Tie-Over Bolster Pressure Dressing Improves Outcomes of Skin Substitutes Xenografts on Athymic Mice
Abstract
:1. Introduction
2. Results
2.1. Mean Surface Area of SASS Grafts Is Larger with the New Technique at Any Time Points Postoperatively
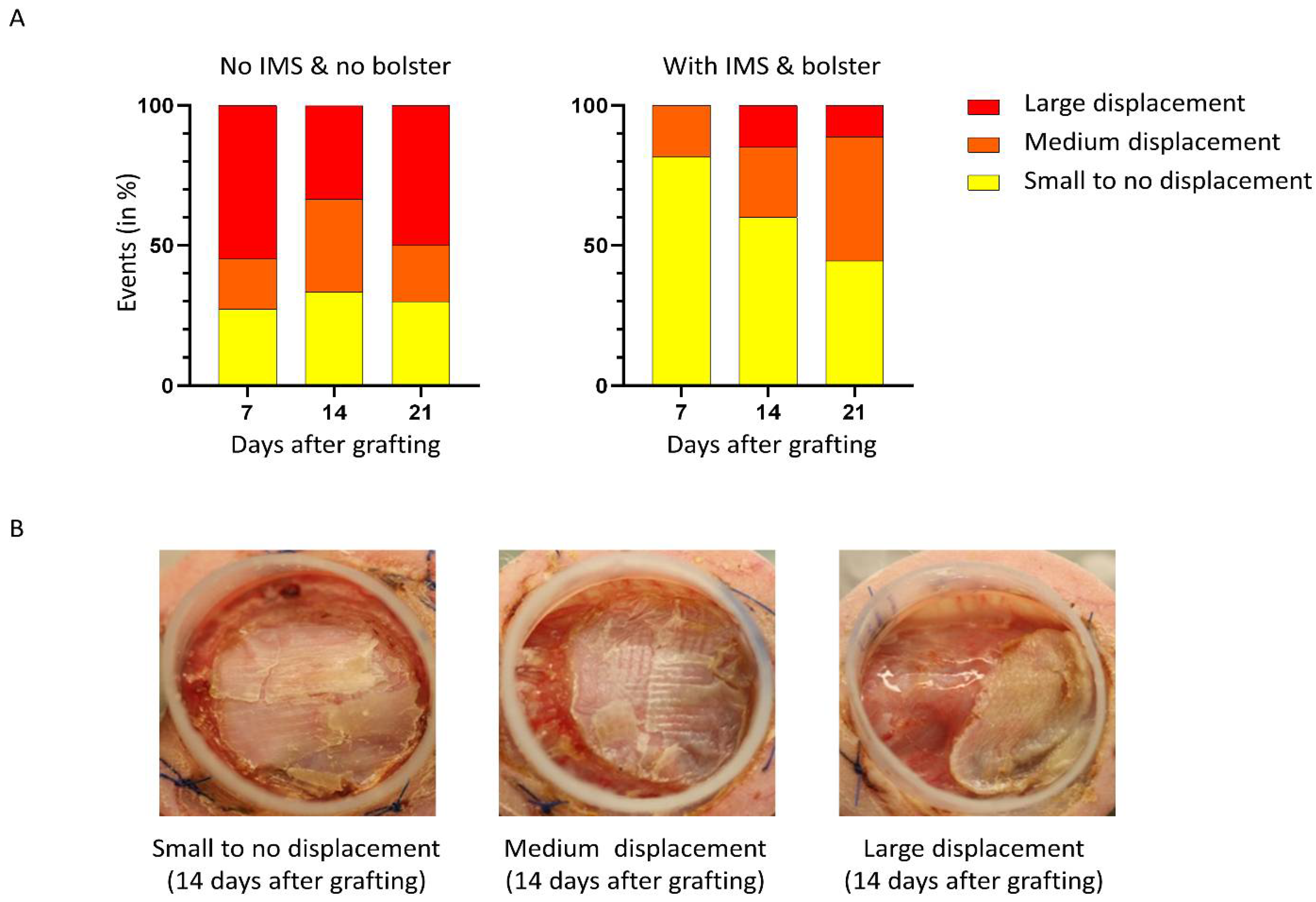
2.2. The Use of Tie-Over Dressing and Intramuscular Sutures Significantly Reduces SASS Grafts Displacement
2.3. The Use of Tie-Over Dressing and Intramuscular Sutures Significantly Reduces Contraction of SASS Grafts
2.4. Hematoxylin and Eosin Staining Showed No Significant Difference between the Two Methods in the Histological Analysis of the SASS Grafts
3. Discussion
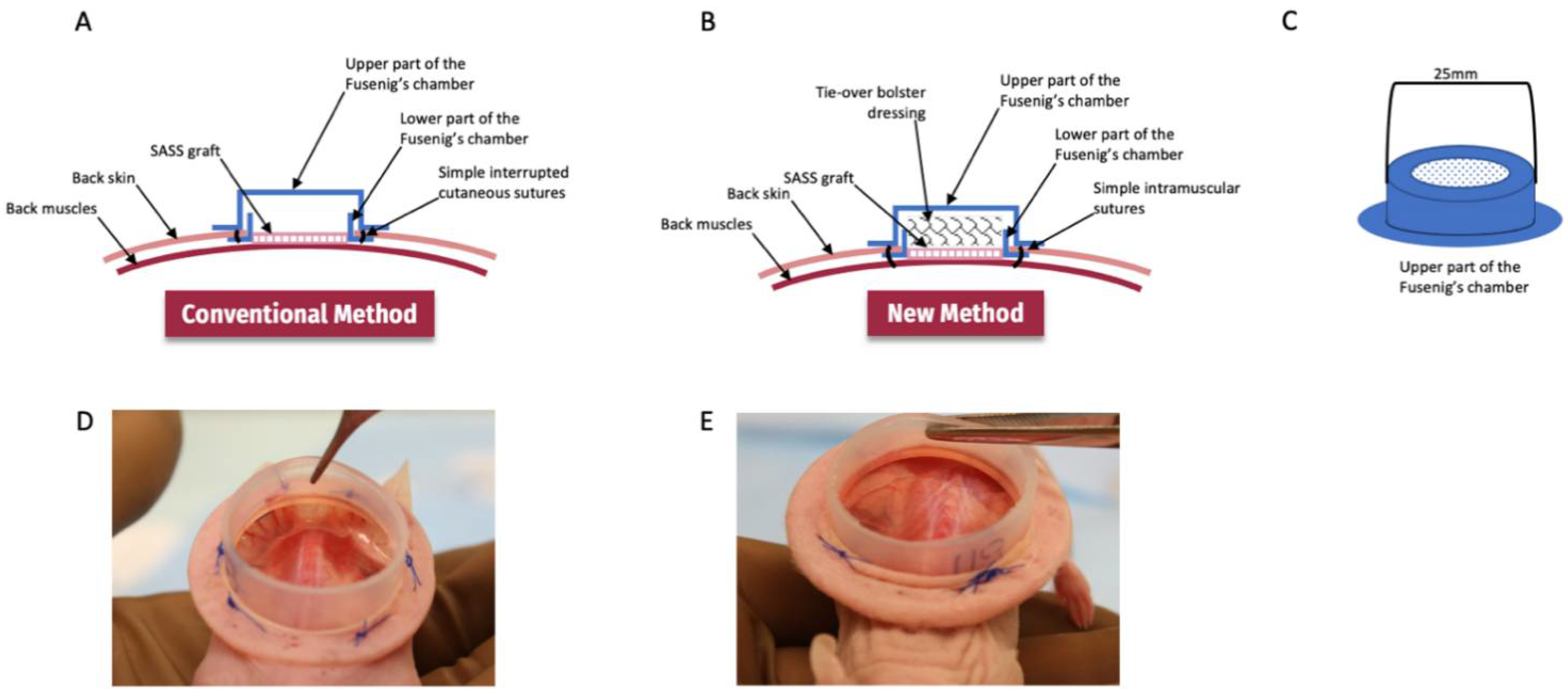
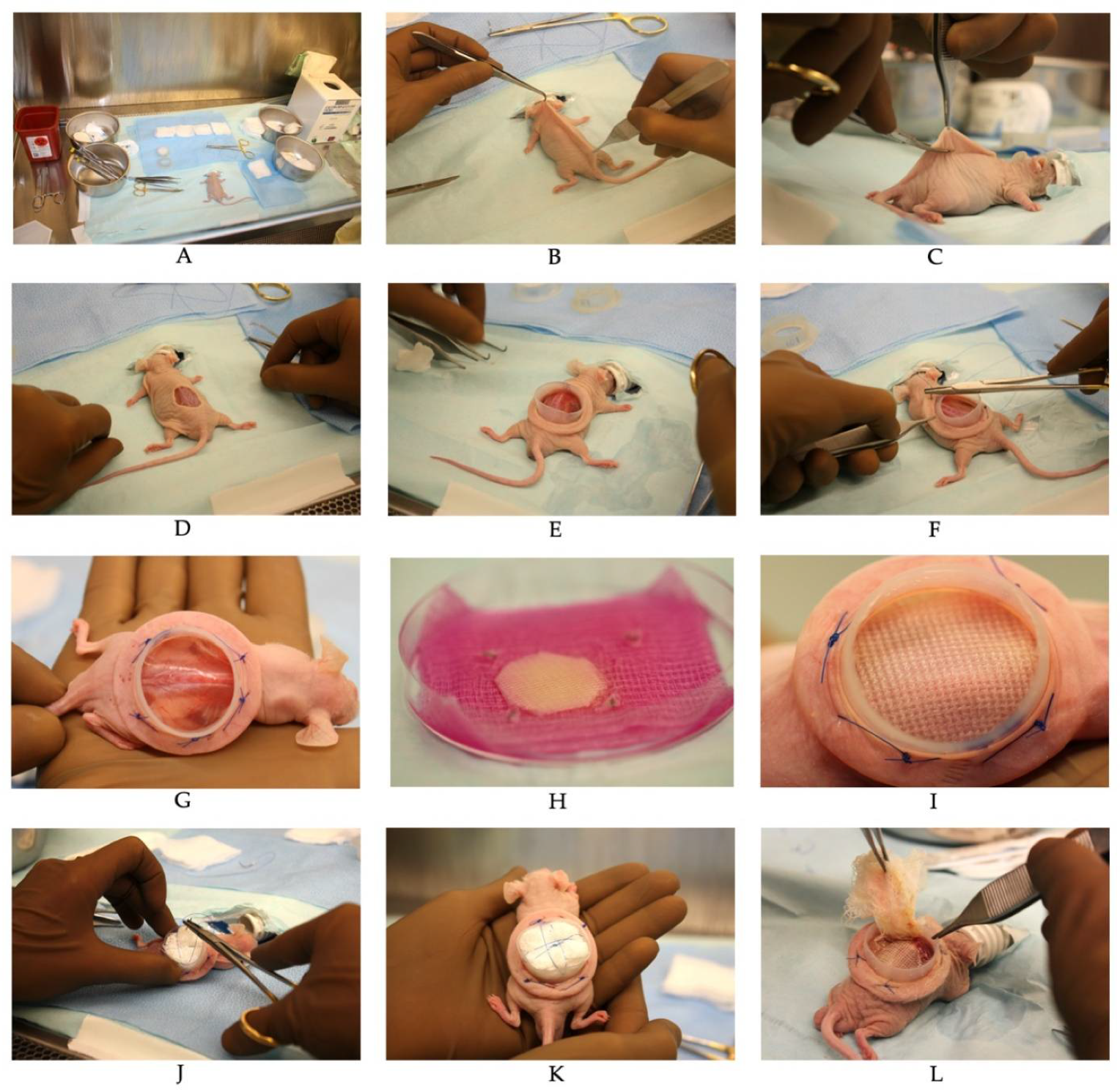
4. Materials and Methods
4.1. Isolation of Human Skin Fibroblasts and Keratinocytes
4.2. Human Feeder Layer
4.3. Monolayer Culture of Primary Human Fibroblasts and Keratinocytes
4.4. Self-Assembled Skin Substitute Production
4.5. Skin Substitutes Preparation for Grafting
4.6. Fusenig’s Chamber
4.7. Skin Substitutes Grafting on CD1-Foxn1nu Mice
4.8. Graft Area Analysis
4.9. Histological Analysis
4.10. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, S.H.; Jeong, S.K.; Ahn, S.K. An update of the defensive barrier function of skin. Yonsei Med. J. 2006, 47, 293–306. [Google Scholar] [CrossRef] [Green Version]
- Ramos-e-Silva, M.; Jacques, C. Epidermal barrier function and systemic diseases. Clin. Dermatol. 2012, 30, 277–279. [Google Scholar] [CrossRef]
- Laimer, M.; Prodinger, C.; Bauer, J.W. Hereditary epidermolysis bullosa. J. Dtsch. Dermatol. Ges. 2015, 13, 1125–1133. [Google Scholar] [CrossRef] [Green Version]
- Herndon, D.N.; Parks, D.H. Comparison of serial debridement and autografting and early massive excision with cadaver skin overlay in the treatment of large burns in children. J. Trauma 1986, 26, 149–152. [Google Scholar] [CrossRef]
- Herndon, D.N.; Barrow, R.E.; Rutan, R.L.; Rutan, T.C.; Desai, M.H.; Abston, S. A comparison of conservative versus early excision. Therapies in severely burned patients. Ann. Surg. 1989, 209, 547–552; Discussion 552–543. [Google Scholar] [CrossRef]
- Moulik, P.K.; Mtonga, R.; Gill, G.V. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care 2003, 26, 491–494. [Google Scholar] [CrossRef] [Green Version]
- Gould, L.; Abadir, P.; Brem, H.; Carter, M.; Conner-Kerr, T.; Davidson, J.; DiPietro, L.; Falanga, V.; Fife, C.; Gardner, S.; et al. Chronic wound repair and healing in older adults: Current status and future research. Wound Repair Regen. 2015, 23, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Cheung, C. Older adults and ulcers: Chronic wounds in the geriatric population. Adv. Ski. Wound Care 2010, 23, 39–44, quiz 36–45. [Google Scholar] [CrossRef]
- El-Ftesi, S.; Chang, E.I.; Longaker, M.T.; Gurtner, G.C. Aging and diabetes impair the neovascular potential of adipose-derived stromal cells. Plast. Reconstr. Surg. 2009, 123, 475–485. [Google Scholar] [CrossRef] [Green Version]
- Olsson, M.; Järbrink, K.; Divakar, U.; Bajpai, R.; Upton, Z.; Schmidtchen, A.; Car, J. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen. 2019, 27, 114–125. [Google Scholar] [CrossRef] [Green Version]
- Posnett, J.; Gottrup, F.; Lundgren, H.; Saal, G. The resource impact of wounds on health-care providers in Europe. J. Wound Care 2009, 18, 154–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Low, Z.W.K.; Li, Z.; Owh, C.; Chee, P.L.; Ye, E.; Dan, K.; Chan, S.Y.; Young, D.J.; Loh, X.J. Recent innovations in artificial skin. Biomater. Sci. 2020, 8, 776–797. [Google Scholar] [CrossRef] [PubMed]
- Auger, F.A.; Berthod, F.; Moulin, V.; Pouliot, R.; Germain, L. Tissue-engineered skin substitutes: From in vitro constructs to in vivo applications. Biotechnol. Appl. Biochem. 2004, 39, 263–275. [Google Scholar] [CrossRef]
- Przekora, A. A Concise Review on Tissue Engineered Artificial Skin Grafts for Chronic Wound Treatment: Can We Reconstruct Functional Skin Tissue In Vitro? Cells 2020, 9, 1622. [Google Scholar] [CrossRef] [PubMed]
- Germain, L.; Larouche, D.; Nedelec, B.; Perreault, I.; Duranceau, L.; Bortoluzzi, P.; Beaudoin Cloutier, C.; Genest, H.; Caouette-Laberge, L.; Dumas, A.; et al. Autologous bilayered self-assembled skin substitutes (SASSs) as permanent grafts: A case series of 14 severely burned patients indicating clinical effectiveness. Eur. Cell Mater. 2018, 36, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.R.; Navarro, J.; Coburn, J.C.; Mahadik, B.; Molnar, J.; Holmes, J.H.t.; Nam, A.J.; Fisher, J.P. Current and Future Perspectives on Skin Tissue Engineering: Key Features of Biomedical Research, Translational Assessment, and Clinical Application. Adv. Healthc. Mater. 2019, 8, e1801471. [Google Scholar] [CrossRef] [PubMed]
- Vig, K.; Chaudhari, A.; Tripathi, S.; Dixit, S.; Sahu, R.; Pillai, S.; Dennis, V.A.; Singh, S.R. Advances in Skin Regeneration Using Tissue Engineering. Int. J. Mol. Sci. 2017, 18, 789. [Google Scholar] [CrossRef]
- Belsky, K.; Smiell, J. Navigating the Regulatory Pathways and Requirements for Tissue-Engineered Products in the Treatment of Burns in the United States. J. Burn Care Res. 2021, 42, 774–784. [Google Scholar] [CrossRef]
- Lu, L.; Arbit, H.M.; Herrick, J.L.; Segovis, S.G.; Maran, A.; Yaszemski, M.J. Tissue engineered constructs: Perspectives on clinical translation. Ann. Biomed. Eng. 2015, 43, 796–804. [Google Scholar] [CrossRef]
- Ghahary, A.; Ghaffari, A. Role of keratinocyte-fibroblast cross-talk in development of hypertrophic scar. Wound Repair Regen. 2007, 15 (Suppl. S1), S46–S53. [Google Scholar] [CrossRef]
- Gottrup, F.; Agren, M.S.; Karlsmark, T. Models for use in wound healing research: A survey focusing on in vitro and in vivo adult soft tissue. Wound Repair Regen. 2000, 8, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Boyko, T.V.; Longaker, M.T.; Yang, G.P. Laboratory Models for the Study of Normal and Pathologic Wound Healing. Plast. Reconstr. Surg. 2017, 139, 654–662. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.; Sorkin, M.; Glotzbach, J.P.; Longaker, M.T.; Gurtner, G.C. Surgical approaches to create murine models of human wound healing. J. Biomed. Biotechnol. 2011, 2011, 969618. [Google Scholar] [CrossRef] [PubMed]
- Abdullahi, A.; Amini-Nik, S.; Jeschke, M.G. Animal models in burn research. Cell. Mol. Life Sci. CMLS 2014, 71, 3241–3255. [Google Scholar] [CrossRef] [Green Version]
- Grose, R.; Werner, S. Wound-healing studies in transgenic and knockout mice. Mol. Biotechnol. 2004, 28, 147–166. [Google Scholar] [CrossRef]
- Mestas, J.; Hughes, C.C. Of mice and not men: Differences between mouse and human immunology. J. Immunol. 2004, 172, 2731–2738. [Google Scholar] [CrossRef] [Green Version]
- Zomer, H.D.; Trentin, A.G. Skin wound healing in humans and mice: Challenges in translational research. J. Dermatol. Sci. 2018, 90, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Davidson, J.M. Animal models for wound repair. Arch. Dermatol. Res. 1998, 290, S1–S11. [Google Scholar] [CrossRef]
- Cross, S.E.; Naylor, I.L.; Coleman, R.A.; Teo, T.C. An experimental model to investigate the dynamics of wound contraction. Br. J. Plast. Surg. 1995, 48, 189–197. [Google Scholar] [CrossRef]
- Boyce, S.T. Methods for the Serum-Free Culture of Keratinocytes and Transplantation of Collagen-GAG-Based Skin Substitutes. Methods Mol. Med. 1999, 18, 365–389. [Google Scholar] [CrossRef]
- Boyce, S.T.; Foreman, T.J.; English, K.B.; Stayner, N.; Cooper, M.L.; Sakabu, S.; Hansbrough, J.F. Skin wound closure in athymic mice with cultured human cells, biopolymers, and growth factors. Surgery 1991, 110, 866–876. [Google Scholar] [PubMed]
- Boyce, S.T.; Lloyd, C.M.; Kleiner, M.C.; Swope, V.B.; Abdel-Malek, Z.; Supp, D.M. Restoration of cutaneous pigmentation by transplantation to mice of isogeneic human melanocytes in dermal-epidermal engineered skin substitutes. Pigment Cell Melanoma Res. 2017, 30, 531–540. [Google Scholar] [CrossRef] [PubMed]
- van Kilsdonk, J.W.; van den Bogaard, E.H.; Jansen, P.A.; Bos, C.; Bergers, M.; Schalkwijk, J. An in vitro wound healing model for evaluation of dermal substitutes. Wound Repair Regen. 2013, 21, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Hansbrough, J.F.; Boyce, S.T.; Cooper, M.L.; Foreman, T.J. Burn wound closure with cultured autologous keratinocytes and fibroblasts attached to a collagen-glycosaminoglycan substrate. JAMA 1989, 262, 2125–2130. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Santamaría, L.; Guerrero-Aspizua, S.; Del Río, M. Skin bioengineering: Preclinical and clinical applications. Actas Dermosifiliogr. 2012, 103, 5–11. [Google Scholar] [CrossRef]
- Schenck, T.L.; Chávez, M.N.; Condurache, A.P.; Hopfner, U.; Rezaeian, F.; Machens, H.G.; Egaña, J.T. A full skin defect model to evaluate vascularization of biomaterials in vivo. J. Vis. Exp. 2014, 90, e51428. [Google Scholar] [CrossRef] [Green Version]
- Larcher, F.; Dellambra, E.; Rico, L.; Bondanza, S.; Murillas, R.; Cattoglio, C.; Mavilio, F.; Jorcano, J.L.; Zambruno, G.; Del Rio, M. Long-term engraftment of single genetically modified human epidermal holoclones enables safety pre-assessment of cutaneous gene therapy. Mol. Ther. 2007, 15, 1670–1676. [Google Scholar] [CrossRef]
- Escámez, M.J.; García, M.; Larcher, F.; Meana, A.; Muñoz, E.; Jorcano, J.L.; Del Río, M. An in vivo model of wound healing in genetically modified skin-humanized mice. J. Investig. Dermatol. 2004, 123, 1182–1191. [Google Scholar] [CrossRef] [Green Version]
- Cheshire, P.A.; Herson, M.R.; Cleland, H.; Akbarzadeh, S. Artificial dermal templates: A comparative study of NovoSorb™ Biodegradable Temporising Matrix (BTM) and Integra(®) Dermal Regeneration Template (DRT). Burns 2016, 42, 1088–1096. [Google Scholar] [CrossRef]
- Killat, J.; Reimers, K.; Choi, C.Y.; Jahn, S.; Vogt, P.M.; Radtke, C. Cultivation of keratinocytes and fibroblasts in a three-dimensional bovine collagen-elastin matrix (Matriderm®) and application for full thickness wound coverage in vivo. Int. J. Mol. Sci. 2013, 14, 14460–14474. [Google Scholar] [CrossRef]
- Murphy, S.V.; Skardal, A.; Song, L.; Sutton, K.; Haug, R.; Mack, D.L.; Jackson, J.; Soker, S.; Atala, A. Solubilized Amnion Membrane Hyaluronic Acid Hydrogel Accelerates Full-Thickness Wound Healing. Stem Cells Transl. Med. 2017, 6, 2020–2032. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, D.; Oberdoerfer, D.; Fernandes, M.C.; Meurer, R.T.; Pereira-Filho, G.A.; Cruz, P.; Vargas, M.; Chem, R.C.; Camassola, M.; Nardi, N.B. Mesenchymal stem cells combined with an artificial dermal substitute improve repair in full-thickness skin wounds. Burns 2012, 38, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Wosgrau, A.C.; Jeremias Tda, S.; Leonardi, D.F.; Pereima, M.J.; Di Giunta, G.; Trentin, A.G. Comparative experimental study of wound healing in mice: Pelnac versus Integra. PLoS ONE 2015, 10, e0120322. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Mithieux, S.M.; Kong, Y.; Wang, X.Q.; Chong, C.; Fathi, A.; Dehghani, F.; Panas, E.; Kemnitzer, J.; Daniels, R.; et al. Tropoelastin incorporation into a dermal regeneration template promotes wound angiogenesis. Adv. Healthc. Mater. 2015, 4, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Dunn, L.; Prosser, H.C.; Tan, J.T.; Vanags, L.Z.; Ng, M.K.; Bursill, C.A. Murine model of wound healing. J. Vis. Exp. 2013, 75, e50265. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Ge, J.; Tredget, E.E.; Wu, Y. The mouse excisional wound splinting model, including applications for stem cell transplantation. Nat. Protoc. 2013, 8, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Galiano, R.D.; Michaels, J.t.; Dobryansky, M.; Levine, J.P.; Gurtner, G.C. Quantitative and reproducible murine model of excisional wound healing. Wound Repair Regen. 2004, 12, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Michael, S.; Sorg, H.; Peck, C.T.; Koch, L.; Deiwick, A.; Chichkov, B.; Vogt, P.M.; Reimers, K. Tissue engineered skin substitutes created by laser-assisted bioprinting form skin-like structures in the dorsal skin fold chamber in mice. PLoS ONE 2013, 8, e57741. [Google Scholar] [CrossRef]
- Beaudoin Cloutier, C.; Goyer, B.; Perron, C.; Guignard, R.; Larouche, D.; Moulin, V.J.; Germain, L.; Gauvin, R.; Auger, F.A. In Vivo Evaluation and Imaging of a Bilayered Self-Assembled Skin Substitute Using a Decellularized Dermal Matrix Grafted on Mice. Tissue Eng. Part A 2017, 23, 313–322. [Google Scholar] [CrossRef]
- Böttcher-Haberzeth, S.; Biedermann, T.; Reichmann, E. Tissue engineering of skin. Burns 2010, 36, 450–460. [Google Scholar] [CrossRef]
- Fusenig, N.E.; Breitkreutz, D.; Dzarlieva, R.T.; Boukamp, P.; Bohnert, A.; Tilgen, W. Growth and differentiation characteristics of transformed keratinocytes from mouse and human skin in vitro and in vivo. J. Investig. Dermatol. 1983, 81, 168s–175s. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lichti, U.; Anders, J.; Yuspa, S.H. Isolation and short-term culture of primary keratinocytes, hair follicle populations and dermal cells from newborn mice and keratinocytes from adult mice for in vitro analysis and for grafting to immunodeficient mice. Nat. Protoc. 2008, 3, 799–810. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; Sadri, A.R.; Belo, C.; Amini-Nik, S. A Surgical Device to Study the Efficacy of Bioengineered Skin Substitutes in Mice Wound Healing Models. Tissue Eng. Part C Methods 2017, 23, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Hüging, M.; Biedermann, T.; Sobrio, M.; Meyer, S.; Böttcher-Haberzeth, S.; Manuel, E.; Horst, M.; Hynes, S.; Reichmann, E.; Schiestl, C.; et al. The Effect of Wound Dressings on a Bio-Engineered Human Dermo-Epidermal Skin Substitute in a Rat Model. J. Burn Care Res. 2017, 38, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Klar, A.S.; Biedermann, T.; Simmen-Meuli, C.; Reichmann, E.; Meuli, M. Comparison of in vivo immune responses following transplantation of vascularized and non-vascularized human dermo-epidermal skin substitutes. Pediatr. Surg. Int. 2017, 33, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Klar, A.S.; Güven, S.; Biedermann, T.; Luginbühl, J.; Böttcher-Haberzeth, S.; Meuli-Simmen, C.; Meuli, M.; Martin, I.; Scherberich, A.; Reichmann, E. Tissue-engineered dermo-epidermal skin grafts prevascularized with adipose-derived cells. Biomaterials 2014, 35, 5065–5078. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Xiao, J.; Leung, W.Y.; Lu, W.W.; Hu, Y.; Luk, K.D. The dorsal skinfold chamber: A versatile tool for preclinical research in tissue engineering and regenerative medicine. Eur. Cell Mater. 2016, 32, 216–227. [Google Scholar] [CrossRef]
- Schreiter, J.; Meyer, S.; Schmidt, C.; Schulz, R.M.; Langer, S. Dorsal skinfold chamber models in mice. GMS Interdiscip. Plast. Reconstr. Surg. DGPW 2017, 6, Doc10. [Google Scholar] [CrossRef]
- Michael, S.; Sorg, H.; Peck, C.T.; Reimers, K.; Vogt, P.M. The mouse dorsal skin fold chamber as a means for the analysis of tissue engineered skin. Burns 2013, 39, 82–88. [Google Scholar] [CrossRef]
- Esteban-Vives, R.; Young, M.T.; Ziembicki, J.; Corcos, A.; Gerlach, J.C. Effects of wound dressings on cultured primary keratinocytes. Burns 2016, 42, 81–90. [Google Scholar] [CrossRef]
- Burd, A.; Kwok, C.H.; Hung, S.C.; Chan, H.S.; Gu, H.; Lam, W.K.; Huang, L. A comparative study of the cytotoxicity of silver-based dressings in monolayer cell, tissue explant, and animal models. Wound Repair Regen. 2007, 15, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Duc, Q.; Breetveld, M.; Middelkoop, E.; Scheper, R.J.; Ulrich, M.M.; Gibbs, S. A cytotoxic analysis of antiseptic medication on skin substitutes and autograft. Br. J. Dermatol. 2007, 157, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Matoušková, E.; Mestak, O. The effect of different biologic and biosynthetic wound covers on keratinocyte growth, stratification and differentiation in vitro. J. Tissue Eng. 2014, 5, 2041731414554966. [Google Scholar] [CrossRef] [PubMed]
- Kromka, W.; Cameron, M.; Fathi, R. Tie-Over Bolster Dressings vs Basting Sutures for the Closure of Full-Thickness Skin Grafts: A Review of the Literature. J. Cutan. Med. Surg. 2018, 22, 602–606. [Google Scholar] [CrossRef]
- Balls, M. It’s Time to Reconsider The Principles of Humane Experimental Technique. Altern. Lab. Anim. 2020, 48, 40–46. [Google Scholar] [CrossRef]
- Xu, W.; Germain, L.; Goulet, F.; Auger, F.A. Permanent grafting of living skin substitutes: Surgical parameters to control for successful results. J. Burn Care Rehabil. 1996, 17, 7–13. [Google Scholar] [CrossRef]
- López Valle, C.A.; Germain, L.; Rouabhia, M.; Xu, W.; Guignard, R.; Goulet, F.; Auger, F.A. Grafting on nude mice of living skin equivalents produced using human collagens. Transplantation 1996, 62, 317–323. [Google Scholar] [CrossRef]
- López Valle, C.A.; Glaude, P.; Auger, F.A. Surgical model for in vivo evaluation of cultured epidermal sheets in mice. Plast. Reconstr. Surg. 1992, 89, 139–143. [Google Scholar] [CrossRef]
- Pouliot, R.; Larouche, D.; Auger, F.A.; Juhasz, J.; Xu, W.; Li, H.; Germain, L. Reconstructed human skin produced in vitro and grafted on athymic mice. Transplantation 2002, 73, 1751–1757. [Google Scholar] [CrossRef]
- Shimizu, I.; MacFarlane, D.F. Full-thickness skin grafts may not need tie-over bolster dressings. Dermatol. Surg. Off. Publ. Am. Soc. Dermatol. Surg. 2013, 39, 726–728. [Google Scholar] [CrossRef]
- Yuki, A.; Takenouchi, T.; Takatsuka, S.; Fujikawa, H.; Abe, R. Investigating the use of tie-over dressing after skin grafting. J. Dermatol. 2017, 44, 1317–1319. [Google Scholar] [CrossRef] [PubMed]
- Boyce, S.T.; Supp, A.P.; Swope, V.B.; Warden, G.D. Vitamin C regulates keratinocyte viability, epidermal barrier, and basement membrane in vitro, and reduces wound contraction after grafting of cultured skin substitutes. J. Investig. Dermatol. 2002, 118, 565–572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Supp, D.M.; Hahn, J.M.; Glaser, K.; McFarland, K.L.; Boyce, S.T. Deep and superficial keloid fibroblasts contribute differentially to tissue phenotype in a novel in vivo model of keloid scar. Plast. Reconstr. Surg. 2012, 129, 1259–1271. [Google Scholar] [CrossRef] [PubMed]
- Windsor, M.L.; Eisenberg, M.; Gordon-Thomson, C.; Moore, G.P. A novel model of wound healing in the SCID mouse using a cultured human skin substitute. Australas. J. Dermatol. 2009, 50, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Mayumi, H.; Nomoto, K.; Good, R.A. A surgical technique for experimental free skin grafting in mice. Jpn. J. Surg. 1988, 18, 548–557. [Google Scholar] [CrossRef]
- ImageJ. Available online: https://imagej.nih.gov/ij/ (accessed on 22 January 2022).
- GraphPad Software, Inc. Available online: https://www.graphpad.com (accessed on 22 January 2022).




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cartier, A.; Barbier, M.A.; Larouche, D.; Morissette, A.; Bussières, A.; Montalin, L.; Beaudoin Cloutier, C.; Germain, L. Tie-Over Bolster Pressure Dressing Improves Outcomes of Skin Substitutes Xenografts on Athymic Mice. Int. J. Mol. Sci. 2022, 23, 5507. https://doi.org/10.3390/ijms23105507
Cartier A, Barbier MA, Larouche D, Morissette A, Bussières A, Montalin L, Beaudoin Cloutier C, Germain L. Tie-Over Bolster Pressure Dressing Improves Outcomes of Skin Substitutes Xenografts on Athymic Mice. International Journal of Molecular Sciences. 2022; 23(10):5507. https://doi.org/10.3390/ijms23105507
Chicago/Turabian StyleCartier, Andréanne, Martin A. Barbier, Danielle Larouche, Amélie Morissette, Ariane Bussières, Livia Montalin, Chanel Beaudoin Cloutier, and Lucie Germain. 2022. "Tie-Over Bolster Pressure Dressing Improves Outcomes of Skin Substitutes Xenografts on Athymic Mice" International Journal of Molecular Sciences 23, no. 10: 5507. https://doi.org/10.3390/ijms23105507





