The Use of Distinctive Monoclonal Antibodies in FMD VLP- and P1-Based Blocking ELISA for the Seromonitoring of Vaccinated Swine
Abstract
:1. Introduction
2. Results
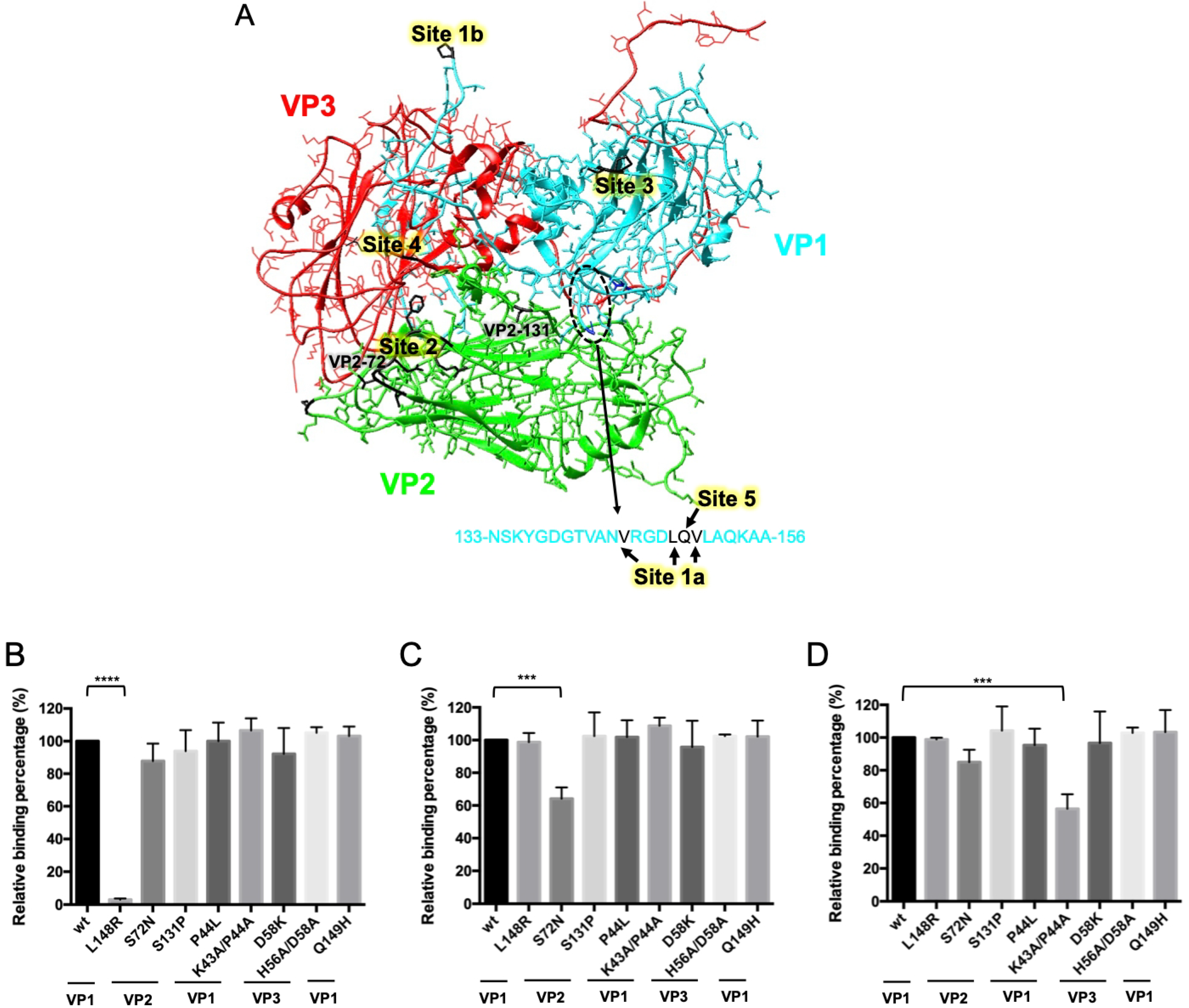
2.1. Identification of Binding Site for S11B Monoclonal Antibody
2.2. Establishment of VLP- and GST-P1-Based bELISA
2.3. Evaluation of VLP- and GST-P1-Based bELISA
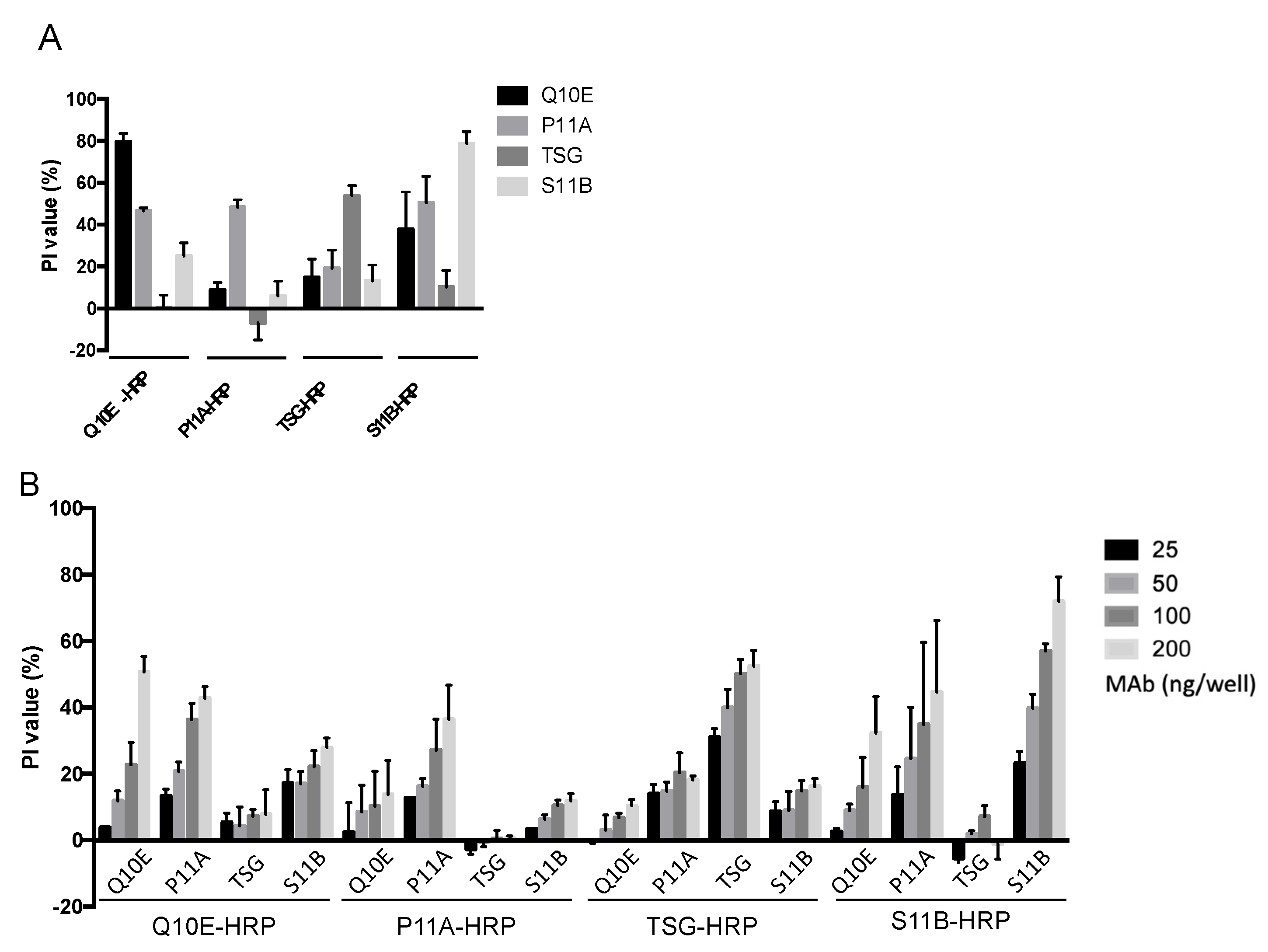
2.4. Steric Effect between Q10E, P11A, S11B, and the Non-Neutralizing Antibody TSG
3. Discussion
4. Materials and Methods
4.1. Viruses and Cells
4.2. Swine Sera
4.3. Plasmid Constructions
4.4. Purification and Conjugation of MAbs
4.5. Expression of VLPs and mVLPs for ELISA
4.6. Sandwich ELISA
4.7. Expression and Purification of GST-P1
4.8. Serum Neutralization Test (SNT)
4.9. VLP-Based bELISA
4.10. P1-Based bELISA
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jamal, S.M.; Belsham, G.J. Foot-and-mouth disease: Past, present and future. Vet. Res. 2013, 44, 116. [Google Scholar] [CrossRef] [PubMed]
- Mason, P.W.; Grubman, M.J.; Baxt, B. Molecular basis of pathogenesis of FMDV. Virus Res. 2003, 91, 9–32. [Google Scholar] [CrossRef]
- Dunn, C.S.; Donaldson, A.I. Natural adaptation to pigs of a Taiwanese isolate of foot-and-mouth disease virus. Vet. Rec. 1997, 141, 174–175. [Google Scholar] [CrossRef] [PubMed]
- OIE. Foot and mouth disease. In OIE Terrestrial Manual; OIE: Paris, France, 2021. [Google Scholar]
- Knowles, N.J.; Samuel, A.R.; Davies, P.R.; Midgley, R.J.; Valarcher, J.F. Pandemic strain of foot-and-mouth disease virus serotype O. Emerg. Infect Dis. 2005, 11, 1887–1893. [Google Scholar] [CrossRef] [PubMed]
- Mason, P.W.; Pacheco, J.M.; Zhao, Q.Z.; Knowles, N.J. Comparisons of the complete genomes of Asian, African and European isolates of a recent foot-and-mouth disease virus type O pandemic strain (PanAsia). J. Gen. Virol. 2003, 84 Pt 6, 1583–1593. [Google Scholar] [CrossRef]
- Wang, G.; Wang, Y.; Shang, Y.; Zhang, Z.; Liu, X. How foot-and-mouth disease virus receptor mediates foot-and-mouth disease virus infection. Virol. J. 2015, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, P.; Rai, D.; Conderino, J.S.; Uddowla, S.; Rieder, E. Role of Jumonji C-domain containing protein 6 (JMJD6) in infectivity of foot-and-mouth disease virus. Virology 2016, 492, 38–52. [Google Scholar] [CrossRef]
- Asfor, A.S.; Upadhyaya, S.; Knowles, N.J.; King, D.P.; Paton, D.J.; Mahapatra, M. Novel antibody binding determinants on the capsid surface of serotype O foot-and-mouth disease virus. J. Gen. Virol. 2014, 95 Pt 5, 1104–1116. [Google Scholar] [CrossRef] [PubMed]
- Barnett, P.V.; Samuel, A.R.; Pullen, L.; Ansell, D.; Butcher, R.N.; Parkhouse, R.M. Monoclonal antibodies, against O1 serotype foot-and-mouth disease virus, from a natural bovine host, recognize similar antigenic features to those defined by the mouse. J. Gen. Virol. 1998, 79 Pt 7, 1687–1697. [Google Scholar] [CrossRef] [PubMed]
- Crowther, J.R.; Farias, S.; Carpenter, W.C.; Samuel, A.R. Identification of a fifth neutralizable site on type O foot-and-mouth disease virus following characterization of single and quintuple monoclonal antibody escape mutants. J. Gen. Virol. 1993, 74 Pt 8, 1547–1553. [Google Scholar] [CrossRef]
- Kitson, J.D.; McCahon, D.; Belsham, G.J. Sequence analysis of monoclonal antibody resistant mutants of type O foot and mouth disease virus: Evidence for the involvement of the three surface exposed capsid proteins in four antigenic sites. Virology 1990, 179, 26–34. [Google Scholar] [CrossRef]
- McCahon, D.; Crowther, J.R.; Belsham, G.J.; Kitson, J.D.; Duchesne, M.; Have, P.; Meloen, R.H.; Morgan, D.O.; De Simone, F. Evidence for at least four antigenic sites on type O foot-and-mouth disease virus involved in neutralization; identification by single and multiple site monoclonal antibody-resistant mutants. J. Gen. Virol. 1989, 70 Pt 3, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Grazioli, S.; Fallacara, F.; Brocchi, E. Mapping of neutralising sites on FMD virus type Asia 1 and relationships with sites described in other serotypes. In Report of the Session of the Research Group of the Standing Committee of the European Commisssion of Foot and Mouth Disease; Chania: Crete, Greece, 2004; p. 44. [Google Scholar]
- Lee, H.W.; Deng, M.C.; Pan, C.H.; Chang, H.W.; Cheng, I.C. Neutralizing monoclonal antibodies against porcinophilic foot-and-mouth disease virus mapped to antigenic site 2 by utilizing novel mutagenic virus-like particles to detect the antigenic change. Vet. Microbiol. 2018, 222, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.N.; Zhang, J.; Chen, H.T.; Zhou, J.H.; Ding, Y.Z.; Liu, Y.S. An overview on ELISA techniques for FMD. Virol. J. 2011, 8, 419. [Google Scholar] [CrossRef]
- Mackay, D.K.; Bulut, A.N.; Rendle, T.; Davidson, F.; Ferris, N.P. A solid-phase competition ELISA for measuring antibody to foot-and-mouth disease virus. J. Virol. Methods 2001, 97, 33–48. [Google Scholar] [CrossRef]
- Chenard, G.; Miedema, K.; Moonen, P.; Schrijver, R.S.; Dekker, A. A solid-phase blocking ELISA for detection of type O foot-and-mouth disease virus antibodies suitable for mass serology. J. Virol. Methods 2003, 107, 89–98. [Google Scholar] [CrossRef]
- Ran, X.; Yang, Z.; Bai, M.; Zhang, Y.; Wen, X.; Guo, H.; Sun, S. Development and validation of a competitive ELISA based on bacterium-original virus-like particles of serotype O foot-and-mouth disease virus for detecting serum antibodies. Appl. Microbiol. Biotechnol. 2019, 103, 3015–3024. [Google Scholar] [CrossRef]
- Salem, R.; El-Kholy, A.A.; Omar, O.A.; Abu El-Naga, M.N.; Ibrahim, M.; Osman, G. Construction, Expression and Evaluation of Recombinant VP2 Protein for serotype-independent Detection of FMDV Seropositive Animals in Egypt. Sci. Rep. 2019, 9, 10135. [Google Scholar] [CrossRef]
- Biswal, J.K.; Bisht, P.; Mohapatra, J.K.; Ranjan, R.; Sanyal, A.; Pattnaik, B. Application of a recombinant capsid polyprotein (P1) expressed in a prokaryotic system to detect antibodies against foot-and-mouth disease virus serotype O. J. Virol. Methods 2015, 215–216, 45–51. [Google Scholar] [CrossRef]
- Cheng, I.C.; Liang, S.M.; Tu, W.J.; Chen, C.M.; Lai, S.Y.; Cheng, Y.C.; Lee, F.; Huang, T.S.; Jong, M.H. Study on the porcinophilic foot-and-mouth disease virus I. production and characterization of monoclonal antibodies against VP1. J. Vet. Med. Sci. 2006, 68, 859–864. [Google Scholar] [CrossRef]
- Basagoudanavar, S.H.; Hosamani, M.; Tamil Selvan, R.P.; Sreenivasa, B.P.; Saravanan, P.; Chandrasekhar Sagar, B.K.; Venkataramanan, R. Development of a liquid-phase blocking ELISA based on foot-and-mouth disease virus empty capsid antigen for seromonitoring vaccinated animals. Arch. Virol. 2013, 158, 993–1001. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Su, G.; Wu, Q.; Liu, J.; Tian, Y.; Liu, X.; Zhou, J.; Gao, J.; Chen, W.; Chen, D.; et al. Rab11-mediated recycling endosome role in nervous system development and neurodegenerative diseases. Int. J. Neurosci. 2021, 131, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Xu, W.; Goolia, M.; Zhang, Z. Characterization of monoclonal antibodies against foot-and-mouth disease virus serotype O and application in identification of antigenic variation in relation to vaccine strain selection. Virol. J. 2014, 11, 136. [Google Scholar] [CrossRef]
- Dong, H.; Liu, P.; Bai, M.; Wang, K.; Feng, R.; Zhu, D.; Sun, Y.; Mu, S.; Li, H.; Harmsen, M.; et al. Structural and molecular basis for foot-and-mouth disease virus neutralization by two potent protective antibodies. Protein Cell 2021, 13, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zhao, L.; Li, W.; Zhou, G.; Yu, L. Identification of a conformational epitope on the VP1 G-H Loop of type Asia1 foot-and-mouth disease virus defined by a protective monoclonal antibody. Vet. Microbiol. 2011, 148, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, P.; LaRocco, M.; Baxt, B.; Rieder, E. Examination of soluble integrin resistant mutants of foot-and-mouth disease virus. Virol. J. 2013, 10, 2. [Google Scholar] [CrossRef]
- Brown, F.; Cartwright, B. Dissociation of foot-and-mouth disease virus into its nucleic acid and protein components. Nature 1961, 192, 1163–1164. [Google Scholar] [CrossRef]
- Mahapatra, M.; Hamblin, P.; Paton, D.J. Foot-and-mouth disease virus epitope dominance in the antibody response of vaccinated animals. J. Gen. Virol. 2012, 93 Pt 3, 488–493. [Google Scholar] [CrossRef]
- Fuerst, T.R.; Niles, E.G.; Studier, F.W.; Moss, B. Eukaryotic transient-expression system based on recombinant vaccinia virus that synthesizes bacteriophage T7 RNA polymerase. Proc. Natl. Acad. Sci. USA 1986, 83, 8122–8126. [Google Scholar] [CrossRef]
- Donaldson, A.I.; JKitching, R.P.; Barnett, P.V. Foot and mouth disease. In OIE Standards Commission, Manual of Standards for Diagnostic Tests and Vaacines; Office International des Epizooties: Paris, Frace, 1996; Capter 2.1.1. [Google Scholar]


| Q10E | P11A | S11B | TSG | |
|---|---|---|---|---|
| Isotype | IgG2a/κ | IgG3/κ | IgA/κ | IgG1/κ |
| Unprocessed protomer | + | + | − | + |
| Neutralizing activity | + | + | + | − |
| Binding site | Site 1 (VP1-148) | Site 2 (VP2-72) | Site 3 (VP1-43,44) | Unknown |
| Antigen | VLP | GST-P1 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tracer | Q10E | P11A | TSG | S11B | Q10E | P11A | TSG | ||||||||
| SN | Number | + | − | + | − | + | − | + | − | + | − | + | − | + | − |
| <16 | 26 | 1 | 25 | 1 | 25 | 1 | 25 | 1 | 25 | 1 | 25 | 1 | 25 | 1 | 25 |
| 16–32 | 14 | 1 | 13 | 1 | 13 | 2 | 12 | 4 | 10 | 1 | 13 | 2 | 12 | 0 | 14 |
| >32 | 23 | 17 | 6 | 17 | 6 | 17 | 6 | 22 | 1 | 18 | 5 | 15 | 8 | 14 | 9 |
| Cut-off value | 39.55 | 30.06 | 49.65 | 33.06 | 47.45 | 26.13 | 72.15 | ||||||||
| Sensitivity * | 73.91 | 73.91 | 73.91 | 95.65 | 78.26 | 65.22 | 60.87 | ||||||||
| Specificity * | 96.15 | 96.15 | 96.15 | 96.15 | 96.15 | 96.15 | 96.15 | ||||||||
| Kappa value | 0.71 | 0.71 | 0.71 | 0.92 | 0.75 | 0.63 | 0.58 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-W.; Yang, C.-Y.; Lee, M.-C.; Chen, S.-P.; Chang, H.-W.; Cheng, I.-C. The Use of Distinctive Monoclonal Antibodies in FMD VLP- and P1-Based Blocking ELISA for the Seromonitoring of Vaccinated Swine. Int. J. Mol. Sci. 2022, 23, 8542. https://doi.org/10.3390/ijms23158542
Lee H-W, Yang C-Y, Lee M-C, Chen S-P, Chang H-W, Cheng I-C. The Use of Distinctive Monoclonal Antibodies in FMD VLP- and P1-Based Blocking ELISA for the Seromonitoring of Vaccinated Swine. International Journal of Molecular Sciences. 2022; 23(15):8542. https://doi.org/10.3390/ijms23158542
Chicago/Turabian StyleLee, Heng-Wei, Cheng-Yao Yang, Ming-Chang Lee, Shih-Ping Chen, Hui-Wen Chang, and Ivan-Chen Cheng. 2022. "The Use of Distinctive Monoclonal Antibodies in FMD VLP- and P1-Based Blocking ELISA for the Seromonitoring of Vaccinated Swine" International Journal of Molecular Sciences 23, no. 15: 8542. https://doi.org/10.3390/ijms23158542






