Emerging Concepts in Defective Macrophage Phagocytosis in Cystic Fibrosis
Abstract
1. Introduction
2. Receptor-Initiated Phagocytosis
2.1. Pattern Recognition Receptors
2.2. Opsonic Receptors
2.3. Apoptotic Receptors
2.4. Factors That Influence Phagocytosis
2.5. Fcγ Receptors
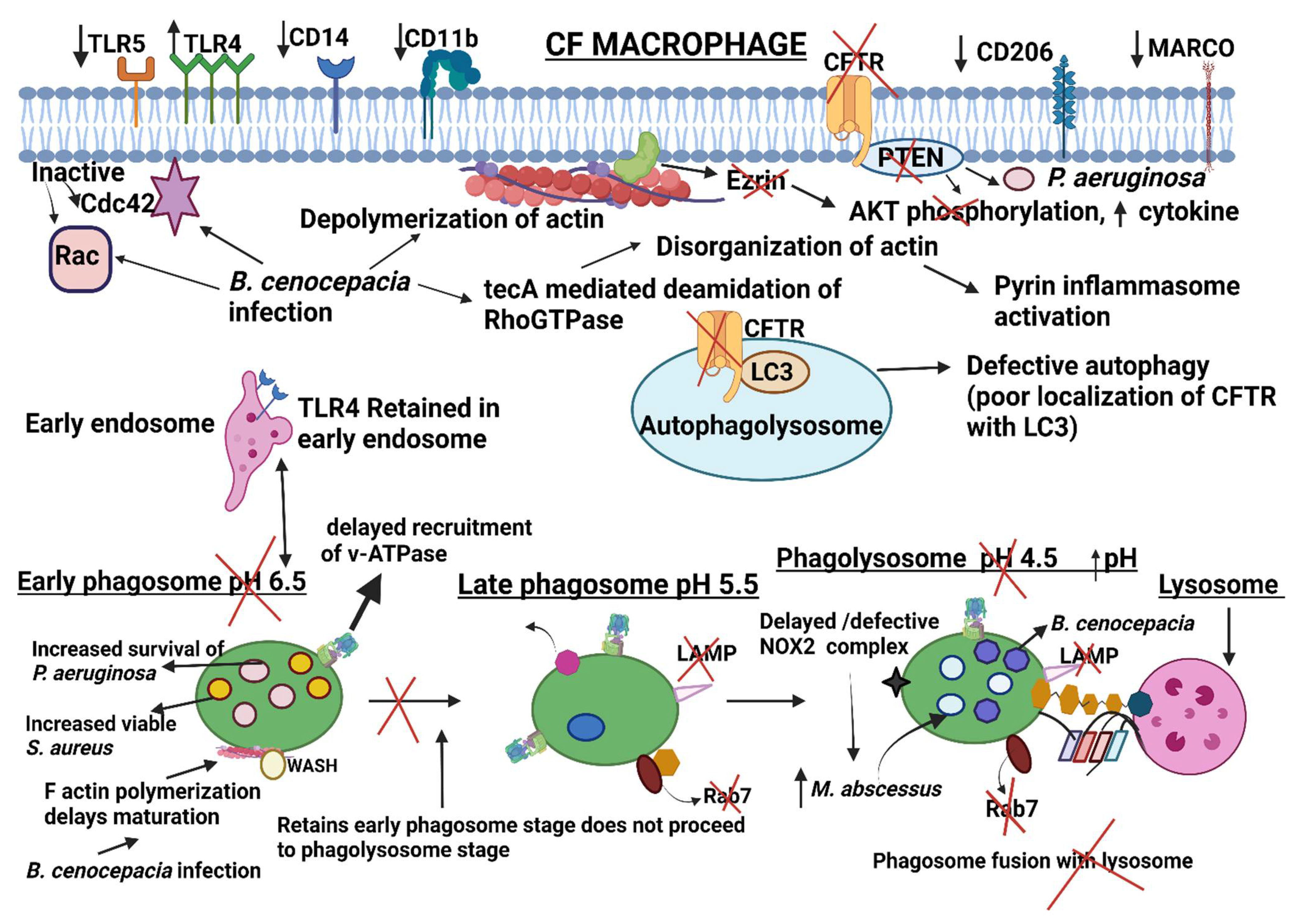
2.6. Dysregulation of Receptors during Phagocytosis in CF Macrophages
3. Phagosome Formation
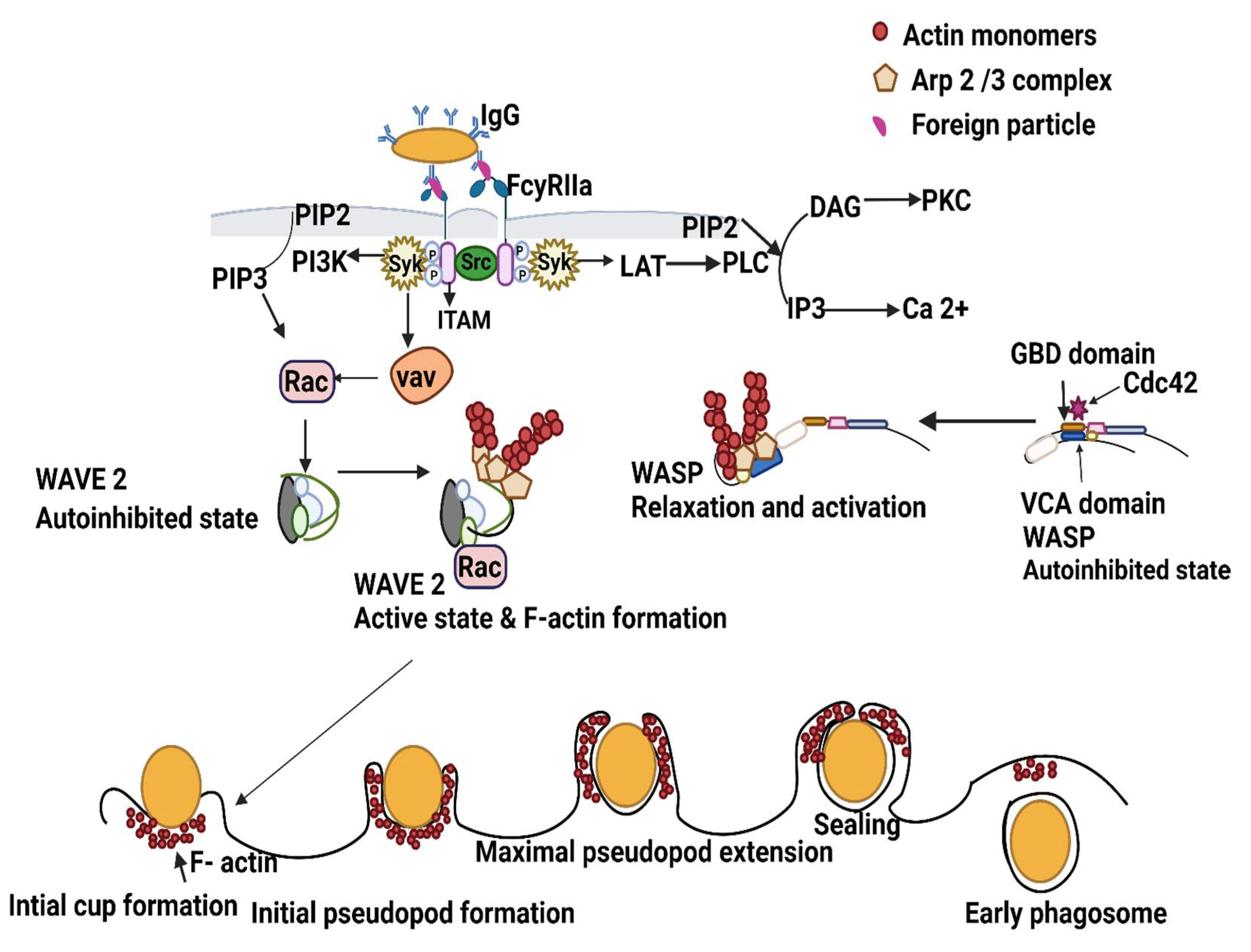
3.1. Overview of FcγR-Mediated Normal Phagosome Formation
3.2. Dysregulated Actin and Actin Regulating Proteins/Lipids during Infection with Opportunistic CF Pathogens
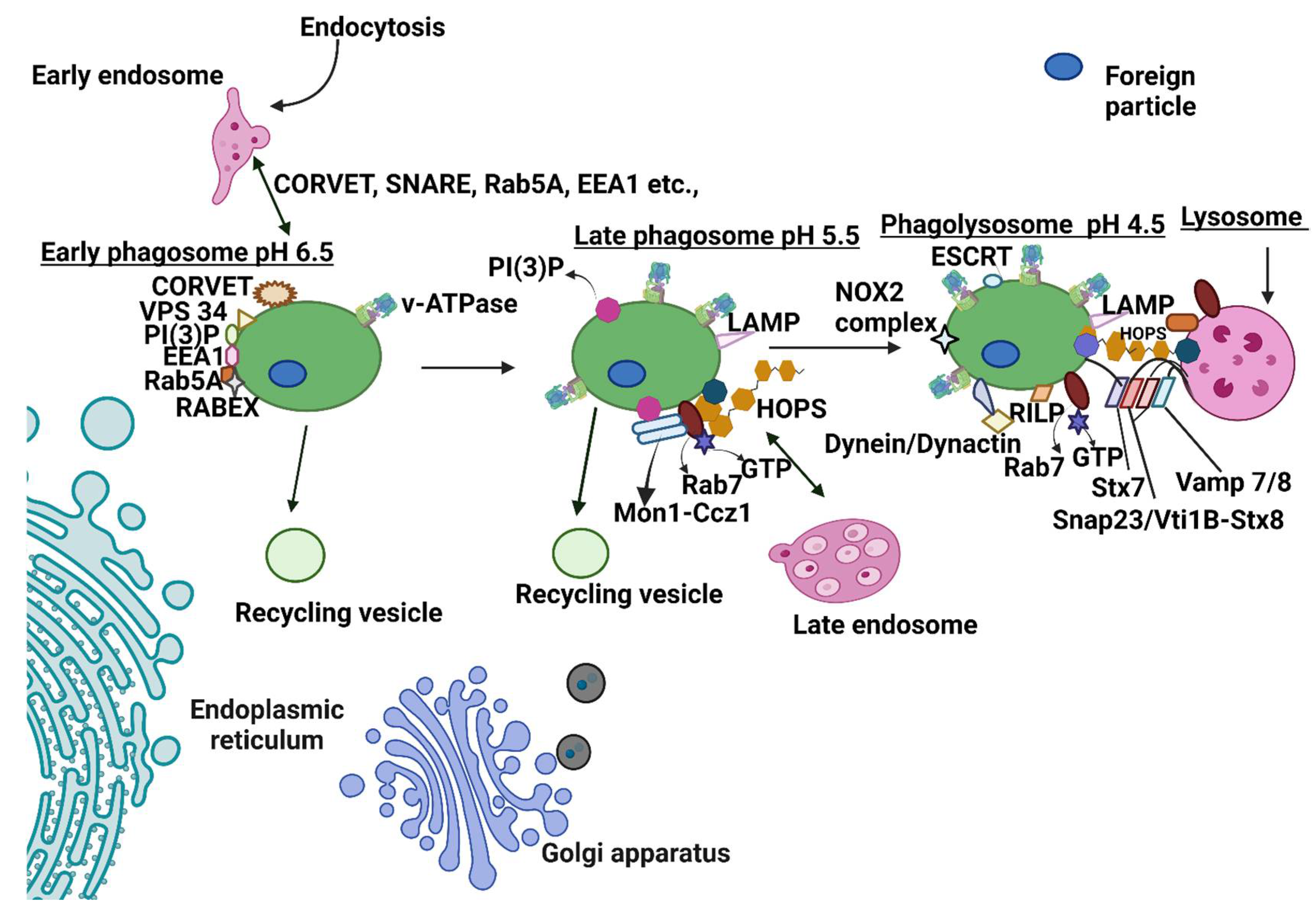
4. Normal Phagosome Maturation
4.1. Early Phagosome: Fusion of Early Phagosome with Early Endosome
4.2. Late Phagosome: Late-Stage Phagosome Fusion with a Late Endosome
4.3. Phagolysosome Formation: Fusion with the Lysosome
5. Specialized Vacuoles: Autophagy and LC3-Associated Phagocytosis (LAP) in CF
Inhibition of Phagosome Maturation in CF and Impairment of Antimicrobial Properties by Pathogens
6. CFTR Modulators/Other Therapeutics and CF Phagocytosis
6.1. CFTR Modulators
6.2. Alternative Agents: Epigallocatechin-3-Gallate, Cysteamine, and Roscovitine
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McGarry, M.E.; McColley, S.A. Cystic fibrosis patients of minority race and ethnicity less likely eligible for cftr modulators based on cftr genotype. Pediatr. Pulmonol. 2021, 56, 1496–1503. [Google Scholar] [CrossRef] [PubMed]
- Fraser-Pitt, D.; O’Neil, D. Cystic fibrosis—a multiorgan protein misfolding disease. Future Sci. OA 2015, 1, FSO57. [Google Scholar] [CrossRef]
- De Boeck, K. Cystic fibrosis in the year 2020: A disease with a new face. Acta Paediatr. 2020, 109, 893–899. [Google Scholar] [CrossRef]
- Kreda, S.M.; Davis, C.W.; Rose, M.C. Cftr, mucins, and mucus obstruction in cystic fibrosis. Cold Spring Harb. Perspect Med. 2012, 2, a009589. [Google Scholar] [CrossRef]
- Keown, K.; Brown, R.; Doherty, D.F.; Houston, C.; McKelvey, M.C.; Creane, S.; Linden, D.; McAuley, D.F.; Kidney, J.C.; Weldon, S.; et al. Airway inflammation and host responses in the era of cftr modulators. Int. J. Mol. Sci. 2020, 21, 6379. [Google Scholar] [CrossRef]
- Aghasafari, P.; George, U.; Pidaparti, R. A review of inflammatory mechanism in airway diseases. Inflamm. Res. 2019, 68, 59–74. [Google Scholar] [CrossRef]
- Allard, B.; Panariti, A.; Martin, J.G. Alveolar macrophages in the resolution of inflammation, tissue repair, and tolerance to infection. Front Immunol. 2018, 9, 1777. [Google Scholar] [CrossRef]
- Neupane, A.S.; Willson, M.; Chojnacki, A.K.; Vargas, E.S.C.F.; Morehouse, C.; Carestia, A.; Keller, A.E.; Peiseler, M.; DiGiandomenico, A.; Kelly, M.M.; et al. Patrolling alveolar macrophages conceal bacteria from the immune system to maintain homeostasis. Cell 2020, 183, 110–125.e11. [Google Scholar] [CrossRef]
- Prame Kumar, K.; Nicholls, A.J.; Wong, C.H.Y. Partners in crime: Neutrophils and monocytes/macrophages in inflammation and disease. Cell Tissue Res. 2018, 371, 551–565. [Google Scholar] [CrossRef]
- Shapouri-Moghaddam, A.; Mohammadian, S.; Vazini, H.; Taghadosi, M.; Esmaeili, S.A.; Mardani, F.; Seifi, B.; Mohammadi, A.; Afshari, J.T.; Sahebkar, A. Macrophage plasticity, polarization, and function in health and disease. J. Cell Physiol. 2018, 233, 6425–6440. [Google Scholar] [CrossRef]
- Leveque, M.; Le Trionnaire, S.; Del Porto, P.; Martin-Chouly, C. The impact of impaired macrophage functions in cystic fibrosis disease progression. J. Cyst. Fibros 2017, 16, 443–453. [Google Scholar] [CrossRef]
- Donnelly, L.E.; Barnes, P.J. Defective phagocytosis in airways disease. Chest 2012, 141, 1055–1062. [Google Scholar] [CrossRef]
- Lee, H.J.; Woo, Y.; Hahn, T.W.; Jung, Y.M.; Jung, Y.J. Formation and maturation of the phagosome: A key mechanism in innate immunity against intracellular bacterial infection. Microorganisms 2020, 8, 1298. [Google Scholar] [CrossRef]
- Herre, J.; Marshall, A.S.; Caron, E.; Edwards, A.D.; Williams, D.L.; Schweighoffer, E.; Tybulewicz, V.; Reis e Sousa, C.; Gordon, S.; Brown, G.D. Dectin-1 uses novel mechanisms for yeast phagocytosis in macrophages. Blood 2004, 104, 4038–4045. [Google Scholar] [CrossRef]
- Ezekowitz, R.A.; Sastry, K.; Bailly, P.; Warner, A. Molecular characterization of the human macrophage mannose receptor: Demonstration of multiple carbohydrate recognition-like domains and phagocytosis of yeasts in cos-1 cells. J. Exp. Med. 1990, 172, 1785–1794. [Google Scholar] [CrossRef]
- Schiff, D.E.; Kline, L.; Soldau, K.; Lee, J.D.; Pugin, J.; Tobias, P.S.; Ulevitch, R.J. Phagocytosis of gram-negative bacteria by a unique cd14-dependent mechanism. J. Leukoc. Biol. 1997, 62, 786–794. [Google Scholar] [CrossRef] [PubMed]
- Peiser, L.; Gough, P.J.; Kodama, T.; Gordon, S. Macrophage class a scavenger receptor-mediated phagocytosis of escherichia coli: Role of cell heterogeneity, microbial strain, and culture conditions in vitro. Infect. Immun. 2000, 68, 1953–1963. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.N.; Serghides, L.; Smith, T.G.; Febbraio, M.; Silverstein, R.L.; Kurtz, T.W.; Pravenec, M.; Kain, K.C. Cd36 mediates the phagocytosis of plasmodium falciparum-infected erythrocytes by rodent macrophages. J. Infect. Dis. 2004, 189, 204–213. [Google Scholar] [CrossRef]
- Anderson, C.L.; Shen, L.; Eicher, D.M.; Wewers, M.D.; Gill, J.K. Phagocytosis mediated by three distinct fc gamma receptor classes on human leukocytes. J. Exp. Med. 1990, 171, 1333–1345. [Google Scholar] [CrossRef]
- Descamps, D.; Le Gars, M.; Balloy, V.; Barbier, D.; Maschalidi, S.; Tohme, M.; Chignard, M.; Ramphal, R.; Manoury, B.; Sallenave, J.M. Toll-like receptor 5 (tlr5), il-1beta secretion, and asparagine endopeptidase are critical factors for alveolar macrophage phagocytosis and bacterial killing. Proc. Natl. Acad. Sci. USA 2012, 109, 1619–1624. [Google Scholar] [CrossRef] [PubMed]
- van Spriel, A.B.; van den Herik-Oudijk, I.E.; van Sorge, N.M.; Vile, H.A.; van Strijp, J.A.; van de Winkel, J.G. Effective phagocytosis and killing of candida albicans via targeting fcgammari (cd64) or fcalphari (cd89) on neutrophils. J. Infect. Dis. 1999, 179, 661–669. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Daeron, M.; Malbec, O.; Bonnerot, C.; Latour, S.; Segal, D.M.; Fridman, W.H. Tyrosine-containing activation motif-dependent phagocytosis in mast cells. J. Immunol. 1994, 152, 783–792. [Google Scholar] [PubMed]
- Ghiran, I.; Barbashov, S.F.; Klickstein, L.B.; Tas, S.W.; Jensenius, J.C.; Nicholson-Weller, A. Complement receptor 1/cd35 is a receptor for mannan-binding lectin. J. Exp. Med. 2000, 192, 1797–1808. [Google Scholar] [CrossRef] [PubMed]
- Ross, G.D.; Reed, W.; Dalzell, J.G.; Becker, S.E.; Hogg, N. Macrophage cytoskeleton association with cr3 and cr4 regulates receptor mobility and phagocytosis of ic3b-opsonized erythrocytes. J. Leukoc. Biol. 1992, 51, 109–117. [Google Scholar] [CrossRef]
- Ravichandran, K.S. Find-me and eat-me signals in apoptotic cell clearance: Progress and conundrums. J. Exp. Med. 2010, 207, 1807–1817. [Google Scholar] [CrossRef]
- Kobayashi, N.; Karisola, P.; Pena-Cruz, V.; Dorfman, D.M.; Jinushi, M.; Umetsu, S.E.; Butte, M.J.; Nagumo, H.; Chernova, I.; Zhu, B.; et al. Tim-1 and tim-4 glycoproteins bind phosphatidylserine and mediate uptake of apoptotic cells. Immunity 2007, 27, 927–940. [Google Scholar] [CrossRef]
- Park, D.; Tosello-Trampont, A.C.; Elliott, M.R.; Lu, M.; Haney, L.B.; Ma, Z.; Klibanov, A.L.; Mandell, J.W.; Ravichandran, K.S. Bai1 is an engulfment receptor for apoptotic cells upstream of the elmo/dock180/rac module. Nature 2007, 450, 430–434. [Google Scholar] [CrossRef]
- Greenberg, M.E.; Sun, M.; Zhang, R.; Febbraio, M.; Silverstein, R.; Hazen, S.L. Oxidized phosphatidylserine-cd36 interactions play an essential role in macrophage-dependent phagocytosis of apoptotic cells. J. Exp. Med. 2006, 203, 2613–2625. [Google Scholar] [CrossRef]
- Hanayama, R.; Tanaka, M.; Miwa, K.; Shinohara, A.; Iwamatsu, A.; Nagata, S. Identification of a factor that links apoptotic cells to phagocytes. Nature 2002, 417, 182–187. [Google Scholar] [CrossRef]
- Albert, M.L.; Kim, J.I.; Birge, R.B. Alphavbeta5 integrin recruits the crkii-dock180-rac1 complex for phagocytosis of apoptotic cells. Nat. Cell Biol. 2000, 2, 899–905. [Google Scholar] [CrossRef]
- Park, S.Y.; Jung, M.Y.; Kim, H.J.; Lee, S.J.; Kim, S.Y.; Lee, B.H.; Kwon, T.H.; Park, R.W.; Kim, I.S. Rapid cell corpse clearance by stabilin-2, a membrane phosphatidylserine receptor. Cell Death Differ. 2008, 15, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Elmore, S. Apoptosis: A review of programmed cell death. Toxicol. Pathol. 2007, 35, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Quarleri, J.; Cevallos, C.; Delpino, M.V. Apoptosis in infectious diseases as a mechanism of immune evasion and survival. Adv. Protein Chem. Struct. Biol. 2021, 125, 1–24. [Google Scholar] [PubMed]
- Obeng, E. Apoptosis (programmed cell death) and its signals—A review. Braz J. Biol. 2021, 81, 1133–1143. [Google Scholar] [CrossRef]
- Jaumouille, V.; Grinstein, S. Receptor mobility, the cytoskeleton, and particle binding during phagocytosis. Curr. Opin. Cell Biol. 2011, 23, 22–29. [Google Scholar] [CrossRef]
- Caron, E.; Self, A.J.; Hall, A. The gtpase rap1 controls functional activation of macrophage integrin alphambeta2 by lps and other inflammatory mediators. Curr. Biol. 2000, 10, 974–978. [Google Scholar] [CrossRef]
- Ortiz-Stern, A.; Rosales, C. Cross-talk between fc receptors and integrins. Immunol. Lett. 2003, 90, 137–143. [Google Scholar] [CrossRef]
- Vachon, E.; Martin, R.; Kwok, V.; Cherepanov, V.; Chow, C.W.; Doerschuk, C.M.; Plumb, J.; Grinstein, S.; Downey, G.P. Cd44-mediated phagocytosis induces inside-out activation of complement receptor-3 in murine macrophages. Blood 2007, 110, 4492–4502. [Google Scholar] [CrossRef]
- Nimmerjahn, F.; Ravetch, J.V. Fcgammars in health and disease. Curr. Top. Microbiol. Immunol. 2011, 350, 105–125. [Google Scholar]
- Zhang, Y.; Hoppe, A.D.; Swanson, J.A. Coordination of fc receptor signaling regulates cellular commitment to phagocytosis. Proc. Natl. Acad. Sci. USA 2010, 107, 19332–19337. [Google Scholar] [CrossRef]
- Sanchez-Mejorada, G.; Rosales, C. Signal transduction by immunoglobulin fc receptors. J. Leukoc. Biol. 1998, 63, 521–533. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Mejorada, G.; Rosales, C. Fcgamma receptor-mediated mitogen-activated protein kinase activation in monocytes is independent of ras. J. Biol. Chem. 1998, 273, 27610–27619. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Tohyama, Y.; Kadono, T.; He, J.; Miah, S.M.; Hazama, R.; Tanaka, C.; Tohyama, K.; Yamamura, H. Protein-tyrosine kinase syk is required for pathogen engulfment in complement-mediated phagocytosis. Blood 2006, 107, 4554–4562. [Google Scholar] [CrossRef]
- Tabata, H.; Morita, H.; Kaji, H.; Tohyama, K.; Tohyama, Y. Syk facilitates phagosome-lysosome fusion by regulating actin-remodeling in complement-mediated phagocytosis. Sci. Rep. 2020, 10, 22086. [Google Scholar] [CrossRef]
- Simonin-Le Jeune, K.; Le Jeune, A.; Jouneau, S.; Belleguic, C.; Roux, P.F.; Jaguin, M.; Dimanche-Boitre, M.T.; Lecureur, V.; Leclercq, C.; Desrues, B.; et al. Impaired functions of macrophage from cystic fibrosis patients: Cd11b, tlr-5 decrease and scd14, inflammatory cytokines increase. PLoS ONE 2013, 8, e75667. [Google Scholar] [CrossRef]
- Ettorre, M.; Verze, G.; Caldrer, S.; Johansson, J.; Calcaterra, E.; Assael, B.M.; Melotti, P.; Sorio, C.; Buffelli, M. Electrophysiological evaluation of cystic fibrosis conductance transmembrane regulator (cftr) expression in human monocytes. Biochim. Biophys. Acta 2014, 1840, 3088–3095. [Google Scholar] [CrossRef]
- Tarique, A.A.; Sly, P.D.; Cardenas, D.G.; Luo, L.; Stow, J.L.; Bell, S.C.; Wainwright, C.E.; Fantino, E. Differential expression of genes and receptors in monocytes from patients with cystic fibrosis. J. Cyst. Fibros 2019, 18, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Sturges, N.C.; Wikstrom, M.E.; Winfield, K.R.; Gard, S.E.; Brennan, S.; Sly, P.D.; Upham, J.W.; Australian Respiratory Early Surveillance Team for Cystic Fibrosis. Monocytes from children with clinically stable cystic fibrosis show enhanced expression of toll-like receptor 4. Pediatr. Pulmonol. 2010, 45, 883–889. [Google Scholar] [CrossRef]
- Bruscia, E.M.; Zhang, P.X.; Satoh, A.; Caputo, C.; Medzhitov, R.; Shenoy, A.; Egan, M.E.; Krause, D.S. Abnormal trafficking and degradation of tlr4 underlie the elevated inflammatory response in cystic fibrosis. J. Immunol. 2011, 186, 6990–6998. [Google Scholar] [CrossRef]
- Alexis, N.E.; Muhlebach, M.S.; Peden, D.B.; Noah, T.L. Attenuation of host defense function of lung phagocytes in young cystic fibrosis patients. J. Cyst. Fibros 2006, 5, 17–25. [Google Scholar] [CrossRef]
- Wright, A.K.; Rao, S.; Range, S.; Eder, C.; Hofer, T.P.; Frankenberger, M.; Kobzik, L.; Brightling, C.; Grigg, J.; Ziegler-Heitbrock, L. Pivotal advance: Expansion of small sputum macrophages in cf: Failure to express marco and mannose receptors. J. Leukoc. Biol. 2009, 86, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Van de Weert-van Leeuwen, P.B.; Van Meegen, M.A.; Speirs, J.J.; Pals, D.J.; Rooijakkers, S.H.; Van der Ent, C.K.; Terheggen-Lagro, S.W.; Arets, H.G.; Beekman, J.M. Optimal complement-mediated phagocytosis of pseudomonas aeruginosa by monocytes is cystic fibrosis transmembrane conductance regulator-dependent. Am. J. Respir. Cell Mol. Biol. 2013, 49, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Kummarapurugu, A.B.; Hawkridge, A.; Ghosh, S.; Zheng, S.; Voynow, J.A. Neutrophil elastase-regulated macrophage sheddome/secretome and phagocytic failure. Am. J. Physiol. Lung Cell Mol. Physiol. 2021, 321, L555–L565. [Google Scholar] [CrossRef] [PubMed]
- Mylvaganam, S.; Freeman, S.A.; Grinstein, S. The cytoskeleton in phagocytosis and macropinocytosis. Curr. Biol. 2021, 31, R619–R632. [Google Scholar] [CrossRef]
- Tsuboi, S.; Takada, H.; Hara, T.; Mochizuki, N.; Funyu, T.; Saitoh, H.; Terayama, Y.; Yamaya, K.; Ohyama, C.; Nonoyama, S.; et al. Fbp17 mediates a common molecular step in the formation of podosomes and phagocytic cups in macrophages. J. Biol. Chem. 2009, 284, 8548–8556. [Google Scholar] [CrossRef]
- Magenau, A.; Benzing, C.; Proschogo, N.; Don, A.S.; Hejazi, L.; Karunakaran, D.; Jessup, W.; Gaus, K. Phagocytosis of igg-coated polystyrene beads by macrophages induces and requires high membrane order. Traffic 2011, 12, 1730–1743. [Google Scholar] [CrossRef]
- Guo, S.; Sokolova, O.S.; Chung, J.; Padrick, S.; Gelles, J.; Goode, B.L. Abp1 promotes arp2/3 complex-dependent actin nucleation and stabilizes branch junctions by antagonizing gmf. Nat. Commun. 2018, 9, 2895. [Google Scholar] [CrossRef]
- Rougerie, P.; Miskolci, V.; Cox, D. Generation of membrane structures during phagocytosis and chemotaxis of macrophages: Role and regulation of the actin cytoskeleton. Immunol. Rev. 2013, 256, 222–239. [Google Scholar] [CrossRef]
- Campellone, K.G.; Cheng, H.C.; Robbins, D.; Siripala, A.D.; McGhie, E.J.; Hayward, R.D.; Welch, M.D.; Rosen, M.K.; Koronakis, V.; Leong, J.M. Repetitive n-wasp-binding elements of the enterohemorrhagic escherichia coli effector espf(u) synergistically activate actin assembly. PLoS Pathog. 2008, 4, e1000191. [Google Scholar] [CrossRef]
- Zuchero, J.B.; Coutts, A.S.; Quinlan, M.E.; Thangue, N.B.; Mullins, R.D. P53-cofactor jmy is a multifunctional actin nucleation factor. Nat. Cell Biol. 2009, 11, 451–459. [Google Scholar] [CrossRef]
- Kheir, W.A.; Gevrey, J.C.; Yamaguchi, H.; Isaac, B.; Cox, D. A wave2-abi1 complex mediates csf-1-induced f-actin-rich membrane protrusions and migration in macrophages. J. Cell Sci. 2005, 118, 5369–5379. [Google Scholar] [CrossRef] [PubMed]
- Griffin, F.M., Jr.; Griffin, J.A.; Silverstein, S.C. Studies on the mechanism of phagocytosis. Ii. The interaction of macrophages with anti-immunoglobulin igg-coated bone marrow-derived lymphocytes. J. Exp. Med. 1976, 144, 788–809. [Google Scholar] [CrossRef] [PubMed]
- Beemiller, P.; Zhang, Y.; Mohan, S.; Levinsohn, E.; Gaeta, I.; Hoppe, A.D.; Swanson, J.A. A cdc42 activation cycle coordinated by pi 3-kinase during fc receptor-mediated phagocytosis. Mol. Biol. Cell 2010, 21, 470–480. [Google Scholar] [CrossRef]
- Vergne, I.; Chua, J.; Lee, H.H.; Lucas, M.; Belisle, J.; Deretic, V. Mechanism of phagolysosome biogenesis block by viable mycobacterium tuberculosis. Proc. Natl. Acad. Sci. USA 2005, 102, 4033–4038. [Google Scholar] [CrossRef]
- Niebuhr, K.; Giuriato, S.; Pedron, T.; Philpott, D.J.; Gaits, F.; Sable, J.; Sheetz, M.P.; Parsot, C.; Sansonetti, P.J.; Payrastre, B. Conversion of ptdins(4,5)p(2) into ptdins(5)p by the s.Flexneri effector ipgd reorganizes host cell morphology. EMBO J. 2002, 21, 5069–5078. [Google Scholar] [CrossRef] [PubMed]
- Bakowski, M.A.; Braun, V.; Lam, G.Y.; Yeung, T.; Heo, W.D.; Meyer, T.; Finlay, B.B.; Grinstein, S.; Brumell, J.H. The phosphoinositide phosphatase sopb manipulates membrane surface charge and trafficking of the salmonella-containing vacuole. Cell Host Microbe 2010, 7, 453–462. [Google Scholar] [CrossRef]
- Swanson, J.A. Phosphoinositides and engulfment. Cell Microbiol. 2014, 16, 1473–1483. [Google Scholar] [CrossRef]
- Levin, R.; Grinstein, S.; Schlam, D. Phosphoinositides in phagocytosis and macropinocytosis. Biochim. Biophys. Acta 2015, 1851, 805–823. [Google Scholar] [CrossRef]
- Jeschke, A.; Haas, A. Deciphering the roles of phosphoinositide lipids in phagolysosome biogenesis. Commun. Integr. Biol. 2016, 9, e1174798. [Google Scholar] [CrossRef]
- Lees, J.A.; Li, P.; Kumar, N.; Weisman, L.S.; Reinisch, K.M. Insights into lysosomal pi(3,5)p2 homeostasis from a structural-biochemical analysis of the pikfyve lipid kinase complex. Mol. Cell 2020, 80, 736–743.e4. [Google Scholar] [CrossRef]
- Park, H.; Cox, D. Cdc42 regulates fc gamma receptor-mediated phagocytosis through the activation and phosphorylation of wiskott-aldrich syndrome protein (wasp) and neural-wasp. Mol. Biol. Cell 2009, 20, 4500–4508. [Google Scholar] [CrossRef] [PubMed]
- Caron, E.; Hall, A. Identification of two distinct mechanisms of phagocytosis controlled by different rho gtpases. Science 1998, 282, 1717–1721. [Google Scholar] [CrossRef]
- Colucci, A.M.; Spinosa, M.R.; Bucci, C. Expression, assay, and functional properties of rilp. Methods Enzymol. 2005, 403, 664–675. [Google Scholar]
- Kim, J.G.; Moon, M.Y.; Kim, H.J.; Li, Y.; Song, D.K.; Kim, J.S.; Lee, J.Y.; Kim, J.; Kim, S.C.; Park, J.B. Ras-related gtpases rap1 and rhoa collectively induce the phagocytosis of serum-opsonized zymosan particles in macrophages. J. Biol. Chem. 2012, 287, 5145–5155. [Google Scholar] [CrossRef] [PubMed]
- Biswas, L.; Gotz, F. Molecular mechanisms of staphylococcus and pseudomonas interactions in cystic fibrosis. Front Cell Infect. Microbiol. 2021, 11, 824042. [Google Scholar] [CrossRef] [PubMed]
- Armbruster, C.R.; Wolter, D.J.; Mishra, M.; Hayden, H.S.; Radey, M.C.; Merrihew, G.; MacCoss, M.J.; Burns, J.; Wozniak, D.J.; Parsek, M.R.; et al. Staphylococcus aureus protein a mediates interspecies interactions at the cell surface of pseudomonas aeruginosa. mBio 2016, 7, e00538-16. [Google Scholar] [CrossRef]
- Isles, A.; Maclusky, I.; Corey, M.; Gold, R.; Prober, C.; Fleming, P.; Levison, H. Pseudomonas cepacia infection in cystic fibrosis: An emerging problem. J. Pediatr. 1984, 104, 206–210. [Google Scholar] [CrossRef]
- Saldias, M.S.; Valvano, M.A. Interactions of burkholderia cenocepacia and other burkholderia cepacia complex bacteria with epithelial and phagocytic cells. Microbiology 2009, 155, 2809–2817. [Google Scholar] [CrossRef]
- Schwab, U.; Abdullah, L.H.; Perlmutt, O.S.; Albert, D.; Davis, C.W.; Arnold, R.R.; Yankaskas, J.R.; Gilligan, P.; Neubauer, H.; Randell, S.H.; et al. Localization of burkholderia cepacia complex bacteria in cystic fibrosis lungs and interactions with pseudomonas aeruginosa in hypoxic mucus. Infect. Immun. 2014, 82, 4729–4745. [Google Scholar] [CrossRef]
- Flannagan, R.S.; Jaumouille, V.; Huynh, K.K.; Plumb, J.D.; Downey, G.P.; Valvano, M.A.; Grinstein, S. Burkholderia cenocepacia disrupts host cell actin cytoskeleton by inactivating rac and cdc42. Cell Microbiol. 2012, 14, 239–254. [Google Scholar] [CrossRef]
- Aubert, D.F.; Xu, H.; Yang, J.; Shi, X.; Gao, W.; Li, L.; Bisaro, F.; Chen, S.; Valvano, M.A.; Shao, F. A burkholderia type vi effector deamidates rho gtpases to activate the pyrin inflammasome and trigger inflammation. Cell Host Microbe 2016, 19, 664–674. [Google Scholar] [CrossRef] [PubMed]
- Walpole, G.F.W.; Plumb, J.D.; Chung, D.; Tang, B.; Boulay, B.; Osborne, D.G.; Piotrowski, J.T.; Catz, S.D.; Billadeau, D.D.; Grinstein, S.; et al. Inactivation of rho gtpases by burkholderia cenocepacia induces a wash-mediated actin polymerization that delays phagosome maturation. Cell Rep. 2020, 31, 107721. [Google Scholar] [CrossRef] [PubMed]
- Miki, H.; Takenawa, T. Regulation of actin dynamics by wasp family proteins. J. Biochem. 2003, 134, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Rosales-Reyes, R.; Aubert, D.F.; Tolman, J.S.; Amer, A.O.; Valvano, M.A. Burkholderia cenocepacia type vi secretion system mediates escape of type ii secreted proteins into the cytoplasm of infected macrophages. PLoS ONE 2012, 7, e41726. [Google Scholar]
- Rosales-Reyes, R.; Skeldon, A.M.; Aubert, D.F.; Valvano, M.A. The type vi secretion system of burkholderia cenocepacia affects multiple rho family gtpases disrupting the actin cytoskeleton and the assembly of nadph oxidase complex in macrophages. Cell Microbiol. 2012, 14, 255–273. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Yang, J.; Gao, W.; Li, L.; Li, P.; Zhang, L.; Gong, Y.N.; Peng, X.; Xi, J.J.; Chen, S.; et al. Innate immune sensing of bacterial modifications of rho gtpases by the pyrin inflammasome. Nature 2014, 513, 237–241. [Google Scholar] [CrossRef]
- Guggino, W.B.; Stanton, B.A. New insights into cystic fibrosis: Molecular switches that regulate cftr. Nat. Rev. Mol. Cell Biol. 2006, 7, 426–436. [Google Scholar] [CrossRef]
- Gautreau, A.; Poullet, P.; Louvard, D.; Arpin, M. Ezrin, a plasma membrane-microfilament linker, signals cell survival through the phosphatidylinositol 3-kinase/akt pathway. Proc. Natl. Acad. Sci. USA 1999, 96, 7300–7305. [Google Scholar] [CrossRef]
- Di Pietro, C.; Zhang, P.X.; O’Rourke, T.K.; Murray, T.S.; Wang, L.; Britto, C.J.; Koff, J.L.; Krause, D.S.; Egan, M.E.; Bruscia, E.M. Ezrin links cftr to tlr4 signaling to orchestrate anti-bacterial immune response in macrophages. Sci. Rep. 2017, 7, 10882. [Google Scholar] [CrossRef]
- Lovewell, R.R.; Hayes, S.M.; O’Toole, G.A.; Berwin, B. Pseudomonas aeruginosa flagellar motility activates the phagocyte pi3k/akt pathway to induce phagocytic engulfment. Am. J. Physiol. Lung Cell Mol. Physiol. 2014, 306, L698–L707. [Google Scholar] [CrossRef]
- Leveque, M.; Penna, A.; Le Trionnaire, S.; Belleguic, C.; Desrues, B.; Brinchault, G.; Jouneau, S.; Lagadic-Gossmann, D.; Martin-Chouly, C. Phagocytosis depends on trpv2-mediated calcium influx and requires trpv2 in lipids rafts: Alteration in macrophages from patients with cystic fibrosis. Sci. Rep. 2018, 8, 4310. [Google Scholar] [CrossRef] [PubMed]
- Poerio, N.; De Santis, F.; Rossi, A.; Ranucci, S.; De Fino, I.; Henriquez, A.; D’Andrea, M.M.; Ciciriello, F.; Lucidi, V.; Nisini, R.; et al. Liposomes loaded with phosphatidylinositol 5-phosphate improve the antimicrobial response to pseudomonas aeruginosa in impaired macrophages from cystic fibrosis patients and limit airway inflammatory response. Front. Immunol. 2020, 11, 532225. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Ghosh, R.N.; Maxfield, F.R. Endocytosis. Physiol. Rev. 1997, 77, 759–803. [Google Scholar] [CrossRef]
- Novick, P.; Medkova, M.; Dong, G.; Hutagalung, A.; Reinisch, K.; Grosshans, B. Interactions between rabs, tethers, snares and their regulators in exocytosis. Biochem. Soc. Trans. 2006, 34, 683–686. [Google Scholar] [CrossRef]
- Jovic, M.; Sharma, M.; Rahajeng, J.; Caplan, S. The early endosome: A busy sorting station for proteins at the crossroads. Histol. Histopathol. 2010, 25, 99–112. [Google Scholar]
- Lurick, A.; Kummel, D.; Ungermann, C. Multisubunit tethers in membrane fusion. Curr. Biol. 2018, 28, R417–R420. [Google Scholar] [CrossRef]
- Lobingier, B.T.; Merz, A.J. Sec1/munc18 protein vps33 binds to snare domains and the quaternary snare complex. Mol. Biol. Cell 2012, 23, 4611–4622. [Google Scholar] [CrossRef]
- McBride, H.M.; Rybin, V.; Murphy, C.; Giner, A.; Teasdale, R.; Zerial, M. Oligomeric complexes link rab5 effectors with nsf and drive membrane fusion via interactions between eea1 and syntaxin 13. Cell 1999, 98, 377–386. [Google Scholar] [CrossRef]
- Christoforidis, S.; McBride, H.M.; Burgoyne, R.D.; Zerial, M. The rab5 effector eea1 is a core component of endosome docking. Nature 1999, 397, 621–625. [Google Scholar] [CrossRef]
- Botelho, R.J.; Hackam, D.J.; Schreiber, A.D.; Grinstein, S. Role of copi in phagosome maturation. J. Biol. Chem. 2000, 275, 15717–15727. [Google Scholar] [CrossRef]
- Rojas, R.; van Vlijmen, T.; Mardones, G.A.; Prabhu, Y.; Rojas, A.L.; Mohammed, S.; Heck, A.J.; Raposo, G.; van der Sluijs, P.; Bonifacino, J.S. Regulation of retromer recruitment to endosomes by sequential action of rab5 and rab7. J. Cell Biol. 2008, 183, 513–526. [Google Scholar] [CrossRef]
- Damiani, M.T.; Pavarotti, M.; Leiva, N.; Lindsay, A.J.; McCaffrey, M.W.; Colombo, M.I. Rab coupling protein associates with phagosomes and regulates recycling from the phagosomal compartment. Traffic 2004, 5, 785–797. [Google Scholar] [CrossRef] [PubMed]
- Maxfield, F.R.; McGraw, T.E. Endocytic recycling. Nat. Rev. Mol. Cell Biol. 2004, 5, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Henne, W.M.; Buchkovich, N.J.; Emr, S.D. The escrt pathway. Dev. Cell 2011, 21, 77–91. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, A.; Haas, A. Sequential actions of phosphatidylinositol phosphates regulate phagosome-lysosome fusion. Mol. Biol. Cell 2018, 29, 452–465. [Google Scholar] [CrossRef]
- Barry, A.O.; Boucherit, N.; Mottola, G.; Vadovic, P.; Trouplin, V.; Soubeyran, P.; Capo, C.; Bonatti, S.; Nebreda, A.; Toman, R.; et al. Impaired stimulation of p38alpha-mapk/vps41-hops by lps from pathogenic coxiella burnetii prevents trafficking to microbicidal phagolysosomes. Cell Host Microbe 2012, 12, 751–763. [Google Scholar] [CrossRef]
- Jiang, P.; Nishimura, T.; Sakamaki, Y.; Itakura, E.; Hatta, T.; Natsume, T.; Mizushima, N. The hops complex mediates autophagosome-lysosome fusion through interaction with syntaxin 17. Mol. Biol. Cell 2014, 25, 1327–1337. [Google Scholar] [CrossRef]
- Khatter, D.; Raina, V.B.; Dwivedi, D.; Sindhwani, A.; Bahl, S.; Sharma, M. The small gtpase arl8b regulates assembly of the mammalian hops complex on lysosomes. J. Cell Sci. 2015, 128, 1746–1761. [Google Scholar] [CrossRef]
- Nickerson, D.P.; Brett, C.L.; Merz, A.J. Vps-c complexes: Gatekeepers of endolysosomal traffic. Curr. Opin. Cell Biol. 2009, 21, 543–551. [Google Scholar] [CrossRef]
- Weiss, G.; Schaible, U.E. Macrophage defense mechanisms against intracellular bacteria. Immunol. Rev. 2015, 264, 182–203. [Google Scholar] [CrossRef]
- Odorizzi, G. The multiple personalities of alix. J. Cell Sci. 2006, 119, 3025–3032. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Johansson, M.; Rocha, N.; Zwart, W.; Jordens, I.; Janssen, L.; Kuijl, C.; Olkkonen, V.M.; Neefjes, J. Activation of endosomal dynein motors by stepwise assembly of rab7-rilp-p150glued, orp1l, and the receptor betalll spectrin. J. Cell Biol. 2007, 176, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Jordens, I.; Fernandez-Borja, M.; Marsman, M.; Dusseljee, S.; Janssen, L.; Calafat, J.; Janssen, H.; Wubbolts, R.; Neefjes, J. The rab7 effector protein rilp controls lysosomal transport by inducing the recruitment of dynein-dynactin motors. Curr. Biol. 2001, 11, 1680–1685. [Google Scholar] [CrossRef]
- Nguyen, J.A.; Yates, R.M. Better together: Current insights into phagosome-lysosome fusion. Front Immunol. 2021, 12, 636078. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Wickner, W. Tethering guides fusion-competent trans-snare assembly. Proc. Natl. Acad. Sci. USA 2019, 116, 13952–13957. [Google Scholar] [CrossRef] [PubMed]
- Starai, V.J.; Hickey, C.M.; Wickner, W. Hops proofreads the trans-snare complex for yeast vacuole fusion. Mol. Biol. Cell 2008, 19, 2500–2508. [Google Scholar] [CrossRef]
- Stroupe, C.; Hickey, C.M.; Mima, J.; Burfeind, A.S.; Wickner, W. Minimal membrane docking requirements revealed by reconstitution of rab gtpase-dependent membrane fusion from purified components. Proc. Natl. Acad. Sci. USA 2009, 106, 17626–17633. [Google Scholar] [CrossRef]
- Xu, H.; Jun, Y.; Thompson, J.; Yates, J.; Wickner, W. Hops prevents the disassembly of trans-snare complexes by sec17p/sec18p during membrane fusion. EMBO J. 2010, 29, 1948–1960. [Google Scholar] [CrossRef]
- Ungermann, C.; Nichols, B.J.; Pelham, H.R.; Wickner, W. A vacuolar v-t-snare complex, the predominant form in vivo and on isolated vacuoles, is disassembled and activated for docking and fusion. J. Cell Biol. 1998, 140, 61–69. [Google Scholar] [CrossRef]
- Hanson, P.I.; Otto, H.; Barton, N.; Jahn, R. The n-ethylmaleimide-sensitive fusion protein and alpha-snap induce a conformational change in syntaxin. J. Biol. Chem. 1995, 270, 16955–16961. [Google Scholar] [CrossRef]
- Yates, R.M.; Hermetter, A.; Russell, D.G. The kinetics of phagosome maturation as a function of phagosome/lysosome fusion and acquisition of hydrolytic activity. Traffic 2005, 6, 413–420. [Google Scholar] [CrossRef]
- Nauseef, W.M. The phagocyte nox2 nadph oxidase in microbial killing and cell signaling. Curr. Opin. Immunol. 2019, 60, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Faure, M.; Lafont, F. Pathogen-induced autophagy signaling in innate immunity. J. Innate Immun. 2013, 5, 456–470. [Google Scholar] [CrossRef]
- Crotzer, V.L.; Blum, J.S. Autophagy and its role in mhc-mediated antigen presentation. J. Immunol. 2009, 182, 3335–3341. [Google Scholar] [CrossRef]
- Klionsky, D.J.; Abdel-Aziz, A.K.; Abdelfatah, S.; Abdellatif, M.; Abdoli, A.; Abel, S.; Abeliovich, H.; Abildgaard, M.H.; Abudu, Y.P.; Acevedo-Arozena, A.; et al. Guidelines for the use and interpretation of assays for monitoring autophagy (4th edition)(1). Autophagy 2021, 17, 1–382. [Google Scholar] [CrossRef] [PubMed]
- Tazi, M.F.; Dakhlallah, D.A.; Caution, K.; Gerber, M.M.; Chang, S.W.; Khalil, H.; Kopp, B.T.; Ahmed, A.E.; Krause, K.; Davis, I.; et al. Elevated mirc1/mir17-92 cluster expression negatively regulates autophagy and cftr (cystic fibrosis transmembrane conductance regulator) function in cf macrophages. Autophagy 2016, 12, 2026–2037. [Google Scholar] [CrossRef] [PubMed]
- Assani, K.; Tazi, M.F.; Amer, A.O.; Kopp, B.T. Ifn-gamma stimulates autophagy-mediated clearance of burkholderia cenocepacia in human cystic fibrosis macrophages. PLoS ONE 2014, 9, e96681. [Google Scholar] [CrossRef] [PubMed]
- Abdulrahman, B.A.; Khweek, A.A.; Akhter, A.; Caution, K.; Kotrange, S.; Abdelaziz, D.H.; Newland, C.; Rosales-Reyes, R.; Kopp, B.; McCoy, K.; et al. Autophagy stimulation by rapamycin suppresses lung inflammation and infection by burkholderia cenocepacia in a model of cystic fibrosis. Autophagy 2011, 7, 1359–1370. [Google Scholar] [CrossRef] [PubMed]
- Assani, K.; Shrestha, C.L.; Rinehardt, H.; Zhang, S.; Robledo-Avila, F.; Wellmerling, J.; Partida-Sanchez, S.; Cormet-Boyaka, E.; Reynolds, S.D.; Schlesinger, L.S.; et al. Ar-13 reduces antibiotic-resistant bacterial burden in cystic fibrosis phagocytes and improves cystic fibrosis transmembrane conductance regulator function. J. Cyst. Fibros 2019, 18, 622–629. [Google Scholar] [CrossRef]
- Krause, K.; Kopp, B.T.; Tazi, M.F.; Caution, K.; Hamilton, K.; Badr, A.; Shrestha, C.; Tumin, D.; Hayes, D., Jr.; Robledo-Avila, F.; et al. The expression of mirc1/mir17-92 cluster in sputum samples correlates with pulmonary exacerbations in cystic fibrosis patients. J. Cyst. Fibros 2018, 17, 454–461. [Google Scholar] [CrossRef]
- Shrestha, C.L.; Assani, K.D.; Rinehardt, H.; Albastroiu, F.; Zhang, S.; Shell, R.; Amer, A.O.; Schlesinger, L.S.; Kopp, B.T. Cysteamine-mediated clearance of antibiotic-resistant pathogens in human cystic fibrosis macrophages. PLoS ONE 2017, 12, e0186169. [Google Scholar] [CrossRef] [PubMed]
- Abdulrahman, B.A.; Khweek, A.A.; Akhter, A.; Caution, K.; Tazi, M.; Hassan, H.; Zhang, Y.; Rowland, P.D.; Malhotra, S.; Aeffner, F.; et al. Depletion of the ubiquitin-binding adaptor molecule sqstm1/p62 from macrophages harboring cftr deltaf508 mutation improves the delivery of burkholderia cenocepacia to the autophagic machinery. J. Biol. Chem. 2013, 288, 2049–2058. [Google Scholar] [CrossRef] [PubMed]
- Arora, K.; Liyanage, P.; Zhong, Q.; Naren, A.P. A snare protein syntaxin 17 captures cftr to potentiate autophagosomal clearance under stress. FASEB J. 2021, 35, e21185. [Google Scholar] [CrossRef]
- Badr, A.; Eltobgy, M.; Krause, K.; Hamilton, K.; Estfanous, S.; Daily, K.P.; Abu Khweek, A.; Hegazi, A.; Anne, M.N.K.; Carafice, C.; et al. Cftr modulators restore acidification of autophago-lysosomes and bacterial clearance in cystic fibrosis macrophages. Front Cell Infect. Microbiol. 2022, 12, 819554. [Google Scholar] [CrossRef]
- Bodas, M.; Vij, N. Adapting proteostasis and autophagy for controlling the pathogenesis of cystic fibrosis lung disease. Front Pharmacol. 2019, 10, 20. [Google Scholar] [CrossRef]
- Chen, H.; Chen, W.; Yao, Y.; Ye, N.; Hou, N.; Luo, J. Upregulation of cftr protects against palmitate-induced endothelial dysfunction by enhancing autophagic flux. Oxid. Med. Cell Longev. 2020, 2020, 8345246. [Google Scholar] [CrossRef]
- Ferrari, E.; Monzani, R.; Villella, V.R.; Esposito, S.; Saluzzo, F.; Rossin, F.; D’Eletto, M.; Tosco, A.; De Gregorio, F.; Izzo, V.; et al. Cysteamine re-establishes the clearance of pseudomonas aeruginosa by macrophages bearing the cystic fibrosis-relevant f508del-cftr mutation. Cell Death Dis. 2017, 8, e2544. [Google Scholar] [CrossRef]
- Iannitti, R.G.; Napolioni, V.; Oikonomou, V.; De Luca, A.; Galosi, C.; Pariano, M.; Massi-Benedetti, C.; Borghi, M.; Puccetti, M.; Lucidi, V.; et al. Il-1 receptor antagonist ameliorates inflammasome-dependent inflammation in murine and human cystic fibrosis. Nat. Commun. 2016, 7, 10791. [Google Scholar] [CrossRef]
- Junkins, R.D.; Shen, A.; Rosen, K.; McCormick, C.; Lin, T.J. Autophagy enhances bacterial clearance during p. Aeruginosa lung infection. PLoS ONE 2013, 8, e72263. [Google Scholar] [CrossRef]
- Luciani, A.; Villella, V.R.; Esposito, S.; Brunetti-Pierri, N.; Medina, D.; Settembre, C.; Gavina, M.; Pulze, L.; Giardino, I.; Pettoello-Mantovani, M.; et al. Defective cftr induces aggresome formation and lung inflammation in cystic fibrosis through ros-mediated autophagy inhibition. Nat. Cell Biol. 2010, 12, 863–875. [Google Scholar] [CrossRef]
- Mayer, M.L.; Blohmke, C.J.; Falsafi, R.; Fjell, C.D.; Madera, L.; Turvey, S.E.; Hancock, R.E. Rescue of dysfunctional autophagy attenuates hyperinflammatory responses from cystic fibrosis cells. J. Immunol. 2013, 190, 1227–1238. [Google Scholar] [CrossRef]
- Noh, S.H.; Gee, H.Y.; Kim, Y.; Piao, H.; Kim, J.; Kang, C.M.; Lee, G.; Mook-Jung, I.; Lee, Y.; Cho, J.W.; et al. Specific autophagy and escrt components participate in the unconventional secretion of cftr. Autophagy 2018, 14, 1761–1778. [Google Scholar] [CrossRef]
- Rimessi, A.; Pozzato, C.; Carparelli, L.; Rossi, A.; Ranucci, S.; De Fino, I.; Cigana, C.; Talarico, A.; Wieckowski, M.R.; Ribeiro, C.M.P.; et al. Pharmacological modulation of mitochondrial calcium uniporter controls lung inflammation in cystic fibrosis. Sci. Adv. 2020, 6, eaax9093. [Google Scholar] [CrossRef]
- Martinez, J.; Malireddi, R.K.; Lu, Q.; Cunha, L.D.; Pelletier, S.; Gingras, S.; Orchard, R.; Guan, J.L.; Tan, H.; Peng, J.; et al. Molecular characterization of lc3-associated phagocytosis reveals distinct roles for rubicon, nox2 and autophagy proteins. Nat. Cell Biol. 2015, 17, 893–906. [Google Scholar] [CrossRef]
- Lamothe, J.; Huynh, K.K.; Grinstein, S.; Valvano, M.A. Intracellular survival of burkholderia cenocepacia in macrophages is associated with a delay in the maturation of bacteria-containing vacuoles. Cell Microbiol. 2007, 9, 40–53. [Google Scholar] [CrossRef]
- Huynh, K.K.; Plumb, J.D.; Downey, G.P.; Valvano, M.A.; Grinstein, S. Inactivation of macrophage rab7 by burkholderia cenocepacia. J. Innate Immun. 2010, 2, 522–533. [Google Scholar] [CrossRef]
- Al-Khodor, S.; Marshall-Batty, K.; Nair, V.; Ding, L.; Greenberg, D.E.; Fraser, I.D. Burkholderia cenocepacia j2315 escapes to the cytosol and actively subverts autophagy in human macrophages. Cell Microbiol. 2014, 16, 378–395. [Google Scholar] [CrossRef]
- Di, A.; Brown, M.E.; Deriy, L.V.; Li, C.; Szeto, F.L.; Chen, Y.; Huang, P.; Tong, J.; Naren, A.P.; Bindokas, V.; et al. Cftr regulates phagosome acidification in macrophages and alters bactericidal activity. Nat. Cell Biol. 2006, 8, 933–944. [Google Scholar] [CrossRef]
- Haggie, P.M.; Verkman, A.S. Cystic fibrosis transmembrane conductance regulator-independent phagosomal acidification in macrophages. J. Biol. Chem. 2007, 282, 31422–31428. [Google Scholar] [CrossRef]
- Deriy, L.V.; Gomez, E.A.; Zhang, G.; Beacham, D.W.; Hopson, J.A.; Gallan, A.J.; Shevchenko, P.D.; Bindokas, V.P.; Nelson, D.J. Disease-causing mutations in the cystic fibrosis transmembrane conductance regulator determine the functional responses of alveolar macrophages. J. Biol. Chem. 2009, 284, 35926–35938. [Google Scholar] [CrossRef]
- Barriere, H.; Bagdany, M.; Bossard, F.; Okiyoneda, T.; Wojewodka, G.; Gruenert, D.; Radzioch, D.; Lukacs, G.L. Revisiting the role of cystic fibrosis transmembrane conductance regulator and counterion permeability in the ph regulation of endocytic organelles. Mol. Biol. Cell 2009, 20, 3125–3141. [Google Scholar] [CrossRef]
- Assani, K.; Shrestha, C.L.; Robledo-Avila, F.; Rajaram, M.V.; Partida-Sanchez, S.; Schlesinger, L.S.; Kopp, B.T. Human cystic fibrosis macrophages have defective calcium-dependent protein kinase c activation of the nadph oxidase, an effect augmented by burkholderia cenocepacia. J. Immunol. 2017, 198, 1985–1994. [Google Scholar] [CrossRef]
- Robledo-Avila, F.H.; Ruiz-Rosado, J.D.; Brockman, K.L.; Kopp, B.T.; Amer, A.O.; McCoy, K.; Bakaletz, L.O.; Partida-Sanchez, S. Dysregulated calcium homeostasis in cystic fibrosis neutrophils leads to deficient antimicrobial responses. J. Immunol. 2018, 201, 2016–2027. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, X.; Grassme, H.; Doring, G.; Gulbins, E. Alterations in ceramide concentration and ph determine the release of reactive oxygen species by cftr-deficient macrophages on infection. J. Immunol. 2010, 184, 5104–5111. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, X.; Carpinteiro, A.; Gulbins, E. Acid sphingomyelinase amplifies redox signaling in pseudomonas aeruginosa-induced macrophage apoptosis. J. Immunol. 2008, 181, 4247–4254. [Google Scholar] [CrossRef]
- Degiacomi, G.; Sammartino, J.C.; Chiarelli, L.R.; Riabova, O.; Makarov, V.; Pasca, M.R. Mycobacterium abscessus, an emerging and worrisome pathogen among cystic fibrosis patients. Int. J. Mol. Sci. 2019, 20, 5868. [Google Scholar] [CrossRef]
- Bernut, A.; Dupont, C.; Ogryzko, N.V.; Neyret, A.; Herrmann, J.L.; Floto, R.A.; Renshaw, S.A.; Kremer, L. Cftr protects against mycobacterium abscessus infection by fine-tuning host oxidative defenses. Cell Rep. 2019, 26, 1828–1840.e4. [Google Scholar] [CrossRef]
- Kim, B.R.; Kim, B.J.; Kook, Y.H.; Kim, B.J. Mycobacterium abscessus infection leads to enhanced production of type 1 interferon and nlrp3 inflammasome activation in murine macrophages via mitochondrial oxidative stress. PLoS Pathog. 2020, 16, e1008294. [Google Scholar] [CrossRef]
- Kim, B.R.; Kim, B.J.; Kook, Y.H.; Kim, B.J. Phagosome escape of rough mycobacterium abscessus strains in murine macrophage via phagosomal rupture can lead to type i interferon production and their cell-to-cell spread. Front Immunol. 2019, 10, 125. [Google Scholar] [CrossRef]
- Laencina, L.; Dubois, V.; Le Moigne, V.; Viljoen, A.; Majlessi, L.; Pritchard, J.; Bernut, A.; Piel, L.; Roux, A.L.; Gaillard, J.L.; et al. Identification of genes required for mycobacterium abscessus growth in vivo with a prominent role of the esx-4 locus. Proc. Natl. Acad. Sci. USA 2018, 115, E1002–E1011. [Google Scholar] [CrossRef]
- Hall-Stoodley, L. Macrophages from cf Patients Are Susceptible to Rough Mycobacterium Abscessus; Pediatric pulmonology; Wiley: Hoboken, NJ, USA, 2019; p. S268. [Google Scholar]
- Lara-Reyna, S.; Holbrook, J.; Jarosz-Griffiths, H.H.; Peckham, D.; McDermott, M.F. Dysregulated signalling pathways in innate immune cells with cystic fibrosis mutations. Cell Mol. Life Sci. 2020, 77, 4485–4503. [Google Scholar] [CrossRef]
- Bucci, C.; Thomsen, P.; Nicoziani, P.; McCarthy, J.; van Deurs, B. Rab7: A key to lysosome biogenesis. Mol. Biol. Cell 2000, 11, 467–480. [Google Scholar] [CrossRef]
- Riquelme, S.A.; Hopkins, B.D.; Wolfe, A.L.; DiMango, E.; Kitur, K.; Parsons, R.; Prince, A. Cystic fibrosis transmembrane conductance regulator attaches tumor suppressor pten to the membrane and promotes anti pseudomonas aeruginosa immunity. Immunity 2017, 47, 1169–1181.e7. [Google Scholar] [CrossRef]
- Shinde, S.R.; Maddika, S. Pten modulates egfr late endocytic trafficking and degradation by dephosphorylating rab7. Nat. Commun. 2016, 7, 10689. [Google Scholar] [CrossRef]
- Itakura, E.; Kishi-Itakura, C.; Mizushima, N. The hairpin-type tail-anchored snare syntaxin 17 targets to autophagosomes for fusion with endosomes/lysosomes. Cell 2012, 151, 1256–1269. [Google Scholar] [CrossRef]
- Pohl, K.; Hayes, E.; Keenan, J.; Henry, M.; Meleady, P.; Molloy, K.; Jundi, B.; Bergin, D.A.; McCarthy, C.; McElvaney, O.J.; et al. A neutrophil intrinsic impairment affecting rab27a and degranulation in cystic fibrosis is corrected by cftr potentiator therapy. Blood 2014, 124, 999–1009. [Google Scholar] [CrossRef]
- Villella, V.R.; Esposito, S.; Bruscia, E.M.; Vicinanza, M.; Cenci, S.; Guido, S.; Pettoello-Mantovani, M.; Carnuccio, R.; De Matteis, M.A.; Luini, A.; et al. Disease-relevant proteostasis regulation of cystic fibrosis transmembrane conductance regulator. Cell Death Differ. 2013, 20, 1101–1115. [Google Scholar] [CrossRef]
- Edmondson, C.; Davies, J.C. Current and future treatment options for cystic fibrosis lung disease: Latest evidence and clinical implications. Ther. Adv. Chronic. Dis. 2016, 7, 170–183. [Google Scholar] [CrossRef]
- Henke, M.O.; Ratjen, F. Mucolytics in cystic fibrosis. Paediatr. Respir. Rev. 2007, 8, 24–29. [Google Scholar] [CrossRef]
- Tyrrell, J.; Callaghan, M. Iron acquisition in the cystic fibrosis lung and potential for novel therapeutic strategies. Microbiology 2016, 162, 191–205. [Google Scholar] [CrossRef]
- Hazlett, H.F.; Hampton, T.H.; Aridgides, D.S.; Armstrong, D.A.; Dessaint, J.A.; Mellinger, D.L.; Nymon, A.B.; Ashare, A. Altered iron metabolism in cystic fibrosis macrophages: The impact of cftr modulators and implications for pseudomonas aeruginosa survival. Sci. Rep. 2020, 10, 10935. [Google Scholar] [CrossRef]
- Barnaby, R.; Koeppen, K.; Nymon, A.; Hampton, T.H.; Berwin, B.; Ashare, A.; Stanton, B.A. Lumacaftor (vx-809) restores the ability of cf macrophages to phagocytose and kill pseudomonas aeruginosa. Am. J. Physiol. Lung Cell Mol. Physiol. 2018, 314, L432–L438. [Google Scholar] [CrossRef]
- Zhang, S.; Shrestha, C.L.; Kopp, B.T. Cystic fibrosis transmembrane conductance regulator (cftr) modulators have differential effects on cystic fibrosis macrophage function. Sci. Rep. 2018, 8, 17066. [Google Scholar] [CrossRef]
- Bratcher, P.E.; Rowe, S.M.; Reeves, G.; Roberts, T.; Szul, T.; Harris, W.T.; Tirouvanziam, R.; Gaggar, A. Alterations in blood leukocytes of g551d-bearing cystic fibrosis patients undergoing treatment with ivacaftor. J. Cyst. Fibros 2016, 15, 67–73. [Google Scholar] [CrossRef]
- Hisert, K.B.; Schoenfelt, K.Q.; Cooke, G.; Grogan, B.; Launspach, J.L.; Gallagher, C.G.; Donnelly, S.C.; Welsh, M.J.; Singh, P.K.; McKone, E.F.; et al. Ivacaftor-induced proteomic changes suggest monocyte defects may contribute to the pathogenesis of cystic fibrosis. Am. J. Respir. Cell Mol. Biol. 2016, 54, 594–597. [Google Scholar] [CrossRef]
- Pedrazzi, M.; Vercellone, S.; Barberis, E.; Capraro, M.; De Tullio, R.; Cresta, F.; Casciaro, R.; Castellani, C.; Patrone, M.; Marengo, E.; et al. Identification of potential leukocyte biomarkers related to drug recovery of cftr: Clinical applications in cystic fibrosis. Int. J. Mol. Sci. 2021, 22, 3928. [Google Scholar] [CrossRef]
- Pohl, K.; Nichols, D.P.; Taylor-Cousar, J.L.; Saavedra, M.T.; Strand, M.J.; Nick, J.A.; Bratcher, P.E. Corticosteroid use and increased cxcr2 levels on leukocytes are associated with lumacaftor/ivacaftor discontinuation in cystic fibrosis patients homozygous for the f508del cftr mutation. PLoS ONE 2018, 13, e0209026. [Google Scholar] [CrossRef]
- Hisert, K.B.; Birkland, T.P.; Schoenfelt, K.Q.; Long, M.E.; Grogan, B.; Carter, S.; Liles, W.C.; McKone, E.F.; Becker, L.; Manicone, A.M.; et al. Cftr modulator therapy enhances peripheral blood monocyte contributions to immune responses in people with cystic fibrosis. Front Pharmacol. 2020, 11, 1219. [Google Scholar] [CrossRef]
- Kopp, B.T.; Fitch, J.; Jaramillo, L.; Shrestha, C.L.; Robledo-Avila, F.; Zhang, S.; Palacios, S.; Woodley, F.; Hayes, D., Jr.; Partida-Sanchez, S.; et al. Whole-blood transcriptomic responses to lumacaftor/ivacaftor therapy in cystic fibrosis. J. Cyst. Fibros 2020, 19, 245–254. [Google Scholar] [CrossRef]
- Harwood, K.H.; McQuade, R.M.; Jarnicki, A.; Schneider-Futschik, E.K. Anti-inflammatory influences of cystic fibrosis transmembrane conductance regulator drugs on lung inflammation in cystic fibrosis. Int. J. Mol. Sci. 2021, 22, 7606. [Google Scholar] [CrossRef]
- Gillan, J.L.; Davidson, D.J.; Gray, R.D. Targeting cystic fibrosis inflammation in the age of cftr modulators: Focus on macrophages. Eur. Respir. J. 2021, 57, 2003502. [Google Scholar] [CrossRef]
- Caution, K.; Pan, A.; Krause, K.; Badr, A.; Hamilton, K.; Vaidya, A.; Gosu, H.; Daily, K.; Estfanous, S.; Gavrilin, M.A.; et al. Methylomic correlates of autophagy activity in cystic fibrosis. J. Cyst. Fibros 2019, 18, 491–500. [Google Scholar] [CrossRef]
- Vij, N.; Chandramani-Shivalingappa, P.; Van Westphal, C.; Hole, R.; Bodas, M. Cigarette smoke-induced autophagy impairment accelerates lung aging, copd-emphysema exacerbations and pathogenesis. Am. J. Physiol. Cell Physiol. 2018, 314, C73–C87. [Google Scholar] [CrossRef]
- Esposito, S.; Tosco, A.; Villella, V.R.; Raia, V.; Kroemer, G.; Maiuri, L. Manipulating proteostasis to repair the f508del-cftr defect in cystic fibrosis. Mol. Cell Pediatr. 2016, 3, 13. [Google Scholar] [CrossRef]
- Tosco, A.; De Gregorio, F.; Esposito, S.; De Stefano, D.; Sana, I.; Ferrari, E.; Sepe, A.; Salvadori, L.; Buonpensiero, P.; Di Pasqua, A.; et al. A novel treatment of cystic fibrosis acting on-target: Cysteamine plus epigallocatechin gallate for the autophagy-dependent rescue of class ii-mutated cftr. Cell Death Differ. 2016, 23, 1380–1393. [Google Scholar] [CrossRef]
- Brockman, S.M.; Bodas, M.; Silverberg, D.; Sharma, A.; Vij, N. Dendrimer-based selective autophagy-induction rescues deltaf508-cftr and inhibits pseudomonas aeruginosa infection in cystic fibrosis. PLoS ONE 2017, 12, e0184793. [Google Scholar]
- Charrier, C.; Rodger, C.; Robertson, J.; Kowalczuk, A.; Shand, N.; Fraser-Pitt, D.; Mercer, D.; O’Neil, D. Cysteamine (lynovex(r)), a novel mucoactive antimicrobial & antibiofilm agent for the treatment of cystic fibrosis. Orphanet. J. Rare Dis. 2014, 9, 189. [Google Scholar]
- Shrestha, C.L.; Zhang, S.; Wisniewski, B.; Hafner, S.; Elie, J.; Meijer, L.; Kopp, B.T. (r)-roscovitine and cftr modulators enhance killing of multi-drug resistant burkholderia cenocepacia by cystic fibrosis macrophages. Sci. Rep. 2020, 10, 21700. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaganathan, D.; Bruscia, E.M.; Kopp, B.T. Emerging Concepts in Defective Macrophage Phagocytosis in Cystic Fibrosis. Int. J. Mol. Sci. 2022, 23, 7750. https://doi.org/10.3390/ijms23147750
Jaganathan D, Bruscia EM, Kopp BT. Emerging Concepts in Defective Macrophage Phagocytosis in Cystic Fibrosis. International Journal of Molecular Sciences. 2022; 23(14):7750. https://doi.org/10.3390/ijms23147750
Chicago/Turabian StyleJaganathan, Devi, Emanuela M. Bruscia, and Benjamin T. Kopp. 2022. "Emerging Concepts in Defective Macrophage Phagocytosis in Cystic Fibrosis" International Journal of Molecular Sciences 23, no. 14: 7750. https://doi.org/10.3390/ijms23147750
APA StyleJaganathan, D., Bruscia, E. M., & Kopp, B. T. (2022). Emerging Concepts in Defective Macrophage Phagocytosis in Cystic Fibrosis. International Journal of Molecular Sciences, 23(14), 7750. https://doi.org/10.3390/ijms23147750





