Liquid Biopsies in the Clinical Management of Germ Cell Tumor Patients: State-of-the-Art and Future Directions
Abstract
:1. Introduction: Current Clinical Challenges in Germ Cell Tumors
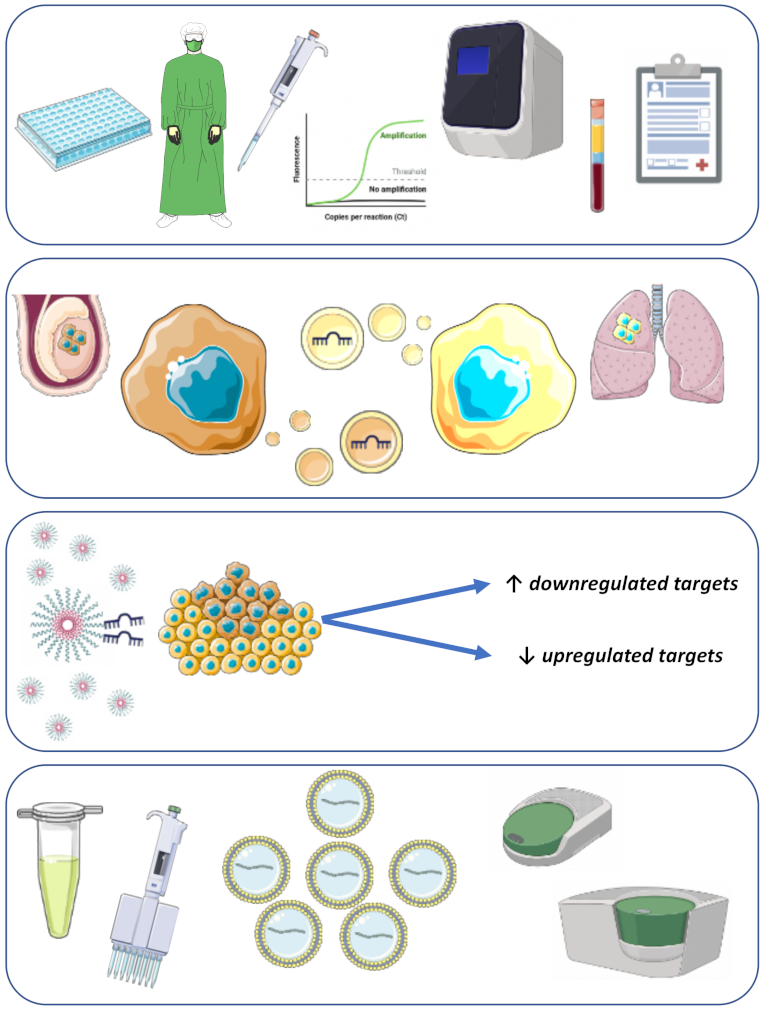
2. Classical Serum Tumor Markers
3. MicroRNAs
3.1. Focus on Diagnosis
3.2. Focus on Follow-Up
3.3. Focus on the Identification of Metastatic Viable Disease/Teratoma
4. Cell Free DNA (cfDNA)
5. CTCs
6. Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Oosterhuis, J.W.; Looijenga, L.H.J. Human germ cell tumours from a developmental perspective. Nat. Rev. Cancer 2019, 19, 522–537. [Google Scholar] [CrossRef] [PubMed]
- Lobo, J.; Gillis, A.J.M.; Jeronimo, C.; Henrique, R.; Looijenga, L.H.J. Human Germ Cell Tumors are Developmental Cancers: Impact of Epigenetics on Pathobiology and Clinic. Int. J. Mol. Sci. 2019, 20, 258. [Google Scholar] [CrossRef] [Green Version]
- Lobo, J.; Costa, A.L.; Vilela-Salgueiro, B.; Rodrigues, A.; Guimaraes, R.; Cantante, M.; Lopes, P.; Antunes, L.; Jerónimo, C.; Henrique, R. Testicular germ cell tumors: Revisiting a series in light of the new WHO classification and AJCC staging systems, focusing on challenges for pathologists. Hum. Pathol. 2018, 82, 113–124. [Google Scholar] [CrossRef]
- Cheng, L.; Albers, P.; Berney, D.M.; Feldman, D.R.; Daugaard, G.; Gilligan, T.; Looijenga, L. Testicular cancer. Nat. Rev. Dis. Primers 2018, 4, 29. [Google Scholar] [CrossRef] [PubMed]
- Bagrodia, A.; Albany, C.; Masterson, T.A. Germ Cell Tumors: Updates on Epidemiology, Biology, and Treatment Considerations. Adv. Urol. 2018, 2018, 4821084.a. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajpert-De Meyts, E.; McGlynn, K.A.; Okamoto, K.; Jewett, M.A.; Bokemeyer, C. Testicular germ cell tumours. Lancet 2016, 387, 1762–1774. [Google Scholar] [CrossRef]
- Park, J.S.; Kim, J.; Elghiaty, A.; Ham, W.S. Recent global trends in testicular cancer incidence and mortality. Medicine 2018, 97, e12390. [Google Scholar] [CrossRef]
- Dieckmann, K.P.; Frey, U.; Lock, G. Contemporary diagnostic work-up of testicular germ cell tumours. Nat. Rev. Urol. 2013, 10, 703–712. [Google Scholar] [CrossRef]
- Dieckmann, K.P.; Simonsen-Richter, H.; Kulejewski, M.; Anheuser, P.; Zecha, H.; Isbarn, H.; Pichlmeier, U. Serum Tumour Markers in Testicular Germ Cell Tumours: Frequencies of Elevated Levels and Extents of Marker Elevation Are Significantly Associated with Clinical Parameters and with Response to Treatment. BioMed Res. Int. 2019, 2019, 5030349. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, K.P.; Kulejewski, M.; Heinemann, V.; Loy, V. Testicular biopsy for early cancer detection—Objectives, technique and controversies. Int. J. Androl. 2011, 34 Pt 2, e7–e13. [Google Scholar] [CrossRef]
- De Rubis, G.; Rajeev Krishnan, S.; Bebawy, M. Liquid Biopsies in Cancer Diagnosis, Monitoring, and Prognosis. Trends Pharmacol. Sci. 2019, 40, 172–186. [Google Scholar] [CrossRef]
- Chovanec, M.; Kalavska, K.; Mego, M.; Cheng, L. Liquid biopsy in germ cell tumors: Biology and clinical management. Expert Rev. Mol. Diagn. 2020, 20, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Chung, P.; O’Malley, M.E.; Jewett, M.A.S.; Bedard, P.L.; Panzarella, T.; Sturgeon, J.; Moore, M.J.; Hamilton, R.; Hansen, A.R.; Anson-Cartwright, L.; et al. Detection of Relapse by Low-dose Computed Tomography During Surveillance in Stage I Testicular Germ Cell Tumours. Eur. Urol. Oncol. 2019, 2, 437–442. [Google Scholar] [CrossRef]
- Chovanec, M.; Hanna, N.; Cary, K.C.; Einhorn, L.; Albany, C. Management of stage I testicular germ cell tumours. Nat. Rev. Urol. 2016, 13, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Leao, R.; Ahmad, A.E.; Hamilton, R.J. Testicular Cancer Biomarkers: A Role for Precision Medicine in Testicular Cancer. Clin. Genitourin. Cancer 2019, 17, e176–e183. [Google Scholar] [CrossRef] [PubMed]
- Chovanec, M.; Abu Zaid, M.; Hanna, N.; El-Kouri, N.; Einhorn, L.H.; Albany, C. Long-term toxicity of cisplatin in germ-cell tumor survivors. Ann. Oncol. 2017, 28, 2670–2679. [Google Scholar] [CrossRef] [PubMed]
- Fung, C.; Dinh, P., Jr.; Ardeshir-Rouhani-Fard, S.; Schaffer, K.; Fossa, S.D.; Travis, L.B. Toxicities Associated with Cisplatin-Based Chemotherapy and Radiotherapy in Long-Term Testicular Cancer Survivors. Adv. Urol. 2018, 2018, 8671832. [Google Scholar] [CrossRef]
- Lago-Hernandez, C.A.; Feldman, H.; O’Donnell, E.; Mahal, B.A.; Perez, V.; Howard, S.; Rosenthal, M.; Cheng, S.C.; Nguyen, P.L.; Beard, C.; et al. A refined risk stratification scheme for clinical stage 1 NSGCT based on evaluation of both embryonal predominance and lymphovascular invasion. Ann. Oncol. 2015, 26, 1396–1401. [Google Scholar] [CrossRef]
- Lobo, J.; Stoop, H.; Gillis, A.J.M.; Looijenga, L.H.J.; Oosterhuis, W. Interobserver Agreement in Vascular Invasion Scoring and the Added Value of Immunohistochemistry for Vascular Markers to Predict Disease Relapse in Stage I Testicular Nonseminomas. Am. J. Surg. Pathol. 2019, 43, 1711–1719. [Google Scholar] [CrossRef]
- Boormans, J.L.; Mayor de Castro, J.; Marconi, L.; Yuan, Y.; Laguna Pes, M.P.; Bokemeyer, C.; Nicolai, N.; Algaba, F.; Oldenburg, J.; Albers, P. Testicular Tumour Size and Rete Testis Invasion as Prognostic Factors for the Risk of Relapse of Clinical Stage I Seminoma Testis Patients Under Surveillance: A Systematic Review by the Testicular Cancer Guidelines Panel. Eur. Urol. 2018, 73, 394–405. [Google Scholar] [CrossRef]
- Leão, R.; Nayan, M.; Punjani, N.; Jewett, M.A.S.; Fadaak, K.; Garisto, J.; Lewin, J.; Atenafu, E.G.; Sweet, J.; Anson-Cartwright, L.; et al. A New Model to Predict Benign Histology in Residual Retroperitoneal Masses After Chemotherapy in Nonseminoma. Eur. Urol. Focus 2018, 4, 995–1001. [Google Scholar] [CrossRef]
- Honecker, F.; Aparicio, J.; Berney, D.; Beyer, J.; Bokemeyer, C.; Cathomas, R.; Cohn-Cedermark, G.; Daugaard, G.; Dieckmann, K.P.; Fizazi, K.; et al. ESMO Consensus Conference on testicular germ cell cancer: Diagnosis, treatment and follow-up. Ann. Oncol. 2018, 29, 1658–1686. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.J.; Huddart, R.A.; Coleman, N. The present and future of serum diagnostic tests for testicular germ cell tumours. Nat. Rev. Urol. 2016, 13, 715–725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milose, J.C.; Filson, C.P.; Weizer, A.Z.; Hafez, K.S.; Montgomery, J.S. Role of biochemical markers in testicular cancer: Diagnosis, staging, and surveillance. Open Access J. Urol. 2011, 4, 1–8. [Google Scholar] [PubMed] [Green Version]
- Almstrup, K.; Lobo, J.; Morup, N.; Belge, G.; Rajpert-De Meyts, E.; Looijenga, L.H.J.; Dieckmann, K.P. Application of miRNAs in the diagnosis and monitoring of testicular germ cell tumours. Nat. Rev. Urol. 2020, 17, 201–213. [Google Scholar] [CrossRef] [PubMed]
- Bergstrand, C.G.; Czar, B. Demonstration of a new protein fraction in serum from the human fetus. Scand. J. Clin. Lab. Investig. 1956, 8, 174. [Google Scholar] [CrossRef]
- Gitlin, D.; Boesman, M. Sites of serum alpha-fetoprotein synthesis in the human and in the rat. J. Clin. Investig. 1967, 46, 1010–1016. [Google Scholar] [CrossRef] [Green Version]
- Abelev, G.I.; Assecritova, I.V.; Kraevsky, N.A.; Perova, S.D.; Perevodchikova, N.I. Embryonal serum alpha-globulin in cancer patients: Diagnostic value. Int. J. Cancer 1967, 2, 551–558. [Google Scholar] [CrossRef]
- Talerman, A.; van der Pompe, W.B.; Haije, W.G.; Baggerman, L.; Boekestein-Tjahjadi, H.M. Alpha-foetoprotein and carcinoembryonic antigen in germ cell neoplasms. Br. J. Cancer 1977, 35, 288–291. [Google Scholar] [CrossRef] [Green Version]
- Germa-Lluch, J.R.; Garcia del Muro, X.; Maroto, P.; Paz-Ares, L.; Arranz, J.A.; Guma, J.; Alba, E.; Sastre, J.; Aparicio, J.; Fernández, A.; et al. Clinical pattern and therapeutic results achieved in 1490 patients with germ-cell tumours of the testis: The experience of the Spanish Germ-Cell Cancer Group (GG). Eur. Urol. 2002, 42, 553–562. [Google Scholar] [CrossRef]
- Blohm, M.E.; Vesterling-Horner, D.; Calaminus, G.; Gobel, U. Alpha 1-fetoprotein (AFP) reference values in infants up to 2 years of age. Pediatr. Hematol. Oncol. 1998, 15, 135–142. [Google Scholar] [CrossRef]
- Kitada, M.; Ozawa, K.; Sato, K.; Matsuda, Y.; Hayashi, S.; Tokusashi, Y.; Miyokawa, N.; Sasajima, T. Alpha-fetoprotein-producing primary lung carcinoma: A case report. World J. Surg. Oncol. 2011, 9, 47. [Google Scholar] [CrossRef] [Green Version]
- Kawamoto, S.; Hiraoka, T.; Kanemitsu, K.; Kimura, M.; Miyauchi, Y.; Takeya, M. Alpha-fetoprotein-producing pancreatic cancer--a case report and review of 28 cases. Hepatogastroenterology 1992, 39, 282–286. [Google Scholar] [PubMed]
- Murakami, T.; Yao, T.; Mitomi, H.; Morimoto, T.; Ueyama, H.; Matsumoto, K.; Saito, T.; Osada, T.; Nagahara, A.; Watanabe, S. Clinicopathologic and immunohistochemical characteristics of gastric adenocarcinoma with enteroblastic differentiation: A study of 29 cases. Gastric Cancer 2016, 19, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Germa, J.R.; Llanos, M.; Tabernero, J.M.; Mora, J. False elevations of alpha-fetoprotein associated with liver dysfunction in germ cell tumors. Cancer 1993, 72, 2491–2494. [Google Scholar] [CrossRef]
- Houwert, A.C.; Giltay, J.C.; Lentjes, E.G.; Lock, M.T. Hereditary persistence of alpha-fetoprotein (HPAF P): Review of the literature. Neth. J. Med. 2010, 68, 354–358. [Google Scholar] [PubMed]
- Cole, L.A. The hCG assay or pregnancy test. Clin. Chem. Lab. Med. 2012, 50, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Rao, C.V.; Lei, Z.M. The past, present and future of nongonadal LH/hCG actions in reproductive biology and medicine. Mol. Cell Endocrinol. 2007, 269, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Weissbach, L.; Bussar-Maatz, R.; Lohrs, U.; Schubert, G.E.; Mann, K.; Hartmann, M.; Dieckmann, K.P.; Fassbinder, J. Prognostic factors in seminomas with special respect to HCG: Results of a prospective multicenter study. Seminoma Study Group. Eur. Urol. 1999, 36, 601–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stenman, U.H.; Alfthan, H.; Hotakainen, K. Human chorionic gonadotropin in cancer. Clin. Biochem. 2004, 37, 549–561. [Google Scholar] [CrossRef]
- Trojan, A.; Joller-Jemelka, H.; Stahel, R.A.; Jacky, E.; Hersberger, M. False-positive human serum chorionic gonadotropin in a patient with a history of germ cell cancer. Oncology 2004, 66, 336–338. [Google Scholar] [CrossRef] [PubMed]
- Germa, J.R.; Arcusa, A.; Casamitjana, R. False elevations of human chorionic gonadotropin associated to iatrogenic hypogonadism in gonadal germ cell tumors. Cancer 1987, 60, 2489–2493. [Google Scholar] [CrossRef]
- Braunstein, G.D.; Thompson, R.; Gross, S.; Soares, J.R. Marijuana use does not spuriously elevate serum human chorionic gonadotropin levels. Urology 1985, 25, 605–606. [Google Scholar] [CrossRef]
- Jialal, I.; Sokoll, L.J. Clinical utility of lactate dehydrogenase: A historical perspective. Am. J. Clin. Pathol. 2015, 143, 158–159. [Google Scholar] [CrossRef]
- Rampello, E.; Fricia, T.; Malaguarnera, M. The management of tumor lysis syndrome. Nat. Clin. Pract. Oncol. 2006, 3, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Allemailem, K.S.; Alhumaydhi, F.A.; Gowder, S.J.T.; Rahmani, A.H. The Biochemical and Clinical Perspectives of Lactate Dehydrogenase: An Enzyme of Active Metabolism. Endocr. Metab. Immune Disord. Drug Targets 2020, 20, 855–868. [Google Scholar] [CrossRef] [PubMed]
- Von Eyben, F.E.; de Graaff, W.E.; Marrink, J.; Blaabjerg, O.; Sleijfer, D.T.; Koops, H.S.; Oosterhuis, J.W.; Petersen, P.H.; Echten-Arends, J.; Jong, B. Serum lactate dehydrogenase isoenzyme 1 activity in patients with testicular germ cell tumors correlates with the total number of copies of the short arm of chromosome 12 in the tumor. Mol. Gen. Genet. 1992, 235, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Salem, M.; Gilligan, T. Serum tumor markers and their utilization in the management of germ-cell tumors in adult males. Expert Rev. Anticancer Ther. 2011, 11, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Gilligan, T.D.; Seidenfeld, J.; Basch, E.M.; Einhorn, L.H.; Fancher, T.; Smith, D.C.; Stephenson, A.J.; Vaughn, D.J.; Cosby, R.; Hayes, D.F.; et al. American Society of Clinical Oncology Clinical Practice Guideline on uses of serum tumor markers in adult males with germ cell tumors. J. Clin. Oncol. 2010, 28, 3388–3404. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, C.; Honecker, F. Cisplatin resistance in germ cell tumours: Models and mechanisms. Andrology 2015, 3, 111–121. [Google Scholar] [CrossRef]
- Oing, C.; Seidel, C.; Bokemeyer, C. Therapeutic approaches for refractory germ cell cancer. Expert Rev. Anticancer Ther. 2018, 18, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Kollmannsberger, C.; Tandstad, T.; Bedard, P.L.; Cohn-Cedermark, G.; Chung, P.W.; Jewett, M.A.; Powles, T.; Warde, P.R.; Daneshmand, S.; Protheroe, A.; et al. Patterns of relapse in patients with clinical stage I testicular cancer managed with active surveillance. J. Clin. Oncol. 2015, 33, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Saito, T.; Kitamura, Y.; Nobushita, T.; Kawasaki, T.; Hara, N.; Takahashi, K. Oncological outcomes in patients with stage I testicular seminoma and nonseminoma: Pathological risk factors for relapse and feasibility of surveillance after orchiectomy. Diagn. Pathol. 2013, 8, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ackers, C.; Rustin, G.J. Lactate dehydrogenase is not a useful marker for relapse in patients on surveillance for stage I germ cell tumours. Br. J. Cancer 2006, 94, 1231–1232. [Google Scholar] [CrossRef] [Green Version]
- Fankhauser, C.D.; Gerke, T.A.; Roth, L.; Sander, S.; Grossmann, N.C.; Kranzbuhler, B.; Eberli, D.; Sulser, T.; Beyer, J.; Hermanns, T. Pre-orchiectomy tumor marker levels should not be used for International Germ Cell Consensus Classification (IGCCCG) risk group assignment. J. Cancer Res. Clin. Oncol. 2019, 145, 781–785. [Google Scholar] [CrossRef] [Green Version]
- Wilkinson, P.M.; Read, G. International Germ Cell Consensus Classification: A prognostic factor-based staging system for metastatic germ cell cancers. International Germ Cell Cancer Collaborative Group. J. Clin. Oncol. 1997, 15, 594–603. [Google Scholar]
- Neumann, A.; Keller, T.; Jocham, D.; Doehn, C. Human placental alkaline phosphatase (hPLAP) is the most frequently elevated serum marker in testicular cancer. Aktuelle Urologie 2011, 42, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Koshida, K.; Uchibayashi, T.; Yamamoto, H.; Hirano, K. Significance of placental alkaline phosphatase (PLAP) in the monitoring of patients with seminoma. Br. J. Urol. 1996, 77, 138–142. [Google Scholar] [CrossRef] [PubMed]
- De Broe, M.E.; Pollet, D.E. Multicenter evaluation of human placental alkaline phosphatase as a possible tumor-associated antigen in serum. Clin. Chem. 1988, 34, 1995–1999. [Google Scholar] [CrossRef]
- Lajer, H.; Daugaard, G.; Andersson, A.M.; Skakkebaek, N.E. Clinical use of serum TRA-1–60 as tumor marker in patients with germ cell cancer. Int. J. Cancer 2002, 100, 244–246. [Google Scholar] [CrossRef]
- Gels, M.E.; Marrink, J.; Visser, P.; Sleijfer, D.T.; Droste, J.H.; Hoekstra, H.J.; Andrews, P.W.; Koops, H.S. Importance of a new tumor marker TRA-1–60 in the follow-up of patients with clinical stage I nonseminomatous testicular germ cell tumors. Ann. Surg. Oncol. 1997, 4, 321–327. [Google Scholar] [CrossRef]
- Fossa, S.D.; Klepp, O.; Paus, E. Neuron-specific enolase—A serum tumour marker in seminoma? Br. J. Cancer 1992, 65, 297–299. [Google Scholar] [CrossRef] [Green Version]
- Tandstad, T.; Klepp, O. Neuron-specific enolase in testicular cancer--clinical experiences with serum neuron-specific enolase in patients with testicular cancer at diagnosis and during follow-up. Acta Oncol. 2003, 42, 202–206. [Google Scholar] [CrossRef]
- Narita, T.; Hatakeyama, S.; Yoneyama, T.; Narita, S.; Yamashita, S.; Mitsuzuka, K.; Sakurai, T.; Kawamura, S.; Tochigi, T.; Takahashi, I.; et al. Clinical implications of serum N-glycan profiling as a diagnostic and prognostic biomarker in germ-cell tumors. Cancer Med. 2017, 6, 739–748. [Google Scholar] [CrossRef]
- Novotny, G.W.; Belling, K.C.; Bramsen, J.B.; Nielsen, J.E.; Bork-Jensen, J.; Almstrup, K.; Sonne, S.B.; Kjems, J.; Rajpert-De-Meyts, E.; Leffers, H. MicroRNA expression profiling of carcinoma in situ cells of the testis. Endocr. Relat. Cancer 2012, 19, 365–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eini, R.; Dorssers, L.C.; Looijenga, L.H. Role of stem cell proteins and microRNAs in embryogenesis and germ cell cancer. Int. J. Dev. Biol. 2013, 57, 319–332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lobo, J.; Gillis, A.J.M.; van den Berg, A.; Dorssers, L.C.J.; Belge, G.; Dieckmann, K.P.; Roest, H.P.; van der Laan, L.J.W.; Gietema, J.; Hamilton, R.J.; et al. Identification and Validation Model for Informative Liquid Biopsy-Based microRNA Biomarkers: Insights from Germ Cell Tumor In Vitro, In Vivo and Patient-Derived Data. Cells 2019, 8, 1637. [Google Scholar] [CrossRef] [Green Version]
- Salvatori, D.C.F.; Dorssers, L.C.J.; Gillis, A.J.M.; Perretta, G.; van Agthoven, T.; Gomes Fernandes, M.; Stoop, H.; Prins, J.B.; Oosterhuis, J.W.; Mummery, C.; et al. The MicroRNA-371 Family as Plasma Biomarkers for Monitoring Undifferentiated and Potentially Malignant Human Pluripotent Stem Cells in Teratoma Assays. Stem Cell Rep. 2018, 11, 1493–1505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmer, R.D.; Murray, M.J.; Saini, H.K.; van Dongen, S.; Abreu-Goodger, C.; Muralidhar, B.; Pett, M.R.; Thornton, C.M.; Nicholson, J.C.; Enright, A.J.; et al. Malignant germ cell tumors display common microRNA profiles resulting in global changes in expression of messenger RNA targets. Cancer Res. 2010, 70, 2911–2923. [Google Scholar] [CrossRef] [Green Version]
- Voorhoeve, P.M.; le Sage, C.; Schrier, M.; Gillis, A.J.; Stoop, H.; Nagel, R.; Liu, Y.P.; Duijse, J.; Drost, J.; Griekspoor, A.; et al. A genetic screen implicates miRNA-372 and miRNA-373 as oncogenes in testicular germ cell tumors. Cell 2006, 124, 1169–1181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gillis, A.J.; Stoop, H.J.; Hersmus, R.; Oosterhuis, J.W.; Sun, Y.; Chen, C.; Guenther, S.; Sherlock, J.; Veltman, I.; Baeten, J.; et al. High-throughput microRNAome analysis in human germ cell tumours. J. Pathol. 2007, 213, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Vilela-Salgueiro, B.; Barros-Silva, D.; Lobo, J.; Costa, A.L.; Guimaraes, R.; Cantante, M.; Lopes, P.; Braga, I.; Oliveira, J.; Henrique, R.; et al. Germ cell tumour subtypes display differential expression of microRNA371a-3p. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2018, 373, 20170338. [Google Scholar] [CrossRef]
- Bing, Z.; Master, S.R.; Tobias, J.W.; Baldwin, D.A.; Xu, X.W.; Tomaszewski, J.E. MicroRNA expression profiles of seminoma from paraffin-embedded formalin-fixed tissue. Virchows Arch. 2012, 461, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, K.P.; Spiekermann, M.; Balks, T.; Flor, I.; Loning, T.; Bullerdiek, J.; Belge, G. MicroRNAs miR-371–3 in serum as diagnostic tools in the management of testicular germ cell tumours. Br. J. Cancer 2012, 107, 1754–1760. [Google Scholar] [CrossRef] [Green Version]
- Radtke, A.; Cremers, J.F.; Kliesch, S.; Riek, S.; Junker, K.; Mohamed, S.A.; Anheuser, P.; Belge, G.; Dieckmann, K.P. Can germ cell neoplasia in situ be diagnosed by measuring serum levels of microRNA371a-3p? J. Cancer Res. Clin. Oncol. 2017, 143, 2383–2392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belge, G.; Hennig, F.; Dumlupinar, C.; Grobelny, F.; Junker, K.; Radtke, A.; Dieckmann, K.P. Graded expression of microRNA-371a-3p in tumor tissues, contralateral testes, and in serum of patients with testicular germ cell tumor. Oncotarget 2020, 11, 1462–1473. [Google Scholar] [CrossRef] [Green Version]
- Rijlaarsdam, M.A.; van Agthoven, T.; Gillis, A.J.; Patel, S.; Hayashibara, K.; Lee, K.Y.; Looijenga, L.H.J. Identification of known and novel germ cell cancer-specific (embryonic) miRs in serum by high-throughput profiling. Andrology 2015, 3, 85–91. [Google Scholar] [CrossRef] [Green Version]
- Murray, M.J.; Halsall, D.J.; Hook, C.E.; Williams, D.M.; Nicholson, J.C.; Coleman, N. Identification of microRNAs from the miR-371~373 and miR-302 clusters as potential serum biomarkers of malignant germ cell tumors. Am. J. Clin. Pathol. 2011, 135, 119–125. [Google Scholar] [CrossRef] [Green Version]
- Murray, M.J.; Scarpini, C.G.; Coleman, N. A Circulating MicroRNA Panel for Malignant Germ Cell Tumor Diagnosis and Monitoring. Methods Mol. Biol. 2021, 2195, 225–243. [Google Scholar]
- Radtke, A.; Hennig, F.; Ikogho, R.; Hammel, J.; Anheuser, P.; Wulfing, C.; Belge, G.; Dieckmann, K.P. The Novel Biomarker of Germ Cell Tumours, Micro-RNA-371a-3p, Has a Very Rapid Decay in Patients with Clinical Stage 1. Urol. Int. 2018, 100, 470–475. [Google Scholar] [CrossRef]
- Belge, G.; Dieckmann, K.P.; Spiekermann, M.; Balks, T.; Bullerdiek, J. Serum levels of microRNAs miR-371–3: A novel class of serum biomarkers for testicular germ cell tumors? Eur. Urol. 2012, 61, 1068–1069. [Google Scholar] [CrossRef] [PubMed]
- Gillis, A.J.; Rijlaarsdam, M.A.; Eini, R.; Dorssers, L.C.; Biermann, K.; Murray, M.J.; Nicholson, J.C.; Coleman, N.; Dieckmann, K.P.; Belge, G. Targeted serum miRNA (TSmiR) test for diagnosis and follow-up of (testicular) germ cell cancer patients: A proof of principle. Mol. Oncol. 2013, 7, 1083–1092. [Google Scholar] [CrossRef]
- Spiekermann, M.; Belge, G.; Winter, N.; Ikogho, R.; Balks, T.; Bullerdiek, J.; Dieckmann, K.P. MicroRNA miR-371a-3p in serum of patients with germ cell tumours: Evaluations for establishing a serum biomarker. Andrology 2015, 3, 78–84. [Google Scholar] [CrossRef]
- Syring, I.; Bartels, J.; Holdenrieder, S.; Kristiansen, G.; Muller, S.C.; Ellinger, J. Circulating serum miRNA (miR-367–3p, miR-371a-3p, miR-372–3p and miR-373–3p) as biomarkers in patients with testicular germ cell cancer. J. Urol. 2015, 193, 331–337. [Google Scholar] [CrossRef]
- Dieckmann, K.P.; Radtke, A.; Spiekermann, M.; Balks, T.; Matthies, C.; Becker, P.; Ruf, C.; Oing, C.; Oechsle, K.; Bokemeyer, C.; et al. Serum Levels of MicroRNA miR-371a-3p: A Sensitive and Specific New Biomarker for Germ Cell Tumours. Eur. Urol. 2017, 71, 213–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Agthoven, T.; Looijenga, L.H.J. Accurate primary germ cell cancer diagnosis using serum based microRNA detection (ampTSmiR test). Oncotarget 2017, 8, 58037–58049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belge, G.; Grobelny, F.; Radtke, A.; Bodes, J.; Matthies, C.; Wulfing, C.; Dieckmann, K.P. Serum levels of microRNA-371a-3p are not elevated in testicular tumours of non-germ cell origin. J. Cancer Res. Clin. Oncol. 2020, 147, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Anheuser, P.; Radtke, A.; Wulfing, C.; Kranz, J.; Belge, G.; Dieckmann, K.P. Serum Levels of MicroRNA371a-3p: A Highly Sensitive Tool for Diagnosing and Staging Testicular Germ Cell Tumours: A Clinical Case Series. Urol. Int. 2017, 99, 98–103. [Google Scholar] [CrossRef] [Green Version]
- Murray, M.J.; Coleman, N. Testicular cancer: A new generation of biomarkers for malignant germ cell tumours. Nat. Rev. Urol. 2012, 9, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, K.P.; Radtke, A.; Geczi, L.; Matthies, C.; Anheuser, P.; Eckardt, U.; Sommer, J.; Zengerling, F.; Trenti, E.; Pichler, R.; et al. Serum Levels of MicroRNA-371a-3p (M371 Test) as a New Biomarker of Testicular Germ Cell Tumors: Results of a Prospective Multicentric Study. J. Clin. Oncol. 2019, 37, 1412–1423. [Google Scholar] [CrossRef] [PubMed]
- Nappi, L.; Thi, M.; Lum, A.; Huntsman, D.; Eigl, B.J.; Martin, C.; O’Neil, B.; Maughan, B.L.; Chi, K.; So, A.; et al. Developing a Highly Specific Biomarker for Germ Cell Malignancies: Plasma miR371 Expression Across the Germ Cell Malignancy Spectrum. J. Clin. Oncol. 2019, 37, 3090–3098. [Google Scholar] [CrossRef] [PubMed]
- Badia, R.R.; Abe, D.; Wong, D.; Singla, N.; Savelyeva, A.; Chertack, N.; Woldu, S.L.; Lotan, Y.; Mauck, R.; Ouyang, D.; et al. Real-World Application of Pre-Orchiectomy miR-371a-3p Test in Testicular Germ Cell Tumor Management. J. Urol. 2021, 205, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Lembeck, A.L.; Puchas, P.; Hutterer, G.; Barth, D.A.; Terbuch, A.; Bauernhofer, T.; Pichler, M. MicroRNAs as Appropriate Discriminators in Non-Specific Alpha-Fetoprotein (AFP) Elevation in Testicular Germ Cell Tumor Patients. Noncoding RNA 2020, 6, 2. [Google Scholar] [CrossRef] [Green Version]
- Nappi, L.; Nichols, C. MicroRNAs as Biomarkers for Germ Cell Tumors. Urol. Clin. N. Am. 2019, 46, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Spiekermann, M.; Dieckmann, K.P.; Balks, T.; Bullerdiek, J.; Belge, G. Is relative quantification dispensable for the measurement of microRNAs as serum biomarkers in germ cell tumors? Anticancer Res. 2015, 35, 117–121. [Google Scholar]
- Myklebust, M.P.; Rosenlund, B.; Gjengsto, P.; Bercea, B.S.; Karlsdottir, A.; Brydoy, M.; Dahl, O. Quantitative PCR Measurement of miR-371a-3p and miR-372-p Is Influenced by Hemolysis. Front. Genet. 2019, 10, 463. [Google Scholar] [CrossRef] [PubMed]
- Morup, N.; Rajpert-De Meyts, E.; Juul, A.; Daugaard, G.; Almstrup, K. Evaluation of Circulating miRNA Biomarkers of Testicular Germ Cell Tumors during Therapy and Follow-up-A Copenhagen Experience. Cancers 2020, 12, 759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dieckmann, K.P.; Spiekermann, M.; Balks, T.; Ikogho, R.; Anheuser, P.; Wosniok, W.; Loening, T.; Bullerdiek, J.; Belge, G. MicroRNA miR-371a-3p—A Novel Serum Biomarker of Testicular Germ Cell Tumors: Evidence for Specificity from Measurements in Testicular Vein Blood and in Neoplastic Hydrocele Fluid. Urol. Int. 2016, 97, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.J.; Bell, E.; Raby, K.L.; Rijlaarsdam, M.A.; Gillis, A.J.; Looijenga, L.H.; Brown, H.; Destenaves, B.; Nicholson, J.C.; Coleman, N. A pipeline to quantify serum and cerebrospinal fluid microRNAs for diagnosis and detection of relapse in paediatric malignant germ-cell tumours. Br. J. Cancer 2016, 114, 151–162. [Google Scholar] [CrossRef] [Green Version]
- Murray, M.J.; Ajithkumar, T.; Harris, F.; Williams, R.M.; Jalloh, I.; Cross, J.; Ronghe, M.; Ward, D.; Scarpini, C.G.; Nicholson, J.C.; et al. Clinical utility of circulating miR-371a-3p for the management of patients with intracranial malignant germ cell tumors. Neurooncol. Adv. 2020, 2, vdaa048. [Google Scholar]
- Pelloni, M.; Coltrinari, G.; Paoli, D.; Pallotti, F.; Lombardo, F.; Lenzi, A.; Gandini, L. Differential expression of miRNAs in the seminal plasma and serum of testicular cancer patients. Endocrine 2017, 57, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Spiller, C.M.; Lobo, J.; Boellaard, W.P.A.; Gillis, A.J.M.; Bowles, J.; Looijenga, L.H.J. CRIPTO and miR-371a-3p Are Serum Biomarkers of Testicular Germ Cell Tumors and Are Detected in Seminal Plasma from Azoospermic Males. Cancers 2020, 12, 760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radtke, A.; Dieckmann, K.P.; Grobelny, F.; Salzbrunn, A.; Oing, C.; Schulze, W.; Belge, G. Expression of miRNA-371a-3p in seminal plasma and ejaculate is associated with sperm concentration. Andrology 2019, 7, 469–474. [Google Scholar] [CrossRef]
- Boellaard, W.P.A.; Gillis, A.J.M.; van Leenders, G.; Stoop, H.; van Agthoven, T.; Dorssers, L.C.J.; Dinkelman-Smit, M.; Boormans, J.L.; Looijenga, L.H.J. Cellular origin of microRNA-371a-3p in healthy males based on systematic urogenital tract tissue evaluation. Andrology 2019, 7, 463–468. [Google Scholar] [CrossRef] [Green Version]
- Flor, I.; Spiekermann, M.; Loning, T.; Dieckmann, K.P.; Belge, G.; Bullerdiek, J. Expression of microRNAs of C19MC in Different Histological Types of Testicular Germ Cell Tumour. Cancer Genom. Proteom. 2016, 13, 281–289. [Google Scholar]
- Murray, M.J.; Smith, S.; Ward, D.; Verduci, L.; Nicholson, J.C.; Scarpini, C.G.; Coleman, N. Circulating microRNAs as biomarkers to assist the management of the malignant germ-cell-tumour subtype choriocarcinoma. Transl. Oncol. 2020, 14, 100904. [Google Scholar] [CrossRef] [PubMed]
- Lobo, J.; Leão, R.; Gillis, A.J.M.; van den Berg, A.; Anson-Cartwright, L.; Atenafu, E.G.; Kuhathaas, K.; Chung, P.; Hansen, A.; Bedard, P.L.; et al. Utility of Serum miR-371a-3p in Predicting Relapse on Surveillance in Patients with Clinical Stage I Testicular Germ Cell Cancer. Eur. Urol. Oncol. 2020, in press. [Google Scholar] [CrossRef]
- Bagrodia, A.; Savelyeva, A.; Lafin, J.T.; Speir, R.W.; Chesnut, G.T.; Frazier, A.L.; Woldu, S.L.; Margulis, V.; Murray, M.J.; Amatruda, J.F.; et al. Impact of circulating microRNA test (miRNA-371a-3p) on appropriateness of treatment and cost outcomes in patients with Stage I non-seminomatous germ cell tumours. BJU Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Terbuch, A.; Adiprasito, J.B.; Stiegelbauer, V.; Seles, M.; Klec, C.; Pichler, G.P.; Resel, M.; Posch, F.; Lembeck, A.L.; Szkandera, J.; et al. MiR-371a-3p Serum Levels Are Increased in Recurrence of Testicular Germ Cell Tumor Patients. Int. J. Mol. Sci. 2018, 19, 3130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Agthoven, T.; Eijkenboom, W.M.H.; Looijenga, L.H.J. microRNA-371a-3p as informative biomarker for the follow-up of testicular germ cell cancer patients. Cell Oncol. 2017, 40, 379–388. [Google Scholar] [CrossRef]
- Rosas Plaza, X.; van Agthoven, T.; Meijer, C.; van Vugt, M.; de Jong, S.; Gietema, J.A.; Looijenga, L.H.J. miR-371a-3p, miR-373–3p and miR-367–3p as Serum Biomarkers in Metastatic Testicular Germ Cell Cancers Before, During and After Chemotherapy. Cells 2019, 8, 1221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mego, M.; van Agthoven, T.; Gronesova, P.; Chovanec, M.; Miskovska, V.; Mardiak, J.; Looijenga, L.H.J. Clinical utility of plasma miR-371a-3p in germ cell tumors. J. Cell Mol. Med. 2019, 23, 1128–1136. [Google Scholar] [CrossRef] [PubMed]
- Leão, R.; van Agthoven, T.; Figueiredo, A.; Jewett, M.A.S.; Fadaak, K.; Sweet, J.; Ahmad, A.E.; Anson-Cartwright, L.; Chung, P.; Hansen, A.; et al. Serum miRNA Predicts Viable Disease after Chemotherapy in Patients with Testicular Nonseminoma Germ Cell Tumor. J. Urol. 2018, 200, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Lafin, J.T.; Singla, N.; Woldu, S.L.; Lotan, Y.; Lewis, C.M.; Majmudar, K.; Savelyeva, A.; Kapur, P.; Margulis, V.; Strand, D.W.; et al. Serum MicroRNA-371a-3p Levels Predict Viable Germ Cell Tumor in Chemotherapy-naive Patients Undergoing Retroperitoneal Lymph Node Dissection. Eur. Urol. 2020, 77, 290–292. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, K.P.; Hennig, F.; Anheuser, P.; Gehrckens, R.; Viehweger, F.; Wulfing, C.; Belge, G. High Expression of microRNA-371a-3p in Cystic Fluid of Post-Chemotherapy Teratoma with Concurrent Normal Serum Levels in Patients with Non-Seminomatous Testicular Germ Cell Tumours. Urol. Int. 2020, 150, 21–26. [Google Scholar]
- Shen, H.; Shih, J.; Hollern, D.P.; Wang, L.; Bowlby, R.; Tickoo, S.K.; Thorsson, V.; Mungall, A.J.; Newton, Y.; Hedge, A.M.; et al. Integrated Molecular Characterization of Testicular Germ Cell Tumors. Cell Rep. 2018, 23, 3392–3406. [Google Scholar] [CrossRef]
- Belge, G.; Grobelny, F.; Matthies, C.; Radtke, A.; Dieckmann, K.P. Serum Level of microRNA-375–3p Is Not a Reliable Biomarker of Teratoma. In Vivo 2020, 34, 163–168. [Google Scholar] [CrossRef]
- Nappi, L.; Thi, M.; Adra, N.; Hamilton, R.J.; Leão, R.; Lavoie, J.M.; Soleimani, M.; Eigl, B.J.; Chi, K.; Gleave, M.; et al. Integrated Expression of Circulating miR375 and miR371 to Identify Teratoma and Active Germ Cell Malignancy Components in Malignant Germ Cell Tumors. Eur. Urol. 2021, 79, 16–19. [Google Scholar] [CrossRef]
- Singla, N.; Lafin, J.T.; Bagrodia, A. MicroRNAs: Turning the Tide in Testicular Cancer. Eur. Urol. 2019, 76, 541–542. [Google Scholar] [CrossRef]
- Regouc, M.; Belge, G.; Lorch, A.; Dieckmann, K.P.; Pichler, M. Non-Coding microRNAs as Novel Potential Tumor Markers in Testicular Cancer. Cancers 2020, 12, 749. [Google Scholar] [CrossRef] [Green Version]
- Costa, A.L.; Lobo, J.; Jeronimo, C.; Henrique, R. The epigenetics of testicular germ cell tumors: Looking for novel disease biomarkers. Epigenomics 2017, 9, 155–169. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, R.B.; Chabner, B.A. Application of Cell-free DNA Analysis to Cancer Treatment. N. Engl. J. Med. 2018, 379, 1754–1765. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwarzenbach, H.; Hoon, D.S.; Pantel, K. Cell-free nucleic acids as biomarkers in cancer patients. Nat. Rev. Cancer 2011, 11, 426–437. [Google Scholar] [CrossRef]
- Ellinger, J.; Wittkamp, V.; Albers, P.; Perabo, F.G.; Mueller, S.C.; von Ruecker, A.; Bastian, P.J. Cell-free circulating DNA: Diagnostic value in patients with testicular germ cell cancer. J. Urol. 2009, 181, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Kubala, E.; Bakardjieva-Mihaylova, V.; Skvarova-Kramarzova, K.; Slamova, M.; Triska, P.; Donatova, Z.; Rozsypalova, A.; Rosova, B.; Trka, J.; Buchler, T.; et al. The impact of circulating free tumor DNA (cfDNA) in testicular germ cell tumors (TGCT) management. J. Clin. Oncol. 2020, 38 (Suppl. 15), e17519. [Google Scholar] [CrossRef]
- Takayasu, T.; Shah, M.; Dono, A.; Yan, Y.; Borkar, R.; Putluri, N.; Zhu, J.J.; Hama, S.; Yamasaki, F.; Tahara, H.; et al. Cerebrospinal fluid ctDNA and metabolites are informative biomarkers for the evaluation of CNS germ cell tumors. Sci. Rep. 2020, 10, 14326. [Google Scholar] [CrossRef]
- Afrifa, J.; Zhao, T.; Yu, J. Circulating mitochondria DNA, a non-invasive cancer diagnostic biomarker candidate. Mitochondrion 2019, 47, 238–243. [Google Scholar] [CrossRef]
- Mehra, N.; Penning, M.; Maas, J.; van Daal, N.; Giles, R.H.; Voest, E.E. Circulating mitochondrial nucleic acids have prognostic value for survival in patients with advanced prostate cancer. Clin. Cancer Res. 2007, 13 Pt 1, 421–426. [Google Scholar] [CrossRef] [Green Version]
- Ellinger, J.; Albers, P.; Muller, S.C.; von Ruecker, A.; Bastian, P.J. Circulating mitochondrial DNA in the serum of patients with testicular germ cell cancer as a novel noninvasive diagnostic biomarker. BJU Int. 2009, 104, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Malpeli, G.; Innamorati, G.; Decimo, I.; Bencivenga, M.; Nwabo Kamdje, A.H.; Perris, R.; Bassi, C. Methylation Dynamics of RASSF1A and Its Impact on Cancer. Cancers 2019, 11, 959. [Google Scholar] [CrossRef] [Green Version]
- Costa, A.L.; Moreira-Barbosa, C.; Lobo, J.; Vilela-Salgueiro, B.; Cantante, M.; Guimarães, R.; Lopes, P.; Braga, I.; Oliveira, J.; Antunes, L.; et al. DNA methylation profiling as a tool for testicular germ cell tumors subtyping. Epigenomics 2018, 10, 1511–1523. [Google Scholar] [CrossRef] [PubMed]
- Lind, G.E.; Skotheim, R.I.; Fraga, M.F.; Abeler, V.M.; Esteller, M.; Lothe, R.A. Novel epigenetically deregulated genes in testicular cancer include homeobox genes and SCGB3A1 (HIN-1). J. Pathol. 2006, 210, 441–449. [Google Scholar] [CrossRef]
- Honorio, S.; Agathanggelou, A.; Wernert, N.; Rothe, M.; Maher, E.R.; Latif, F. Frequent epigenetic inactivation of the RASSF1A tumour suppressor gene in testicular tumours and distinct methylation profiles of seminoma and nonseminoma testicular germ cell tumours. Oncogene 2003, 22, 461–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koul, S.; McKiernan, J.M.; Narayan, G.; Houldsworth, J.; Bacik, J.; Dobrzynski, D.L.; Assaad, A.M.; Mansukhani, M.; Reuter, V.E.; Bosl, G.J.; et al. Role of promoter hypermethylation in Cisplatin treatment response of male germ cell tumors. Mol. Cancer 2004, 3, 16. [Google Scholar] [CrossRef] [Green Version]
- Ellinger, J.; Albers, P.; Perabo, F.G.; Muller, S.C.; von Ruecker, A.; Bastian, P.J. CpG island hypermethylation of cell-free circulating serum DNA in patients with testicular cancer. J. Urol. 2009, 182, 324–329. [Google Scholar] [CrossRef]
- El Messaoudi, S.; Rolet, F.; Mouliere, F.; Thierry, A.R. Circulating cell free DNA: Preanalytical considerations. Clin. Chim. Acta 2013, 424, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Lobo, J.; Nunes, S.P.; Gillis, A.J.M.; Barros-Silva, D.; Miranda-Goncalves, V.; Berg, A.V.D.; van den Berg, A.; Cantante, M.; Guimarães, R.; Henrique, R.; et al. XIST-Promoter Demethylation as Tissue Biomarker for Testicular Germ Cell Tumors and Spermatogenesis Quality. Cancers 2019, 11, 1385. [Google Scholar] [CrossRef] [Green Version]
- Looijenga, L.H.; Gillis, A.J.; van Gurp, R.J.; Verkerk, A.J.; Oosterhuis, J.W. X inactivation in human testicular tumors. XIST expression and androgen receptor methylation status. Am. J. Pathol. 1997, 151, 581–590. [Google Scholar]
- Kawakami, T.; Okamoto, K.; Sugihara, H.; Hattori, T.; Reeve, A.E.; Ogawa, O.; Okada, Y. The roles of supernumerical X chromosomes and XIST expression in testicular germ cell tumors. J. Urol. 2003, 169, 1546–1552. [Google Scholar] [CrossRef]
- Kawakami, T.; Okamoto, K.; Ogawa, O.; Okada, Y. XIST unmethylated DNA fragments in male-derived plasma as a tumour marker for testicular cancer. Lancet 2004, 363, 40–42. [Google Scholar] [CrossRef]
- Fan, Y.; Einhorn, L.; Saxman, S.; Katz, B.; Abonour, R.; Cornetta, K. Detection of germ cell tumor cells in apheresis products using polymerase chain reaction. Clin. Cancer Res. 1998, 4, 93–98. [Google Scholar]
- Hildebrandt, M.O.; Blaser, F.; Beyer, J.; Siegert, W.; Mapara, M.Y.; Huhn, D.; Salama, A. Detection of tumor cells in peripheral blood samples from patients with germ cell tumors using immunocytochemical and reverse transcriptase-polymerase chain reaction techniques. Bone Marrow Transplant. 1998, 22, 771–775. [Google Scholar] [CrossRef] [Green Version]
- Yuasa, T.; Yoshiki, T.; Tanaka, T.; Isono, T.; Okada, Y. Detection of circulating testicular cancer cells in peripheral blood. Cancer Lett. 1999, 143, 57–62. [Google Scholar] [CrossRef]
- Hautkappe, A.L.; Lu, M.; Mueller, H.; Bex, A.; Harstrick, A.; Roggendorf, M.; Ruebben, H. Detection of germ-cell tumor cells in the peripheral blood by nested reverse transcription-polymerase chain reaction for alpha-fetoprotein-messenger RNA and beta human chorionic gonadotropin-messenger RNA. Cancer Res. 2000, 60, 3170–3174. [Google Scholar]
- Bokemeyer, C.; Gillis, A.J.; Pompe, K.; Mayer, F.; Metzner, B.; Schleucher, N.; Schleicher, J.; Pflugrad-Jauch, G.; Oosterhuis, J.W.; Kanz, L.; et al. Clinical impact of germ cell tumor cells in apheresis products of patients receiving high-dose chemotherapy. J. Clin. Oncol. 2001, 19, 3029–3036. [Google Scholar] [CrossRef] [PubMed]
- Ruf, C.; Nastaly, P.; Becker, P.; Isbarn, H.; Honecker, F.; Pantel, K.; Riethdorf, S.; Hoeppner, D.; Fisch, M.; Wagner, W.; et al. Circulating Tumor Cells Can Be Detected in Patients with Testicular Germ Cell Tumors. J. Urol. 2013, 189, e289. [Google Scholar] [CrossRef]
- Nastaly, P.; Ruf, C.; Becker, P.; Bednarz-Knoll, N.; Stoupiec, M.; Kavsur, R.; Isbarn, H.; Matthies, C.; Wagner, W.; Hoppner, D.; et al. Circulating tumor cells in patients with testicular germ cell tumors. Clin. Cancer Res. 2014, 20, 3830–3841. [Google Scholar] [CrossRef] [Green Version]
- Cebotaru, C.L.; Buiga, R.; Placintar, A.N.; Ghilezan, N. P1.16 Detection of Circulating Tumor Cells Could Adjust Therapy in Poor Risk Germ Cell Tumors? A Pilot Study. Ann. Oncol. 2012, 23, v17. [Google Scholar] [CrossRef]
- Nastaly, P.; Honecker, F.; Pantel, K.; Riethdorf, S. Detection of Circulating Tumor Cells (CTCs) in Patients with Testicular Germ Cell Tumors. Methods Mol. Biol. 2021, 2195, 245–261. [Google Scholar] [PubMed]
- Keller, L.; Pantel, K. Unravelling tumour heterogeneity by single-cell profiling of circulating tumour cells. Nat. Rev. Cancer 2019, 19, 553–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cebotaru, C.L.; Olteanu, E.D.; Antone, N.Z.; Buiga, R.; Nagy, V. Circulating tumor cells in germ cell tumors: Are those biomarkers of real prognostic value? A review. Clujul Med. 2016, 89, 203–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, R.; Rai, A.; Chen, M.; Suwakulsiri, W.; Greening, D.W.; Simpson, R.J. Extracellular vesicles in cancer—Implications for future improvements in cancer care. Nat. Rev. Clin. Oncol. 2018, 15, 617–638. [Google Scholar] [CrossRef]
- Doyle, L.M.; Wang, M.Z. Overview of Extracellular Vesicles, Their Origin, Composition, Purpose, and Methods for Exosome Isolation and Analysis. Cells 2019, 8, 727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, M.J.; Coleman, N. MicroRNA Dysregulation in Malignant Germ Cell Tumors: More Than a Biomarker? J. Clin. Oncol. 2019, 37, 1432–1435. [Google Scholar] [CrossRef]
- Murray, M.J.; Saini, H.K.; Siegler, C.A.; Hanning, J.E.; Barker, E.M.; van Dongen, S.; Ward, D.M.; Raby, K.L.; Groves, I.J.; Scarpini, C.G.; et al. LIN28 Expression in malignant germ cell tumors downregulates let-7 and increases oncogene levels. Cancer Res. 2013, 73, 4872–4884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janssen, H.L.; Reesink, H.W.; Lawitz, E.J.; Zeuzem, S.; Rodriguez-Torres, M.; Patel, K.; van der Meer, A.J.; Patick, A.K.; Chen, A.; Zhou, Y.; et al. Treatment of HCV infection by targeting microRNA. N. Engl. J. Med. 2013, 368, 1685–1694. [Google Scholar] [CrossRef] [Green Version]
- Shah, M.Y.; Ferrajoli, A.; Sood, A.K.; Lopez-Berestein, G.; Calin, G.A. microRNA Therapeutics in Cancer—An Emerging Concept. EBioMedicine 2016, 12, 34–42. [Google Scholar] [CrossRef] [Green Version]
- Charytonowicz, D.; Aubrey, H.; Bell, C.; Ferret, M.; Tsui, K.; Atfield, R.; Coleman, N.; Murray, M.J.; Wilson, E.C.F. Cost Analysis of Noninvasive Blood-Based MicroRNA Testing Versus CT Scans for Follow-up in Patients with Testicular Germ-Cell Tumors. Clin. Genitourin. Cancer 2019, 17, e733–e744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cardoso, A.R.; Lobo, J.; Miranda-Goncalves, V.; Henrique, R.; Jeronimo, C. Epigenetic alterations as therapeutic targets in Testicular Germ Cell Tumours: Current and future application of ‘epidrugs’. Epigenetics 2020, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Oing, C.; Skowron, M.A.; Bokemeyer, C.; Nettersheim, D. Epigenetic treatment combinations to effectively target cisplatin-resistant germ cell tumors: Past, present, and future considerations. Andrology 2019, 7, 487–497. [Google Scholar] [CrossRef] [Green Version]
- Cheng, M.L.; Donoghue, M.T.A.; Audenet, F.; Wong, N.C.; Pietzak, E.J.; Bielski, C.M.; Isharwal, S.; Iyer, G.; Funt, S.; Bagrodia, A.; et al. Germ Cell Tumor Molecular Heterogeneity Revealed Through Analysis of Primary and Metastasis Pairs. JCO Precis. Oncol. 2020, 4, 1307–1320. [Google Scholar] [CrossRef]
- Barrett, M.T.; Lenkiewicz, E.; Malasi, S.; Stanton, M.; Slack, J.; Andrews, P.; Pagliaro, L.; Bryce, A.H. Clonal analyses of refractory testicular germ cell tumors. PLoS ONE 2019, 14, e0213815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Necchi, A.; Bratslavsky, G.; Corona, R.J.; Chung, J.H.; Millis, S.Z.; Elvin, J.A.; Vergilio, J.A.; Suh, J.; Ramkissoon, S.; Severson, E.; et al. Genomic Characterization of Testicular Germ Cell Tumors Relapsing After Chemotherapy. Eur. Urol. Focus 2020, 6, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Loveday, C.; Litchfield, K.; Proszek, P.Z.; Cornish, A.J.; Santo, F.; Levy, M.; Macintyre, G.; Holryod, A.; Broderick, P.; Dudakia, D.; et al. Genomic landscape of platinum resistant and sensitive testicular cancers. Nat. Commun. 2020, 11, 2189. [Google Scholar] [CrossRef]
- Fazal, Z.; Singh, R.; Fang, F.; Bikorimana, E.; Baldwin, H.; Corbet, A.; Tomlin, M.; Yerby, C.; Adra, N.; Albany, C.; et al. Hypermethylation and global remodelling of DNA methylation is associated with acquired cisplatin resistance in testicular germ cell tumours. Epigenetics 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Fazal, Z.; Corbet, A.K.; Bikorimana, E.; Rodriguez, J.C.; Khan, E.M.; Shahid, K.; Freemantle, S.J.; Spinella, M.J. Epigenetic Remodeling through Downregulation of Polycomb Repressive Complex 2 Mediates Chemotherapy Resistance in Testicular Germ Cell Tumors. Cancers 2019, 11, 796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albany, C.; Fazal, Z.; Singh, R.; Bikorimana, E.; Adra, N.; Hanna, N.H.; Einhorn, L.H.; Perkins, S.M.; Sandusky, G.E.; Christensen, B.C.; et al. A phase 1 study of combined guadecitabine and cisplatin in platinum refractory germ cell cancer. Cancer Med. 2020, 10, 156–163. [Google Scholar] [CrossRef]
- Kalavska, K.; Schmidtova, S.; Chovanec, M.; Mego, M. Immunotherapy in Testicular Germ Cell Tumors. Front. Oncol. 2020, 10, 573977. [Google Scholar] [CrossRef] [PubMed]
- Milardi, D.; Grande, G.; Vincenzoni, F.; Pierconti, F.; Pontecorvi, A. Proteomics for the Identification of Biomarkers in Testicular Cancer-Review. Front. Endocrinol. 2019, 10, 462. [Google Scholar] [CrossRef] [Green Version]
- Zimmermann, U.; Junker, H.; Kramer, F.; Balabanov, S.; Kleist, B.; Kammer, W.; Nordheim, A.; Walther, R. Comparative proteomic analysis of neoplastic and non-neoplastic germ cell tissue. Biol. Chem. 2006, 387, 437–440. [Google Scholar] [CrossRef] [PubMed]
- Leman, E.S.; Magheli, A.; Yong, K.M.; Netto, G.; Hinz, S.; Getzenberg, R.H. Identification of nuclear structural protein alterations associated with seminomas. J. Cell. Biochem. 2009, 108, 1274–1279. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Hu, Z.; Qi, L.; Wang, J.; Zhou, T.; Guo, Y.; Zeng, Y.; Zheng, B.; Wu, Y.; Zhang, P.; et al. Scanning of novel cancer/testis proteins by human testis proteomic analysis. Proteomics 2013, 13, 1200–1210. [Google Scholar] [CrossRef]
- Castillo, J.; Knol, J.C.; Korver, C.M.; Piersma, S.R.; Pham, T.V.; de Goeij-de Haas, R.R.; van Pelt, A.M.M.; Jimenez, C.R.; Jansen, B.J.H. Human Testis Phosphoproteome Reveals Kinases as Potential Targets in Spermatogenesis and Testicular Cancer. Mol. Cell. Proteom. 2019, 18 (Suppl. 1), S132–S144. [Google Scholar] [CrossRef] [PubMed]
- Bremmer, F.; Bohnenberger, H.; Kuffer, S.; Oellerich, T.; Serve, H.; Urlaub, H.; Strauss, A.; Maatoug, Y.; Behnes, C.L.; Oing, O.; et al. Proteomic Comparison of Malignant Human Germ Cell Tumor Cell Lines. Dis. Markers 2019, 2019, 8298524. [Google Scholar] [CrossRef] [PubMed]
- Strenziok, R.; Hinz, S.; Wolf, C.; Conrad, T.; Krause, H.; Miller, K.; Schrader, M. Surface-enhanced laser desorption/ionization time-of-flight mass spectrometry: Serum protein profiling in seminoma patients. World J. Urol. 2010, 28, 193–197. [Google Scholar] [CrossRef]
- Milardi, D.; Grande, G.; Vincenzoni, F.; Castagnola, M.; Marana, R. Proteomics of human seminal plasma: Identification of biomarker candidates for fertility and infertility and the evolution of technology. Mol. Reprod. Dev. 2013, 80, 350–357. [Google Scholar] [CrossRef]
- Panner Selvam, M.K.; Alves, M.G.; Dias, T.R.; Pushparaj, P.N.; Agarwal, A. Distinct Proteomic Profile of Spermatozoa from Men with Seminomatous and Non-Seminomatous Testicular Germ Cell Tumors. Int. J. Mol. Sci. 2020, 21, 4817. [Google Scholar] [CrossRef]
- Litchfield, K.; Mitchell, J.S.; Shipley, J.; Huddart, R.; Rajpert-De Meyts, E.; Skakkebaek, N.E.; Houlston, R.S.; Turnbull, C. Polygenic susceptibility to testicular cancer: Implications for personalised health care. Br. J. Cancer 2015, 113, 1512–1518. [Google Scholar] [CrossRef] [Green Version]
- Loveday, C.; Law, P.; Litchfield, K.; Levy, M.; Holroyd, A.; Broderick, P.; Kote-Jarai, Z.; Dunning, A.M.; Muir, K.; Peto, J.; et al. Large-scale Analysis Demonstrates Familial Testicular Cancer to have Polygenic Aetiology. Eur. Urol. 2018, 74, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Litchfield, K.; Loveday, C.; Levy, M.; Dudakia, D.; Rapley, E.; Nsengimana, J.; Bishop, D.T.; Reid, A.; Huddart, R.; Broderick, P.; et al. Large-scale Sequencing of Testicular Germ Cell Tumour (TGCT) Cases Excludes Major TGCT Predisposition Gene. Eur. Urol. 2018, 73, 828–831. [Google Scholar] [CrossRef]
- Looijenga, L.H.J.; Kao, C.S.; Idrees, M.T. Predicting Gonadal Germ Cell Cancer in People with Disorders of Sex Development; Insights from Developmental Biology. Int. J. Mol. Sci. 2019, 20, 5017. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Positivity in Histological Types | AFP | HCG | LDH |
|---|---|---|---|
| GCNIS | - | - | - |
| Seminoma | <3% | 18–31% | 29% |
| Non-seminoma | 60–70% | 53% | 39% |
| Embryonal carcinoma | 40% | 25% | 20% |
| Yolk sac tumor | >95% | <5% | 10% |
| Choriocarcinoma | <5% | >95% | 20% |
| Teratoma | 20-25% | 10% | <5% |
| Staging—S stage | AFP (µg/L) | HCG (IU/L) | LDH (U/L) |
| S0 | <ULN | <ULN | <ULN |
| S1 | <1000 | <5000 | <1.5× ULN |
| S2 | 1000–10,000 | 5000–50,000 | 1.5–10× ULN |
| S3 | >10,000 | >50,000 | >10× ULN |
| Prognosis—IGCCCG | Seminoma | Non-seminoma | |
| Good | Any location Normal AFP Any HCG or LDH Absence of non-pulmonary visceral metastases | Testicular or retroperitoneal Absence of non-pulmonary visceral metastases AFP < 1000 HCG < 5000 LDH < 1.5× ULN | |
| Intermediate | Any location Normal AFP Any HCG or LDH Presence of non-pulmonary visceral metastases | Testicular or retroperitoneal Absence of non-pulmonary visceral metastases AFP 1000–10,000 HCG 5000–50,000 LDH 1.5×–10× ULN | |
| Poor | - | All mediastinal tumors; testicular or retroperitoneal with any of the features below: Presence of non-pulmonary visceral metastases AFP > 10,000 HCG > 50,000 LDH > 10× ULN | |
| Diagnostic Performance | |||||
|---|---|---|---|---|---|
| Parameter | AFP | HCG | miR-371a-3p | miR-373-3p | miR-367-3p |
| Positive Predictive Value (%) | 32 | 42 | 97 | 94 | 92 |
| Negative Predictive Value (%) | 78 | 76 | 83 | 58 | 63 |
| AUC (%) | 57 | 69 | 97 | 77 | 86 |
| Focus on Diagnosis | |||
|---|---|---|---|
| Study | Population | Performance | Reference |
| Gillis et al., 2013 | 80 GCT 47 controls 12 non-GCT | Sensitivity: 98% Specificity: 48.3% | [82] |
| Syring et al., 2015 | Discovery cohort: 30 TGCT and 18 controls Validation cohort: 59 TGCT, 17 non-GCT and 84 controls | Sensitivity: 84.7% Specificity: 99.0% | [84] |
| van Agthoven et al., 2017 | 250 GCT 104 controls 60 non-GCT | Sensitivity: 90.0% Specificity: 86.0% | [86] |
| Dieckmann et al., 2017 | 106 TGCT 106 controls | Sensitivity: 88.7% Specificity: 93.4% | [85] |
| Dieckmann et al., 2019 | 616 TGCT 258 controls | Sensitivity: 90.1% Specificity: 94.0% | [90] |
| Badia et al., 2021 | 58 TGCT 11 controls | Sensitivity: 93.0% Specificity: 100% | [92] |
| Focus on Follow-up | |||
| Study | Findings | Reference | |
| van Agthoven et al., 2017 | Identification of disease relapse, outperforming classical markers | [110] | |
| Terbuch et al., 2018 | Confirmation of power to identify patients with refractory disease | [109] | |
| Rosas Plaza et al., 2019 | Confirmation of power to identify patients with refractory disease | [111] | |
| Mego et al., 2019 | miR-371a-3p levels at start of chemotherapy are of prognostic value; association with progression-free survival | [112] | |
| Nappi et al., 2019 | Identification of active germ cell malignancy in 111 patients with history of GCT (Sensitivity: 96.0%, Specificity: 100%) | [91] | |
| Morup et al., 2020 | MicroRNAs related to patient trajectories; comparison of distinct methodologies for isolating and quantifying microRNAs | [97] | |
| Bagrodia et al., 2020 | miR-371a-3p aids in adjusting treatment, in a cost-effective way | [108] | |
| Lobo et al., 2021 | Immediate post-orchiectomy miR-371a-3p levels do not predict relapse of stage I patients put on surveillance, but outperform classical markers during follow-up for identifying relapse | [107] | |
| Focus on Identification of Metastatic Viable Disease/Teratoma | |||
| Study | Findings | Reference | |
| Leão et al., 2018 | miR-371a-3p predicts viable disease after chemotherapy (AUC = 0.874) | [113] | |
| Lobo et al., 2019 | miR-371a-3p confirmed to detect viable disease after chemotherapy | [67] | |
| Lafin et al., 2019 | miR-371a-3p predicts viable disease in chemo-naïve context | [114] | |
| Nappi et al., 2020 | Combination of miR-371a-3p and miR-375 improves discrimination of teratoma from viable disease | [118] | |
| Others | |||
| Study | Findings | Reference | |
| Spiekermann et al., 2015 | Detection in seminal plasma, pleural effusion, no detection in urine | [83] | |
| Dieckmann et al., 2016 | Detection in testicular vein blood and hydrocele fluid | [98] | |
| Murray et al., 2016 | Detection in cerebral spinal fluid of pediatric patients with GCT | [99] | |
| Anheuser et al., 2017 | miR-371a-3p levels would have resulted in change of clinical approach to five seminoma patients | [88] | |
| Pelloni et al., 2017 | Detection in seminal plasma | [101] | |
| Radtke et al., 2017 | Detection of GCNIS in serum | [75] | |
| Radtke et al., 2018 | miR-371a-3p has a very short half-life (<12 h) | [80] | |
| Radtke et al., 2019 | Detection in seminal plasma, but not different from controls | [103] | |
| Boellaard et al., 2019 | Reinforcement of origin of miR-371a-3p from the germ cell compartment | [104] | |
| Spiller and Lobo et al., 2020 | Detection in seminal plasma; positive correlation with CRIPTO | [102] | |
| Dieckmann et al., 2020 | Detection in cystic fluid of post-chemotherapy teratoma, possibly originating from active germ cell tumor before therapy | [115] | |
| Murray et al., 2020 | Detection in cerebral spinal fluid; utility for detection of intracranial GCT | [100] | |
| Belge et al., 2020 | miR-371a-3p is not elevated in non-GCT (n = 99) | [87] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lobo, J.; Leão, R.; Jerónimo, C.; Henrique, R. Liquid Biopsies in the Clinical Management of Germ Cell Tumor Patients: State-of-the-Art and Future Directions. Int. J. Mol. Sci. 2021, 22, 2654. https://doi.org/10.3390/ijms22052654
Lobo J, Leão R, Jerónimo C, Henrique R. Liquid Biopsies in the Clinical Management of Germ Cell Tumor Patients: State-of-the-Art and Future Directions. International Journal of Molecular Sciences. 2021; 22(5):2654. https://doi.org/10.3390/ijms22052654
Chicago/Turabian StyleLobo, João, Ricardo Leão, Carmen Jerónimo, and Rui Henrique. 2021. "Liquid Biopsies in the Clinical Management of Germ Cell Tumor Patients: State-of-the-Art and Future Directions" International Journal of Molecular Sciences 22, no. 5: 2654. https://doi.org/10.3390/ijms22052654









