Hippocampal Sclerosis in Pilocarpine Epilepsy: Survival of Peptide-Containing Neurons and Learning and Memory Disturbances in the Adult NMRI Strain Mouse
Abstract
:1. Introduction
- (1)
- (2)
- (3)
- We aimed to study the effects of HS on the spatial learning and memory processes in the NMRI mouse strain.
2. Results
2.1. Neuronal Loss in the Hippocampus 3.5 Months after the SE
2.2. Microglial Activation and Proliferation 3.5 Months after the SE in the HF
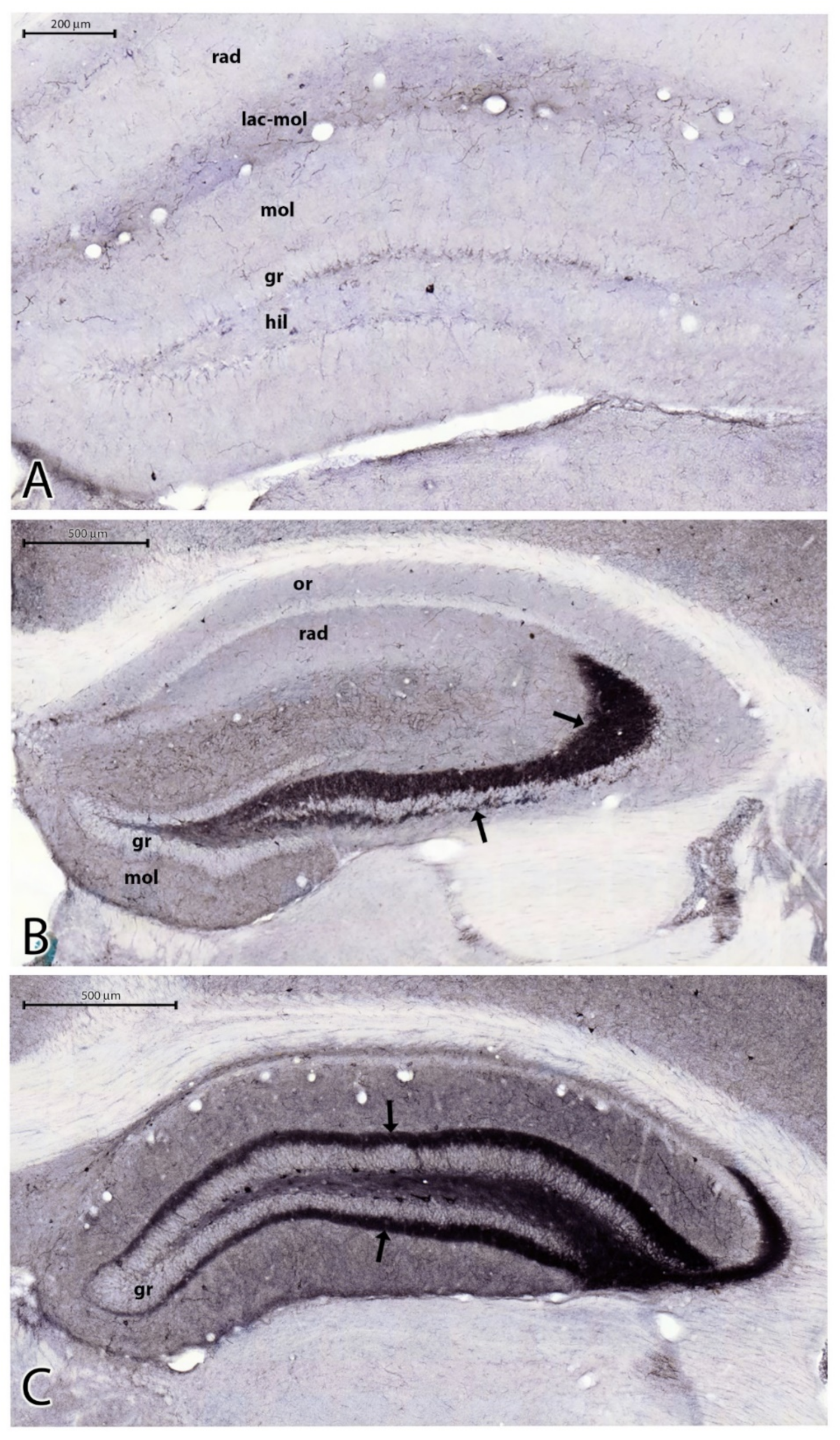
2.3. Sprouting of Mossy Fibers 3.5 Months after the SE
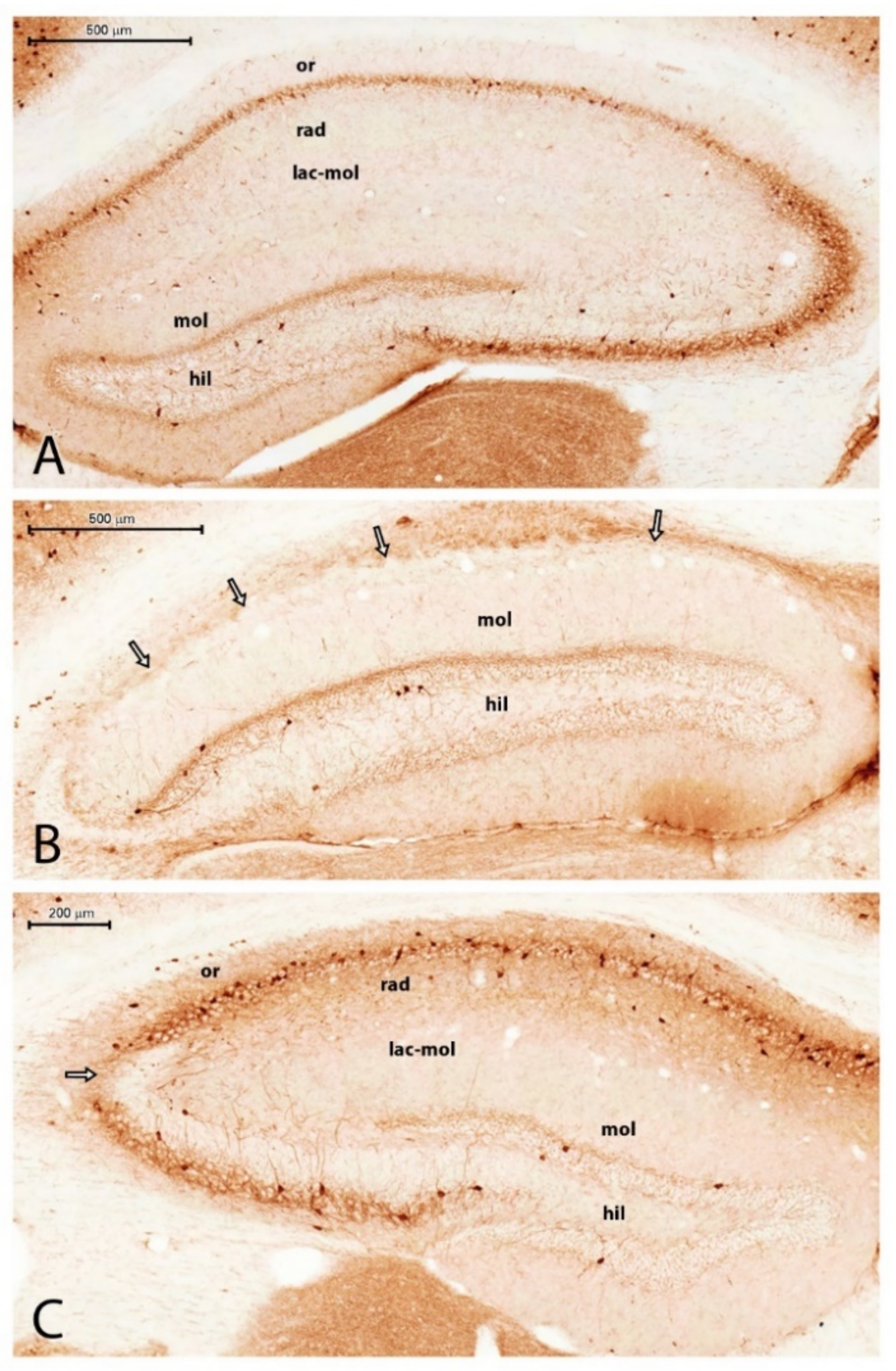
2.4. Parvalbumin Containing Hippocampal Interneurons 3.5 Months after the SE
2.5. Alterations in the Number of Calretinin Immunostained Cells
2.6. The Impairment of Spatial Learning 3 Months after the SE
3. Discussion
3.1. Neuronal Loss in Epileptic Hippocampi
3.2. Microglial Activation in the Epileptic Mice
3.3. Sprouting of Mossy Fibers in the Epileptic Mice
3.4. The Decrease in the Number of the PV-Containing Interneurons
3.5. Alterations of CR Immunoreactivity in the Hippocampal Formation
3.6. Learning and Memory Deficiency in Epileptic Mice
4. Materials and Methods
4.1. Experimental Protocol and Pharmacological Treatment
4.2. Tissue Preparation
4.3. Immunocytochemistry
4.4. Morphometry and Evaluation of the Data
4.5. Spatial Learning Test
5. Conclusions
- The HS in epileptic NMRI mice was characterized by neuronal loss, microgliosis, and axonal sprouting. The neuronal loss in the Ammon’s horn was approximately 50% compared with the controls. The neuronal loss in the DG was less, being approximately 30% compared with the controls.
- A large population (approximately 50%) of the hippocampal PV-containing GABAergic neurons was lost in HS. The loss of PV interneurons possibly contributed to the decay in learning and memory performance of the PT animals.
- The degeneration of hippocampal CR-containing interneurons was less pronounced, as approximately 20% of the CR-containing cells degenerated in HS.
- Axonal sprouting involved large areas of the epileptic hippocampal neuropil. The hilum and IML of the DG, the stratum lucidum, and stratum oriens of the CA3 were heavily innervated by axons containing the NPY transmitter peptide.
- The strong increase in NPY expression proved that in HS, the peptidergic component of the hippocampal neurotransmission survived better than the glutamate system. This possibly could lead to alterations of the hippocampal synaptic transmission. Instead of fast glutamate signaling, the slow, metabotropic peptidergic signaling prevailed. The slowdown of signaling could also contribute to the worsening of learning and memory functions.
- We summarized the neurochemical transformation of the sclerosed hippocampus in Figure 10.
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AOI | area of interest |
| BBB | blood–brain barrier |
| CA | Cornu Ammonis (Ammon’s horn) |
| CI | confidence interval |
| CR | calretinin |
| CR-IR | calretinin immunoreactivity or immunoreactive |
| DG | dentate gyrus |
| HF | hippocampal formation |
| HS | hippocampal sclerosis |
| Iba1 | Ionized calcium binding adaptor molecule 1 |
| i.p. | intraperitoneally |
| IML | internal molecular layer |
| MRI | magnetic resonance imaging |
| NMDA | N-methyl-D-aspartic acid |
| NMRI | Naval Medical Research Institute (inbred albino mouse line) |
| NPY | neuropeptide Y |
| PILO | pilocarpine |
| PT | pilocarpine treated |
| PV | parvalbumin |
| SD | standard deviation |
| SE | status epilepticus |
| SRS | spontaneous recurrent seizures |
| SZR104 | N-(2-(dimethylamino)ethyl)-3-(morpholinomethyl)-4-hydroxyquinoline-2-carboxamide |
| TLE | temporal lobe epilepsy |
References
- Curia, G.; Longo, D.; Biagini, G.; Jones, R.S.; Avoli, M. The pilocarpine model of temporal lobe epilepsy. J. Neurosci. Methods 2008, 172, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Scarr, E.; Seo, M.S.; Aumann, T.D.; Chana, G.; Everall, I.P.; Dean, B. The distribution of muscarinic M1 receptors in the human hippocampus. J. Chem. Neuroanat. 2016, 77, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Smolders, I.; Khan, G.M.; Manil, J.; Ebinger, G.; Michotte, Y. NMDA receptor-mediated pilocarpine-induced seizures: Characterization in freely moving rats by microdialysis. Br. J. Pharmacol. 1997, 121, 1171–1179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szente, M.; Mihály, A.; Tóth, G.; Joó, F. Neocortical cytopathology in focal aminopyridine seizures as related to the intracortical diffusion of [3H] 4-aminopyridine. Acta Neuropathol. 1985, 66, 145–154. [Google Scholar] [CrossRef]
- Mihály, A.; Bozoky, B. Immunohistochemical localization of extravasated serum albumin in the hippocampus of human subjects with partial and generalized epilepsies and epileptiform convulsions. Acta Neuropathol. 1984, 65, 25–34. [Google Scholar] [CrossRef]
- Weiczner, R.; Krisztin-Peva, B.; Mihály, A. Blockade of AMPA-receptors attenuates 4-aminopyridine seizures, decreases the activation of inhibitory neurons but is ineffective against seizure-related astrocytic swelling. Epilepsy Res. 2008, 78, 22–32. [Google Scholar] [CrossRef] [Green Version]
- Farkas, I.G.; Czigner, A.; Farkas, E.; Dobó, E.; Soós, K.; Penke, B.; Endrész, V.; Mihály, A. Beta-amyloid peptide-induced blood-brain barrier disruption facilitates T-cell entry into the rat brain. Acta Histochem. 2003, 105, 115–125. [Google Scholar] [CrossRef] [Green Version]
- Gorter, J.A.; van Vliet, E.A.; Aronica, E. Status epilepticus, blood-brain barrier disruption, inflammation and epileptogenesis. Epilepsy Behav. 2015, 49, 13–16. [Google Scholar] [CrossRef]
- Turski, W.A.; Cavalheiro, E.; Bortolotto, Z.A.; Mello, L.M.; Schwarz, M.; Turski, L. Seizures produced by pilocarpine in mice: A behavioral, electroencephalographic and morphological analysis. Brain Res. 1984, 321, 237–253. [Google Scholar] [CrossRef]
- Cavalheiro, E.A.; Santos, N.F.; Priel, M.R. The Pilocarpine Model of Epilepsy in Mice. Epilepsia 1996, 37, 1015–1019. [Google Scholar] [CrossRef]
- Schidlitzki, A.; Twele, F.; Klee, R.; Waltl, I.; Römermann, K.; Bröer, S.; Meller, S.; Gerhauser, I.; Rankovic, V.; Li, D.; et al. A combination of NMDA and AMPA receptor antagonists retards granule cell dispersion and epileptogenesis in a model of acquired epilepsy. Sci. Rep. 2017, 7, 12191. [Google Scholar] [CrossRef] [Green Version]
- Thom, M. Review: Hippocampal sclerosis in epilepsy: A neuropathology review. Neuropathol. Appl. Neurobiol. 2014, 40, 520–543. [Google Scholar] [CrossRef]
- Fabene, P.; Weiczner, R.; Marzola, P.; Nicolato, E.; Calderan, L.; Andrioli, A.; Farkas, E.; Süle, Z.; Mihaly, A.; Sbarbati, A. Structural and functional MRI following 4-aminopyridine-induced seizures: A comparative imaging and anatomical study. Neurobiol. Dis. 2006, 21, 80–89. [Google Scholar] [CrossRef] [Green Version]
- Kienzler-Norwood, F.; Costard, L.; Sadangi, C.; Müller, P.; Neubert, V.; Bauer, S.; Rosenow, F.; Norwood, B.A. A novel animal model of acquired human temporal lobe epilepsy based on the simultaneous administration of kainic acid and lorazepam. Epilepsia 2017, 58, 222–230. [Google Scholar] [CrossRef] [Green Version]
- Mihaly, A.; Bencsik, K.; Nógrádi, A. Pharmacological inhibition of brain carbonic anhydrase protects against 4-aminopyridine seizures. Acta Physiol. Hung. 1994, 82, 99–108. [Google Scholar]
- Borbély, S.; Dobó, E.; Czégé, D.; Molnár, E.; Bakos, M.; Szűcs, B.; Vincze, A.; Világi, I.; Mihály, A. Modification of ionotropic glutamate receptor mediated processes in the rat hippocampus following repeated, brief seizures. Neuroscience 2009, 159, 358–368. [Google Scholar] [CrossRef]
- Dobó, E.; Török, I.; Mihály, A.; Károly, N.; Krisztin-Peva, B. Interstrain differences of ionotropic glutamate receptor subunits in the hippocampus and induction of hippocampal sclerosis with pilocarpine in mice. J. Chem. Neuroanat. 2015, 64–65, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Károly, N.; Dobó, E.; Mihaly, A. Comparative immunohistochemical study of the effects of pilocarpine on the mossy cells, mossy fibres and inhibitory neurones in murine dentate gyrus. Acta Neurobiol. Exp. 2015, 75, 220–237. [Google Scholar]
- Mello, L.; Cavalheiro, E.; Tan, A.M.; Kupfer, W.R.; Pretorius, J.K.; Babb, T.L.; Finch, D.M. Circuit Mechanisms of Seizures in the Pilocarpine Model of Chronic Epilepsy: Cell Loss and Mossy Fiber Sprouting. Epilepsia 1993, 34, 985–995. [Google Scholar] [CrossRef]
- Mihály, A. The Reactive Plasticity of Hippocampal Ionotropic Glutamate Receptors in Animal Epilepsies. Int. J. Mol. Sci. 2019, 20, 1030. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Song, X.; Wu, L.; Nadler, J.V.; Zhan, R.-Z. Persistent Hyperactivity of Hippocampal Dentate Interneurons after a Silent Period in the Rat Pilocarpine Model of Epilepsy. Front. Cell. Neurosci. 2016, 10, 94. [Google Scholar] [CrossRef] [Green Version]
- Maglóczky, Z.; Freund, T.F. Impaired and repaired inhibitory circuits in the epileptic human hippocampus. Trends Neurosci. 2005, 28, 334–340. [Google Scholar] [CrossRef]
- Sloviter, R.S. “Epileptic” brain damage in rats induced by sustained electrical stimulation of the perforant path. I. Acute electrophysiological and light-microscopic studies. Brain Res. Bull. 1983, 10, 675–697. [Google Scholar] [CrossRef]
- Rzezak, P.; Lima, E.M.; Gargaro, A.C.; Coimbra, E.; de Vincentiis, S.; Velasco, T.R.; Leite, J.P.; Busatto, G.F.; Valente, K.D. Everyday memory impairment in patients with temporal lobe epilepsy caused by hippocampal sclerosis. Epilepsy Behav. 2017, 69, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Mullen, R.; Buck, C.; Smith, A. NeuN, a neuronal specific nuclear protein in vertebrates. Development 1992, 116, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Károly, N.; Mihály, A.; Dobó, E. Comparative immunohistochemistry of synaptic markers in the rodent hippocampus in pilocarpine epilepsy. Acta Histochem. 2011, 113, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Lajkó, N.; Kata, D.; Szabó, M.; Mátyás, A.; Dulka, K.; Földesi, I.; Fülöp, F.; Gulya, K.; Vécsei, L.; Mihály, A. Sensitivity of Rodent Microglia to Kynurenines in Models of Epilepsy and Inflammation In Vivo and In Vitro: Microglia Activation is Inhibited by Kynurenic Acid and the Synthetic Analogue SZR104. Int. J. Mol. Sci. 2020, 21, 9333. [Google Scholar] [CrossRef] [PubMed]
- Volz, F.; Bock, H.H.; Gierthmuehlen, M.; Zentner, J.; Haas, C.A.; Freiman, T.M. Stereologic estimation of hippocampal GluR2/3- and calretinin-immunoreactive hilar neurons (presumptive mossy cells) in two mouse models of temporal lobe epilepsy. Epilepsia 2011, 52, 1579–1589. [Google Scholar] [CrossRef]
- Zombori, T. Animal Experiments Investigating Epilepsy. Master’s Thesis, Faculty of Medicine, University of Szeged, Szeged, Hungary, 2012; pp. 1–47. (In Hungarian). [Google Scholar]
- Vezzani, A.; Lang, B.; Aronica, E. Immunity and Inflammation in Epilepsy. Cold Spring Harb. Perspect. Med. 2015, 6, a022699. [Google Scholar] [CrossRef] [Green Version]
- Olney, J.W. Excitatory transmitters and epilepsy-related brain damage. Int. Rev. Neurobiol. 1985, 27, 337–362. [Google Scholar] [CrossRef]
- Walker, M.C. Pathophysiology of status epilepticus. Neurosci. Lett. 2018, 667, 84–91. [Google Scholar] [CrossRef]
- Honavar, M.; Meldrum, B.S. Epilepsy. In Greenfield’s Neuropathology, 7th ed.; Graham, P.I., Lantos, P.L., Eds.; Arnold: London, UK, 2002; Volume 1, pp. 899–941. [Google Scholar]
- Tai, X.Y.; Bernhardt, B.; Thom, M.; Thompson, P.; Baxendale, S.; Koepp, M.; Bernasconi, N. Review: Neurodegenerative processes in temporal lobe epilepsy with hippocampal sclerosis: Clinical, pathological and neuroimaging evidence. Neuropathol. Appl. Neurobiol. 2017, 44, 70–90. [Google Scholar] [CrossRef]
- Pocock, J.M.; Kettenmann, H. Neurotransmitter receptors on microglia. Trends Neurosci. 2007, 30, 527–535. [Google Scholar] [CrossRef]
- Priller, J.; Prinz, M. Trageting microglia in brain disorders. Science 2019, 365, 32–33. [Google Scholar] [CrossRef]
- Deczkowska, A.; Keren-Shaul, H.; Weiner, A.; Colonna, M.; Schwartz, M.; Amit, I. Disease-Associated Microglia: A Universal Immune Sensor of Neurodegeneration. Cell 2018, 173, 1073–1081. [Google Scholar] [CrossRef] [Green Version]
- Buckmaster, P.S. Mossy fiber sprouting in the dentate gyrus. In Jasper’s Basic Mechanisms of the Epilepsies, 4th ed.; Rogawski, M.A., Delagado-Escueta, A.V., Noebels, J.L., Avoli, M., Eds.; Oxford University Press: New York, NY, USA, 2012; pp. 611–630. ISBN 019976540. [Google Scholar]
- Thom, M.; Martinian, L.; Catarino, C.; Yogarajah, M.; Koepp, M.J.; Caboclo, L.; Sisodiya, S.M. Bilateral reorganization of the dentate gyrus in hippocampal sclerosis: A postmortem study. Neurology 2009, 73, 1033–1040. [Google Scholar] [CrossRef] [Green Version]
- Lurton, D.; Cavalheiro, E.A. Neuropeptide-Y immunoreactivity in the pilocarpine model of temporal lobe epilepsy. Exp. Brain Res. 1997, 116, 186–190. [Google Scholar] [CrossRef]
- Wu, Y.-F.; Li, S.-B. Neuropeptide Y expression in mouse hippocampus and its role in neuronal excitotoxicity. Acta Pharmacol. Sin. 2005, 26, 63–68. [Google Scholar] [CrossRef] [Green Version]
- Nadler, J.V.; Tu, B.; Timofeeva, O.; Jiao, Y.; Herzog, H. Neuropeptide Y in the recurrent mossy fiber pathway. Peptides 2007, 28, 357–364. [Google Scholar] [CrossRef] [Green Version]
- Freund, T.F.; Buzsáki, G. Interneurons of the hippocampus. Hippocampus 1996, 6, 347–470. [Google Scholar] [CrossRef]
- Papp, P.; Kovács, Z.; Szocsics, P.; Juhász, G.; Maglóczky, Z. Alterations in hippocampal and cortical densities of functionally different interneurons in rat models of absence epilepsy. Epilepsy Res. 2018, 145, 40–50. [Google Scholar] [CrossRef]
- Botterill, J.; Nogovitsyn, N.; Caruncho, H.; Kalynchuk, L. Selective plasticity of hippocampal GABAergic interneuron populations following kindling of different brain regions. J. Comp. Neurol. 2016, 525, 389–406. [Google Scholar] [CrossRef]
- Cameron, S.; Lopez, A.; Glabman, R.; Abrams, E.; Johnson, S.; Field, C.; Gulland, F.M.D.; Buckmaster, P.S. Proportional loss of parvalbumin-immunoreactive synaptic boutons and granule cells from the hippocampus of sea lions with temporal lobe epilepsy. J. Comp. Neurol. 2019, 527, 2341–2355. [Google Scholar] [CrossRef]
- Filice, F.; Celio, M.R.; Babalian, A.; Blum, W.; Szabolcsi, V. Parvalbumin-expressing ependymal cells in rostral lateral ventricle wall adhesions contribute to aging-related ventricle stenosis in mice. J. Comp. Neurol. 2017, 525, 3266–3285. [Google Scholar] [CrossRef] [Green Version]
- Lichvarova, L.; Blum, W.; Schwaller, B.; Szabolcsi, V. Parvalbumin expression in oligodendrocyte-like CG4 cells causes a reduction in mitochondrial volume, attenuation in reactive oxygen species production and a decrease in cell processes’ length and branching. Sci. Rep. 2019, 9, 2341–2355. [Google Scholar] [CrossRef] [Green Version]
- Tóth, K.; Erőss, L.; Vajda, J.; Halász, P.; Freund, T.F.; Maglóczky, Z. Loss and reorganization of calretinin-containing interneurons in the epileptic human hippocampus. Brain 2010, 133, 2763–2777. [Google Scholar] [CrossRef] [Green Version]
- Blümcke, I.; Beck, H.; Nitsch, R.; Eickhoff, C.; Scheffler, B.; Celio, M.; Schramm, J.; Elger, C.E.; Wolf, H.K.; Wiestler, O.D. Preservation of calretinin-immunoreactive neurons in the hippocampus of epilepsy patients with Ammon’s horn sclerosis. J. Neuropathol. Exp. Neurol. 1996, 55, 329–341. [Google Scholar]
- Blümcke, I.; Beck, H.; Suter, B.; Hoffmann, D.; Födisch, H.J.; Wolf, H.K.; Schramm, J.; Elger, C.E.; Wiestler, O.D. An increase of hippocampal calretinin-immunoreactive neurons correlates with early febrile seizures in temporal lobe epilepsy. Acta Neuropathol. 1999, 97, 31–39. [Google Scholar] [CrossRef]
- Herrewegen, Y.V.D.; Denewet, L.; Buckinx, A.; Albertini, G.; Van Eeckhaut, A.; Smolders, I.; De Bundel, D. The Barnes Maze Task Reveals Specific Impairment of Spatial Learning Strategy in the Intrahippocampal Kainic Acid Model for Temporal Lobe Epilepsy. Neurochem. Res. 2018, 44, 600–608. [Google Scholar] [CrossRef]
- Hauser, J.; López, L.H.L.; Feldon, J.; Gargiulo, P.A.; Yee, B.K. Small lesions of the dorsal or ventral hippocampus subregions are associated with distinct impairments in working memory and reference memory retrieval, and combining them attenuates the acquisition rate of spatial reference memory. Hippocampus 2020, 30, 938–957. [Google Scholar] [CrossRef]
- Kopniczky, Z.; Dochnal, R.; Mácsai, M.; Pál, Á.; Kiss, G.; Mihály, A.; Szabó, G. Alterations of behavior and spatial learning after unilateral entorhinal ablation of rats. Life Sci. 2006, 78, 2683–2688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, C.J.; Gröticke, I.; Bankstahl, M.; Löscher, W. Behavioral and cognitive alterations, spontaneous seizures, and neuropathology developing after a pilocarpine-induced status epilepticus in C57BL/6 mice. Exp. Neurol. 2009, 219, 284–297. [Google Scholar] [CrossRef] [PubMed]
- Reyes, A.; Holden, H.M.; Chang, Y.-H.A.; Uttarwar, V.S.; Sheppard, D.P.; DeFord, N.E.; DeJesus, S.Y.; Kansal, L.; Gilbert, P.E.; McDonald, C.R. Impaired spatial pattern separation performance in temporal lobe epilepsy is associated with visuospatial memory deficits and hippocampal volume loss. Neuropsychologia 2018, 111, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Franklin, K.B.J.; Paxinos, G. The Mouse Brain in Stereotaxic Coordinates; Academic Press: San Diego, CA, USA, 1997. [Google Scholar]
- Pitts, M.W. Barnes Maze Procedure for Spatial Learning and Memory in Mice. BIO-Protocol 2018, 8, e2744. [Google Scholar] [CrossRef] [Green Version]
- Khakshooy, A.M.; Chiappelli, F. Practical Biostatistics in Translational Healthcare; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar] [CrossRef]








| Pilocarpine-Treated (PT) Mouse Number | Localization of the Light Microscopic Neuronal Loss in the Hippocampal Formation Stained with Anti-NeuN Serum |
|---|---|
| PT1 | CA1, CA2, CA3 degenerated |
| PT2 | only CA2 degenerated |
| PT3 | CA1, CA2, CA3, hilum degenerated, granule cells dispersed |
| PT4 | CA1, CA2, CA3 completely degenerated |
| PT5 | cell loss in CA1, CA3 and hilum |
| PT6 | cell loss in the hilum and upper blade of dentate granule cell layer |
| PT7 | CA1, CA2 and CA3 completely degenerated, minor loss of the upper blade of the dentate granule cell layer was present |
| PT8 | CA1, CA3: patchy neuronal losses in the stratum pyramidale |
| PT9 | CA1, CA3 degenerated, hilum partial loss, CA2 normal |
| Day 1 | Day 2 | Day 3 | Day 4 | ||
|---|---|---|---|---|---|
| Control | mean | 52.3 | 57.2 | 46.9 | 36.1 * |
| SD | 34.1 | 27.1 | 31.7 | 25.4 | |
| Pilo-treated | mean | 109.2 | 93.8 | 131.1 | 139.8 * |
| SD | 97.0 | 109.9 | 103.4 | 113.0 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mátyás, A.; Borbély, E.; Mihály, A. Hippocampal Sclerosis in Pilocarpine Epilepsy: Survival of Peptide-Containing Neurons and Learning and Memory Disturbances in the Adult NMRI Strain Mouse. Int. J. Mol. Sci. 2022, 23, 204. https://doi.org/10.3390/ijms23010204
Mátyás A, Borbély E, Mihály A. Hippocampal Sclerosis in Pilocarpine Epilepsy: Survival of Peptide-Containing Neurons and Learning and Memory Disturbances in the Adult NMRI Strain Mouse. International Journal of Molecular Sciences. 2022; 23(1):204. https://doi.org/10.3390/ijms23010204
Chicago/Turabian StyleMátyás, Adrienne, Emőke Borbély, and András Mihály. 2022. "Hippocampal Sclerosis in Pilocarpine Epilepsy: Survival of Peptide-Containing Neurons and Learning and Memory Disturbances in the Adult NMRI Strain Mouse" International Journal of Molecular Sciences 23, no. 1: 204. https://doi.org/10.3390/ijms23010204
APA StyleMátyás, A., Borbély, E., & Mihály, A. (2022). Hippocampal Sclerosis in Pilocarpine Epilepsy: Survival of Peptide-Containing Neurons and Learning and Memory Disturbances in the Adult NMRI Strain Mouse. International Journal of Molecular Sciences, 23(1), 204. https://doi.org/10.3390/ijms23010204





