The Link between Gut Microbiota and Hepatic Encephalopathy
Abstract
:1. Introduction
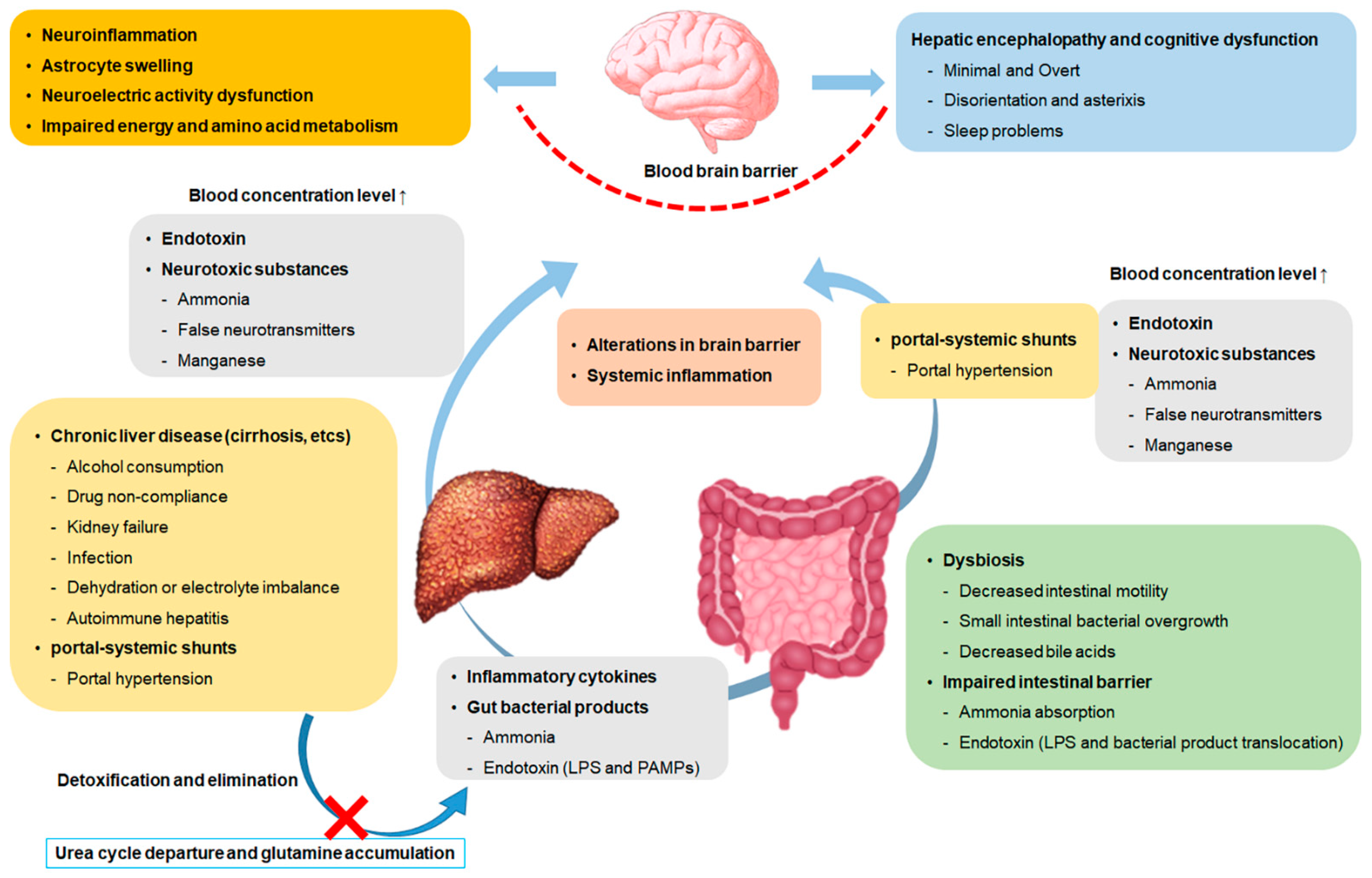
2. Gut Microbiota
3. Hepatic Encephalopathy
4. Linkage of Gut Microbiota with Hepatic Encephalopathy
4.1. Gut Microbiota in Hepatic Encephalopathy Diagnosis
| Author | Scheme | Group | Result | Ref. |
|---|---|---|---|---|
| Sung et al., 2019 | Profiled fecal microbiome changes for a cohort patients | Control/compensated cirrhosis/decompensated cirrhosis/Acute HE | Higher Firmicute, Proteobacteria, Actinobacteria and Veillonella parvula and lower Bacteroidetes phylum in AHE patients compared compensated cirrhosis. | [66] |
| Zhang et al., 2013 | Gut microbiome analysis of MHE patients with cirrhosis | MHE/cirrhotic patients without MHE | Higher Streptococcus salivarius in MHE cirrhotic patients compared no-MHE cirrhotic patients. Gut ammonia-increasing bacteria Streptococcus salivarius can be a potential biomarker in MHE cirrhotic patients. | [67] |
| Bajaj et al., 2012 | Stool analysis of cirrhosis patients and age-matched controls | Cirrhotic patients with or without HE/control | Higher Veillonellaceae in HE cirrhotic patients. Alcaligenaceae and Porphyromonadaceae were positively correlated with cognitive impairment in cirrhotic patients | [68] |
| Bajaj et al., 2012 | Sigmoid mucosal and fecal microbiome analysis to study linkage with cognition and inflammation | OHE patients/no-OHE patients/control | Higher Enterococcus, Veillonella, Megasphaera and Burkholderia in mucosal microbiota of HE patients. Lower Roseburia in mucosal microbiota of HE patients. Blautia, Fecalibacterium, Roseburia and Dorea are associated with a positive cognition state and Enterococcus, Megasphaera and Burkholderia are associated with a poor cognition state. | [49] |
4.2. Gut Microbiota in HE Treatment
4.2.1. Probiotics and Prebiotics
| Author | Scheme | Group | Result | Ref. |
|---|---|---|---|---|
| Bajaj et al., 2014 | A randomized clinical phase 1, placebo-controlled trial | LGG or placebo in cirrhotic patients with MHE | In the LGG group, Enterobacteriaceae decreased and the relative abundance of Clostridiales Incertae Sedis XIV and Lachnospiraceae increased. Endotoxemia and TNF-α were decreased in the LGG group but there was no change in cognitive function. | [52] |
| Xia et al., 2018 | A randomized clinical trial | Probiotics (Clostridium butyricum combined with Bifidobacterium infantis) or no probiotics | Clostridium cluster I and Bifidobacterium increased and Enterococcus and Enterobacteriaceae decreased in the group treated with probiotics in HBV cirrhosis patients with MHE. There was also a reduction in venous ammonia and cognitive improvement. | [69] |
| Lunia et al., 2014 | A prospective, randomized controlled trial | Cirrhosis patients without OHE given probiotics (VSL#3)/cirrhosis patients without OHE not given probiotics (VSL#3) | Treatment with probiotics for 3 months significantly reduced arterial ammonia, SIBO and OCTT levels. Probiotics have shown a preventing effect on HE. | [70] |
| Liu et al., 2004 | A randomized clinical trial | Synbiotic preparation/fermentable fiber alone/placebo | Synbiotic treatment increased the fecal content of Lactobacillus species that do not produce urease. Modulation of the gut microbiota showed a reduction in blood ammonia levels and reversal of MHE in 50% of patients. | [12] |
| Malaguarnera et al., 2010 | A randomized controlled trial | Bifidobacterium + fructooligosaccharides or lactulose in HE patients | The combination of Bifidobacterium and fructooligosaccharide at 30 days of treatment showed improvement in psychometric tests compared to the lactulose group. Treatment for 60 days showed significant improvement in psychometric tests and blood ammonia levels. | [74] |
| Moratalla et al., 2017 | Observational cohort study of cirrhosis patients with MHE | First cohort: MHE patients with or without lactulose Second cohort: Non-lactulose MHE patients going to initiate lactulose therapy | Lactulose reduces bacterial DNA translocation and improves neurocognitive test scores in MHE patients. | [71] |
| Wang et al., 2019 | A multicenter, open-label randomized controlled trial | Lactulose or control in cirrhotic patients | Treatment with lactulose significantly improved MHE recovery. Significant differences were found between lactulose responders and non-responders in Bacteroidetes, Firmicutes, Actinobacteria and Proteobacteria. | [72] |
4.2.2. Fecal Microbiota Transplantation
4.2.3. Antibiotics
| Author | Scheme | Group | Result | Ref. |
|---|---|---|---|---|
| Kang et al., 2017 | A retrospective cohort study | Rifaximin + lactulose or lactulose in non-HCC cohort or HCC cohort | In the non-HCC cohort, rifaximin was significantly associated with a lower risk of death and reduced the risk of recurrent HE, spontaneous bacterial peritonitis. In the HCC cohort, rifaximin was not associated with a risk of death. It was associated with a lower risk of spontaneous bacterial peritonitis but not with varicose bleeding or recurrent HE. The risk of Clostridium difficile-associated diarrhea was not different between the two groups. | [85] |
| Kaji et al., 2017 | A clinical trial | 20 patients with decompensated cirrhosis (Child–Pugh score > 7) | Treatment with rifaximin for 4 weeks resulted in a decrease in endotoxin activity and serum ammonia levels. Treatment with rifaximin for 4 weeks resulted in a decrease in endotoxin activity and serum ammonia levels. There was no significant difference in the diversity and composition of gut microbiota at baseline and after 4 weeks of treatment but the relative abundance of genus Veillonella and Streptococcus was lowered. | [86] |
| Bajaj et al., 2013 | A clinical trial | 20 patients with cirrhosis who had been diagnosed with MHE | There was a significant cognitive improvement and a decrease in endotoxemia after rifaximin treatment. Serum saturated and unsaturated fatty acids were significantly increased after rifaximin treatment. No significant changes in gut microbiota were observed except for the decrease of Veillonellaceae and the increase of Eubacteriaceae. | [87] |
| Zuo et al., 2017 | A randomized clinical trial | Rifaximin or rifaximin and probiotics in cirrhotic patients with MHE | Both treatments reduced overall microbiome diversity and decreased abundance of specific ammonia-producing bacteria. The treatment with rifaximin + probiotics showed a more definite effect. Patients with nonalcoholic MHE were more responsive to microbiota alteration therapy. | [88] |
| Suzuki et al., 2018 Kawaguchi et al., 2019 | A prospective, randomized studies (a phase II/III study and a phase III study) | Rifaximin or lactitol with grade I or II HE and hyperammonemia patients | Blood ammonia concentrations were significantly improved in the rifaximin group. The portal systemic encephalopathy index was significantly improved in both groups. As a result of fecal microbiome analysis of 17 participants in the clinical trial, the number of Streptococcus, Veillonella and Lactobacillus decreased after rifaximin treatment. Rifaximin alters the composition of microbial taxa linked to hepatic/neuropsychological function. | [89,90] |
| Schulz et al., 2019 | A randomized clinical trial | Rifaximin or rifaximin and lactulose in cirrhotic patients with MHE | An improvement in MHE was confirmed after treatment. Microbiological analysis was performed on duodenum and stool samples and no statistically significant changes were found in the bacterial profile. Rifaximin therapy with or without lactulose for 3 months has no effect on microbiome composition. HE improvement with rifaximin persisted after termination. | [91] |
4.2.4. Dietary
5. Challenges and Limitations
6. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AASLD | American Association for the Study of Liver Diseases |
| AMP | Antimicrobial peptide |
| AHE | Acute episode of overt hepatic encephalopathy |
| EASL | European Association for the Study of the Liver |
| FMT | Fecal microbiota transplantation |
| GABA | γ-aminobutyric acid |
| HCC | hepatocellular carcinoma |
| HE | Hepatic encephalopathy |
| LBP | Lipopolysaccharide-binding protein |
| LGG | Lactobacillus rhamnosus GG |
| LPS | Lipopolysaccharide |
| MELD | Model for End-Stage Liver Disease |
| MHE | Minimal hepatic encephalopathy |
| OCTT | Orocecal transit time |
| OHE | Overt hepatic encephalopathy |
| PAMPs | Pathogen-associated molecular patterns |
| SIBO | Small intestinal bacterial overgrowth |
| SOC | Standard of care |
References
- Vilstrup, H.; Amodio, P.; Bajaj, J.; Cordoba, J.; Ferenci, P.; Mullen, K.D.; Weissenborn, K.; Wong, P. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 2014, 60, 715–735. [Google Scholar] [CrossRef]
- Dhiman, R.K.; Saraswat, V.A.; Sharma, B.K.; Sarin, S.K.; Chawla, Y.K.; Butterworth, R.; Duseja, A.; Aggarwal, R.; Amarapurkar, D.; Sharma, P.; et al. Minimal hepatic encephalopathy: Consensus statement of a working party of the Indian National Association for Study of the Liver. J. Gastroenterol. Hepatol. 2010, 25, 1029–1041. [Google Scholar] [CrossRef]
- Prasad, S.; Dhiman, R.K.; Duseja, A.; Chawla, Y.K.; Sharma, A.; Agarwal, R. Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology 2007, 45, 549–559. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Gillevet, P.M.; Patel, N.R.; Ahluwalia, V.; Ridlon, J.M.; Kettenmann, B.; Schubert, C.M.; Sikaroodi, M.; Heuman, D.M.; Crossey, M.M.; et al. A longitudinal systems biology analysis of lactulose withdrawal in hepatic encephalopathy. Metab. Brain Dis. 2012, 27, 205–215. [Google Scholar] [CrossRef]
- Dhiman, R.K. Gut microbiota, inflammation and hepatic encephalopathy: A puzzle with a solution in sight. J. Clin. Exp. Hepatol. 2012, 2, 207–210. [Google Scholar] [CrossRef]
- Quigley, E.M.; Stanton, C.; Murphy, E.F. The gut microbiota and the liver. Pathophysiological and clinical implications. J. Hepatol. 2013, 58, 1020–1027. [Google Scholar] [CrossRef]
- Bajaj, J.S. The role of microbiota in hepatic encephalopathy. Gut Microbes 2014, 5, 397–403. [Google Scholar] [CrossRef]
- Sturgeon, J.A.; Darnall, B.D.; Kao, M.C.; Mackey, S.C. Physical and psychological correlates of fatigue and physical function: A Collaborative Health Outcomes Information Registry (CHOIR) study. J. Pain 2015, 16, 291–298.e1. [Google Scholar] [CrossRef]
- Guarner, F.; Malagelada, J.R. Gut flora in health and disease. Lancet 2003, 361, 512–519. [Google Scholar] [CrossRef]
- Bajaj, J.S. Review article: The modern management of hepatic encephalopathy. Aliment. Pharmacol. Ther. 2010, 31, 537–547. [Google Scholar] [CrossRef]
- Amodio, P.; Bemeur, C.; Butterworth, R.; Cordoba, J.; Kato, A.; Montagnese, S.; Uribe, M.; Vilstrup, H.; Morgan, M.Y. The nutritional management of hepatic encephalopathy in patients with cirrhosis: International Society for Hepatic Encephalopathy and Nitrogen Metabolism Consensus. Hepatology 2013, 58, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Duan, Z.P.; Ha, D.K.; Bengmark, S.; Kurtovic, J.; Riordan, S.M. Synbiotic modulation of gut flora: Effect on minimal hepatic encephalopathy in patients with cirrhosis. Hepatology 2004, 39, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Marlicz, W.; Wunsch, E.; Mydlowska, M.; Milkiewicz, M.; Serwin, K.; Mularczyk, M.; Milkiewicz, P.; Raszeja-Wyszomirska, J. The effect of short term treatment with probiotic VSL#3 on various clinical and biochemical parameters in patients with liver cirrhosis. J. Physiol. Pharmacol. 2016, 67, 867–877. [Google Scholar] [PubMed]
- Hassanein, T.I.; Tofteng, F.; Brown, R.S., Jr.; McGuire, B.; Lynch, P.; Mehta, R.; Larsen, F.S.; Gornbein, J.; Stange, J.; Blei, A.T. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology 2007, 46, 1853–1862. [Google Scholar] [CrossRef] [PubMed]
- Pazgan-Simon, M.; Zuwala-Jagiello, J.; Serafinska, S.; Simon, K. Nutrition principles and recommendations in different types of hepatic encephalopathy. Clin. Exp. Hepatol. 2016, 1, 121–126. [Google Scholar] [CrossRef]
- Cho, I.; Blaser, M.J. The human microbiome: At the interface of health and disease. Nat. Rev. Genet. 2012, 13, 260–270. [Google Scholar] [CrossRef]
- Backhed, F.; Ding, H.; Wang, T.; Hooper, L.V.; Koh, G.Y.; Nagy, A.; Semenkovich, C.F.; Gordon, J.I. The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl. Acad. Sci. USA 2004, 101, 15718–15723. [Google Scholar] [CrossRef]
- Lynch, S.V.; Pedersen, O. The Human Intestinal Microbiome in Health and Disease. N. Engl. J. Med. 2016, 375, 2369–2379. [Google Scholar] [CrossRef]
- Zeuzem, S. Gut-liver axis. Int. J. Colorectal. Dis. 2000, 15, 59–82. [Google Scholar] [CrossRef]
- Ridlon, J.M.; Alves, J.M.; Hylemon, P.B.; Bajaj, J.S. Cirrhosis, bile acids and gut microbiota: Unraveling a complex relationship. Gut Microbes 2013, 4, 382–387. [Google Scholar] [CrossRef]
- Butterworth, R.F. Hepatic encephalopathy: A central neuroinflammatory disorder? Hepatology 2011, 53, 1372–1376. [Google Scholar] [CrossRef] [PubMed]
- Shawcross, D.L.; Wright, G.; Olde Damink, S.W.; Jalan, R. Role of ammonia and inflammation in minimal hepatic encephalopathy. Metab. Brain Dis. 2007, 22, 125–138. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Heuman, D.M.; Hylemon, P.B.; Sanyal, A.J.; White, M.B.; Monteith, P.; Noble, N.A.; Unser, A.B.; Daita, K.; Fisher, A.R.; et al. Altered profile of human gut microbiome is associated with cirrhosis and its complications. J. Hepatol. 2014, 60, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, Y.; Zhang, X.; Liu, J.; Zhang, Q.; Zhao, Y.; Peng, J.; Feng, Q.; Dai, J.; Sun, S.; et al. Gut Microbial Dysbiosis Is Associated with Altered Hepatic Functions and Serum Metabolites in Chronic Hepatitis B Patients. Front. Microbiol. 2017, 8, 2222. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Thacker, L.R.; Fagan, A.; White, M.B.; Gavis, E.A.; Hylemon, P.B.; Brown, R.; Acharya, C.; Heuman, D.M.; Fuchs, M.; et al. Gut microbial RNA and DNA analysis predicts hospitalizations in cirrhosis. JCI Insight 2018, 3, e98019. [Google Scholar] [CrossRef]
- D’Amico, G.; Morabito, A.; Pagliaro, L.; Marubini, E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig. Dis. Sci. 1986, 31, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Ding, A.; Lee, A.; Callender, M.; Loughrey, M.; Quah, S.P.; Dinsmore, W.W. Hepatic encephalopathy as an unusual late complication of transjugular intrahepatic portosystemic shunt insertion for non-cirrhotic portal hypertension caused by nodular regenerative hyperplasia in an HIV-positive patient on highly active antiretroviral therapy. Int. J. STD AIDS 2010, 21, 71–72. [Google Scholar] [CrossRef]
- Butterworth, R.F. Role of circulating neurotoxins in the pathogenesis of hepatic encephalopathy: Potential for improvement following their removal by liver assist devices. Liver Int. 2003, 23 (Suppl. 3), 5–9. [Google Scholar] [CrossRef]
- Cornberg, M.; Tacke, F.; Karlsen, T.H.; European Association for the Study of the Liver. Clinical Practice Guidelines of the European Association for the study of the Liver—Advancing methodology but preserving practicability. J. Hepatol. 2019, 70, 5–7. [Google Scholar] [CrossRef]
- Tajiri, K.; Shimizu, Y. Branched-chain amino acids in liver diseases. Transl. Gastroenterol. Hepatol. 2018, 3, 47. [Google Scholar] [CrossRef]
- Acharya, C.; Bajaj, J.S. Altered Microbiome in Patients with Cirrhosis and Complications. Clin. Gastroenterol. Hepatol. 2019, 17, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Fiati Kenston, S.S.; Song, X.; Li, Z.; Zhao, J. Mechanistic insight, diagnosis, and treatment of ammonia-induced hepatic encephalopathy. J. Gastroenterol. Hepatol. 2019, 34, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Aldridge, D.R.; Tranah, E.J.; Shawcross, D.L. Pathogenesis of hepatic encephalopathy: Role of ammonia and systemic inflammation. J. Clin. Exp. Hepatol. 2015, 5, S7–S20. [Google Scholar] [CrossRef] [PubMed]
- Wijdicks, E.F. Hepatic Encephalopathy. N. Engl. J. Med. 2016, 375, 1660–1670. [Google Scholar] [CrossRef]
- Levitt, D.G.; Levitt, M.D. A model of blood-ammonia homeostasis based on a quantitative analysis of nitrogen metabolism in the multiple organs involved in the production, catabolism, and excretion of ammonia in humans. Clin. Exp. Gastroenterol. 2018, 11, 193–215. [Google Scholar] [CrossRef]
- Sawhney, R.; Jalan, R. Liver: The gut is a key target of therapy in hepatic encephalopathy. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 7–8. [Google Scholar] [CrossRef]
- Wierling, C. Bridging the gap between metabolic liver processes and functional tissue structure by integrated spatiotemporal modeling applied to hepatic ammonia detoxification. Hepatology 2014, 60, 1823–1825. [Google Scholar] [CrossRef]
- Mitchell, S.; Ellingson, C.; Coyne, T.; Hall, L.; Neill, M.; Christian, N.; Higham, C.; Dobrowolski, S.F.; Tuchman, M.; Summar, M.; et al. Genetic variation in the urea cycle: A model resource for investigating key candidate genes for common diseases. Hum. Mutat. 2009, 30, 56–60. [Google Scholar] [CrossRef]
- Fleming, K.E.; Wanless, I.R. Glutamine synthetase expression in activated hepatocyte progenitor cells and loss of hepatocellular expression in congestion and cirrhosis. Liver Int. 2013, 33, 525–534. [Google Scholar] [CrossRef]
- Hansen, B.A.; Vilstrup, H. Increased intestinal hydrolysis of urea in patients with alcoholic cirrhosis. Scand. J. Gastroenterol. 1985, 20, 346–350. [Google Scholar] [CrossRef]
- Blei, A.T. Portal hypertension and its complications. Curr. Opin. Gastroenterol. 2007, 23, 275–282. [Google Scholar] [CrossRef] [PubMed]
- De Franchis, R.; Baveno, V.I.F. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J. Hepatol. 2015, 63, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Takefuta, K.; Senzaki, H.; Shimabukuro, A.; Nishibata, M.; Sato, S.; Nakayashiro, M. Portosystemic shunt with hyperammonemia and high cardiac output as a complication after Fontan surgery. J. Cardiol. Cases 2021, 23, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Ohnishi, K.; Sato, S.; Saito, M.; Terabayashi, H.; Nakayama, T.; Saito, M.; Chin, N.; Iida, S.; Nomura, F.; Okuda, K. Clinical and portal hemodynamic features in cirrhotic patients having a large spontaneous splenorenal and/or gastrorenal shunt. Am. J. Gastroenterol. 1986, 81, 450–455. [Google Scholar]
- Haussinger, D.; Kircheis, G.; Fischer, R.; Schliess, F.; Vom Dahl, S. Hepatic encephalopathy in chronic liver disease: A clinical manifestation of astrocyte swelling and low-grade cerebral edema? J. Hepatol. 2000, 32, 1035–1038. [Google Scholar] [CrossRef]
- Jover, R.; Rodrigo, R.; Felipo, V.; Insausti, R.; Saez-Valero, J.; Garcia-Ayllon, M.S.; Suarez, I.; Candela, A.; Compan, A.; Esteban, A.; et al. Brain edema and inflammatory activation in bile duct ligated rats with diet-induced hyperammonemia: A model of hepatic encephalopathy in cirrhosis. Hepatology 2006, 43, 1257–1266. [Google Scholar] [CrossRef]
- Gorg, B.; Schliess, F.; Haussinger, D. Osmotic and oxidative/nitrosative stress in ammonia toxicity and hepatic encephalopathy. Arch. Biochem. Biophys. 2013, 536, 158–163. [Google Scholar] [CrossRef]
- Raabe, W. Effects of hyperammonemia on neuronal function: NH4+, IPSP and Cl(−)-extrusion. Adv. Exp. Med. Biol. 1993, 341, 71–82. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Hylemon, P.B.; Ridlon, J.M.; Heuman, D.M.; Daita, K.; White, M.B.; Monteith, P.; Noble, N.A.; Sikaroodi, M.; Gillevet, P.M. Colonic mucosal microbiome differs from stool microbiome in cirrhosis and hepatic encephalopathy and is linked to cognition and inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 303, G675–G685. [Google Scholar] [CrossRef]
- Gupta, A.; Dhiman, R.K.; Kumari, S.; Rana, S.; Agarwal, R.; Duseja, A.; Chawla, Y. Role of small intestinal bacterial overgrowth and delayed gastrointestinal transit time in cirrhotic patients with minimal hepatic encephalopathy. J. Hepatol. 2010, 53, 849–855. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Betrapally, N.S.; Hylemon, P.B.; Heuman, D.M.; Daita, K.; White, M.B.; Unser, A.; Thacker, L.R.; Sanyal, A.J.; Kang, D.J.; et al. Salivary microbiota reflects changes in gut microbiota in cirrhosis with hepatic encephalopathy. Hepatology 2015, 62, 1260–1271. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Heuman, D.M.; Hylemon, P.B.; Sanyal, A.J.; Puri, P.; Sterling, R.K.; Luketic, V.; Stravitz, R.T.; Siddiqui, M.S.; Fuchs, M.; et al. Randomised clinical trial: Lactobacillus GG modulates gut microbiome, metabolome and endotoxemia in patients with cirrhosis. Aliment. Pharmacol. Ther. 2014, 39, 1113–1125. [Google Scholar] [CrossRef] [PubMed]
- Dhiman, R.K.; Rana, B.; Agrawal, S.; Garg, A.; Chopra, M.; Thumburu, K.K.; Khattri, A.; Malhotra, S.; Duseja, A.; Chawla, Y.K. Probiotic VSL#3 reduces liver disease severity and hospitalization in patients with cirrhosis: A randomized, controlled trial. Gastroenterology 2014, 147, 1327–1337.e3. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Kassam, Z.; Fagan, A.; Gavis, E.A.; Liu, E.; Cox, I.J.; Kheradman, R.; Heuman, D.; Wang, J.; Gurry, T.; et al. Fecal microbiota transplant from a rational stool donor improves hepatic encephalopathy: A randomized clinical trial. Hepatology 2017, 66, 1727–1738. [Google Scholar] [CrossRef] [PubMed]
- Gluud, L.L.; Vilstrup, H.; Morgan, M.Y. Non-absorbable disaccharides versus placebo/no intervention and lactulose versus lactitol for the prevention and treatment of hepatic encephalopathy in people with cirrhosis. Cochrane Database Syst. Rev. 2016, 4, CD003044. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Wade, J.B.; Sanyal, A.J. Spectrum of neurocognitive impairment in cirrhosis: Implications for the assessment of hepatic encephalopathy. Hepatology 2009, 50, 2014–2021. [Google Scholar] [CrossRef]
- Montagnese, S.; Amodio, P.; Morgan, M.Y. Methods for diagnosing hepatic encephalopathy in patients with cirrhosis: A multidimensional approach. Metab. Brain Dis. 2004, 19, 281–312. [Google Scholar] [CrossRef]
- Ferenci, P. Hepatic encephalopathy. Gastroenterol. Rep. 2017, 5, 138–147. [Google Scholar] [CrossRef]
- Guerit, J.M.; Amantini, A.; Fischer, C.; Kaplan, P.W.; Mecarelli, O.; Schnitzler, A.; Ubiali, E.; Amodio, P.; members of the I.c.N.I. Neurophysiological investigations of hepatic encephalopathy: ISHEN practice guidelines. Liver Int. 2009, 29, 789–796. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Riggio, O.; Allampati, S.; Prakash, R.; Gioia, S.; Onori, E.; Piazza, N.; Noble, N.A.; White, M.B.; Mullen, K.D. Cognitive dysfunction is associated with poor socioeconomic status in patients with cirrhosis: An international multicenter study. Clin. Gastroenterol. Hepatol. 2013, 11, 1511–1516. [Google Scholar] [CrossRef]
- Ridola, L.; Nardelli, S.; Gioia, S.; Riggio, O. Quality of life in patients with minimal hepatic encephalopathy. World J. Gastroenterol. 2018, 24, 5446–5453. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Pinkerton, S.D.; Sanyal, A.J.; Heuman, D.M. Diagnosis and treatment of minimal hepatic encephalopathy to prevent motor vehicle accidents: A cost-effectiveness analysis. Hepatology 2012, 55, 1164–1171. [Google Scholar] [CrossRef] [PubMed]
- Wallace, T.C.; Guarner, F.; Madsen, K.; Cabana, M.D.; Gibson, G.; Hentges, E.; Sanders, M.E. Human gut microbiota and its relationship to health and disease. Nutr. Rev. 2011, 69, 392–403. [Google Scholar] [CrossRef]
- Goodrich, J.K.; Di Rienzi, S.C.; Poole, A.C.; Koren, O.; Walters, W.A.; Caporaso, J.G.; Knight, R.; Ley, R.E. Conducting a microbiome study. Cell 2014, 158, 250–262. [Google Scholar] [CrossRef] [PubMed]
- Saboo, K.; Petrakov, N.V.; Shamsaddini, A.; Fagan, A.; Gavis, E.A.; Sikaroodi, M.; McGeorge, S.; Gillevet, P.M.; Iyer, R.K.; Bajaj, J.S. Stool microbiota are superior to saliva in distinguishing cirrhosis and hepatic encephalopathy using machine learning. J. Hepatol. 2022, 76, 600–607. [Google Scholar] [CrossRef] [PubMed]
- Sung, C.M.; Lin, Y.F.; Chen, K.F.; Ke, H.M.; Huang, H.Y.; Gong, Y.N.; Tsai, W.S.; You, J.F.; Lu, M.J.; Cheng, H.T.; et al. Predicting Clinical Outcomes of Cirrhosis Patients with Hepatic Encephalopathy from the Fecal Microbiome. Cell Mol. Gastroenterol. Hepatol. 2019, 8, 301–318.E2. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhai, H.; Geng, J.; Yu, R.; Ren, H.; Fan, H.; Shi, P. Large-scale survey of gut microbiota associated with MHE Via 16S rRNA-based pyrosequencing. Am. J. Gastroenterol. 2013, 108, 1601–1611. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Ridlon, J.M.; Hylemon, P.B.; Thacker, L.R.; Heuman, D.M.; Smith, S.; Sikaroodi, M.; Gillevet, P.M. Linkage of gut microbiome with cognition in hepatic encephalopathy. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 302, G168–G175. [Google Scholar] [CrossRef]
- Xia, X.; Chen, J.; Xia, J.; Wang, B.; Liu, H.; Yang, L.; Wang, Y.; Ling, Z. Role of probiotics in the treatment of minimal hepatic encephalopathy in patients with HBV-induced liver cirrhosis. J. Int. Med. Res. 2018, 46, 3596–3604. [Google Scholar] [CrossRef]
- Lunia, M.K.; Sharma, B.C.; Sharma, P.; Sachdeva, S.; Srivastava, S. Probiotics prevent hepatic encephalopathy in patients with cirrhosis: A randomized controlled trial. Clin. Gastroenterol. Hepatol. 2014, 12, 1003–1008.E1. [Google Scholar] [CrossRef]
- Moratalla, A.; Ampuero, J.; Bellot, P.; Gallego-Duran, R.; Zapater, P.; Roger, M.; Figueruela, B.; Martinez-Moreno, B.; Gonzalez-Navajas, J.M.; Such, J.; et al. Lactulose reduces bacterial DNA translocation, which worsens neurocognitive shape in cirrhotic patients with minimal hepatic encephalopathy. Liver Int. 2017, 37, 212–223. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.Y.; Bajaj, J.S.; Wang, J.B.; Shang, J.; Zhou, X.M.; Guo, X.L.; Zhu, X.; Meng, L.N.; Jiang, H.X.; Mi, Y.Q.; et al. Lactulose improves cognition, quality of life, and gut microbiota in minimal hepatic encephalopathy: A multicenter, randomized controlled trial. J. Dig. Dis. 2019, 20, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Woodhouse, C.A.; Patel, V.C.; Singanayagam, A.; Shawcross, D.L. Review article: The gut microbiome as a therapeutic target in the pathogenesis and treatment of chronic liver disease. Aliment. Pharmacol. Ther. 2018, 47, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Malaguarnera, M.; Gargante, M.P.; Malaguarnera, G.; Salmeri, M.; Mastrojeni, S.; Rampello, L.; Pennisi, G.; Li Volti, G.; Galvano, F. Bifidobacterium combined with fructo-oligosaccharide versus lactulose in the treatment of patients with hepatic encephalopathy. Eur. J. Gastroenterol. Hepatol. 2010, 22, 199–206. [Google Scholar] [CrossRef]
- Vindigni, S.M.; Surawicz, C.M. Fecal Microbiota Transplantation. Gastroenterol. Clin. N. Am. 2017, 46, 171–185. [Google Scholar] [CrossRef]
- Wang, W.W.; Zhang, Y.; Huang, X.B.; You, N.; Zheng, L.; Li, J. Fecal microbiota transplantation prevents hepatic encephalopathy in rats with carbon tetrachloride-induced acute hepatic dysfunction. World J. Gastroenterol. 2017, 23, 6983–6994. [Google Scholar] [CrossRef]
- Kao, D.; Roach, B.; Park, H.; Hotte, N.; Madsen, K.; Bain, V.; Tandon, P. Fecal microbiota transplantation in the management of hepatic encephalopathy. Hepatology 2016, 63, 339–340. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Salzman, N.H.; Acharya, C.; Sterling, R.K.; White, M.B.; Gavis, E.A.; Fagan, A.; Hayward, M.; Holtz, M.L.; Matherly, S.; et al. Fecal Microbial Transplant Capsules Are Safe in Hepatic Encephalopathy: A Phase 1, Randomized, Placebo-Controlled Trial. Hepatology 2019, 70, 1690–1703. [Google Scholar] [CrossRef]
- Bloom, P.P.; Donlan, J.; Torres Soto, M.; Daidone, M.; Hohmann, E.; Chung, R.T. Fecal microbiota transplant improves cognition in hepatic encephalopathy and its effect varies by donor and recipient. Hepatol. Commun. 2022, 6, 2079–2089. [Google Scholar] [CrossRef]
- Patidar, K.R.; Bajaj, J.S. Antibiotics for the treatment of hepatic encephalopathy. Metab. Brain Dis. 2013, 28, 307–312. [Google Scholar] [CrossRef]
- Zhang, S.; Chen, D.C. Facing a new challenge: The adverse effects of antibiotics on gut microbiota and host immunity. Chin. Med. J. 2019, 132, 1135–1138. [Google Scholar] [CrossRef] [PubMed]
- Rose, C.F.; Amodio, P.; Bajaj, J.S.; Dhiman, R.K.; Montagnese, S.; Taylor-Robinson, S.D.; Vilstrup, H.; Jalan, R. Hepatic encephalopathy: Novel insights into classification, pathophysiology and therapy. J. Hepatol. 2020, 73, 1526–1547. [Google Scholar] [CrossRef] [PubMed]
- Bass, N.M.; Mullen, K.D.; Sanyal, A.; Poordad, F.; Neff, G.; Leevy, C.B.; Sigal, S.; Sheikh, M.Y.; Beavers, K.; Frederick, T.; et al. Rifaximin treatment in hepatic encephalopathy. N. Engl. J. Med. 2010, 362, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Kimer, N.; Krag, A.; Moller, S.; Bendtsen, F.; Gluud, L.L. Systematic review with meta-analysis: The effects of rifaximin in hepatic encephalopathy. Aliment. Pharmacol. Ther. 2014, 40, 123–132. [Google Scholar] [CrossRef]
- Kang, S.H.; Lee, Y.B.; Lee, J.H.; Nam, J.Y.; Chang, Y.; Cho, H.; Yoo, J.J.; Cho, Y.Y.; Cho, E.J.; Yu, S.J.; et al. Rifaximin treatment is associated with reduced risk of cirrhotic complications and prolonged overall survival in patients experiencing hepatic encephalopathy. Aliment. Pharmacol. Ther. 2017, 46, 845–855. [Google Scholar] [CrossRef]
- Kaji, K.; Takaya, H.; Saikawa, S.; Furukawa, M.; Sato, S.; Kawaratani, H.; Kitade, M.; Moriya, K.; Namisaki, T.; Akahane, T.; et al. Rifaximin ameliorates hepatic encephalopathy and endotoxemia without affecting the gut microbiome diversity. World J. Gastroenterol. 2017, 23, 8355–8366. [Google Scholar] [CrossRef]
- Bajaj, J.S.; Heuman, D.M.; Sanyal, A.J.; Hylemon, P.B.; Sterling, R.K.; Stravitz, R.T.; Fuchs, M.; Ridlon, J.M.; Daita, K.; Monteith, P.; et al. Modulation of the metabiome by rifaximin in patients with cirrhosis and minimal hepatic encephalopathy. PLoS ONE 2013, 8, e60042. [Google Scholar] [CrossRef]
- Zuo, Z.; Fan, H.; Tang, X.D.; Chen, Y.M.; Xun, L.T.; Li, Y.; Song, Z.J.; Zhai, H.Q. Effect of different treatments and alcohol addiction on gut microbiota in minimal hepatic encephalopathy patients. Exp. Ther. Med. 2017, 14, 4887–4895. [Google Scholar] [CrossRef]
- Suzuki, K.; Endo, R.; Takikawa, Y.; Moriyasu, F.; Aoyagi, Y.; Moriwaki, H.; Terai, S.; Sakaida, I.; Sakai, Y.; Nishiguchi, S.; et al. Efficacy and safety of rifaximin in Japanese patients with hepatic encephalopathy: A phase II/III, multicenter, randomized, evaluator-blinded, active-controlled trial and a phase III, multicenter, open trial. Hepatol. Res. 2018, 48, 411–423. [Google Scholar] [CrossRef]
- Kawaguchi, T.; Suzuki, F.; Imamura, M.; Murashima, N.; Yanase, M.; Mine, T.; Fujisawa, M.; Sato, I.; Yoshiji, H.; Okita, K.; et al. Rifaximin-altered gut microbiota components associated with liver/neuropsychological functions in patients with hepatic encephalopathy: An exploratory data analysis of phase II/III clinical trials. Hepatol. Res. 2019, 49, 404–418. [Google Scholar] [CrossRef]
- Schulz, C.; Schutte, K.; Vilchez-Vargas, R.; Vasapolli, R.; Malfertheiner, P. Long-Term Effect of Rifaximin with and without Lactulose on the Active Bacterial Assemblages in the Proximal Small Bowel and Faeces in Patients with Minimal Hepatic Encephalopathy. Dig. Dis. 2019, 37, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.J.; Kakiyama, G.; Betrapally, N.S.; Herzog, J.; Nittono, H.; Hylemon, P.B.; Zhou, H.; Carroll, I.; Yang, J.; Gillevet, P.M.; et al. Rifaximin Exerts Beneficial Effects Independent of its Ability to Alter Microbiota Composition. Clin. Transl. Gastroenterol. 2016, 7, e187. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Gao, J.; Gillilland, M., 3rd; Wu, X.; Song, I.; Kao, J.Y.; Owyang, C. Rifaximin alters intestinal bacteria and prevents stress-induced gut inflammation and visceral hyperalgesia in rats. Gastroenterology 2014, 146, 484–496.E4. [Google Scholar] [CrossRef] [PubMed]
- Maccaferri, S.; Vitali, B.; Klinder, A.; Kolida, S.; Ndagijimana, M.; Laghi, L.; Calanni, F.; Brigidi, P.; Gibson, G.R.; Costabile, A. Rifaximin modulates the colonic microbiota of patients with Crohn’s disease: An in vitro approach using a continuous culture colonic model system. J. Antimicrob. Chemother. 2010, 65, 2556–2565. [Google Scholar] [CrossRef]
- Riggio, O.; Ridola, L.; Pasquale, C. Hepatic encephalopathy therapy: An overview. World J. Gastrointest. Pharmacol. Ther. 2010, 1, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Campion, D.; Giovo, I.; Ponzo, P.; Saracco, G.M.; Balzola, F.; Alessandria, C. Dietary approach and gut microbiota modulation for chronic hepatic encephalopathy in cirrhosis. World J. Hepatol. 2019, 11, 489–512. [Google Scholar] [CrossRef]
- Fan, Y.; Pedersen, O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 2021, 19, 55–71. [Google Scholar] [CrossRef]
- Merli, M.; Iebba, V.; Giusto, M. What is new about diet in hepatic encephalopathy. Metab. Brain Dis. 2016, 31, 1289–1294. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J. Hepatol. 2019, 70, 172–193. [Google Scholar] [CrossRef]
- Summerskill, W.H.; Wolfe, S.J.; Davidson, C.S. The management of hepatic coma in relation to protein withdrawal and certain specific measures. Am. J. Med. 1957, 23, 59–76. [Google Scholar] [CrossRef]
- Cordoba, J.; Lopez-Hellin, J.; Planas, M.; Sabin, P.; Sanpedro, F.; Castro, F.; Esteban, R.; Guardia, J. Normal protein diet for episodic hepatic encephalopathy: Results of a randomized study. J. Hepatol. 2004, 41, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Campollo, O.; Sprengers, D.; Dam, G.; Vilstrup, H.; McIntyre, N. Protein tolerance to standard and high protein meals in patients with liver cirrhosis. World J. Hepatol. 2017, 9, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Taniguchi, E.; Sata, M. Effects of oral branched-chain amino acids on hepatic encephalopathy and outcome in patients with liver cirrhosis. Nutr. Clin. Pract. 2013, 28, 580–588. [Google Scholar] [CrossRef]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schutz, T.; Bischoff, S.C. ESPEN guideline on clinical nutrition in liver disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef] [PubMed]
- Fassarella, M.; Blaak, E.E.; Penders, J.; Nauta, A.; Smidt, H.; Zoetendal, E.G. Gut microbiome stability and resilience: Elucidating the response to perturbations in order to modulate gut health. Gut 2021, 70, 595–605. [Google Scholar] [CrossRef]
- Fukui, H. Role of Gut Dysbiosis in Liver Diseases: What Have We Learned So Far? Diseases 2019, 7, 58. [Google Scholar] [CrossRef]
- Ohtani, N.; Kawada, N. Role of the Gut-Liver Axis in Liver Inflammation, Fibrosis, and Cancer: A Special Focus on the Gut Microbiota Relationship. Hepatol. Commun. 2019, 3, 456–470. [Google Scholar] [CrossRef]
- Mohajeri, M.H.; Brummer, R.J.M.; Rastall, R.A.; Weersma, R.K.; Harmsen, H.J.M.; Faas, M.; Eggersdorfer, M. The role of the microbiome for human health: From basic science to clinical applications. Eur. J. Nutr. 2018, 57, 1–14. [Google Scholar] [CrossRef]
- Sbahi, H.; Di Palma, J.A. Faecal microbiota transplantation: Applications and limitations in treating gastrointestinal disorders. BMJ Open Gastroenterol. 2016, 3, e000087. [Google Scholar] [CrossRef]
- Zellmer, C.; Sater, M.R.A.; Huntley, M.H.; Osman, M.; Olesen, S.W.; Ramakrishna, B. Shiga Toxin-Producing Escherichia coli Transmission via Fecal Microbiota Transplant. Clin. Infect. Dis. 2021, 72, e876–e880. [Google Scholar] [CrossRef]
- DeFilipp, Z.; Bloom, P.P.; Torres Soto, M.; Mansour, M.K.; Sater, M.R.A.; Huntley, M.H.; Turbett, S.; Chung, R.T.; Chen, Y.B.; Hohmann, E.L. Drug-Resistant E. coli Bacteremia Transmitted by Fecal Microbiota Transplant. N. Engl. J. Med. 2019, 381, 2043–2050. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.C.; Yang, Y.S. Fecal microbiota transplantation: Current status and challenges in China. JGH Open 2018, 2, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, J.; Prado, V.; Trebicka, J.; Amoros, A.; Gustot, T.; Wiest, R.; Deulofeu, C.; Garcia, E.; Acevedo, J.; Fuhrmann, V.; et al. Multidrug-resistant bacterial infections in patients with decompensated cirrhosis and with acute-on-chronic liver failure in Europe. J. Hepatol. 2019, 70, 398–411. [Google Scholar] [CrossRef] [PubMed]
- Caraceni, P.; Vargas, V.; Sola, E.; Alessandria, C.; De Wit, K.; Trebicka, J.; Angeli, P.; Mookerjee, R.P.; Durand, F.; Pose, E.; et al. The Use of Rifaximin in Patients with Cirrhosis. Hepatology 2021, 74, 1660–1673. [Google Scholar] [CrossRef]
- Kircheis, G.; Nilius, R.; Held, C.; Berndt, H.; Buchner, M.; Gortelmeyer, R.; Hendricks, R.; Kruger, B.; Kuklinski, B.; Meister, H.; et al. Therapeutic efficacy of L-ornithine-L-aspartate infusions in patients with cirrhosis and hepatic encephalopathy: Results of a placebo-controlled, double-blind study. Hepatology 1997, 25, 1351–1360. [Google Scholar] [CrossRef]
- Stauch, S.; Kircheis, G.; Adler, G.; Beckh, K.; Ditschuneit, H.; Gortelmeyer, R.; Hendricks, R.; Heuser, A.; Karoff, C.; Malfertheiner, P.; et al. Oral L-ornithine-L-aspartate therapy of chronic hepatic encephalopathy: Results of a placebo-controlled double-blind study. J. Hepatol. 1998, 28, 856–864. [Google Scholar] [CrossRef]
- Poo, J.L.; Gongora, J.; Sanchez-Avila, F.; Aguilar-Castillo, S.; Garcia-Ramos, G.; Fernandez-Zertuche, M.; Rodriguez-Fragoso, L.; Uribe, M. Efficacy of oral L-ornithine-L-aspartate in cirrhotic patients with hyperammonemic hepatic encephalopathy. Results of a randomized, lactulose-controlled study. Ann. Hepatol. 2006, 5, 281–288. [Google Scholar] [CrossRef]
- Jalan, R.; Wright, G.; Davies, N.A.; Hodges, S.J. L-Ornithine phenylacetate (OP): A novel treatment for hyperammonemia and hepatic encephalopathy. Med. Hypotheses 2007, 69, 1064–1069. [Google Scholar] [CrossRef]
- Efrati, C.; Masini, A.; Merli, M.; Valeriano, V.; Riggio, O. Effect of sodium benzoate on blood ammonia response to oral glutamine challenge in cirrhotic patients: A note of caution. Am. J. Gastroenterol. 2000, 95, 3574–3578. [Google Scholar] [CrossRef]
- Spann, A.; Yasodhara, A.; Kang, J.; Watt, K.; Wang, B.; Goldenberg, A.; Bhat, M. Applying Machine Learning in Liver Disease and Transplantation: A Comprehensive Review. Hepatology 2020, 71, 1093–1105. [Google Scholar] [CrossRef]
- Guarner, C.; Soriano, G. Bacterial translocation and its consequences in patients with cirrhosis. Eur. J. Gastroenterol. Hepatol. 2005, 17, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Scheline, R.R. Metabolism of foreign compounds by gastrointestinal microorganisms. Pharmacol. Rev. 1973, 25, 451–523. [Google Scholar] [PubMed]
- Scheline, R.R. Drug metabolism by intestinal microorganisms. J. Pharm. Sci. 1968, 57, 2021–2037. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Wang, B.; Zhang, M.; Rantalainen, M.; Wang, S.; Zhou, H.; Zhang, Y.; Shen, J.; Pang, X.; Zhang, M.; et al. Symbiotic gut microbes modulate human metabolic phenotypes. Proc. Natl. Acad. Sci. USA 2008, 105, 2117–2122. [Google Scholar] [CrossRef] [PubMed]
- Rubio, T.; Felipo, V.; Tarazona, S.; Pastorelli, R.; Escudero-Garcia, D.; Tosca, J.; Urios, A.; Conesa, A.; Montoliu, C. Multi-omic analysis unveils biological pathways in peripheral immune system associated to minimal hepatic encephalopathy appearance in cirrhotic patients. Sci. Rep. 2021, 11, 1907. [Google Scholar] [CrossRef]
- Turnbaugh, P.J.; Ley, R.E.; Mahowald, M.A.; Magrini, V.; Mardis, E.R.; Gordon, J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006, 444, 1027–1031. [Google Scholar] [CrossRef]
- Nicholson, J.K. Global systems biology, personalized medicine and molecular epidemiology. Mol. Syst. Biol. 2006, 2, 52. [Google Scholar] [CrossRef]
- Gazda, J.; Drotar, P.; Drazilova, S.; Gazda, J.; Gazda, M.; Janicko, M.; Jarcuska, P. Artificial Intelligence and Its Application to Minimal Hepatic Encephalopathy Diagnosis. J. Pers. Med. 2021, 11, 1090. [Google Scholar] [CrossRef]
- Chen, H.J.; Chen, R.; Yang, M.; Teng, G.J.; Herskovits, E.H. Identification of minimal hepatic encephalopathy in patients with cirrhosis based on white matter imaging and Bayesian data mining. AJNR Am. J. Neuroradiol. 2015, 36, 481–487. [Google Scholar] [CrossRef]
- Chen, Q.F.; Zou, T.X.; Yang, Z.T.; Chen, H.J. Identification of patients with and without minimal hepatic encephalopathy based on gray matter volumetry using a support vector machine learning algorithm. Sci. Rep. 2020, 10, 2490. [Google Scholar] [CrossRef]
- Yang, H.; Li, X.; Cao, H.; Cui, Y.; Luo, Y.; Liu, J.; Zhang, Y. Using machine learning methods to predict hepatic encephalopathy in cirrhotic patients with unbalanced data. Comput. Methods Programs Biomed. 2021, 211, 106420. [Google Scholar] [CrossRef] [PubMed]
- Franzosa, E.A.; Huang, K.; Meadow, J.F.; Gevers, D.; Lemon, K.P.; Bohannan, B.J.; Huttenhower, C. Identifying personal microbiomes using metagenomic codes. Proc. Natl. Acad. Sci. USA 2015, 112, E2930–E2938. [Google Scholar] [CrossRef] [PubMed]
- Bloom, P.P.; Tapper, E.B.; Young, V.B.; Lok, A.S. Microbiome therapeutics for hepatic encephalopathy. J. Hepatol. 2021, 75, 1452–1464. [Google Scholar] [CrossRef] [PubMed]
| Author | Scheme | Group | Result | Ref. |
|---|---|---|---|---|
| Bajaj et al., 2017 | An open-label, randomized clinical trial | FMT or SOC alone in Cirrhotic patients with recurrent HE on SOC | FMT resulted in cognitive improvement and reduced dysbiosis in cirrhotic patients with recurrent HE. | [54] |
| Kao et al., 2016 | A case report | 57-year-old man suffering from grade 1–2 HE with liver cirrhosis | Cognitive function improvement was confirmed as a result of evaluation of Stroop test and inhibitory control test after continuous FMT in patients with mild HE. | [77] |
| Bajaj et al., 2019 | A randomized clinical phase 1, placebo-controlled trial | FMT capsules or placebo in Cirrhotic patients with recurrent HE | Oral FMT capsules have demonstrated safety and tolerability in patients with cirrhosis and recurrent HE. Oral FMT capsules improved duodenal mucosal diversity, dysbiosis and AMP expression and reduced serum LBP. | [78] |
| Bloom et al., 2022 | A randomized clinical phase 2, trial | 10 Overt HE patients (five FMT donors) | There was no change in MELD scores. After FMT, the psychometric HE score improved. In stool analysis of FMT responders, the levels of Bifidobacterium and beneficial taxa were high. 13 minor adverse events and one serious adverse event were reported. The effect varied according to the difference between donor and recipient. | [79] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Won, S.-M.; Oh, K.K.; Gupta, H.; Ganesan, R.; Sharma, S.P.; Jeong, J.-J.; Yoon, S.J.; Jeong, M.K.; Min, B.H.; Hyun, J.Y.; et al. The Link between Gut Microbiota and Hepatic Encephalopathy. Int. J. Mol. Sci. 2022, 23, 8999. https://doi.org/10.3390/ijms23168999
Won S-M, Oh KK, Gupta H, Ganesan R, Sharma SP, Jeong J-J, Yoon SJ, Jeong MK, Min BH, Hyun JY, et al. The Link between Gut Microbiota and Hepatic Encephalopathy. International Journal of Molecular Sciences. 2022; 23(16):8999. https://doi.org/10.3390/ijms23168999
Chicago/Turabian StyleWon, Sung-Min, Ki Kwang Oh, Haripriya Gupta, Raja Ganesan, Satya Priya Sharma, Jin-Ju Jeong, Sang Jun Yoon, Min Kyo Jeong, Byeong Hyun Min, Ji Ye Hyun, and et al. 2022. "The Link between Gut Microbiota and Hepatic Encephalopathy" International Journal of Molecular Sciences 23, no. 16: 8999. https://doi.org/10.3390/ijms23168999
APA StyleWon, S.-M., Oh, K. K., Gupta, H., Ganesan, R., Sharma, S. P., Jeong, J.-J., Yoon, S. J., Jeong, M. K., Min, B. H., Hyun, J. Y., Park, H. J., Eom, J. A., Lee, S. B., Cha, M. G., Kwon, G. H., Choi, M. R., Kim, D. J., & Suk, K. T. (2022). The Link between Gut Microbiota and Hepatic Encephalopathy. International Journal of Molecular Sciences, 23(16), 8999. https://doi.org/10.3390/ijms23168999









