Integrated Genomics Identifies miR-181/TFAM Pathway as a Critical Driver of Drug Resistance in Melanoma
Abstract
1. Introduction
2. Results
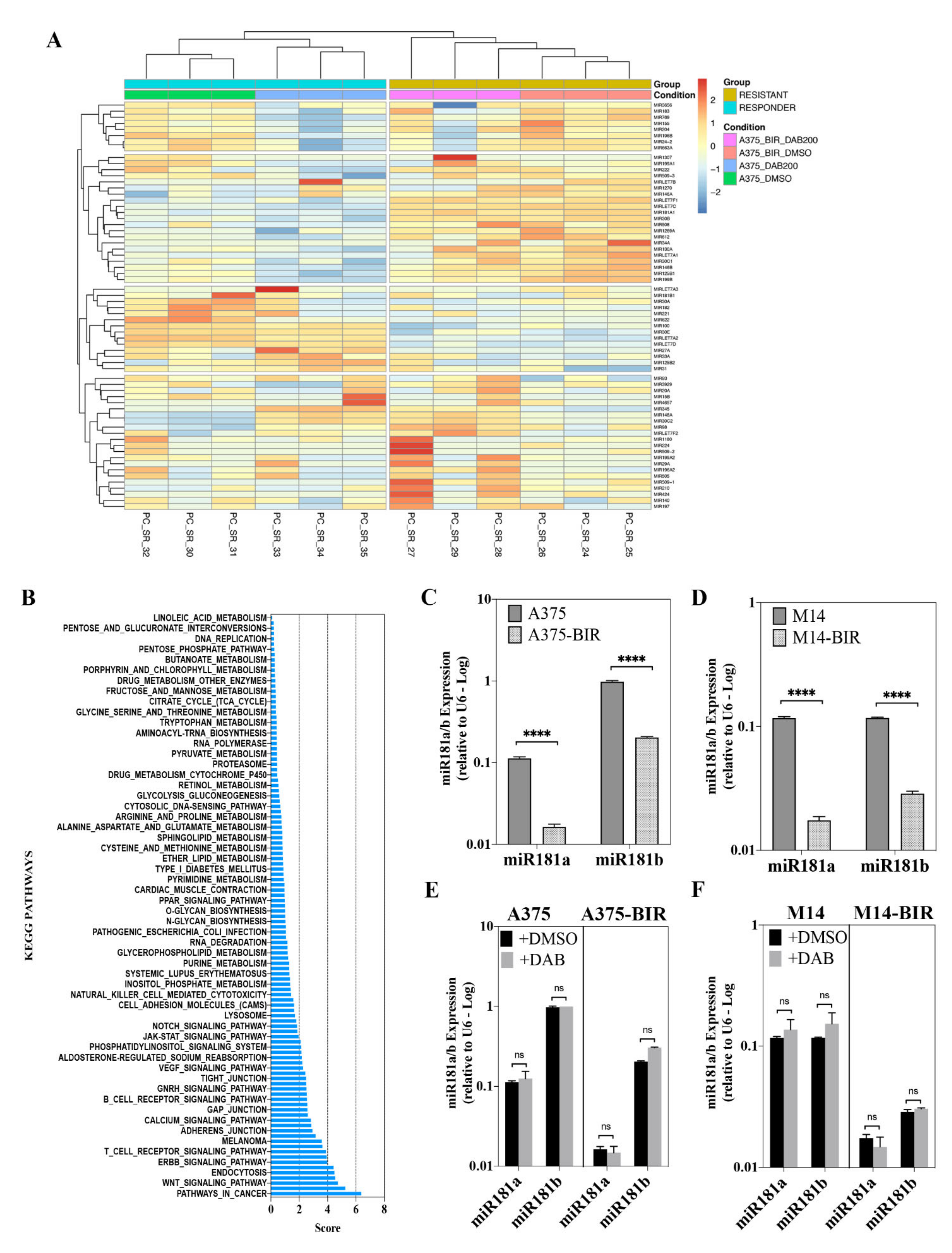
2.1. Melanoma Cells with Acquired Resistance to Dabrafenib Display Changes in miRNA Expression Pattern
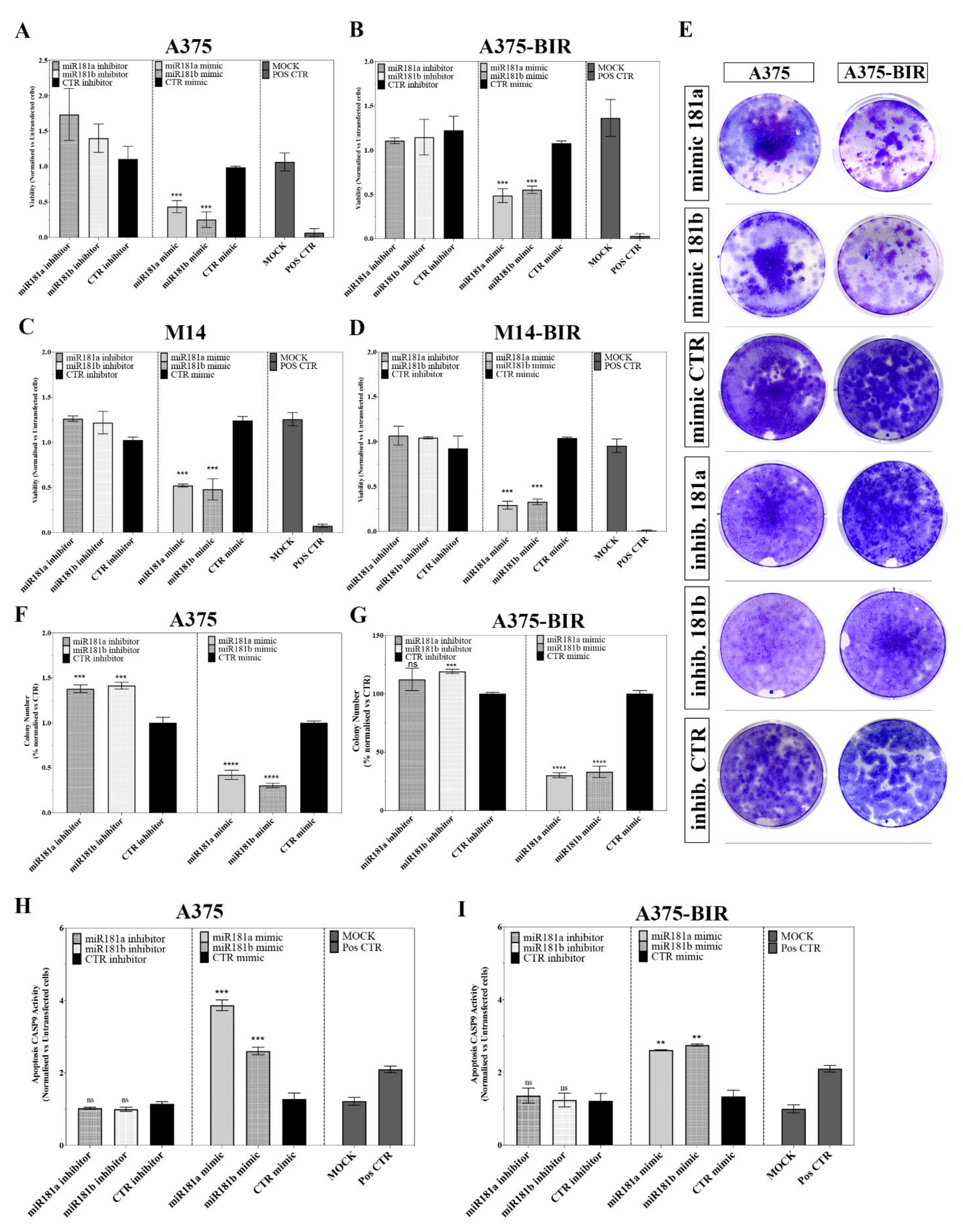
2.2. miR-181a/b Replacement Affects the Growth of Melanoma Cells Sensitive and Resistant Cells to Dabrafenib
2.3. miR-181a/b Replacement Sensitizes Resistant Cells to Dabrafenib
2.4. Increased Expression of miR-181a/b in Melanoma and Its Relationship with Patient Survival
2.5. miR-181a/b Modulate Sensitivity and Resistance to BRAF-Inhibitors by Targeting Key Signalling Networks in Melanoma
2.6. MiR-181a/b Regulate Melanoma Resistance by Targeting TFAM
3. Discussion
4. Materials and Methods
4.1. Human Samples
4.2. Cell Culture and Transfections
4.3. RNA Extraction and Quantitative Reverse Transcription PCR
4.4. Proliferation Assay
4.5. Colony Formation Assay
4.6. Caspase Activity Assay
4.7. RNAseq and Small-RNAseq Library Preparation and Deep Sequencing
4.8. Computational Analysis of Deep Sequencing Data
4.9. Identification of Differentially Expressed miRNAs and Specific miRNAs
4.10. Integrated Analysis of miRNA and mRNA Based on Correlation between mir181a/b and Related Target Gene in Melanoma Patients
4.11. Reporter Assay
4.12. Statistical Analysis
4.13. Survival Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fischer, G.M.; Gopal, Y.N.V.; McQuade, J.L.; Peng, W.; DeBerardinis, R.J.; Davies, M.A. Metabolic strategies of melanoma cells: Mechanisms, interactions with the tumor microenvironment, and therapeutic implications. Pigment. Cell Melanoma Res. 2017, 31, 11–30. [Google Scholar] [CrossRef]
- Rajkumar, S.; Watson, I.R. Molecular characterisation of cutaneous melanoma: Creating a framework for targeted and immune therapies. Br. J. Cancer 2016, 115, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Paluncic, J.; Kovacevic, Z.; Jansson, P.J.; Kalinowski, D.; Merlot, A.M.; Huang, M.L.-H.; Lok, H.C.; Sahni, S.; Lane, D.J.; Richardson, D.R. Roads to melanoma: Key pathways and emerging players in melanoma progression and oncogenic signaling. Biochim. et Biophys. Acta BBA Bioenerg. 2016, 1863, 770–784. [Google Scholar] [CrossRef] [PubMed]
- Luke, J.J.; Flaherty, K.T.; Ribas, A.; Long, G.V. Targeted agents and immunotherapies: Optimizing outcomes in melanoma. Nat. Rev. Clin. Oncol. 2017, 14, 463–482. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, R.J.; Flaherty, K.T. Resistance to BRAF-targeted therapy in melanoma. Eur. J. Cancer 2013, 49, 1297–1304. [Google Scholar] [CrossRef] [PubMed]
- Kozar, I.; Margue, C.; Rothengatter, S.; Haan, C.; Kreis, S. Many ways to resistance: How melanoma cells evade targeted therapies. Biochim. et Biophys. Acta (BBA) Bioenerg. 2019, 1871, 313–322. [Google Scholar] [CrossRef]
- Gide, T.N.; Wilmott, J.S.; Scolyer, R.A.; Long, G.V. Primary and Acquired Resistance to Immune Checkpoint Inhibitors in Metastatic Melanoma. Clin. Cancer Res. 2018, 24, 1260–1270. [Google Scholar] [CrossRef]
- Fattore, L.; Costantini, S.; Malpicci, D.; Ruggiero, C.F.; Ascierto, P.A.; Croce, C.M.; Mancini, R.; Ciliberto, G. MicroRNAs in melanoma development and resistance to target therapy. Oncotarget 2017, 8, 22262–22278. [Google Scholar] [CrossRef]
- Stark, M.S.; Tyagi, S.; Nancarrow, D.J.; Boyle, G.M.; Cook, A.L.; Whiteman, D.C.; Parsons, P.G.; Schmidt, C.; Sturm, R.A.; Hayward, N.K. Characterization of the Melanoma miRNAome by Deep Sequencing. PLoS ONE 2010, 5, e9685. [Google Scholar] [CrossRef]
- Voortman, J.; Goto, A.; Mendiboure, J.; Sohn, J.J.; Schetter, A.J.; Saito, M.; Dunant, A.; Pham, T.C.; Petrini, I.; Lee, A.; et al. MicroRNA Expression and Clinical Outcomes in Patients Treated with Adjuvant Chemotherapy after Complete Resection of Non–Small Cell Lung Carcinoma. Cancer Res. 2010, 70, 8288–8298. [Google Scholar] [CrossRef]
- Previdi, M.C.; Carotenuto, P.; Zito, D.; Pandolfo, R.; Braconi, C. Noncoding RNAs as novel biomarkers in pancreatic cancer: What do we know? Futur. Oncol. 2017, 13, 443–453. [Google Scholar] [CrossRef]
- Carotenuto, P.; Hedayat, S.; Fassan, M.; Cardinale, V.; Lampis, A.; Guzzardo, V.; Vicentini, C.; Scarpa, A.; Cascione, L.; Costantini, D.; et al. Modulation of Biliary Cancer Chemo-Resistance through MicroRNA-Mediated Rewiring of the Expansion of CD133+ Cells. Hepatology 2020, 72, 982–996. [Google Scholar] [CrossRef]
- Indrieri, A.; Carrella, S.; Carotenuto, P.; Banfi, S.; Franco, B. The Pervasive Role of the miR-181 Family in Development, Neurodegeneration, and Cancer. Int. J. Mol. Sci. 2020, 21, 2092. [Google Scholar] [CrossRef]
- Miller, T.E.; Ghoshal, K.; Ramaswamy, B.; Roy, S.; Datta, J.; Shapiro, C.L.; Jacob, S.; Majumder, S. MicroRNA-221/222 confers tamoxifen resistance in breast cancer by targeting p27Kip1. J. Biol. Chem. 2008, 283, 29897–29903. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Xing, Y.; Rong, L. miR-181 regulates cisplatin-resistant non-small cell lung cancer via downregulation of autophagy through the PTEN/PI3K/AKT pathway. Oncol. Rep. 2018, 39, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, G.; Hayashi, K.; Xi, Y.; Kudo, K.; Uchida, K.; Takasaki, K.; Yamamoto, M.; Ju, J. Non-coding microRNAs hsa-let-7g and hsa-miR-181b are associated with chemoresponse to S-1 in colon cancer. Cancer Genom. Proteom. 2006, 3, 317–324. [Google Scholar]
- Hasegawa, S.; Eguchi, H.; Nagano, H.; Konno, M.; Tomimaru, Y.; Wada, H.; Hama, N.; Kawamoto, K.; Kobayashi, S.; Nishida, N.; et al. MicroRNA-1246 expression associated with CCNG2-mediated chemoresistance and stemness in pancreatic cancer. Br. J. Cancer 2014, 111, 1572–1580. [Google Scholar] [CrossRef] [PubMed]
- Caporali, S.; Amaro, A.; Levati, L.; Alvino, E.; Lacal, P.M.; Mastroeni, S.; Ruffini, F.; Bonmassar, L.; Cappellini, G.C.A.; Felli, N.; et al. miR-126-3p down-regulation contributes to dabrafenib acquired resistance in melanoma by up-regulating ADAM9 and VEGF-A. J. Exp. Clin. Cancer Res. 2019, 38, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Fattore, L.; Mancini, R.; Acunzo, M.; Romano, G.; Laganà, A.; Pisanu, M.E.; Malpicci, D.; Madonna, G.; Mallardo, D.; Caponea, M.; et al. miR-579-3p controls melanoma progression and resistance to target therapy. Proc. Natl. Acad. Sci. USA 2016, 113, E5005–E5013. [Google Scholar] [CrossRef]
- Lunavat, T.R.; Cheng, L.; Einarsdottir, B.O.; Bagge, R.O.; Muralidharan, S.V.; Sharples, R.A.; Lässer, C.; Gho, Y.S.; Hill, A.F.; Nilsson, J.A.; et al. BRAFV600 inhibition alters the microRNA cargo in the vesicular secretome of malignant melanoma cells. Proc. Natl. Acad. Sci. USA 2017, 114, E5930–E5939. [Google Scholar] [CrossRef]
- Patil, S.L.; Palat, A.; Pan, Y.; Rajapakshe, K.; Mirchandani, R.; Bondesson, M.; Yustein, J.T.; Coarfa, C.; Gunaratne, P.H. MicroRNA-509-3p inhibits cellular migration, invasion, and proliferation, and sensitizes osteosarcoma to cisplatin. Sci. Rep. 2019, 9, 1–11. [Google Scholar] [CrossRef]
- Zhou, B.; Li, C.; Jing, Q.; Liu, M.F.; Zhai, Q.; Qi, W.; Zhang, Y.; Zhang, F.; Wu, J.X.; Hu, Y.N.; et al. Downregulation of miR-181a upregulates sirtuin-1 (SIRT1) and improves hepatic insulin sensitivity. Diabetologia 2012, 55, 2032–2043. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Z.; Dong, X.; Sun, Q.; Li, X.; Yan, B. Clinical significance of up-regulated miR-181a in prognosis and progression of esophageal cancer. Acta Biochim. et Biophys. Sin. 2014, 46, 1007–1010. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Zeng, S.; Zhou, Z.W.; He, Z.X.; Zhou, S.F. Hsa-microRNA-181a is a regulator of a number of cancer genes and a biomarker for endometrial carcinoma in patients: A bioinformatic and clinical study and the therapeutic implication. Drug Des. Devel. Ther. 2015, 9, 1103–1175. [Google Scholar] [PubMed]
- Ebert, M.S.; Sharp, P.A. MicroRNA sponges: Progress and possibilities. RNA 2010, 16, 2043–2050. [Google Scholar] [CrossRef] [PubMed]
- Tay, F.C.; Lim, J.K.; Zhu, H.; Hin, L.C.; Wang, S. Using artificial microRNA sponges to achieve microRNA loss-of-function in cancer cells. Adv. Drug Deliv. Rev. 2015, 81, 117–127. [Google Scholar] [CrossRef]
- Indrieri, A.; Grimaldi, C.; Zucchelli, S.; Tammaro, R.; Gustincich, S.; Franco, B. Synthetic long non-coding RNAs [SINEUPs] rescue defective gene expression in vivo. Sci. Rep. 2016, 6, 27315. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.Y.L.; Habib, N.A.; Chuah, Y.W.; Yau, Y.H.; Geifman-Shochat, S.; Chen, W.N. Identification of Cellular Targets of MicroRNA-181a in HepG2 Cells: A New Approach for Functional Analysis of MicroRNAs. PLoS ONE 2015, 10, e0123167. [Google Scholar] [CrossRef][Green Version]
- Song, J.; Yang, S.; Yin, R.; Xiao, Q.; Ma, A.; Pan, X. MicroRNA-181a regulates the activation of the NLRP3 inflammatory pathway by targeting MEK1 in THP-1 macrophages stimulated by ox-LDL. J. Cell. Biochem. 2019, 120, 13640–13650. [Google Scholar] [CrossRef]
- Li, S.; Yang, J.; Xia, Y.; Fan, Q.; Yang, K.-P. Long Noncoding RNA NEAT1 Promotes Proliferation and Invasion via Targeting miR-181a-5p in Non-Small Cell Lung Cancer. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2018, 26, 289–296. [Google Scholar] [CrossRef]
- Araujo, L.F.; Siena, A.D.D.; Plaça, J.R.; Brotto, D.B.; Barros, I.I.; Muys, B.R.; Biagi, C.A.O.; Peronni, K.C.; Sousa, J.F.; Molfetta, G.A.; et al. Mitochondrial transcription factor A (TFAM) shapes metabolic and invasion gene signatures in melanoma. Sci. Rep. 2018, 8, 14190. [Google Scholar] [CrossRef] [PubMed]
- Moriceau, G.; Hugo, W.; Hong, A.; Shi, H.; Kong, X.; Yu, C.C.; Koya, R.C.; Samatar, A.A.; Khanlou, N.; Braun, J.; et al. Tunable-Combinatorial Mechanisms of Acquired Resistance Limit the Efficacy of BRAF/MEK Cotargeting but Result in Melanoma Drug Addiction. Cancer Cell 2015, 27, 240–256. [Google Scholar] [CrossRef] [PubMed]
- Roesch, A.; Paschen, A.; Landsberg, J.; Helfrich, I.; Becker, J.C.; Schadendorf, D. Phenotypic tumour cell plasticity as a resistance mechanism and therapeutic target in melanoma. Eur. J. Cancer 2016, 59, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Mueller, D.W.; Rehli, M.; Bosserhoff, A.K. miRNA Expression Profiling in Melanocytes and Melanoma Cell Lines Reveals miRNAs Associated with Formation and Progression of Malignant Melanoma. J. Investig. Dermatol. 2009, 129, 1740–1751. [Google Scholar] [CrossRef]
- Chakraborty, C.; Sharma, A.R.; Sharma, G.; Doss, C.G.P.; Lee, S.-S. Therapeutic miRNA and siRNA: Moving from Bench to Clinic as Next Generation Medicine. Mol. Ther. Nucleic Acids 2017, 8, 132–143. [Google Scholar] [CrossRef]
- Rupaimoole, R.; Slack, F.J. MicroRNA therapeutics: Towards a new era for the management of cancer and other diseases. Nat. Rev. Drug Discov. 2017, 16, 203–222. [Google Scholar] [CrossRef]
- Li, X.J.; Ren, Z.J.; Tang, J.H. MicroRNA-34a: A potential therapeutic target in human cancer. Cell Death Dis. 2014, 5, e1327. [Google Scholar] [CrossRef]
- Ouyang, M.; Li, Y.; Ye, S.; Ma, J.; Lu, L.; Lv, W.; Chang, G.; Li, X.; Li, Q.; Wang, S.; et al. MicroRNA Profiling Implies New Markers of Chemoresistance of Triple-Negative Breast Cancer. PLoS ONE 2014, 9, e96228. [Google Scholar] [CrossRef]
- Chen, Y.; Ke, G.; Han, D.; Liang, S.; Yang, G.; Wu, X. MicroRNA-181a enhances the chemoresistance of human cervical squamous cell carcinoma to cisplatin by targeting PRKCD. Exp. Cell Res. 2014, 320, 12–20. [Google Scholar] [CrossRef]
- Jornayvaz, F.R.; Shulman, G.I. Regulation of mitochondrial biogenesis. Essays Biochem. 2010, 47, 69–84. [Google Scholar] [CrossRef]
- Zhang, G.; Frederick, D.T.; Wu, L.; Wei, Z.; Krepler, C.; Srinivasan, S.; Chae, Y.C.; Xu, X.; Choi, H.; Dimwamwa, E.; et al. Targeting mitochondrial biogenesis to overcome drug resistance to MAPK inhibitors. J. Clin. Investig. 2016, 126, 1834–1856. [Google Scholar] [CrossRef]
- Indrieri, A.; Carrella, S.; Romano, A.; Spaziano, A.; Marrocco, E.; Fernandez-Vizarra, E.; Barbato, S.; Pizzo, M.; Ezhova, Y.; Golia, F.M.; et al. miR-181a/b downregulation exerts a protective action on mitochondrial disease models. EMBO Mol. Med. 2019, 11, e8734. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Li, J.; Sun, Y.; Zhang, Y.; Dong, L.; Shen, C.; Yang, L.; Yang, M.; Li, Y.; Shen, G.; et al. miR-7 reverses the resistance to BRAFi in melanoma by targeting EGFR/IGF-1R/CRAF and inhibiting the MAPK and PI3K/AKT signaling pathways. Oncotarget 2016, 7, 53558–53570. [Google Scholar] [CrossRef] [PubMed]
- Koetz-Ploch, L.; Hanniford, U.; Dolgalev, I.; Sokolova, E.; Zhong, J.; Díaz-Martínez, M.; Bernstein, E.; Darvishian, F.; Flaherty, K.T.; Chapman, P.B.; et al. MicroRNA-125a promotes resistance to BRAF inhibitors through suppression of the intrinsic apoptotic pathway. Pigment. Cell Melanoma Res. 2017, 30, 328–338. [Google Scholar] [CrossRef]
- de Filippis, D.; Russo, A.; de Stefano, D.; Cipriano, M.; Esposito, D.; Grassia, G.; Carnuccio, R.; Russo, G.; Iuvone, T. Palmitoylethanolamide inhibits rMCP-5 expression by regulating MITF activation in rat chronic granulomatous inflammation. Eur. J. Pharmacol. 2014, 725, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Lampis, A.; Carotenuto, P.; Vlachogiannis, G.; Cascione, L.; Hedayat, S.; Burke, R.; Clarke, P.A.; Bosma, E.; Simbolo, M.; Scarpa, A.; et al. MIR21 Drives Resistance to Heat Shock Protein 90 Inhibition in Cholangiocarcinoma. Gastroenterology 2018, 154, 1066–1079.e5. [Google Scholar] [CrossRef]
- Pecoraro, A.; Carotenuto, P.; Franco, B.; De Cegli, R.; Russo, G.; Russo, A. Role of uL3 in the Crosstalk between Nucleolar Stress and Autophagy in Colon Cancer Cells. Int. J. Mol. Sci. 2020, 21, 2143. [Google Scholar] [CrossRef]
- Robinson, M.D.; Oshlack, A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 2010, 11, R25. [Google Scholar] [CrossRef]




| MicroRNA ID | logFC | FDR | Regulation |
|---|---|---|---|
| microRNA 224 | −5.863656346 | 2.89 × 10−5 | DOWN |
| microRNA 1270 | −5.796946495 | 5.23 × 10−5 | DOWN |
| microRNA 31 | −4.893572244 | 1.68 × 10−86 | DOWN |
| microRNA 130a | −4.666019353 | 6.41 × 10−7 | DOWN |
| microRNA 1269a | −4.482898282 | 1.25 × 10−21 | DOWN |
| microRNA 3929 | −3.74725201 | 4.40 × 10−5 | DOWN |
| microRNA 33a | −3.475625978 | 2.69 × 10−2 | DOWN |
| microRNA 622 | −2.886943306 | 5.68 × 10−4 | DOWN |
| microRNA 30a | −2.703339809 | 2.05 × 10−24 | DOWN |
| microRNA 505 | −2.627997044 | 1.89 × 10−3 | DOWN |
| microRNA 196b | −2.528703752 | 3.84 × 10−11 | DOWN |
| microRNA 210 | −2.469223892 | 8.77 × 10−8 | DOWN |
| microRNA 182 | −2.461507371 | 2.54 × 10−38 | DOWN |
| microRNA let-7c | −2.393014183 | 1.88 × 10−31 | DOWN |
| microRNA 146b | −2.268652948 | 2.10 × 10−18 | DOWN |
| microRNA 15b | −1.995340697 | 3.87 × 10−10 | DOWN |
| microRNA 183 | −1.969984406 | 1.46 × 10−3 | DOWN |
| microRNA 222 | −1.886429667 | 3.50 × 10−28 | DOWN |
| microRNA 424 | −1.683371 | 4.29 × 10−5 | DOWN |
| microRNA 30c-2 | −1.67640615 | 3.28 × 10−11 | DOWN |
| microRNA 34a | −1.668911618 | 4.39 × 10−6 | DOWN |
| microRNA 29a | −1.631521943 | 4.39 × 10−6 | DOWN |
| microRNA 30c-1 | −1.616623692 | 6.56 × 10−9 | DOWN |
| microRNA 125b-2 | −1.434360093 | 1.65 × 10−7 | DOWN |
| microRNA 20a | −1.264913487 | 2.95 × 10−2 | DOWN |
| microRNA 100 | −1.24322378 | 9.16 × 10−6 | DOWN |
| microRNA 221 | −1.185152679 | 2.29 × 10−5 | DOWN |
| microRNA 27a | −1.177996843 | 1.30 × 10−4 | DOWN |
| microRNA 125b-1 | −1.133330102 | 5.88 × 10−8 | DOWN |
| microRNA 24-2 | −1.121098474 | 1.01 × 10−6 | DOWN |
| microRNA 769 | −1.116258565 | 3.42 × 10−4 | DOWN |
| microRNA 93 | −1.087377219 | 1.17 × 10−2 | DOWN |
| microRNA 1307 | −1.077056378 | 9.18 × 10−5 | DOWN |
| microRNA 196a-2 | −0.782047919 | 3.08 × 10−3 | DOWN |
| microRNA 30e | −0.737216081 | 1.48 × 10−2 | DOWN |
| microRNA let-7a-2 | −0.732269399 | 2.66 × 10−5 | DOWN |
| microRNA let-7a-1 | −0.729090427 | 3.26 × 10−5 | DOWN |
| microRNA let-7a-3 | −0.724904576 | 3.19 × 10−5 | DOWN |
| microRNA let-7b | 0.551945479 | 3.73 × 10−2 | UP |
| microRNA 197 | 0.655730622 | 1.36 × 10−2 | UP |
| microRNA 612 | 0.797582759 | 2.93 × 10−2 | UP |
| microRNA 663a | 0.855598474 | 3.68 × 10−4 | UP |
| microRNA let-7f-1 | 0.873310731 | 3.20 × 10−6 | UP |
| microRNA let-7d | 0.87390186 | 5.69 × 10−7 | UP |
| microRNA let-7f-2 | 0.904197222 | 1.14 × 10−6 | UP |
| microRNA 30b | 0.947032776 | 1.15 × 10−3 | UP |
| microRNA 1180 | 1.099377126 | 1.46 × 10−5 | UP |
| microRNA 140 | 1.253304012 | 5.15 × 10−5 | UP |
| microRNA 345 | 1.308512546 | 1.85 × 10−2 | UP |
| microRNA 98 | 1.44563401 | 9.26 × 10−8 | UP |
| microRNA 199b | 1.624916736 | 9.50 × 10−4 | UP |
| microRNA 199a-2 | 1.945384932 | 1.24 × 10−4 | UP |
| microRNA 199a-1 | 1.978424668 | 8.68 × 10−5 | UP |
| microRNA 3656 | 2.044965985 | 2.65 × 10−4 | UP |
| microRNA 148a | 2.072112903 | 4.99 × 10−11 | UP |
| microRNA 4657 | 2.179581553 | 2.76 × 10−2 | UP |
| microRNA 181b-1 | 2.338861601 | 1.59 × 10−3 | UP |
| microRNA 181a-1 | 2.361601036 | 1.71 × 10−3 | UP |
| microRNA 204 | 3.622749398 | 2.41 × 10−30 | UP |
| microRNA 508 | 4.093425037 | 7.10 × 10−9 | UP |
| microRNA 155 | 4.335109793 | 1.58 × 10−52 | UP |
| microRNA 146a | 4.399501991 | 4.11 × 10−76 | UP |
| microRNA 509-3 | 4.724501129 | 2.50 × 10−23 | UP |
| microRNA 509-2 | 4.959344912 | 7.21 × 10−24 | UP |
| microRNA 509-1 | 4.959393713 | 6.68 × 10−24 | UP |
| Case | Sex | Age (Years) | Stage a | BRAF STATUS | Previous Therapy | Targeted Therapy c | BR d | TTF e (Months) |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 46 | III–IV | MUT | None | ENCO+BIN | PD | 16.90 |
| 2 | M | 42 | IV | MUT | None | VEMU | PD | 20.83 |
| 3 | F | 50 | IV | MUT | None | DAB | PD | 9.60 |
| 4 | M | 59 | IV | MUT | None | VEMU | PD | 18.47 |
| 5 | M | 61 | III/IV | MUT | Dacarbazine | VEMU | PD | 18.47 |
| 6 | M | 48 | NA | MUT | Radiotherapy | VEMU | PR | 73.77 |
| 7 | F | 56 | IV | MUT | None | VEMU | PD | 7.20 |
| 8 | F | 50 | III/IV | MUT | None | DAB | PD | 15.17 |
| 9 | M | 48 | NA | MUT | Radiotherapy | VEMU | PR | 73.77 |
| 10 | M | 77 | III–IV | MUT | None | DAB + TRAM | PR | 43.53 |
| 11 | F | 86 | IV | MUT | None | DAB + TRAM | SD | 37.23 |
| 12 | F | 70 | IV | MUT | None | VEMU + COBI | PR | 20.33 |
| 13 | F | 67 | III/IV | MUT | None | VEMU + COBI | CR | 25.17 |
| 14 | F | 45 | NA | MUT | None | DAB + TRAM | PR | 21.93 |
| 15 | M | 65 | IV | MUT | None | DAB + TRAM | PR | 13.43 |
| 16 | M | 47 | III/IV | MUT | None | VEMU + COBI | PR | 11.53 |
| GENE SET | pval | padj | ES | NES |
|---|---|---|---|---|
| E2F_TARGETS | 0.025 | 0.067476383 | −0.645120028 | −2.362223392 |
| MYC_TARGETS_V1 | 0.025641026 | 0.067476383 | −0.578931346 | −2.098724203 |
| MYC_TARGETS_V2 | 0.005263158 | 0.029239766 | −0.653683002 | −2.054477496 |
| G2M_CHECKPOINT | 0.025641026 | 0.067476383 | −0.53100629 | −1.925856679 |
| UNFOLDED_PROTEIN_RESPONSE | 0.010204082 | 0.051020408 | −0.543515092 | −1.895494756 |
| MTORC1_SIGNALING | 0.025 | 0.067476383 | −0.493595313 | −1.804927713 |
| DNA_REPAIR | 0.015151515 | 0.067476383 | −0.472340422 | −1.677943319 |
| GLYCOLYSIS | 0.023255814 | 0.067476383 | −0.443156625 | −1.576560747 |
| OXIDATIVE_PHOSPHORYLATION | 0.023255814 | 0.067476383 | −0.436113647 | −1.557784166 |
| HEDGEHOG_SIGNALING | 0.03930131 | 0.098253275 | −0.545687766 | −1.479472244 |
| APOPTOSIS | 0.050437567 | 0.153125145 | 0.480331268 | 1.267604291 |
| ROS_PATHWAY | 0.084367246 | 0.162244703 | 0.559128155 | 1.311901032 |
| P53_PATHWAY | 0.003115265 | 0.019778481 | 0.529555328 | 1.416399563 |
| IL2_STAT5_SIGNALING | 0.002089864 | 0.018705574 | 0.548857874 | 1.463005267 |
| IL6_JAK_STAT3_SIGNALING | 0.001157407 | 0.014467593 | 0.649692129 | 1.607476866 |
| IFNγ_RESPONSE | 0.001042753 | 0.014467593 | 0.628035534 | 1.675781046 |
| IFNα_RESPONSE | 0.002244669 | 0.018705574 | 0.627922857 | 1.596308497 |
| GENE NAME | cor | pvals |
|---|---|---|
| ANKRD13C | −0.574 | 0.032 |
| ARID2 | −0.588 | 0.027 |
| ARL5A | −0.637 | 0.014 |
| ATG7 | −0.538 | 0.047 |
| ATL3 | −0.535 | 0.049 |
| CCNK | −0.715 | 0.004 |
| LRRC32 | −0.571 | 0.033 |
| NAA50 | −0.546 | 0.044 |
| PAWR | −0.586 | 0.028 |
| PDCD6IP | −0.538 | 0.047 |
| SLC16A7 | −0.565 | 0.035 |
| SS18L1 | −0.575 | 0.032 |
| TFAM | −0.535 | 0.049 |
| TMEM134 | −0.715 | 0.004 |
| TMF1 | −0.556 | 0.039 |
| UBP1 | −0.696 | 0.006 |
| ZFP36L1 | −0.581 | 0.029 |
| ZNF791 | −0.551 | 0.041 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbato, A.; Iuliano, A.; Volpe, M.; D’Alterio, R.; Brillante, S.; Massa, F.; De Cegli, R.; Carrella, S.; Salati, M.; Russo, A.; et al. Integrated Genomics Identifies miR-181/TFAM Pathway as a Critical Driver of Drug Resistance in Melanoma. Int. J. Mol. Sci. 2021, 22, 1801. https://doi.org/10.3390/ijms22041801
Barbato A, Iuliano A, Volpe M, D’Alterio R, Brillante S, Massa F, De Cegli R, Carrella S, Salati M, Russo A, et al. Integrated Genomics Identifies miR-181/TFAM Pathway as a Critical Driver of Drug Resistance in Melanoma. International Journal of Molecular Sciences. 2021; 22(4):1801. https://doi.org/10.3390/ijms22041801
Chicago/Turabian StyleBarbato, Anna, Antonella Iuliano, Mariagrazia Volpe, Romina D’Alterio, Simona Brillante, Filomena Massa, Rossella De Cegli, Sabrina Carrella, Massimiliano Salati, Annapina Russo, and et al. 2021. "Integrated Genomics Identifies miR-181/TFAM Pathway as a Critical Driver of Drug Resistance in Melanoma" International Journal of Molecular Sciences 22, no. 4: 1801. https://doi.org/10.3390/ijms22041801
APA StyleBarbato, A., Iuliano, A., Volpe, M., D’Alterio, R., Brillante, S., Massa, F., De Cegli, R., Carrella, S., Salati, M., Russo, A., Russo, G., Riccardo, S., Cacchiarelli, D., Capone, M., Madonna, G., Ascierto, P. A., Franco, B., Indrieri, A., & Carotenuto, P. (2021). Integrated Genomics Identifies miR-181/TFAM Pathway as a Critical Driver of Drug Resistance in Melanoma. International Journal of Molecular Sciences, 22(4), 1801. https://doi.org/10.3390/ijms22041801







