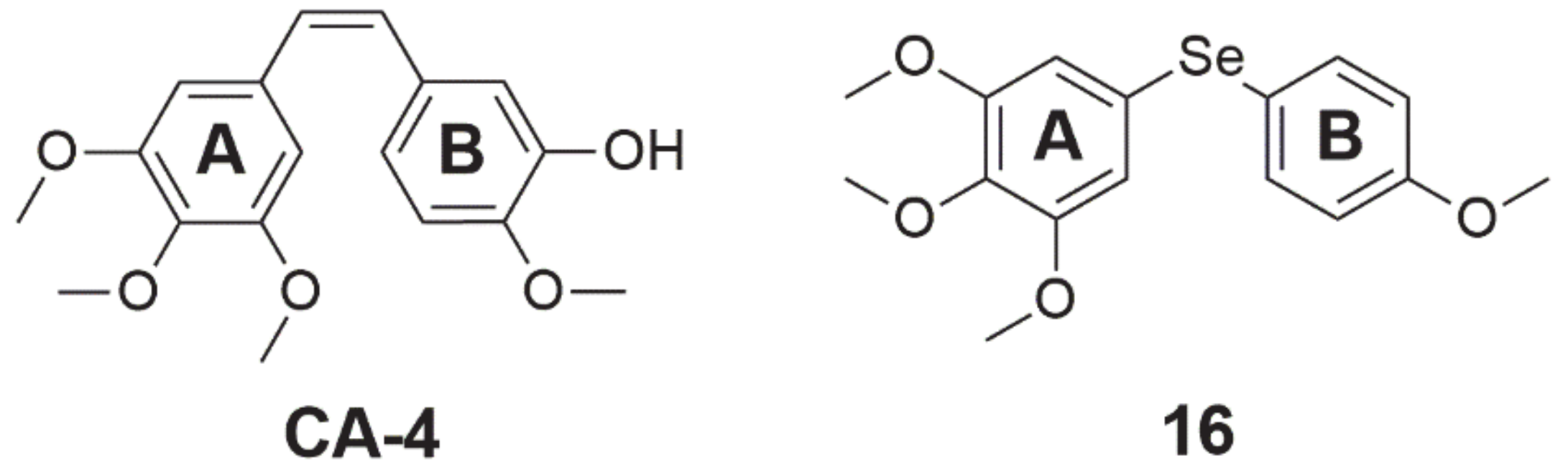
3.1. Diselenides
3.2. Selenides
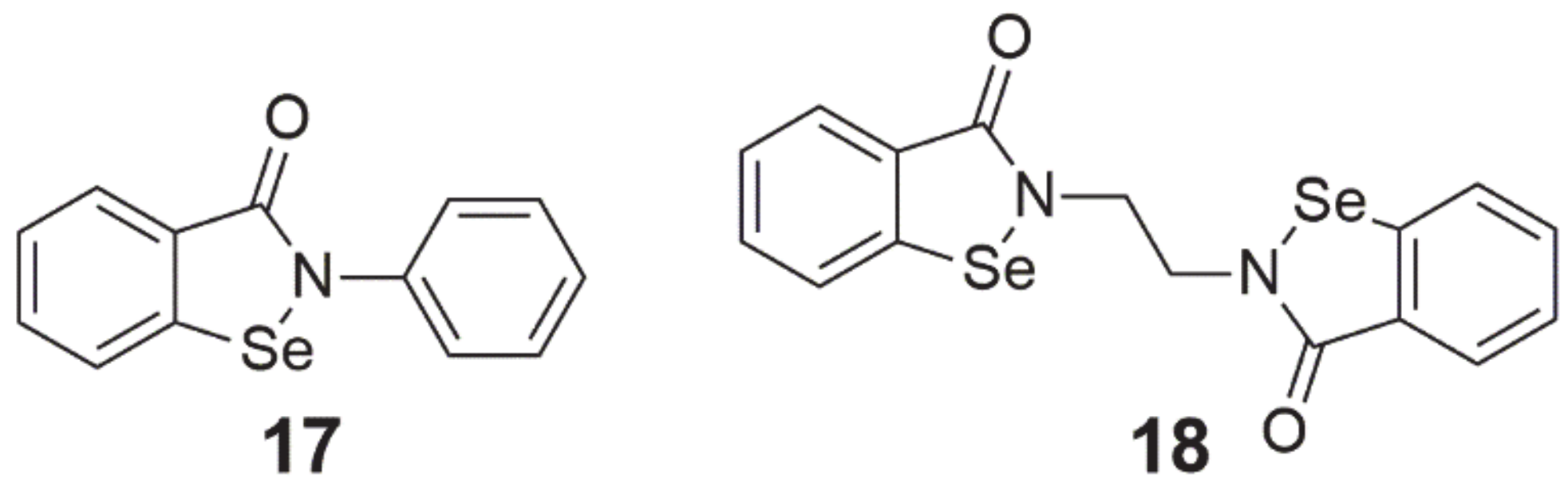
3.3. 1,2-Benzisoselenazole-3[2H]-One Derivatives
3.4. Selenophene-Based Derivative
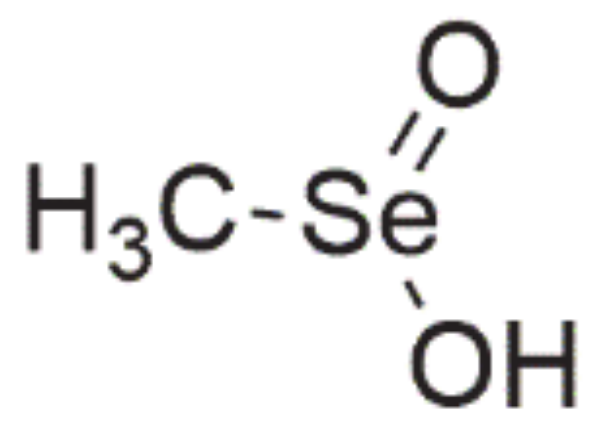
3.5. Seleninic Acids
3.6. Selenoesters
3.7. Selol
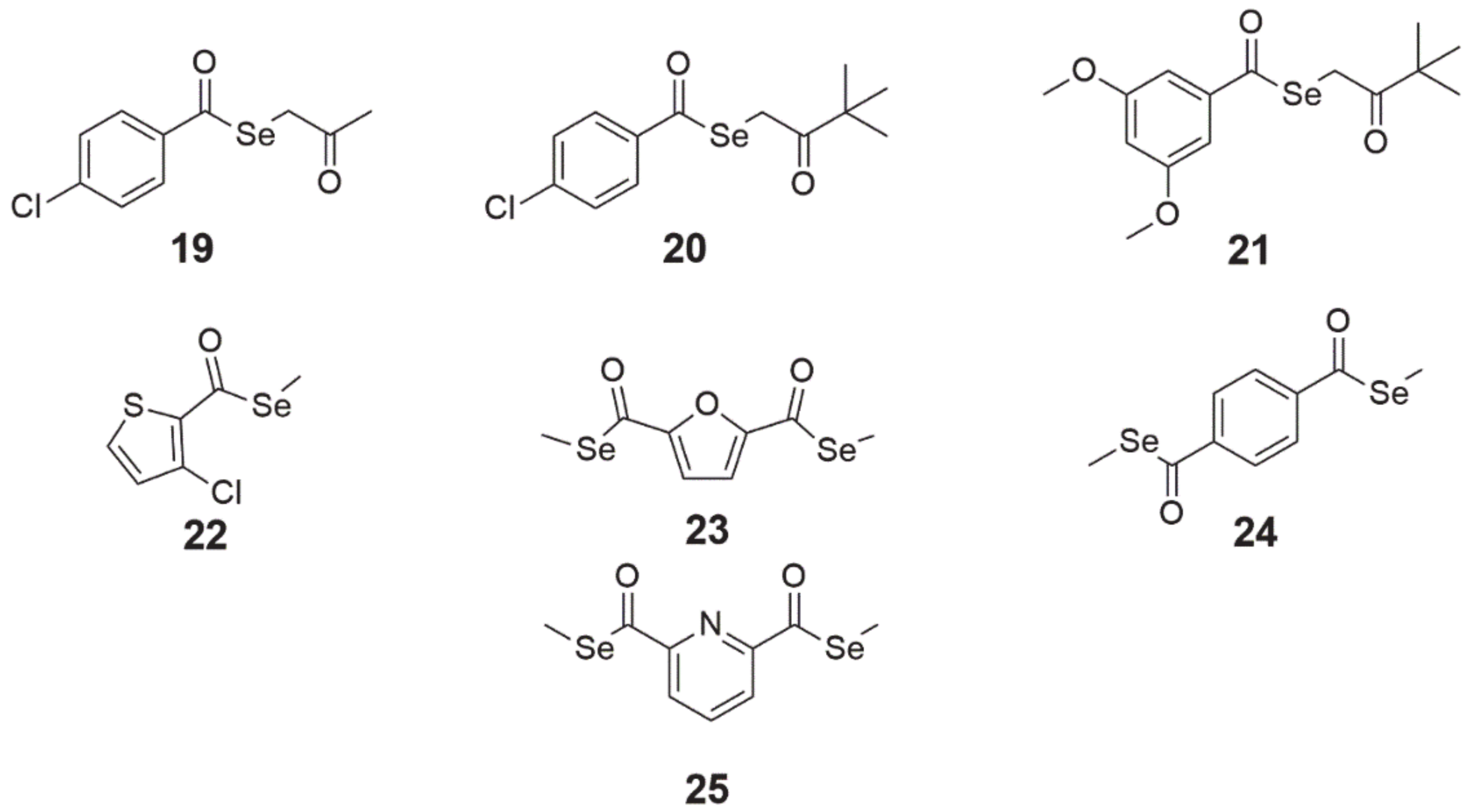
4. Selenoamino Acids
4.1. Selenomethionine
4.2. Methylselenocysteine
4.3. Selenocysteine
4.4. Selenocystine
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rocha, J.B.; Piccoli, B.; Oliveira, C.S.; Joule, J. Biological and chemical interest in selenium: A brief historical account. Arkivoc 2017, 2017, 457–491. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; El-Bayoumy, K. Apoptosis is a critical cellular event in cancer chemoprevention and chemotherapy by selenium compounds. Curr. Cancer Drug Targets 2004, 4, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Soriano-Garcia, M. Organoselenium compounds as potential therapeutic and chemopreventive agents: A review. Curr. Med. Chem. 2004, 11, 1657–1669. [Google Scholar] [CrossRef] [PubMed]
- Naithani, R. Organoselenium compounds in cancer chemoprevention. Mini Rev. Med. Chem. 2008, 8, 657–668. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.W.; Mo, H.-Y.; Lau, A.T.Y.; Xu, Y.-M. Selenium species: Current status and potentials in cancer prevention and therapy. Int. J. Mol. Sci. 2018, 20, 75. [Google Scholar] [CrossRef]
- Sanmartín, C.; Plano, D.; Sharma, A.K.; Palop, J.A. Selenium compounds, apoptosis and other types of cell death: An overview for cancer therapy. Int. J. Mol. Sci. 2012, 13, 9649–9672. [Google Scholar] [CrossRef]
- Gandin, V.; Khalkar, P.; Braude, J.; Fernandes, A.P. Organic selenium compounds as potential chemotherapeutic agents for improved cancer treatment. Free Radic. Biol. Med. 2018, 127, 80–97. [Google Scholar] [CrossRef]
- Harmanci, D.; Erbayraktar, Z.; Sayin, O.; Guner, G.A. In vitro effects of selenium on human glioblastoma multiforme cell lines: A preliminary study. Acta Clin. Croat. 2017, 56, 48–57. [Google Scholar] [CrossRef]
- Zeng, H.; Wu, M. The inhibitory efficacy of methylseleninic acid against colon cancer xenografts in C57BL/6 Mice. Nutr. Cancer 2015, 67, 831–838. [Google Scholar] [CrossRef]
- Zeng, H.; Briske-Anderson, M.; Wu, M.; Moyer, M.P. Methylselenol, a selenium metabolite, plays common and different roles in cancerous colon HCT116 cell and noncancerous NCM460 colon cell proliferation. Nutr. Cancer 2012, 64, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Lai, H.; Hou, L.; Chen, T. Rational design and action mechanisms of chemically innovative organoselenium in cancer therapy. Chem. Commun. 2020, 56, 179–196. [Google Scholar] [CrossRef] [PubMed]
- Misra, S.; Boylan, M.; Selvam, A.; Spallholz, J.E.; Björnstedt, M. Redox-active selenium compounds-from toxicity and cell death to cancer treatment. Nutrients 2015, 7, 3536–3556. [Google Scholar] [CrossRef] [PubMed]
- Subburayan, K.; Thayyullathil, F.; Pallichankandy, S.; Cheratta, A.R.; Galadari, S. Superoxide-mediated ferroptosis in human cancer cells induced by sodium selenite. Transl. Oncol. 2020, 13, 100843. [Google Scholar] [CrossRef] [PubMed]
- Khalkar, P.; Díaz-Argelich, N.; Antonio Palop, J.; Sanmartín, C.; Fernandes, A.P. Novel methylselenoesters induce programed cell death via entosis in pancreatic cancer cells. Int. J. Mol. Sci. 2018, 19, 2849. [Google Scholar] [CrossRef]
- Jiang, C.; Wang, Z.; Ganther, H.; Lu, J. Caspases as key executors of methyl selenium-induced apoptosis (Anoikis) of DU-145 prostate cancer cells. Cancer Res. 2001, 61, 3062–3070. [Google Scholar] [PubMed]
- Zhang, Y.; Cartland, S.P.; Henriquez, R.; Patel, S.; Gammelgaard, B.; Flouda, K.; Hawkins, C.L.; Rayner, B.S. Selenomethionine supplementation reduces lesion burden, improves vessel function and modulates the inflammatory response within the setting of atherosclerosis. Redox Biol. 2020, 29, 101409. [Google Scholar] [CrossRef]
- Mou, Y.; Wang, J.; Wu, J.; He, D.; Zhang, C.; Duan, C.; Li, B. Ferroptosis, a new form of cell death: Opportunities and challenges in cancer. J. Hematol. Oncol. 2019, 12, 34. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, S.; Li, J.; Li, Z.; Quan, J.; Liu, X.; Tang, Y.; Liu, B. The latest view on the mechanism of ferroptosis and its research progress in spinal cord injury. Oxid. Med. Cell. Longev. 2020, 2020, 6375938. [Google Scholar] [CrossRef]
- Tang, D.; Chen, X.; Kang, R.; Kroemer, G. Ferroptosis: Molecular mechanisms and health implications. Cell Res. 2020. [Google Scholar] [CrossRef]
- Ursini, F.; Maiorino, M. Lipid peroxidation and ferroptosis: The role of GSH and GPx4. Free Radic. Biol. Med. 2020, 152, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Ingold, I.; Conrad, M. Selenium and iron, two elemental rivals in the ferroptotic death process. Oncotarget 2018, 9, 22241–22242. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, B.R.; Hare, D.J.; Bush, A.I.; Roberts, B.R. Glutathione peroxidase 4: A new player in neurodegeneration? Mol. Psychiatry 2017, 22, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Li, G.-X.; Hu, H.; Jiang, C.; Schuster, T.; Lü, J. Differential involvement of reactive oxygen species in apoptosis induced by two classes of selenium compounds in human prostate cancer cells. Int. J. Cancer 2007, 120, 2034–2043. [Google Scholar] [CrossRef] [PubMed]
- Gasparian, A.V.; Yao, Y.J.; Lü, J.; Yemelyanov, A.Y.; Lyakh, L.A.; Slaga, T.J.; Budunova, I.V. Selenium compounds inhibit IκB Kinase (IKK) and Nuclear Factor-κB (NF-κB) in prostate cancer cells. Mol. Cancer Ther. 2002, 1, 1079–1087. [Google Scholar]
- Jiang, C.; Wang, Z.; Ganther, H.; Lü, J. Distinct effects of methylseleninic acid versus selenite on apoptosis, cell cycle, and protein kinase pathways in DU145 human prostate cancer cells. Mol. Cancer Ther. 2002, 1, 1059–1066. [Google Scholar]
- Li, G.-x.; Lee, H.-J.; Wang, Z.; Hu, H.; Liao, J.D.; Watts, J.C.; Combs, G.F., Jr.; Lü, J. Superior in vivo inhibitory efficacy of methylseleninic acid against human prostate cancer over selenomethionine or selenite. Carcinogenesis 2008, 29, 1005–1012. [Google Scholar] [CrossRef]
- Shen, C.L.; Song, W.; Pence, B.C. Interactions of selenium compounds with other antioxidants in DNA damage and apoptosis in human normal keratinocytes. Cancer Epidemiol. Biomarkers Prev. 2001, 10, 385–390. [Google Scholar]
- Gopalakrishna, R.; Gundimeda, U. Protein kinase C as a molecular target for cancer prevention by selenocompounds. Nutr. Cancer 2001, 40, 55–63. [Google Scholar] [CrossRef]
- Rikiishi, H. Apoptotic cellular events for selenium compounds involved in cancer prevention. J. Bioenerg. Biomembr. 2007, 39, 91–98. [Google Scholar] [CrossRef]
- Zhou, N.; Xiao, H.; Li, T.K.; Nur, E.K.A.; Liu, L.F. DNA damage-mediated apoptosis induced by selenium compounds. J. Biol. Chem. 2003, 278, 29532–29537. [Google Scholar] [CrossRef] [PubMed]
- De Miranda, J.X.; Andrade, F.d.O.; Conti, A.d.; Dagli, M.L.Z.; Moreno, F.S.; Ong, T.P. Effects of selenium compounds on proliferation and epigenetic marks of breast cancer cells. J. Trace Elem. Med. Biol. 2014, 28, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Chen, J.; Wu, Z.; Li, Y.; Zhu, Y.; Ren, Y.; Zhou, Q. Selenium compounds induce ROS in human high-metastatic large cell lung cancer cell line L9981. Zhongguo Fei Ai Za Zhi 2008, 11, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.-M.; Ding, W.-X.; Ong, C.-N. Intracellular glutathione is a cofactor in methylseleninic acid-induced apoptotic cell death of human hepatoma HEPG2 cells. Free Radic. Biol. Med. 2002, 33, 552–561. [Google Scholar] [CrossRef]
- Soukupová, K.; Rudolf, E. Suppression of proliferation and activation of cell death by sodium selenite involves mitochondria and lysosomes in chemoresistant bladder cancer cells. J. Trace Elem. Med. Biol. 2019, 52, 58–67. [Google Scholar] [CrossRef]
- Pang, K.-L.; Chin, K.-Y. Emerging Anticancer Potentials of Selenium on Osteosarcoma. Int. J. Mol. Sci. 2019, 20, 5318. [Google Scholar] [CrossRef]
- Shigemi, Z.; Manabe, K.; Hara, N.; Baba, Y.; Hosokawa, K.; Kagawa, H.; Watanabe, T.; Fujimuro, M. Methylseleninic acid and sodium selenite induce severe ER stress and subsequent apoptosis through UPR activation in PEL cells. Chem. Biol. Interact. 2017, 266, 28–37. [Google Scholar] [CrossRef]
- Kim, T.-S.; Yun, B.Y.; Kim, I.Y. Induction of the mitochondrial permeability transition by selenium compounds mediated by oxidation of the protein thiol groups and generation of the superoxide. Biochem. Pharmacol. 2003, 66, 2301–2311. [Google Scholar] [CrossRef]
- Gajdács, M.; Spengler, G.; Sanmartín, C.; Marć, M.A.; Handzlik, J.; Domínguez-Álvarez, E. Selenoesters and selenoanhydrides as novel multidrug resistance reversing agents: A confirmation study in a colon cancer MDR cell line. Bioorg. Med. Chem. Lett. 2017, 27, 797–802. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Study Evaluating Sodium Selenite in Combination with Abiraterone in Castrate Resistant Prostate Cancer Progressing on Abiraterone. Available online: https://clinicaltrials.gov/ct2/show/NCT04296578 (accessed on 7 January 2021).
- ClinicalTrials.gov. Phase I Sodium Selenite in Combination with Docetaxel in Castration-resistant Prostate Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT01155791 (accessed on 7 January 2021).
- ClinicalTrials.gov. Sodium Selenite and Radiation Therapy in Treating Patients with Metastatic Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT02184533 (accessed on 7 January 2021).
- ClinicalTrials.gov. The Use of Selenium to Treat Secondary Lymphedema—Breast Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT00188604 (accessed on 7 January 2021).
- ClinicalTrials.gov. Sodium Selenite as a Cytotoxic Agent in Advanced Carcinoma (SECAR). Available online: https://clinicaltrials.gov/ct2/show/NCT01959438 (accessed on 7 January 2021).
- ClinicalTrials.gov. High Dose Inorganic Selenium for Preventing Chemotherapy Induced Peripheral Neuropathy (SELENIUM). Available online: https://clinicaltrials.gov/ct2/show/NCT04201561 (accessed on 7 January 2021).
- Álvarez-Pérez, M.; Ali, W.; Marć, M.A.; Handzlik, J.; Domínguez-Álvarez, E. Selenides and Diselenides: A Review of Their Anticancer and Chemopreventive Activity. Molecules 2018, 23, 628. [Google Scholar] [CrossRef]
- Brigelius-Flohé, R. Selenium compounds and selenoproteins in cancer. Chem. Biodivers. 2008, 5, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Nedel, F.; Campos, V.F.; Alves, D.; McBride, A.J.A.; Dellagostin, O.A.; Collares, T.; Savegnago, L.; Seixas, F.K. Substituted diaryl diselenides: Cytotoxic and apoptotic effect in human colon adenocarcinoma cells. Life Sci. 2012, 91, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Posser, T.; de Paula, M.T.; Franco, J.L.; Leal, R.B.; da Rocha, J.B.T. Diphenyl diselenide induces apoptotic cell death and modulates ERK1/2 phosphorylation in human neuroblastoma SH-SY5Y cells. Arch. Toxicol. 2011, 85, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Lee, J.; Park, M.-S. Synthesis of new diorganodiselenides from organic halides: Their antiproliferative effects against human breast cancer MCF-7 cells. Arch. Pharmacal. Res. 2015, 38, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Krasowska, D.; Iraci, N.; Santi, C.; Drabowicz, J.; Cieslak, M.; Kaźmierczak-Barańska, J.; Palomba, M.; Królewska-Golińska, K.; Magiera, J.; Sancineto, L. Diselenides and benzisoselenazolones as antiproliferative agents and glutathione-s-transferase inhibitors. Molecules 2019, 24, 2914. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, C.W.; Rocha, J.B. Toxicology and pharmacology of selenium: Emphasis on synthetic organoselenium compounds. Arch. Toxicol. 2011, 85, 1313–1359. [Google Scholar] [CrossRef] [PubMed]
- Rosa, R.M.; Roesler, R.; Braga, A.L.; Saffi, J.; Henriques, J.A.P. Pharmacology and toxicology of diphenyl diselenide in several biological models. Braz. J. Med. Biol. Res. 2007, 40, 1287–1304. [Google Scholar] [CrossRef] [PubMed]
- Meinerz, D.F.; Allebrandt, J.; Mariano, D.O.C.; Waczuk, E.P.; Soares, F.A.; Hassan, W.; Rocha, J.B.T. Differential genotoxicity of diphenyl diselenide (PhSe)2 and diphenyl ditelluride (PhTe)2. PeerJ 2014, 2, e290. [Google Scholar] [CrossRef]
- Stefanello, S.T.; Dobrachinski, F.; de Carvalho, N.R.; Amaral, G.P.; Barcelos, R.P.; Oliveira, V.A.; Oliveira, C.S.; Giordani, C.F.A.; Pereira, M.E.; Rodrigues, O.E.D.; et al. Free radical scavenging in vitro and biological activity of diphenyl diselenide-loaded nanocapsules: DPDS-NCS antioxidant and toxicological effects. Int. J. Nanomed. 2015, 10, 5663–5670. [Google Scholar] [CrossRef]
- Chagas, P.M.; Bortolatto, C.F.; Wilhelm, E.A.; Nogueira, C.W. High doses of 2,2′-dithienyl diselenide cause systemic toxicity in rats: An in vitro and in vivo study. J. Appl. Toxicol. 2013, 33, 480–487. [Google Scholar] [CrossRef]
- Savegnago, L.; Jesse, C.R.; Nogueira, C.W. Structural modifications into diphenyl diselenide molecule do not cause toxicity in mice. Environ. Toxicol. Pharmacol. 2009, 27, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Marcondes Sari, M.H.; Ferreira, L.M.; Zborowski, V.A.; Araujo, P.C.O.; Cervi, V.F.; Brüning, C.A.; Cruz, L.; Nogueira, C.W. p,p’-Methoxyl-diphenyl diselenide-loaded polymeric nanocapsules are chemically stable and do not induce toxicity in mice. Eur. J. Pharm. Biopharm. 2017, 117, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, E.d.A.; Hamel, E.; Bai, R.; Burnett, J.C.; Tozatti, C.S.S.; Bogo, D.; Perdomo, R.T.; Antunes, A.M.M.; Marques, M.M.; Matos, M.d.F.C.; et al. Synthesis and evaluation of diaryl sulfides and diaryl selenide compounds for antitubulin and cytotoxic activity. Bioorg. Med. Chem. Lett. 2013, 23, 4669–4673. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhou, L.; Du, J.; Li, M.; Qian, C.; Cheng, Y.; Peng, Y.; Xie, J.; Wang, D. Induction of apoptosis in human multiple myeloma cell lines by ebselen via enhancing the endogenous reactive oxygen species production. Biomed Res. Int. 2014, 2014, 696107. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.F.; Shen, H.M.; Ong, C.N. Protective effect of ebselen against hydrogen peroxide-induced cytotoxicity and DNA damage in HepG2 cells. Biochem. Pharmacol. 1999, 57, 273–279. [Google Scholar] [CrossRef]
- Sharma, V.; Tewari, R.; Sk, U.H.; Joseph, C.; Sen, E. Ebselen sensitizes glioblastoma cells to Tumor Necrosis Factor (TNFalpha)-induced apoptosis through two distinct pathways involving NF-kappaB downregulation and Fas-mediated formation of death inducing signaling complex. Int. J. Cancer 2008, 123, 2204–2212. [Google Scholar] [CrossRef]
- Thabet, N.M.; Moustafa, E.M. Synergistic effect of Ebselen and gamma radiation on breast cancer cells. Int. J. Radiat. Biol. 2017, 93, 784–792. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Study to Evaluate the Safety and Pharmacokinetics of SPI-1005. Available online: https://clinicaltrials.gov/ct2/show/NCT01452607 (accessed on 7 January 2021).
- ClinicalTrials.gov. SPI-1005 for Prevention and Treatment of Chemotherapy Induced Hearing Loss. Available online: https://www.clinicaltrials.gov/ct2/show/NCT01451853 (accessed on 7 January 2021).
- Wang, L.; Yang, Z.; Fu, J.; Yin, H.; Xiong, K.; Tan, Q.; Jin, H.; Li, J.; Wang, T.; Tang, W.; et al. Ethaselen: A potent mammalian thioredoxin reductase 1 inhibitor and novel organoselenium anticancer agent. Free Radic. Biol. Med. 2012, 52, 898–908. [Google Scholar] [CrossRef]
- Tan, Q.; Li, J.; Yin, H.-w.; Wang, L.-h.; Tang, W.-c.; Zhao, F.; Liu, X.-m.; Zeng, H.-h. Augmented antitumor effects of combination therapy of cisplatin with ethaselen as a novel thioredoxin reductase inhibitor on human A549 cell in vivo. Investig. New Drugs 2010, 28, 205–215. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Ethaselen for the Treatment of Thioredoxin Reductase High Expression Advanced Non-small Cell Lung Cancers. Available online: https://clinicaltrials.gov/ct2/show/NCT02166242 (accessed on 27 November 2020).
- Sinha, I.; Allen, J.E.; Pinto, J.T.; Sinha, R. Methylseleninic acid elevates REDD1 and inhibits prostate cancer cell growth despite AKT activation and mTOR dysregulation in hypoxia. Cancer Med. 2014, 3, 252–264. [Google Scholar] [CrossRef]
- Li, Z.; Carrier, L.; Rowan, B.G. Methylseleninic acid synergizes with tamoxifen to induce caspase-mediated apoptosis in breast cancer cells. Mol. Cancer Ther. 2008, 7, 3056–3063. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Bonorden, M.J.L.; Li, G.-x.; Lee, H.-J.; Hu, H.; Zhang, Y.; Liao, J.D.; Cleary, M.P.; Lü, J. Methyl-selenium compounds inhibit prostate carcinogenesis in the transgenic adenocarcinoma of mouse prostate model with survival benefit. Cancer Prev. Res. 2009, 2, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Sinha, I.; Null, K.; Wolter, W.; Suckow, M.A.; King, T.; Pinto, J.T.; Sinha, R. Methylseleninic acid downregulates hypoxia-inducible factor-1α in invasive prostate cancer. Int. J. Cancer 2012, 130, 1430–1439. [Google Scholar] [CrossRef] [PubMed]
- Gundimeda, U.; Schiffman, J.E.; Chhabra, D.; Wong, J.; Wu, A.; Gopalakrishna, R. Locally generated methylseleninic acid induces specific inactivation of protein kinase C isoenzymes: Relevance to selenium-induced apoptosis in prostate cancer cells. J. Biol. Chem. 2008, 283, 34519–34531. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.D.; Jiang, C.; Malewicz, B.; Dong, Y.; Young, C.Y.F.; Kang, K.-S.; Lee, Y.-S.; Ip, C.; Lü, J. Methyl selenium metabolites decrease prostate-specific antigen expression by inducing protein degradation and suppressing androgen-stimulated transcription. Mol. Cancer Ther. 2004, 3, 605–612. [Google Scholar]
- Wu, X.; Zhang, Y.; Pei, Z.; Chen, S.; Yang, X.; Chen, Y.; Lin, D.; Ma, R.Z. Methylseleninic acid restricts tumor growth in nude mice model of metastatic breast cancer probably via inhibiting angiopoietin-2. BMC Cancer 2012, 12, 192. [Google Scholar] [CrossRef]
- Wang, L.; Walia, B.; Evans, J.; Gewirtz, A.T.; Merlin, D.; Sitaraman, S.V. IL-6 Induces NF-κB Activation in the Intestinal Epithelia. J. Immunol. 2003, 171, 3194–3201. [Google Scholar] [CrossRef]
- Hu, H.; Jiang, C.; Ip, C.; Rustum, Y.M.; Lü, J. Methylseleninic Acid Potentiates Apoptosis Induced by Chemotherapeutic Drugs in Androgen-Independent Prostate Cancer Cells. Clin. Cancer Res. 2005, 11, 2379–2388. [Google Scholar] [CrossRef][Green Version]
- Qi, Y.; Fu, X.; Xiong, Z.; Zhang, H.; Hill, S.M.; Rowan, B.G.; Dong, Y. Methylseleninic acid enhances paclitaxel efficacy for the treatment of triple-negative breast cancer. PLoS ONE 2012, 7, e31539. [Google Scholar] [CrossRef]
- Liu, Y.; Li, W.; Guo, M.; Li, C.; Qiu, C. Protective Role of Selenium Compounds on the Proliferation, Apoptosis, and Angiogenesis of a Canine Breast Cancer Cell Line. Biol. Trace Elem. Res. 2016, 169, 86–93. [Google Scholar] [CrossRef]
- Lafin, J.T.; Sarsour, E.H.; Kalen, A.L.; Wagner, B.A.; Buettner, G.R.; Goswami, P.C. Methylseleninic acid induces lipid peroxidation and radiation sensitivity in head and neck cancer cells. Int. J. Mol. Sci. 2019, 20, 225. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Argelich, N.; Encío, I.; Plano, D.; Fernandes, A.P.; Palop, J.A.; Sanmartín, C. Novel methylselenoesters as antiproliferative agents. Molecules 2017, 22, 1288. [Google Scholar] [CrossRef] [PubMed]
- Angeli, A.; Carta, F.; Supuran, C.T. Carbonic anhydrases: Versatile and useful biocatalysts in chemistry and biochemistry. Catalysts 2020, 10, 1008. [Google Scholar] [CrossRef]
- Delfino, R.T.; Ribeiro, T.S.; Figueroa-Villar, J.D. Organophosphorus compounds as chemical warfare agents: A review. J. Braz. Chem. Soc. 2009, 20, 407–428. [Google Scholar] [CrossRef]
- Domínguez-Álvarez, E.; Plano, D.; Font, M.; Calvo, A.; Prior, C.; Jacob, C.; Palop, J.A.; Sanmartín, C. Synthesis and antiproliferative activity of novel selenoester derivatives. Eur. J. Med. Chem. 2014, 73, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Álvarez, E.; Gajdács, M.; Spengler, G.; Palop, J.A.; Marć, M.A.; Kieć-Kononowicz, K.; Amaral, L.; Molnár, J.; Jacob, C.; Handzlik, J.; et al. Identification of selenocompounds with promising properties to reverse cancer multidrug resistance. Bioorg. Med. Chem. Lett. 2016, 26, 2821–2824. [Google Scholar] [CrossRef]
- Spengler, G.; Gajdács, M.; Marć, M.A.; Domínguez-Álvarez, E.; Sanmartín, C. Organoselenium compounds as novel adjuvants of chemotherapy drugs-a promising approach to fight cancer drug resistance. Molecules 2019, 24, 336. [Google Scholar] [CrossRef]
- White, E. Entosis: It’s a cell-eat-cell world. Cell 2007, 131, 840–842. [Google Scholar] [CrossRef]
- Rahden-Staroń, I.; Suchocki, P.; Czeczot, H. Evaluation of mutagenic activity of the organo-selenium compound Selol by use of the Salmonella typhimurium mutagenicity assay. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2010, 699, 44–46. [Google Scholar] [CrossRef]
- Jastrzebski, Z.; Czyzewska-Szafran, H.; Fijatek, Z.; Suchocki, P.; Fitak, B.A. Toxicity studies of a new selenium compound, Selol, in rats. Drugs Exp. Clin. Res. 1995, 21, 217–220. [Google Scholar]
- Ślusarczyk, J.; Dudek, M.; Wierzbicka, M.; Suchocki, P.; Kuraś, M. Antimitotic effect of Selol and sodium selenate (IV) on Allium test cells. Caryologia 2014, 67, 250–259. [Google Scholar] [CrossRef]
- Suchocki, P.; Misiewicz-Krzemińska, I.; Skupińska, K.; Niedźwiecka, K.; Lubelska, K.; Fijałek, Z.; Kasprzycka-Guttman, T. Selenitetriglicerydes affect CYP1A1 and QR activity by involvement of reactive oxygen species and Nrf2 transcription factor. Pharmacol. Rep. 2010, 62, 352–361. [Google Scholar] [CrossRef]
- Sonet, J.; Mosca, M.; Bierla, K.; Modzelewska, K.; Flis-Borsuk, A.; Suchocki, P.; Ksiazek, I.; Anuszewska, E.; Bulteau, A.-L.; Szpunar, J.; et al. Selenized plant oil is an efficient source of selenium for selenoprotein biosynthesis in human cell lines. Nutrients 2019, 11, 1524. [Google Scholar] [CrossRef] [PubMed]
- Suchocki, P.; Misiewicz, I.; Skupinska, K.; Waclawek, K.; Fijalek, Z.; Kasprzycka-Guttman, T. The activity of Selol in multidrug-resistant and sensitive human leukemia cells. Oncol. Rep. 2007, 18, 893–899. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Flis, A.; Suchocki, P.; Królikowska, M.A.; Suchocka, Z.; Remiszewska, M.; Śliwka, L.; Książek, I.; Sitarz, K.; Sochacka, M.; Hoser, G.; et al. Selenitetriglycerides-Redox-active agents. Pharmacol. Rep. 2015, 67, 1–8. [Google Scholar] [CrossRef]
- Grosicka-Maciąg, E.; Kurpios-Piec, D.; Woźniak, K.; Kowalewski, C.; Szumiło, M.; Drela, N.; Kiernozek, E.; Suchocki, P.; Rahden-Staroń, I. Selol (Se IV) modulates adhesive molecules in control and TNF-α-stimulated HMEC-1 cells. J. Trace Elem. Med. Biol. 2019, 51, 106–114. [Google Scholar] [CrossRef]
- Sochacka, M.; Giebułtowicz, J.; Remiszewska, M.; Suchocki, P.; Wroczyński, P. Effects of Selol 5% supplementation on the activity or concentration of antioxidants and malondialdehyde level in the blood of healthy mice. Pharmacol. Rep. 2014, 66, 301–310. [Google Scholar] [CrossRef]
- Dudkiewicz-Wilczyńska, J.; Grabowska, A.; Książek, I.; Sitarz, K.; Suchocki, P.; Anuszewska, E. Comparison of selected gene expression profiles in sensitive and resistant cancer cells treated with doxorubicin and Selol. Contemp. Oncol. 2014, 18, 90–94. [Google Scholar] [CrossRef]
- Bujalska, M.; Gumułka, S.W. Effect of selenium compound (selol) on the opioid activity in vincristine induced hyperalgesia. Neuro Endocrinol. Lett. 2008, 29, 552–557. [Google Scholar]
- Fan, C.-D.; Fu, X.-Y.; Zhang, Z.-Y.; Cao, M.-Z.; Sun, J.-Y.; Yang, M.-F.; Fu, X.-T.; Zhao, S.-J.; Shao, L.-R.; Zhang, H.-F.; et al. Selenocysteine induces apoptosis in human glioma cells: Evidence for TrxR1-targeted inhibition and signaling crosstalk. Sci. Rep. 2017, 7, 6465. [Google Scholar] [CrossRef]
- Smith, M.L.; Lancia, J.K.; Mercer, T.I.; Ip, C. Selenium compounds regulate p53 by common and distinctive mechanisms. Anticancer Res. 2004, 24, 1401–1408. [Google Scholar] [PubMed]
- Evans, S.O.; Jacobson, G.M.; Goodman, H.J.B.; Bird, S.; Jameson, M.B. Comparative Safety and Pharmacokinetic Evaluation of Three Oral Selenium Compounds in Cancer Patients. Biol. Trace Elem. Res. 2019, 189, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.; Oh, J.-H.; Park, J.-M.; Chung, A.-S. Methylselenol generated from selenomethionine by methioninase downregulates integrin expression and induces caspase-mediated apoptosis of B16F10 melanoma cells. J. Cell. Physiol. 2007, 212, 386–400. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Angulo, A.M.; Fuloria, J.; Prakash, O. Cyclooxygenase 2 inhibitors and colon cancer. Ochsner. J. 2002, 4, 176–179. [Google Scholar] [PubMed]
- Zeng, H.; Wu, M.; Botnen, J.H. Methylselenol, a selenium metabolite, induces cell cycle arrest in G1 phase and apoptosis via the extracellular-regulated kinase 1/2 pathway and other cancer signaling genes. J. Nutr. 2009, 139, 1613–1618. [Google Scholar] [CrossRef]
- Lee, J.-I.; Nian, H.; Cooper, A.J.L.; Sinha, R.; Dai, J.; Bisson, W.H.; Dashwood, R.H.; Pinto, J.T. Alpha-keto acid metabolites of naturally occurring organoselenium compounds as inhibitors of histone deacetylase in human prostate cancer cells. Cancer Prev. Res. 2009, 2, 683–693. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Selenomethionine in Treating Patients Undergoing Surgery or Internal Radiation Therapy for Stage I or Stage II Prostate Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT00736164 (accessed on 7 January 2021).
- ClinicalTrials.gov. Carboplatin, Paclitaxel, Selenomethionine, and Radiation Therapy in Treating Patients With Stage III Non-Small Cell Lung Cancer That Cannot Be Removed by Surgery. Available online: https://www.clinicaltrials.gov/ct2/show/NCT00526890 (accessed on 7 January 2021).
- ClinicalTrials.gov. Selenomethionine and Finasteride before Surgery or Radiation Therapy in Treating Patients with Stage I or Stage II Prostate Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT00736645 (accessed on 7 January 2021).
- ClinicalTrials.gov. S9917, Selenium in Preventing Cancer in Patients with Neoplasia of the Prostate. Available online: https://clinicaltrials.gov/ct2/show/NCT00030901 (accessed on 7 January 2021).
- ClinicalTrials.gov. Capecitabine, Oxaliplatin, Selenomethionine, and Radiation Therapy in Treating Patients Undergoing Surgery for Newly Diagnosed Stage II or III Rectal Adenocarcinoma. Available online: https://clinicaltrials.gov/ct2/show/NCT00625183 (accessed on 7 January 2021).
- ClinicalTrials.gov. Colon Cancer Prevention Using Selenium. Available online: https://clinicaltrials.gov/ct2/show/NCT01211561 (accessed on 7 January 2021).
- ClinicalTrials.gov. Selenium in Preventing Tumor Growth in Patients with Previously Resected Stage I Non-small Cell Lung Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT00008385 (accessed on 7 January 2021).
- ClinicalTrials.gov. Selenium in Treating Patients Who Are Undergoing Brachytherapy for Stage I or Stage II Prostate Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT00217516 (accessed on 7 January 2021).
- ClinicalTrials.gov. Irinotecan and Selenium in Treating Patients with Advanced Solid Tumors. Available online: https://clinicaltrials.gov/ct2/show/NCT00112892 (accessed on 7 January 2021).
- ClinicalTrials.gov. Se-Methyl-Seleno-L-Cysteine or Selenomethionine in Preventing Prostate Cancer in Healthy Participants. Available online: https://clinicaltrials.gov/ct2/show/NCT01497431 (accessed on 7 January 2021).
- ClinicalTrials.gov. Selenomethionine in Reducing Mucositis in Patients With Locally Advanced Head and Neck Cancer Who Are Receiving Cisplatin and Radiation Therapy. Available online: https://clinicaltrials.gov/ct2/show/NCT01682031 (accessed on 7 January 2021).
- ClinicalTrials.gov. S0000 Selenium and Vitamin E in Preventing Prostate Cancer (SELECT). Available online: https://www.clinicaltrials.gov/ct2/show/NCT00006392 (accessed on 7 January 2021).
- ClinicalTrials.gov. S0000D: Effect of Vitamin E and/or Selenium on Colorectal Polyps in Men Enrolled on SELECT Trial SWOG-S0000 (ACP). Available online: https://clinicaltrials.gov/ct2/show/NCT00706121 (accessed on 7 January 2021).
- ClinicalTrials.gov. SLM + Axitinib for Clear Cell RCC. Available online: https://clinicaltrials.gov/ct2/show/NCT02535533 (accessed on 7 January 2021).
- ClinicalTrials.gov. Clinical Study on the Effect of Selenium Yeast Capsule on Prognosis of Differentiated Thyroid Carcinoma. Available online: https://clinicaltrials.gov/ct2/show/NCT04683575 (accessed on 7 January 2021).
- Li, Z.; Carrier, L.; Belame, A.; Thiyagarajah, A.; Salvo, V.A.; Burow, M.E.; Rowan, B.G. Combination of methylselenocysteine with tamoxifen inhibits MCF-7 breast cancer xenografts in nude mice through elevated apoptosis and reduced angiogenesis. Breast Cancer Res. Treat. 2009, 118, 33–43. [Google Scholar] [CrossRef]
- Sinha, R.; Kiley, S.C.; Lu, J.X.; Thompson, H.J.; Moraes, R.; Jaken, S.; Medina, D. Effects of methylselenocysteine on PKC activity, cdk2 phosphorylation and gadd gene expression in synchronized mouse mammary epithelial tumor cells. Cancer Lett. 1999, 146, 135–145. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Chemoprevention of Breast and Prostate Cancers in Shift Workers by Dietary Methylselenocysteine: Effects on Circadian Rhythm and Estrogen Receptor-B Cycling. Available online: https://clinicaltrials.gov/ct2/show/NCT01611038 (accessed on 7 January 2021).
- ClinicalTrials.gov. Se-Methyl-Seleno-L-Cysteine, Rituximab, Ifosfamide, Carboplatin, and Etoposide in Treating Patients With Diffuse Large B-Cell Lymphoma That Has Relapsed or Not Responded to Treatment. Available online: https://clinicaltrials.gov/ct2/show/NCT00829205 (accessed on 7 January 2021).
- Labunskyy, V.M.; Hatfield, D.L.; Gladyshev, V.N. Selenoproteins: Molecular pathways and physiological roles. Physiol. Rev. 2014, 94, 739–777. [Google Scholar] [CrossRef]
- Zhang, Y.; Roh, Y.J.; Han, S.-J.; Park, I.; Lee, H.M.; Ok, Y.S.; Lee, B.C.; Lee, S.-R. Role of selenoproteins in redox regulation of signaling and the antioxidant system: A review. Antioxidants 2020, 9, 383. [Google Scholar] [CrossRef]
- Yang, R.; Liu, Y.; Zhou, Z. Selenium and selenoproteins, from structure, function to food resource and nutrition. Food Sci. Technol. Res. 2017, 23, 363–373. [Google Scholar] [CrossRef]
- Cao, W.; Li, X.; Zheng, S.; Zheng, W.; Wong, Y.-S.; Chen, T. Selenocysteine derivative overcomes TRAIL resistance in melanoma cells: Evidence for ROS-dependent synergism and signaling crosstalk. Oncotarget 2014, 5, 7431–7445. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-C.; Wang, F.-Z.; Tsai, M.-L.; Lo, C.-Y.; Badmaev, V.; Ho, C.-T.; Wang, Y.-J.; Pan, M.-H. Se-Allylselenocysteine induces autophagy by modulating the AMPK/mTOR signaling pathway and epigenetic regulation of PCDH17 in human colorectal adenocarcinoma cells. Mol. Nutr. Food Res. 2015, 59, 2511–2522. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Wong, Y.-S. Selenocystine induces reactive oxygen species–mediated apoptosis in human cancer cells. Biomed. Pharmacother. 2009, 63, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Wong, Y.-S. Selenocystine induces caspase-independent apoptosis in MCF-7 human breast carcinoma cells with involvement of p53 phosphorylation and reactive oxygen species generation. Int. J. Biochem. Cell Biol. 2009, 41, 666–676. [Google Scholar] [CrossRef] [PubMed]
- Weisberger, A.S.; Suhrland, L.G. Studies on analogues of L-Cysteine and L-Cystine: III. The effect of selenium cystine on leukemia. Blood 1956, 11, 19–30. [Google Scholar] [CrossRef] [PubMed]


| NCT Number | Study Title | Clinical Trial Status | Study Design | References |
|---|---|---|---|---|
| NCT04296578 | Study evaluating sodium selenite in combination with abiraterone in castration-resistant prostate cancer progressing on abiraterone | Phase 1 not yet recruiting | Non-randomized, open-label, single-group assignment | [40] |
| NCT01155791 | Phase I sodium selenite in combination with docetaxel in castration-resistant prostate cancer | Phase 1 terminated | Open-label, single-group assignment | [41] |
| NCT02184533 | Sodium selenite and radiation therapy in treating patients with metastatic cancer | Phase 1 completed | Open-label, single-group assignment | [42] |
| NCT00188604 | The use of selenium to treat secondary lymphedema breast cancer | Phase 2 completed | Randomized, double-blind, placebo-controlled, crossover assignment | [43] |
| NCT01959438 | Sodium selenite as a cytotoxic agent in advanced carcinoma (SECAR) | Unknown | Open-label, single-group assignment | [44] |
| NCT04201561 | High dose inorganic selenium for preventing chemotherapy induced peripheral neuropathy (SELENIUM) | Phase 3 recruiting | Randomized, triple-blind (participant, care provider, investigator), placebo-controlled, parallel assignment | [45] |
| NCT Number | Study Title | Clinical Trial Status | Study Design | References |
|---|---|---|---|---|
| NCT00736164 | Selenomethionine in treating patients undergoing surgery or internal radiation therapy for stage I or stage II prostate cancer | Phase 2 withdrawn | Randomized, double-blind, placebo-controlled | [106] |
| NCT00526890 | Carboplatin, paclitaxel, selenomethionine, and radiation therapy in treating patients with stage III non-small cell lung cancer that cannot be removed by surgery | Phase 2 terminated | Open-label, single-group assignment | [107] |
| NCT00736645 | Selenomethionine and finasteride before surgery or radiation therapy in treating patients with stage I or stage II prostate cancer | Phase 2 completed | Randomized, double-blind (participant, investigator), placebo-controlled, parallel assignment | [108] |
| NCT00030901 | S9917, Selenium in preventing cancer in patients with neoplasia of the prostate | Phase 3 completed | Randomized, triple-blind (participant, care provider, investigator), placebo-controlled, parallel assignment | [109] |
| NCT00625183 | Capecitabine, oxaliplatin, selenomethionine, and radiation therapy in treating patients undergoing surgery for newly diagnosed stage II or III rectal adenocarcinoma | Phase 2 terminated | Open-label, single-group assignment | [110] |
| NCT01211561 | Colon cancer prevention using selenium | Unknown | Randomized, double-blind (participant, investigator), placebo-controlled, single group assignment | [111] |
| NCT00008385 | Selenium in preventing tumor growth in patients with previously resected stage I non-small cell lung cancer | Phase 3 completed | Randomized, triple-blind (participant, care provider, investigator), placebo-controlled, parallel assignment | [112] |
| NCT00217516 | Selenium in treating patients who are undergoing brachytherapy for stage I or stage II prostate cancer | Phase 1 completed | Non-randomized, open-label, single-group assignment | [113] |
| NCT00112892 | Irinotecan and selenium in treating patients with advanced solid tumors | Phase 1 completed | Dose-escalation | [114] |
| NCT01497431 | Se-methyl-seleno-l-cysteine or selenomethionine in preventing prostate cancer in healthy participants | Phase 1 completed | Randomized, double-blind (participant, investigator), placebo-controlled, parallel assignment | [115] |
| NCT01682031 | Selenomethionine in reducing mucositis in patients with locally advanced head and neck cancer who are receiving cisplatin and radiation therapy | Phase 2 terminated | Randomized, double-blind, placebo-controlled, parallel assignment | [116] |
| NCT00006392 | S0000 Selenium and vitamin E in preventing prostate cancer (SELECT) | Phase 3 completed | Randomized, quadruple -blind (participant, care provider, investigator, outcomes assessor), placebo-controlled, parallel assignment | [117] |
| NCT00706121 | S0000D: Effect of vitamin E and/or selenium on colorectal polyps in men enrolled on SELECT trial SWOG-S0000 (ACP) | Phase 3 completed | Randomized, quadruple -blind (participant, care provider, investigator, outcomes assessor), placebo-controlled, parallel assignment | [118] |
| NCT02535533 | SLM + axitinib for clear cell RCC | Phase 1/2 recruiting | Open-label, single-group assignment | [119] |
| NCT04683575 | Clinical study on the effect of selenium yeast capsule on prognosis of differentiated thyroid carcinoma | Phase 4 not yet recruiting (new) | Randomized, double-blind (participant, investigator), placebo-controlled, parallel assignment | [120] |
| NCT Number | Study Title | Clinical Trial Status | Study Design | References |
|---|---|---|---|---|
| NCT01611038 | Chemoprevention of breast and prostate cancers in shift workers by dietary methylselenocysteine: effects on circadian rhythm and estrogen receptor-B cycling | Not applicable | Randomized, triple-blind (participant, investigator, outcomes assessor), placebo-controlled, parallel assignment | [123] |
| NCT01497431 | Se-methyl-seleno-l-cysteine or selenomethionine in preventing prostate cancer in healthy participants | Phase 1 completed | Randomized, double-blind (participant, investigator), placebo-controlled, parallel assignment | [115] |
| NCT00829205 | Se-methyl-seleno-l-cysteine, rituximab, ifosfamide, carboplatin, and etoposide in treating patients with diffuse large B-cell lymphoma that has relapsed or not responded to treatment | Phase 1/2 withdrawn | Non-randomized, open-label | [124] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radomska, D.; Czarnomysy, R.; Radomski, D.; Bielawski, K. Selenium Compounds as Novel Potential Anticancer Agents. Int. J. Mol. Sci. 2021, 22, 1009. https://doi.org/10.3390/ijms22031009
Radomska D, Czarnomysy R, Radomski D, Bielawski K. Selenium Compounds as Novel Potential Anticancer Agents. International Journal of Molecular Sciences. 2021; 22(3):1009. https://doi.org/10.3390/ijms22031009
Chicago/Turabian StyleRadomska, Dominika, Robert Czarnomysy, Dominik Radomski, and Krzysztof Bielawski. 2021. "Selenium Compounds as Novel Potential Anticancer Agents" International Journal of Molecular Sciences 22, no. 3: 1009. https://doi.org/10.3390/ijms22031009
APA StyleRadomska, D., Czarnomysy, R., Radomski, D., & Bielawski, K. (2021). Selenium Compounds as Novel Potential Anticancer Agents. International Journal of Molecular Sciences, 22(3), 1009. https://doi.org/10.3390/ijms22031009






