Generation of Liposomes to Study the Effect of Mycobacterium Tuberculosis Lipids on HIV-1 cis- and trans-Infections
Abstract
1. Introduction
2. Results
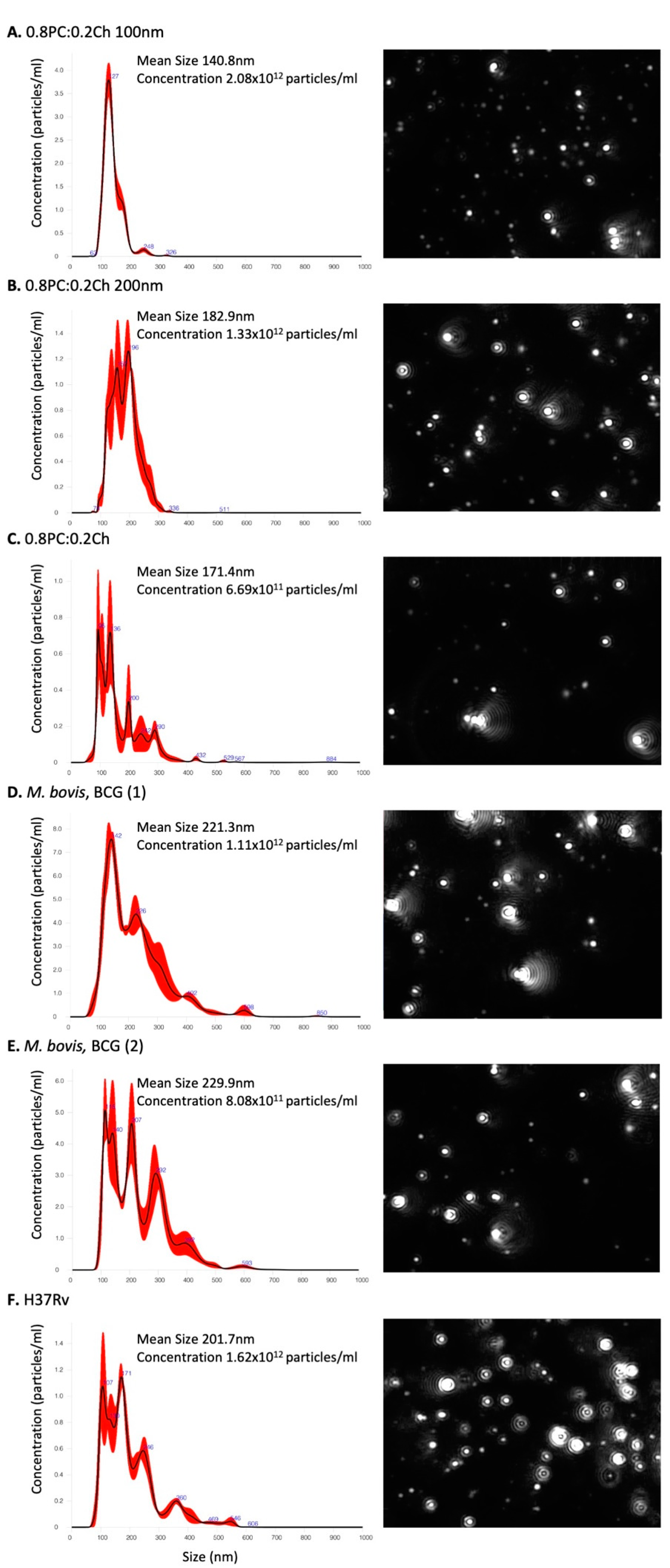
2.1. Production of Liposomes Containing Mycobacterium Total Lipids
2.2. Mycobacterium Lipids Do Not Affect HIV-1 Cis-Infection
2.3. M. bovis, Mtb H37Rv and EU127 Lipids Interfere with HIV-1 Trans-Infection Mediated by DC-SIGN
2.4. Implication of SL1, PDIM and TDM Lipids in HIV-1 Trans-Infection Mediated by DC-SIGN
2.5. Differential Effects of Mtb Glycolipids on HIV-1 Trans-Infection Mediated via iDC and mDC
3. Discussion
4. Materials and Methods
4.1. Commercial Lipids
4.2. M. Tuberculosis Strains and H37Rv Mutants
4.3. Lipids Extractions
4.4. Liposomes
4.5. Liposomes Characterisation
4.6. Cells
4.7. Cell Viability in the Presence of Liposomes
4.8. Virus Production
4.9. HIV-1 Cis-Infection
4.10. HIV-1 Trans-Infection
4.11. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AG | Arabinogalactan |
| BCG | Bacille Calmette Guerin |
| CCR5 | CC chemokine receptor 5 |
| Ch | Cholesterol |
| CXCR4 | CXC chemokine receptor 4 |
| DC | Dendritic cell |
| DC-SIGN | Dendritic cell-specific ICAM-3-grabbing non-integrin |
| HIV-1 | Human Immunodeficiency Virus type 1 |
| iDC | Immature dendritic cell |
| LAM | lipoarabinomannan |
| LM | lipomannan |
| LTR | Long Terminal Repeat |
| MA | Mycolic acids |
| Mincle | macrophage-inducible C-type lectin |
| mDC | Mature dendritic cell |
| MR | Mannose receptor |
| Mtb | Mycobacterium tuberculosis |
| PAMPs | Pathogen associated molecular patterns |
| papA1 | Polyketide associated-protein-1 |
| PC | Phosphatidylcholine |
| PDIM | Phthiocerol dimycocerosate |
| PG | Peptidoglycan |
| PGL | Phenolic glycolipids |
| PIM | Phosphatidylinositol mannoside |
| PRR | Pattern recognition receptors |
| SL | Sulfolipid |
| TB | Tuberculosis |
| TDM | Trehalose dimycolate |
| TLC | Thin-layer chromatography |
References
- World Health Organization Global Tuberculosis Report; WHO: Geneva, Switzerland, 2020.
- Sullivan, Z.A.; Wong, E.B.; Ndung’u, T.; Kasprowicz, V.O.; Bishai, W.R. Latent and Active Tuberculosis Infection Increase Immune Activation in Individuals Co-Infected with HIV. EBioMedicine 2015, 2, 334–340. [Google Scholar] [CrossRef]
- Bell, L.C.K.; Noursadeghi, M. Pathogenesis of HIV-1 and Mycobacterium tuberculosis co-infection. Nat. Rev. Microbiol. 2018, 16, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Waters, R.; Ndengane, M.; Abrahams, M.-R.; Diedrich, C.R.; Wilkinson, R.J.; Coussens, A.K. The Mtb-HIV syndemic interaction: Why treating M. tuberculosis infection may be crucial for HIV-1 eradication. Future Virol. 2020, 15, 101–125. [Google Scholar] [CrossRef]
- Naqvi, K.F.; Endsley, J.J. Myeloid C-Type Lectin Receptors in Tuberculosis and HIV Immunity: Insights Into Co-infection? Front. Cell. Infect. Microbiol. 2020, 10, 263. [Google Scholar] [CrossRef]
- Nguyen, D.G.; Hildreth, J.E.K. Involvement of macrophage mannose receptor in the binding and transmission of HIV by macrophages. Eur. J. Immunol. 2003, 33, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Cameron, P.U.; Freudenthal, P.S.; Barker, J.M.; Gezelter, S.; Inaba, K.; Steinman, R.M. Dendritic cells exposed to human immunodeficiency virus type-1 transmit a vigorous cytopathic infection to CD4+ T cells. Science 1992, 257, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Gummuluru, S.; KewalRamani, V.N.; Emerman, M. Dendritic cell-mediated viral transfer to T cells is required for human immunodeficiency virus type 1 persistence in the face of rapid cell turnover. J. Virol. 2002, 76, 10692–10701. [Google Scholar] [CrossRef]
- Garcia, E.; Pion, M.; Pelchen-Matthews, A.; Collinson, L.; Arrighi, J.F.; Blot, G.; Leuba, F.; Escola, J.M.; Demaurex, N.; Marsh, M.; et al. HIV-1 trafficking to the dendritic cell-T-cell infectious synapse uses a pathway of tetraspanin sorting to the immunological synapse. Traffic 2005, 6, 488–501. [Google Scholar] [CrossRef] [PubMed]
- Sallusto, F.; Cella, M.; Danieli, C.; Lanzavecchia, A. Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: Downregulation by cytokines and bacterial products. J. Exp. Med. 1995, 182, 389–400. [Google Scholar] [CrossRef]
- Turville, S.G.; Cameron, P.U.; Handley, A.; Lin, G.; Pöhlmann, S.; Doms, R.W.; Cunningham, A.L. Diversity of receptors binding HIV on dendritic cell subsets. Nat. Immunol. 2002, 3, 975–983. [Google Scholar] [CrossRef]
- Geijtenbeek, T.B.; Kwon, D.S.; Torensma, R.; van Vliet, S.J.; van Duijnhoven, G.C.; Middel, J.; Cornelissen, I.L.M.H.; Nottet, H.S.L.; KewalRamani, V.N.; Littman, D.R.; et al. DC-SIGN, a dendritic cell-specific HIV-1-binding protein that enhances trans-infection of T cells. Cell 2000, 100, 587–597. [Google Scholar] [CrossRef]
- Turville, S.; Wilkinson, J.; Cameron, P.; Dable, J.; Cunningham, A.L. The role of dendritic cell C-type lectin receptors in HIV pathogenesis. J. Leukoc. Biol. 2003, 74, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Moris, A.; Pajot, A.; Blanchet, F.; Guivel-Benhassine, F.; Salcedo, M.; Schwartz, O. Dendritic cells and HIV-specific CD4+ T cells: HIV antigen presentation, T-cell activation, and viral transfer. Blood 2006, 108, 1643–1651. [Google Scholar] [CrossRef]
- Van Montfort, T.; Nabatov, A.A.; Geijtenbeek, T.B.H.; Pollakis, G.; Paxton, W.A. Efficient capture of antibody neutralized HIV-1 by cells expressing DC-SIGN and transfer to CD4+ T lymphocytes. J. Immunol. 2007, 178, 3177–3185. [Google Scholar] [CrossRef] [PubMed]
- Bobardt, M.D.; Saphire, A.C.S.; Hung, H.-C.; Yu, X.; Van der Schueren, B.; Zhang, Z.; David, G.; Gallay, P.A. Syndecan captures, protects, and transmits HIV to T lymphocytes. Immunity 2003, 18, 27–39. [Google Scholar] [CrossRef]
- De Witte, L.; Bobardt, M.; Chatterji, U.; Degeest, G.; David, G.; Geijtenbeek, T.B.H.; Gallay, P. Syndecan-3 is a dendritic cell-specific attachment receptor for HIV-1. Proc. Natl. Acad. Sci. USA 2007, 104, 19464–19469. [Google Scholar] [CrossRef]
- Puryear, W.B.; Yu, X.; Ramirez, N.P.; Reinhard, B.M.; Gummuluru, S. HIV-1 incorporation of host-cell-derived glycosphingolipid GM3 allows for capture by mature dendritic cells. Proc. Natl. Acad. Sci. USA 2012, 109, 7475–7480. [Google Scholar] [CrossRef]
- Izquierdo-Useros, N.; Lorizate, M.; McLaren, P.J.; Telenti, A.; Kräusslich, H.-G.; Martinez-Picado, J. HIV-1 capture and transmission by dendritic cells: The role of viral glycolipids and the cellular receptor Siglec-1. PLoS Pathog. 2014, 10, e1004146. [Google Scholar] [CrossRef]
- Akiyama, H.; Ramirez, N.-G.P.; Gudheti, M.V.; Gummuluru, S. CD169-mediated trafficking of HIV to plasma membrane invaginations in dendritic cells attenuates efficacy of anti-gp120 broadly neutralizing antibodies. PLoS Pathog. 2015, 11, e1004751. [Google Scholar] [CrossRef]
- Hoffmann, C.; Leis, A.; Niederweis, M.; Plitzko, J.M.; Engelhardt, H. Disclosure of the mycobacterial outer membrane: Cryo-electron tomography and vitreous sections reveal the lipid bilayer structure. Proc. Natl. Acad. Sci. USA 2008, 105, 3963–3967. [Google Scholar] [CrossRef]
- Zuber, B.; Chami, M.; Houssin, C.; Dubochet, J.; Griffiths, G.; Daffé, M. Direct visualization of the outer membrane of mycobacteria and corynebacteria in their native state. J. Bacteriol. 2008, 190, 5672–5680. [Google Scholar] [CrossRef]
- Angala, S.K.; Belardinelli, J.M.; Huc-Claustre, E.; Wheat, W.H.; Jackson, M. The cell envelope glycoconjugates of Mycobacterium tuberculosis. Crit. Rev. Biochem. Mol. Biol. 2014, 49, 361–399. [Google Scholar] [CrossRef] [PubMed]
- Bansal-Mutalik, R.; Nikaido, H. Mycobacterial outer membrane is a lipid bilayer and the inner membrane is unusually rich in diacyl phosphatidylinositol dimannosides. Proc. Natl. Acad. Sci. USA 2014, 111, 4958–4963. [Google Scholar] [CrossRef]
- Grzegorzewicz, A.E.; de Sousa-d’Auria, C.; McNeil, M.R.; Huc-Claustre, E.; Jones, V.; Petit, C.; Angala, S.K.; Zemanová, J.; Wang, Q.; Belardinelli, J.M.; et al. Assembling of the Mycobacterium tuberculosis Cell Wall Core. J. Biol. Chem. 2016, 291, 18867–18879. [Google Scholar] [CrossRef]
- Singh, P.; Rameshwaram, N.R.; Ghosh, S.; Mukhopadhyay, S. Cell envelope lipids in the pathophysiology of Mycobacterium tuberculosis. Future Microbiol. 2018, 13, 689–710. [Google Scholar] [CrossRef] [PubMed]
- Barry, C.E.; Lee, R.E.; Mdluli, K.; Sampson, A.E.; Schroeder, B.G.; Slayden, R.A.; Yuan, Y. Mycolic acids: Structure, biosynthesis and physiological functions. Prog. Lipid Res. 1998, 37, 143–179. [Google Scholar] [CrossRef]
- Dubnau, E.; Chan, J.; Raynaud, C.; Mohan, V.P.; Lanéelle, M.A.; Yu, K.; Quémard, A.; Smith, I.; Daffé, M. Oxygenated mycolic acids are necessary for virulence of Mycobacterium tuberculosis in mice. Mol. Microbiol. 2000, 36, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Vander Beken, S.; Al Dulayymi, J.R.; Naessens, T.; Koza, G.; Maza-Iglesias, M.; Rowles, R.; Theunissen, C.; De Medts, J.; Lanckacker, E.; Baird, M.S.; et al. Molecular structure of the Mycobacterium tuberculosis virulence factor, mycolic acid, determines the elicited inflammatory pattern. Eur. J. Immunol. 2011, 41, 450–460. [Google Scholar] [CrossRef]
- Dkhar, H.K.; Nanduri, R.; Mahajan, S.; Dave, S.; Saini, A.; Somavarapu, A.K.; Arora, A.; Parkesh, R.; Thakur, K.G.; Mayilraj, S.; et al. Mycobacterium tuberculosis Keto-Mycolic Acid and Macrophage Nuclear Receptor TR4 Modulate Foamy Biogenesis in Granulomas: A Case of a Heterologous and Noncanonical Ligand-Receptor Pair. J. Immunol. 2014, 193, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Means, T.K.; Wang, S.; Lien, E.; Yoshimura, A.; Golenbock, D.T.; Fenton, M.J. Human toll-like receptors mediate cellular activation by Mycobacterium tuberculosis. J. Immunol. 1999, 163, 3920–3927. [Google Scholar]
- Ryll, R.; Watanabe, K.; Fujiwara, N.; Takimoto, H.; Hasunuma, R.; Kumazawa, Y.; Okada, M.; Yano, I. Mycobacterial cord factor, but not sulfolipid, causes depletion of NKT cells and upregulation of CD1d1 on murine macrophages. Microbes Infect. 2001, 3, 611–619. [Google Scholar] [CrossRef]
- Geisel, R.E.; Sakamoto, K.; Russell, D.G.; Rhoades, E.R. In vivo activity of released cell wall lipids of Mycobacterium bovis bacillus Calmette-Guérin is due principally to trehalose mycolates. J. Immunol. 2005, 174, 5007–5015. [Google Scholar] [CrossRef] [PubMed]
- Linares, C.; Bernabéu, A.; Luquin, M.; Valero-Guillén, P.L. Cord factors from atypical mycobacteria (Mycobacterium alvei, Mycobacterium brumae) stimulate the secretion of some pro-inflammatory cytokines of relevance in tuberculosis. Microbiology 2012, 158, 2878–2885. [Google Scholar] [CrossRef] [PubMed]
- Welsh, K.J.; Hunter, R.L.; Actor, J.K. Trehalose 6,6′-dimycolate—A coat to regulate tuberculosis immunopathogenesis. Tuberculosis (Edinb.) 2013, 93, S3–S9. [Google Scholar] [CrossRef]
- Indrigo, J.; Hunter, R.L.; Actor, J.K. Influence of trehalose 6,6′-dimycolate (TDM) during mycobacterial infection of bone marrow macrophages. Microbiology 2002, 148, 1991–1998. [Google Scholar] [CrossRef]
- Ishikawa, E.; Ishikawa, T.; Morita, Y.S.; Toyonaga, K.; Yamada, H.; Takeuchi, O.; Kinoshita, T.; Akira, S.; Yoshikai, Y.; Yamasaki, S. Direct recognition of the mycobacterial glycolipid, trehalose dimycolate, by C-type lectin Mincle. J. Exp. Med. 2009, 206, 2879–2888. [Google Scholar] [CrossRef]
- Kan-Sutton, C.; Jagannath, C.; Hunter, R.L. Trehalose 6,6′-dimycolate on the surface of Mycobacterium tuberculosis modulates surface marker expression for antigen presentation and costimulation in murine macrophages. Microbes Infect. 2009, 11, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Hamasaki, N.; Isowa, K.; Kamada, K.; Terano, Y.; Matsumoto, T.; Arakawa, T.; Kobayashi, K.; Yano, I. In vivo administration of mycobacterial cord factor (Trehalose 6,6′-dimycolate) can induce lung and liver granulomas and thymic atrophy in rabbits. Infect. Immun. 2000, 68, 3704–3709. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, K.; Kim, M.J.; Rhoades, E.R.; Allavena, R.E.; Ehrt, S.; Wainwright, H.C.; Russell, D.G.; Rohde, K.H. Mycobacterial trehalose dimycolate reprograms macrophage global gene expression and activates matrix metalloproteinases. Infect. Immun. 2013, 81, 764–776. [Google Scholar] [CrossRef]
- Converse, S.E.; Mougous, J.D.; Leavell, M.D.; Leary, J.A.; Bertozzi, C.R.; Cox, J.S. MmpL8 is required for sulfolipid-1 biosynthesis and Mycobacterium tuberculosis virulence. Proc. Natl. Acad. Sci. USA 2003, 100, 6121–6126. [Google Scholar] [CrossRef]
- Domenech, P.; Reed, M.B.; Dowd, C.S.; Manca, C.; Kaplan, G.; Barry, C.E. The role of MmpL8 in sulfatide biogenesis and virulence of Mycobacterium tuberculosis. J. Biol. Chem. 2004, 279, 21257–21265. [Google Scholar] [CrossRef]
- Goren, M.B.; Brokl, O.; Schaefer, W.B. Lipids of putative relevance to virulence in Mycobacterium tuberculosis: Phthiocerol dimycocerosate and the attenuation indicator lipid. Infect. Immun. 1974, 9, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.S.; Chen, B.; McNeil, M.; Jacobs, W.R. Complex lipid determines tissue-specific replication of Mycobacterium tuberculosis in mice. Nature 1999, 402, 79–83. [Google Scholar] [CrossRef]
- Astarie-Dequeker, C.; Le Guyader, L.; Malaga, W.; Seaphanh, F.-K.; Chalut, C.; Lopez, A.; Guilhot, C. Phthiocerol dimycocerosates of M. tuberculosis participate in macrophage invasion by inducing changes in the organization of plasma membrane lipids. PLoS Pathog. 2009, 5, e1000289. [Google Scholar] [CrossRef] [PubMed]
- Quigley, J.; Hughitt, V.K.; Velikovsky, C.A.; Mariuzza, R.A.; El-Sayed, N.M.; Briken, V. The Cell Wall Lipid PDIM Contributes to Phagosomal Escape and Host Cell Exit of Mycobacterium tuberculosis. mBio 2017, 8, e00148-17. [Google Scholar] [CrossRef]
- Rousseau, C.; Winter, N.; Pivert, E.; Bordat, Y.; Neyrolles, O.; Avé, P.; Huerre, M.; Gicquel, B.; Jackson, M. Production of phthiocerol dimycocerosates protects Mycobacterium tuberculosis from the cidal activity of reactive nitrogen intermediates produced by macrophages and modulates the early immune response to infection. Cell. Microbiol. 2004, 6, 277–287. [Google Scholar] [CrossRef]
- Cambier, C.J.; Takaki, K.K.; Larson, R.P.; Hernandez, R.E.; Tobin, D.M.; Urdahl, K.B.; Cosma, C.L.; Ramakrishnan, L. Mycobacteria manipulate macrophage recruitment through coordinated use of membrane lipids. Nature 2014, 505, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Koppel, E.A.; Ludwig, I.S.; Sanchez Hernandez, M.; Lowary, T.L.; Gadikota, R.R.; Tuzikov, A.B.; Vandenbroucke-Grauls, C.M.J.E.; van Kooyk, Y.; Appelmelk, B.J.; Geijtenbeek, T.B.H. Identification of the mycobacterial carbohydrate structure that binds the C-type lectins DC-SIGN, L-SIGN and SIGNR1. Immunobiology 2004, 209, 117–127. [Google Scholar] [CrossRef]
- Pitarque, S.; Herrmann, J.-L.; Duteyrat, J.-L.; Jackson, M.; Stewart, G.R.; Lecointe, F.; Payre, B.; Schwartz, O.; Young, D.B.; Marchal, G.; et al. Deciphering the molecular bases of Mycobacterium tuberculosis binding to the lectin DC-SIGN reveals an underestimated complexity. Biochem. J. 2005, 392, 615–624. [Google Scholar] [CrossRef]
- Driessen, N.N.; Ummels, R.; Maaskant, J.J.; Gurcha, S.S.; Besra, G.S.; Ainge, G.D.; Larsen, D.S.; Painter, G.F.; Vandenbroucke-Grauls, C.M.J.E.; Geurtsen, J.; et al. Role of Phosphatidylinositol Mannosides in the Interaction between Mycobacteria and DC-SIGN. Infect. Immun. 2009, 77, 4538–4547. [Google Scholar] [CrossRef] [PubMed]
- Vignal, C.; Guérardel, Y.; Kremer, L.; Masson, M.; Legrand, D.; Mazurier, J.; Elass, E. Lipomannans, but not lipoarabinomannans, purified from Mycobacterium chelonae and Mycobacterium kansasii induce TNF-α and IL-8 secretion by a CD14-toll-like receptor 2-dependent mechanism. J. Immunol. 2003, 171, 2014–2023. [Google Scholar] [CrossRef]
- Quesniaux, V.J.; Nicolle, D.M.; Torres, D.; Kremer, L.; Guérardel, Y.; Nigou, J.; Puzo, G.; Erard, F.; Ryffel, B. Toll-like receptor 2 (TLR2)-dependent-positive and TLR2-independent-negative regulation of proinflammatory cytokines by mycobacterial lipomannans. J. Immunol. 2004, 172, 4425–4434. [Google Scholar] [CrossRef]
- Gilleron, M.; Nigou, J.; Nicolle, D.; Quesniaux, V.; Puzo, G. The acylation state of mycobacterial lipomannans modulates innate immunity response through toll-like receptor 2. Chem. Biol. 2006, 13, 39–47. [Google Scholar] [CrossRef]
- Doz, E.; Rose, S.; Nigou, J.; Gilleron, M.; Puzo, G.; Erard, F.; Ryffel, B.; Quesniaux, V.F.J. Acylation determines the toll-like receptor (TLR)-dependent positive versus TLR2-, mannose receptor-, and SIGNR1-independent negative regulation of pro-inflammatory cytokines by mycobacterial lipomannan. J. Biol. Chem. 2007, 282, 26014–26025. [Google Scholar] [CrossRef] [PubMed]
- Puissegur, M.-P.; Lay, G.; Gilleron, M.; Botella, L.; Nigou, J.; Marrakchi, H.; Mari, B.; Duteyrat, J.-L.; Guerardel, Y.; Kremer, L.; et al. Mycobacterial lipomannan induces granuloma macrophage fusion via a TLR2-dependent, ADAM9- and β1 integrin-mediated pathway. J. Immunol. 2007, 178, 3161–3169. [Google Scholar] [CrossRef]
- Guenin-Macé, L.; Siméone, R.; Demangel, C. Lipids of Pathogenic Mycobacteria: Contributions to Virulence and Host Immune Suppression. Transbound. Emerg. Dis. 2009, 56, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Daffé, M.; Crick, D.C.; Jackson, M. Genetics of Capsular Polysaccharides and Cell Envelope (Glyco)lipids. Microbiol. Spectr. 2014, 2, MGM2-0021-2013. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Zhang, M.; Barnes, P.F. Chemokine production by a human alveolar epithelial cell line in response to Mycobacterium tuberculosis. Infect. Immun. 1998, 66, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Theus, S.A.; Cave, M.D.; Eisenach, K.D. Intracellular Macrophage Growth Rates and Cytokine Profiles of Mycobacterium tuberculosis Strains with Different Transmission Dynamics. J. Infect. Dis. 2005, 191, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Mvubu, N.E.; Pillay, B.; McKinnon, L.R.; Pillay, M. Mycobacterium tuberculosis strains induce strain-specific cytokine and chemokine response in pulmonary epithelial cells. Cytokine 2018, 104, 53–64. [Google Scholar] [CrossRef]
- Mourik, B.C.; de Steenwinkel, J.E.M.; de Knegt, G.J.; Huizinga, R.; Verbon, A.; Ottenhoff, T.H.M.; van Soolingen, D.; Leenen, P.J.M. Mycobacterium tuberculosis clinical isolates of the Beijing and East-African Indian lineage induce fundamentally different host responses in mice compared to H37Rv. Sci. Rep. 2019, 9, 19922. [Google Scholar] [CrossRef]
- Manca, C.; Reed, M.B.; Freeman, S.; Mathema, B.; Kreiswirth, B.; Barry, C.E.; Kaplan, G. Differential monocyte activation underlies strain-specific Mycobacterium tuberculosis pathogenesis. Infect. Immun. 2004, 72, 5511–5514. [Google Scholar] [CrossRef]
- Reed, M.B.; Domenech, P.; Manca, C.; Su, H.; Barczak, A.K.; Kreiswirth, B.N.; Kaplan, G.; Barry, C.E. A glycolipid of hypervirulent tuberculosis strains that inhibits the innate immune response. Nature 2004, 431, 84–87. [Google Scholar] [CrossRef]
- Tsenova, L.; Ellison, E.; Harbacheuski, R.; Moreira, A.L.; Kurepina, N.; Reed, M.B.; Mathema, B.; Barry, C.E.; Kaplan, G. Virulence of selected Mycobacterium tuberculosis clinical isolates in the rabbit model of meningitis is dependent on phenolic glycolipid produced by the bacilli. J. Infect. Dis. 2005, 192, 98–106. [Google Scholar] [CrossRef]
- Theus, S.; Eisenach, K.; Fomukong, N.; Silver, R.F.; Cave, M.D. Beijing family Mycobacterium tuberculosis strains differ in their intracellular growth in THP-1 macrophages. Int. J. Tuberc. Lung Dis. 2007, 11, 1087–1093. [Google Scholar]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, preparation, and applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef] [PubMed]
- Sprott, G.D.; Dicaire, C.J.; Gurnani, K.; Sad, S.; Krishnan, L. Activation of Dendritic Cells by Liposomes Prepared from Phosphatidylinositol Mannosides from Mycobacterium bovis Bacillus Calmette-Guerin and Adjuvant Activity In Vivo. Infect. Immun. 2004, 72, 5235–5246. [Google Scholar] [CrossRef] [PubMed]
- Rosenkrands, I.; Agger, E.M.; Olsen, A.W.; Korsholm, K.S.; Andersen, C.S.; Jensen, K.T.; Andersen, P. Cationic liposomes containing mycobacterial lipids: A new powerful Th1 adjuvant system. Infect. Immun. 2005, 73, 5817–5826. [Google Scholar] [CrossRef]
- Cardona, P.-J. RUTI: A new chance to shorten the treatment of latent tuberculosis infection. Tuberculosis 2006, 86, 273–289. [Google Scholar] [CrossRef] [PubMed]
- Homhuan, A.; Kogure, K.; Akaza, H.; Futaki, S.; Naka, T.; Fujita, Y.; Yano, I.; Harashima, H. New packaging method of mycobacterial cell wall using octaarginine-modified liposomes: Enhanced uptake by and immunostimulatory activity of dendritic cells. J. Control. Release 2007, 120, 60–69. [Google Scholar] [CrossRef]
- Kawasaki, N.; Rillahan, C.D.; Cheng, T.-Y.; Van Rhijn, I.; Macauley, M.S.; Moody, D.B.; Paulson, J.C. Targeted Delivery of Mycobacterial Antigens to Human Dendritic Cells via Siglec-7 Induces Robust T Cell Activation. J. Immunol. 2014, 193, 1560–1566. [Google Scholar] [CrossRef] [PubMed]
- Khademi, F.; Taheri, R.A.; Momtazi-Borojeni, A.A.; Farnoosh, G.; Johnston, T.P.; Sahebkar, A. Potential of Cationic Liposomes as Adjuvants/Delivery Systems for Tuberculosis Subunit Vaccines. Rev. Physiol. Biochem. Pharmacol. 2018, 175, 47–69. [Google Scholar] [CrossRef]
- Ioerger, T.R.; Feng, Y.; Ganesula, K.; Chen, X.; Dobos, K.M.; Fortune, S.; Jacobs, W.R.; Mizrahi, V.; Parish, T.; Rubin, E.; et al. Variation among genome sequences of H37Rv strains of Mycobacterium tuberculosis from multiple laboratories. J. Bacteriol. 2010, 192, 3645–3653. [Google Scholar] [CrossRef]
- Nakata, K.; Rom, W.N.; Honda, Y.; Condos, R.; Kanegasaki, S.; Cao, Y.; Weiden, M. Mycobacterium tuberculosis enhances human immunodeficiency virus-1 replication in the lung. Am. J. Respir. Crit. Care Med. 1997, 155, 996–1003. [Google Scholar] [CrossRef]
- Lawn, S.D.; Pisell, T.L.; Hirsch, C.S.; Wu, M.; Butera, S.T.; Toossi, Z. Anatomically compartmentalized human immunodeficiency virus replication in HLA-DR+ cells and CD14+ macrophages at the site of pleural tuberculosis coinfection. J. Infect. Dis. 2001, 184, 1127–1133. [Google Scholar] [CrossRef]
- McDonald, D.; Wu, L.; Bohks, S.M.; KewalRamani, V.N.; Unutmaz, D.; Hope, T.J. Recruitment of HIV and its receptors to dendritic cell-T cell junctions. Science 2003, 300, 1295–1297. [Google Scholar] [CrossRef]
- Wu, L. Biology of HIV mucosal transmission. Curr. Opin. HIV AIDS 2008, 3, 534–540. [Google Scholar] [CrossRef]
- Miyake, Y.; Toyonaga, K.; Mori, D.; Kakuta, S.; Hoshino, Y.; Oyamada, A.; Yamada, H.; Ono, K.-I.; Suyama, M.; Iwakura, Y.; et al. C-type lectin MCL is an FcRγ-coupled receptor that mediates the adjuvanticity of mycobacterial cord factor. Immunity 2013, 38, 1050–1062. [Google Scholar] [CrossRef]
- Rousseau, C.; Turner, O.C.; Rush, E.; Bordat, Y.; Sirakova, T.D.; Kolattukudy, P.E.; Ritter, S.; Orme, I.M.; Gicquel, B.; Jackson, M. Sulfolipid deficiency does not affect the virulence of Mycobacterium tuberculosis H37Rv in mice and guinea pigs. Infect. Immun. 2003, 71, 4684–4690. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Schelle, M.W.; Jain, M.; Lin, F.L.; Petzold, C.J.; Leavell, M.D.; Leary, J.A.; Cox, J.S.; Bertozzi, C.R. PapA1 and PapA2 are acyltransferases essential for the biosynthesis of the Mycobacterium tuberculosis virulence factor sulfolipid-1. Proc. Natl. Acad. Sci. USA 2007, 104, 11221–11226. [Google Scholar] [CrossRef] [PubMed]
- Granelli-Piperno, A.; Delgado, E.; Finkel, V.; Paxton, W.; Steinman, R.M. Immature dendritic cells selectively replicate macrophagetropic (M-tropic) human immunodeficiency virus type 1, while mature cells efficiently transmit both M- and T-tropic virus to T cells. J. Virol. 1998, 72, 2733–2737. [Google Scholar] [CrossRef]
- Sanders, R.W.; de Jong, E.C.; Baldwin, C.E.; Schuitemaker, J.H.N.; Kapsenberg, M.L.; Berkhout, B. Differential transmission of human immunodeficiency virus type 1 by distinct subsets of effector dendritic cells. J. Virol. 2002, 76, 7812–7821. [Google Scholar] [CrossRef]
- Perot, B.P.; García-Paredes, V.; Luka, M.; Ménager, M.M. Dendritic Cell Maturation Regulates TSPAN7 Function in HIV-1 Transfer to CD4+ T Lymphocytes. Front. Cell. Infect. Microbiol. 2020, 10, 70. [Google Scholar] [CrossRef] [PubMed]
- Bafica, A.; Scanga, C.A.; Schito, M.L.; Hieny, S.; Sher, A. Cutting Edge: In Vivo Induction of Integrated HIV-1 Expression by Mycobacteria Is Critically Dependent on Toll-Like Receptor 2. J. Immunol. 2003, 171, 1123–1127. [Google Scholar] [CrossRef]
- Equils, O.; Schito, M.L.; Karahashi, H.; Madak, Z.; Yarali, A.; Michelsen, K.S.; Sher, A.; Arditi, M. Toll-Like Receptor 2 (TLR2) and TLR9 Signaling Results in HIV-Long Terminal Repeat Trans-Activation and HIV Replication in HIV-1 Transgenic Mouse Spleen Cells: Implications of Simultaneous Activation of TLRs on HIV Replication. J. Immunol. 2003, 170, 5159–5164. [Google Scholar] [CrossRef] [PubMed]
- Larson, E.C.; Novis, C.L.; Martins, L.J.; Macedo, A.B.; Kimball, K.E.; Bosque, A.; Planelles, V.; Barrows, L.R. Mycobacterium tuberculosis reactivates latent HIV-1 in T cells in vitro. PLoS ONE 2017, 12, e0185162. [Google Scholar] [CrossRef] [PubMed]
- Goletti, D.; Weissman, D.; Jackson, R.W.; Collins, F.; Kinter, A.; Fauci, A.S. The in vitro induction of human immunodeficiency virus (HIV) replication in purified protein derivative-positive HIV-infected persons by recall antigen response to Mycobacterium tuberculosis is the result of a balance of the effects of endogenous interleu. J. Infect. Dis. 1998, 177, 1332–1338. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoshino, Y.; Tse, D.B.; Rochford, G.; Prabhakar, S.; Hoshino, S.; Chitkara, N.; Kuwabara, K.; Ching, E.; Raju, B.; Gold, J.A.; et al. Mycobacterium tuberculosis-induced CXCR4 and chemokine expression leads to preferential X4 HIV-1 replication in human macrophages. J. Immunol. 2004, 172, 6251–6258. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.E.; Loyd, C.M.; Ding, X.; Karim, A.F.; McDonald, D.J.; Canaday, D.H.; Rojas, R.E. Mycobacterial phosphatidylinositol mannoside 6 (PIM6) up-regulates TCR-triggered HIV-1 replication in CD4+ T cells. PLoS ONE 2013, 8, e80938. [Google Scholar] [CrossRef]
- Tomlinson, G.S.; Bell, L.C.K.; Walker, N.F.; Tsang, J.; Brown, J.S.; Breen, R.; Lipman, M.; Katz, D.R.; Miller, R.F.; Chain, B.M.; et al. HIV-1 infection of macrophages dysregulates innate immune responses to Mycobacterium tuberculosis by inhibition of interleukin-10. J. Infect. Dis. 2014, 209, 1055–1065. [Google Scholar] [CrossRef]
- Bhatt, K.; Gurcha, S.S.; Bhatt, A.; Besra, G.S.; Jacobs, W.R. Two polyketide-synthase-associated acyltransferases are required for sulfolipid biosynthesis in Mycobacterium tuberculosis. Microbiology 2007, 153, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Dobson, G.; Minnikin, D.E.; Minnikin, S.M.; Parlett, J.H.; Goodfellow, M.; Ridell, M.; Magnusson, M. Systematic analysis of complex mycobacterial lipids. In Chemical Methodscin Bacterial Systematics; Goodfellow, M., Minnikin, D.E., Eds.; Academic Press: London, UK, 1985; Volume 1, pp. 237–265. [Google Scholar]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pouget, M.; Coussens, A.K.; Ruggiero, A.; Koch, A.; Thomas, J.; Besra, G.S.; Wilkinson, R.J.; Bhatt, A.; Pollakis, G.; Paxton, W.A. Generation of Liposomes to Study the Effect of Mycobacterium Tuberculosis Lipids on HIV-1 cis- and trans-Infections. Int. J. Mol. Sci. 2021, 22, 1945. https://doi.org/10.3390/ijms22041945
Pouget M, Coussens AK, Ruggiero A, Koch A, Thomas J, Besra GS, Wilkinson RJ, Bhatt A, Pollakis G, Paxton WA. Generation of Liposomes to Study the Effect of Mycobacterium Tuberculosis Lipids on HIV-1 cis- and trans-Infections. International Journal of Molecular Sciences. 2021; 22(4):1945. https://doi.org/10.3390/ijms22041945
Chicago/Turabian StylePouget, Marion, Anna K. Coussens, Alessandra Ruggiero, Anastasia Koch, Jordan Thomas, Gurdyal S. Besra, Robert J. Wilkinson, Apoorva Bhatt, Georgios Pollakis, and William A. Paxton. 2021. "Generation of Liposomes to Study the Effect of Mycobacterium Tuberculosis Lipids on HIV-1 cis- and trans-Infections" International Journal of Molecular Sciences 22, no. 4: 1945. https://doi.org/10.3390/ijms22041945
APA StylePouget, M., Coussens, A. K., Ruggiero, A., Koch, A., Thomas, J., Besra, G. S., Wilkinson, R. J., Bhatt, A., Pollakis, G., & Paxton, W. A. (2021). Generation of Liposomes to Study the Effect of Mycobacterium Tuberculosis Lipids on HIV-1 cis- and trans-Infections. International Journal of Molecular Sciences, 22(4), 1945. https://doi.org/10.3390/ijms22041945






