Insights into the Mechanisms of Action of Proanthocyanidins and Anthocyanins in the Treatment of Nicotine-Induced Non-Small Cell Lung Cancer
Abstract
:1. Introduction
2. Methods
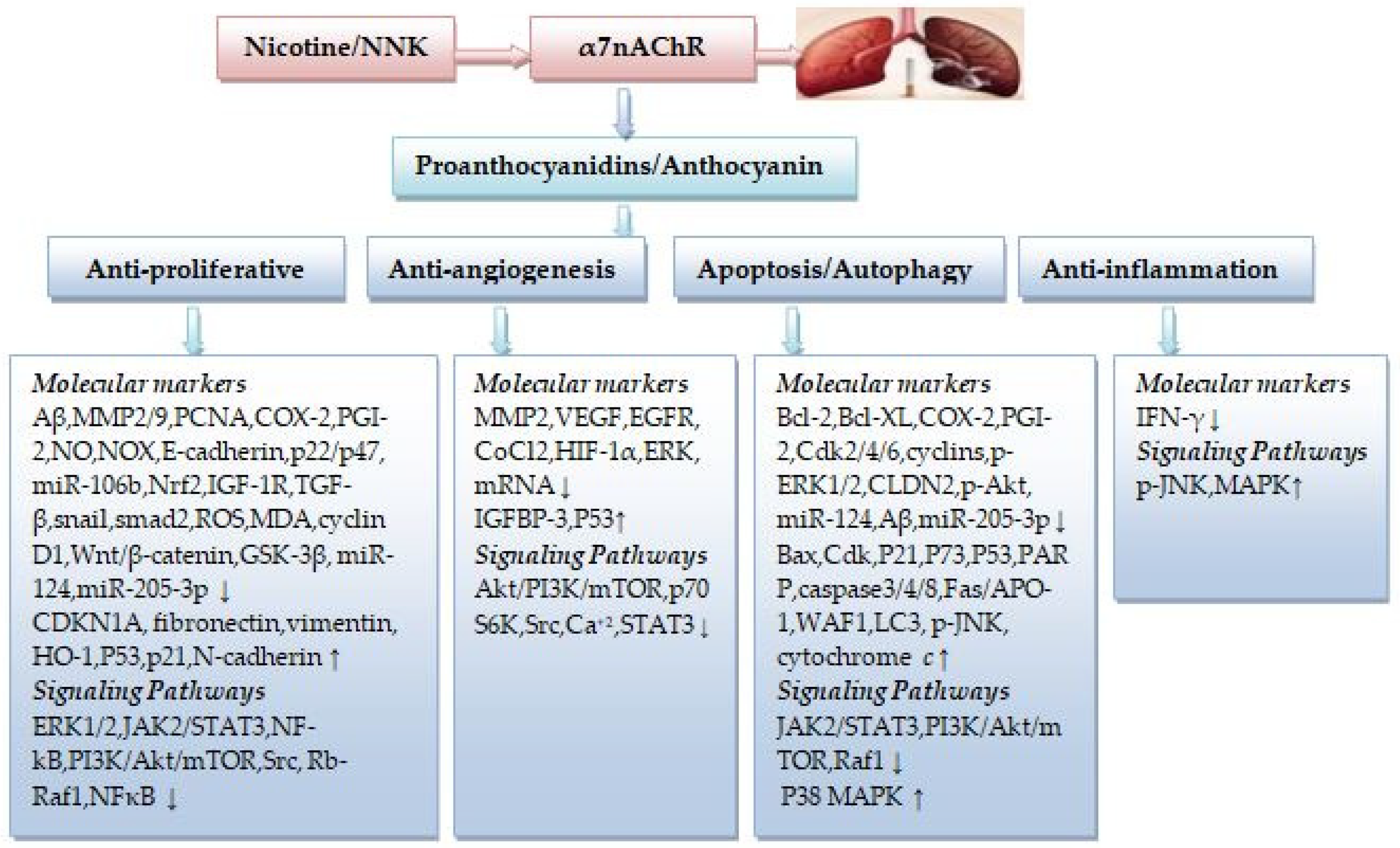
3. Proanthocyanidins in Nicotine-Induced NSCLC Treatment
4. Anthocyanins in Nicotine-Induced NSCLC Treatment
5. Combination of Proanthocyanidins and Anthocyanins with Chemotherapeutics/Radiotherapy in Nicotine-Induced NSCLC Treatment
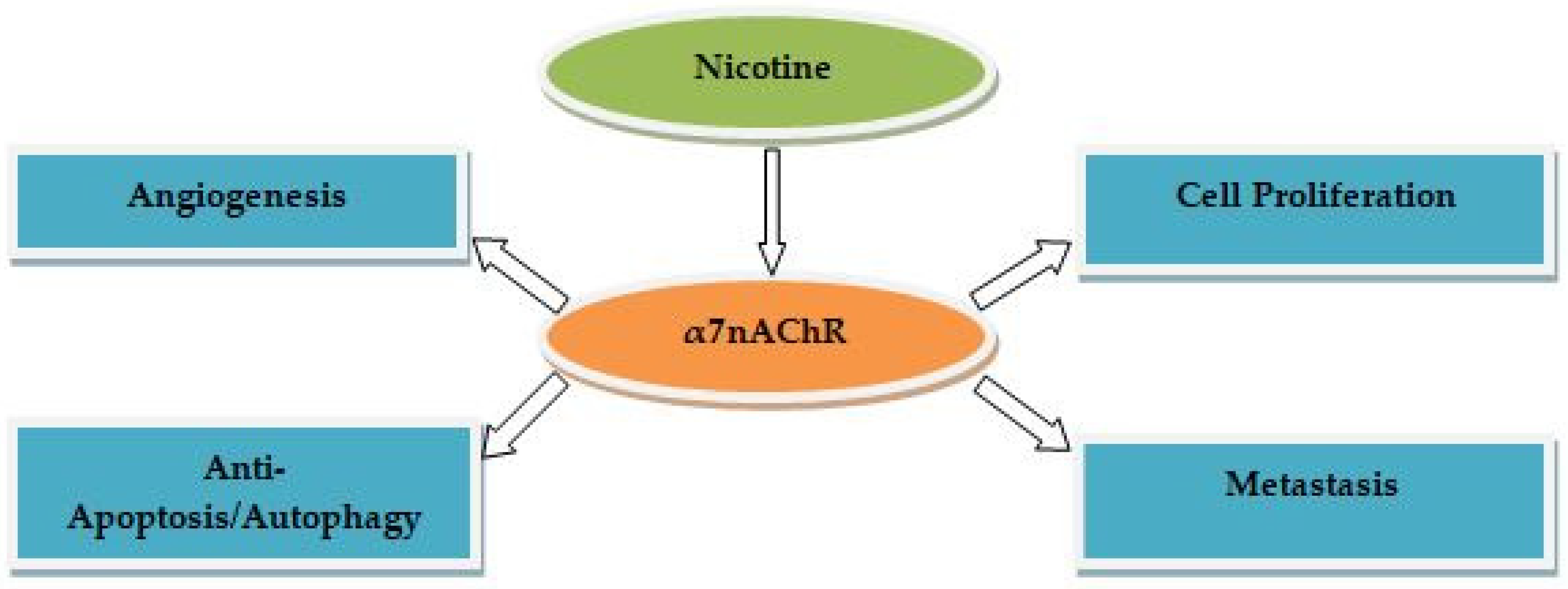
6. PCs and ACNs as Positive Modulators of Human α7nAChR
7. Limitations
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bray, F.; Jacques, F.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molina, J.R.; Yang, P.; Cassivi, S.D.; Schild, S.E.; Adjei, A.A. Non-small cell lung cancer: Epidemiology, risk factors, treatment, and survivorship. Mayo Clin. Proc. 2008, 83, 584–594. [Google Scholar] [CrossRef]
- Alsharairi, N.A. The effects of dietary supplements on asthma and lung cancer risk in smokers and non-smokers: A review of the literature. Nutrients 2019, 11, 725. [Google Scholar] [CrossRef] [Green Version]
- Xue, J.; Yang, S.; Seng, S. Mechanisms of cancer induction by tobacco-specific NNK and NNN. Cancers 2014, 6, 1138–1156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hecht, S.S. Lung Carcinogenesis by tobacco smoke. Int. J. Cancer 2012, 131, 2724–2732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hecht, S.S.; Stepanov, I.; Carmella, S.G. Exposure and metabolic activation biomarkers of carcinogenic tobacco-spesficnitrosommines. ACS Chem. Res. 2016, 49, 106–114. [Google Scholar] [CrossRef] [Green Version]
- Tournier, J.-M.; Birembaut, P. Nicotinic acetylcholine receptors and predisposition to lung cancer. Curr. Opin. Oncol. 2011, 23, 83–87. [Google Scholar] [CrossRef]
- Warren, G.W.; Singh, A.K. Nicotine and lung cancer. J. Carcinog. 2013, 12, 1. [Google Scholar] [CrossRef]
- Schaal, S.; Chellappan, S.P. Nicotine-mediated cell proliferation and tumor progression in smoking-related cancers. Mol. Cancer Res. 2014, 12, 14–23. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Hu, Y. α7 nicotinic acetylcholine receptors in lung cancer (Review). Oncol. Lett. 2018, 16, 1375–1382. [Google Scholar] [CrossRef] [Green Version]
- Zhao, H.; Wang, Y.; Ren, X. Nicotine promotes the development of non-small cell lung cancer through activating LINC00460 and PI3K/Akt signaling. Biosci. Rep. 2019, 39, BSR20182443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hajiasgharzadeh, K.; Sadigh-Eteghad, S.; Mansoori, B.; Mokhtarzadeh, A.; Shanehbandi, D.; Doustvandi, M.A.; Asadzadeh, Z.; Baradaran, B. Alpha7 nicotinic acetylcholine receptors in lung inflammation and carcinogenesis: Friends or foes? J. Cell Physiol. 2019, 234, 14666–14679. [Google Scholar] [CrossRef]
- Alsharairi, N.A. Scutellaria baicalensis and their natural flavone compounds as potential medicinal drugs for the treatment of nicotine-induced non-small-cell lung cancer and asthma. Int. J. Environ. Res. Public Health 2021, 18, 5243. [Google Scholar] [CrossRef] [PubMed]
- Alsharairi, N.A. Supplements for smoking-related lung diseases. Encyclopedia 2021, 1, 76–86. [Google Scholar] [CrossRef]
- Dafni, U.; Tsourti, Z.; Vervita, K.; Peters, S. Immune checkpoint inhibitors, alone or in combination with chemotherapy, as first-line treatment for advanced non-small cell lung cancer. A systematic review and network meta-analysis. Lung Cancer 2019, 134, 127–140. [Google Scholar] [CrossRef] [PubMed]
- Zanoaga, O.; Braicu, C.; Jurj, A.; Rusu, A.; Buiga, R.; Berindan-Neagoe, I. Progress in research on the role of flavonoids in lung cancer. Int. J. Mol. Sci. 2019, 20, 4291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skrovankova, S.; Sumczynski, D.; Mlcek, J.; Jurikova, T.; Sochor, J. Bioactive compounds and antioxidant activity in different types of berries. Int. J. Mol. Sci. 2015, 16, 24673–24706. [Google Scholar] [CrossRef] [Green Version]
- Sayago-Ayerdi, S.; García-Martínez, D.L.; Ramírez-Castillo, A.C.; Ramírez-Concepción, H.R.; Viuda-Martos, M. Tropical fruits and their co-products as bioactive compounds and their health effects: A review. Foods 2021, 10, 1952. [Google Scholar] [CrossRef]
- Samtiya, M.; Aluko, R.E.; Dhewa, T.; Moreno-Rojas, J.M. Potential health benefits of plant food-derived bioactive components: An overview. Foods 2021, 10, 839. [Google Scholar] [CrossRef]
- Smeriglio, A.; Barreca, A.; Bellocco, E.; Trombetta, D. Proanthocyanidins and hydrolysable tannins: Occurrence, dietary intake and pharmacological effects. Br. J. Pharmacol. 2017, 174, 1244–1262. [Google Scholar] [CrossRef] [Green Version]
- Rue, E.A.; Rush, M.D.; van Breemen, R.B. Procyanidins: A comprehensive review encompassing structure elucidation via mass spectrometry. Phytochem. Rev. 2017, 17, 1–16. [Google Scholar] [CrossRef]
- Mannino, G.; Chinigò, G.; Serio, G.; Genova, T.; Gentile, C.; Munaron, L.; Bertea, C.M. Proanthocyanidins and where to find them: A meta-analytic approach to investigate their chemistry, biosynthesis, distribution, and effect on human health. Antioxidants 2021, 10, 1229. [Google Scholar] [CrossRef] [PubMed]
- Khoo, H.E.; Azlan, A.; Tang, S.T.; Lim, S.M. Anthocyanidins and anthocyanins: Colored pigments as food, pharmaceutical ingredients, and the potential health benefits. Food Nutr. Res. 2017, 61, 1361779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, B.-W.; Gong, C.-C.; Song, H.-F.; Cui, Y.-Y. Effects of anthocyanins on the prevention and treatment of cancer. Br. J. Pharmacol. 2017, 174, 1226–1243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattioli, R.; Francioso, A.; Mosca, L.; Silva, P. Anthocyanins: A comprehensive review of their chemical properties and health effects on cardiovascular and neurodegenerative diseases. Molecules 2020, 25, 3809. [Google Scholar] [CrossRef]
- Winkel-Shirley, B. Flavonoid biosynthesis. A colorful model for genetics, biochemistry, cell biology, and biotechnology. Plant Physiol. 2001, 126, 485–493. [Google Scholar] [CrossRef] [Green Version]
- Marles, M.A.S.; Ray, H.; Gruber, M.Y. New perspectives on proanthocyanidin biochemistry and molecular regulation. Phytochemistry 2003, 64, 367–383. [Google Scholar] [CrossRef]
- Limtrakul, P.; Semmarath, W.; Mapoung, S. Anthocyanins and proanthocyanidins in natural pigmented rice and their bioactivities. In Phytochemicals in Human Health; Intechopen: London, UK, 2019. [Google Scholar] [CrossRef] [Green Version]
- Wu, X.; Gu, L.; Prior, R.L.; McKay, S. Characterization of anthocyanins and proanthocyanidins in some cultivars of Ribes, Aronia, and Sambucus and their antioxidant capacity. J. Agric. Food Chem. 2004, 52, 7846–7856. [Google Scholar] [CrossRef]
- Karppinen, K.; Zoratti, L.; Nguyenquynh, N.; Häggman, H.; Jaakola, L. On the developmental and environmental regulation of secondary metabolism in Vaccinium spp. berries. Front Plant Sci. 2016, 7, 655. [Google Scholar] [CrossRef] [Green Version]
- Kumar, R.; Khurana, A.; Sharma, A.K. Role of plant hormones and their interplay in development and ripening of fleshy fruits. J. Exp. Bot. 2014, 65, 4561–4575. [Google Scholar] [CrossRef] [Green Version]
- Osorio, S.; Scossa, F.; Fernie, A.R. Molecular regulation of fruit ripening. Front. Plant Sci. 2013, 4, 198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bapat, V.A.; Trivedi, P.K.; Ghosh, A.; Sane, V.A.; Ganapathi, T.R.; Nath, P. Ripening of fleshy fruit: Molecular insight and the role of ethylene. Biotechnol. Adv. 2010, 28, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Pan, H.; Li, J. Molecular insights into potential contributions of natural polyphenols to lung cancer treatment. Cancers 2019, 11, 1565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGhie, T.K.; Walton, M.C. The bioavailability and absorption of anthocyanins: Towards a better understanding. Mol. Nutr. Food Res. 2007, 51, 702–713. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, S.; Rudloff, S.; Asseburg, H.; Borsch, C.; Fröhling, B.; Unger, F.; Dold, S.; Spengler, B.; Römpp, A.; Kunz, C. Uptake and bioavailability of anthocyanins and phenolic acids from grape/blueberry juice and smoothie in vitro and in vivo. Br. J. Nutr. 2015, 113, 1044–1055. [Google Scholar] [CrossRef] [Green Version]
- Tena, N.; Martín, J.; Asuero, A.G. State of the art of anthocyanins: Antioxidant activity, sources, bioavailability, and therapeutic effect in human health. Antioxidants 2020, 9, 451. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, D.; Wu, Y.; Wang, D.; Wei, Y.; Wu, J.; Ji, B. Stability and absorption of anthocyanins from blueberries subjected to a simulated digestion process. Int. J. Food Sci. Nutr. 2014, 65, 440–448. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, Y.; Li, D.; Ho, C.-T.; Li, J.; Wan, X. The absorption, distribution, metabolism and excretion of procyanidins. Food Funct. 2016, 7, 1273–1281. [Google Scholar] [CrossRef]
- Ferguson, P.J.; Kurowska, E.; Freeman, D.J.; Chambers, A.F.; Koropatnick, D.J. A flavonoid fraction from cranberry extract inhibits proliferation of human tumor cell lines. J. Nutr. 2004, 134, 1529–1535. [Google Scholar] [CrossRef] [Green Version]
- Neto, C.C.; Krueger, C.G.; Lamoureaux, T.L.; Kondo, M.; Vaisberg, A.J.; Hurta, R.A.R.; Curtis, S.; Matchett, M.D.; Yeung, H.; Sweeney, M.I.; et al. Maldi-TOF MS characterization of proanthocyanidins from cranberry fruit (Vaccinium macrocarpon) that inhibit tumor cell growth and matrix metalloproteinase expression in vitro. J. Sci. Food. Agric. 2006, 86, 18–25. [Google Scholar] [CrossRef]
- Kresty, L.A.; Howell, A.B.; Baird, M. Cranberry proanthocyanidins mediate growth arrest of lung cancer cells through modulation of gene expression and rapid induction of apoptosis. Molecules 2011, 16, 2375–2390. [Google Scholar] [CrossRef]
- Zhai, W.-Y.; Jia, C.-P.; Zhao, H.; Xu, Y.-S. Procyanidins inhibit tumor angiogenesis by crosslinking extracellular matrix. Chin. J Cancer Res. 2011, 23, 99–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akhtar, S.; Meeran, S.M.; Katiyar, N.; Katiyar, S.K. Grape seed proanthocyanidins inhibit the growth of human non-small cell lung cancer xenografts by targeting insulin-like growth factor binding protein-3, tumor cell proliferation, and angiogenic factors. Clin. Cancer Res. 2009, 15, 821–831. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, S.D.; Meeran, S.M.; Katiyar, S.K. Proanthocyanidins inhibit in vitro and in vivo growth of human non-small cell lung cancer cells by inhibiting the prostaglandin E(2) and prostaglandin E(2) receptors. Mol. Cancer Ther. 2010, 9, 569–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Punathil, T.; Katiyar, S.K. Inhibition of non-small cell lung cancer cell migration by grape seed proanthocyanidins is mediated through the inhibition of nitric oxide, guanylate cyclase, and ERK1/2. Mol. Carcinog. 2009, 48, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.T.; Smoake, J.; Park, H.K.; Lu, Q.-Y.; Xue, B. Grape seed procyanidin extract mediates antineoplastic effects against lung cancer via modulations of prostacyclin and 15-HETE eicosanoid pathways. Cancer Prev. Res. 2016, 9, 925–932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaid, M.; Katiyar, S.K. Grape seed proanthocyanidins inhibit cigarette smoke condensate-induced lung cancer cell migration through inhibition of NADPH oxidase and reduction in the binding of p22(phox) and p47(phox) proteins. Mol. Carcinog. 2015, 54, E61–E71. [Google Scholar] [CrossRef] [PubMed]
- Singh, T.; Sharma, S.D.; Katiyar, S.K. Grape proanthocyanidins induce apoptosis by loss of mitochondrial membrane potential of human non-small cell lung cancer cells in vitro and in vivo. PLoS ONE 2011, 6, e27444. [Google Scholar] [CrossRef]
- Xue, B.; Lu, Q.-Y.; Massie, L.; Qualls, C.; Mao, J.T. Grape seed procyanidin extract against lung cancer: The role of microrna-106b, bioavailability, and bioactivity. Oncotarget 2018, 9, 15579–15590. [Google Scholar] [CrossRef] [Green Version]
- Ohnuma, T.; Anzai, E.; Suzuki, Y.; Shimoda, M.; Saito, S.; Nishiyama, T.; Ogura, K.; Hiratsuka, A. Selective antagonization of activated Nrf2 and inhibition of cancer cell proliferation by procyanidins from Cinnamomi Cortex extract. Arch. Biochem. Biophys. 2015, 585, 17–24. [Google Scholar] [CrossRef]
- Ohnuma, T.; Sakamoto, K.; Shinoda, A.; Takagi, C.; Ohno, S.; Nishiyama, T.; Ogura, K.; Hiratsuka, A. Procyanidins from Cinnamomi Cortex promote proteasome-independent degradation of nuclear Nrf2 through phosphorylation of insulin-like growth factor-1 receptor in A549 cells. Arch. Biochem. Biophys. 2017, 635, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Kin, R.; Kato, S.; Kaneto, N.; Sakurai, H.; Hayakawa, Y.; Li, F.; Tanaka, K.; Saiki, I.; Yokoyama, S. Procyanidin C1 from Cinnamomi Cortex inhibits TGF-β-induced epithelial-to-mesenchymal transition in the A549 lung cancer cell line. Int. J. Oncol. 2013, 43, 1901–1906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, C.; Jin, W.; Shi, H. Oligomeric proanthocyanidins protects A549 cells against H2O2-induced oxidative stress via the Nrf2-ARE pathway. Int. J. Mol. Med. 2017, 39, 1548–1554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, Y.; Liu, C.; Niu, Y.; Xia, J.; Fan, L.; Wu, Y.; Gao, W. Procyanidins mediates antineoplastic effects against non-small cell lung cancer via the JAK2/STAT3 pathway. Transl. Cancer Res. 2021, 10, 2023–2035. [Google Scholar] [CrossRef]
- Kuo, P.L.; Hsu, Y.L.; Lin, T.C.; Lin, C.C. The antiproliferative activity of prodelphinidin B-2 3’-O-gallate from green tea leaf is through cell cycle arrest and Fas-mediated apoptotic pathway in A549 cells. Food Chem. Toxicol. 2005, 43, 315–323. [Google Scholar] [CrossRef]
- Kuo, P.L.; Hsu, Y.L.; Lin, T.A.; Lin, C.C. Prodelphinidin B-2 3,3’-di-O-gallate from Myrica rubra inhibits proliferation of A549 carcinoma cells via blocking cell cycle progression and inducing apoptosis. Eur. J. Pharmacol. 2004, 501, 41–48. [Google Scholar] [CrossRef]
- Way, T.-D.; Tsai, S.-J.; Wang, C.-M.; Jhan, Y.-L.; Ho, C.-T.; Chou, C.-H. Cinnamtannin D1 from Rhododendron formosanum induces autophagy via the inhibition of Akt/mTOR and activation of ERK1/2 in non-small-cell lung carcinoma cells. J. Agric. Food Chem. 2015, 63, 10407–10417. [Google Scholar] [CrossRef]
- Oak, M.-H.; Bedoui, J.E.; Madeira, S.V.F.; Chalupsky, K.; Schini-Kerth, V.B. Delphinidin and cyanidin inhibit PDGF(AB)-induced VEGF release in vascular smooth muscle cells by preventing activation of p38 MAPK and JNK. Br. J. Pharmacol. 2006, 149, 283–290. [Google Scholar] [CrossRef] [Green Version]
- Lu, J.N.; Panchanathan, R.; Lee, W.S.; Kim, H.J.; Kim, D.H.; Choi, Y.H.; Kim, G.; Shin, S.C.; Hong, S.C. Anthocyanins from the fruit of Vitis coignetiae Pulliatinhibit TNF-augmented cancer proliferation, migration, and invasion in A549 cells. Asian Pac. J. Cancer Prev. 2017, 18, 2919–2923. [Google Scholar]
- Chen, P.-N.; Chu, S.-C.; Chiou, H.-L.; Kuo, W.-H.; Chiang, C.-L.; Hsieh, Y.-S. Mulberry anthocyanins, cyanidin 3-rutinoside and cyanidin 3-glucoside, exhibited an inhibitory effect on the migration and invasion of a human lung cancer cell line. Cancer Lett. 2006, 235, 248–259. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, W.; Xu, X. Cyanidin-3-glucoside suppresses the progression of lung adenocarcinoma by downregulating TP53I3 and inhibiting PI3K/AKT/mTOR pathway. World J. Surg. Oncol. 2021, 19, 232. [Google Scholar] [CrossRef]
- Pal, H.C.; Sharma, S.; Strickland, L.R.; Agarwal, J.; Athar, M.; Elmets, C.A.; Afaq, F. Delphinidin reduces cell proliferation and induces apoptosis of non-small-cell lung cancer cells by targeting EGFR/VEGFR2 signaling pathways. PLoS ONE. 2013, 8, e77270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.-H.; Jeong, Y.-J.; Cho, H.-J.; Hoe, H.-S.; Park, K.-K.; Park, Y.-Y.; Choi, Y.-H.; Kim, C.-H.; Chang, H.-W.; Park, Y.-J.; et al. Delphinidin inhibits angiogenesis through the suppression of HIF-1α and VEGF expression in A549 lung cancer cells. Oncol. Rep. 2017, 37, 777–784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kausar, H.; Jeyabalan, J.; Aqil, F.; Chabba, D.; Sidana, J.; Singh, I.P.; Gupta, R.C. Berry anthocyanidins synergistically suppress growth and invasive potential of human non-small-cell lung cancer cells. Cancer Lett. 2012, 325, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Aqil, F.; Gupta, A.; Munagala, R.; Jeyabalan, J.; Kausar, H.; Sharma, R.J.; Singh, I.P.; Gupta, R.C. Antioxidant and antiproliferative activities of anthocyanin/ellagitannin-enriched extracts from Syzygium cumini L. (Jamun, the Indian Blackberry). Nutr. Cancer 2012, 64, 428–438. [Google Scholar] [CrossRef] [Green Version]
- Ohnuma, T.; Matsumoto, T.; Itoi, A.; Kawana, A.; Nishiyama, T.; Ogura, K.; Hiratsuka, A. Enhanced sensitivity of A549 cells to the cytotoxic action of anticancer drugs via suppression of Nrf2 by procyanidins from Cinnamomi Cortex extract. Biochem. Biophys. Res. Commun. 2011, 413, 623–629. [Google Scholar] [CrossRef]
- Xu, Y.; Huang, Y.; Chen, Y.; Cao, K.; Liu, Z.; Wan, Z.; Liao, Z.; Li, B.; Cui, J.; Yang, Y.; et al. Grape seed proanthocyanidins play the roles of radioprotection on normal lung and radiosensitization on lung cancer via differential regulation of the MAPK signaling pathway. J. Cancer 2021, 12, 2844–2854. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Bak, D.-H.; Chung, B.Y.; Bai, H.-W.; Kang, B.S. Delphinidin enhances radio-therapeutic effects via autophagy induction and JNK/MAPK pathway activation in non-small cell lung cancer. Korean J. Physiol. Pharmacol. 2020, 24, 413–422. [Google Scholar] [CrossRef]
- Eguchi, H.; Matsunaga, H.; Onuma, S.; Yoshino, Y.; Matsunaga, T.; Ikari, A. Down-regulation of claudin-2 expression by cyanidin-3-glucoside enhances sensitivity to anticancer drugs in the spheroid of human lung adenocarcinoma A549 cells. Int. J. Mol. Sci. 2021, 22, 499. [Google Scholar] [CrossRef]
- Liao, W.; Chen, L.; Ma, X.; Jiao, R.; Li, X.; Wang, Y. Protective effects of kaempferol against reactive oxygen species-induced hemolysis and its antiproliferative activity on human cancer cells. Eur. J. Med. Chem. 2016, 114, 24–32. [Google Scholar] [CrossRef]
- Cheng, W.; Chen, K.; Lee, K.; Feng, P.; Wu, S. Nicotinic-nAChR signaling mediates drug resistance in lung cancer. J. Cancer 2020, 11, 1125–1140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bordas, A.; Cedillo, J.L.; Arnalich, F.; Esteban-Rodriguez, I.; Guerra-Pastrián, L.; de Castro, J.; Martín-Sánchez, C.; Atienza, G.; Fernández-Capitan, C.; Rios, J.J.; et al. Expression patterns for nicotinic acetylcholine receptor subunit genes in smoking-related lung cancers. Oncotarget 2017, 8, 67878–67890. [Google Scholar] [CrossRef] [Green Version]
- Schuller, H.M. Nitrosamines as nicotinic receptor ligands. Life Sci. 2007, 80, 2274–2280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirata, N.; Yamada, S.; Sekino, Y.; Kanda, Y. Tobacco nitrosamine NNK increases ALDH-positive cells via ROS-Wnt signaling pathway in A549 human lung cancer cells. J. Toxicol. Sci. 2017, 42, 193–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wen, J.; Fu, J.-H.; Zhang, W.; Guo, M. Lung carcinoma signaling pathways activated by smoking. Chin. J. Cancer. 2011, 30, 551–558. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Marti, A.; Navarro, A.; Felip, E. COX-2 inhibitors in NSCLC: Never-ending story or misplaced? Transl. Lung Cancer Res. 2018, 7 (Suppl. S3), S191–S194. [Google Scholar] [CrossRef]
- Huang, R.-Y.; Li, M.-Y.; Hsin, M.K.Y.; Underwood, M.J.; Ma, L.T.; Mok, T.S.K.; Warner, T.D.; Chen, G.G. 4-Methylnitrosamino-1-3-pyridyl-1-butanone (NNK) promotes lung cancer cell survival by stimulating thromboxane A2 and its receptor. Oncogene 2011, 30, 106–116. [Google Scholar] [CrossRef] [Green Version]
- Al-Wadei, H.A.N.; Al-Wadei, M.H.; Schuller, H.M. Cooperative regulation of non-small cell lung carcinoma by nicotinic and beta-adrenergic receptors: A novel target for intervention. PLoS ONE 2012, 7, e29915. [Google Scholar] [CrossRef] [Green Version]
- Czyżykowski, R.; Połowinczak-Przybyłek, J.; Potemski, P. Nicotine-induced resistance of non-small cell lung cancer to treatment-possible mechanisms. Adv. Hyg. Exp. Med./Postepy Hig. I Med. Dosw. 2016, 70, 186–193. [Google Scholar] [CrossRef]
- Zhang, Q.; Tang, X.; Zhang, Z.-F.; Velikina, R.; Shi, S.; Le, A.D. Nicotine induces hypoxia-inducible factor-1alpha expression in human lung cancer cells via nicotinic acetylcholine receptor-mediated signaling pathways. Clin. Cancer Res. 2007, 13, 4686–4694. [Google Scholar] [CrossRef] [Green Version]
- Dasgupta, P.; Rastogi, S.; Pillai, S.; Ordonez-Ercan, D.; Morris, M.; Haura, E.; Chellappan, S. Nicotine induces cell proliferation by β-arrestin–mediated activation of Src and Rb–Raf-1 pathways. J. Clin. Investig. 2006, 116, 2208–2217. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, P.; Rizwani, W.; Pillai, S.; Davis, R.; Banerjee, S.; Hug, K.; Lloyd, M.; Coppola, D.; Haura, E.; Chellappan, S.P. ARRB1-mediated regulation of E2F target genes in nicotine-induced growth of lung tumors. J. Natl. Cancer Inst. 2011, 103, 317–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsurutani, J.; Castillo, S.S.; Brognard, J.; Granville, G.A.; Zhang, C.; Gills, J.J.; Sayyah, J.; Dennis, P.A. Tobacco components stimulate Akt-dependent proliferation and NFkappaB-dependent survival in lung cancer cells. Carcinogenesis 2005, 26, 1182–1195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaal, C.; Chellappan, S. Nicotine-mediated regulation of nicotinic acetylcholine receptors in non-small cell lung adenocarcinoma by E2F1 and STAT1 transcription factors. PLoS ONE 2016, 11, e0156451. [Google Scholar] [CrossRef] [PubMed]
- Deng, X. Bcl2 family functions as signaling target in nicotine-/NNK-induced survival of human lung cancer cells. Scientifica 2014, 2014, 215426. [Google Scholar] [CrossRef] [Green Version]
- Memmott, R.M.; Dennis, P.A. The role of the Akt/mTOR pathway in tobacco-carcinogen induced lung tumorigenesis. Clin. Cancer Res. 2010, 16, 4–10. [Google Scholar] [CrossRef] [Green Version]
- Kalscheuer, S.; Zhang, X.; Zeng, Y.; Upadhyaya, P. Differential expression of microRNAs in early-stage neoplastic transformation in the lungs of F344 rats chronically treated with the tobacco carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone. Carcinogenesis 2008, 29, 2394–2399. [Google Scholar] [CrossRef]
- Doukas, S.G.; Vageli, D.P.; Lazopoulos, G.; Spandidos, D.A.; Sasaki, C.T.; Tsatsakis, A. The effect of NNK, a tobacco smoke carcinogen, on the miRNA and mismatch DNA repair expression profiles in lung and head and neck squamous cancer cells. Cells 2020, 9, 1031. [Google Scholar] [CrossRef] [Green Version]
- Jin, H.; Li, Q.; Cao, F.; Wang, S.-N.; Wang, R.-T.; Wang, Y.; Tan, Q.-Y.; Li, C.-R.; Zou, H.; Wang, D.; et al. miR-124 inhibits lung tumorigenesis induced by K-ras mutation and NNK. Mol. Ther. Nucleic Acids. 2017, 9, 145–154. [Google Scholar] [CrossRef] [Green Version]
- Xie, H.; Wang, J.-R.; Yau, L.-F.; Liu, Y.; Liu, L.; Han, Q.-B.; Zhao, Z.; Jiang, Z.-H. Catechins and procyanidins of Ginkgo biloba show potent activities towards the inhibition of β-amyloid peptide aggregation and destabilization of preformed fibrils. Molecules 2014, 19, 5119–5134. [Google Scholar] [CrossRef] [Green Version]
- Jin, W.; Bu, X.; Liu, Y.; Shen, L.; Zhuang, Z.; Jiao, S.; Zhu, C.; Wang, Q.; Zhou, H.; Zhang, T.; et al. Plasma amyloid-beta levels in patients with different types of cancer. Neurotox. Res. 2017, 31, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Dorandish, S.; Williams, A.; Atali, S.; Sendo, S.; Price, D.; Thompson, C.; Guthrie, J.; Heyl, D.; Evans, H.G. Regulation of amyloid-β levels by matrix metalloproteinase-2/9 (MMP2/9) in the media of lung cancer cells. Sci. Rep. 2021, 11, 9708. [Google Scholar] [CrossRef] [PubMed]
- Atali, S.; Dorandish, S.; Devos, J.; Williams, A.; Price, D.; Taylor, J.; Guthrie, J.; Heyl, D.; Evans, H.G. Interaction of amyloid beta with humanin and acetylcholinesterase is modulated by ATP. FEBS Open Biol. 2020, 10, 2805–2823. [Google Scholar] [CrossRef] [PubMed]
- Niu, X.-M.; Lu, S. Acetylcholine receptor pathway in lung cancer: New twists to an old story. World J. Clin. Oncol. 2014, 5, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.R.; Richbart, S.D.; Merritt, J.C.; Brown, K.C.; Nolan, N.A.; Akers, A.T.; Lau, J.K.; Robateau, Z.R.; Miles, S.L.; Dasgupta, P. Acetylcholine signaling system in progression of lung cancers. Pharmacol. Ther. 2019, 194, 222–254. [Google Scholar] [CrossRef]
- Xi, H.-J.; Wu, R.-P.; Liu, J.-J.; Zhang, L.-J.; Li, Z.-S. Role of acetylcholinesterase in lung cancer. Thorac. Cancer. 2015, 6, 390–398. [Google Scholar] [CrossRef]
- Pinheiro, N.M.; Miranda, C.J.C.P.; Perini, A.; Câmara, N.O.S.; Costa, S.K.P.; Alonso-Vale, M.I.C.; Caperuto, L.C.; Tibério, I.L.F.C.; Prado, M.A.M.; Martinsm, M.A.; et al. Pulmonary inflammation is regulated by the levels of the vesicular acetylcholine transporter. PLoS ONE. 2015, 10, e0120441. [Google Scholar] [CrossRef] [Green Version]
- Huang, Q.; Du, J.; Fan, J.; Lv, Z.; Qian, X.; Zhang, X.; Han, J.; Chen, C.; Wu, F.; Jin, Y. The effect of proinflammatory cytokines on IL-17RA expression in NSCLC. Med. Oncol. 2014, 31, 144. [Google Scholar] [CrossRef]
- Mohrherr, J.; Uras, I.Z.; Moll, H.P.; Casanova, E. STAT3: Versatile functions in non-small cell lung cancer. Cancers 2020, 12, 1107. [Google Scholar] [CrossRef]
- Parakh, S.; Ernst, M.; Poh, A.R. Multicellular effects of STAT3 in non-small cell lung cancer: Mechanistic insights and therapeutic opportunities. Cancers 2021, 13, 6228. [Google Scholar] [CrossRef]
- Jiang, M.; Zhang, P.; Hu, G.; Xiao, Z.; Xu, F.; Zhong, T.; Huang, F.; Kuang, H.; Zhang, W. Relative expressions of miR-205-5p, miR-205-3p, and miR-21 in tissues and serum of non-small cell lung cancer patients. Mol. Cell Biochem. 2013, 383, 67–75. [Google Scholar] [CrossRef]
- Sheng, W.; Guo, W.; Lu, F.; Liu, H.; Xia, R.; Dong, F. Upregulation of Linc00284 promotes lung cancer progression by regulating the miR-205-3p/c-met axis. Front. Genet. 2021, 12, 694571. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Xiong, J.; Zhang, Y.; Dai, Y.; Ren, X.; Ren, Y.; Han, D.; Wei, S.; Qi, M. miR-205-3p promotes lung cancer progression by targeting APBB2. Mol. Med. Rep. 2021, 24, 588. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.; Jung, H.; Hwang, K.T. Bioconversion of cyanidin-3-rutinoside to cyanidin-3-glucoside in black raspberry by crude α-L-rhamnosidase from aspergillus species. J. Microbiol. Biotechnol. 2015, 25, 1842–1848. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.-J.; Zhu, C.-T.; Zhang, L.-Y.; You, S.; Wu, F.-A.; Wang, J. Enrichment and purification of red pigments from defective mulberry fruits using biotransformation in a liquid-liquid-solid three-phase system. Environ. Sci. Pollut. Res. Int. 2021, 28, 24432–24440. [Google Scholar] [CrossRef]
| Study Type | NSCLC Cell Type | Extract/Compound | Concentrations | Activity | Mechanisms of Action | Reference |
|---|---|---|---|---|---|---|
| In vitro | DMS114 | Cranberry presscake | 200–300 µmol/L | Anti-proliferative, apoptosis | NA | [40] |
| In vitro | H460 | Cranberry (Vaccinium macrocarpon) | 20–80 µg/mL | Anti-proliferative | MMP2, MMP9↓ | [41] |
| In vitro | H460 | Cranberry (Vaccinium macrocarpon) | 50 µg/mL | Apoptosis, cell cycle arrest | P21, P73, PARP, cytochrome c, caspase3/4/8↑ Bcl-2↓ | [42] |
| In vitro/vivo | A549 | Grape seed | 100 µg/mL (in vitro) 30 mg PC/kg bodyweight (in vivo) | Inhibition of tumor angiogenesis | MMP2↓ | [43] |
| In vitro/vivo | A549, H1299 | Grape seed | 60, 80 µg/mL (in vitro) Administration of PCs (0.1%, 0.2%, and 0.5%, bodyweight) (in vivo) | Anti-proliferative, anti-angiogenic, apoptosis | PCNA↓ IGFBP-3↑ | [44] |
| In vitro/vivo | H157, H226, H460, H1299, A549 | Grape seed | 20, 40, and 60 µg/mL (in vitro) Administration of PCs (0.5%, bodyweight) (in vivo) | Anti-proliferative, apoptosis | COX-2, PGI-2↓ | [45] |
| In vitro | A549, H1299 | Grape seed | 10, 20, 40, and 60 µg/mL | Anti-migration | NO, L-NAME, MAPK, ERK1/2↓ | [46] |
| In vitro | A549 | Grape seed | 6 µg/mL | Anti-proliferative, apoptosis | caspase 3, PTGIS/PGI2↑ | [47] |
| In vitro | A549, H1299, H460 | Grape seed | 20 and 40 µg/mL | Anti-migration | E-cadherin, NOX, p22/p47(phox)↓ N-cadherin, fibronectin, vimentin↑ | [48] |
| In vitro/vivo | A549, H1299 | Grape seed | 20, 40, and 60 µg/mL (in vitro) 50, 100, and 200 mg PC/kg bodyweight (in vivo) | Apoptosis | G1arrest, Bax, caspases-3/9, Cdki, PARP↑ Bcl-2,Bcl-xl, Cdk2/4/6, cyclins↓ | [49] |
| In vitro/vivo | A549 | Grape seed | 45 µg/mL (in vitro) 112 mg PC/kg bodyweight (in vivo) | Anti-proliferative, anti-invasive | CDKN1A, p21↑, miR-106b↓ | [50] |
| In vitro | A549 | Cinnamomi Cortex | 2.5 µg/mL | Inhibition of cell viability and proliferation | Nrf2↓ | [51] |
| In vitro | A549 | Cinnamomi Cortex | 10 µg/mL | Inhibition of cell proliferation | Nrf2, IGF-1R↓ | [52] |
| In vitro | A549 | Cinnamomi Cortex | 12.5, 25, 50, and 100 µg/mL | Anti-metastatic | TGF-β, snail, E-cadherin, smad2↓ | [53] |
| In vitro | A549 | PCs | ≥100 mg/L | Inhibition of cell viability | ROS, MDA, Nrf2↓ HO-1, NQO1, TXNRD1, glutathione, catalase, superoxide dismutase↑ | [54] |
| In vitro | A549 | PCs | 12.5, 25, 50, 100, and 200 µM | Inhibition of cell viability and proliferation, apoptosis, cell cycle arrest | N-cadherin, vimentin, Bcl-2, MMP2/9, JAK2/STAT3↓, Bax↑ | [55] |
| In vitro | A549 | Green tea leaf | 1, 5, 10, 20 µM | Anti-proliferative, apoptosis, cell cycle arrest | P21, P53, Fas/sFasL, Fas/APO-1↑ | [56] |
| In vitro | A549 | Myrica rubra | 0.5, 2.5, 5, and 10 µM | Anti-proliferative, apoptosis, cell cycle arrest | Fas/APO-1, P21/WAF1, P53, Fas/sFasL↑ | [57] |
| In vitro | A549, H460 | Rhododendron formosanum | 125, 150, and 175 µM | Autophagy | Akt/mTOR↓ | [58] |
| Study Type | NSCLC Cell Type | Extract/Compound | Concentrations | Activity | Mechanisms of Action | Reference |
|---|---|---|---|---|---|---|
| In vitro | A549 | Vitis coignetiae Pulliat | 200 µg/mL | Anti-proliferative, anti-invasive, anti-angiogenic, anti-migration | MMP2/9, cyclin D1, C-myc, COX-2, VEGF↓ | [60] |
| In vitro | A549 | Morus alba L. | 25, 50, and 100 µM | Anti-migration, anti-invasive | MMP2, c-Jun, C-fos, NF-kB↓ | [61] |
| In vitro | A549, H1299 | Cyanidin-3-glucoside | 5, 10, 20, 40, and 80 µM | Anti-proliferative, anti-migration, anti-invasive, apoptosis | TP53I3 andPI3K/Akt/mTOR↓ | [62] |
| In vitro/vivo | A549, H441, SK-MES-1 | Delphinidin | 5–100 µM (in vitro) 1, 2 mg PC/kg bodyweight (in vivo) | Inhibition of tumor growth, anti-proliferative, anti-angiogenic, apoptosis | EGFR, Bcl-2, PCNA, cyclin D1, VEGFA, Akt/PI3K/MAPK↓ Bax, caspase-3/9↑ | [63] |
| In vitro/vivo | A549 | Delphinidin | 10, 20, and 40 µM (in vitro) 80 µM (in vivo) | Anti-angiogenic | EGF, CoCl2, HIF-1α, ERK, VEGF mRNA, Akt/mTOR/PI3K/p70S6K↓ | [64] |
| In vitro/vivo | A549, H1299 | Bilberry and blueberry | 3.125–12.5 µM (in vitro) 1.5 mg PC/kg bodyweight (in vivo) | Anti-metastatic, anti-invasive, apoptosis, cell cyclearrest | TNFα-induced NF-kB, Notch, Wnt/β-catenin, cyclinD1/B1, VEGF, p-ERK, bcl-2, MMP9 ↓ | [65] |
| In vitro | A549 | Syzygium cumini L. | 2.5, 5, 10, 20, and 25 µM | Anti-proliferative | NA | [66] |
| Study Type | NSCLC Cell Type | Extract/Compound | Concentrations | Activity | Mechanisms of Action | Reference |
|---|---|---|---|---|---|---|
| In vitro | A549 | Cinnamomi Cortex | 100–300 µg/mL | Anti-proliferative | Nrf2↓ | [67] |
| In vitro/In vivo | A549 | Grape seed | 20 µg/mL (in vitro) 2 mg PC/kg bodyweight (in vivo) | Anti-inflammation, apoptosis | ROS, IL-6, IFN-γ↓ P53, p-JNK, MAPK↑ | [68] |
| In vitro | A549 | Delphinidin | 10, 20, and 50 µM | Apoptosis, autophagy | p-ERK1/2↓, caspase-3, LC3, p-JNK, MAPK ↑ | [69] |
| In vitro | A549 | Cyanidin-3-glucoside | 1, 10, 20, and 50 µM | Apoptosis, autophagy | CLDN2, p-Akt↓, P38 MAPK↑ | [70] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsharairi, N.A. Insights into the Mechanisms of Action of Proanthocyanidins and Anthocyanins in the Treatment of Nicotine-Induced Non-Small Cell Lung Cancer. Int. J. Mol. Sci. 2022, 23, 7905. https://doi.org/10.3390/ijms23147905
Alsharairi NA. Insights into the Mechanisms of Action of Proanthocyanidins and Anthocyanins in the Treatment of Nicotine-Induced Non-Small Cell Lung Cancer. International Journal of Molecular Sciences. 2022; 23(14):7905. https://doi.org/10.3390/ijms23147905
Chicago/Turabian StyleAlsharairi, Naser A. 2022. "Insights into the Mechanisms of Action of Proanthocyanidins and Anthocyanins in the Treatment of Nicotine-Induced Non-Small Cell Lung Cancer" International Journal of Molecular Sciences 23, no. 14: 7905. https://doi.org/10.3390/ijms23147905
APA StyleAlsharairi, N. A. (2022). Insights into the Mechanisms of Action of Proanthocyanidins and Anthocyanins in the Treatment of Nicotine-Induced Non-Small Cell Lung Cancer. International Journal of Molecular Sciences, 23(14), 7905. https://doi.org/10.3390/ijms23147905






