Effect of Mortalin on Scar Formation in Human Dermal Fibroblasts and a Rat Incisional Scar Model
Abstract
:1. Introduction
2. Results
2.1. In Vitro Study
2.1.1. Mortalin Acts as Profibrotic Molecules in HDFs
2.1.2. Mortalin Increased Intracellular Signaling via TGF-β1 and NF-κB
2.1.3. Mortalin Activates the IL-1α Receptor, Interacts with the IL-1α Receptor in the Cytosol, and Internalizes the IL-1α Receptor in Keloid Tissues
2.2. In Vivo Study
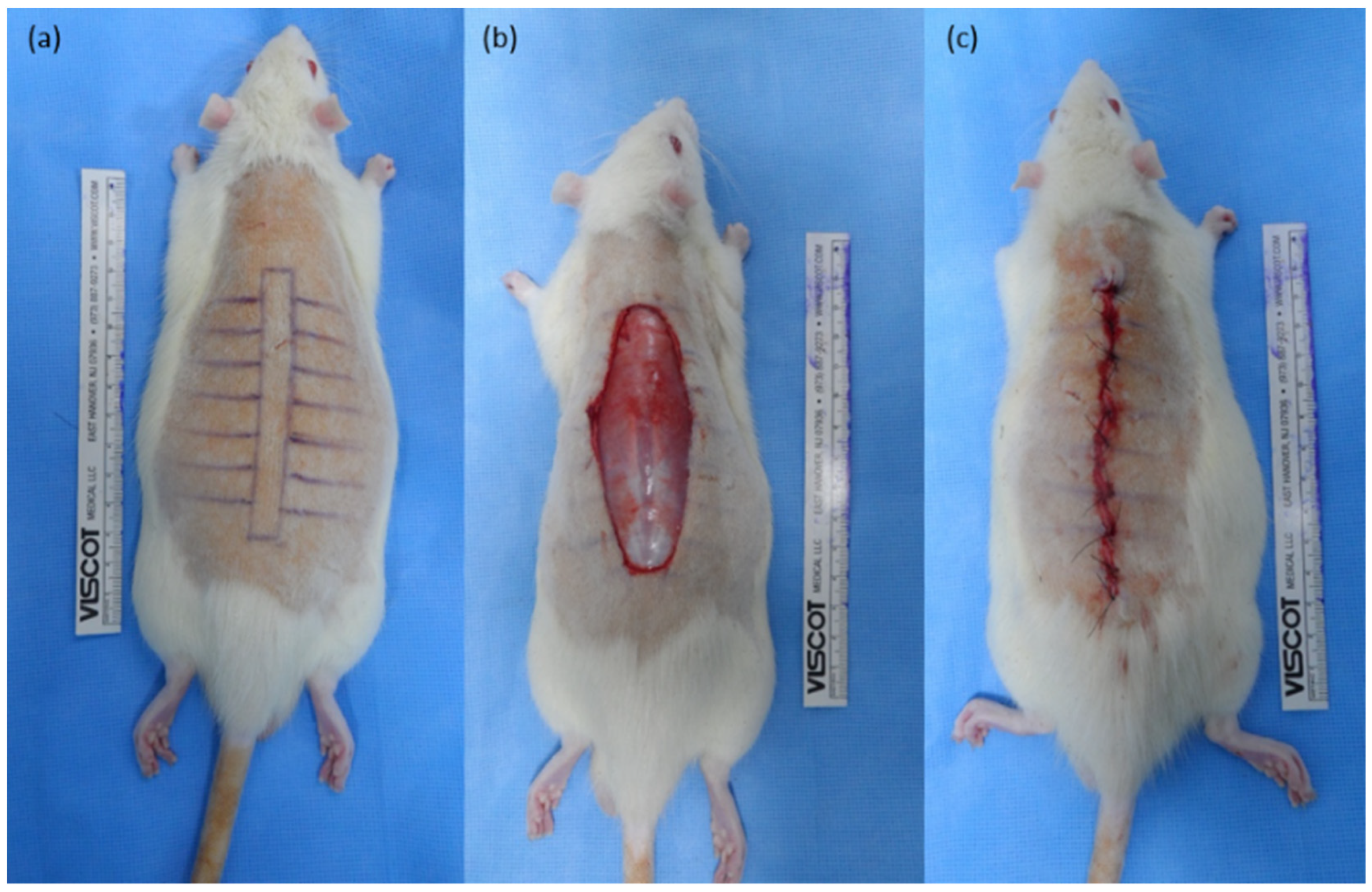
2.2.1. Mortalin-Specific shRNA-Expressing Ad Vectors Decreased Scar Size in Rat Incisional Scar Model
2.2.2. Mortalin-Specific shRNA-Expressing Ad Decreases Collagen Type I Expression in Rat Incisional Scar Tissue
2.2.3. Mortalin-Specific shRNA-Expressing Ad Decreases the Expression of α-SMA and pSmad2/3 Complex in Rat Incisional Scar Tissue
3. Discussion
4. Materials and Methods
4.1. In Vitro Studies
4.1.1. Keloid Tissue, HDF, and Normal Abdominal Tissue
4.1.2. Cell Viability Assay
4.1.3. qRT-PCR
4.1.4. Western Blot Analysis
4.1.5. Immunofluorescence Assay
4.1.6. Immunoprecipitation Assay
4.2. In Vivo Rat Incisional Scar Model
4.2.1. Animal Model
4.2.2. Generating shMot-Expressing Adenoviral Vectors
4.2.3. Injection of Ad into the Rat Incision Model
4.2.4. Histologic Analysis
4.2.5. Western Blot Analysis
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bran, G.M.; Goessler, U.R.; Hormann, K.; Riedel, F.; Sadick, H. Keloids: Current concepts of pathogenesis (review). Int. J. Mol. Med. 2009, 24, 283–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, C.H.; Ogawa, R. Keloid research: Current status and future directions. Scars Burn. Heal. 2019, 5, 2059513119868659. [Google Scholar] [CrossRef] [PubMed]
- Chike-Obi, C.J.; Cole, P.D.; Brissett, A.E. Keloids: Pathogenesis, clinical features, and management. Semin. Plast. Surg. 2009, 23, 178–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nosrati, H.; Aramideh Khouy, R.; Nosrati, A.; Khodaei, M.; Banitalebi-Dehkordi, M.; Ashrafi-Dehkordi, K.; Sanami, S.; Alizadeh, Z. Nanocomposite scaffolds for accelerating chronic wound healing by enhancing angiogenesis. J. Nanobiotechnol. 2021, 19, 1. [Google Scholar] [CrossRef]
- Xu, Z.; Liu, G.; Liu, P.; Hu, Y.; Chen, Y.; Fang, Y.; Sun, G.; Huang, H.; Wu, J. Hyaluronic acid-based glucose-responsive antioxidant hydrogel platform for enhanced diabetic wound repair. Acta Biomater. 2022, 147, 147–157. [Google Scholar] [CrossRef]
- Xu, Z.; Liu, G.; Huang, J.; Wu, J. Novel Glucose-Responsive Antioxidant Hybrid Hydrogel for Enhanced Diabetic Wound Repair. ACS Appl. Mater. Interfaces 2022, 14, 7680–7689. [Google Scholar] [CrossRef]
- Xian, C.H.; Zhang, Z.; You, X.R.; Fang, Y.F.; Wu, J. Nanosized Fat Emulsion Injection Modulating Local Microenvironment Promotes Angiogenesis in Chronic Wound Healing. Adv. Funct. Mater. 2022, 2202410. [Google Scholar] [CrossRef]
- Tuan, T.L.; Nichter, L.S. The molecular basis of keloid and hypertrophic scar formation. Mol. Med. Today 1998, 4, 19–24. [Google Scholar] [CrossRef]
- Boxman, I.; Lowik, C.; Aarden, L.; Ponec, M. Modulation of IL-6 production and IL-1 activity by keratinocyte-fibroblast interaction. J. Investig. Dermatol. 1993, 101, 316–324. [Google Scholar] [CrossRef] [Green Version]
- Dmitrieva, O.S.; Shilovskiy, I.P.; Khaitov, M.R.; Grivennikov, S.I. Interleukins 1 and 6 as Main Mediators of Inflammation and Cancer. Biochemistry 2016, 81, 80–90. [Google Scholar] [CrossRef]
- Wadhwa, R.; Taira, K.; Kaul, S.C. An Hsp70 family chaperone, mortalin/mthsp70/PBP74/Grp75: What, when, and where? Cell Stress Chaperones 2002, 7, 309–316. [Google Scholar] [CrossRef]
- Bellaye, P.S.; Burgy, O.; Causse, S.; Garrido, C.; Bonniaud, P. Heat shock proteins in fibrosis and wound healing: Good or evil? Pharmacol. Ther. 2014, 143, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Ahn, H.M.; Na, Y.; Wadhwa, R.; Hong, J.; Yun, C.O. Mortalin deficiency suppresses fibrosis and induces apoptosis in keloid spheroids. Sci. Rep. 2017, 7, 12957. [Google Scholar] [CrossRef] [Green Version]
- Sacht, G.; Brigelius-Flohe, R.; Kiess, M.; Sztajer, H.; Flohe, L. ATP-sensitive association of mortalin with the IL-1 receptor type I. Biofactors 1999, 9, 49–60. [Google Scholar] [CrossRef]
- Chartier, C.; Degryse, E.; Gantzer, M.; Dieterle, A.; Pavirani, A.; Mehtali, M. Efficient generation of recombinant adenovirus vectors by homologous recombination in Escherichia coli. J. Virol. 1996, 70, 4805–4810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.; Cho, J.Y.; Kim, J.H.; Jung, K.C.; Yun, C.O. Evaluation of E1B gene-attenuated replicating adenoviruses for cancer gene therapy. Cancer Gene Ther. 2002, 9, 725–736. [Google Scholar] [CrossRef] [Green Version]
- Ahi, Y.S.; Bangari, D.S.; Mittal, S.K. Adenoviral vector immunity: Its implications and circumvention strategies. Curr. Gene Ther. 2011, 11, 307–320. [Google Scholar] [CrossRef]
- Choi, J.W.; Kang, E.; Kwon, O.J.; Yun, T.J.; Park, H.K.; Kim, P.H.; Kim, S.W.; Kim, J.H.; Yun, C.O. Local sustained delivery of oncolytic adenovirus with injectable alginate gel for cancer virotherapy. Gene Ther. 2013, 20, 880–892. [Google Scholar] [CrossRef] [Green Version]
- Supp, D.M. Animal Models for Studies of Keloid Scarring. Adv. Wound Care 2019, 8, 77–89. [Google Scholar] [CrossRef]
- Lee, W.J.; Choi, I.K.; Lee, J.H.; Kim, Y.O.; Yun, C.O. A novel three-dimensional model system for keloid study: Organotypic multicellular scar model. Wound Repair Regen. 2013, 21, 155–165. [Google Scholar] [CrossRef]
- Lei, J.A.; Zhou, Y.; Qin, Z.L. Research advances on inflammatory responses involved in keloid development. Zhonghua Shao Shang Za Zhi 2021, 37, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Elsaie, M.L. Update on management of keloid and hypertrophic scars: A systemic review. J. Cosmet. Dermatol. 2021, 20, 2729–2738. [Google Scholar] [CrossRef]
- Van den Broek, L.J.; Limandjaja, G.C.; Niessen, F.B.; Gibbs, S. Human hypertrophic and keloid scar models: Principles, limitations and future challenges from a tissue engineering perspective. Exp. Dermatol. 2014, 23, 382–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Limandjaja, G.C.; van den Broek, L.J.; Breetveld, M.; Waaijman, T.; Monstrey, S.; de Boer, E.M.; Scheper, R.J.; Niessen, F.B.; Gibbs, S. Characterization of In Vitro Reconstructed Human Normotrophic, Hypertrophic, and Keloid Scar Models. Tissue Eng. Part. C Methods 2018, 24, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Limandjaja, G.C.; Niessen, F.B.; Scheper, R.J.; Gibbs, S. The Keloid Disorder: Heterogeneity, Histopathology, Mechanisms and Models. Front. Cell Dev. Biol. 2020, 8, 360. [Google Scholar] [CrossRef]
- Dong, X.; Mao, S.; Wen, H. Upregulation of proinflammatory genes in skin lesions may be the cause of keloid formation (Review). Biomed. Rep. 2013, 1, 833–836. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Akaishi, S.; Hyakusoku, H.; Ogawa, R. Are keloid and hypertrophic scar different forms of the same disorder? A fibroproliferative skin disorder hypothesis based on keloid findings. Int. Wound J. 2014, 11, 517–522. [Google Scholar] [CrossRef]
- Meenakshi, J.; Jayaraman, V.; Ramakrishnan, K.M.; Babu, M. Ultrastructural differentiation of abnormal scars. Ann. Burn. Fire Disasters 2005, 18, 83–88. [Google Scholar]
- Ueda, K.; Yasuda, Y.; Furuya, E.; Oba, S. Inadequate blood supply persists in keloids. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2004, 38, 267–271. [Google Scholar] [CrossRef]
- Ueda, K.; Furuya, E.; Yasuda, Y.; Oba, S.; Tajima, S. Keloids have continuous high metabolic activity. Plast. Reconstr. Surg. 1999, 104, 694–698. [Google Scholar] [CrossRef]
- Le, A.D.; Zhang, Q.; Wu, Y.; Messadi, D.V.; Akhondzadeh, A.; Nguyen, A.L.; Aghaloo, T.L.; Kelly, A.P.; Bertolami, C.N. Elevated vascular endothelial growth factor in keloids: Relevance to tissue fibrosis. Cells Tissues Organs 2004, 176, 87–94. [Google Scholar] [CrossRef]
- Akaishi, S.; Ogawa, R.; Hyakusoku, H. Keloid and hypertrophic scar: Neurogenic inflammation hypotheses. Med. Hypotheses 2008, 71, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Zachariae, H. Delayed wound healing and keloid formation following argon laser treatment or dermabrasion during isotretinoin treatment. Br. J. Dermatol. 1988, 118, 703–706. [Google Scholar] [CrossRef] [PubMed]
- Shih, B.; Garside, E.; McGrouther, D.A.; Bayat, A. Molecular dissection of abnormal wound healing processes resulting in keloid disease. Wound Repair Regen. 2010, 18, 139–153. [Google Scholar] [CrossRef] [PubMed]
- Ghahary, A.; Shen, Y.J.; Scott, P.G.; Tredget, E.E. Expression of mRNA for transforming growth factor-beta 1 is reduced in hypertrophic scar and normal dermal fibroblasts following serial passage in vitro. J. Investig. Dermatol. 1994, 103, 684–686. [Google Scholar] [CrossRef] [Green Version]
- Lin, R.Y.; Sullivan, K.M.; Argenta, P.A.; Meuli, M.; Lorenz, H.P.; Adzick, N.S. Exogenous transforming growth factor-beta amplifies its own expression and induces scar formation in a model of human fetal skin repair. Ann. Surg. 1995, 222, 146–154. [Google Scholar] [CrossRef]
- Huang, Y.; Wang, Y.; Wang, X.; Lin, L.; Wang, P.; Sun, J.; Jiang, L. The Effects of the Transforming Growth Factor-beta1 (TGF-beta1) Signaling Pathway on Cell Proliferation and Cell Migration are Mediated by Ubiquitin Specific Protease 4 (USP4) in Hypertrophic Scar Tissue and Primary Fibroblast Cultures. Med. Sci. Monit. 2020, 26, e920736. [Google Scholar] [CrossRef]
- Zhang, D.; Li, B.; Zhao, M. Therapeutic Strategies by Regulating Interleukin Family to Suppress Inflammation in Hypertrophic Scar and Keloid. Front. Pharmacol. 2021, 12, 667763. [Google Scholar] [CrossRef]
- Gabay, O.; Sanchez, C.; Taboas, J.M. Bio-ingénierie du cartilage. Rev. Rhum. Ed. Fr. 2010, 77, 319–322. [Google Scholar] [CrossRef] [Green Version]
- Gallant-Behm, C.L.; Du, P.; Lin, S.M.; Marucha, P.T.; DiPietro, L.A.; Mustoe, T.A. Epithelial regulation of mesenchymal tissue behavior. J. Investig. Dermatol. 2011, 131, 892–899. [Google Scholar] [CrossRef] [Green Version]
- Hao, Y.; Dong, X.; Zhang, M.; Liu, H.; Zhu, L.; Wang, Y. Effects of hyperbaric oxygen therapy on the expression levels of the inflammatory factors interleukin-12p40, macrophage inflammatory protein-1beta, platelet-derived growth factor-BB, and interleukin-1 receptor antagonist in keloids. Medicine 2020, 99, e19857. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.K.; Hong, S.K.; Park, J.I. Mortalin depletion induces MEK/ERK-dependent and ANT/CypD-mediated death in vemurafenib-resistant B-Raf(V600E) melanoma cells. Cancer Lett. 2021, 502, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Meng, Z.; Wu, X.; Zhang, M.; Zhang, S.; Jin, T. Mortalin promotes breast cancer malignancy. Exp. Mol. Pathol. 2021, 118, 104593. [Google Scholar] [CrossRef] [PubMed]
- Ramraj, S.K.; Elayapillai, S.P.; Pelikan, R.C.; Zhao, Y.D.; Isingizwe, Z.R.; Kennedy, A.L.; Lightfoot, S.A.; Benbrook, D.M. Novel ovarian cancer maintenance therapy targeted at mortalin and mutant p53. Int. J. Cancer 2020, 147, 1086–1097. [Google Scholar] [CrossRef]
- Starenki, D.; Sosonkina, N.; Hong, S.K.; Lloyd, R.V.; Park, J.I. Mortalin (GRP75/HSPA9) Promotes Survival and Proliferation of Thyroid Carcinoma Cells. Int. J. Mol. Sci. 2019, 20, 2069. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Garron, T.M.; Li, X.J.; Liu, Y.; Zhang, X.; Li, Y.Y.; Xu, W.S. Recombinant human decorin inhibits TGF-beta1-induced contraction of collagen lattice by hypertrophic scar fibroblasts. Burns 2009, 35, 527–537. [Google Scholar] [CrossRef]
- Lee, C.H.; Hong, C.H.; Chen, Y.T.; Chen, Y.C.; Shen, M.R. TGF-beta1 increases cell rigidity by enhancing expression of smooth muscle actin: Keloid-derived fibroblasts as a model for cellular mechanics. J. Dermatol. Sci. 2012, 67, 173–180. [Google Scholar] [CrossRef]
- Fang, X.; Hu, X.; Zheng, Z.; Tao, K.; Wang, H.; Guan, H.; Shi, J.; Ji, P.; Cai, W.; Bai, X.; et al. Smad interacting protein 1 influences transforming growth factor-beta1/Smad signaling in extracellular matrix protein production and hypertrophic scar formation. J. Mol. Histol. 2019, 50, 503–514. [Google Scholar] [CrossRef]
- Zhu, G.; Cai, J.; Zhang, J.; Zhao, Y.; Xu, B. Abnormal nuclear factor (NF)-kappaB signal pathway and aspirin inhibits tumor necrosis factor alpha-induced NF-kappaB activation in keloid fibroblasts. Dermatol. Surg. 2007, 33, 697–708. [Google Scholar] [CrossRef]
- Gao, J.; Tao, J.; Zhang, N.; Liu, Y.; Jiang, M.; Hou, Y.; Wang, Q.; Bai, G. Formula optimization of the Jiashitang scar removal ointment and antiinflammatory compounds screening by NF-kappaB bioactivity-guided dual-luciferase reporter assay system. Phytother. Res. 2015, 29, 241–250. [Google Scholar] [CrossRef]
- Messadi, D.V.; Doung, H.S.; Zhang, Q.; Kelly, A.P.; Tuan, T.L.; Reichenberger, E.; Le, A.D. Activation of NFkappaB signal pathways in keloid fibroblasts. Arch. Dermatol. Res. 2004, 296, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Hinata, K.; Gervin, A.M.; Jennifer Zhang, Y.; Khavari, P.A. Divergent gene regulation and growth effects by NF-kappa B in epithelial and mesenchymal cells of human skin. Oncogene 2003, 22, 1955–1964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, W.J.; Kim, Y.O.; Choi, I.K.; Rah, D.K.; Yun, C.O. Adenovirus-relaxin gene therapy for keloids: Implication for reversing pathological fibrosis. Br. J. Dermatol. 2011, 165, 673–677. [Google Scholar] [CrossRef]
- Lee, W.J.; Choi, I.K.; Lee, J.H.; Lee, J.S.; Kim, Y.O.; Rah, D.K.; Yun, C.O. Relaxin-expressing adenovirus decreases collagen synthesis and up-regulates matrix metalloproteinase expression in keloid fibroblasts: In vitro experiments. Plast. Reconstr. Surg. 2012, 130, 407e–417e. [Google Scholar] [CrossRef] [PubMed]
- Yun, I.S.; Kang, E.; Ahn, H.M.; Kim, Y.O.; Rah, D.K.; Roh, T.S.; Lee, W.J.; Yun, C.O. Effect of Relaxin Expression from an Alginate Gel-Encapsulated Adenovirus on Scar Remodeling in a Pig Model. Yonsei Med. J. 2019, 60, 854–863. [Google Scholar] [CrossRef]
- Wu, H.; Yoon, A.R.; Li, F.; Yun, C.O.; Mahato, R.I. RGD peptide-modified adenovirus expressing hepatocyte growth factor and X-linked inhibitor of apoptosis improves islet transplantation. J. Gene Med. 2011, 13, 658–669. [Google Scholar] [CrossRef] [Green Version]
- Yoo, J.Y.; Ryu, J.; Gao, R.; Yaguchi, T.; Kaul, S.C.; Wadhwa, R.; Yun, C.O. Tumor suppression by apoptotic and anti-angiogenic effects of mortalin-targeting adeno-oncolytic virus. J. Gene Med. 2010, 12, 586–595. [Google Scholar] [CrossRef]
- Yoo, J.Y.; Kim, J.H.; Kim, J.; Huang, J.H.; Zhang, S.N.; Kang, Y.A.; Kim, H.; Yun, C.O. Short hairpin RNA-expressing oncolytic adenovirus-mediated inhibition of IL-8: Effects on antiangiogenesis and tumor growth inhibition. Gene Ther. 2008, 15, 635–651. [Google Scholar] [CrossRef]
- Yoo, J.Y.; Kim, J.H.; Kwon, Y.G.; Kim, E.C.; Kim, N.K.; Choi, H.J.; Yun, C.O. VEGF-specific short hairpin RNA-expressing oncolytic adenovirus elicits potent inhibition of angiogenesis and tumor growth. Mol. Ther. 2007, 15, 295–302. [Google Scholar] [CrossRef]








| Group | MTT Assay | |
|---|---|---|
| Mean ± SD | (% of Control) | |
| Control (HDFs only) | 1.64 ± 0.083 | 100 |
| HDFs + 10 ng TGF-β1 | 1.78 ± 0.067 | 108.54 |
| HDFs + 100 ng mortalin | 1.79 ± 0.088 | 108.96 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, B.K.; Roh, T.S.; Roh, H.; Lee, J.H.; Yun, C.-O.; Lee, W.J. Effect of Mortalin on Scar Formation in Human Dermal Fibroblasts and a Rat Incisional Scar Model. Int. J. Mol. Sci. 2022, 23, 7918. https://doi.org/10.3390/ijms23147918
Jung BK, Roh TS, Roh H, Lee JH, Yun C-O, Lee WJ. Effect of Mortalin on Scar Formation in Human Dermal Fibroblasts and a Rat Incisional Scar Model. International Journal of Molecular Sciences. 2022; 23(14):7918. https://doi.org/10.3390/ijms23147918
Chicago/Turabian StyleJung, Bok Ki, Tai Suk Roh, Hyun Roh, Ju Hee Lee, Chae-Ok Yun, and Won Jai Lee. 2022. "Effect of Mortalin on Scar Formation in Human Dermal Fibroblasts and a Rat Incisional Scar Model" International Journal of Molecular Sciences 23, no. 14: 7918. https://doi.org/10.3390/ijms23147918
APA StyleJung, B. K., Roh, T. S., Roh, H., Lee, J. H., Yun, C.-O., & Lee, W. J. (2022). Effect of Mortalin on Scar Formation in Human Dermal Fibroblasts and a Rat Incisional Scar Model. International Journal of Molecular Sciences, 23(14), 7918. https://doi.org/10.3390/ijms23147918







