Cerebral Organoids for Modeling of HSV-1-Induced-Amyloid β Associated Neuropathology and Phenotypic Rescue
Abstract
:1. Introduction
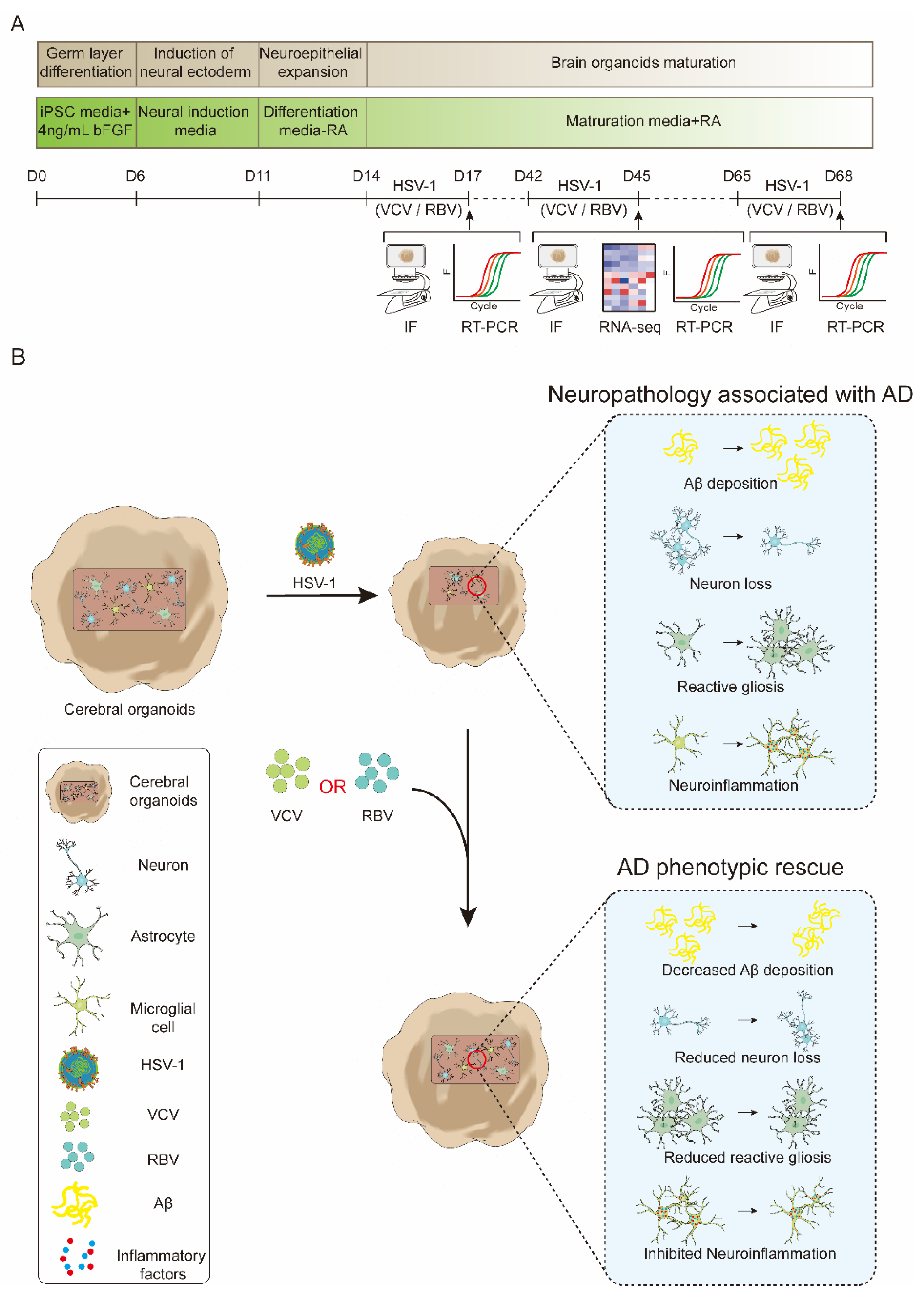
2. Results
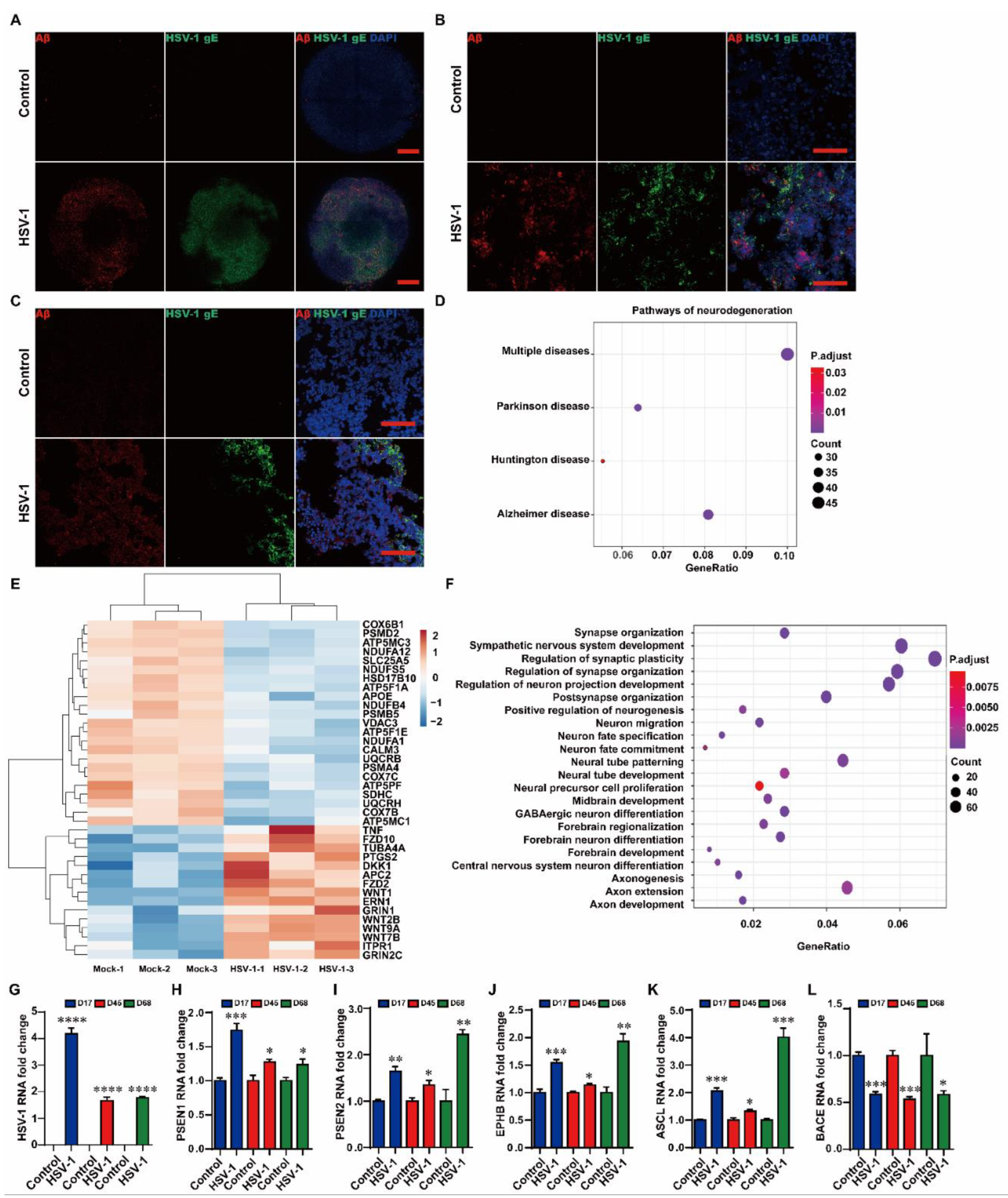
2.1. HSV-1 Led to Aβ Deposition in the Cerebral Organoids
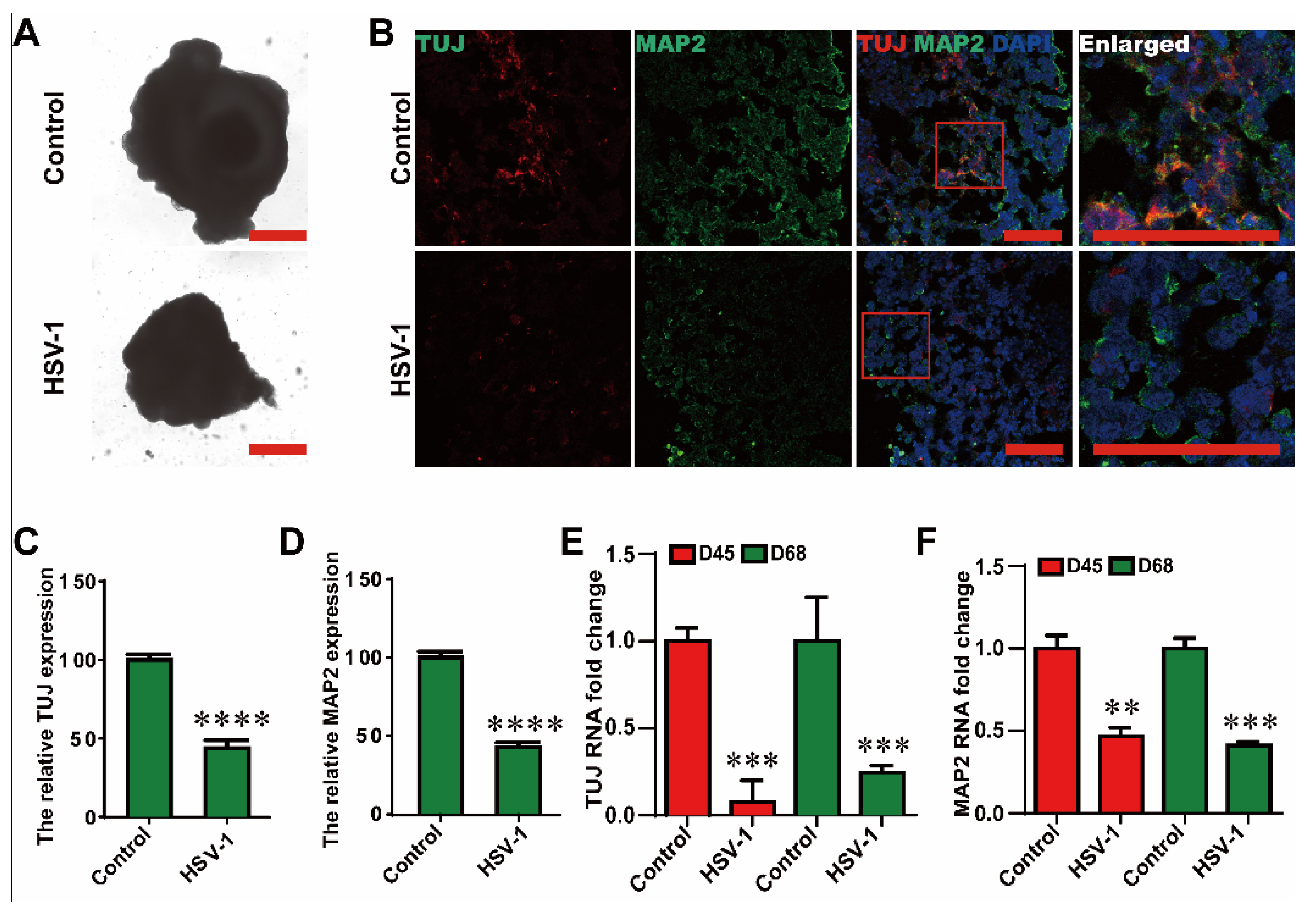
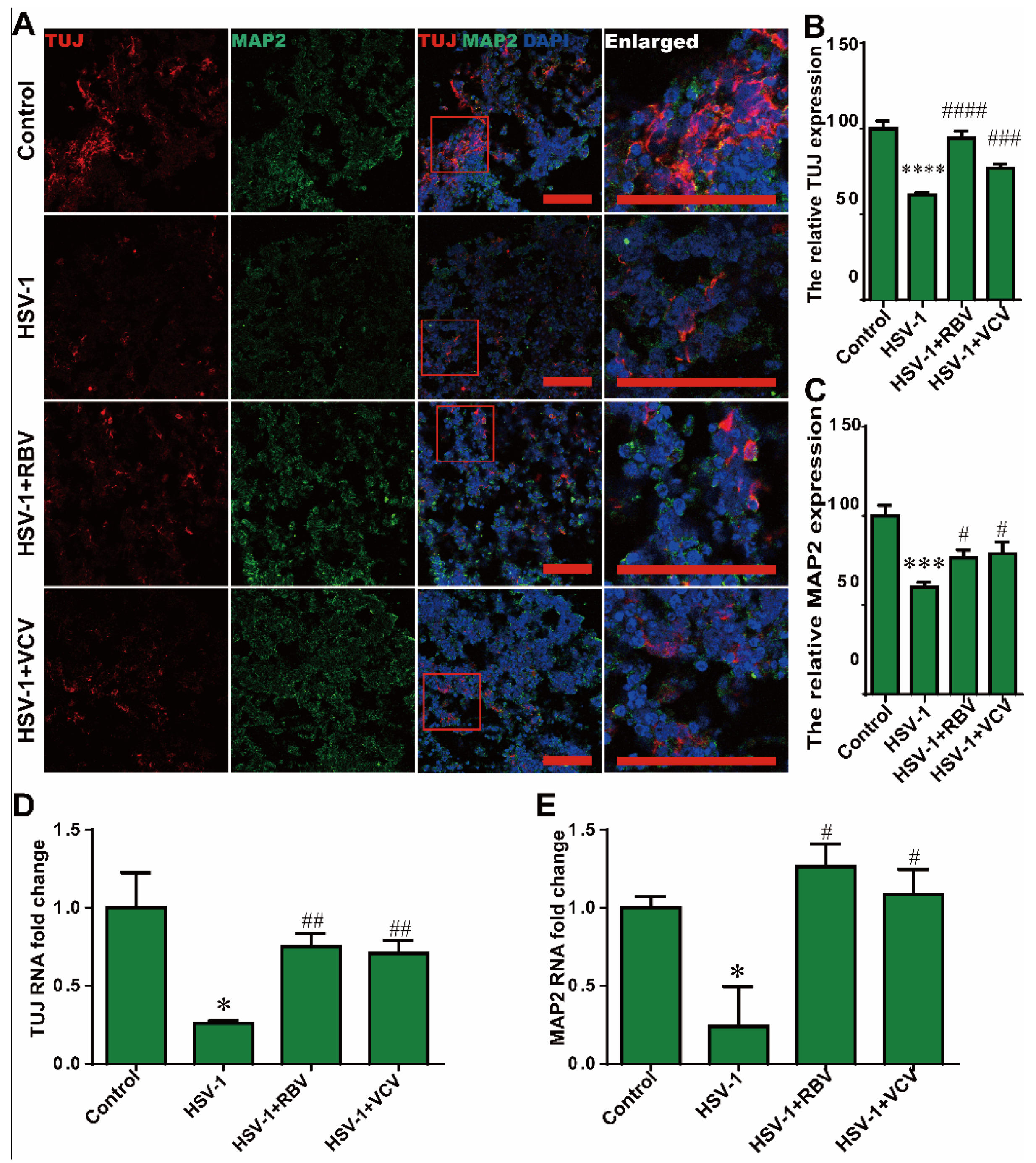
2.2. HSV-1 Infection Resulted in the Neuron Loss
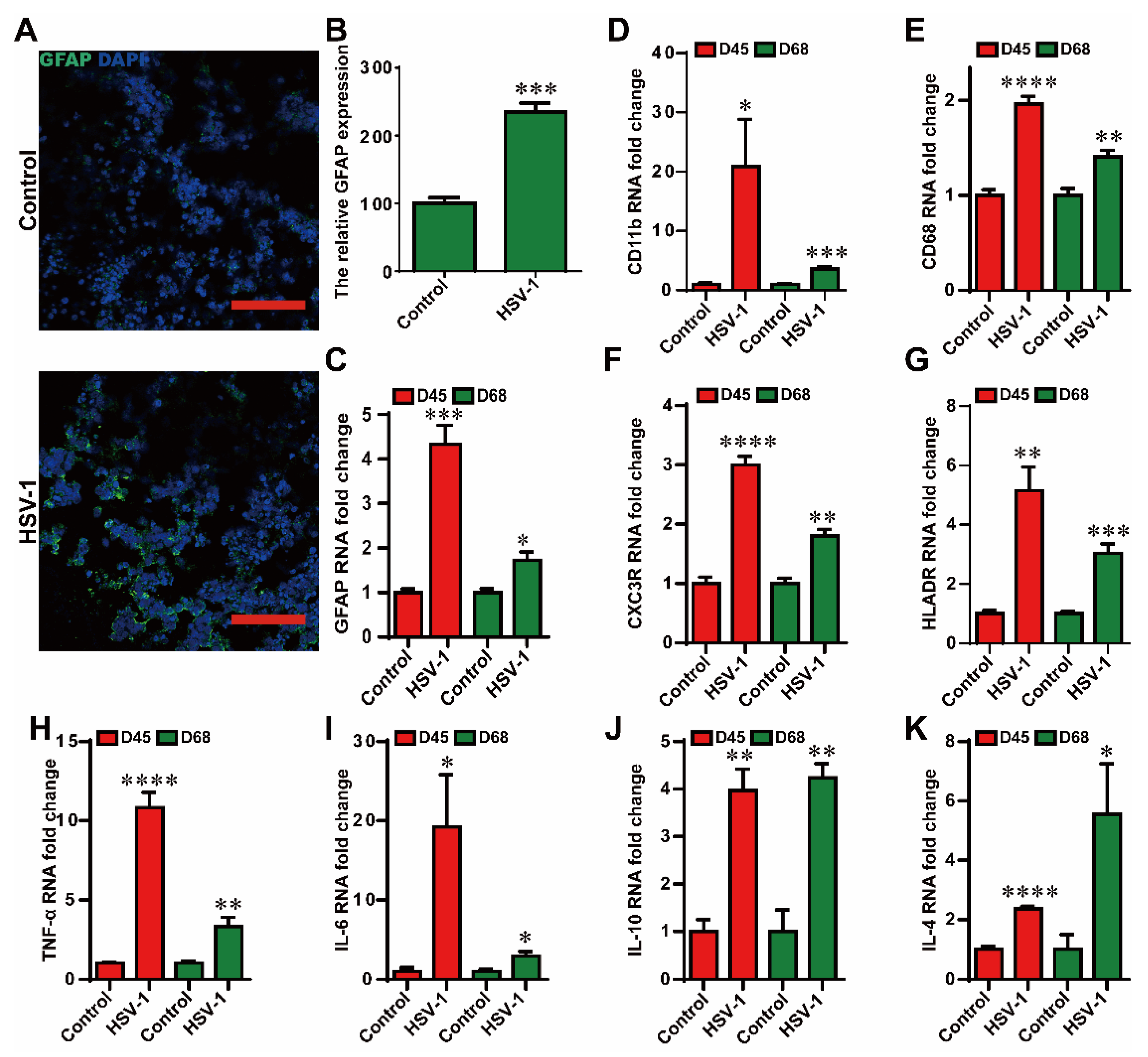
2.3. HSV-1 Infection Led to Reactive Gliosis and Neuroinflammation in the Cerebral Organoids
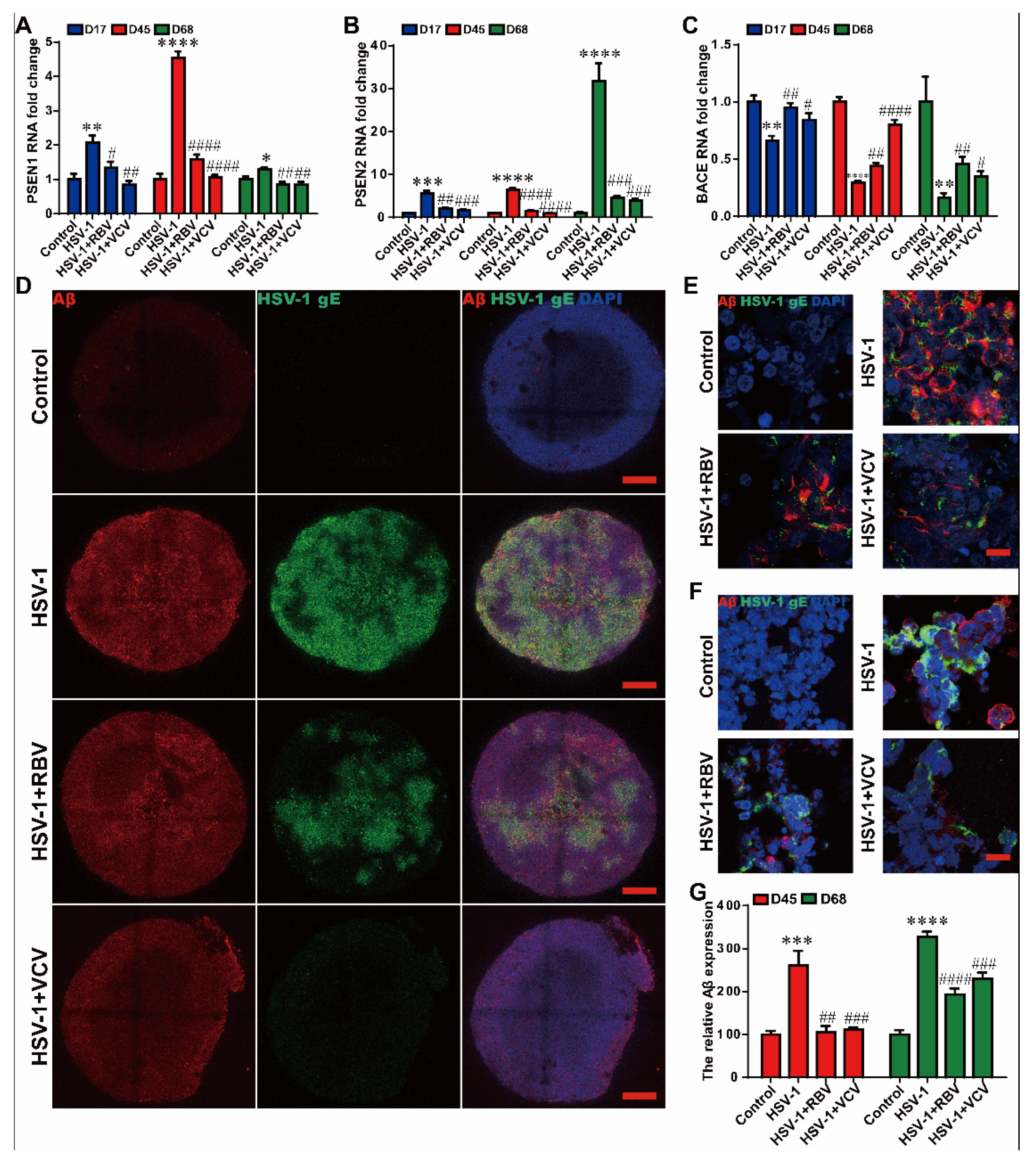
2.4. RBV and VCV Treatments Resulted in Decreased Aβ Deposition and Normalized AD-Mediator Expression in the Cerebral Organoids
2.5. RBV and VCV Treatments Reduced Reactive Gliosis and Neuroinflammation in the Cerebral Organoids
2.6. RBV and VCV Treatments Reduced the Neuron Loss
3. Discussion
4. Materials and Methods
4.1. Generation of Human Cerebral Organoids
4.2. HSV-1 Infection and Phenotypic Rescue
4.3. Histology and Immunofluorescence
4.4. Whole-Mount Immunostaining of Organoids
4.5. RT-PCR
4.6. RNA-Seq and Data Analysis
4.7. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Alzheimer’s Association. 2016 Alzheimer’s disease facts and figures. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2016, 12, 459–509. [Google Scholar] [CrossRef] [PubMed]
- Najm, R.; Jones, E.A.; Huang, Y. Apolipoprotein E4, inhibitory network dysfunction, and Alzheimer’s disease. Mol. Neurodegener. 2019, 14, 24. [Google Scholar] [CrossRef] [PubMed]
- Dallemagne, P.; Rochais, C. Facing the complexity of Alzheimer’s disease. Future Med. Chem. 2020, 12, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Laval, K.; Enquist, L.W. The Potential Role of Herpes Simplex Virus Type 1 and Neuroinflammation in the Pathogenesis of Alzheimer’s Disease. Front. Neurol. 2021, 12, 658695. [Google Scholar] [CrossRef] [PubMed]
- Carter, C.J. Genetic, Transcriptome, Proteomic, and Epidemiological Evidence for Blood-Brain Barrier Disruption and Polymicrobial Brain Invasion as Determinant Factors in Alzheimer’s Disease. J. Alzheimer’s Dis. Rep. 2017, 1, 125–157. [Google Scholar] [CrossRef]
- Ashraf, G.M.; Tarasov, V.V.; Makhmutovsmall, C.A.; Chubarev, V.N.; Avila-Rodriguez, M.; Bachurin, S.O.; Aliev, G. The Possibility of an Infectious Etiology of Alzheimer Disease. Mol. Neurobiol. 2019, 56, 4479–4491. [Google Scholar] [CrossRef]
- Xu, F.; Sternberg, M.R.; Kottiri, B.J.; McQuillan, G.M.; Lee, F.K.; Nahmias, A.J.; Berman, S.M.; Markowitz, L.E. Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. JAMA 2006, 296, 964–973. [Google Scholar] [CrossRef] [Green Version]
- Protto, V.; Marcocci, M.E.; Miteva, M.T.; Piacentini, R.; Li Puma, D.D.; Grassi, C.; Palamara, A.T.; De Chiara, G. Role of HSV-1 in Alzheimer’s disease pathogenesis: A challenge for novel preventive/therapeutic strategies. Curr. Opin. Pharmacol. 2022, 63, 102200. [Google Scholar] [CrossRef]
- Readhead, B.; Haure-Mirande, J.V.; Funk, C.C.; Richards, M.A.; Shannon, P.; Haroutunian, V.; Sano, M.; Liang, W.S.; Beckmann, N.D.; Price, N.D.; et al. Multiscale Analysis of Independent Alzheimer’s Cohorts Finds Disruption of Molecular, Genetic, and Clinical Networks by Human Herpesvirus. Neuron 2018, 99, 64–82.e7. [Google Scholar] [CrossRef] [Green Version]
- Tzeng, N.S.; Chung, C.H.; Lin, F.H.; Chiang, C.P.; Yeh, C.B.; Huang, S.Y.; Lu, R.B.; Chang, H.A.; Kao, Y.C.; Yeh, H.W.; et al. Anti-herpetic Medications and Reduced Risk of Dementia in Patients with Herpes Simplex Virus Infections-a Nationwide, Population-Based Cohort Study in Taiwan. Neurother. J. Am. Soc. Exp. Neuro Ther. 2018, 15, 417–429. [Google Scholar] [CrossRef] [Green Version]
- Li Puma, D.D.; Piacentini, R.; Leone, L.; Gironi, K.; Marcocci, M.E.; De Chiara, G.; Palamara, A.T.; Grassi, C. Herpes Simplex Virus Type-1 Infection Impairs Adult Hippocampal Neurogenesis via Amyloid-beta Protein Accumulation. Stem Cells 2019, 37, 1467–1480. [Google Scholar] [CrossRef] [PubMed]
- De Chiara, G.; Piacentini, R.; Fabiani, M.; Mastrodonato, A.; Marcocci, M.E.; Limongi, D.; Napoletani, G.; Protto, V.; Coluccio, P.; Celestino, I.; et al. Recurrent herpes simplex virus-1 infection induces hallmarks of neurodegeneration and cognitive deficits in mice. PLoS Pathog. 2019, 15, e1007617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ezzat, K.; Pernemalm, M.; Palsson, S.; Roberts, T.C.; Jarver, P.; Dondalska, A.; Bestas, B.; Sobkowiak, M.J.; Levanen, B.; Skold, M.; et al. The viral protein corona directs viral pathogenesis and amyloid aggregation. Nat. Commun. 2019, 10, 2331. [Google Scholar] [CrossRef] [Green Version]
- Eimer, W.A.; Vijaya Kumar, D.K.; Navalpur Shanmugam, N.K.; Rodriguez, A.S.; Mitchell, T.; Washicosky, K.J.; Gyorgy, B.; Breakefield, X.O.; Tanzi, R.E.; Moir, R.D. Alzheimer’s Disease-Associated beta-Amyloid Is Rapidly Seeded by Herpesviridae to Protect against Brain Infection. Neuron 2018, 99, 56–63.e3. [Google Scholar] [CrossRef] [Green Version]
- Yakoub, A.M.; Sadek, M. Analysis of Synapses in Cerebral Organoids. Cell Transpl. 2019, 28, 1173–1182. [Google Scholar] [CrossRef] [Green Version]
- Velasco, S.; Kedaigle, A.J.; Simmons, S.K.; Nash, A.; Rocha, M.; Quadrato, G.; Paulsen, B.; Nguyen, L.; Adiconis, X.; Regev, A.; et al. Individual brain organoids reproducibly form cell diversity of the human cerebral cortex. Nature 2019, 570, 523–527. [Google Scholar] [CrossRef]
- Lopez-Tobon, A.; Villa, C.E.; Cheroni, C.; Trattaro, S.; Caporale, N.; Conforti, P.; Iennaco, R.; Lachgar, M.; Rigoli, M.T.; Marco de la Cruz, B.; et al. Human Cortical Organoids Expose a Differential Function of GSK3 on Cortical Neurogenesis. Stem Cell Rep. 2019, 13, 847–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qian, X.; Nguyen, H.N.; Song, M.M.; Hadiono, C.; Ogden, S.C.; Hammack, C.; Yao, B.; Hamersky, G.R.; Jacob, F.; Zhong, C.; et al. Brain-Region-Specific Organoids Using Mini-bioreactors for Modeling ZIKV Exposure. Cell 2016, 165, 1238–1254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerakis, Y.; Hetz, C. Brain organoids: A next step for humanized Alzheimer’s disease models? Mol. Psychiatry 2019, 24, 474–478. [Google Scholar] [CrossRef] [Green Version]
- Lancaster, M.A.; Renner, M.; Martin, C.A.; Wenzel, D.; Bicknell, L.S.; Hurles, M.E.; Homfray, T.; Penninger, J.M.; Jackson, A.P.; Knoblich, J.A. Cerebral organoids model human brain development and microcephaly. Nature 2013, 501, 373–379. [Google Scholar] [CrossRef]
- Gonzalez, C.; Armijo, E.; Bravo-Alegria, J.; Becerra-Calixto, A.; Mays, C.E.; Soto, C. Modeling amyloid beta and tau pathology in human cerebral organoids. Mol. Psychiatry 2018, 23, 2363–2374. [Google Scholar] [CrossRef] [PubMed]
- Qiao, H.; Guo, M.; Shang, J.; Zhao, W.; Wang, Z.; Liu, N.; Li, B.; Zhou, Y.; Wu, Y.; Chen, P. Herpes simplex virus type 1 infection leads to neurodevelopmental disorder-associated neuropathological changes. PLoS Pathog. 2020, 16, e1008899. [Google Scholar] [CrossRef] [PubMed]
- D’Aiuto, L.; Bloom, D.C.; Naciri, J.N.; Smith, A.; Edwards, T.G.; McClain, L.; Callio, J.A.; Jessup, M.; Wood, J.; Chowdari, K.; et al. Modeling Herpes Simplex Virus 1 Infections in Human Central Nervous System Neuronal Cells Using Two- and Three-Dimensional Cultures Derived from Induced Pluripotent Stem Cells. J. Virol. 2019, 93, e00111-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palomer, E.; Buechler, J.; Salinas, P.C. Wnt Signaling Deregulation in the Aging and Alzheimer’s Brain. Front. Cell. Neurosci. 2019, 13, 227. [Google Scholar] [CrossRef]
- Belloy, M.E.; Napolioni, V.; Greicius, M.D. A Quarter Century of APOE and Alzheimer’s Disease: Progress to Date and the Path Forward. Neuron 2019, 101, 820–838. [Google Scholar] [CrossRef] [Green Version]
- Ng, A.; Tam, W.W.; Zhang, M.W.; Ho, C.S.; Husain, S.F.; McIntyre, R.S.; Ho, R.C. IL-1β, IL-6, TNF-α and CRP in Elderly Patients with Depression or Alzheimer’s disease: Systematic Review and Meta-Analysis. Sci. Rep. 2018, 8, 12050. [Google Scholar] [CrossRef]
- Piacentini, R.; De Chiara, G.; Li Puma, D.D.; Ripoli, C.; Marcocci, M.E.; Garaci, E.; Palamara, A.T.; Grassi, C. HSV-1 and Alzheimer’s disease: More than a hypothesis. Front. Pharmacol. 2014, 5, 97. [Google Scholar] [CrossRef]
- Harris, S.A.; Harris, E.A. Herpes Simplex Virus Type 1 and Other Pathogens are Key Causative Factors in Sporadic Alzheimer’s Disease. J. Alzheimer’s Dis. JAD 2015, 48, 319–353. [Google Scholar] [CrossRef] [Green Version]
- Martin, C.; Aguila, B.; Araya, P.; Vio, K.; Valdivia, S.; Zambrano, A.; Concha, M.I.; Otth, C. Inflammatory and neurodegeneration markers during asymptomatic HSV-1 reactivation. J. Alzheimer’s Dis. JAD 2014, 39, 849–859. [Google Scholar] [CrossRef]
- Miklossy, J. Emerging roles of pathogens in Alzheimer disease. Expert Rev. Mol. Med. 2011, 13, e30. [Google Scholar] [CrossRef] [Green Version]
- Mangold, C.A.; Szpara, M.L. Persistent Infection with Herpes Simplex Virus 1 and Alzheimer’s Disease—A Call to Study How Variability in Both Virus and Host may Impact Disease. Viruses 2019, 11, 966. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nilsson, P.; Iwata, N.; Muramatsu, S.; Tjernberg, L.O.; Winblad, B.; Saido, T.C. Gene therapy in Alzheimer’s disease—Potential for disease modification. J. Cell. Mol. Med. 2010, 14, 741–757. [Google Scholar] [CrossRef] [Green Version]
- Baranello, R.J.; Bharani, K.L.; Padmaraju, V.; Chopra, N.; Lahiri, D.K.; Greig, N.H.; Pappolla, M.A.; Sambamurti, K. Amyloid-beta protein clearance and degradation (ABCD) pathways and their role in Alzheimer’s disease. Curr. Alzheimer Res. 2015, 12, 32–46. [Google Scholar] [CrossRef] [Green Version]
- Mullane, K.; Williams, M. Alzheimer’s disease (AD) therapeutics—2: Beyond amyloid—Re-defining AD and its causality to discover effective therapeutics. Biochem. Pharmacol. 2018, 158, 376–401. [Google Scholar] [CrossRef] [PubMed]
- Linard, M.; Letenneur, L.; Garrigue, I.; Doize, A.; Dartigues, J.F.; Helmer, C. Interaction between APOE4 and herpes simplex virus type 1 in Alzheimer’s disease. Alzheimer’s Dement. J. Alzheimer’s Assoc. 2020, 16, 200–208. [Google Scholar] [CrossRef]
- Panza, F.; Solfrizzi, V.; Imbimbo, B.P.; Giannini, M.; Santamato, A.; Seripa, D.; Logroscino, G. Efficacy and safety studies of gantenerumab in patients with Alzheimer’s disease. Expert Rev. Neurother. 2014, 14, 973–986. [Google Scholar] [CrossRef]
- Panza, F.; Solfrizzi, V.; Imbimbo, B.P.; Tortelli, R.; Santamato, A.; Logroscino, G. Amyloid-based immunotherapy for Alzheimer’s disease in the time of prevention trials: The way forward. Expert Rev. Clin. Immunol. 2014, 10, 405–419. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.L.; Tong, G.; Ballard, C. Treatment Combinations for Alzheimer’s Disease: Current and Future Pharmacotherapy Options. J. Alzheimer’s Dis. JAD 2019, 67, 779–794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joe, E.; Ringman, J.M. Cognitive symptoms of Alzheimer’s disease: Clinical management and prevention. BMJ 2019, 367, l6217. [Google Scholar] [CrossRef] [Green Version]
- Devanand, D.P. Viral Hypothesis and Antiviral Treatment in Alzheimer’s Disease. Curr. Neurol. Neurosci. Rep. 2018, 18, 55. [Google Scholar] [CrossRef]
- Lin, Z.; Li, Y.; Gong, G.; Xia, Y.; Wang, C.; Chen, Y.; Hua, L.; Zhong, J.; Tang, Y.; Liu, X.; et al. Restriction of H1N1 influenza virus infection by selenium nanoparticles loaded with ribavirin via resisting caspase-3 apoptotic pathway. Int. J. Nanomed. 2018, 13, 5787–5797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galli, A.; Mens, H.; Gottwein, J.M.; Gerstoft, J.; Bukh, J. Antiviral Effect of Ribavirin against HCV Associated with Increased Frequency of G-to-A and C-to-U Transitions in Infectious Cell Culture Model. Sci. Rep. 2018, 8, 4619. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Xu, X.; Chen, J. Clinically relevant concentration of anti-viral drug ribavirin selectively targets pediatric osteosarcoma and increases chemosensitivity. Biochem. Biophys. Res. Commun. 2018, 506, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Cairns, D.M.; Rouleau, N.; Parker, R.N.; Walsh, K.G.; Gehrke, L.; Kaplan, D.L. A 3D human brain-like tissue model of herpes-induced Alzheimer’s disease. Sci. Adv. 2020, 6, eaay8828. [Google Scholar] [CrossRef]
- Vogt, N.M.; Hunt, J.F.; Adluru, N.; Dean, D.C.; Johnson, S.C.; Asthana, S.; Yu, J.J.; Alexander, A.L.; Bendlin, B.B. Cortical Microstructural Alterations in Mild Cognitive Impairment and Alzheimer’s Disease Dementia. Cereb. Cortex 2020, 30, 2948–2960. [Google Scholar] [CrossRef]
- Fjell, A.M.; McEvoy, L.; Holland, D.; Dale, A.M.; Walhovd, K.B.; Alzheimer’s Disease Neuroimaging, I. What is normal in normal aging? Effects of aging, amyloid and Alzheimer’s disease on the cerebral cortex and the hippocampus. Prog. Neurobiol. 2014, 117, 20–40. [Google Scholar] [CrossRef] [Green Version]
- Meyer, K.; Feldman, H.M.; Lu, T.; Drake, D.; Lim, E.T.; Ling, K.H.; Bishop, N.A.; Pan, Y.; Seo, J.; Lin, Y.T.; et al. REST and Neural Gene Network Dysregulation in iPSC Models of Alzheimer’s Disease. Cell Rep. 2019, 26, 1112–1127.e9. [Google Scholar] [CrossRef] [Green Version]
- Gao, M.; Long, H.; Ma, W.; Liao, L.; Yang, X.; Zhou, Y.; Shan, D.; Huang, R.; Jian, F.; Wang, Y.; et al. The role of periodontal ASIC3 in orofacial pain induced by experimental tooth movement in rats. Eur. J. Orthod. 2016, 38, 577–583. [Google Scholar] [CrossRef] [Green Version]

| Medium Name | Component | Supplier | Identifier | Volume or Concentration |
|---|---|---|---|---|
| EB formation medium | mTeSR1 | Stem Cell Technologies, Vancouver, BC, Canada | 05850 | 50 mL |
| bFGF | Peprotech | 100-18B | 4 ng/mL | |
| ROCK inhibitor Y27632 | Stem Cell Technologies | 72304 | 50 μM | |
| Induction medium | DMEM/F12 | Gibco | 11330032 | 50 mL |
| N2 supplement (100×) | Invitrogen, MA, USA | 17502048 | 1× | |
| Non-Essential Amino Acids (100×) | Gibco | 11140050 | 1× | |
| GlutaMAX (100×) | Gibco | 35050061 | 1× | |
| Heparin | Sigma | H3149 | 1 μg/mL | |
| Neural expansion medium | DMEM/F12 | Gibco | 11330032 | 24 mL |
| Neurobasal medium | Gibco | 21103049 | 24 mL | |
| N2 supplement (100×) | Gibco | 17502048 | 0.5× | |
| B27 supplement—Vitamin A (50×) | Gibco | 12587010 | 0.5× | |
| GlutaMAX (100×) | Gibco | 35050061 | 1× | |
| Non-Essential Amino Acids (100×) | Gibco | 11140050 | 0.5× | |
| Human insulin | Sigma-Aldrich, MO, USA | I9278-5ML | 2.5 µg/mL | |
| beta-mercaptoethanol | Merck, NJ, United States | 8057400005 | 25 nM | |
| Neural maturation medium | DMEM/F12 | Gibco | 11330032 | 24 mL |
| neurobasal medium | Gibco | 21103049 | 24 mL | |
| N2 supplement (100×) | Gibco | 17502048 | 0.5× | |
| B27 supplement + vitamin A (50×) | Gibco | 17504044 | 0.5× | |
| GlutaMAX (100×) | Gibco | 35050061 | 1× | |
| Non-Essential Amino Acids (100×) | Gibco | 11140050 | 0.5× | |
| Human insulin | Sigma-Aldrich | I9278-5ML | 2.5 µg/mL | |
| beta-mercaptoethanol | Merck | 8057400005 | 25 nM |
| Antibodies | Dilution | Source | Identifier |
|---|---|---|---|
| HSV-1 gE | 1:200 | Abcam, Cambridge, UK | Ab6510 |
| Amyloid-β1–42 (Aβ) | 1:200 | Abcam | ab10148 |
| MAP2 | 1:200 | Abcam | ab11267 |
| TUJ | 1:200 | Abcam | ab7751 |
| TUJ | 1:200 | ABclonal Technology | A17913 |
| GFAP | 1:200 | Invitrogen | MA5-12023 |
| Genes | Forward Primers | Reverse Primers |
|---|---|---|
| HSV-1 | CTGCACGCACATGCTTGCCT | CTCGGGTGTAACGTTAGACC |
| PSEN1 | TGGCTACCATTAAGTCAGTCAGC | CCCACAGTCTCGGTATCTTCT |
| PSEN2 | CTGACCGCTATGTCTGTAGTGG | CTTCGCTCCGTATTTGAGGGT |
| BACE | CCATCCTTCCGCAGCAATA | CGTAGAAGCCCTCCATGATAAC |
| ASCL1 | AACAGTCAACCAACCCCATC | GCTGTGCGTGTTAGAGGTGA |
| TUJ | TGATGCGGTCGGGATACTC | TGGGCCAAGGGTCACTACAC |
| MAP2 | CAGGAGACAGAGATGAGAATTCC | CAGGAGTGATGGCAGTAGAC |
| CD11b | CCAGAGAATCCAGTGTGA | GTTATGCGAGGTCTTGATG |
| CD68 | CTTCTCTCATTCCCCTATGGACA | GAAGGACACATTGTACTCCACC |
| HLADR | CCCAGGGAAGACCACCTTT | CACCCTGCAGTCGTAAACGT |
| CX3CR1 | CTTACGATGGCACCCAGTGA | CAAGGCAGTCCAGGAGAGTT |
| GFAP | ACTGGCAGAGCTTGTTAGTG | AGTGACAGGAAGAGGTGAGA |
| TNF-α | GTGAGGAGGACGAACATC | GAGCCAGAAGAGGTTGAG |
| IL-6 | TGAGAGTAGTGAGGAACAAG | CGCAGAATGAGATGAGTTG |
| IL-10 | TGGAGCAGGTGAAGAATG | TCTATGTAGTTGATGAAGATGTC |
| IL-4 | CCTCTGTTCTTCCTGCTA | AGATGTCTGTTACGGTCAA |
| GAPDH | GGACCTGACCTGCCGTCTAG | GTAGCCCAGGATGCCCTTGA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qiao, H.; Zhao, W.; Guo, M.; Zhu, L.; Chen, T.; Wang, J.; Xu, X.; Zhang, Z.; Wu, Y.; Chen, P. Cerebral Organoids for Modeling of HSV-1-Induced-Amyloid β Associated Neuropathology and Phenotypic Rescue. Int. J. Mol. Sci. 2022, 23, 5981. https://doi.org/10.3390/ijms23115981
Qiao H, Zhao W, Guo M, Zhu L, Chen T, Wang J, Xu X, Zhang Z, Wu Y, Chen P. Cerebral Organoids for Modeling of HSV-1-Induced-Amyloid β Associated Neuropathology and Phenotypic Rescue. International Journal of Molecular Sciences. 2022; 23(11):5981. https://doi.org/10.3390/ijms23115981
Chicago/Turabian StyleQiao, Haowen, Wen Zhao, Moujian Guo, Lili Zhu, Tao Chen, Jibo Wang, Xiaodong Xu, Zhentao Zhang, Ying Wu, and Pu Chen. 2022. "Cerebral Organoids for Modeling of HSV-1-Induced-Amyloid β Associated Neuropathology and Phenotypic Rescue" International Journal of Molecular Sciences 23, no. 11: 5981. https://doi.org/10.3390/ijms23115981
APA StyleQiao, H., Zhao, W., Guo, M., Zhu, L., Chen, T., Wang, J., Xu, X., Zhang, Z., Wu, Y., & Chen, P. (2022). Cerebral Organoids for Modeling of HSV-1-Induced-Amyloid β Associated Neuropathology and Phenotypic Rescue. International Journal of Molecular Sciences, 23(11), 5981. https://doi.org/10.3390/ijms23115981






