Challenges and Future of Drug-Induced Liver Injury Research—Laboratory Tests
Abstract
:1. Introduction
2. Differential Diagnosis—Causality Assessment Methods
3. Drug-Induced Autoimmune Hepatitis and Autoimmune Hepatitis Differences and Overlaps in Presentation and Diagnosis
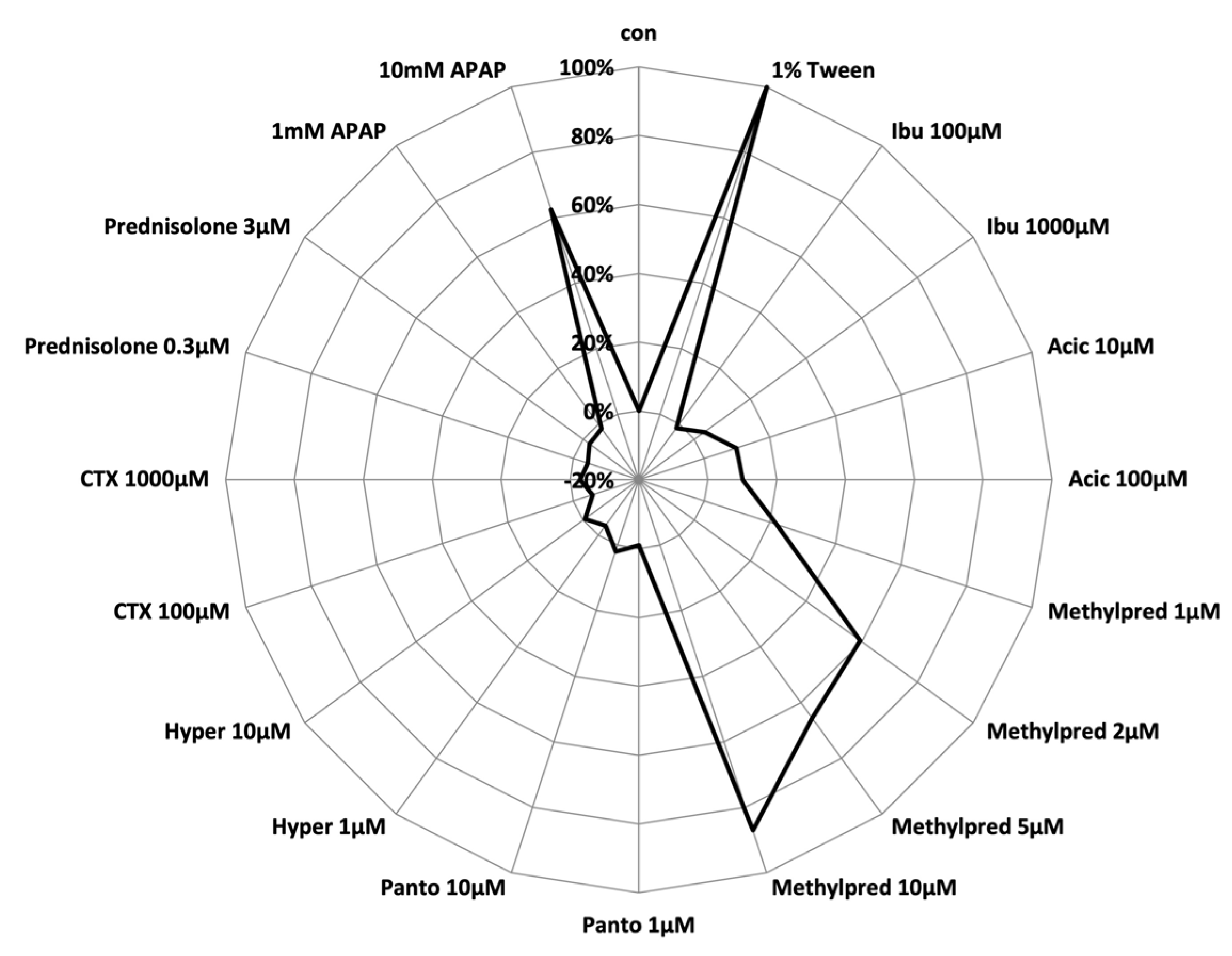
4. Differential Diagnosis—Use of In Vitro Assessment Tools
5. Biomarkers in DILI—Promising Diagnostic Candidates
6. Consortia Efforts for Biomarker Development in Drug-Induced Organ Injuries
7. Prognostic Biomarkers—Recent Advances in DILI Research
| Marker | Literature Reference | Summary |
|---|---|---|
| Proposed biomarkers/biomarker panels for DILI detection and or differentiation from other liver diseases | ||
| miR-122 | Thulin P, et al. Liver Int. 2014 [50] Howell LS, et al. Expert Rev Mol Diagn. 2018 [49] Rupprechter SAE, et al. Br J Clin Pharmacol. 2021 [47] | miR-122 as a liver-enriched miRNA has been observed before ALT elevation in patients with paracetamol overdose and has repeatedly been shown to be an early biomarker for DILI with higher sensitivity and specificity compared to ALT. |
| Church RJ, et al. J Dig Dis. 2019 [53] | Controversially, a lower correlation of miR-122 with ALT compared to GLDH as well as a high inter- and intra-individual variability have been observed. | |
| miR-129 | Wang K, et al. Proc Natl Acad Sci USA. 2009 [54] | Another liver-enriched miRNA, which has been proposed as an early biomarker for DILI showing dose-dependent changes parallel to ALT in patients with paracetamol overdose. |
| Liu XL, et al. Hepatology. 2020 [55] | Specificity for DILI is questioned by the observation that miR-129 could serve as a marker for NAFLD progression. | |
| GLDH | Church RJ, et al. J Dig Dis. 2019 [53] Schomaker S, et al. PLoS One. 2020 [57] Roth SE, et al. Clin Pharmacol Ther. 2020 [58] Church RJ, et al. PLoS One. 2020 [81] | GLDH was shown to correlate better with ALT in DILI patients when compared to miR-122 and thus has been proposed as a promising biomarker for DILI detection. More specific marker for liver injury than ALT as demonstrated by a study in patients with Duchene muscular dystrophy. Only mildly influenced by age and gender with low intra- and inter-subject variability. Potential marker for mitochondrial damage or mitophagy. |
| Harrill AH, et al. Clin Pharmacol Ther. 2012 [59] Roth SE, et al. Clin Pharmacol Ther. 2020 [58] | GLDH elevation might occur as consequence of biliary obstruction, congestive hepatitis or clinically non-significant liver injury following exposure to heparins, limiting the specificity for DILI. | |
| K18 | Thulin P, et al. Liver Int. 2014 [50] | The K18 marker M65 has been shown to not only increase earlier and to a higher extent in patients with paracetamol overdose than ALT but also to decline earlier after drug withdrawal. |
| K18, GLDH, miR-122 | Llewellyn HP, et al. Toxicol Sci. 2021 [60] | The combination of full-length K18, miR-122 and HMBG1 predicted paracetamol-induced acute liver injury better than ALT. However, when evaluated individually, none of the markers showed better diagnostic accuracy in comparison to ALT. |
| miR-122, HMGB1, K18 | Antoine DJ, et al. Hepatology. 2013 [51] | The combination of full-length K18, miR-122 and HMGB1 could predict ALI after paracetamol overdose before increase in ALT. |
| ITGB3 | Dragoi D, et al. Front Pharmacol. 2018 [61] | ITGB3 was shown to be upregulated in MH cells from patients with diclofenac-induced DILI and is therefore proposed as a specific marker for this type of DILI. |
| Apolipoprotein E | Bell LN, et al. Aliment Pharmacol Ther. 2012 [62] | Potential diagnostic DILI marker with high diagnostic accuracy (AUROC 0.97). |
| γ-Glu-Citrulline | Soga T, et al. J Hepatol. 2011 [65] | Good differentiation of DILI and other types of liver injury in combination with ALT (AUROC 0.817). |
| Serum metabolites (bile acids) | Ma Z, et al. Medicine (Baltimore). 2019 [63] | Serum metabolites for bile acid synthesis, i.e., palmitic acid, taurochenodeoxycholic acid, glycocholic acid and tauroursodeoxycholic acid, were identified as possible diagnostic markers for DILI with a higher expression when compared to healthy controls. |
| Metabolomic classification model (P-cresol sulfate vs. phenylalanine and inosine vs. bilirubin) | Huang Y, et al. Front Med (Lausanne). 2020 [66] | A classification model consisting of P-cresol sulfate vs. phenylalanine and inosine vs. bilirubin could distinguish between PM-DILI, AIH and HBV with a diagnostic accuracy of 89.8% (sensitivity 92.3%, specificity 88.9%). |
| GWAS for genetic susceptibility | Lucena MI, et al. Gastroenterology. 2011 [70] Urban TJ, et al. J Hepatol. 2017 [73] Donaldson PT, et al. J Hepatol. 2010 [71] Andrade RJ, et al. Hepatology. 2004 [72] | Various GWAS have shown genetic susceptibility for specific types of DILI, e.g., HLA DRB1*15:01-DQB1*06:02 and HLA-A*0201 in amoxicillin–clavulanate DILI or HLA-B*35-02 in minocycline-induced liver injury. However, the positive predictive value of HLA risk alleles is comparably low impeding the use for DILI diagnosis. |
| Proposed biomarkers/biomarker panels for severity prediction in DILI patients in the clinical setting | ||
| K18, OPN, MCSFR | Church RJ, et al. J Dig Dis. 2019 [53] | A strong correlation between K18, OPN and MCSFR and liver-related death or transplant within six months of DILI onset has been described. |
| HMBG1 | Dear JW, et al. Lancet Gastroenterol Hepatol. 2018 [52] | In paracetamol-induced liver injury, out of miR-122, HMGB1 and K18, only HMGB1 was predictive of coagulopathy with a sensitivity of 88% at a specificity of 95%. |
| miR-122-5p (+/− miR-382-5p) | Vliegenthart AD, et al. Sci Rep. 2015 [76] | miR-122-5p alone or in combination with miR-382-5p has been shown to predict paracetamol-induced liver failure with higher sensitivity than ALT. |
| miR-122, miR-4463 and pre-miR-4270 | Russo MW, et al. Liver Int. 2017 [77] | miR-122, miR-4463 and pre-miR-4270 inversely correlated with a fatal outcome within the first six months after DILI onset. miR-122 in combination with albumin could predict a fatal outcome with a sensitivity and specificity of 100% and 81%, respectively. |
| Serum metabolites (bile acids) | Ma Z, et al. Medicine (Baltimore). 2019 [63] | The serum metabolites glycocholic acid, taurocholic acid, tauroursodeoxycholic acid, glycochenodeoxycholic acid, glycochenodeoxycholic sulfate and taurodeoxycholic acid were shown to correlate well with more severe DILI. |
| IL-9, IL-17, PDGF-bb, RANTES | Steuerwald NM, et al. PLoS One. 2013 [79] | Lower levels of IL-9, IL-17, PDGF-bb and RANTES predicted a fatal outcome within six months of DILI onset with an accuracy of 92%. The accuracy of those four markers was even higher in combination with albumin (96%). |
| Bonkovsky HL, et al. PLoS One. 2018 [80] | The predictive accuracy of IL-9, IL-17, PDGF-bb and RANTES could not be validated in a larger cohort from the DILIN and Acute Liver Failure Study cohort, in this cohort the only predictive panel was RANTES and albumin, which at lower levels predicted mortality within six months with a specificity of 91% at a low sensitivity of 39%. | |
8. Prediction of DILI—Where Do We Stand?
9. Predictive Human Models—The Future of DILI Detection?
10. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldberg, D.S.; Forde, K.A.; Carbonari, D.M.; Lewis, J.D.; Leidl, K.B.; Reddy, K.R.; Haynes, K.; Roy, J.; Sha, D.; Marks, A.R.; et al. Population-representative incidence of drug-induced acute liver failure based on an analysis of an integrated health care system. Gastroenterology 2015, 148, 1353–1361.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reuben, A.; Koch, D.G.; Lee, W.M.; Acute Liver Failure Study, G. Drug-induced acute liver failure: Results of a U.S. multicenter, prospective study. Hepatology 2010, 52, 2065–2076. [Google Scholar] [CrossRef] [Green Version]
- Kullak-Ublick, G.A.; Andrade, R.J.; Merz, M.; End, P.; Benesic, A.; Gerbes, A.L.; Aithal, G.P. Drug-induced liver injury: Recent advances in diagnosis and risk assessment. Gut 2017, 66, 1154–1164. [Google Scholar] [CrossRef] [Green Version]
- Aithal, G.P.; Watkins, P.B.; Andrade, R.J.; Larrey, D.; Molokhia, M.; Takikawa, H.; Hunt, C.M.; Wilke, R.A.; Avigan, M.; Kaplowitz, N.; et al. Case definition and phenotype standardization in drug-induced liver injury. Clin. Pharmacol. Ther. 2011, 89, 806–815. [Google Scholar] [CrossRef] [PubMed]
- Nathwani, R.A.; Pais, S.; Reynolds, T.B.; Kaplowitz, N. Serum alanine aminotransferase in skeletal muscle diseases. Hepatology 2005, 41, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, J.; Hindorf, U.; Persson, P.; Bengtsson, T.; Malmqvist, U.; Werkstrom, V.; Ekelund, M. Muscular exercise can cause highly pathological liver function tests in healthy men. Br. J. Clin. Pharmacol. 2008, 65, 253–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lala, V.; Goyal, A.; Minter, D.A. Liver Function Tests. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Church, R.J.; Watkins, P.B. Serum biomarkers of drug-induced liver injury: Current status and future directions. J. Dig. Dis. 2019, 20, 2–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, Q.; Hong, H.; Senior, J.; Tong, W. Biomarkers for drug-induced liver injury. Expert Rev. Gastroenterol. Hepatol. 2010, 4, 225–234. [Google Scholar] [CrossRef] [Green Version]
- Atallah, E.; Freixo, C.; Alvarez-Alvarez, I.; Cubero, F.J.; Gerbes, A.L.; Kullak-Ublick, G.A.; Aithal, G.P. Biomarkers of idiosyncratic drug-induced liver injury (DILI)—A systematic review. Expert Opin. Drug Metab. Toxicol. 2021, 17, 1327–1343. [Google Scholar] [CrossRef] [PubMed]
- Hoofnagle, J.H.; Bjornsson, E.S. Drug-induced liver injury—Types and phenotypes. N. Engl. J. Med. 2019, 381, 264–273. [Google Scholar] [CrossRef]
- Chalasani, N.P.; Maddur, H.; Russo, M.W.; Wong, R.J.; Reddy, K.R. Practice Parameters Committee of the American College of Gastroenterology. ACG Clinical Guideline: Diagnosis and management of idiosyncratic drug-induced liver injury. Am. J. Gastroenterol. 2021, 116, 878–898. [Google Scholar] [CrossRef] [PubMed]
- Danan, G.; Benichou, C. Causality assessment of adverse reactions to drugs—I. A novel method based on the conclusions of international consensus meetings: Application to drug-induced liver injuries. J. Clin. Epidemiol. 1993, 46, 1323–1330. [Google Scholar] [CrossRef]
- Garcia-Cortes, M.; Stephens, C.; Lucena, M.I.; Fernandez-Castaner, A.; Andrade, R.J. Causality assessment methods in drug induced liver injury: Strengths and weaknesses. J. Hepatol. 2011, 55, 683–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Danan, G.; Teschke, R. RUCAM in Drug and Herb Induced Liver Injury: The Update. Int. J. Mol. Sci. 2015, 17, 14. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, P.; Wang, F.; Liu, L.; Zhang, Y.; Liu, Y.; Shi, R. Comparison of diagnostic accuracy of 3 diagnostic criteria combined with refined pathological scoring system for drug-induced liver injury. Medicine 2020, 99, e22259. [Google Scholar] [CrossRef]
- Kleiner, D.E. Histopathological challenges in suspected drug-induced liver injury. Liver Int. 2018, 38, 198–209. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, A.; Brunt, E.M.; Kleiner, D.E.; Miquel, R.; Smyrk, T.C.; Andrade, R.J.; Lucena, M.I.; Castiella, A.; Lindor, K.; Bjornsson, E. The use of liver biopsy evaluation in discrimination of idiopathic autoimmune hepatitis versus drug-induced liver injury. Hepatology 2011, 54, 931–939. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, P.H.; Lucena, M.I.; Fontana, R.J.; Bjornsson, E.S.; Aithal, G.P.; Barnhart, H.; Gonzalez Jimenez, A.; Yang, Q.; Gu, J.; Andrade, R.J.; et al. A revised electronic version of RUCAM for the diagnosis of drug induced liver injury. Hepatology 2022. [Google Scholar] [CrossRef]
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Available online: https://www.ncbi.nlm.nih.gov/books/NBK547852/ (accessed on 10 April 2022).
- de Boer, Y.S.; Kosinski, A.S.; Urban, T.J.; Zhao, Z.; Long, N.; Chalasani, N.; Kleiner, D.E.; Hoofnagle, J.H.; Drug-Induced Liver Injury, N. Features of autoimmune hepatitis in patients with drug-induced liver injury. Clin. Gastroenterol. Hepatol. 2017, 15, 103–112.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sebode, M.; Schulz, L.; Lohse, A.W. “Autoimmune(-like)” drug and herb induced liver injury: New insights into molecular pathogenesis. Int. J. Mol. Sci. 2017, 18, 1954. [Google Scholar] [CrossRef] [Green Version]
- Gerussi, A.; Natalini, A.; Antonangeli, F.; Mancuso, C.; Agostinetto, E.; Barisani, D.; Di Rosa, F.; Andrade, R.; Invernizzi, P. Immune-mediated drug-induced liver injury: Immunogenetics and experimental models. Int. J. Mol. Sci. 2021, 22, 4557. [Google Scholar] [CrossRef] [PubMed]
- deLemos, A.S.; Foureau, D.M.; Jacobs, C.; Ahrens, W.; Russo, M.W.; Bonkovsky, H.L. Drug-induced liver injury with autoimmune features. Semin. Liver Dis. 2014, 34, 194–204. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Autoimmune hepatitis. J. Hepatol. 2015, 63, 971–1004. [Google Scholar] [CrossRef] [PubMed]
- Hennes, E.M.; Zeniya, M.; Czaja, A.J.; Pares, A.; Dalekos, G.N.; Krawitt, E.L.; Bittencourt, P.L.; Porta, G.; Boberg, K.M.; Hofer, H.; et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology 2008, 48, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Bjornsson, E.; Talwalkar, J.; Treeprasertsuk, S.; Kamath, P.S.; Takahashi, N.; Sanderson, S.; Neuhauser, M.; Lindor, K. Drug-induced autoimmune hepatitis: Clinical characteristics and prognosis. Hepatology 2010, 51, 2040–2048. [Google Scholar] [CrossRef]
- Bjornsson, E.S.; Bergmann, O.; Jonasson, J.G.; Grondal, G.; Gudbjornsson, B.; Olafsson, S. Drug-induced autoimmune hepatitis: Response to corticosteroids and lack of relapse after cessation of steroids. Clin. Gastroenterol. Hepatol. 2017, 15, 1635–1636. [Google Scholar] [CrossRef] [Green Version]
- Weber, S.; Benesic, A.; Buchholtz, M.L.; Rotter, I.; Gerbes, A.L. Antimitochondrial rather than antinuclear antibodies correlate with severe drug-induced liver injury. Dig. Dis. 2021, 39, 275–282. [Google Scholar] [CrossRef]
- Stephens, C.; Castiella, A.; Gomez-Moreno, E.M.; Otazua, P.; Lopez-Nevot, M.A.; Zapata, E.; Ortega-Alonso, A.; Ruiz-Cabello, F.; Medina-Caliz, I.; Robles-Diaz, M.; et al. Autoantibody presentation in drug-induced liver injury and idiopathic autoimmune hepatitis: The influence of human leucocyte antigen alleles. Pharm. Genom. 2016, 26, 414–422. [Google Scholar] [CrossRef]
- Leung, P.S.; Rossaro, L.; Davis, P.A.; Park, O.; Tanaka, A.; Kikuchi, K.; Miyakawa, H.; Norman, G.L.; Lee, W.; Gershwin, M.E.; et al. Antimitochondrial antibodies in acute liver failure: Implications for primary biliary cirrhosis. Hepatology 2007, 46, 1436–1442. [Google Scholar] [CrossRef] [Green Version]
- Pichler, W.J.; Tilch, J. The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy 2004, 59, 809–820. [Google Scholar] [CrossRef]
- Maria, V.A.; Victorino, R.M. Diagnostic value of specific T cell reactivity to drugs in 95 cases of drug induced liver injury. Gut 1997, 41, 534–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walton, B. Lymphocyte transformation. JAMA 1973, 225, 494–498. [Google Scholar] [CrossRef] [PubMed]
- Victorino, R.M.; Maria, V.A.; Pinto, L.A. Evidence for prostaglandin-producing suppressor cells in drug-induced liver injury and implications in the diagnosis of drug sensitization. Clin. Exp. Immunol 1992, 87, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Whritenour, J.; Ko, M.; Zong, Q.; Wang, J.; Tartaro, K.; Schneider, P.; Olson, E.; Van Volkenburg, M.; Serrano, J.; Hayashi, P.; et al. Development of a modified lymphocyte transformation test for diagnosing drug-induced liver injury associated with an adaptive immune response. J. Immunotoxicol. 2017, 14, 31–38. [Google Scholar] [CrossRef]
- Jee, A.; Sernoskie, S.C.; Uetrecht, J. Idiosyncratic drug-induced liver injury: Mechanistic and clinical challenges. Int. J. Mol. Sci. 2021, 22, 2954. [Google Scholar] [CrossRef] [PubMed]
- Tillmann, H.L.; Suzuki, A.; Barnhart, H.X.; Serrano, J.; Rockey, D.C. Tools for causality assessment in drug-induced liver disease. Curr. Opin. Gastroenterol. 2019, 35, 183–190. [Google Scholar] [CrossRef]
- Hanatani, T.; Sai, K.; Tohkin, M.; Segawa, K.; Kimura, M.; Hori, K.; Kawakami, J.; Saito, Y. A detection algorithm for drug-induced liver injury in medical information databases using the Japanese diagnostic scale and its comparison with the Council for International Organizations of Medical Sciences/the Roussel Uclaf Causality Assessment Method scale. Pharmacoepidemiol. Drug Saf. 2014, 23, 984–988. [Google Scholar] [CrossRef]
- Beeler, A.; Zaccaria, L.; Kawabata, T.; Gerber, B.O.; Pichler, W.J. CD69 upregulation on T cells as an in vitro marker for delayed-type drug hypersensitivity. Allergy 2008, 63, 181–188. [Google Scholar] [CrossRef]
- Benesic, A.; Rahm, N.L.; Ernst, S.; Gerbes, A.L. Human monocyte-derived cells with individual hepatocyte characteristics: A novel tool for personalized in vitro studies. Lab. Investig. 2012, 92, 926–936. [Google Scholar] [CrossRef] [PubMed]
- Benesic, A.; Leitl, A.; Gerbes, A.L. Monocyte-derived hepatocyte-like cells for causality assessment of idiosyncratic drug-induced liver injury. Gut 2016, 65, 1555–1563. [Google Scholar] [CrossRef]
- Benesic, A.; Rotter, I.; Dragoi, D.; Weber, S.; Leitl, A.; Buchholtz, M.L.; Gerbes, A.L. Development and validation of a test to identify drugs that cause idiosyncratic drug-induced liver injury. Clin. Gastroenterol. Hepatol. 2018, 16, 1488–1494.e5. [Google Scholar] [CrossRef] [PubMed]
- Pessayre, D.; Fromenty, B.; Berson, A.; Robin, M.A.; Letteron, P.; Moreau, R.; Mansouri, A. Central role of mitochondria in drug-induced liver injury. Drug Metab. Rev. 2012, 44, 34–87. [Google Scholar] [CrossRef]
- Thompson, R.A.; Isin, E.M.; Li, Y.; Weidolf, L.; Page, K.; Wilson, I.; Swallow, S.; Middleton, B.; Stahl, S.; Foster, A.J.; et al. In vitro approach to assess the potential for risk of idiosyncratic adverse reactions caused by candidate drugs. Chem. Res. Toxicol. 2012, 25, 1616–1632. [Google Scholar] [CrossRef] [PubMed]
- McGill, M.R.; Jaeschke, H. Mechanistic biomarkers in acetaminophen-induced hepatotoxicity and acute liver failure: From preclinical models to patients. Expert Opin. Drug Metab. Toxicol. 2014, 10, 1005–1017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rupprechter, S.A.E.; Sloan, D.J.; Oosthuyzen, W.; Bachmann, T.T.; Hill, A.T.; Dhaliwal, K.; Templeton, K.; Matovu, J.; Sekaggya-Wiltshire, C.; Dear, J.W. MicroRNA-122 and cytokeratin-18 have potential as a biomarkers of drug-induced liver injury in European and African patients on treatment for mycobacterial infection. Br. J. Clin. Pharmacol. 2021, 87, 3206–3217. [Google Scholar] [CrossRef]
- Zhang, Y.; Jia, Y.; Zheng, R.; Guo, Y.; Wang, Y.; Guo, H.; Fei, M.; Sun, S. Plasma microRNA-122 as a biomarker for viral-, alcohol-, and chemical-related hepatic diseases. Clin. Chem. 2010, 56, 1830–1838. [Google Scholar] [CrossRef]
- Howell, L.S.; Ireland, L.; Park, B.K.; Goldring, C.E. MiR-122 and other microRNAs as potential circulating biomarkers of drug-induced liver injury. Expert Rev. Mol. Diagn. 2018, 18, 47–54. [Google Scholar] [CrossRef]
- Thulin, P.; Nordahl, G.; Gry, M.; Yimer, G.; Aklillu, E.; Makonnen, E.; Aderaye, G.; Lindquist, L.; Mattsson, C.M.; Ekblom, B.; et al. Keratin-18 and microRNA-122 complement alanine aminotransferase as novel safety biomarkers for drug-induced liver injury in two human cohorts. Liver Int. 2014, 34, 367–378. [Google Scholar] [CrossRef]
- Antoine, D.J.; Dear, J.W.; Lewis, P.S.; Platt, V.; Coyle, J.; Masson, M.; Thanacoody, R.H.; Gray, A.J.; Webb, D.J.; Moggs, J.G.; et al. Mechanistic biomarkers provide early and sensitive detection of acetaminophen-induced acute liver injury at first presentation to hospital. Hepatology 2013, 58, 777–787. [Google Scholar] [CrossRef] [Green Version]
- Dear, J.W.; Clarke, J.I.; Francis, B.; Allen, L.; Wraight, J.; Shen, J.; Dargan, P.I.; Wood, D.; Cooper, J.; Thomas, S.H.L.; et al. Risk stratification after paracetamol overdose using mechanistic biomarkers: Results from two prospective cohort studies. Lancet Gastroenterol. Hepatol. 2018, 3, 104–113. [Google Scholar] [CrossRef] [Green Version]
- Church, R.J.; Kullak-Ublick, G.A.; Aubrecht, J.; Bonkovsky, H.L.; Chalasani, N.; Fontana, R.J.; Goepfert, J.C.; Hackman, F.; King, N.M.P.; Kirby, S.; et al. Candidate biomarkers for the diagnosis and prognosis of drug-induced liver injury: An international collaborative effort. Hepatology 2019, 69, 760–773. [Google Scholar] [CrossRef]
- Wang, K.; Zhang, S.; Marzolf, B.; Troisch, P.; Brightman, A.; Hu, Z.; Hood, L.E.; Galas, D.J. Circulating microRNAs, potential biomarkers for drug-induced liver injury. Proc. Natl. Acad. Sci. USA 2009, 106, 4402–4407. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.L.; Pan, Q.; Cao, H.X.; Xin, F.Z.; Zhao, Z.H.; Yang, R.X.; Zeng, J.; Zhou, H.; Fan, J.G. Lipotoxic hepatocyte-derived exosomal microRNA 192-5p activates macrophages through rictor/Akt/forkhead box transcription factor O1 signaling in nonalcoholic fatty liver disease. Hepatology 2020, 72, 454–469. [Google Scholar] [CrossRef] [PubMed]
- Yamaura, Y.; Tatsumi, N.; Takagi, S.; Tokumitsu, S.; Fukami, T.; Tajiri, K.; Minemura, M.; Yokoi, T.; Nakajima, M. Serum microRNA profiles in patients with chronic hepatitis B, chronic hepatitis C, primary biliary cirrhosis, autoimmune hepatitis, nonalcoholic steatohepatitis, or drug-induced liver injury. Clin. Biochem. 2017, 50, 1034–1039. [Google Scholar] [CrossRef] [Green Version]
- Schomaker, S.; Potter, D.; Warner, R.; Larkindale, J.; King, N.; Porter, A.C.; Owens, J.; Tomlinson, L.; Sauer, J.M.; Johnson, K.; et al. Serum glutamate dehydrogenase activity enables early detection of liver injury in subjects with underlying muscle impairments. PLoS ONE 2020, 15, e0229753. [Google Scholar] [CrossRef]
- Roth, S.E.; Avigan, M.I.; Bourdet, D.; Brott, D.; Church, R.; Dash, A.; Keller, D.; Sherratt, P.; Watkins, P.B.; Westcott-Baker, L.; et al. Next-generation DILI biomarkers: Prioritization of biomarkers for qualification and best practices for biospecimen collection in drug development. Clin. Pharmacol. Ther. 2020, 107, 333–346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrill, A.H.; Roach, J.; Fier, I.; Eaddy, J.S.; Kurtz, C.L.; Antoine, D.J.; Spencer, D.M.; Kishimoto, T.K.; Pisetsky, D.S.; Park, B.K.; et al. The effects of heparins on the liver: Application of mechanistic serum biomarkers in a randomized study in healthy volunteers. Clin. Pharmacol. Ther. 2012, 92, 214–220. [Google Scholar] [CrossRef]
- Llewellyn, H.P.; Vaidya, V.S.; Wang, Z.; Peng, Q.; Hyde, C.; Potter, D.; Wang, J.; Zong, Q.; Arat, S.; Martin, M.; et al. Evaluating the sensitivity and specificity of promising circulating biomarkers to diagnose liver injury in humans. Toxicol. Sci. 2021, 181, 23–34. [Google Scholar] [CrossRef]
- Dragoi, D.; Benesic, A.; Pichler, G.; Kulak, N.A.; Bartsch, H.S.; Gerbes, A.L. Proteomics analysis of monocyte-derived hepatocyte-like cells identifies integrin beta 3 as a specific biomarker for drug-induced liver injury by diclofenac. Front. Pharmacol. 2018, 9, 699. [Google Scholar] [CrossRef]
- Bell, L.N.; Vuppalanchi, R.; Watkins, P.B.; Bonkovsky, H.L.; Serrano, J.; Fontana, R.J.; Wang, M.; Rochon, J.; Chalasani, N.; for the US Drug-Induced Liver Injury Network (DILIN) Research Group. Serum proteomic profiling in patients with drug-induced liver injury. Aliment. Pharmacol. Ther. 2012, 35, 600–612. [Google Scholar] [CrossRef] [Green Version]
- Ma, Z.; Wang, X.; Yin, P.; Wu, R.; Zhou, L.; Xu, G.; Niu, J. Serum metabolome and targeted bile acid profiling reveals potential novel biomarkers for drug-induced liver injury. Medicine 2019, 98, e16717. [Google Scholar] [CrossRef] [PubMed]
- Quintas, G.; Martinez-Sena, T.; Conde, I.; Pareja Ibars, E.; Kleinjans, J.; Castell, J.V. Metabolomic analysis to discriminate drug-induced liver injury (DILI) phenotypes. Arch. Toxicol. 2021, 95, 3049–3062. [Google Scholar] [CrossRef] [PubMed]
- Soga, T.; Sugimoto, M.; Honma, M.; Mori, M.; Igarashi, K.; Kashikura, K.; Ikeda, S.; Hirayama, A.; Yamamoto, T.; Yoshida, H.; et al. Serum metabolomics reveals gamma-glutamyl dipeptides as biomarkers for discrimination among different forms of liver disease. J. Hepatol. 2011, 55, 896–905. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, X.; Zhang, Z.T.; Chen, S.S.; Li, S.S.; Shi, Z.; Jing, J.; Huang, A.; Guo, Y.M.; Bai, Z.F.; et al. Metabolomics profiling and diagnosis biomarkers searching for drug-induced liver injury implicated to polygonum multiflorum: A cross-sectional cohort study. Front. Med. 2020, 7, 592434. [Google Scholar] [CrossRef]
- Nicoletti, P.; Werk, A.N.; Sawle, A.; Shen, Y.; Urban, T.J.; Coulthard, S.A.; Bjornsson, E.S.; Cascorbi, I.; Floratos, A.; Stammschulte, T.; et al. HLA-DRB1*16: 01-DQB1*05: 02 is a novel genetic risk factor for flupirtine-induced liver injury. Pharm. Genom. 2016, 26, 218–224. [Google Scholar] [CrossRef]
- Nicoletti, P.; Aithal, G.P.; Bjornsson, E.S.; Andrade, R.J.; Sawle, A.; Arrese, M.; Barnhart, H.X.; Bondon-Guitton, E.; Hayashi, P.H.; Bessone, F.; et al. Association of liver injury from specific drugs, or groups of drugs, with polymorphisms in HLA and other genes in a genome-wide association study. Gastroenterology 2017, 152, 1078–1089. [Google Scholar] [CrossRef] [Green Version]
- Hoofnagle, J.H.; Bonkovsky, H.L.; Phillips, E.J.; Li, Y.J.; Ahmad, J.; Barnhart, H.; Durazo, F.; Fontana, R.J.; Gu, J.; Khan, I.; et al. HLA-B*35:01 and green tea-induced liver injury. Hepatology 2021, 73, 2484–2493. [Google Scholar] [CrossRef]
- Lucena, M.I.; Molokhia, M.; Shen, Y.; Urban, T.J.; Aithal, G.P.; Andrade, R.J.; Day, C.P.; Ruiz-Cabello, F.; Donaldson, P.T.; Stephens, C.; et al. Susceptibility to amoxicillin-clavulanate-induced liver injury is influenced by multiple HLA class I and II alleles. Gastroenterology 2011, 141, 338–347. [Google Scholar] [CrossRef]
- Donaldson, P.T.; Daly, A.K.; Henderson, J.; Graham, J.; Pirmohamed, M.; Bernal, W.; Day, C.P.; Aithal, G.P. Human leucocyte antigen class II genotype in susceptibility and resistance to co-amoxiclav-induced liver injury. J. Hepatol. 2010, 53, 1049–1053. [Google Scholar] [CrossRef]
- Andrade, R.J.; Lucena, M.I.; Alonso, A.; Garcia-Cortes, M.; Garcia-Ruiz, E.; Benitez, R.; Fernandez, M.C.; Pelaez, G.; Romero, M.; Corpas, R.; et al. HLA class II genotype influences the type of liver injury in drug-induced idiosyncratic liver disease. Hepatology 2004, 39, 1603–1612. [Google Scholar] [CrossRef]
- Urban, T.J.; Nicoletti, P.; Chalasani, N.; Serrano, J.; Stolz, A.; Daly, A.K.; Aithal, G.P.; Dillon, J.; Navarro, V.; Odin, J.; et al. Minocycline hepatotoxicity: Clinical characterization and identification of HLA-B *35:02 as a risk factor. J. Hepatol. 2017, 67, 137–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stephens, C.; Andrade, R.J. Genetic predisposition to drug-induced liver injury. Clin. Liver Dis. 2020, 24, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Translational Safety Biomarker Pipeline (TransBioLine): Enabling Development and Implementation of novel Safety Biomarkers in Clinical Trials and Diagnosis of Disease. Available online: https://cordis.europa.eu/project/id/821283/reporting (accessed on 10 April 2022).
- Vliegenthart, A.D.; Shaffer, J.M.; Clarke, J.I.; Peeters, L.E.; Caporali, A.; Bateman, D.N.; Wood, D.M.; Dargan, P.I.; Craig, D.G.; Moore, J.K.; et al. Comprehensive microRNA profiling in acetaminophen toxicity identifies novel circulating biomarkers for human liver and kidney injury. Sci. Rep. 2015, 5, 15501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russo, M.W.; Steuerwald, N.; Norton, H.J.; Anderson, W.E.; Foureau, D.; Chalasani, N.; Fontana, R.J.; Watkins, P.B.; Serrano, J.; Bonkovsky, H.L. Profiles of miRNAs in serum in severe acute drug induced liver injury and their prognostic significance. Liver Int. 2017, 37, 757–764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, Z.; Chen, E.; Ouyang, X.; Xu, X.; Ma, S.; Ji, F.; Wu, D.; Zhang, S.; Zhao, Y.; Li, L. Metabolomics and cytokine analysis for identification of severe drug-induced liver injury. J. Proteome Res. 2019, 18, 2514–2524. [Google Scholar] [CrossRef]
- Steuerwald, N.M.; Foureau, D.M.; Norton, H.J.; Zhou, J.; Parsons, J.C.; Chalasani, N.; Fontana, R.J.; Watkins, P.B.; Lee, W.M.; Reddy, K.R.; et al. Profiles of serum cytokines in acute drug-induced liver injury and their prognostic significance. PLoS ONE 2013, 8, e81974. [Google Scholar] [CrossRef]
- Bonkovsky, H.L.; Barnhart, H.X.; Foureau, D.M.; Steuerwald, N.; Lee, W.M.; Gu, J.; Fontana, R.J.; Hayashi, P.J.; Chalasani, N.; Navarro, V.M.; et al. Cytokine profiles in acute liver injury-Results from the US Drug-Induced Liver Injury Network (DILIN) and the Acute Liver Failure Study Group. PLoS ONE 2018, 13, e0206389. [Google Scholar] [CrossRef] [Green Version]
- Church, R.J.; Schomaker, S.J.; Eaddy, J.S.; Boucher, G.G.; Kreeger, J.M.; Aubrecht, J.; Watkins, P.B. Glutamate dehydrogenase as a biomarker for mitotoxicity; insights from furosemide hepatotoxicity in the mouse. PLoS ONE 2020, 15, e0240562. [Google Scholar] [CrossRef]
- Ho, C.M.; Chen, C.L.; Chang, C.H.; Lee, M.R.; Wang, J.Y.; Hu, R.H.; Lee, P.H. Circulatory inflammatory mediators in the prediction of anti-tuberculous drug-induced liver injury using RUCAM for causality assessment. Biomedicines 2021, 9, 891. [Google Scholar] [CrossRef]
- Luster, A.D.; Unkeless, J.C.; Ravetch, J.V. Gamma-interferon transcriptionally regulates an early-response gene containing homology to platelet proteins. Nature 1985, 315, 672–676. [Google Scholar] [CrossRef]
- Cornberg, M.; Wiegand, S.B. Importance of IP-10 in hepatitis, B. Antivir. Ther. 2016, 21, 93–96. [Google Scholar] [CrossRef] [PubMed]
- You, E.; Kim, M.H.; Lee, W.I.; Kang, S.Y. Evaluation of IL-2, IL-10, IL-17 and IP-10 as potent discriminative markers for active tuberculosis among pulmonary tuberculosis suspects. Tuberculosis 2016, 99, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Dufour, J.H.; Dziejman, M.; Liu, M.T.; Leung, J.H.; Lane, T.E.; Luster, A.D. IFN-gamma-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J. Immunol. 2002, 168, 3195–3204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Etzerodt, A.; Berg, R.M.; Plovsing, R.R.; Andersen, M.N.; Bebien, M.; Habbeddine, M.; Lawrence, T.; Moller, H.J.; Moestrup, S.K. Soluble ectodomain CD163 and extracellular vesicle-associated CD163 are two differently regulated forms of ‘soluble CD163’ in plasma. Sci. Rep. 2017, 7, 40286. [Google Scholar] [CrossRef] [PubMed]
- Kazankov, K.; Barrera, F.; Moller, H.J.; Bibby, B.M.; Vilstrup, H.; George, J.; Gronbaek, H. Soluble CD163, a macrophage activation marker, is independently associated with fibrosis in patients with chronic viral hepatitis B and, C. Hepatology 2014, 60, 521–530. [Google Scholar] [CrossRef]
- Parkner, T.; Sorensen, L.P.; Nielsen, A.R.; Fischer, C.P.; Bibby, B.M.; Nielsen, S.; Pedersen, B.K.; Moller, H.J. Soluble CD163: A biomarker linking macrophages and insulin resistance. Diabetologia 2012, 55, 1856–1862. [Google Scholar] [CrossRef] [Green Version]
- Martin, J.C.; Beriou, G.; Heslan, M.; Chauvin, C.; Utriainen, L.; Aumeunier, A.; Scott, C.L.; Mowat, A.; Cerovic, V.; Houston, S.A.; et al. Interleukin-22 binding protein (IL-22BP) is constitutively expressed by a subset of conventional dendritic cells and is strongly induced by retinoic acid. Mucosal Immunol. 2014, 7, 101–113. [Google Scholar] [CrossRef]
- Schwarzkopf, K.; Ruschenbaum, S.; Barat, S.; Cai, C.; Mucke, M.M.; Fitting, D.; Weigert, A.; Brune, B.; Zeuzem, S.; Welsch, C.; et al. IL-22 and IL-22-binding protein are associated with development of and mortality from acute-on-chronic liver failure. Hepatol. Commun. 2019, 3, 392–405. [Google Scholar] [CrossRef] [Green Version]
- Watkins, P.B. The DILI-sim Initiative: Insights into hepatotoxicity mechanisms and biomarker interpretation. Clin. Transl. Sci. 2019, 12, 122–129. [Google Scholar] [CrossRef] [Green Version]
- Watkins, P.B. Quantitative systems toxicology approaches to understand and predict drug-induced liver injury. Clin. Liver Dis. 2020, 24, 49–60. [Google Scholar] [CrossRef]
- Hermann, R.; Rockey, D.C.; Suzuki, A.; Merz, M.; Tillmann, H.L. A novel phenotype-based drug-induced liver injury causality assessment tool (DILI-CAT) allows for signal confirmation in early drug development. Aliment. Pharmacol. Ther. 2022, 55, 1028–1037. [Google Scholar] [CrossRef] [PubMed]
- Morgan, R.E.; Trauner, M.; van Staden, C.J.; Lee, P.H.; Ramachandran, B.; Eschenberg, M.; Afshari, C.A.; Qualls, C.W., Jr.; Lightfoot-Dunn, R.; Hamadeh, H.K. Interference with bile salt export pump function is a susceptibility factor for human liver injury in drug development. Toxicol. Sci. 2010, 118, 485–500. [Google Scholar] [CrossRef] [PubMed]
- Petrov, P.D.; Soluyanova, P.; Sanchez-Campos, S.; Castell, J.V.; Jover, R. Molecular mechanisms of hepatotoxic cholestasis by clavulanic acid: Role of NRF2 and FXR pathways. Food Chem. Toxicol. 2021, 158, 112664. [Google Scholar] [CrossRef] [PubMed]
- Dawson, S.; Stahl, S.; Paul, N.; Barber, J.; Kenna, J.G. In vitro inhibition of the bile salt export pump correlates with risk of cholestatic drug-induced liver injury in humans. Drug Metab. Dispos. 2012, 40, 130–138. [Google Scholar] [CrossRef]
- Fattinger, K.; Funk, C.; Pantze, M.; Weber, C.; Reichen, J.; Stieger, B.; Meier, P.J. The endothelin antagonist bosentan inhibits the canalicular bile salt export pump: A potential mechanism for hepatic adverse reactions. Clin. Pharmacol. Ther. 2001, 69, 223–231. [Google Scholar] [CrossRef]
- Funk, C.; Ponelle, C.; Scheuermann, G.; Pantze, M. Cholestatic potential of troglitazone as a possible factor contributing to troglitazone-induced hepatotoxicity: In vivo and in vitro interaction at the canalicular bile salt export pump (BSEP) in the rat. Mol. Pharmacol. 2001, 59, 627–635. [Google Scholar] [CrossRef]
- Brecklinghaus, T.; Albrecht, W.; Kappenberg, F.; Duda, J.; Vartak, N.; Edlund, K.; Marchan, R.; Ghallab, A.; Cadenas, C.; Gunther, G.; et al. The hepatocyte export carrier inhibition assay improves the separation of hepatotoxic from non-hepatotoxic compounds. Chem. Biol. Interact. 2021, 351, 109728. [Google Scholar] [CrossRef]
- PSTC Webinar Series: Current Trends in BSEP Inhibition and Perturbation to Bile Acid Homeostasis as Mechanisms of Drug-Induced Liver Injury. Available online: https://c-path.org/current-trends-in-bsep-inhibition-and-perturbation-to-bile-acid-homeostasis-as-mechanisms-of-drug-induced-liver-injury/ (accessed on 10 April 2022).
- EMA Guideline on the Investigation of Drug Interactions. Available online: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guide-line/2012/07/WC500129606.pdf (accessed on 10 April 2022).
- FDA Guidance for Industry—Drug Interaction Studies. Available online: https://www.fda.gov/drugs/guidance-compliance-regulatory-information/guidances-drugs (accessed on 10 April 2022).
- Chan, R.; Benet, L.Z. Measures of BSEP inhibition in vitro are not useful predictors of DILI. Toxicol. Sci. 2018, 162, 499–508. [Google Scholar] [CrossRef] [Green Version]
- Masubuchi, N.; Sugihara, M.; Sugita, T.; Amano, K.; Nakano, M.; Matsuura, T. Oxidative stress markers, secondary bile acids and sulfated bile acids classify the clinical liver injury type: Promising diagnostic biomarkers for cholestasis. Chem. Biol. Interact. 2016, 255, 83–91. [Google Scholar] [CrossRef]
- Labbe, G.; Pessayre, D.; Fromenty, B. Drug-induced liver injury through mitochondrial dysfunction: Mechanisms and detection during preclinical safety studies. Fundam. Clin. Pharmacol. 2008, 22, 335–353. [Google Scholar] [CrossRef]
- Pereira, C.V.; Nadanaciva, S.; Oliveira, P.J.; Will, Y. The contribution of oxidative stress to drug-induced organ toxicity and its detection in vitro and in vivo. Expert Opin. Drug Metab. Toxicol. 2012, 8, 219–237. [Google Scholar] [CrossRef] [PubMed]
- Jaeschke, H.; McGill, M.R.; Ramachandran, A. Oxidant stress, mitochondria, and cell death mechanisms in drug-induced liver injury: Lessons learned from acetaminophen hepatotoxicity. Drug Metab. Rev. 2012, 44, 88–106. [Google Scholar] [CrossRef] [Green Version]
- Aleo, M.D.; Luo, Y.; Swiss, R.; Bonin, P.D.; Potter, D.M.; Will, Y. Human drug-induced liver injury severity is highly associated with dual inhibition of liver mitochondrial function and bile salt export pump. Hepatology 2014, 60, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Mills, E.L.; Kelly, B.; O’Neill, L.A.J. Mitochondria are the powerhouses of immunity. Nat. Immunol. 2017, 18, 488–498. [Google Scholar] [CrossRef] [PubMed]
- Magnani, N.D.; Marchini, T.; Calabro, V.; Alvarez, S.; Evelson, P. Role of mitochondria in the redox signaling network and its outcomes in high impact inflammatory syndromes. Front. Endocrinol. 2020, 11, 568305. [Google Scholar] [CrossRef]
- Kenna, J.G.; Neuberger, J.; Williams, R. An enzyme-linked immunosorbent assay for detection of antibodies against halothane-altered hepatocyte antigens. J. Immunol. Methods 1984, 75, 3–14. [Google Scholar] [CrossRef]
- Gómez-Lechón, M.J.; Carrasquer, J.; Berenguer, J.; Castell, J.V. Evidence of antibodies to erythromycin in serum of a patient following an episode of acute drug-induced hepatitis. Clin. Exp. Allergy 1996, 26, 590–596. [Google Scholar] [CrossRef]
- Fernandez-Checa, J.C.; Bagnaninchi, P.; Ye, H.; Sancho-Bru, P.; Falcon-Perez, J.M.; Royo, F.; Garcia-Ruiz, C.; Konu, O.; Miranda, J.; Lunov, O.; et al. Advanced preclinical models for evaluation of drug-induced liver injury—Consensus statement by the European Drug-Induced Liver Injury Network [PRO-EURO-DILI-NET]. J. Hepatol. 2021, 75, 935–959. [Google Scholar] [CrossRef]
- Nelson, L.J.; Morgan, K.; Treskes, P.; Samuel, K.; Henderson, C.J.; LeBled, C.; Homer, N.; Grant, M.H.; Hayes, P.C.; Plevris, J.N. Human hepatic HepaRG cells maintain an organotypic phenotype with high intrinsic CYP450 activity/metabolism and significantly outperform standard HepG2/C3A cells for pharmaceutical and therapeutic applications. Basic Clin. Pharmacol. Toxicol. 2017, 120, 30–37. [Google Scholar] [CrossRef]
- Takahashi, K.; Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 2006, 126, 663–676. [Google Scholar] [CrossRef] [Green Version]
- Shi, Y.; Inoue, H.; Wu, J.C.; Yamanaka, S. Induced pluripotent stem cell technology: A decade of progress. Nat. Rev. Drug Discov. 2017, 16, 115–130. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.J.; Hay, D.C.; Park, I.H.; Fletcher, J.; Hannoun, Z.; Payne, C.M.; Dalgetty, D.; Black, J.R.; Ross, J.A.; Samuel, K.; et al. Generation of functional human hepatic endoderm from human induced pluripotent stem cells. Hepatology 2010, 51, 329–335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yi, F.; Liu, G.H.; Izpisua Belmonte, J.C. Human induced pluripotent stem cells derived hepatocytes: Rising promise for disease modeling, drug development and cell therapy. Protein Cell 2012, 3, 246–250. [Google Scholar] [CrossRef]
- Avior, Y.; Levy, G.; Zimerman, M.; Kitsberg, D.; Schwartz, R.; Sadeh, R.; Moussaieff, A.; Cohen, M.; Itskovitz-Eldor, J.; Nahmias, Y. Microbial-derived lithocholic acid and vitamin K2 drive the metabolic maturation of pluripotent stem cells-derived and fetal hepatocytes. Hepatology 2015, 62, 265–278. [Google Scholar] [CrossRef]
- Gieseck, R.L., III; Hannan, N.R.; Bort, R.; Hanley, N.A.; Drake, R.A.; Cameron, G.W.; Wynn, T.A.; Vallier, L. Maturation of induced pluripotent stem cell derived hepatocytes by 3D-culture. PLoS ONE 2014, 9, e86372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boon, R.; Kumar, M.; Tricot, T.; Elia, I.; Ordovas, L.; Jacobs, F.; One, J.; De Smedt, J.; Eelen, G.; Bird, M.; et al. Amino acid levels determine metabolism and CYP450 function of hepatocytes and hepatoma cell lines. Nat. Commun. 2020, 11, 1393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novik, E.; Maguire, T.J.; Chao, P.; Cheng, K.C.; Yarmush, M.L. A microfluidic hepatic coculture platform for cell-based drug metabolism studies. Biochem. Pharmacol. 2010, 79, 1036–1044. [Google Scholar] [CrossRef] [Green Version]
- Mun, S.J.; Ryu, J.S.; Lee, M.O.; Son, Y.S.; Oh, S.J.; Cho, H.S.; Son, M.Y.; Kim, D.S.; Kim, S.J.; Yoo, H.J.; et al. Generation of expandable human pluripotent stem cell-derived hepatocyte-like liver organoids. J. Hepatol. 2019, 71, 970–985. [Google Scholar] [CrossRef]
- Gomez-Lechon, M.J.; Tolosa, L. Human hepatocytes derived from pluripotent stem cells: A promising cell model for drug hepatotoxicity screening. Arch. Toxicol. 2016, 90, 2049–2061. [Google Scholar] [CrossRef]
- Tostoes, R.M.; Leite, S.B.; Serra, M.; Jensen, J.; Bjorquist, P.; Carrondo, M.J.; Brito, C.; Alves, P.M. Human liver cell spheroids in extended perfusion bioreactor culture for repeated-dose drug testing. Hepatology 2012, 55, 1227–1236. [Google Scholar] [CrossRef]
- Shinozawa, T.; Kimura, M.; Cai, Y.; Saiki, N.; Yoneyama, Y.; Ouchi, R.; Koike, H.; Maezawa, M.; Zhang, R.R.; Dunn, A.; et al. High-fidelity drug-induced liver injury screen using human pluripotent stem cell-derived organoids. Gastroenterology 2021, 160, 831–846e10. [Google Scholar] [CrossRef] [PubMed]
- Jang, K.J.; Otieno, M.A.; Ronxhi, J.; Lim, H.K.; Ewart, L.; Kodella, K.R.; Petropolis, D.B.; Kulkarni, G.; Rubins, J.E.; Conegliano, D.; et al. Reproducing human and cross-species drug toxicities using a Liver-Chip. Sci. Transl. Med. 2019, 11, eaax5516. [Google Scholar] [CrossRef] [PubMed]
| Item 1: Time to Onset | Assessment 2 | ||||
| Hepatocellular Type 1 | Cholestatic Type 1 | ||||
| Initial treatment | Subsequent treatment | Initial treatment | Subsequent treatment | ||
| 5–90 days <5 or >90 days | 1–15 days >15 days | 5–90 days <5 or >90 days | 1–90 days >90 days | +2 +1 |
| ≤15 days | ≤15 days | ≤30 days | ≤30 days | +1 |
| Note: If reaction begins before starting the medication or >15 days (hepatocellular)/>30 days (cholestatic) after stopping the medication, the injury should be considered unrelated and RUCAM cannot be calculated | |||||
| Item 2: Course | Change in ALT between peak value and ULN | Change in ALP (OR TBIL) between peak value and ULN | |||
After stopping the drug
| Decrease ≥ 50% within 8 days Decrease ≥ 50% within 30 days Not applicable No information or decrease ≥ 50% after 30 days Decrease < 50% after 30 days or recurrent increase | Not applicable Decrease ≥ 50% within 180 days Decrease < 50% within 180 days Persistence or increase or no information Not applicable | +3 +2 +1 0 −2 | ||
If drug is continued
| All situations | All situations | 0 | ||
| Item 3: Risk factors | Ethanol | Ethanol or Pregnancy (either) | |||
| Alcohol or Pregnancy | Presence | Presence | +1 | ||
| Absence | Absence | 0 | |||
| Age | Age ≥ 55 years Age < 55 years | Age ≥ 55 years Age < 55 years | +1 | ||
| 0 | |||||
| Item 4: Concomitant drug(s) | |||||
| 0 −1 −2 −3 | ||||
| Item 5: Exclusion of other causes of liver injury | |||||
| All causes in Group 1 and 2 ruled out | +2 | |||
| All causes in Group 1 ruled out | +1 | ||||
| 4 or 5 causes in Group 1 ruled out | 0 | ||||
| <4 causes in Group 1 ruled out | −2 | ||||
| Non-drug cause highly probable | −3 | ||||
| Item 6: Previous information on hepatotoxicity of the drug | |||||
| +2 +1 0 | ||||
| Item 7: Response to readministration: | |||||
| Doubling of ALT with drug alone | Doubling of ALP (or TBIL) with drug alone | +3 | ||
| Doubling of ALT with the suspect drug combined with another drug which had been given at the time of onset of the initial injury | Doubling of ALP (or TBIL) with the suspect drug combined with another drug which had been given at the time of onset of the initial injury | +1 | ||
| Increase in ALT but less than ULN with drug alone | Increase in ALP (or TBIL) but less than ULN with drug alone | −2 | ||
| Other situations | Other situations | 0 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weber, S.; Gerbes, A.L. Challenges and Future of Drug-Induced Liver Injury Research—Laboratory Tests. Int. J. Mol. Sci. 2022, 23, 6049. https://doi.org/10.3390/ijms23116049
Weber S, Gerbes AL. Challenges and Future of Drug-Induced Liver Injury Research—Laboratory Tests. International Journal of Molecular Sciences. 2022; 23(11):6049. https://doi.org/10.3390/ijms23116049
Chicago/Turabian StyleWeber, Sabine, and Alexander L. Gerbes. 2022. "Challenges and Future of Drug-Induced Liver Injury Research—Laboratory Tests" International Journal of Molecular Sciences 23, no. 11: 6049. https://doi.org/10.3390/ijms23116049
APA StyleWeber, S., & Gerbes, A. L. (2022). Challenges and Future of Drug-Induced Liver Injury Research—Laboratory Tests. International Journal of Molecular Sciences, 23(11), 6049. https://doi.org/10.3390/ijms23116049







