Muscarinic Acetylcholine Receptors in the Retina—Therapeutic Implications
Abstract
:1. Introduction
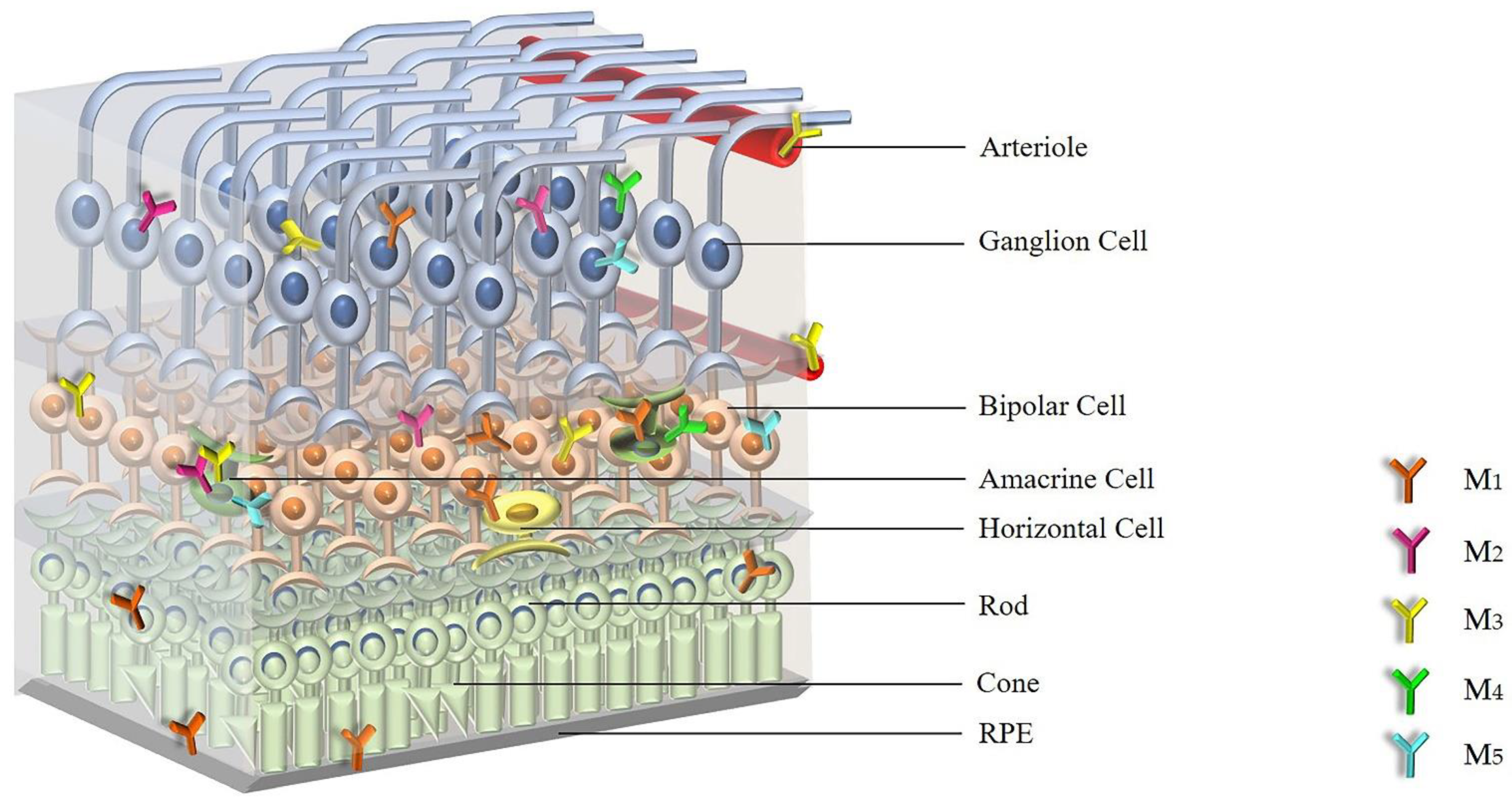
2. Expression and Distribution of mAChRs in the Retina
3. Cellular Signaling of mAChRs
4. Functional Roles of Individual mAChR Subtypes in the Retina
5. Strategies to Target Individual mAChR Subtypes
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dale, H.H. The Action of Certain Esters and Ethers of Choline, and Their Relation to Muscarine. J. Pharmacol. Exp. Ther. 1914, 6, 147. [Google Scholar]
- McCorry, L.K. Physiology of the Autonomic Nervous System. Am. J. Pharm Educ. 2007, 71, 78. [Google Scholar] [CrossRef] [Green Version]
- Caulfield, M.P.; Birdsall, N.J.M. International Union of Pharmacology. XVII. Classification of Muscarinic Acetylcholine Receptors. Pharmacol. Rev. 1998, 50, 279. [Google Scholar] [PubMed]
- Wessler, I.; Kirkpatrick, C.J. Acetylcholine Beyond Neurons: The Non-neuronal Cholinergic System in Humans. Br. J. Pharmacol. 2008, 154, 1558–1571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Li, J. Expression and Function of Muscarinic Receptor Subtypes on Human Cornea and Conjunctiva. Investig. Ophthalmol. Vis. Sci. 2007, 48, 2987–2996. [Google Scholar] [CrossRef]
- Ríos, J.D.; Forde, K. Development of Conjunctival Goblet Cells and Their Neuroreceptor Subtype Expression. Investig. Ophthalmol. Vis. Sci. 2000, 41, 2127–2137. [Google Scholar]
- Liu, Q.; Wu, J. Changes in Muscarinic Acetylcholine Receptor Expression in Form Deprivation Myopia in Guinea Pigs. Mol. Vis. 2007, 13, 1234–1244. [Google Scholar]
- Mitchelson, F. Muscarinic Receptor Agonists and Antagonists: Effects on Ocular Function. In Muscarinic Receptors; Fryer, A.D., Christopoulos, A., Eds.; Springer: Berlin/Heidelberg, Germany, 2012; pp. 263–298. [Google Scholar]
- Sloniecka, M. Neuropeptides and Neurotransmitters in Keratocytes: Importance in Corneal Wound Healing Processes. Ph.D. Thesis, Comprehensive Summary, Umeå University, Umeå, Sweden, 2015. [Google Scholar]
- Smith, E.L., III; Redburn, D.A. Permanent Alterations in Muscarinic Receptors and Pupil Size Produced by Chronic Atropinization in Kittens. Investig. Ophthalmol. Vis. Sci. 1984, 25, 239–243. [Google Scholar]
- McBrien, N.A.; Jobling, A.I. Expression of Muscarinic Receptor Subtypes in Tree Shrew Ocular Tissues and Their Regulation during the Development of Myopia. Mol. Vis. 2009, 15, 464–475. [Google Scholar] [PubMed]
- Ríos, J.D.; Zoukhri, D. Immunolocalization of Muscarinic and Vip Receptor Subtypes and Their Role in Stimulating Goblet Cell Secretion. Investig. Ophthalmol. Vis. Sci 1999, 40, 1102–1111. [Google Scholar]
- Duncan, G.; Collison, D.J. Role of the Non-neuronal Cholinergic System in the Eye: A Review. Life Sci. 2003, 72, 2013–2019. [Google Scholar] [CrossRef]
- Lin, H.-J.; Wan, L. Muscarinic Acetylcholine Receptor 3 is Dominant in Myopia Progression. Investig. Ophthalmol. Vis. Sci. 2012, 53, 6519–6525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almasieh, M.; Zhou, Y. Structural and Functional Neuroprotection in Glaucoma: Role of Galantamine-mediated Activation of Muscarinic Acetylcholine Receptors. Cell Death Dis. 2010, 1, e27. [Google Scholar] [CrossRef] [Green Version]
- Weinreb, R.N.; Aung, T. The Pathophysiology and Treatment of Glaucoma: A Review. JAMA 2014, 311, 1901–1911. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quigley, H.A.; Broman, A.T. The Number of People with Glaucoma Worldwide in 2010 and 2020. Br. J. Ophthalmol. 2006, 90, 262–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tham, Y.-C.; Li, X. Global Prevalence of Glaucoma and Projections of Glaucoma Burden Through 2040: A Systematic Review and Meta-analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef]
- Quigley, H.A.; Addicks, E.M. Optic Nerve Damage in Human Glaucoma. II. The Site of Injury and Susceptibility to Damage. Arch. Ophthalmol. 1981, 99, 635–649. [Google Scholar] [CrossRef] [PubMed]
- Weinreb, R.N.; Khaw, P.T. Primary Open-angle Glaucoma. Lancet 2004, 363, 1711–1720. [Google Scholar] [CrossRef]
- Heijl, A.; Leske, M.C. Reduction of Intraocular Pressure and Glaucoma Progression: Results from the Early Manifest Glaucoma trial. Arch. Ophthalmol. 2002, 120, 1268–1279. [Google Scholar] [CrossRef]
- Nucci, C.; Martucci, A. Neuroprotective Agents in the Management of Glaucoma. Eye 2018, 32, 938–945. [Google Scholar] [CrossRef]
- Grossniklaus, H.E.; Green, W.R. Pathologic Findings in Pathologic Myopia. Retina 1992, 12, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Morgan, I.; Rose, K. How Genetic is School Myopia? Prog. Retin. Eye Res. 2005, 24, 1–38. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A.; Fricke, T.R. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 Through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schultz, G.; Rosenthal, W. Role of G Proteins in Calcium Channel Modulation. Annu. Rev. Physiol. 1990, 52, 275–292. [Google Scholar] [CrossRef]
- Simon, M.I.; Strathmann, M.P. Diversity of G Proteins in Signal Transduction. Science 1991, 252, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, F. Acetylcholine Receptor. Br. J. Anaesth. 1982, 54, 115–130. [Google Scholar] [CrossRef] [Green Version]
- Kostenis, E.; Zeng, F.-Y. Structure-function Analysis of Muscarinic Receptors and Their Associated G Proteins. Life Sci. 1999, 64, 355–362. [Google Scholar] [CrossRef]
- Laspas, P.; Zhutdieva, M.B. The M(1) Muscarinic Acetylcholine Receptor Subtype is Important for Retinal Neuron Survival in Aging Mice. Sci. Rep. 2019, 9, 5222. [Google Scholar] [CrossRef]
- Yu, P.; Dong, W.-P. Huperzine a Lowers Intraocular Pressure via the M3 mAChR and Provides Retinal Neuroprotection via the M1 mAChR: A Promising Agent for the Treatment of Glaucoma. Ann. Transl. Med. 2021, 9, 332. [Google Scholar] [CrossRef]
- Broadley, K.J.; Kelly, D.R. Muscarinic Receptor Agonists and Antagonists. Molecules 2001, 6, 142–193. [Google Scholar] [CrossRef] [Green Version]
- Barathi, V.A.; Beuerman, R.W. Molecular Mechanisms of Muscarinic Receptors in Mouse Scleral Fibroblasts: Prior to and after Induction of Experimental Myopia with Atropine Treatment. Mol. Vis. 2011, 17, 680–692. [Google Scholar] [PubMed]
- Marquis, R.E.; Whitson, J.T. Management of Glaucoma: Focus on Pharmacological Therapy. Drugs Aging 2005, 22, 1–21. [Google Scholar] [CrossRef]
- Lusthaus, J.; Goldberg, I. Current Management of Glaucoma. Med. J. Aust. 2019, 210, 180–187. [Google Scholar] [CrossRef] [PubMed]
- McBrien, N.A.; Stell, W.K. How does Atropine Exert Its Anti-myopia Effects? Ophthalmic Physiol. Opt. 2013, 33, 373–378. [Google Scholar] [CrossRef]
- Hutchins, J.B. Review: Acetylcholine as a Neurotransmitter in the Vertebrate Retina. Exp. Eye Res. 1987, 45, 1–38. [Google Scholar] [CrossRef]
- Hruska, R.E.; White, R. Muscarinic Cholinergic Receptors in Mammalian Retina. Brain Res. 1978, 148, 493–498. [Google Scholar] [CrossRef]
- Atterwill, C.K.; Mahoney, A. The Uptake and Subcellular Distribution of 3-h-choline by the Retina. Br. J. Pharmacol. 1975, 53, 447P. [Google Scholar]
- Sugiyama, H.; Daniels, M.P. Muscarinic Acetylcholine Receptors of the Developing Retina. Proc. Natl. Acad. Sci. USA 1977, 74, 5524–5528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polans, A.S.; Hutchins, J.B. Muscarinic Cholinergic Receptors in the Retina of the Larval Tiger Salamander. Brain Res. 1985, 340, 355–362. [Google Scholar] [CrossRef]
- Hutchins, J.B.; Hollyfield, J.G. Acetylcholine Receptors in the Human Retina. Investig. Ophthalmol. Vis. Sci. 1985, 26, 1550–1557. [Google Scholar]
- Cho, N.J.; Klein, W.L. Muscarinic Acetylcholine Receptors from Avian Retina and Heart Undergo Different Patterns of Molecular Maturation. J. Neurochem. 1988, 50, 1403–1411. [Google Scholar] [CrossRef]
- Hutchins, J.B. Development of Muscarinic Acetylcholine Receptors in the Ferret Retina. Dev. Brain Res. 1994, 82, 45–61. [Google Scholar] [CrossRef]
- Townes-Anderson, E.; Vogt, B.A. Distribution of Muscarinic Acetylcholine Receptors on Processes of Isolated Retinal Cells. J. Comp. Neurol. 1989, 290, 369–383. [Google Scholar] [CrossRef] [PubMed]
- Moroi-Fetters, S.E.; Neff, N.H. Muscarinic Receptor-mediated Phosphoinositide Hydrolysis in the Rat Retina. J. Pharmacol. Exp. Ther. 1988, 246, 553. [Google Scholar] [PubMed]
- Bonner, T.I. New Subtypes of Muscarinic Acetylcholine Receptors. Trends Pharmacol. Sci. 1989, (Suppl.), 11–15. [Google Scholar] [PubMed]
- Wall, S.J.; Yasuda, R.P. The Ontogeny of M1–M5 Muscarinic Receptor Subtypes in Rat Forebrain. Dev. Brain Res. 1992, 66, 181–185. [Google Scholar] [CrossRef]
- Bonner, T.I. The Molecular Basis of Muscarinic Receptor Diversity. Trends Neurosci. 1989, 12, 148–151. [Google Scholar] [CrossRef]
- McKinnon, L.A.; Rosoff, M. Regulation of Muscarinic Receptor Expression and Function in Cultured Cells and in Knock-out Mice. Life Sci. 1997, 60, 1101–1104. [Google Scholar] [CrossRef]
- Fischer, A.J.; McKinnon, L.A. Identification and Localization of Muscarinic Acetylcholine Receptors in the Ocular Tissues of the Chick. J. Comp. Neurol. 1998, 392, 273–284. [Google Scholar] [CrossRef]
- Belmonte, K.E.; McKinnon, L.A. Developmental Expression of Muscarinic Acetylcholine Receptors in Chick Retina: Selective Induction of M2 Muscarinic Receptor Expression in ovo by a Factor Secreted by Muller Glial Cells. J. Neurosci. 2000, 20, 8417–8425. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.H.; Yan, D.S. Expression of Muscarinic Acetylcholine Receptor-1 in Human Retinal Pigment Epithelium. Zhonghua Yan Ke Za Zhi Chin. J. Ophthalmol. 2006, 42, 1109–1112. [Google Scholar]
- Tao, Y.; Li, X.-L. Effect of Green Flickering Light on Myopia Development and Expression of M1 Muscarinic Acetylcholine Receptor in Guinea Pigs. Int. J. Ophthalmol. 2018, 11, 1755–1760. [Google Scholar] [PubMed]
- Strang, C.E.; Renna, J.M. Muscarinic Acetylcholine Receptor Localization and Activation Effects on Ganglion Response Properties. Investig. Ophthalmol. Vis. Sci. 2010, 51, 2778–2789. [Google Scholar] [CrossRef]
- Gericke, A.; Sniatecki, J.J. Identification of the Muscarinic Acetylcholine Receptor Subtype Mediating Cholinergic Vasodilation in Murine Retinal Arterioles. Investig. Ophthalmol. Vis. Sci. 2011, 52, 7479–7484. [Google Scholar] [CrossRef]
- Gericke, A.; Mayer, V.G.A. Cholinergic Responses of Ophthalmic Arteries in M3 and M5 Muscarinic Acetylcholine Receptor Knockout Mice. Investig. Ophthalmol. Vis. Sci. 2009, 50, 4822–4827. [Google Scholar] [CrossRef] [PubMed]
- Peralta, E.G.; Ashkenazi, A. Distinct Primary Structures, Ligand-binding Properties and Tissue-specific Expression of Four Human Muscarinic Acetylcholine Receptors. EMBO J. 1987, 6, 3923–3929. [Google Scholar] [CrossRef] [PubMed]
- Bonner, T.I.; Young, A.C. Cloning and Expression of the Human and Rat M5 Muscarinic Acetylcholine Receptor Genes. Neuron 1988, 1, 403–410. [Google Scholar] [CrossRef]
- van Koppen, C.J.; Kaiser, B. Regulation of Muscarinic Acetylcholine Receptor Signaling. Pharmacol. Ther. 2003, 98, 197–220. [Google Scholar] [CrossRef]
- Rümenapp, U.; Asmus, M. The M3 Muscarinic Acetylcholine Receptor Expressed in HEK-293 Cells Signals to Phospholipase D via G12 but not Gq-type G Proteins: Regulators of G Proteins as Tools to Dissect Pertussis Toxin-resistant G Proteins in Receptor-Effector Coupling. J. Biol. Chem. 2001, 276, 2474–2479. [Google Scholar] [CrossRef] [Green Version]
- Mathes, C.; Thompson, S.H. The Nitric Oxide/Cgmp Pathway Couples Muscarinic Receptors to the Activation of Ca2+ Influx. J. Neurosci. 1996, 16, 1702–1709. [Google Scholar] [CrossRef]
- Haga, T. Molecular Properties of Muscarinic Acetylcholine Receptors. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2013, 89, 226–256. [Google Scholar] [CrossRef] [Green Version]
- Goin, J.C.; Nathanson, N.M. Subtype-specific Regulation of the Expression and Function of Muscarinic Acetylcholine Receptors in Embryonic Chicken Retinal Cells. J. Neurochem. 2002, 83, 964–972. [Google Scholar] [CrossRef] [Green Version]
- Jardon, B.; Bonaventure, N. Possible Involvement of Cholinergic and Glycinergic Amacrine Cells in the Inhibition Exerted by the on Retinal Channel on the Off Retinal Channel. Eur. J. Pharmacol. 1992, 210, 201–207. [Google Scholar] [CrossRef]
- Dowling, J.E. The Retina: An Approachable Part of the Brain; Harvard University Press: London, UK, 1987. [Google Scholar]
- Niemeyer, G.; Jurklies, B. Binding and Electrophysiology of the Muscarinic Antagonist QNB in the Mammalian Retina. Klin. Mon. Augenheilkd. 1995, 206, 380–383. [Google Scholar] [CrossRef] [PubMed]
- Jositsch, G.; Papadakis, T. Suitability of Muscarinic Acetylcholine Receptor Antibodies for Immunohistochemistry Evaluated on Tissue Sections of Receptor Gene-deficient Mice. Naunyn Schmiedebergs Arch. Pharmacol. 2009, 379, 389–395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamilton, S.E.; Loose, M.D. Disruption of the M1 Receptor Gene Ablates Muscarinic Receptor-dependent M Current Regulation and Seizure Activity in Mice. Proc. Natl. Acad. Sci. USA 1997, 94, 13311. [Google Scholar] [CrossRef] [Green Version]
- Gomeza, J.; Shannon, H. Pronounced Pharmacologic Deficits in M2 Muscarinic Acetylcholine Receptor Knockout Mice. Proc. Natl. Acad. Sci. USA 1999, 96, 1692–1697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsui, M.; Motomura, D. Multiple Functional Defects in Peripheral Autonomic Organs in Mice Lacking Muscarinic Acetylcholine Receptor Gene for the M3 Subtype. Proc. Natl. Acad. Sci. USA 2000, 97, 9579. [Google Scholar] [CrossRef] [Green Version]
- Gomeza, J.; Zhang, L. Enhancement of d1 Dopamine Receptor-mediated Locomotor Stimulation in M4 Muscarinic Acetylcholine Receptor Knockout Mice. Proc. Natl. Acad. Sci. USA 1999, 96, 10483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woolley, M.L.; Carter, H.J. Attenuation of Amphetamine-induced Activity by the Non-selective Muscarinic Receptor Agonist, Xanomeline, is Absent in Muscarinic M4 Receptor Knockout Mice and Attenuated in Muscarinic M1 Receptor Knockout Mice. Eur. J. Pharmacol. 2009, 603, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Lamping, K.G. Cholinergic Dilation of Cerebral Blood Vessels is Abolished in M(5) Muscarinic Acetylcholine Receptor Knockout Mice. Proc. Natl. Acad. Sci. USA 2001, 98, 14096. [Google Scholar] [CrossRef] [Green Version]
- Steidl, S.; Yeomans, J.S. M5 Muscarinic Receptor Knockout Mice Show Reduced Morphine-induced Locomotion but Increased Locomotion after Cholinergic Antagonism in the Ventral Tegmental Area. J. Pharmacol. Exp. Ther. 2009, 328, 263. [Google Scholar] [CrossRef]
- Barathi, V.A.; Kwan, J.L. Muscarinic Cholinergic Receptor (M2) Plays a Crucial Role in the Development of Myopia in Mice. Dis. Model. Mech. 2013, 6, 1146–1158. [Google Scholar] [CrossRef] [Green Version]
- Gericke, A.; Steege, A. Role of the M3 Muscarinic Acetylcholine Receptor Subtype in Murine Ophthalmic Arteries after Endothelial Removal. Investig. Ophthalmol. Vis. Sci. 2014, 55, 625–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laspas, P.; Sniatecki, J.J. Effect of the M1 Muscarinic Acetylcholine Receptor on Retinal Neuron Number Studied with Gene-Targeted Mice. J. Mol. Neurosci. 2015, 56, 472–479. [Google Scholar] [CrossRef]
- Lanzafame, A.A.; Christopoulos, A. Cellular Signaling Mechanisms for Muscarinic Acetylcholine Receptors. Recept. Channels 2003, 9, 241–260. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.A.; Abogadie, F.C. Muscarinic Mechanisms in Nerve Cells. Life Sci. 1997, 60, 1137–1144. [Google Scholar] [CrossRef]
- Brown, D.A.; Selyanko, A.A. Membrane Currents Underlying the Cholinergic Slow Excitatory Post-synaptic Potential in the Rat Sympathetic Ganglion. J. Physiol. 1985, 365, 365–387. [Google Scholar] [CrossRef]
- Wess, J.; Liu, J. Structural Basis of Receptor/G Protein Coupling Selectivity Studied with Muscarinic Receptors as Model Systems. Life Sci. 1997, 60, 1007–1014. [Google Scholar] [CrossRef]
- Tan, P.-P.; Yuan, H.-H. Activation of Muscarinic Receptors Protects Against Retinal Neurons Damage and Optic Nerve Degeneration in Vitro and in Vivo Models. CNS Neurosci. Ther. 2014, 20, 227–236. [Google Scholar] [CrossRef]
- Zhou, W.; Zhu, X. Neuroprotection of Muscarinic Receptor Agonist Pilocarpine Against Glutamate-induced Apoptosis in Retinal Neurons. Cell. Mol. Neurobiol. 2008, 28, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.P.F.; Medina, S.V. Cholinergic Activity Modulates the Survival of Retinal Ganglion Cells in Culture: The Role of M1 Muscarinic Receptors. Int. J. Dev. Neurosci. 2001, 19, 559–567. [Google Scholar] [CrossRef]
- Zhu, X.; Zhou, W. Pilocarpine Protects Cobalt Chloride-induced Apoptosis of rgc-5 Cells: Involvement of Muscarinic Receptors and hif-1 Alpha Pathway. Cell. Mol. Neurobiol. 2010, 30, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Zhou, W. L-satropane Prevents Retinal Neuron Damage by Attenuating Cell Apoptosis and aβ Production via Activation of M1 Muscarinic Acetylcholine Receptor. Curr. Eye Res. 2017, 42, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Granja, M.G.; Gomes Braga, L.E. Igf-1 and igf-1r Modulate the Effects of il-4 on Retinal Ganglion Cells Survival: The Involvement of M1 Muscarinic Receptor. Biochem. Biophys. Res. Commun. 2019, 519, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Braga, L.E.G.; Miranda, R.L. Pkc Delta Activation Increases Neonatal Rat Retinal Cells Survival in Vitro: Involvement of Neurotrophins and M1 Muscarinic Receptors. Biochem. Biophys. Res. Commun. 2018, 500, 917–923. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, A.A.; Medina, S.V. Protein Kinase C Regulates the Expression of M1 Receptors and BDNF in Rat Retinal Cells. Neurochem. Res. 2009, 34, 884–890. [Google Scholar] [CrossRef]
- Braga, L.E.G.; Granja, M.G. Pma Increases M3 Muscarinic Receptor Levels and Decreases Retinal Cells Proliferation Through a Change in the Levels of Cell-cycle Regulatory Proteins. Neurosci. Lett. 2013, 550, 29–34. [Google Scholar] [CrossRef] [Green Version]
- Borda, E.; Berra, A. Correlations between Neuronal Nitric Oxide Synthase and Muscarinic M3/M1 Receptors in the Rat Retina. Exp. Eye Res. 2005, 80, 391–399. [Google Scholar] [CrossRef]
- Berra, A.; Ganzinelli, S. Inducible Nitric Oxide Synthase Subserves Cholinergic Vasodilation in Retina. Vis. Neurosci. 2005, 22, 371–377. [Google Scholar] [CrossRef]
- Liu, J.; McGlinn, A.M. Nicotinic Acetylcholine Receptor Subunits in Rhesus Monkey Retina. Investig. Ophthalmol. Vis. Sci. 2009, 50, 1408–1415. [Google Scholar] [CrossRef]
- Strang, C.E.; Amthor, F.R. Rabbit Retinal Ganglion Cell Responses to Nicotine can be Mediated by Beta2-containing Nicotinic Acetylcholine Receptors. Vis. Neurosci. 2003, 20, 651–662. [Google Scholar] [CrossRef]
- Strang, C.E.; Andison, M.E. Rabbit Retinal Ganglion Cells Express Functional Aalpha7 Nicotinic Acetylcholine Receptors. Am. J. Physiol. Cell Physiol. 2005, 289, C644–C655. [Google Scholar] [CrossRef] [Green Version]
- Strang, C.E.; Long, Y. Nicotinic and Muscarinic Acetylcholine Receptors Shape Ganglion Cell Response Properties. J. Neurophysiol. 2015, 113, 203–217. [Google Scholar] [CrossRef] [Green Version]
- Smith, M.L.; Souza, F.G.O. Acetylcholine Receptors in the Retinas of the α7 Nicotinic Acetylcholine Receptor Knockout Mouse. Mol. Vis. 2014, 20, 1328–1356. [Google Scholar] [PubMed]
- Schmidt, M.; Bienek, C. Differential Calcium Signalling by M2 and M3 Muscarinic Acetylcholine Receptors in a Single Cell Type. Naunyn Schmiedebergs Arch. Pharmacol. 1995, 352, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Pals-Rylaarsdam, R.; Hosey, M.M. Two Homologous Phosphorylation Domains Differentially Contribute to Desensitization and Internalization of the M2 Muscarinic Acetylcholine Receptor. J. Biol. Chem. 1997, 272, 14152–14158. [Google Scholar] [CrossRef] [Green Version]
- Zang, W.J.; Yu, X.J. On the Role of G Protein Activation and Phosphorylation in Desensitization to Acetylcholine in Guinea-Pig Atrial Cells. J. Physiol. 1993, 464, 649–679. [Google Scholar] [CrossRef] [Green Version]
- Antal, M.; Acuna-Goycolea, C. Cholinergic Activation of M2 Receptors Leads to Context-dependent Modulation of Feedforward Inhibition in the Visual Thalamus. PLoS Biol. 2010, 8, e1000348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cimini, B.A.; Strang, C.E. Role of Acetylcholine in Nitric Oxide Production in the Salamander Retina. J. Comp. Neurol. 2008, 507, 1952–1963. [Google Scholar] [CrossRef]
- Onali, P.; Olianas, M. Muscarinic M4 Receptor Inhibition of Dopamine d1-like Receptor Signalling in Rat Nucleus Accumbens. Eur. J. Pharmacol. 2002, 448, 105–111. [Google Scholar] [CrossRef]
- Arumugam, B.; McBrien, N.A. Muscarinic Antagonist Control of Myopia: Evidence for M4 and M1 Receptor-based Pathways in the Inhibition of Experimentally-induced Axial Myopia in the Tree Shrew. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5827–5837. [Google Scholar] [CrossRef] [Green Version]
- Cottriall, C.L.; Truong, H.-T. Inhibition of Myopia Development in Chicks Using Himbacine: A Role for M4 Receptors? Neuroreport 2001, 12, 2453–2456. [Google Scholar] [CrossRef]
- Inagaki, Y.; Mashima, Y. Polymorphism of Beta-adrenergic Receptors and Susceptibility to Open-angle Glaucoma. Mol. Vis. 2006, 12, 673–680. [Google Scholar]
- Liao, Q.; Wang, D.-H. Association of Genetic Polymorphisms of Enos with Glaucoma. Mol. Vis. 2011, 17, 153–158. [Google Scholar] [PubMed]
- Michel, M.C.; Teitsma, C.A. Polymorphisms in Human Muscarinic Receptor Subtype Genes. Handb. Exp. Pharmacol. 2012, 208, 49–59. [Google Scholar] [CrossRef]
- Fisher, A. Cholinergic Modulation of Amyloid Precursor Protein Processing with Emphasis on M1 Muscarinic Receptor: Perspectives and Challenges in Treatment of Alzheimer’s Disease. J. Neurochem. 2012, 120, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Dencker, D.; Thomsen, M. Muscarinic Acetylcholine Receptor Subtypes as Potential Drug Targets for the Treatment of Schizophrenia, Drug abuse, and Parkinson’s Disease. ACS Chem. Neurosci. 2012, 3, 80–89. [Google Scholar] [CrossRef]
- Weston-Green, K.; Huang, X.-F. Second Generation Antipsychotic-induced Type 2 Diabetes: A Role for the Muscarinic M3 Receptor. CNS Drugs 2013, 27, 1069–1080. [Google Scholar] [CrossRef] [PubMed]
- Seibold, L.K.; Wagner, B.D. The Diurnal and Nocturnal Effects of Pilocarpine on Intraocular Pressure in Patients Receiving Prostaglandin Analog Monotherapy. J. Ocul. Pharmacol. Ther. 2018, 34, 590–595. [Google Scholar] [CrossRef]
- Leung, K.C.M.; McMillan, A.S. The Efficacy of Cevimeline Hydrochloride in the Treatment of Xerostomia in Sjögren’s Syndrome in Southern Chinese Patients: A Randomised Double-blind, Placebo-controlled Crossover Study. Clin. Rheumatol. 2008, 27, 429–436. [Google Scholar] [CrossRef]
- Fife, R.S.; Chase, W.F. Cevimeline for the Treatment of Xerostomia in Patients with Sjögren Syndrome: A Randomized Trial. Arch. Intern. Med. 2002, 162, 1293–1300. [Google Scholar] [CrossRef]
- Petrone, D.; Condemi, J.J. A Double-blind, Randomized, Placebo-controlled Study of Cevimeline in Sjögren’s Syndrome Patients with Xerostomia and Keratoconjunctivitis Sicca. Arthritis Rheum. 2002, 46, 748–754. [Google Scholar] [CrossRef]
- Ono, M.; Takamura, E. Therapeutic Effect of Cevimeline on Dry Eye in Patients with Sjögren’s Syndrome: A Randomized, Double-blind Clinical Study. Am. J. Ophthalmol. 2004, 138, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Weaver, C.D.; Sheffler, D.J. Discovery and Development of a Potent and Highly Selective Small Molecule Muscarinic Acetylcholine Receptor Subtype i (mAChR 1 or M1) Antagonist in Vitro and in Vivo Probe. Curr. Top. Med. Chem. 2009, 9, 1217–1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conn, P.J.; Jones, C.K. Subtype-selective Allosteric Modulators of Muscarinic Receptors for the Treatment of CNS Disorders. Trends Pharmacol. Sci. 2009, 30, 148–155. [Google Scholar] [CrossRef] [Green Version]
- Digby, G.J.; Shirey, J.K. Allosteric Activators of Muscarinic Receptors as Novel Approaches for Treatment of CNS Disorders. Mol. Biosyst. 2010, 6, 1345–1354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinney, G.G. Muscarinic Receptor Activation for the Treatment of Schizophrenia. Neuropsychopharmacology 2006, 31, S26. [Google Scholar]
- Thomas, R.L.; Mistry, R. G Protein Coupling and Signaling Pathway Activation by M1 Muscarinic Acetylcholine Receptor Orthosteric and Allosteric Agonists. J. Pharmacol. Exp. Ther. 2008, 327, 365–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, C.K.; Brady, A.E. Tbpb is a Highly Selective M1 Allosteric Mscarinic Receptor Agonist in Vitro and Produces Robust Antipsychotic-like Effects in Vivo. In Proceedings of the Neuropsychopharmacology, Paris, France, 16–20 September 2006; pp. S116–S117. [Google Scholar]
- Shirey, J.K.; Xiang, Z. An Allosteric Potentiator of M4 mAChR Modulates Hippocampal Synaptic Transmission. Nat. Chem. Biol. 2008, 4, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Scarr, E. Muscarinic Receptors: Their Roles in Disorders of the Central Nervous System and Potential as Therapeutic Targets. CNS Neurosci. Ther. 2012, 18, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Matera, C.; Tata, A.M. Pharmacological Approaches to Targeting Muscarinic Acetylcholine Receptors. Recent Pat. CNS Drug Discov. 2014, 9, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Greig, N.H.; Reale, M. New Pharmacological Approaches to the Cholinergic System: An Overview on Muscarinic Receptor Ligands and Cholinesterase Inhibitors. Recent Pat. CNS Drug Discov. 2013, 8, 123–141. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruan, Y.; Patzak, A.; Pfeiffer, N.; Gericke, A. Muscarinic Acetylcholine Receptors in the Retina—Therapeutic Implications. Int. J. Mol. Sci. 2021, 22, 4989. https://doi.org/10.3390/ijms22094989
Ruan Y, Patzak A, Pfeiffer N, Gericke A. Muscarinic Acetylcholine Receptors in the Retina—Therapeutic Implications. International Journal of Molecular Sciences. 2021; 22(9):4989. https://doi.org/10.3390/ijms22094989
Chicago/Turabian StyleRuan, Yue, Andreas Patzak, Norbert Pfeiffer, and Adrian Gericke. 2021. "Muscarinic Acetylcholine Receptors in the Retina—Therapeutic Implications" International Journal of Molecular Sciences 22, no. 9: 4989. https://doi.org/10.3390/ijms22094989
APA StyleRuan, Y., Patzak, A., Pfeiffer, N., & Gericke, A. (2021). Muscarinic Acetylcholine Receptors in the Retina—Therapeutic Implications. International Journal of Molecular Sciences, 22(9), 4989. https://doi.org/10.3390/ijms22094989






